Abstract
Background:
Data on hypertension among Asian Americans is lacking and often aggregated, which can mask important ethnic differences. This study aims to provide a comprehensive view of hypertension and hypertension related behaviors, including hypertension treatment, management, and information seeking, among Chinese, Korean, and Vietnamese Americans.
Methods:
Data were collected from 600 foreign-born Asian Americans (201 Chinese, 198 Korean, and 201 Vietnamese participants) in the Washington-Baltimore metropolitan area, aged 18 years and over, from 2013–2014. Hypertension was assessed using direct measurement and self-report of having ever been told by a physician. Hypertension prevalence was compared based on the method of assessment, ethnicity, and sex.
Results:
The age-adjusted hypertension prevalence from direct measurement was 27.5%, which is higher than the 2011–2014 National Health and Nutrition Examination Survey estimate for Asians (24.9%). Hypertension prevalences from self-report among Chinese, Korean, and Vietnamese were 13.4%, 23.2%, and 22.9%, respectively, which are lower than 2014 California Health Interview Survey estimates (15.6%, 18.4%, and 25.8%) with the exception of Korean participants. In regards to hypertension-related behaviors, 67.8% of hypertensive adults received management, 64.3% took antihypertensive medication, and 67.0% sought information to improve their hypertension.
Conclusions:
Disaggregated data on hypertension based on measured blood pressure may prevent underestimation from self-report, particularly among those with limited healthcare access. More accurate and objective assessment of hypertension is needed for improved monitoring of hypertension among Asian American subgroups.
Keywords: Asian Americans, hypertension, prevalence, disease management, information seeking behavior
INTRODUCTION
Asian Americans are the fastest growing racial group in the United States, having increased by 43% between 2000 and 2010 [1]. Despite the growth and diversity of this population, there have been limited disaggregated data, particularly related to cardiovascular health [2]. Previous literature has identified Asian Americans as being at lower risk for hypertension than other racial groups. For instance, the American Heart Association estimates that for a 45 year old non-hypertensive individual, the 40-year risk for hypertension is 84.1% for Asians, which is lower than 92.7% among Black, 92.4% among Hispanic, and 86.0% among White adults [3]. In addition, the prevalence of hypertension among Asian Americans has been reported to be lower as compared to other racial/ethnic groups. One study by Yoon et al. examining 2011–2014 National Health and Nutrition Examination Survey (NHANES) data found that non-Hispanic Asians had a lower hypertension prevalence (as determined by systolic blood pressure ≥140, diastolic blood pressure ≥90, or taking blood pressure medication) of 24.9% as compared to non-Hispanic White, non-Hispanic Black, and Hispanic adults (28.0%, 41.2%, and 25.9%, respectively) [4]. Any mention of Hispanic populations in this article refers to Hispanic/Latino populations. Due to such estimates of lower risk and prevalence of cardiovascular risk factors, such as hypertension, cardiovascular health among Asian Americans has often been overlooked. Nevertheless, heart disease, for which hypertension is a well-established contributing risk factor, ranks second in the leading causes of death among Asian Americans [5].
Hypertension is of particular concern given that it is well-known to increase risk for a variety of potentially life threatening conditions such as heart attack, heart failure, stroke, and kidney disease [6]. In addition to hypertension, prehypertension is also known to increase risk of cardiovascular events but less reported in the literature and often missing for Asian Americans [7]. One NHANES study reported prehypertension prevalence to be 31.0% overall being higher in men (39.7%) than women (22.9%) [8]. In terms of race and ethnicity, prehypertension prevalences were only provided for the following categories: non-Hispanic White (31.2%), non-Hispanic Black (30.4%), Mexican American (30.9%), and other (31.0%).
Despite the low prevalence reported for Asian Americans, some studies have found relatively higher hypertension prevalence among several Asian subgroups [9, 10]. In a study observing hypertension among Chinese Americans in San Francisco, aged 19 and older, 69% (n=489), most of which were immigrants from China, were found to have hypertension (defined as having blood pressure higher than 140/90 mmHg or taking antihypertensive medication) [11]. However, this prevalence was not age-adjusted, and participants were mainly older adults (the mean age for the sample was 60 years). In this same study, only 41% reported taking antihypertensive medications among hypertensive participants. In addition, a study by Kim et al. found the prevalence of hypertension to be 32% among Korean American adults, aged 18 and older, in Maryland [12]. Of those who were hypertensive, only 40% of hypertensive Korean Americans were taking medication. Another study among Korean American seniors in the Baltimore, Maryland area revealed that 71.2% were hypertensive, which was higher than that of other racial/ethnic groups of equivalent age (64.3% of White, 70.9% of Black, and 58.1% of Hispanic participants) [13]. Only 23.9% of those with high blood pressure were taking antihypertensive medication. Furthermore, in a study examining 201 Vietnamese-American immigrants from a rural community in the southern U.S., a high hypertension prevalence (as assessed by blood pressure greater than 140/90 mmHg) of 43.7% was also observed [14].
Further reasons why high blood pressure is of major concern among Asian Americans is the low awareness, treatment, and control of hypertension that has been documented [15, 16]. A study based on 2011–2012 NHANES data found that age-adjusted awareness of hypertension (defined as having ever been told by a physician that the individual has hypertension) was similar among non-Hispanic Black (85.7%), non-Hispanic White (82.7%), and Hispanic adults (82.2%), but lower among non-Hispanic Asians (72.8%) [17]. In addition, a 2004–2006 National Health Interview Surveys (NHIS) study found that 17.1% of Chinese, 17.0% of Korean, and 21.6% of Vietnamese Americans have ever been told that they have hypertension as compared to 35.5% of Black and 24.9% of White adults [18]. Likewise in a study of 445 middle-aged Korean Americans with hypertension in the Baltimore-Washington metropolitan area, less than one-third had controlled blood pressure (<140/90 mm Hg) [19].
