Abstract
Background:
Disability in older adults leads to poor quality of life, is costly for the health system and is a risk for mortality. Little is known about disability in older immigrants to the United States.
Objective:
To synthesize the evidence on the prevalence and factors associated with disability in older adult immigrants.
Methods:
We conducted searches in PubMed, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Scopus. Disability was defined as difficulty in performing basic or instrumental activities of daily living. Older adult was defined as 65 years and older. Immigrant status was defined as someone born outside of the United States.
Results:
Eighteen articles met the inclusion criteria. Seven studied Hispanic/Latino immigrants, 6 studied Asian immigrants, 4 studied diverse older immigrant samples, and one studied European immigrants. Prevalence of disability ranged from 2% to 49% in Asians, and 3% to 58.1% in Hispanic/Latinos. In a diverse sample of immigrants, the prevalence of disability was 19.3%. Correlates of disability included female gender, low income, limited education, single status, migration in late adulthood, obesity, arthritis, and diabetes. Factors protective against disability in older adult immigrants were: acculturation, migrating at a younger age, exercise, alcohol intake, and church attendance.
Conclusion:
Disability prevalence was generally lower in Asian immigrants compared to Hispanic/Latino immigrants. Identification of the precise rates and factors associated with disability in older immigrants can inform health interventions for this population.
Keywords: Immigrants, Older adults, Disability, Activities of Daily Living, Instrumental Activities of Daily Living
Introduction
Disability is an important outcome of age-related changes and chronic illness in older adults worldwide [1]. Disability is an umbrella term for impairments, activity limitations, and participation restrictions [2]. Between 110 million and 190 million people worldwide have a disability [2]. Disability is reported by 60% of older adults in the United States (U.S.) [3]. Disability status increases with age [4–6] and is more common among women[4, 7, 8], minorities[8], persons with less than a high school education[9], and low socioeconomic status[10, 11]. Medical conditions associated with disability in U.S born older adults are diabetes [7, 12, 13], musculoskeletal disorders [6, 7], stroke [4, 5, 7, 12, 13], vision impairment [5, 13], depression [5, 6, 14], arthritis [5, 6, 12, 13], hypertension [6, 12], obesity [5, 6, 13], and hearing impairment [13]. Understanding the prevalence and risk factors for disability can inform prevention and treatment of disability in older adults.
Currently numbering over 43 million, the U.S. immigrant population is growing rapidly [15]. Older immigrants make up 11.9% of older adults in the U.S. [16, 17]. Most older adult immigrants are Hispanic/Latinos (38%), followed by Asians (29%), and Europeans (28%) [17]. The growth of the older immigrant population is attributable to the aging of current adult immigrants and the influx of middle-age and older adults through immigration programs such as the Family Reunification policy [16] and the Diversity Lottery program. The number of older immigrants admitted into legal permanent residency in the past ten years has doubled [18]. In 2015, approximately 59,000 adults over 65 years gained legal permanent residency status, a significant increase from 48,000 two years before [19]. It is projected that in the next four decades, 42% of the older adults will be minorities [20]. Aging immigrants will be a significant contributor to the projected increase in the racial and ethnic diversity in the older adult population [21, 22]. Most immigrants arrive in the U.S. without disabilities, but the aging process combined with health issues and socioeconomic inequity in immigrants may contribute to increased disability in this population.
It is crucial to understand disability in older adults because it is associated with significant personal, societal, and economic cost [23, 24]. Older adults with disability report poorer quality of life, subsequent poor self-rated health and higher mortality over two years compared to those without disability [25, 26]. The Department of Health and Human Services estimates that providing care and needed services for an older adult turning 65 within 2015–2019 will cost about $138,000 in the future in part due to higher likelihood of needing to be in an institutional setting [27].
The immigration process may affect disability and its correlates in older adult immigrants. Immigration impacts health outcomes through factors such as acculturation and migration selectivity [28]. Acculturation is a process of cultural and psychological change after migrating to the U.S.[29–31]. Acculturation is associated with negative health outcomes including disability [30, 32] and positive health outcomes in immigrants [33]. Additionally, older adult immigrants are described as “aging out of place”; a concept of aging without previous community ties that is associated with negative health outcomes [34].Thus, the immigration process may pose unique health challenges for older adult immigrants.
Older immigrants have worse socioeconomic characteristics, but correlates of disability in immigrants as a whole have not been synthesized. Older adult immigrants typically are classified as low-income and continue to be employed later in older age [17]. Some studies have identified correlates of disability in specific racial/ethnic immigrant groups. Synthesizing the prevalence and correlates of disability in older adult immigrants is an important step in understanding functional health outcomes of this growing population which is the purpose of this review.
