ABSTRACT
Introduction
Prophylactic antibiotics have been shown to reduce the rate of surgical site infection (SSI) 1, however there is little evidence supporting the effectiveness of one antibiotic over another. We have studied SSI rates and antibiotic prophylaxis protocols in Northern Ireland trauma surgery over a 10-year period to Identify the most effective antibiotic protocol associated with lowest rate of SSI.
Method
Antibiotic prophylaxis protocols from 2004-2014 were sought from each of the region’s 4 trauma hospitals and their dates of introduction recorded. For the same period, the number of trauma procedures carried out quarterly and the number of SSIs were recorded for each hospital from the return of prospectively collected SSI surveillance forms.
Results
26849 trauma procedures were included with an overall SSI rate of 1.34% (95% Confidence interval [CI] 1.21 to 1.49). Single dose flucloxacillin (2 grams) with single dose gentamicin (3mg/kg) was the most commonly used protocol used in 3 different hospitals for a combined 13.5 years covering 11445 procedures. The SSI rate was 0.72% (95% CI 0.58-0.89). Triple dose cefuroxime (1.5 grams) was used in 2 different hospitals for a combined 10 years covering 8864 procedures. The SSI rate for this regime was 2.46% (95% CI 2.16-2.80). Single dose cefuroxime (1.5 grams) was used in 2 different hospitals for a combined 8 years covering 6540 procedures. The SSI rate was 0.92% (95% CI 0.71-1.18).
Conclusion
In this prospective observational cohort study prophylaxis using flucloxacillin and gentamicin was associated with the lowest SSI rate. Single dose cefuroxime was associated with a lower rate of SSI compared to triple dose (p<0.001). Identification of antibiotic regimes associated with the lowest SSI rates will promote the judicious use of antibiotics, improve antibiotic stewardship while allowing for continued benefit in the prevention of SSI in an era of ever-increasing antibiotic resistance.
INTRODUCTION
Surgical site infection (SSI) remains an important complication of surgical trauma care. It results in increased mortality, prolonged hospital stays, further revision surgery, increased antibiotic use and extended follow up and rehabilitation 2. SSI is the second most common healthcare associated infection in Northern Ireland accounting for 19% of reported infections 2. Overall risk of developing SSI following surgery for fractures of the hip has been reported to be 4.97% with a third of these cases representing a deep infection. The cost of treating one such patient has been estimated to be £31,164. An annual report published by Public Health England for 2016-2017 reported SSI rates in fracture surgery between 1-1.5% 3
Prophylactic antibiotics have been shown to reduce the rate of SSI and their use has been integral to orthopaedic and trauma surgery practice in the prevention of SSI 1. Despite the established strong evidence for prophylaxis there is little evidence supporting the use of one antibiotic over another or the use of single over multiple dose prophylactic regimes 4.
Staphylococcus aureus (S.aureus) and coagulase negative staphylococci such as Staphylococcus epidermidis are the most common causative organisms while gram negative bacilli can also be implicated. Cephlosporins (e.g. cefuroxime) offer cover against most S.aureus and some gram-negative organisms. They also have a good safety profile, long half-life and good penetration in bone, synovium and muscle. Despite this however their use in the UK has been limited by concerns over Clostridium Difficile infection (CDI) 4.
Flucloxacillin is a penicillinase-resistant penicillin with good S. aureus cover. It has very commonly been combined with gentamicin for prophylaxis in both elective orthopaedic and trauma surgery. Indeed, this regime been used in up to 50% of NHS trusts in the UK for prophylaxis 5. Gentamicin, an aminoglycoside, offers activity against gram-negative and gram-positive bacteria including S.aureus. Teicoplanin and Vancomycin, glycopeptides, have been reserved for prophylaxis in patients who are Methicillin Resistant Staphylococcus aureus (MRSA) positive or patients who have a penicillin allergy. Teicoplanin is usually favored over Vancomycin in penicillin allergic patients due to increased development of vancomycin resistance 6.
In an era of evolving antibiotic resistance, vigilant surveillance and judicious use of antibiotics for prophylaxis in trauma surgery is essential to ensure effectiveness as resistance and SSI pose a significant threat to future outcomes. In this prospective observational cohort study, trends in antibiotic prophylaxis and SSI rates in Northern Ireland trauma surgery are reported.