Health information on Asian Americans and ethnic groups are limited in many large surveys, which often lack sufficient sample sizes for data analysis, particularly after factoring in covariates, and have sampling bias related to language inclusivity (i.e., offering linguistically appropriate materials) during data collection [20]. In addition, data on hypertension among Asian Americans is often presented in aggregate form, which can mask important ethnic differences [21]. The method used to assess hypertension also varies by study, with some surveys using measured blood pressure readings by trained staff and information on antihypertensive medication use, while others have relied on self-report from participants regarding whether a physician has diagnosed them with the condition. Use of these different methods can impact hypertension prevalence, particularly among immigrants who do not have access to healthcare and do not regularly see a physician.
Large epidemiologic studies have measured hypertension in different ways and many, such as the NHIS [22] and Behavioral Risk Factor Surveillance System (BRFSS) [23, 24], have had limited language inclusivity, offering survey materials only in English and Spanish. Others, such as the California Health Interview Survey (CHIS) [25, 26], have conducted data collection using Asian languages (e.g., Chinese, Korean, and Vietnamese) to increase the inclusion of linguistically isolated populations, and more recently, Chinese, Korean, and Vietnamese materials have been included in NHANES after Asian populations began to be oversampled in 2011 [27]. NHIS, BRFSS, and CHIS assess hypertension prevalence using self-report, while NHANES uses both self-report as well as measured blood pressure and anti-hypertensive medication use.
This study aims to examine hypertension prevalence, management, treatment, and health information seeking among Chinese, Korean, and Vietnamese Americans. Moreover, hypertension was assessed in this study using two methods for comparison with other large surveys. Unlike many previous studies that define hypertension based on whether participants have been diagnosed by a physician, bias from a lack of access to health care is reduced in this study by also examining hypertension prevalence based on measured blood pressure readings and inforation on antihypertensive medication.
METHODS
Participant Recruitment and Data Collection.
This study examined data from a randomized controlled trial for a hepatitis B vaccination intervention, which consisted of 600 foreign-born Asian Americans (201 Chinese, 198 Korean, and 201 Vietnamese participants) in the Washington-Baltimore metropolitan area, who were aged 18 years and older. Participants were recruited through various outlets including local community and faith based organizations, community events, health clinics, Asian grocery stores, ethnic newspapers, and personal networks. After informed consent, participants completed a self-administered questionnaire in their preferred language (English, Chinese, Korean, or Vietnamese). Data were collected from April 2013 to March 2014. Further details on recruitment and data collection are described elsewhere [28]. This study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Blood Pressure.
Participants had three blood pressure measurements taken by trained staff at the beginning, middle, and end of the questionnaire using automatic blood pressure monitors. Hypertension was assessed using two methods: (1) measured blood pressure or antihypertensive medication use (henceforth referred to as measured blood pressure) and (2) self-report. For measured blood pressure, the average systolic (SBP) and diastolic blood pressure (DBP) were calculated using the second and third readings to assess blood pressure levels [29, 30]. The second blood pressure reading was used for those missing the third reading (n=2). In classifying measured blood pressure, the following categories were employed based on definitions from the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) and National Heart, Lung, and Blood Institute [6, 31]: low blood pressure (SBP<90 or DBP<60), normal blood pressure (SBP from 90–119 and DBP from 60–79), prehypertension (SBP from 120–139 or DBP from 80–89), and hypertension (SBP≥140 or DBP≥90). Hypertension based on measured blood pressure was defined as any participant having SBP≥140 mmHg, DBP≥90 mmHg, or currently taking antihypertensive medication. Hypertension based on self-report was defined as whether a doctor had ever told participants that they have hypertension or high blood pressure.
Sample Size Ascertainment.
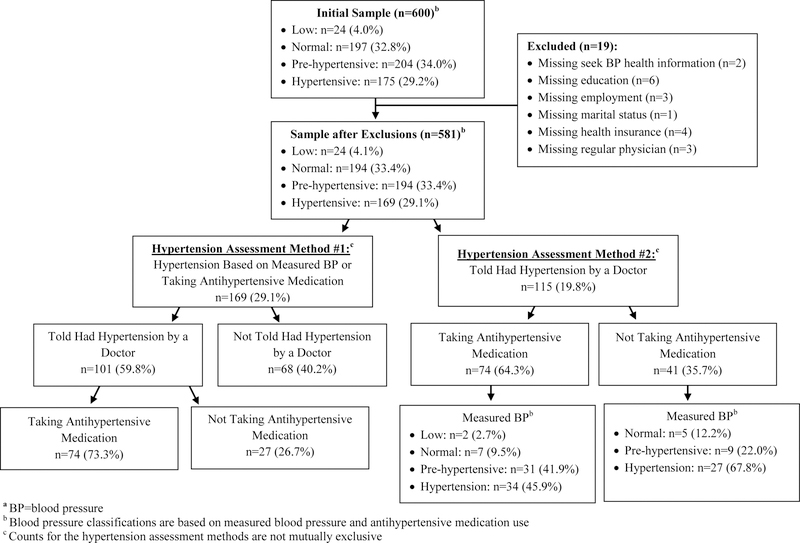
Several sub-samples of the initial 600 participants were examined in this study for different purposes (Fig. 1). The full sample was used to show blood pressure level categories, since all participants had three blood pressure readings, with the exception of two participants missing the third reading. Next, participants missing information on variables on interest including sociodemographic characteristics and hypertension related behavior were excluded, leaving an analytic sample of 581. Among those told by a doctor that they have hypertension (n=115), further sub-samples were examined including participants who were (1) managing their hypertension using diet, exercise, or weight management for high blood pressure, (2) taking antihypertensive medication, and (3) seeking health information to improve their high blood pressure. Health information seeking behavior was examined in the total analytic sample (n=581) and among those taking antihypertensive medication (n=74).
Fig. 1.
Sample size flowchart and blood pressure classifications by hypertension assessment methoda
Statistical Methods.
