Abstract
Introduction
People living with HIV (PLWH) on antiretroviral therapy (ART) do not progress to AIDS. However, they still suffer from an increased risk of inflammation-associated complications. HIV persists in long-lived CD4+ T cells, which form the major viral reservoir. The persistence of this reservoir despite long-term ART is the major hurdle to curing HIV. Importantly, the size of the HIV reservoir is larger in individuals who start ART late in the course of infection and have a low CD4+/CD8+ ratio. HIV reservoir size is also linked to the levels of persistent inflammation on ART. Thus, novel strategies to reduce immune inflammation and improve the host response to control the HIV reservoir would be a valuable addition to current ART. Among the different strategies under investigation is metformin, a widely used antidiabetic drug that was recently shown to modulate T-cell activation and inflammation. Treatment of non-diabetic individuals with metformin controls inflammation by improving glucose metabolism and by regulating intracellular immunometabolic checkpoints such as the adenosin 5 monophosphate activated protein kinase and mammalian target of rapamycin, in association with microbiota modification.
Methods and analysis
22 PLWH on ART for more than 3 years, at high risk of inflammation or the development of non-AIDS events (low CD4+/CD8+ ratio) will be recruited in a clinical single-arm pilot study. We will test whether supplementing ART with metformin in non-diabetic HIV-infected individuals can reduce the size of the HIV reservoir as determined by various virological assays. The expected outcome of this study is a reduction in both the size of the HIV reservoir and inflammation following the addition of metformin to ART, thus paving the way towards HIV eradication.
Ethics and dissemination
Ethical approval: McGill university Health Centre committee number MP-37-2016-2456. Canadian Canadian Institutes of Health Research/Canadian HIV Trials Network (CTN) protocol CTNPT027. Results will be made available through publication in peer-reviewed journals and through the CTN website.
Trial registration number
Keywords: HIV reservoir, immune activation, metformin, pilot study
Strengths and limitations of this study.
The Lilac study focuses on two main problems of antiretroviral therapy (ART)-treated people living with HIV (PLWH): immune activation and HIV reservoirs.
Metformin is a well-tolerated antihyperglycaemic drug with anti-inflammatory effects which has been shown to restore T-cell function.
We hypothesise that metformin treatment in PLWH on ART will allow immune activation reduction and a diminution of the HIV reservoir size.
We will assess changes induces by metformin in both in blood and colon biopsies.
Although the Lilac study is a pilot trial on 22 PLWH on ART, it should provide sufficient sample size calculations for larger studies.
Introduction
HIV persistence during antiretroviral therapy
Antiretroviral therapy (ART) decreases HIV plasma viral load below the limit of detection of clinical assays, leading to major improvements in the health of people living with HIV (PLWH). However, these individuals on prolonged ART develop significant metabolic complications that contribute to an increased risk of inflammatory non-AIDS events.1 Such clinical events are associated with persistent immune activation, and occur more often when ART initiation is delayed.2–4 ART cannot clear latently infected memory CD4+ T cells, which persist to form the viral reservoir, responsible for the rapid viral rebound upon ART interruption.5 6 Determinants of the size of the HIV reservoir include late ART initiation, low CD4+ T cell count, low CD4+/CD8+ ratio despite CD4+ T cell recovery and high levels of immune activation.7–10 Conversely, elite controllers, who have strong polyfunctional HIV-specific cytotoxic T-lymphocytes, have a smaller reservoir compared with ART-treated individuals.11 12 These observations support a direct relationship between the quality of the HIV-specific immune response, level of inflammation and HIV reservoir size. Therefore, strategies aiming at targeting and reducing immune activation and improving T-cell function may reduce the size of the HIV reservoir.
We and others have demonstrated that during primary HIV infection, the altered metabolic state of HIV-specific CD8+ T cells leads to persistent immune activation and immune exhaustion.13–15 These findings indicate that metabolism acts upstream of immune activation and influences immune responses.16 During chronic HIV infection, the switch from oxidative phosphorylation to aerobic glycolytic metabolism in response to persistent antigenic stimulation leads to terminal differentiation, reducing the pool of central memory T-cells.17 18 Such metabolic changes at the cellular level are regulated by nutrient-sensing and activation signalling pathways mainly mediated by phosphoinositide 3-kinase, mammalian target of rapamycin (mTOR) and adenosine monophosphate-activated protein kinase (AMPK).19 As for cancer cells, a ‘Warburg effect’ occurs whereby glucose transport is markedly increased via aerobic glycolysis following persistent T-cell activation.20 Notably, during chronic viral infections, the energy sensor AMPK modulates glucose uptake for fuelling T-cell cytotoxic function.21 22
Collectively, these findings suggest that immunometabolism, which regulates T-cell proliferation and cytotoxic responses, may influence the size of the HIV reservoir.23 Therefore, medication that improves T-cell metabolism may enhance their function and may contribute to immune control of the HIV reservoir.