Methods
Terminology
In the literature on older adult populations, disability has many related terminologies including functional limitations, functional impairments, functional difficulties, physical disability, physical difficulties, physical limitations, physical function difficulties, and physical function limitations. However, disability is often measured by difficulties in performing basic and instrumental activities of daily living [10, 11, 32, 35, 36]. In this review, we defined disability as difficulty in performing basic or instrumental activities of daily living (ADLs/IADLs). Basic Activities of Daily Living (ADLs) are bathing, dressing, transferring, toileting, continence and feeding [37]. Instrumental Activities of Daily Living (IADLs) are the ability to use the telephone, shopping, food preparation, housekeeping, laundry, mode of transportation, responsibility for own medications and ability to manage finances [38].
While some of these basic and instrumental activities of daily living involve cognitive ability, this review does not focus on cognitive function and/or cognitive disability. Defining disability as limitations in ADLs and IADLs facilitated the literature search, and enabled comparison of similar sub-concepts across different studies. We used the U.S. Census Bureau’s definition of an older adult as a person who is over 65 years [22] and defined an immigrant as a person who was not born in the U.S. but currently lives in the country [39].
Search Strategy
Database search for this review was updated in February 2018 and no new articles were identified. The search was conducted in June 2017 and included 4 electronic databases (PubMed, Embase, CINAHL, and Scopus). Following consultation with a health science librarian, PubMed, Embase, Cumulative Index to Nursing and Allied Health Literature (CINAHL) and Scopus were searched using MESH and Boolean search techniques. Search terms included: “Emigrants and Immigrants” or “Emigration and Immigration” or the truncated word “Immigrant*” or “Alien” and “activities of daily living” or “activity of daily living” or “physical functioning” and “age” or truncations of the words “elder* or senior* or older* or geriatric*”. The reference lists of all articles read were also searched for relevant articles.
Selection of Studies
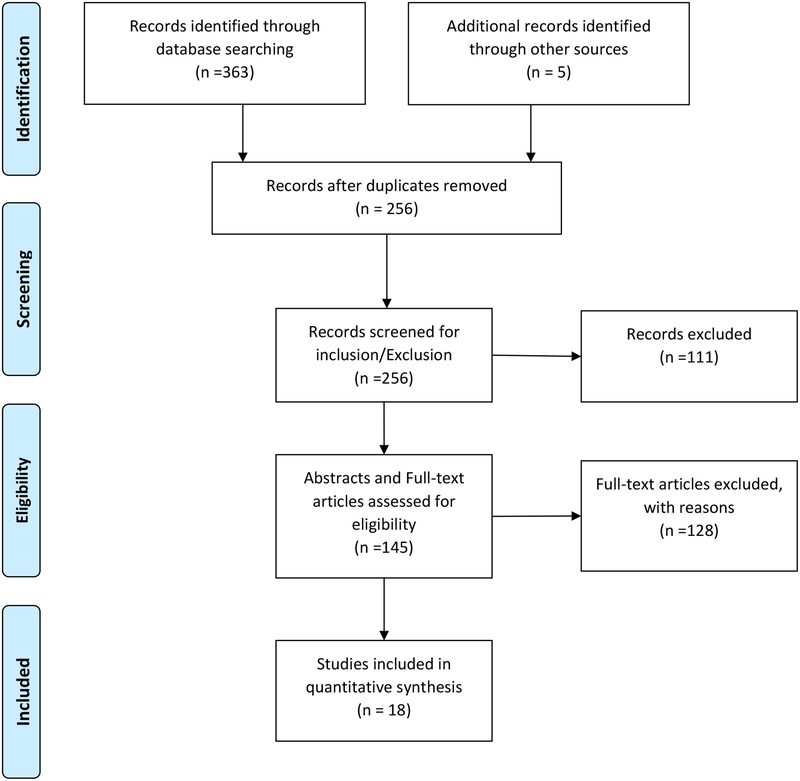
Three hundred and sixty-eight articles were retrieved from the electronic search. After removing duplicates and screening titles for the inclusion criteria, 256 studies remained. Abstracts of the remaining articles were reviewed for the following inclusion criteria: Studies published in English, studies conducted in the U.S. in the last ten years, studies that included older immigrants in the sample (≥65years) and included ADL/IADLs as study variables. One hundred and forty-five abstracts were identified for full text screening. Final articles included in the review reported the prevalence of ADL and IADL difficulties and/or factors associated with them. See Figure 1 for details of this selection process. Two independent reviewers completed each stage of screening. Disagreements were resolved through consensus by the two reviewers. All the studies included here were published articles; this review did not require an institutional ethics review.