METHODS
The 3 most commonly used antibiotic prophylactic regimes over a 10-year period (2004-2014) were identified from each of the region’s 4 trauma units as well as their dates of introduction to the nearest yearly quarter. For the same period, the total number of trauma procedures carried out and the number of SSIs, were provided by The Public Health Agency (PHA), the statutory custodian of all public health data. This data is collected prospectively from Surgical Site Infection Surveillance forms which are filled out immediately post operatively and returned. Only those with fully completed forms were included. Permission for access to each unit’s data held by the PHA was sought and approved from the relevant clinical lead. Exclusion criteria included day case surgery, failure of return of completed surveillance form, invalid procedures (e.g. diagnostic) and spinal surgery. The antibiotic regime used in each trauma unit, time of use to the nearest yearly quarter, the total number of procedures and subsequent SSIs were recorded. Where the same antibiotic regimes were used across different sites and different times these along with their number of associated SSI were combined for analysis. SSI rates per 100 procedures was calculated and compared between antibiotic regimes. There was no individual patient data collected. Statistical analysis was performed using STATA (IC) Version 4 for Microsoft Excel and the Wilson method for calculating binomial confidence intervals 7.
RESULTS
The 3 different prophylactic regimes included single dose flucloxacillin (2 grams) with single dose gentamicin (3mg/ kg), triple dose cefuroxime (1.5 grams) and single dose cefuroxime (1.5 grams). The protocols for MRSA positive and penicillin allergic patients were the same throughout all hospitals (initially Vancomycin 1 gram single dose then changed to Teicoplanin 10mg/kg single dose).
Flucloxacillin and Gentamicin was used across 3 out of the 4 different trauma units for a combined 13.5 years (total number of years used for each hospital combined). It was the most commonly used regime. Triple dose cefuroxime was used across 2 of the 4 trauma units for a combined 10 years and single dose cefuroxime was also used across 2 of the 4 trauma units for a combined 8 years. From the PHA and after screening for exclusion criteria a total of 26,849 procedures were included in the study. The number of procedures covered and the corresponding antibiotic prophylactic regime usage is shown in Figure 1.
Fig 1.
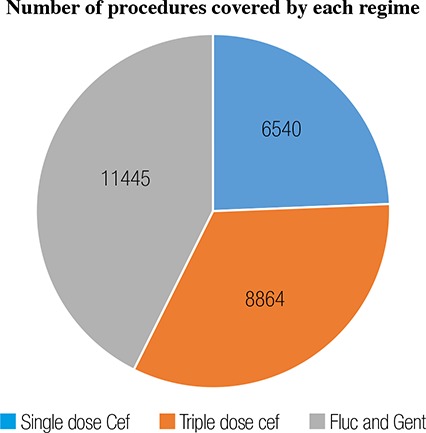
Pie chart showing number of procedures covered by each antibiotic prophylactic regime
Number of procedures covered by each regime
Overall the SSI rate in trauma surgery in Northern Ireland for the 10 years was 1.34%. Flucloxacillin and Gentamicin regime covered 11445 procedures and 82 SSIs were recorded. Triple dose cefuroxime covered 6664 procedures with 218 SSIs and single dose covered 6540 procedures with 60 SSIs. Rate of SSI for each regime is shown in Figure 2.
Fig 2.
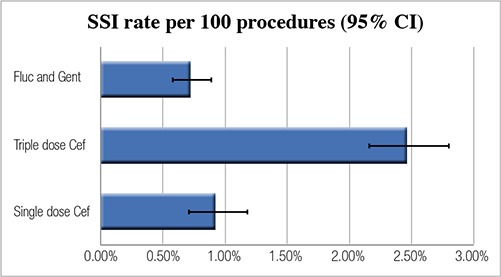
SSI rate (95% confidence interval) and antibiotic prophylactic regime
Fig 3.
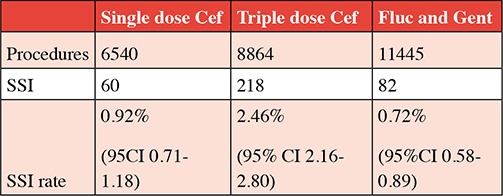
Table of Procedures, Number of SSI and SSI rate
DISCUSSION
The development of SSI is a complex issue. It is multi- factorial and requires best practice to reduce modifiable risk factors. Prophylactic antibiotics are an integral part of trauma care and as such clinicians need to have an up to date understanding of their indications, interactions and associated complications.