Metformin is an antidiabetic drug with immunometabolic effects
Isolated in the 1920s from French lilac, metformin (dimethylbiguanide) is widely used as a first-line treatment for type II diabetes.24 This drug, which has limited side effects, acts as an antihyperglycaemic agent that promotes euglycaemia without the risk of hypoglycaemia.25 By improving insulin sensitivity, metformin decreases insulin resistance in non-insulin-dependent diabetics by activating AMPK, thereby reducing hepatic gluconeogenesis and increasing glucose uptake in skeletal muscles.26
Metformin was recently shown to promote longevity in worms, rodents and diabetic individuals by mimicking a state of induced dietary restriction.27 Metformin has been demonstrated to decrease cancer and myocardial infarction-related mortality in diabetic individuals, in addition to enhancing memory T-cell generation in mice.28 29 Mechanistically, metformin inhibits mTOR signalling independently of the insulin-signalling pathway by: (1) activating AMPK, a heterotrimeric serine/threonine kinase complex that monitors cellular energy levels and acts as an upstream inhibitor of mTOR and (2) inhibiting Rag GTPases.30
Metformin promotes autophagy and modulates T-cell glycolysis by inhibiting mTOR, improving CD4+ T cell counts in diabetic PLWH initiating ART.31 The effects of metformin in PLWH may be due to: (1) its ability to overcome the inhibition AMPK by viral transactivator of transcription (Tat) protein32; (2) an anti-inflammatory effect on the intestine by suppressing nuclear factor κB activation33; (3) an indirect anti-inflammatory effect caused by the reduced production of cytokines such as tumour necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1)34 and/or (4) changes in the composition of the gut microbiota which have been observed in mice and in humans.35–38 This last observation occurred in the absence of a glycaemic effect when metformin was administered intravenously to mice,39 suggesting that the microbiota plays a predominant role in metformin effect. The ability of metformin to affect the composition of the gut microbiota may also contribute to metformin’s antidiabetic effect given that dysbiosis, that is an imbalance in the composition of the microbiota, has been directly associated with insulin resistance related to lipopolysaccharide (LPS)-induced inflammation.35 36 39 Indeed, plasma levels of LPS are elevated in PLWH.40–42
Metformin has been recently considered to be an ‘oncobiguanide’ due to its immunometabolic effect on cancer cells, paving the way for its current investigation in non-diabetic cancer patients.43 Gong et al have further shown that the use of metformin by diabetic, postmenopausal women was associated with a reduced risk of breast cancer and reduced risk of death from cancer, compared with the use of other antidiabetic medications including insulin.44
In non-diabetic women treated for polycystic ovary syndrome, 12 weeks of metformin decreased levels of intracellular adhesion molecule-1, E-selectin, IL-6 and TNF-α.45 Recently, metformin was shown to have limited toxicity compared with placebo in non-diabetic, pregnant, obese women who received a daily prophylactic dose of 3.0 g from 12 to 18 weeks of gestation until delivery.46 Encouragingly, these patients had reduced maternal gestational weight gain and a lower rate of pre-eclampsia compared with patients who received a placebo.
Based on its low toxicity profile46 and its ability to activate AMPK and to inhibit mTOR signalling, metformin is a promising new immunometabolic candidate.19 We hypothesise that in addition to ART, metformin could decrease immune activation and restore CD8+ T cell function to decrease the size of the HIV reservoir. Therefore, we designed a pilot study to test this hypothesis and to obtain estimates for sample size calculations required for larger scale studies.
Objectives
To establish the feasibility and optimal design of a full-scale study on the effect of metformin in ART-treated PLWH, we designed a single-arm pilot study.
Primary outcomes
The primary outcome of this study will be the change in the size of the HIV reservoir in blood before and after 12 weeks of metformin, and after 12 weeks of metformin discontinuation as determined by PCR-based assays (total and integrated HIV DNA).
Secondary outcomes
The secondary outcomes of this study will be the following:
Safety of adding 12 weeks of metformin treatment to suppressive ART in PLWH.
Change in the size of the HIV reservoir in colon biopsies before and after 12 weeks of metformin, as determined by PCR-based assays (total and integrated HIV DNA).
The change in the size of the HIV reservoir before and after 12 weeks of metformin as determined by tat/rev induced limiting dilution assay (TILDA), a novel PCR-based assay that quantifies the frequency of CD4+ T-cells harbouring inducible HIV.47
The change in immune activation before and after 12 weeks of metformin as measured by changes in the percentage of human leukocyte antigen-DR isotype (HLA-DR) and CD38 expressing T-cells, in both blood and colon biopsies.
Exploratory outcomes
The exploratory outcomes of this study will be the changes in the following before and after 12 weeks of metformin use, and after 12 weeks of metformin discontinuation.
The absolute CD4+ and CD8+ T cell counts and the CD4+/CD8+ ratio.
The plasma levels of fasting glucose, glycosylated haemoglobin (HbA1c), lipid profile, total cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides, C reactive protein (CRP) and D-dimer to assess the hepatic and renal functions.
The plasma levels of the following soluble inflammatory factors: interferon-alpha (IFN-α), TNF-α, IL-1, IL-6, IFN-γ-inducible protein 10 (IP-10) and LPS to assess the anti-inflammatory effect of metformin.
The composition of the gut microbiota in stool samples.
Methods and analysis
Study design, settings, sample size and recruitment strategy
The study protocol described herein meets the 2013 Standard Protocol Items: Recommendations for Interventional Trials guidelines.48 49
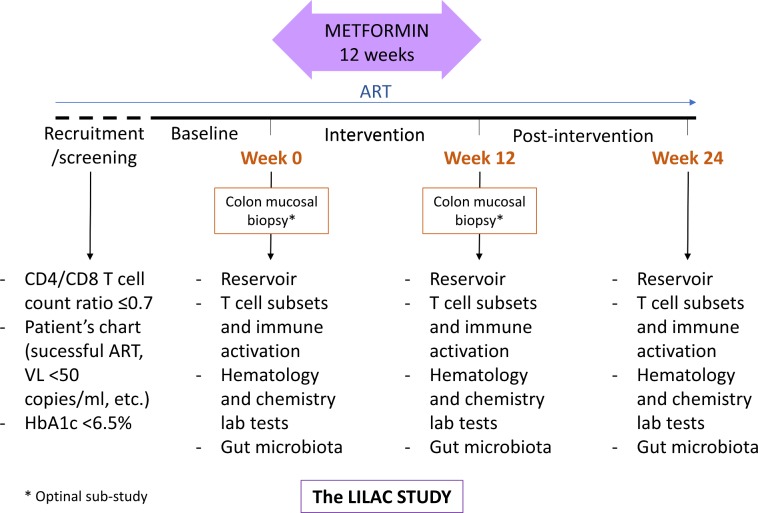
Comparisons will be made by repeated measures of the outcomes at baseline, during and after metformin use (figure 1 and in table 1).