Descriptive analyses were used to examine variable distributions. T-tests were employed to examine mean differences for continuous variables and chi-square tests, and Fisher’s exact tests were used to examine proportions for categorical variables among non-hypertensive and hypertensive participants (Table 1) as well as for hypertension management, treatment, and information seeking (Table 3). Hypertension prevalence was computed using measured blood pressure and self-report. To make comparisons with 2011–2014 NHANES data from previous literature [4], hypertension prevalences were age-adjusted to the standard 2000 U.S. Census population by the direct method using the following age groups: 18 to 39, 40 to 59, and 60 and older as has been done in previous literature [4, 17]. For comparisons based on self-report, hypertension prevalences calculated from the collected data were compared with those calculated from 2014 CHIS data using weighted analysis given that California has the largest Asian American population among all states, CHIS provides rich data on Asian American subgroups, and CHIS provides self-reported hypertension information based on self-report from subjects. Prevalences and 95% confidence intervals are presented (Table 2). Frequencies for different sources of information are also presented for the total sample and among those taking antihypertensive medication (Table 4). Analyses were conducted using SAS 9.4 (SAS Institute) and weighted data analyses for CHIS data were conducted used survey (svy) commands in STATA 14.
Table 1.
Sample characteristics by hypertension status based on measured blood pressure and antihypertension medication use
| Total (n=581) |
Non-Hypertensive (n=412) |
Hypertensive (n=169) |
p-valuea | |||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Systolic Blood Pressure (mmHg) (mean, SD) | 123.9 | 17.1 | 116.7 | 11.4 | 141.6 | 15.9 | <.001 | |
| Diastolic Blood Pressure (mmHg) (mean, SD) | 77.8 | 11.2 | 73.8 | 8.4 | 87.5 | 11.2 | <.001 | |
| Age | <.001 | |||||||
| 18–39 | 133 | 22.9 | 116 | 28.2 | 17 | 10.1 | ||
| 40–59 | 370 | 63.7 | 257 | 62.4 | 113 | 66.9 | ||
| 60 and older | 78 | 13.4 | 39 | 9.5 | 39 | 23.1 | ||
| Sex | <.001 | |||||||
| Male | 242 | 41.7 | 145 | 35.2 | 97 | 57.4 | ||
| Female | 339 | 58.4 | 267 | 64.8 | 72 | 42.6 | ||
| Ethnicity | 0.043 | |||||||
| Chinese | 198 | 34.1 | 153 | 37.1 | 45 | 26.6 | ||
| Korean | 194 | 33.4 | 134 | 32.5 | 60 | 35.5 | ||
| Vietnamese | 189 | 32.5 | 125 | 30.3 | 64 | 37.9 | ||
| Education | 0.004 | |||||||
| Less than High School | 76 | 13.1 | 43 | 10.4 | 33 | 19.5 | ||
| High School/Vocational School/Some College | 221 | 38.0 | 151 | 36.7 | 70 | 41.4 | ||
| College Graduate | 160 | 27.5 | 120 | 29.1 | 40 | 23.7 | ||
| Graduate School | 124 | 21.3 | 98 | 23.8 | 26 | 15.4 | ||
| Annual Household Income | 0.010 | |||||||
| Less than $20,000 | 146 | 25.1 | 103 | 25.0 | 43 | 25.4 | ||
| $20,000-$39,999 | 148 | 25.5 | 105 | 25.5 | 43 | 25.4 | ||
| $40,000-$59,999 | 101 | 17.4 | 66 | 16.0 | 35 | 20.7 | ||
| $60,000-$79,999 | 46 | 7.9 | 32 | 7.8 | 14 | 8.3 | ||
| $80,000 or More | 126 | 21.7 | 101 | 24.5 | 25 | 14.8 | ||
| Unknown | 14 | 2.4 | 5 | 1.2 | 9 | 5.3 | ||
| Employment Status | 0.054 | |||||||
| Employed | 91 | 15.7 | 69 | 16.8 | 22 | 13.0 | ||
| Unemployed/Student | 386 | 66.4 | 279 | 67.7 | 107 | 63.3 | ||
| Retired/Housewife | 104 | 17.9 | 64 | 15.5 | 40 | 23.7 | ||
| Marital Status | 0.030 | |||||||
| Married | 456 | 78.5 | 318 | 77.2 | 138 | 81.7 | ||
| Separated | 49 | 8.4 | 31 | 7.5 | 18 | 10.7 | ||
| Never Married | 76 | 13.1 | 63 | 15.3 | 13 | 7.7 | ||
| Health Insurance | 0.566 | |||||||
| Yes | 303 | 52.2 | 218 | 52.9 | 85 | 50.3 | ||
| No | 278 | 47.9 | 194 | 47.1 | 84 | 49.7 | ||
| Regular Physician | 0.016 | |||||||
| Yes | 278 | 47.9 | 184 | 44.7 | 94 | 55.6 | ||
| No | 303 | 52.2 | 228 | 55.3 | 75 | 44.4 | ||
| Years of U.S. Residency | 0.326 | |||||||
| 0–5 years | 113 | 19.5 | 81 | 19.7 | 32 | 18.9 | ||
| 6–10 years | 57 | 9.8 | 46 | 11.2 | 11 | 6.5 | ||
| 11–20 years | 161 | 27.7 | 111 | 26.9 | 50 | 29.6 | ||
| More than 20 Years | 171 | 29.4 | 115 | 27.9 | 56 | 33.1 | ||
| Unknown | 79 | 13.6 | 59 | 14.3 | 20 | 11.8 | ||
The p values for mean blood pressure comparisons are from t tests and all others are from χ2 tests
Table 3.