Figure I.
PRISMA diagram showing the systematic process of identifying relevant articles for Review of prevalence and correlates of disability in Older Immigrants
Results
Overview of Included Studies
Eighteen articles met the final inclusion criteria. Five articles reported both the prevalence and factors associated with disability, while eight articles reported prevalence only and five reported factors only. Of the 18 articles, 14 explored prevalence of and factors associated with disability by specific country of origin/ethnicity, and four studies included multiple groups and countries in the samples. There were seven articles involving Hispanic/Latinos and six with Asians. Sample sizes ranged from 47 [40], in a study on Filipino immigrants to 48,419,324 in a study with Hispanic/Latinos [10]. Three articles had sample sizes less than 1000 study participants [40–42]. All but one study was a cross sectional design. The one study with a different design was a longitudinal analyses of cross-sectional survey data [43].
Characteristics of the studies reviewed varied significantly. Ten studies reviewed had entirely older adult samples, while eight included adults younger than 65 years. Most of the studies included U.S. born adults and older adults (n=12). Several epidemiologic datasets were utilized in these studies including the Hispanic Established Populations for Epidemiologic Studies for the Elderly (Hispanic EPESE), the California Health Interview Survey (CHIS), American Community Survey (ACS), the National Health Interview Survey (NHIS), and the Public Use Microdata Sample (PUMS). Two studies did not offer a complete assessment of all activities of daily living [42, 44], and seven articles did not assess any instrumental activities of daily living[10, 11, 28, 32, 42, 44, 45].
Prevalence of Disability
Prevalence of disability varied across the immigrant groups reviewed. The prevalence of disability in a sample of U.S. immigrants from multiple countries was 19.3% [30]. These results are presented in chronological order in Table 1.
Table I:
Prevalence of Disability Rates in Older Immigrants
| Citation | Immigrant Group(s) | Data set used | Sample | Disability Measure: Name (Scale utilized) | % >65 years or Mean age | Major Results (Specific population(s): Rate (Disability Type) |
|---|---|---|---|---|---|---|
| (Al Snih et al., 2006) | Mexicans | 1993–1994 Hispanic EPESE | 2675 | Functional Disability (Difficulty on ADLs & IADLs) | 100% | ADLs: 13.4% IADLs: 58.1% |
| (Mejía et al., 2006) | Hispanics | 1993–1994 Hispanic EPESE | 2819 | Functional impairments (Dependency on IADLs) | 100% | Hispanics: 51.7% |
| (Wong et al., 2006) | Mexicans | 1998–1999 Hispanic EPESE | 898 | Functionality (Difficulty with at least one ADL or IADL) | 100% | Mexicans: 21.7% (ADLs) Mexicans: 32.5% (IADLs) |
| (Sorkin et al., 2008) | Vietnamese | California Health Interview Surveys | 359 | ADL Limitations (Equipment/help with ADLs) | 43.4% | Vietnamese: 7.7% (ADLs) |
| (Mendes de Leon, Carlos F et al., 2011) | Hispanics | 2008 American Community Survey (ACS) | 48,419,324 | Disability (Difficulty with self-care (dressing or bathing) & Difficulty with Independent living (visiting doctor’s office or shopping) | 34.4% | Hispanic men: 6.7% (ADLs) Hispanic women: 11% (ADLs) Hispanic men: 11.3% (IADLs Hispanic women: 19.8% (IADLs) Mexican men: 6.7% (ADLs) Mexican women: 8.4% (ADLs) Mexican men: 8.3% (IADLs) Mexican Women: 15.8 % (IADLs) |
| (Melvin et al., 2014) | All Immigrants | 1998–2011 National Health Interview Survey (NHIS) Data | 319,893 | ADL and IADL disability (Requiring assistance with ADL or IADLs) | 100% | Mexican women: 8–57% Puerto Rican women: 6–45% Cuban women: 3–31% Other Hispanic women: 3–52% Asian women: 2–45% Black women: 4–22% White women: 5–38% Mexican Men: 3–47% Puerto Rican Men: 5–39% Cuban Men: 2–37% Other Hispanic Men: 3–35% Asian Men: 2–43% Black Men: 4–26% White Men: 3–25% |
| (Mehta & Elo, 2012) | Russia | 2000 Public Use Microdata Sample 2000–2007 NHIS | PUMS: 9312 NHIS: 219 | Activities of daily living Limitations (ADL and IADL difficulties) | PUMS- 63.3 NHIS- 65 | Russian: 13.2% (ADLs) Russian: 9.7% (IADLs) |