Figure 1.
Study design depicting study visits, intervention and laboratory assessments. ART, antiretroviral therapy; HbA1c, glycosylated haemoglobin; VL, viral load.
Table 1.
Schedule of events
| Visit no | Study visits | |||||
| Week, day | ||||||
| W-4 to −1 Screening |
W0, D1 Baseline |
W1, D1 (±1 day) |
W4, D1 (±3 days) |
W12, D1 (±3 days) |
W24, D1 (±3 days) |
|
| V1 | V2 | V3 | V4 | V5 | V6/final | |
| Consent form | X | X | ||||
| Medical history | X | |||||
| Concomitant medication | X | X | X | X | X | |
| Eligibility criteria | X | X | ||||
| Physical examination | X | X | X | X | ||
| Adverse events | X | X | X | X | X | |
| Haematology* | X | X | X | X | ||
| Chemistry† | X | X | X | X | ||
| T-cell activation and inflammatory markers | X | X | X | |||
| HIV viral load | X | X | X | X | X | |
| Size of HIV reservoir in latently infected CD4+ T cells | X | X | X | |||
| Urine pregnancy test | X | X | ||||
| Metformin administration | X | X | X | |||
| Colon mucosal biopsies‡ | X | X | ||||
| Stool sample collection for microbiota analysis | X | X | X | |||
*Complete blood count, CD4+ and CD8+ T cell counts.
†AST, ALT, Alk Phos, total bilirubin, triglycerides, cholesterol, HDL, LDL, creatinine, blood glucose, lipase, amylase, urea, creatine kinase, serum phosphate and fasting glucose.
‡Optional procedure.
AST, aspartate aminotransferase; ALT, alanine aminotransferase; Alk Phos, alkaline phosphatase; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
A total of 22 HIV-infected participants will be recruited; it is estimated that there will be a 10% lost to follow-up/study non-completion. Based on our prior studies, it is expected that approximately 50% of participants will consent to participate in the optional substudy examining the effect of metformin on the composition of the gut immune environment in gut mucosa samples obtained by colonoscopy.50 51 A convenient sample of 22 participants was chosen without formal power calculations. The data that will be obtained in this study should suffice for calculations for future studies.
Participants will be recruited by clinicians at the Chronic Viral Illness Service at the McGill University Health Centre (Montréal, QC, Canada) and the Immunodeficiency Clinic of the Ottawa Hospital (Ottawa, ON, Canada); each of these clinics provides care to 1300–2300 PLWH. Teleconferences and face-to-face meetings will be organised between the investigators and research nurses to help support patient recruitment. Furthermore, conferences on the importance of inflammation in HIV infection and on innovative therapies to alleviate inflammation (such as metformin) will be organised by the investigators to target community groups, treating physicians and healthcare providers.
Inclusion criteria
Eligible participants will meet the following criteria to be considered eligible for entry into the study: (1) HIV-1-infected male or female at least 18 years of age; (2) successfully treated with ART for at least 3 years, the time necessary to establish a stable reservoir; (3) individuals on a stable ART regimen with plasma viral load below the limit of detection without any recorded blips for at least 3 months, (4) people with a CD4+/CD8+ ratio ≤0.7 at baseline to select participants with high risk of inflammation and non-AIDS events52 and (5) non-diabetic as defined HbA1c <5.9% or prediabetic individuals with HbA1c between 6.0% and ≥6.4%.
Exclusion criteria
Individuals who meet any of the following criteria will be excluded from the study: (1) a known hypersensitivity/allergy to the metformin; (2) active participation in an experimental therapy study or having received experimental therapy within the last 6 months; (3) severe systemic diseases (uncontrolled hypertension, chronic renal failure) or active uncontrolled infections; (4) diabetes mellitus (HbA1c ≥6.5%) as defined by the Canadian Clinical Practice Guidelines for the Prevention and Management of Diabetes24 53; (5) oral hypoglycaemic treatment or insulin; (6) statins or other anticholesterol treatments started in the last 3 months since statins are known to be anti inflammatory54; (7) a history of sickle cell anaemia and/or thalassaemia, impacting HbA1c measurement; (8) a history of congestive heart failure New York Heart Association Classification I-IV or having a cardiac pacemaker; (9) a history of lactic acidosis; (10) current use of stavudine and/or didanosine as metformin can increase the risk of lactic acidosis55; (11) severe liver or kidney disease based on physician evaluation; (12) elevated aspartate aminotransferase and alanine aminotransferase threefold above the upper normal limit; (13) elevated alkaline phosphatase twofold above upper normal limit; (14) elevated creatinine (above 150 µmol/L); (15) current use of oral steroids; (16) a systemic infection within the last 1 month; (17) women who are pregnant or breast feeding.
Study intervention
This study will involve 500 mg and 850 mg doses of metformin hydrochloride (Glucophage; Sanofi-Aventis Canada). Metformin will be taken with meals throughout the study duration; in the first week, orally two times daily as 500 mg tablets to assess tolerability, following which the dose will be increased to 850 mg tablets two times daily (weeks 2–12). These doses were chosen based on the mean dose used in diabetic individuals in whom metabolic improvement has been described56–59; Treatment duration is based on the duration of use in non-diabetic patients treated for polycystic ovary syndrome in whom an inflammatory effect was observed45; Compliance will be monitored by the research study nurse at each visit by assessing pill counts and by telephone calls between each visit.
Since concomitant use of dolutegravir and metformin increases the plasma concentration of metformin60 61; participants using dolutegravir will take the 500 mg dose metformin two times daily throughout the study. Although the coadministration of dolutegravir and metformin was found to be well tolerated in individuals taking both medications,60 61 dose reduction of metformin may be considered according to participant tolerance and to clinician judgement.