Hypertension management, treatment, and information seeking among hypertensive adults (n=115)
| Hypertension Managementa | Take Antihypertensive Medication | Seek Information to Improve Hypertension | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | No | p-valueb | Yes | No | p-valueb | Yes | No | p-valueb | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |||||
| Total | 78 | 67.8 | 37 | 32.2 | 74 | 64.3 | 41 | 35.7 | 77 | 67.0 | 38 | 33.0 | ||||
| Age | 0.193 | 0.004 | 0.555 | |||||||||||||
| 18–39 | 2 | 2.6 | 4 | 10.8 | 0 | 0.0 | 6 | 14.6 | 3 | 3.9 | 3 | 7.9 | ||||
| 40–59 | 51 | 65.4 | 23 | 62.2 | 51 | 68.9 | 23 | 56.1 | 49 | 63.6 | 25 | 65.8 | ||||
| 60 and older | 25 | 32.1 | 10 | 27.0 | 23 | 31.1 | 12 | 29.3 | 25 | 32.5 | 10 | 26.3 | ||||
| Sex | 0.183 | 0.792 | 0.948 | |||||||||||||
| Men | 36 | 46.2 | 22 | 59.5 | 38 | 51.4 | 20 | 48.8 | 39 | 50.7 | 19 | 50.0 | ||||
| Women | 42 | 53.9 | 15 | 40.5 | 36 | 48.7 | 21 | 51.2 | 38 | 49.4 | 19 | 50.0 | ||||
| Ethnicity | 0.109 | 0.369 | 0.064 | |||||||||||||
| Chinese | 22 | 28.2 | 4 | 10.8 | 17 | 23.0 | 9 | 22.0 | 18 | 23.4 | 8 | 21.1 | ||||
| Korean | 29 | 37.2 | 16 | 43.2 | 32 | 43.2 | 13 | 31.7 | 35 | 45.5 | 10 | 26.3 | ||||
| Vietnamese | 27 | 34.6 | 17 | 46.0 | 25 | 33.8 | 19 | 46.3 | 24 | 31.2 | 20 | 52.6 | ||||
| Education | 0.269 | 0.755 | 0.138 | |||||||||||||
| Less Than High School | 15 | 19.2 | 11 | 29.7 | 18 | 24.3 | 8 | 19.5 | 13 | 16.9 | 13 | 34.2 | ||||
| High School/ Vocational School/ Some College | 33 | 42.3 | 16 | 43.2 | 29 | 39.2 | 20 | 48.8 | 33 | 42.9 | 16 | 42.1 | ||||
| College Graduate | 20 | 25.6 | 9 | 24.3 | 19 | 25.7 | 10 | 24.4 | 22 | 28.6 | 7 | 18.4 | ||||
| Graduate School | 10 | 12.8 | 1 | 2.7 | 8 | 10.8 | 3 | 7.3 | 9 | 11.7 | 2 | 5.3 | ||||
| Annual Household Income | 0.300 | 0.418 | 0.317 | |||||||||||||
| Less than $20,000 | 16 | 20.5 | 15 | 40.5 | 17 | 23.0 | 14 | 34.2 | 18 | 23.4 | 13 | 34.2 | ||||
| $20,000-$39,999 | 23 | 29.5 | 9 | 24.3 | 21 | 28.4 | 11 | 26.8 | 20 | 26.0 | 12 | 31.6 | ||||
| $40,000-$59,999 | 15 | 19.2 | 7 | 18.9 | 16 | 21.6 | 6 | 14.6 | 18 | 23.4 | 4 | 10.5 | ||||
| $60,000-$79,999 | 7 | 9.0 | 2 | 5.4 | 4 | 5.4 | 5 | 12.2 | 8 | 10.4 | 1 | 2.6 | ||||
| $80,000 or More | 12 | 15.4 | 3 | 8.1 | 12 | 16.2 | 3 | 7.3 | 9 | 11.7 | 6 | 15.8 | ||||
| Unknown | 5 | 6.4 | 1 | 2.7 | 4 | 5.4 | 2 | 4.9 | 4 | 5.2 | 2 | 5.3 | ||||
| Employment Status | 0.892 | 0.522 | 0.564 | |||||||||||||
| Employed | 11 | 14.1 | 6 | 16.2 | 10 | 13.5 | 7 | 17.1 | 13 | 16.9 | 4 | 10.5 | ||||
| Unemployed/Student | 45 | 57.7 | 22 | 59.5 | 46 | 62.2 | 21 | 51.2 | 45 | 58.4 | 22 | 57.9 | ||||
| Retired/Housewife | 22 | 28.2 | 9 | 24.3 | 18 | 24.3 | 13 | 31.7 | 19 | 24.7 | 12 | 31.6 | ||||
| Marital Status | 0.235 | 0.027 | 0.013 | |||||||||||||
| Married | 67 | 85.9 | 28 | 75.7 | 65 | 87.8 | 30 | 73.2 | 69 | 89.6 | 26 | 68.4 | ||||
| Separated | 10 | 12.8 | 7 | 18.9 | 9 | 12.2 | 8 | 19.5 | 7 | 9.1 | 10 | 26.3 | ||||
| Never Married | 1 | 1.3 | 2 | 5.4 | 0 | 0.0 | 3 | 7.3 | 1 | 1.3 | 2 | 5.3 | ||||
| Health Insurance | 0.972 | 0.393 | 0.543 | |||||||||||||
| Yes | 34 | 43.6 | 16 | 43.2 | 30 | 40.5 | 20 | 48.8 | 35 | 45.5 | 15 | 39.5 | ||||
| No | 44 | 56.4 | 21 | 56.8 | 44 | 59.5 | 21 | 51.2 | 42 | 54.6 | 23 | 60.5 | ||||
| Regular Physician | 0.001 | 0.004 | 0.009 | |||||||||||||
| Yes | 54 | 69.2 | 14 | 37.8 | 51 | 68.9 | 17 | 41.5 | 52 | 67.5 | 16 | 42.1 | ||||
| No | 24 | 30.8 | 23 | 62.2 | 23 | 31.1 | 24 | 58.5 | 25 | 32.5 | 22 | 57.9 | ||||
| Years of U.S. Residency | 0.196 | 0.509 | 0.213 | |||||||||||||
| 0–5 years | 11 | 14.1 | 9 | 24.3 | 13 | 17.6 | 7 | 17.1 | 10 | 13.0 | 10 | 26.3 | ||||
| 6–10 years | 6 | 7.7 | 3 | 8.1 | 4 | 5.4 | 5 | 12.2 | 5 | 6.5 | 4 | 10.5 | ||||
| 11–20 years | 28 | 35.9 | 6 | 16.2 | 25 | 33.8 | 9 | 22.0 | 27 | 35.1 | 7 | 18.4 | ||||
| More than 20 Years | 23 | 29.5 | 11 | 29.7 | 20 | 27.0 | 14 | 34.2 | 22 | 28.6 | 12 | 31.6 | ||||
| Unknown | 10 | 12.8 | 8 | 21.6 | 12 | 16.2 | 6 | 14.6 | 13 | 16.9 | 5 | 13.2 | ||||
Hypertension management was defined as the use of diet, exercise, or weight management for high blood pressure among those who were aware of hypertension
The p values are from Fisher’s exact tests for age group, income, and marital status and χ2 tests for all other variables
Table 2.