In this prospective observational cohort study, we have a single variable (prophylactic antibiotic regime) and a single outcome measure (development of SSI). This is a simplification of a very complex issue, but we believe important points are raised and the strength of the study is enhanced by the large numbers assessed. A clear weakness is not proving the different regimes are statistically similar in terms of other risk factors for development of SSI but it should be highlighted that in the region patient characteristics is unlikely to vary significantly between the different units and therefore the regimes.
In Northern Ireland, Flucloxacillin and Gentamicin is the most commonly used antibiotic regime which corresponds to that of the rest of the UK. It has a very favourable associated SSI rate and, in this study, the lowest. However, it should be noted that concern has arisen from use of this regime with regards to increased risk of acute kidney injury (AKI). Patients undergoing trauma surgery, and in particular, patients with a fractured hip are an at-risk population. Additional risk factors include older age, pre-existing renal impairment, dehydration and concomitant use of diuretics, antihypertensive and non-steroidal anti-inflammatory drugs (NSAIDs). In a large study from Dundee, Scotland 8 of 7666 orthopaedic patients, a change from cefuroxime to flucloxacillin and gentamicin antibiotic prophylaxis was associated with a 94% increase in AKI in orthopaedic trauma surgery and demonstrated that a higher proportion of patients with AKI died within 1 year of surgery than patients without AKI (20.8% versus 8.2% respectively). It is unclear which specific antibiotic is the cause or indeed if it is the combination. Flucloxacillin is associated with acute interstitial nephritis 9 and gentamicin is a direct tubular toxin. The risk of AKI has led to reconsideration of this regime in orthopaedic trauma surgery in Scotland.
Cephalosporins have reduced in use in the UK due to concerns about CDI 5. CDI is an important healthcare associated infection. Antibiotics increase risk of CDI for at least 3 months 10 and even short courses of perioperative antibiotic prophylaxis have been associated with increased risk of CDI particularly in context of established outbreaks11. Third generation cephalosporins have been particularly implicated in CDI and one retrospective review of 625 trauma and orthopaedic patients receiving prophylaxis with cefuroxime compared with 706 patients receiving flucloxacillin and gentamicin showed reduction in CDI from 4% to 1% (p= 0.0004) 12.
In this study, multiple doses of cefuroxime (8864 patients, SSI rate 2.46%) has been associated with an increased risk of SSI compared to a single dose (6540, SSI rate 0.92%) (p<0.001). The reasons for this are not clear. What this study does is add weight to the evidence that there is no increased benefit of multiple dose antibiotic prophylactic regimes over single dose. In a refined meta-analysis reporting outcome for 921 patients who received either single or multiple doses of the same cephalosporin for prophylaxis in hip fracture surgery or closed fracture fixation no significant difference in overall SSI rate was demonstrated 13. A recent review by Bryson et al. highlighted that evidence supporting single dose prophylaxis is not reflected in current practice 6. This suggests a lack of knowledge of current research, fear of SSI or a general aversion to change has made clinicians reluctant to adopt single dose regimes. If there is an associated increase in SSI rate then why do we continue to prescribe multiple doses when there is, in addition, potential to promote resistance, increase risk of hospital acquired infection such as CDI and increase associated costs of intravenous antibiotics, including potential prolonged hospital stay?
One limitation of this study that has already been highlighted is that SSI is a multi-factorial problem and we have only assessed one variable. Additionally, the antibiotic regimes and their date of introduction are to the nearest yearly quarter and so there may have been some overlap when regimes changed. The PHA records do not make note of whether there is a compound injury or indeed if any patients are on antibiotics for a different reason preoperatively. These patient numbers should be very small however. It was not possible to accurately correlate the SSI surveillance form return rate as it was not available for all the years included and for all the units. The PHA previous estimates it to vary between 55-100% in orthopaedic trauma surgery. More consistent higher rates are achieved in elective orthopaedic surgery.
MRSA rates were not assessed in this study and the authors are keen to highlight any effective antibiotic prophylactic protocols are dependent upon robust and efficient pre-operative MRSA screening. The proportion of patients admitted to trauma and orthopaedics in Northern Ireland who are MRSA positive on screening is approximately 1%4. Indeed, it should be noted that MRSA and other antibiotic resistant bacteria are the very reason that studies such as this are important. The threat of increasing bacterial resistance to the future of effective prophylaxis in trauma and orthopaedic is very real. In the United States, at least two million illnesses and 23000 deaths a year are caused by antibiotic resistant bacteria and roughly two in every 100 people carry MRSA 14. While the scale of the problem is not the same in the UK, it may well be in the future and this highlights the importance of judicious use of antibiotics.