Use of medications, alcohol, street drugs and natural remedies will be recorded. There will not be any restrictions on the use of natural remedies since none have been found to interact with metformin.
Adverse events and toxicity management
During each follow-up visit with a participant, information on adverse events (AEs) will be gathered and documented accordingly. AEs will be graded as mild, moderate, severe or life threatening according to the toxicity table and toxicity guidelines provided by the National Institutes of Health Division of AIDS Table for Grading the Severity of Adult and Pediatric Adverse Events, and will be assessed by causality as probably related, possibly related, unlikely to be related or not related to the study drug. The assessment of safety will include clinical observation and monitoring of patient management and changes over times. The Canadian HIV Trials Network (CTN) will be responsible for reporting serious AEs to Health Canada.
Clinical and laboratory assessments
Assessment of HIV reservoir size
The size of the HIV reservoir in peripheral blood and in colon biopsies (optional substudy) will be measured using PCR-based assays (total and integrated HIV DNA). In addition, the size of the inducible reservoir in blood CD4+ T cells will be measured by TILDA.
Frequency of cells harbouring total and integrated HIV DNA will be measured using a nested quantitative PCR that can detect a single copy of the viral genome in 105 cells.62 While integrated HIV DNA is present in both latently and productively infected cells, the ratio between total and integrated has been shown to reflect residual HIV expression and de novo reverse transcription.63
As the majority of HIV DNA molecules are not replication competent,64 we will measure the frequency of cells producing HIV multiply spliced (ms) RNAs after T cell receptor (TCR) stimulation in blood CD4+ T-cells using TILDA.47 The estimate of the size of the reservoir provided by TILDA is intermediate between PCR-based assays and quantitative viral outgrowth assays and requires fewer cells. While unspliced HIV RNAs are frequently detected in latently infected cells in the absence of viral production, HIV msRNA (Tat/Rev) reflect active viral production. We will take advantage of this unique feature of msRNA in a limiting dilution assay to measure the frequency of cells with inducible HIV on maximal stimulation in CD4+ T-cells isolated from blood. Briefly, isolated CD4+ T-cells will be stimulated for 12 hours with phorbol myristate acetate/ionomycin. The stimulated cells will be serially diluted in a 96 well plate, lysed and the lysates will be used immediately for reverse transcriptase PCR. msRNA will be quantified by real-time PCR, and by using the maximum likelihood method, the frequency of cells harbouring inducible HIV msRNA in CD4+ T-cells will be calculated. The difference in the relative frequencies of CD4+ T-cells that are either activated or not activated represents the inducible latently infected cells.
Assessment of T-cell activation in blood
The levels of T-cell activation will be assessed in blood samples drawn at weeks 0, 12 and 24, as specified in figure 1 and table 1. Briefly, peripheral blood mononuclear cells (PBMCs) will be obtained by Ficoll gradient centrifugation. The PBMCs will either be labelled with the appropriate monoclonal antibodies or will be stored in liquid nitrogen until analysed. T-cell analysis will be performed using specific monoclonal antibodies as previously reported.41 65–67 The associated expressions of CD45RA, CCR7 and CD27 will be used to determine the percentages of naive (CD45RA+CCR7+CD27+), central memory (CD45RA–CCR7+CD27+), preterminal effector memory (CD45RA–CCR7–CD27–), transitional memory (CD45RA-CCR7+CD27+) and terminally differentiated (CD45RA+CCR7–CD27–) CD4+ and CD8+ T-cell subsets. The expression of the activation markers HLA-DR and CD38 will be assessed on the CD4+ and CD8+ T-cell subsets. FlowJo software will be used to analyse the data.
Assessment of HIV reservoirs and T-cell activation in gut mucosa samples
Since recent studies suggest that the mucosal immune system is the most important site of T-cell activation in HIV infection,68 the frequency of HLA-DR+CD38+ activated CD8+ T-cells in optional colon mucosal biopsies samples will be determined. Colon biopsies (around 30) will be obtained by colonoscopy performed before metformin administration (week 0) and at the end of metformin treatment (week 12), as specified in figure 1 and table 1.
Gut T-cells will be isolated from biopsy samples by enzyme digestion using a collagenase-based method as reported previously.68–70 Briefly, fresh tissue biopsies will be incubated with type II collagenase for 30 min at 37°C in a shaking incubator. Tissues pieces will be mechanically separated by repeated passage through a syringe. Viable lymphocytes will be separated from debris using Ficoll-Hypaque density gradient centrifugation. HIV reservoir will be measured by PCR-based assays (total and integrated HIV DNA) in sorted CD4+ T cells. It is unlikely that TILDA will be performed in mucosal T-cells are their number should be too low. The total frequency of activated CD4+ and CD8+ T-cells will be determined by flow cytometry as described above.
Assessment of inflammatory cytokines in plasma
Levels of inflammatory markers such as D-dimer and CRP are related to cardiovascular non-AIDS events during HIV infection. The ability of metformin therapy to reduce plasma levels of IFN-α, IL-1, IL-6, IP-10, TNF-α and LPS will be assessed by ELISA as previously reported.41 71
Assessment of gut microbiota composition
Recent studies have shown that metformin can change the composition of the gut microbiota.35 37 72 We hypothesised that changes in microbiota composition influence markers of inflammation and immune activation. To assess this, stool samples will be collected before (week 0) and after (week 12) metformin therapy, and after 12 weeks of metformin discontinuation (week 24) into clean collection tubes. Stool samples will be immediately stored at −80°C until analysed. DNA will be extracted using the Qiagen Stool Mini Kit. The composition of the gut microbiota will be determined using DNA sequencing of 16S ribosomal RNA region of bacterial taxa.
Statistical analysis
Comparisons of HIV reservoir size and percentage of activated T-cells will be made between baseline, week 12 and week 24. The data will be analysed by non-parametric statistical tests such as the Wilcoxon matched pairs test and the Friedman test. The threshold of significance will be 5%.