Hypertension prevalence by race/ethnicity and sex based on the hypertension assessment methoda
| Data Source | Race/Ethnicity | Hypertension
Prevalence |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Men | Women | ||||||||
| % | (95% CI) | % | (95% CI) | % | (95% CI) | |||||
| Hypertension Based on Measured Blood Pressure and Antihypertensive Medication Useb | ||||||||||
| Current Study, 2013–2014 | Asian (n=600) | 27.5 | (23.4–31.5) | 38.7 | (31.2–46.2) | 18.7 | (14.4–23.0) | |||
| Chinese (n=201) | 21.8 | (15.5–28.0) | 33.3 | (21.0–45.6) | 12.1 | (6.5–17.7) | ||||
| Korean (n=198) | 29.9 | (22.4–37.3) | 37.3 | (24.6–50.0) | 25.4 | (16.2–34.7) | ||||
| Vietnamese (n=201) | 31.9 | (24.2–39.5) | 45.9 | (32.0–59.8) | 16.1 | (9.8–22.4) | ||||
| NHANES, 2011–2014c | All Race/Ethnicities | 29.0 | - | 30.0 | - | 28.1 | - | |||
| Non-Hispanic White | 28.0 | - | 29.4 | - | 26.5 | - | ||||
| Non-Hispanic Black | 41.2 | - | 40.8 | - | 41.5 | - | ||||
| Non-Hispanic Asian | 24.9 | - | 26.5 | - | 23.5 | - | ||||
| Hispanic | 25.9 | - | 25.4 | - | 26.2 | - | ||||
| Hypertension Based on Self-Reportd | ||||||||||
| Current Study, 2013–2014 | Asian (n=600) | 19.8 | (16.7–23.3) | 24.2 | (19.1–30.0) | 16.7 | (12.9–21.0) | |||
| Chinese (n=201) | 13.4 | (9.0–18.9) | 15.5 | (8.5–25.0) | 12.0 | (6.7–19.3) | ||||
| Korean (n=198) | 23.2 | (17.4–29.1) | 27.8 | (18.4–39.1) | 20.2 | (13.4–28.5) | ||||
| Vietnamese (n=201) | 22.9 | (17.3–29.3) | 29.2 | (20.1–39.8) | 17.9 | (11.3–26.2) | ||||
| CHIS, 2014e | Asian (n=1,220) | 22.9 | (19.1–27.1) | 24.7 | (19.7–30.4) | 21.2 | (16.7–26.5) | |||
| Chinese (n=598) | 15.6 | (10.5–22.6) | 12.2 | (7.4–19.6) | 18.3 | (10.7–29.7) | ||||
| Korean (n=216) | 18.4 | (12.1, 27.1) | 27.2 | (15.4–43.3) | 13.8 | (7.9–22.8) | ||||
| Vietnamese (n=406) | 25.8 | (16.9–37.1) | 30.9 | (16.6–50.1) | 20.8 | (12.9–31.9) | ||||
NHANES National Health and Nutrition Examination Survey; CHIS California Health Interview Survey; 95% CI 95% Confidence Interval
Hypertension was defined as having measured SBP ≥140 mmHg, DBP ≥90 mmHg, or currently taking antihypertensive medication (Hypertension prevalence estimates were age-adjusted to the 2000 U.S. Census population by the direct method using the following age groups: 18–39, 40–59, and 60 and over)
Hypertension estimates using NHANES data are from the following source: Yoon SS, Fryar CD, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief. 2015(220):1–8 (Sample sizes and 95% CI intervals were not provided)
Hypertension was defined as having a doctor ever tell participants that they have high blood pressure
Hypertension prevalence from 2014 CHIS data was calculated using weighted data analysis in STATA
Table 4.
Sources of health information
| Information Sourcea | Total
Sample (n=581)b |
Hypertensive Adults
taking Antihypertensive Medication (n=74)c |
||
|---|---|---|---|---|
| n | % | n | % | |
| Printed Health Information in a Hospital/Clinic/Pharmacy | 515 | 88.6 | 6 | 8.1 |
| Doctor | 408 | 70.2 | 70 | 94.6 |
| Internet/Computer | 284 | 48.9 | 12 | 16.2 |
| Friends | 137 | 23.6 | 7 | 9.5 |
| Family | 128 | 22.0 | 8 | 10.8 |
| Smartphone | 55 | 9.5 | 2 | 2.7 |
| Pharmacist | 44 | 7.6 | 3 | 4.1 |
| General Print Materials (e.g., Newspaper, Magazine, and Book) | 11 | 1.9 | - | - |
| Community Resources or Events | 4 | 0.7 | - | - |
Information sources are not mutually exclusive
Participants were asked where they usually seek health information. Out of 581 participants, 576 selected at least one information source
Participants were asked where they seek information regarding questions about their antihypertensive medication (Out of 74 participants who were taking antihypertensive medication, 73 selected at least one information source)
RESULTS
When examining the full initial dataset (n=600), 4.0% had low blood pressure (n=24), 32.8% had normal blood pressure (n=197), 34.0% had prehypertension (n=204), and 29.2% had hypertension (n=175) based on measured blood pressure (Figure 1). Hypertension prevalence was found to differ based on the method of assessment and was higher based on measured blood pressure than self-report (29.1% vs. 19.8%). Among those with a self-reported hypertension diagnosis, 64.3% were taking antihypertensive medication and 45.9% of these patients were still hypertensive based on measured blood pressure. In the final analytic sample (n=581), hypertensive participants, as assessed using measured blood pressure, tended to be older, male, Vietnamese, less educated, have lower income, be married, and have a regular physician as compared to those who were non-hypertensive (Table 1).