| (Yang et al., 2012) | Southeast Asians | 2003–2007 ACS | 9351 | ADL and IADL limitations | 64.9% | All: 9.4% (ADLs) Hmong: 21.0% (ADLs) Vietnamese: 7.8% (ADLs) Cambodian: 15.8% (ADLs) Laotians: 11.9% (ADLs) All: 17.5% IADLs) Hmong: 29.7% IADLs Vietnamese: 15.4% IADLs) Cambodian: 27.4(IADLs) Laotians: 21.1 %(IADLs) |
| (Ro & Gee 2012) | Asians | 2000 Public Use Microdata Sample (PUMS) | 294,967 | Disability (Difficulty with Self- care (dressing or bathing) Mobility Disability (difficulty going outside the home alone to shop or visit the doctor’s office) | 41.1–46.4 | Filipinos: 3.34% (ADLs) Chinese: 3.18% (ADLs) Vietnamese: 6.39 % (ADLs) Cambodians: 9.03% (ADLs) Hmong: 11.34% (ADLs) Laotians: 7.77% (ADLs) Filipinos: 15.41%(IADLs) Chinese: 11.26% (IADLs) Vietnamese: 19.61% (IADLs) Cambodians: 22.93%(IADLs) Hmong: 22.48% (IADLs) Laotians:19.6% (IADLs) |
| (Ceria-Ulep et al., 2013) | Filipino | 47 | Physical Function (ADL difficulties & IADL difficulties) | 100% | Filipinos: 34% (ADLs) Filipinos: 49% (IADLs) |
|
| (De Souza & Fuller-Thomson, 2013) | Filipino | 2006 ACS | 5192 | Function limitations (ADL limitations) | 48% | Filipinos: 6.3% (ADLs) |
| (Gubernskaya et al., 2013) | All | 2000–2010 ACS 1998–2010 Integrated Health Interview Survey | ACS- 336,948 IHIS - 44,978 | Disability (limitations with ADLs and IADLs) | ACS- 63 IHIS- 63.8 | All: 19.3% (ADLs& IADLs) |
| (Tran et al., 2014) | Vietnamese | 2000 Integrated Public Use Microdata Sample (IPUMS) | 2610 | Functional disability (Limitations in ADLs) | 100% | Vietnamese: 16% (ADLs) |
Asians:
Six studies involving Asian immigrants also presented country/ethnicity-specific disability prevalence [11, 29, 32, 40, 42, 44]. Disability prevalence ranged from 2%−45% in Asian female older adults and 2%−43% in Asian male older adult immigrants. For Southeast Asian immigrants, the rate of disability was 17.5% from a nationally representative study (American Community Survey) [44]. However, this dataset included participants who were younger than 65 years (disaggregated data for individuals 65+ were not available) which would likely lead to an underestimation of the prevalence of disability in Southeast Asian older adults.
Prevalence for specific groups of Asian ethnicities was reported for Vietnamese, Filipinos Cambodians, Hmong and Laotians. Prevalence of disability in Vietnamese older adults ranged from 6.39% to 19.61% [29, 32, 40, 42, 44]. Three of these studies were nationally representative large samples. Three studies reported disability prevalence in Filipino immigrants of any age. It ranged from 3.34% to 49% [29, 32, 40]. Two of these studies were from large national datasets [29, 32]. Two of the studies reported the prevalence of disability in Cambodians, Hmong, and Laotian immigrants, ranging from 7.7%–27.4% [32, 44]. Amongst these, Cambodians had the highest prevalence of disability at 27.4%. However, two studies included younger immigrants, and one included both U.S. born and immigrant older adults [42]. Also, these studies included younger populations; a mean age of 46.4 was reported in one study [32], and older adults were only 48% of the other sample [29]. These limitations prevent accurate determination of the prevalence of disability in Asian older adult immigrants.
Hispanic/Latinos:
The prevalence of disability reported from a diverse group of Hispanic/Latinos was 51.7% [46]. This prevalence was obtained from the 1993–1994 Hispanic/Latino EPESE dataset which may not represent the current burden of disability in this population. From analyses of the nationally-representative American Community Survey in 2011, the prevalence of disability in Hispanic/Latinos was lower. The prevalence of disability in that study was 6.7% and 11% for ADLs difficulty for men, and women, and 11.3% and 19.8% for IADL difficulties in men and women respectively [10]. However, in this sample only 34.4% of adults were over 65 years, which could lead to underestimation of the disability in Hispanic/Latino older adults.