The same tests will be used to analyse data from blood and colon biopsies. Comparisons will also be made between mucosal and blood compartments within the same participant using the Wilcoxon matched pairs test and the Friedman test.
The Wilcoxon matched pairs test will be used to compare the number of bacterial taxa by type in stool samples before and after metformin therapy.
Patient and public involvement
Patients or public were not involved in the design of this study.
Compliance questionnaires will allow for assessment of participants’ experience.
Final results of the study are expected to be published but will not be specifically disseminated to participants.
Ethics and dissemination plan
Written informed consent will be obtained from all participants. All protocol amendments will be submitted to the research ethics board of each participating centre. The Investigator will seek prior ethics approval for any protocol deviations except when the change is intended to eliminate an immediate hazard to participants. In this case, the protocol deviation will be promptly reported to the data safety and monitoring committee of the CTN.
Dissemination plan
The results of the trial, regardless of outcome, will be disseminated through the traditional routes of scientific peer-reviewed publications, through international and national specialist conferences, and through the press release by CTN.
Discussion
The size of the HIV reservoir is influenced by a number of factors including late ART initiation, low CD4+ T-cell count, low CD4+/CD8+ ratio and high level of immune activation.7–10 Therapies that target and reduce immune activation are therefore critical to reduce the size of the HIV reservoir.
It has been shown that in HIV-specific CD8+ T-cells cellular metabolism is linked to immune responses and acts upstream of immune activation.13–15 We further propose that immunometabolism, which has been shown to affect the ability of T-cells to proliferate, would regulate optimal cytotoxic responses and influence the size of the HIV reservoir.23 Given metformin’s immunomodulatory properties,28–34 43 45 and its ability to improve CD4+ T-cell counts in one study of participants initiating ART,31 we propose that this antidiabetic medication may enhance T-cell effector function to control the HIV reservoir.
This study will test the hypothesis that the coadministration of metformin and ART will decrease the size of the viral reservoir and the levels of immune activation. If so, after 12 weeks of metformin therapy, participants should manifest a decrease in T-cell activation (ie, from week 0 to week 12) that may reverse after metformin discontinuation (ie, from week 12 to week 24) as metformin’s anti-inflammatory effects are lost.
We have previously reported a 10-fold difference in the frequency of HLA-DR+CD38+ activated CD8+ T-cells between uninfected controls and aviraemic ART-treated individuals.65 73 A 50% reduction in the number of activated CD8+CD38+HLA-DR+ T-cells is estimated following metformin treatment. It is expected that the reduction of the frequency of activated CD8+ T-cells by metformin therapy will be more significant in the gut mucosa than in peripheral blood since this mucosal site is the major source of microbial translocation, a process that results in T-cell activation via activation of toll-like receptors.
Furthermore, measurements of circulating cytokines, of inflammatory mediators, and of LPS will be made to determine whether metformin treatment can also reduce or suppress inflammatory mediators known to drive immune activation.
This single-arm pilot study will include 22 participants. Should the results of this study suggest that metformin can reduce immune activation and/or the size of the viral reservoir in HIV-infected participants on suppressive ART, formal sample size calculations can be done for larger future studies.
Supplementary Material
Acknowledgments
The authors would like to thank Michael Pollak, Rafick Sékaly and Jean-François Yale for their contributions to the study hypothesis and design, Gina M Graziani for her help writing the manuscript, Angie Massicotte, Josee Girouard, Guillaume Theriault and Cynthia Dion for their help with coordination. The authors thank John Lin for manuscript improvement.
Footnotes
Contributors: J-PR, VM, MO, NC, PA and JBA designed the study. J-PR, SI and VM wrote the manuscript. RP, DP, FPD and SI will participate in data collection and analysis. All authors critically reviewed the manuscript and approved the final version.
Funding: This study was funded by the Canadian Institutes of Health Research (CIHR) Canadian HIV trials Network (CTN) (CTN PT027 grant to JPR), CIHR (IBC-154053 grant to PA) and by the Canadian HIV Cure Enterprise (CanCURE) (Team Grant HIG-133050 to JPR), awarded by the CIHR in partnership with the Canadian Foundation for AIDS Research (CANFAR) and with the International AIDS Society (IAS). Authors who are CTN and/or CanCURE members were involved in the study design and in the writing of the manuscript, and will also be involved in data collection, analysis and interpretation.
Competing interests: J-PR has performed contract research and/or served on Advisory Boards for Gilead Sciences Canada, Merck Canada, Abbvie, ViiV Healthcare, Bristol Myers Squibb, Janssen, Argos Pharmaceuticals from InnaVirVax and has served on the Advisory Board of Theravectys. JBA has performed contract research and/or served on Advisory Boards for Gilead Sciences Canada, Merck Canada, Abbvie, ViiV Healthcare, Bristol Myers Squibb, Janssen and Argos Pharmaceuticals. MO has performed contract research and/or served on Advisory Boards for Gilead Sciences Canada, Merck Canada, Abbvie, ViiV Healthcare, Bristol Myers Squibb and Janssen. NC has received research funding from Merck & Co. and from InnaVirVax and has served on the Advisory Board of Theravectys.
Ethics approval: This study was approved by the Research Ethics Boards of the Research Institute of the McGill University Health Centre (MUHC) number MP-37-2016-2456 and by the Health Canada Therapeutic Products Directorate, and will be conducted in accordance with the Declaration of Helsinki of 1975, as revised in 2000.
Provenance and peer review: Not commissioned; externally peer reviewed.
Collaborators: Group Authorship/Collaborating Author Names: J-PR, SI, VM, MO, NC, PA, RP, DP, FPD and JBA for the Lilac Study Group.
Patient consent for publication: Not required.