Based on measured blood pressure, the overall age-adjusted hypertension prevalence was 27.5%, which is higher than that found using 2011–2014 NHANES data on Asian Americans (24.9%) (Table 2) [4]. As in this study, NHANES assessed hypertension using measured blood pressure readings and antihypertensive medication use. For comparability, hypertension prevalences based on measured blood pressure in this study were age-adjusted to the 2000 U.S. Census population. The age-adjusted prevalences of hypertension among Chinese, Korean, and Vietnamese in the current study were 21.8%, 29.9%, and 31.9%, respectively. Hypertension prevalence varied by race/ethnicity and sex. Compared to 2011–2014 NHANES data, the hypertension prevalences for Korean and Vietnamese Americans were higher than that among non-Hispanic White adults (28.0%), and Vietnamese men had the highest prevalence (45.9%) compared to men of all other racial/ethnic groups (25.4%−40.8%) [4].
CHIS assesses hypertension based on self-report by participants of whether a doctor has told them that they have high blood pressure. Given that this information was also collected in this study, crude hypertension prevalences based on self-report from the current study were compared with weighted hypertension prevalences calculated using 2014 CHIS data (Table 2). In this study, 13.4% of Chinese, 23.2% of Korean, 22.9% of Vietnamese, and 19.8% overall were hypertensive based on self-report. All hypertension prevalences found using 2014 CHIS data were lower, with the exception of among Korean Americans (23.2% in this study vs. 18.4% using 2014 CHIS data) [25]. In addition, there were significant sex differences in overall hypertension prevalence (24.2% for men vs. 16.7% for women) in this study, which were primarily driven by differences among Vietnamese participants (29.2% for men vs. 17.9% for women). Similarly, men had a higher hypertension prevalence than women based on 2014 CHIS data (24.7% for men and 21.2% for women overall) specifically among Koreans (27.2% for men and 13.8% for women) and Vietnamese subjects (30.9% for men and 20.8% for women).
Table 3 presents findings on hypertension management, treatment, and information seeking. Having a regular physician promoted healthier behaviors related to hypertension. Compared to those who do not, those undergoing hypertension management (i.e., through diet, exercise, or weight management) (69.2% vs. 37.8%), taking antihypertensive medication (68.9% vs. 41.5%), and seeking information to improve their hypertension (67.5% vs. 42.1%) tended to have a regular physician.
Table 4 presents sources of health information as reported by participants. The top five sources reported in the total sample (n=581) were printed health information from hospitals, clinics, and pharmacies (88.6%); a doctor (70.2%); the internet/computer (48.9%); friends (23.6%); and family (22.0%). Others included smartphones, pharmacists, general print materials (e.g., newspapers, magazines, and books), and community resources or events. Specifically among hypertensive adults taking antihypertensive medication (n=74), the top five sources of information were a doctor (94.6%), the internet/computer (16.2%), family (10.8%), friends (9.5%), and printed health information from hospitals, clinics, and pharmacies (8.1%).
DISCUSSION
In this study, the prevalence of hypertension was shown to be greatly dependent on the method of assessment. Although not statistically different, the prevalence of hypertension based on measured blood pressure and antihypertensive medication use among Asian Americans was higher in this study than among Asian Americans using 2011–2014 NHANES data (27.5% vs. 24.9%), while hypertension prevalences among Korean and Vietnamese Americans were found to be also higher than some other racial groups, including non-Hispanic White and Hispanic adults [17, 4]. Similar to our findings using measured blood pressure, a study examining 2003–2005 NHIS data found that Chinese adults (OR=0.75; 95% CI: 0.59–0.96) and other Asian adults (OR=0.69; 95% CI: 0.54–0.85) were less likely to have hypertension (as determined by whether a doctor told participants they had hypertension) compared to non-Hispanic Whites [32].
When examining hypertension based on self-report, the hypertension prevalence for Asians overall, Chinese, and Vietnamese participants in this study were lower as compared to 2014 CHIS data, while that for Koreans participants was higher. These dissimilarities between our data and 2014 CHIS data may be a result of differences in the sociodemographic characteristics of the samples. Specifically, there was a smaller percentage of Chinese (41.8% men in our sample vs. 44.3% men in 2014 CHIS) and Vietnamese men (44.3% men in our sample vs. 49.1% men in 2014 CHIS) than women and larger percentage of Korean men (39.9% men in our sample vs. 34.7% men in 2014 CHIS) than women in our sample as compared to the 2014 CHIS sample. Considering that men are known to have greater risk for hypertension than women of similar ages [33], this may be one contributing factor. Furthermore, in regards to treatment, there were fewer individuals on antihypertensive medication in this study (64.3% vs. 73.5%−77.4%) as compared to other racial groups nationally based on NHANES data [17].
Based on a prior study using 2011 BRFSS data, a lack of access to healthcare was noted as an issue among those with self-reported hypertension, with 19.1% having no health insurance, 18.1% having no regular doctor, and 23.6% being unable to visit a doctor because of costs [34]. In this study, having a regular physician was found to significantly differ among those with healthier hypertension behaviors. Specifically, more individuals who practiced hypertension management, were taking antihypertensive medication, and sought information to improve their hypertension reported having a regular physician as compared to those who did not. Additionally, another study found that among adults with cardiovascular disease and hypertension, Asian adults had fewer doctor visits (4.6±0.3 visits per year) compared to non-Hispanic White adults (6.7±0.2 visits per year) based on 2011 to 2012 CHIS data [35].
Previous literature suggests that cultural and language barriers, low health literacy, economic difficulties, limited health access, lack of health insurance, self-efficacy can contribute to lower antihypertensive medication use and hypertension management behaviors [11, 36–38]. Moreover, prior literature has suggested that some Asian Americans do not fully understood the cause and prevention of hypertension and heart disease [37]. Thus, interventions that use interpreter services, increase access to medical insurance, provide translated educational materials, and organize community fairs could be valuable in addressing the need for cultural sensitivity and appropriate approaches for Asian American subgroups [12, 14, 37, 39]. Based on the findings from this study, future interventions addressing these barriers could incorporate printed health information in medical facilities, doctors, and the internet, given that these were the top resources for general health information and information on antihypertensive medication. These resources can be important targets for promoting hypertension management and treatment in future interventions in this population.
