The direct ophthalmoscope was first developed in 1851 by Hermann Von Helmholtz (Figure 1).1 Helmholtz noticed that the pupil normally appeared black, but under certain conditions seemed bright and red. He realised that the emitted light was reflected light, and advanced understanding by analysing how the emitted rays formed optical images. In order to obtain an image of the fundus he devised an instrument that would allow his own eye to be placed directly in line with the light rays entering and leaving the eye. Microscopic cover glasses served as mirrors to reflect light, and being transparent, allowed visualisation of the retina.1
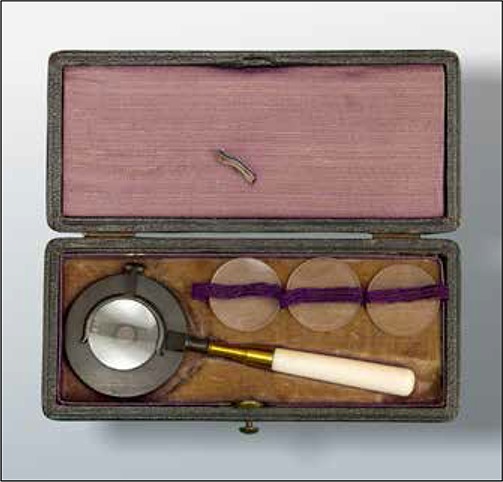
Fig 1.

An example of the first direct ophthalmoscope, Hermann von Helmholtz, 1851, held in the museum of the Royal College of Ophthalmologists’ Collection, London, image courtesy of Mr Richard Keeler
His discovery transformed healthcare. Ophthalmoscopy became an integral part of the general medical examination as the new technology became generally adopted. Richard Liebreich produced an ophthalmoscope which offered a choice of correcting lenses, each held in turn in a clip behind the viewing mirror (Figure 2). It was first produced in the 1860s, and still available 80 years later. In 1880, Pickard and Curry produced an ophthalmoscope with a rotating disc of lenses, and a folding handle (Figure 3) and in 1886, the first ophthalmoscope with a built-in bulb, by Henry Juler, became available. Today technology is similarly developing in ways that would fascinate those who worked to improve the ophthalmoscopes of the 19th century. With little regard for the beauty of the original ophthalmoscopes however, debate exists as to whether the ophthalmoscope still has a place in healthcare education, given the likely advent of mobile retinal imaging systems.
Fig 2.
An example of Richard Liebreich’s ophthalmoscope, c1860, held in the museum of the Royal College of Ophthalmologists’ Collection, London, image courtesy of Mr Richard Keeler.
Fig 3.

Pickard and Curry’s ophthalmoscope, c1880, held in the museum of the Royal College of Ophthalmologists’ Collection, London, image courtesy of Mr Richard Keeler.
Visualising the fundus is a critical skill as identification of retinal signs can be both life-saving and sight saving, as signs may have systemic relevance, for example swollen discs reflecting papilloedema, a retinal vein occlusion as the presenting manifestation of undiagnosed hypertension or a choroidal metastasis from a colorectal carcinoma. For medical students, it has been considered by some unrealistic to expect them to achieve a reliable level ophthalmoscopic proficiency during their course.2 While identification of fundus signs is important, how it is done is not essential.
The direct ophthalmoscope instrument offers several advantages over alternative imaging methods. It gives a x15 magnified view of the fundus, facilitating the appreciation of small changes in the retina, such as small fronds of new blood vessels. Being a ‘live’ imaging system, dynamic changes can also be seen, i.e. venous pulsation at the disc. The ophthalmoscope is widely available and is part of the culture of healthcare such that some medics maintain their ophthalmoscopy skills and can teach others. It is portable and inexpensive, and so can be part of the literal toolbox, for example during home visits where other modalities of ocular fundus examination are unavailable or impractical. It is also useful for patients with low grade nystagmus or unstable visual fixation.3 Educationally, ophthalmoscopy reinforces understanding of ocular anatomy, taking advantage as it does of the accessibility of the eyes to direct visualisation. Also, learning how to perform ophthalmoscopy allows learning of a more generic skill: that of how to interact with patients in seeking their collaboration in what is quite an intimate examination, given the close proximity of patient and doctor during ophthalmoscopy. Thus, having medical students wield the ophthalmoscope allows them to rehearse negotiation with patients on the examination process.
On the other hand, a fundus camera is relatively simple to use with minimal training, as demonstrated in the ‘Fundus photography vs. Ophthalmoscopy Trial Outcomes in the Emergency Department’ (FOTO-ED) study.4 In this study 350 patients presenting to an ED had fundal photos taken by nurse practitioners. The nurse practitioners’ training consisted of written materials, up to 30 minutes of direct training and a period of being observed. The images were then assessed by ophthalmologists. Eighty-three percent of patients had at least one eye with an image of gradable quality, and only 3% had no gradable images. The ease, comfort and speed of obtaining images was rated highly by nurses and patients alike.
The fundus camera has the added ability to zoom-in on areas of interest. A permanent objective record is created which can be kept on file and compared on re-attendance or compared to text books or images online. Lesions can be measured. Patients can be shown their pathology, useful for patient education.