References
- 1. Kesselring A, Gras L, Smit C, et al. Immunodeficiency as a risk factor for non-AIDS-defining malignancies in HIV-1-infected patients receiving combination antiretroviral therapy. Clin Infect Dis 2011;52:1458–65. 10.1093/cid/cir207 [DOI] [PubMed] [Google Scholar]
- 2. Routy JP, Mehraj V. Very early antiretroviral therapy permits CD8 T cells to keep HIV reservoirs at bay. Ann Transl Med 2017;5:434 10.21037/atm.2017.08.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sandler NG, Sereti I. Can early therapy reduce inflammation? Curr Opin HIV AIDS 2014;9:72–9. 10.1097/COH.0000000000000020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hsu DC, Sereti I. Serious Non-AIDS events: therapeutic targets of immune activation and chronic inflammation in HIV Infection. Drugs 2016;76:533–49. 10.1007/s40265-016-0546-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Pierson T, McArthur J, Siliciano RF. Reservoirs for HIV-1: mechanisms for viral persistence in the presence of antiviral immune responses and antiretroviral therapy. Annu Rev Immunol 2000;18:665–708. 10.1146/annurev.immunol.18.1.665 [DOI] [PubMed] [Google Scholar]
- 6. Deeks SG, Lewin SR, Ross AL, et al. International AIDS Society global scientific strategy: towards an HIV cure 2016. Nat Med 2016;22:839–50. 10.1038/nm.4108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boulassel MR, Chomont N, Pai NP, et al. CD4 T cell nadir independently predicts the magnitude of the HIV reservoir after prolonged suppressive antiretroviral therapy. J Clin Virol 2012;53:29–32. 10.1016/j.jcv.2011.09.018 [DOI] [PubMed] [Google Scholar]
- 8. Chomont N, El-Far M, Ancuta P, et al. HIV reservoir size and persistence are driven by T cell survival and homeostatic proliferation. Nat Med 2009;15:893–900. 10.1038/nm.1972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lu W, Mehraj V, Vyboh K, et al. CD4:CD8 ratio as a frontier marker for clinical outcome, immune dysfunction and viral reservoir size in virologically suppressed HIV-positive patients. J Int AIDS Soc 2015;18:20052 10.7448/IAS.18.1.20052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Massanella M, Fromentin R, Chomont N. Residual inflammation and viral reservoirs: alliance against an HIV cure. Curr Opin HIV AIDS 2016;11:234–41. 10.1097/COH.0000000000000230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saag M, Deeks SG. How do HIV elite controllers do what they do? Clin Infect Dis 2010;51:239–41. 10.1086/653678 [DOI] [PubMed] [Google Scholar]
- 12. van Grevenynghe J, Procopio FA, He Z, et al. Transcription factor FOXO3a controls the persistence of memory CD4(+) T cells during HIV infection. Nat Med 2008;14:266–74. 10.1038/nm1728 [DOI] [PubMed] [Google Scholar]
- 13. Cao W, Mehraj V, Trottier B, et al. Early initiation rather than prolonged duration of antiretroviral therapy in hiv infection contributes to the normalization of CD8 T-Cell Counts. Clin Infect Dis 2016;62:250–7. 10.1093/cid/civ809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Man K, Kallies A. Synchronizing transcriptional control of T cell metabolism and function. Nat Rev Immunol 2015;15:574–84. 10.1038/nri3874 [DOI] [PubMed] [Google Scholar]
- 15. Trautmann L, Mbitikon-Kobo FM, Goulet JP, et al. Profound metabolic, functional, and cytolytic differences characterize HIV-specific CD8 T cells in primary and chronic HIV infection. Blood 2012;120:3466–77. 10.1182/blood-2012-04-422550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Aounallah M, Dagenais-Lussier X, El-Far M, et al. Current topics in HIV pathogenesis, part 2: Inflammation drives a Warburg-like effect on the metabolism of HIV-infected subjects. Cytokine Growth Factor Rev 2016;28:1–10. 10.1016/j.cytogfr.2016.01.001 [DOI] [PubMed] [Google Scholar]
- 17. Delgoffe GM, Powell JD. Sugar, fat, and protein: new insights into what T cells crave. Curr Opin Immunol 2015;33:49–54. 10.1016/j.coi.2015.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wherry EJ, Kurachi M. Molecular and cellular insights into T cell exhaustion. Nat Rev Immunol 2015;15:486–99. 10.1038/nri3862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Dagenais-Lussier X, Mouna A, Routy JP, et al. Current topics in HIV-1 pathogenesis: The emergence of deregulated immuno-metabolism in HIV-infected subjects. Cytokine Growth Factor Rev 2015;26:603–13. 10.1016/j.cytogfr.2015.09.001 [DOI] [PubMed] [Google Scholar]
- 20. Faubert B, Boily G, Izreig S, et al. AMPK is a negative regulator of the Warburg effect and suppresses tumor growth in vivo. Cell Metab 2013;17:113–24. 10.1016/j.cmet.2012.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Blagih J, Coulombe F, Vincent EE, et al. The energy sensor AMPK regulates T cell metabolic adaptation and effector responses in vivo. Immunity 2015;42:41–54. 10.1016/j.immuni.2014.12.030 [DOI] [PubMed] [Google Scholar]
- 22. Palmer CS, Ostrowski M, Balderson B, et al. Glucose metabolism regulates T cell activation, differentiation, and functions. Front Immunol 2015;6:1 10.3389/fimmu.2015.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Routy JP, Mehraj V, Vyboh K, et al. Clinical relevance of kynurenine pathway in hiv/aids: an immune checkpoint at the crossroads of metabolism and inflammation. AIDS Rev 2015;17:96–106. [PubMed] [Google Scholar]
- 24. Harper W, Clement M, Goldenberg R, et al. Policies, guidelines and consensus statements: pharmacologic management of Type 2 Diabetes-2015 Interim Update. Can J Diabetes 2015;39:250–2. 10.1016/j.jcjd.2015.05.009 [DOI] [PubMed] [Google Scholar]