A limitation of this study is its generalizability given that a non-probability sampling method was employed and all participants were foreign-born. In addition, all subjects resided in the Washington-Baltimore metropolitan area and many subjects were highly educated (49% received a college or graduate school education as shown in Table 1), which could impact comparisons with other Asian American populations including those from NHANES and CHIS. However, this study provides a descriptive look at hypertension among three Asian American subgroups, which is a strength given that the majority of past data presents aggregated estimates of very heterogeneous Asian subgroups [40]. In previous literature, hypertension prevalence among Asian Americans has often been reported based on self-report of a doctor’s diagnosis of hypertension [41], which is likely to lead to underestimation of the true prevalence due to a lack of access to care among many Asian American immigrants [42]. Another strength of the current study is the inclusion of objective measures to determine hypertension status. Furthermore, given that hypertension has been assessed differently in previous studies, the comparability of our findings were improved by assessing hypertension using objective measurements and self-report as well as by using age-adjusted estimates for comparison with NHANES data.
The prevalence of hypertension was shown to be greatly dependent on the method of assessment with prevalence based on measured blood pressure and antihypertensive medication use resulting in higher estimates than self-report. Thus, hypertension prevalence based on self-report may exclude those at high risk, who have limited access to health care or no regular physician, potentially leading to an underestimation of the true prevalence [43]. Thus, varying prevalence in the literature for Asian Americans may result from different definitions of hypertension (e.g., objectively measured blood pressure versus self-report), healthcare access and utilization, as well as language barriers, which may result in the exclusion of non-English speaking Asian Americans in survey data collection. The considerable racial/ethnic and sex variation in hypertension prevalence underscores the need for disaggregated blood pressure data among Asian American subgroups. Better assessment of hypertension is needed for improved understanding and monitoring of hypertension in this population.
Acknowledgment:
Funding: This study was supported by the National Cancer Institute (R01CA163805).
Footnotes
Compliance with Ethical Standards
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical approval: All procedures performed involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants in the study.
Contributor Information
Mary Y. Jung, University of Maryland School of Public Health, Department of Epidemiology and Biostatistics, 4200 Valley Drive, College Park, Maryland 20742, USA.
Sunmin Lee, University of Maryland School of Public Health, Department of Epidemiology and Biostatistics, 4200 Valley Drive, College Park, Maryland 20742, USA.
Stephen B. Thomas, University of Maryland School of Public Health, Department of Health Services Administration, 4200 Valley Drive, College Park, Maryland 20742, USA.
Hee-Soon Juon, Thomas Jefferson University, Department of Medical Oncology, Division of Population Science, 834 Chestnut St, Philadelphia, Pennsylvania, USA.
REFERENCES
- 1.Hoeffel EM, Rastogi S, Kim MO, Hasan S. The Asian population: 2010. In: 2010 U.S. Census Briefs. U.S. Department of Commerce, Economics and Statistics Administration, U.S. Census Bureau 2012. https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. Accessed December 14 2017.
- 2.Palaniappan LP, Araneta MRG, Assimes TL, Barrett-Connor EL, Carnethon MR, Criqui MH et al. Call to action: cardiovascular disease in Asian Americans a science advisory from the American Heart Association. Circulation 2010;122(12):1242–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation 2016;133(4):e38–e360. [DOI] [PubMed] [Google Scholar]
- 4.Yoon SS, Fryar CD, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS Data Brief 2015(220):1–8. [PubMed] [Google Scholar]
- 5.Hastings KG, Jose PO, Kapphahn KI, Frank AT, Goldstein BA, Thompson CA et al. Leading causes of death among Asian American subgroups (2003–2011). PLoS One 2015;10(4):e0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003;289(19):2560–71. [DOI] [PubMed] [Google Scholar]
- 7.Pimenta E, Oparil S. Prehypertension: epidemiology, consequences and treatment. Nat Rev Nephrol 2010;6(1):21–30. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med 2004;164(19):2126–34. [DOI] [PubMed] [Google Scholar]
- 9.Zhao B, Jose PO, Pu J, Chung S, Ancheta IB, Fortmann SP et al. Racial/ethnic differences in hypertension prevalence, treatment, and control for outpatients in northern California 2010–2012. Am J Hypertens 2015;28(5):631–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kramer H, Han C, Post W, Goff D, Diez-Roux A, Cooper R et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Hypertens 2004;17(10):963–70. [DOI] [PubMed] [Google Scholar]
- 11.Lau DS, Lee G, Wong CC, Fung GL, Cooper BA, Mason DT. Characterization of systemic hypertension in the San Francisco Chinese community. Am J Cardiol 2005;96(4):570–3. [DOI] [PubMed] [Google Scholar]
- 12.Kim MT, Kim KB, Juon HS, Hill MN. Prevalence and factors associated with high blood pressure in Korean Americans. Ethn Dis 2000;10(3):364–74. [PubMed] [Google Scholar]
- 13.Kim MT, Juon HS, Hill MN, Post W, Kim KB. Cardiovascular disease risk factors in Korean American elderly. Western J Nurs Res 2001;23(3):269–82. [DOI] [PubMed] [Google Scholar]
- 14.Duong DA, Bohannon AS, Ross MC. A descriptive study of hypertension in Vietnamese Americans. J Community Health Nurs 2001;18(1):1–11. [DOI] [PubMed] [Google Scholar]
- 15.Watson RE, Karnchanasorn R, Gossain VV. Hypertension in Asian/Pacific Island Americans. J Clin Hypertens 2009;11(3):148–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith SC, Clark LT, Cooper RS, Daniels SR, Kumanyika SK, Ofili E et al. Discovering the full spectrum of cardiovascular disease minority health summit 2003: report of the obesity, metabolic syndrome, and hypertension writing group. Circulation 2005;111(10):e134–e9. [DOI] [PubMed] [Google Scholar]