As with radiology and dermatology, retinal photography does not necessarily require an ophthalmologist to be present with the patient, so images can be transmitted for review remotely. Fundus photography also facilitates teaching of signs, in that teaching time is not spent learning the skill of seeing the retina, with the teacher of ophthalmoscopy uncertain as to whether the student has seen the relevant sign or not. This was demonstrated in the ‘Teaching Ophthalmoscopy To Medical Students study’ (The TOTeMS Study) 5, a prospective randomised study comparing direct ophthalmoscopy with non-mydriatic fundus photography for examination of the retina by medical students. Fundal photographs were preferred by 77% of the 138 students, and diagnostic accuracy was significantly better when photographs were used compared to ophthalmoscopy, a difference that persisted when retested one year later. 6 From the patient’s viewpoint, the fundus camera avoids light being shone in the eye for what may be a prolonged period of time during ophthalmoscopy. The disadvantages of ophthalmoscopy and photography are then self-evident.
Ophthalmoscopy is a difficult skill to master for several reasons. The view is time-limited as patients cannot tolerate the examination indefinitely. The view may be made more difficult by media opacities. The field of view is narrow (to visualize the entire retina it would require the clinician to systematically review 172 fields in order not to miss a sizeable lesion of 2 disc diameters). 7 Pharmacological dilatation makes retinal visualization easier but is time-consuming and uncomfortable for the patient. In a questionnaire-based study of 150 medical primary care practitioners, only 53% expressed confidence in using the ophthalmoscope. 8 Merely attempting ophthalmoscopy is said to be not good enough as ocular findings need to be reliably detected, and incompetent ophthalmoscopy may lead the practitioner to mistakenly exclude signs.9 In the FOTO-ED study, comparing ophthalmoscopy to fundal photography in patients presenting to the ED, clinically important signs were missed with ophthalmoscopy.10 Furthermore anecdotally, ophthalmoscopes are sometimes poorly maintained throughout hospitals.
Fundus cameras however, are expensive and not portable. This may all change as novel innovations such as the Peek Retina emerge (https://www.peekvision.org accessed November 2018). Peek Retina is a 0.35kg camera that is clipped onto a smartphone and allows non-mydriatric fundal photography. Validation is ongoing: agreement of cup to disc ratio measurement for example using images taken with the Peek Retina compared to standard fundal photographs has been demonstrated.11 Making fundal photography accessible to all may transform ophthalmic examination, and may have particular impact in the developing world.
In conclusion however, it is the authors’ view that until validation and wide availability of portable digital ophthalmoscopy occurs, direct ophthalmoscopy should still be taught to medical students, but must be done so in the context of its limitations and in the knowledge, that it may not always be the modality of choice for fundus imaging when they graduate. Studies are needed to determine the practice and preferences of medics with regard to fundal visualization.
Footnotes
None of the authors have any conflict of interest to declare.
No funding was sought or supplied for this project.
Provenance: externally peer reviewed.
UMJ is an open access publication of the Ulster Medical Society (http://www.ums.ac.uk).
REFERENCES
- 1.Pearce JM. The ophthalmoscope: Helmholtz’s Augenspiegel. Eur Neurol. 2009;61((4):):244–9. doi: 10.1159/000198418. [DOI] [PubMed] [Google Scholar]
- 2.Ah-Kee E, Husni D, Khan A, Lim LT. An alternative to direct ophthalmoscopy. Clin Teach. 2016;13((4)):316. doi: 10.1111/tct.12506. [DOI] [PubMed] [Google Scholar]
- 3.Mackay DD, Garza PS, Bruce BB, Newman NJ, Biousse V. The demise of direct ophthalmoscopy: A modern clinical challenge. Neurol Clin Pract. 2015;5((2)):150–7. doi: 10.1212/CPJ.0000000000000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bruce BB, Lamirel C, Biousse V, Ward A, Heilpern KL, Newman NJ, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: Phase I of the FOTO-ED study. Acad Emerg Med. 2011;18((9)):928–33. doi: 10.1111/j.1553-2712.2011.01147.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly LP, Garza PS, Bruce BB, Graubart EB, Newman NJ, Biousse V. Teaching ophthalmoscopy to medical students (the TOTeMS study). Am J Ophthalmol. 2013;156((5)):1056–61 e10. doi: 10.1016/j.ajo.2013.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mackay DD, Garza PS, Bruce BB, Bidot S, Graubart EB, Newman NJ, et al. Teaching ophthalmoscopy to medical students (TOTeMS) II: A one-year retention study. Am J Ophthalmol. 2014;157((3)):747–8. doi: 10.1016/j.ajo.2013.12.013. [DOI] [PubMed] [Google Scholar]
- 7.Orlans HO. Direct ophthalmoscopy should be taught within the context of its limitations. Eye (Lond). 2016;30((2)):326–7. doi: 10.1038/eye.2015.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shuttleworth GN, Marsh GW. How effective is undergraduate and postgraduate teaching in ophthalmology? Eye (Lond). 1997;11((Pt 5)):744–50. doi: 10.1038/eye.1997.189. [DOI] [PubMed] [Google Scholar]
- 9.Purbrick RM, Chong NV. Direct ophthalmoscopy should be taught to undergraduate medical students--No. Eye (Lond). 2015;29((8)):990–1. doi: 10.1038/eye.2015.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bruce BB, Lamirel C, Wright DW, Ward A, Heilpern KL, Biousse V, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med. 2011;364((4)):387–9. doi: 10.1056/NEJMc1009733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bastawrous A, Giardini ME, Bolster NM, Peto T, Shah N, Livingstone IA, et al. Clinical validation of a smartphone-based adapter for optic disc imaging in Kenya. JAMA Ophthalmol. 2016;134((2)):151–8. doi: 10.1001/jamaophthalmol.2015.4625. [DOI] [PMC free article] [PubMed] [Google Scholar]