- 25. Prasad-Reddy L, Isaacs D. A clinical review of GLP-1 receptor agonists: efficacy and safety in diabetes and beyond. Drugs Context 2015;4:1–19. 10.7573/dic.212283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fantus IG, Brosseau R. Mechanism of action of metformin: insulin receptor and postreceptor effects in vitro and in vivo. J Clin Endocrinol Metab 1986;63:898–905. 10.1210/jcem-63-4-898 [DOI] [PubMed] [Google Scholar]
- 27. De Haes W, Frooninckx L, Van Assche R, et al. Metformin promotes lifespan through mitohormesis via the peroxiredoxin PRDX-2. Proc Natl Acad Sci U S A 2014;111:E2501–E2509. 10.1073/pnas.1321776111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Anisimov VN. Metformin: do we finally have an anti-aging drug? Cell Cycle 2013;12:3483–9. 10.4161/cc.26928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Son HJ, Lee J, Lee SY, et al. Metformin attenuates experimental autoimmune arthritis through reciprocal regulation of Th17/Treg balance and osteoclastogenesis. Mediators Inflamm 2014;2014:1–13. 10.1155/2014/973986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Araki K, Turner AP, Shaffer VO, et al. mTOR regulates memory CD8 T-cell differentiation. Nature 2009;460:108–12. 10.1038/nature08155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Moyo D, Tanthuma G, Cary MS, et al. Cohort study of diabetes in HIV-infected adult patients: evaluating the effect of diabetes mellitus on immune reconstitution. Diabetes Res Clin Pract 2014;103:e34–e36. 10.1016/j.diabres.2013.12.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zhang HS, Wu MR, Mr W. SIRT1 regulates Tat-induced HIV-1 transactivation through activating AMP-activated protein kinase. Virus Res 2009;146:51–7. 10.1016/j.virusres.2009.08.005 [DOI] [PubMed] [Google Scholar]
- 33. Koh SJ, Kim JM, Kim IK, et al. Anti-inflammatory mechanism of metformin and its effects in intestinal inflammation and colitis-associated colon cancer. J Gastroenterol Hepatol 2014;29:502–10. 10.1111/jgh.12435 [DOI] [PubMed] [Google Scholar]
- 34. Jin Q, Cheng J, Liu Y, et al. Improvement of functional recovery by chronic metformin treatment is associated with enhanced alternative activation of microglia/macrophages and increased angiogenesis and neurogenesis following experimental stroke. Brain Behav Immun 2014;40:131–42. 10.1016/j.bbi.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 35. Forslund K, Hildebrand F, Nielsen T, et al. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 2015;528:262–6. 10.1038/nature15766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Forslund K, Hildebrand F, Nielsen T, et al. Corrigendum: disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 2017;545:116 10.1038/nature22318 [DOI] [PubMed] [Google Scholar]
- 37. Lee H, Ko G. Effect of metformin on metabolic improvement and gut microbiota. Appl Environ Microbiol 2014;80:5935–43. 10.1128/AEM.01357-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sun L, Xie C, Wang G, et al. Gut microbiota and intestinal FXR mediate the clinical benefits of metformin. Nat Med 2018;24:1919–29. 10.1038/s41591-018-0222-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cabreiro F. Metformin joins forces with microbes. Cell Host Microbe 2016;19:1–3. 10.1016/j.chom.2015.12.012 [DOI] [PubMed] [Google Scholar]
- 40. Ancuta P, Kamat A, Kunstman KJ, et al. Microbial translocation is associated with increased monocyte activation and dementia in AIDS patients. PLoS One 2008;3:e2516 10.1371/journal.pone.0002516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Brenchley JM, Price DA, Schacker TW, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med 2006;12:1365–71. 10.1038/nm1511 [DOI] [PubMed] [Google Scholar]
- 42. Jenabian MA, El-Far M, Vyboh K, et al. Immunosuppressive tryptophan catabolism and gut mucosal dysfunction following early HIV Infection. J Infect Dis 2015;212:355–66. 10.1093/infdis/jiv037 [DOI] [PubMed] [Google Scholar]
- 43. Menendez JA, Quirantes-Piné R, Rodríguez-Gallego E, et al. Oncobiguanides: Paracelsus' law and nonconventional routes for administering diabetobiguanides for cancer treatment. Oncotarget 2014;5:2344–8. 10.18632/oncotarget.1965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gong Z, Aragaki AK, Chlebowski RT, et al. Diabetes, metformin and incidence of and death from invasive cancer in postmenopausal women: Results from the women’s health initiative. Int J Cancer 2016;138:1915–27. 10.1002/ijc.29944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Victor VM, Rovira-Llopis S, Bañuls C, et al. Metformin modulates human leukocyte/endothelial cell interactions and proinflammatory cytokines in polycystic ovary syndrome patients. Atherosclerosis 2015;242:167–73. 10.1016/j.atherosclerosis.2015.07.017 [DOI] [PubMed] [Google Scholar]
- 46. Syngelaki A, Nicolaides KH, Balani J, et al. Metformin versus Placebo in Obese Pregnant Women without Diabetes Mellitus. N Engl J Med 2016;374:434–43. 10.1056/NEJMoa1509819 [DOI] [PubMed] [Google Scholar]