- 17.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief 2013(133):1–8. [PubMed] [Google Scholar]
- 18.Barnes PM, Adams PF, Powell-Griner E. Health characteristics of the Asian adult population: United States, 2004–2006. Adv Data 2008;(394):1–22. [PubMed] [Google Scholar]
- 19.Han H-R, Kim KB, Kang J, Jeong S, Kim E-Y, Kim MT. Knowledge, beliefs, and behaviors about hypertension control among middle-aged Korean Americans with hypertension. J Community Health 2007;32(5):324–42. [DOI] [PubMed] [Google Scholar]
- 20.Devers K, Gray B, Ramos C, Shah A, Blavin F, Waidmann T. The feasibility of using Electronic Health Records (EHRs) and other electronic health data for research on small populations. The Urban Institute Health Policy Center, Washington, DC: 2013. https://aspe.hhs.gov/report/feasibility-using-electronic-health-data-research-small-populations. Accessed December 14 2016. [Google Scholar]
- 21.Jose P, Zhao B, Baek M, Chung S, Fortmann S, Palaniappan L. Variation in hypertension prevalence among Asian American subgroups: results from Pacs (Pan Asian Cohort Study). Clin Med Res 2013;11(3):136. [Google Scholar]
- 22.Centers for Disease Control and Prevention/National Center for Health Statistics. 2015 National Health Interview Survey Questionnaire- Sample Adult Hyattsville, Maryland: U.S. Department of Health and Human Services; 2016. ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2015/english/qadult.pdf. Accessed 12 December 2018. [Google Scholar]
- 23.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System 2015 codebook report land-line and cell-phone data Atlanta, Georgia: U.S. Department of Health and Human Services; 2016. https://www.cdc.gov/brfss/annual_data/2017/pdf/codebook17_llcp-v2-508.pdf. Accessed 12 December 2018. [Google Scholar]
- 24.National Center for Chronic Disease Prevention and Health Promotion. Division of Population Health. BRFSS frequently asked questions (FAQs) U.S. Department of Health & Human Services, Atlanta, GA: 2015. http://www.cdc.gov/brfss/about/brfss_faq.htm. Accessed December 14 2017. [Google Scholar]
- 25.California Health Interview Survey. CHIS 2014 adult survey public use file. [computer file] Los Angeles, CA: UCLA Center for Health Policy Research; July 2017. http://healthpolicy.ucla.edu/chis/data/Pages/public-use-data.aspx. Accessed 12 December 2018. [Google Scholar]
- 26.UCLA Center for Health Policy Research. CHIS methods to accurately represent California’s diverse population. In: CHIS Data Quality 2012. http://healthpolicy.ucla.edu/chis/design/Pages/data-quality7.aspx. Accessed August 26 2016.
- 27.Centers for Disease Control and Prevention/National Center for Health Statistics. NHANES 2011–2012 questionnaire data overview: questionnaire and interview languages U.S. Department of Health & Human Services, Atlanta, GA: 2014. https://wwwn.cdc.gov/nchs/nhanes/ContinuousNhanes/OverviewQuex.aspx?BeginYear=2011. Accessed 12 December 2018. [Google Scholar]
- 28.Juon H-S, Strong C, Kim F, Park E, Lee S. Lay health worker intervention improved compliance with hepatitis B vaccination in Asian Americans: randomized controlled trial. PLoS One 2016;11(9):e0162683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daskalopoulou SS, Rabi DM, Zarnke KB, Dasgupta K, Nerenberg K, Cloutier L et al. The 2015 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol 2015;31(5):549–68. [DOI] [PubMed] [Google Scholar]
- 30.Eguchi K, Kuruvilla S, Ishikawa J, Ogedegbe G, Gerin W, Schwartz JE et al. Correlations between different measures of clinic, home, and ambulatory blood pressure in hypertensive patients. Blood Press Monit 2011;16(3):142–8. [DOI] [PubMed] [Google Scholar]
- 31.National Heart L, and Blood Institute. What Is hypotension? National Institutes of Health, Bethesda, MD: 2010. https://www.nhlbi.nih.gov/health/health-topics/topics/hyp. Accessed July 15 2017. [Google Scholar]
- 32.Ye J, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol 2009;19(10):718–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Reckelhoff JF. Gender differences in the regulation of blood pressure. Hypertension 2001;37(5):1199–208. [DOI] [PubMed] [Google Scholar]
- 34.Fang J, Yang Q, Ayala C, Loustalot F. Disparities in access to care among US adults with self-reported hypertension. Am J Hypertens 2014;27(11):1377–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tran H, Do V, Baccaglini L. Health Care Access, Utilization, and Management in Adult Chinese, Koreans, and Vietnamese with Cardiovascular Disease and Hypertension. J Racial Ethn Health Disparities 2016;3(2):340–8. [DOI] [PubMed] [Google Scholar]
- 36.Lee J-E, Han H-R, Song H, Kim J, Kim KB, Ryu JP et al. Correlates of self-care behaviors for managing hypertension among Korean Americans: a questionnaire survey. Int J Nurs Stud 2010;47(4):411–7. [DOI] [PubMed] [Google Scholar]
- 37.Pham TM, Rosenthal MP, Diamond JJ. Hypertension, cardiovascular disease, and health care dilemmas in the Philadelphia Vietnamese community. Fam Med 1999;31:647–51. [PubMed] [Google Scholar]
- 38.Vawter L, Tong X, Gemilyan M, Yoon PW. Barriers to antihypertensive medication adherence among adults—United States, 2005. J Clin Hypertens 2008;10(12):922–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ferdinand KC. Hypertension in minority populations. J Clin Hypertens 2006;8(5):365–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Souza RJ, Anand SS. Cardiovascular disease in Asian Americans: unmasking heterogeneity. J Am Coll Cardiol 2014;64(23):2495–7. [DOI] [PubMed] [Google Scholar]
- 41.Ma GX, Lee M, Bhimla A, Tan Y, Gadegbeku CA, Yeh MC et al. Risk assessment and prevention of hypertension in Filipino Americans. J Community Health 2017;42(4):797–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clough J, Lee S, Chae DH. Barriers to health care among Asian immigrants in the United States: a traditional review. J Health Care Poor Underserved 2013;24(1):384–403. [DOI] [PubMed] [Google Scholar]
- 43.Vargas CM, Burt VL, Gillum RF, Pamuk ER. Validity of self-reported hypertension in the National Health and Nutrition Examination Survey III, 1988–1991. Prev Med 1997;26(5):678–85. [DOI] [PubMed] [Google Scholar]