CONCLUSION
In this prospective observational cohort study prophylaxis using flucloxacillin and gentamicin was associated with the lowest SSI rate. Although used in fewer procedures, single dose cefuroxime was associated with a lower rate of SSI compared to triple dose. Additional consideration must be given to side effect profiles not assessed in this study. Identification of antibiotic regimes associated with lower SSI rates will promote the judicious use of antibiotics and improve antibiotic stewardship while allowing for continued benefit in the prevention of SSI in an era of ever-increasing antibiotic resistance.
Footnotes
Provenance: externally peer reviewed.
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Boxma H, Broekhuizen T, Patka P, Oosting H. Randomised controlled trial of single dose antibiotic prophylaxis in surgical treatment of closed fractures: The Dutch Trauma Trial. Lancet. 1996;347((9009)):1133–7. doi: 10.1016/s0140-6736(96)90606-6. [DOI] [PubMed] [Google Scholar]
- 2.Public Health Agency. Belfast: Northern Ireland Public Health Agency;; 2012. Northern Ireland point prevalence survey of hospital acquired infections and antimicrobial use. [Google Scholar]
- 3.Public Health England. [Last accessed: 26th January 2019]. Surveillance of surgical site infections in NHS Hospitals in England. April 2016 to March 2017. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/ file/666465/SSI_annual_report_NHS_hospitals_2016-17.pdf. [Google Scholar]
- 4.Mackay DC, Harrison WJ, Bates JH, Dickenson D. Audit of deep wound infection following hip fracture surgery. JR Coll Edinb. 2000;45((1)): 56–9. [PubMed] [Google Scholar]
- 5.Edwards C, Counsell A, Boulton C, Moran CG. Early infection after hip fracture surgery; risk factors, costs and outcome. J Bone Joint Surg Br. 2008;90((6)):770–7. doi: 10.1302/0301-620X.90B6.20194. [DOI] [PubMed] [Google Scholar]
- 6.Bryson DJ, Morris DL, Shivji FS, Rollins KR, Snape S, Ollivere BJ. Antibiotic prophylaxis in orthopaedic surgery. Bone Joint J. 2016;98- B((8)):1014–9. doi: 10.1302/0301-620X.98B8.37359. [DOI] [PubMed] [Google Scholar]
- 7.Wilson EB. Probable inference, the law of succession, and statistical inference. J Am Stat Assoc. 1927;22:209–12. [Google Scholar]
- 8.Bell S, Davey P, Nathwani D, Marwick C, Vadiveloo T, Sneddon J, et al. Risk of AKI with gentamicin as surgical prophylaxis. J Am Soc Nephrol. 2014;25(11):2625–32. doi: 10.1681/ASN.2014010035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pusey CD, Saltissi D, Bloodworth L, Rainford DJ, Christie JL. Drug associated acute intersitital nephritis: clinical and pathological features and response to high dose steroid therapy. Q J Med. 1983;52((206)):194– 211. [PubMed] [Google Scholar]
- 10.Hensgens MP, Goorhuis A, Dekkers OM, Kuijper EJ. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012;67((3)):742–8. doi: 10.1093/jac/dkr508. [DOI] [PubMed] [Google Scholar]
- 11.Carignan A, Allard C, Pépin J, Cossette B, Nault V, Valiquette L. Risk of Clostridium difficile infection after perioperative antibacterial prophylaxis before and during an outbreak of infection due to a hypervirulent strain. Clin Infect Dis. 2008;46((12)):1838–43. doi: 10.1086/588291. [DOI] [PubMed] [Google Scholar]
- 12.Al-Obaydi W, Smith CD, Foguet P. Changing prophylactic antibiotic protocol for reducing Clostridium difficile-associated diarrhoeal infections. Orthop Surg (Hong Kong) 2010;18:320–323. doi: 10.1177/230949901001800312. [DOI] [PubMed] [Google Scholar]
- 13.Morrison S, White N, Asadodallahi S, Lade J. SIngle versus multiple doses of antibiotic prophylaxis in limb fracture surgery. ANZ J Surg. 2012;82((12)):902–7. doi: 10.1111/j.1445-2197.2012.06143.x. [DOI] [PubMed] [Google Scholar]
- 14.Bingyun L, Webster TJ. BacteriaAntibiotic Resistance: New Challenges and Opportunities for Implant-Associated Orthopaedic Infections. J Orthop Res. 2018 Jan;;36((1)):22–32. doi: 10.1002/jor.23656. [DOI] [PMC free article] [PubMed] [Google Scholar]