- 47. Procopio FA, Fromentin R, Kulpa DA, et al. A novel assay to measure the magnitude of the inducible viral reservoir in HIV-infected individuals. EBioMedicine 2015;2:874–83. 10.1016/j.ebiom.2015.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chan AW, Tetzlaff JM, Altman DG, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med 2013;158:200–7. 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chan AW, Tetzlaff JM, Gøtzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mehraj V, Ghali P, Ramendra R, et al. The evaluation of risk-benefit ratio for gut tissue sampling in HIV cure research. J Virus Erad 2017;3:212–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sereti I, Estes JD, Thompson WL, et al. Decreases in colonic and systemic inflammation in chronic HIV infection after IL-7 administration. PLoS Pathog 2014;10:e1003890 10.1371/journal.ppat.1003890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Serrano-Villar S, Sainz T, Lee SA, et al. HIV-infected individuals with low CD4/CD8 ratio despite effective antiretroviral therapy exhibit altered T cell subsets, heightened CD8+ T cell activation, and increased risk of non-AIDS morbidity and mortality. PLoS Pathog 2014;10:e1004078 10.1371/journal.ppat.1004078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Goldenberg R, Punthakee Z. Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes 2013;37(Suppl 1):S8–S11. 10.1016/j.jcjd.2013.01.011 [DOI] [PubMed] [Google Scholar]
- 54. Eckard AR, McComsey GA. The role of statins in the setting of HIV infection. Curr HIV/AIDS Rep 2015;12:305–12. 10.1007/s11904-015-0273-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Worth L, Elliott J, Anderson J, et al. A cautionary tale: fatal lactic acidosis complicating nucleoside analogue and metformin therapy. Clin Infect Dis 2003;37:315–6. 10.1086/375850 [DOI] [PubMed] [Google Scholar]
- 56. Bailey CJ, Turner RC. Metformin. N Engl J Med 1996;334:574–9. 10.1056/NEJM199602293340906 [DOI] [PubMed] [Google Scholar]
- 57. Onken B, Driscoll M. Metformin induces a dietary restriction-like state and the oxidative stress response to extend C. elegans Healthspan via AMPK, LKB1, and SKN-1. PLoS One 2010;5:e8758 10.1371/journal.pone.0008758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Scarpello JH. Improving survival with metformin: the evidence base today. Diabetes Metab 2003;29:6S36–6S43. 10.1016/S1262-3636(03)72786-4 [DOI] [PubMed] [Google Scholar]
- 59. Zhou G, Myers R, Li Y, et al. Role of AMP-activated protein kinase in mechanism of metformin action. J Clin Invest 2001;108:1167–74. 10.1172/JCI13505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ribera E, Podzamczer D. [Mechanisms of action, pharmacology and interactions of dolutegravir]. Enferm Infecc Microbiol Clin 2015;33(Suppl 1):2–8. 10.1016/S0213-005X(15)30002-1 [DOI] [PubMed] [Google Scholar]
- 61. Zong J, Borland J, Jerva F, et al. The effect of dolutegravir on the pharmacokinetics of metformin in healthy subjects. J Int AIDS Soc 2014;17:19584 10.7448/IAS.17.4.19584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Vandergeeten C, Fromentin R, Merlini E, et al. Cross-clade ultrasensitive PCR-based assays to measure HIV persistence in large-cohort studies. J Virol 2014;88:12385–96. 10.1128/JVI.00609-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Mexas AM, Graf EH, Pace MJ, et al. Concurrent measures of total and integrated HIV DNA monitor reservoirs and ongoing replication in eradication trials. AIDS 2012;26:2295–306. 10.1097/QAD.0b013e32835a5c2f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Eriksson S, Graf EH, Dahl V, et al. Comparative analysis of measures of viral reservoirs in HIV-1 eradication studies. PLoS Pathog 2013;9:e1003174 10.1371/journal.ppat.1003174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Boulassel MR, Mercier F, Gilmore N, et al. Immunophenotypic patterns of CD8+ T cell subsets expressing CD8alphaalpha and IL-7Ralpha in viremic, aviremic and slow progressor HIV-1-infected subjects. Clin Immunol 2007;124:149–57. 10.1016/j.clim.2007.05.005 [DOI] [PubMed] [Google Scholar]
- 66. Favre D, Mold J, Hunt PW, et al. Tryptophan catabolism by indoleamine 2,3-dioxygenase 1 alters the balance of TH17 to regulatory T cells in HIV disease. Sci Transl Med 2010;2:32ra36 10.1126/scitranslmed.3000632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Mehraj V, Jenabian MA, Ponte R, et al. The plasma levels of soluble ST2 as a marker of gut mucosal damage in early HIV infection. AIDS 2016;30:1617–27. 10.1097/QAD.0000000000001105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Shacklett BL, Critchfield JW, Ferre AL, et al. Mucosal T-cell responses to HIV: responding at the front lines. J Intern Med 2009;265:58–66. 10.1111/j.1365-2796.2008.02042.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Gosselin A, Wiche Salinas TR, Planas D, et al. HIV persists in CCR6+CD4+ T cells from colon and blood during antiretroviral therapy. AIDS 2017;31:35–48. 10.1097/QAD.0000000000001309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Planas D, Zhang Y, Monteiro P, et al. HIV-1 selectively targets gut-homing CCR6+CD4+ T cells via mTOR-dependent mechanisms. JCI Insight 2017;2:2 10.1172/jci.insight.93230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Boulassel MR, Smith GH, Edwardes MD, et al. Influence of RANTES, SDF-1 and TGF-beta levels on the value of interleukin-7 as a predictor of virological response in HIV-1-infected patients receiving double boosted protease inhibitor-based therapy. HIV Med 2005;6:268–77. 10.1111/j.1468-1293.2005.00306.x [DOI] [PubMed] [Google Scholar]
- 72. Greenhill C. Effects of metformin mediated by gut microbiota. Nat Rev Endocrinol 2018;15:2 10.1038/s41574-018-0133-y [DOI] [PubMed] [Google Scholar]
- 73. Mercier F, Boulassel MR, Yassine-Diab B, et al. Persistent human immunodeficiency virus-1 antigenaemia affects the expression of interleukin-7Ralpha on central and effector memory CD4+ and CD8+ T cell subsets. Clin Exp Immunol 2008;152:72–80. 10.1111/j.1365-2249.2008.03610.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.