Amongst the Hispanic/Latino ethnic groups, prevalence of disability in Mexicans were reported in studies. Prevalence of ADL and IADL difficulties ranged from 6.7% to 58.1% (58.1% was obtained from analyses of the Hispanic/Latino EPESE which is over 20 years) [10, 41, 46, 47]. These results were from nationally representative large samples; the 1993–1994 &1998–1999 Hispanic/Latino EPESE surveys, 1998–2011 National Health Interview surveys and the 2008 American Community survey. In Mexicans, disability prevalence was about 2%−10% higher in women than in Mexican men [10, 46].
Differences in the Prevalence of Disability
From an old dataset, Hispanic/Latinos had the highest burden of disability compared to all the groups reviewed. The highest prevalence of disability (49%) in Asians was also seen in a small sample of Filipino older adults [40]. However, comparing reports from the same dataset, the American Community Survey (ACS), disability was higher in Asians than Hispanic/Latinos. From the 2008 ACS data set, the disability prevalence among Hispanic/Latino immigrants were: 6.7% and 11% for ADLs for men and women, and 11.3% and 19.8 % for IADLs for men and women [10]. Using the 2003–2007 ACS cohorts, the prevalence of disability was higher in Asians. Disability in Southeast Asian immigrants was 17.5%, but even higher rates were observed for some of the countries/ethnicities studied [44]. These were: 29.7% for Hmong, 27.4 % for Cambodians, and 21.1% for Laotians [44]. The ACS study with Asians combined ADLs and IADLs to give a joint proportion and also combined the 2003–2007 ACS cohorts to obtain large samples for the subgroup analyses, which could have led to an overestimation of disability in Asians.
We discuss the differences across immigrants groups here but many of the articles reviewed compared the differences between the immigrant groups examined and U.S Born whites older adults [42, 44–46, 48, 49], back in home country[10], did not do a comparison or a comparison was not tested statistically[30, 32]. In these studies, foreign-born older adults had higher disability burden than U.S. born older adults [31, 44, 49], except in one study which Hispanic/Latino immigrants had lower disability rates than U.S. born Blacks [10]. Therefore, the differences within immigrant groups discussed here should be interpreted with caution.
Factors Associated with Disability
Ten studies reviewed reported factors associated with disability in immigrants. Findings from the individual studies reviewed are listed in Table 2. Nine factors were associated with higher prevalence of disability and 5 factors were associated with lower disability. For factors associated with higher disability, three medical conditions (obesity, diabetes, and arthritis) and sociodemographic factors (older age, limited education, low income, female, and being single (unmarried) were identified. Four studies reported older age as a factor associated with higher disability [11, 29, 31, 45]. Limited education was associated with increased disability in three studies [11, 28, 29], and low income was reported in one study [10]. Migrating at an older age and being female were reported in two studies each [30, 45, 50, 51]. Additionally, being single was associated with disability in one study [29]. Obesity, diabetes, and arthritis were medical conditions associated with disability in older immigrants [47, 50]. These factors are from studies with large sample sizes ranging from 2019 to 33,6948 participants. Although some of these samples included adults younger than 65 years [10, 16, 29], these results were from studies that controlled for potential confounders, increasing the validity of the reported associations.
Table II:
Correlates of Disability Rates in Older Immigrants
| Citation | Immigrant Group(s) | Data set used | Sample | Disability Measure: Name (Scale used) | Major results | Factors (effect on Disability) |
|---|---|---|---|---|---|---|
| (Al Snih et al., 2006) | Mexicans | 1993 – 1994 Hispanic EPESE | 2675 | Functional Disability (Difficulty on ADLs & IADLs) |
|
|
| (Wakabayashi, 2010) | Mexicans | 1996–2006 Health & Retirement studies | 14,792 (includes Whites, Black and Mexicans) | ADL limitations (Difficulty/unable to perform ADLS) |
|
|
| (Lum & Vanderaa, 2010) | Hispanic/Latino, African, White Immigrants | Asset and Health Dynamic of the Oldest old (AHEAD) study | 7345 | ADL& IADL Difficulties (ADL difficulty 1–6 IADL difficulty 1–5) |
|
|
| (Mendes de Leon, Carlos F et al., 2011) | Hispanic/Latinos | American Community survey (ACS) 2008 | 48,419,324 | Disability (Difficulty with self-care (ADLs) Difficulty with Independent living (IADLs) |
|
|
| (Gubernskaya et al., 2013) | All immigrants | 2000–2010 ACS data 1998–2010 Integrated Health Interview Series (IHIS) | ACS- 336,948 IHIS - 44,978 | Disability (limitations with ADLs and IADLs) |
|
|
| (Son, 2013) | All immigrants | 2004 National health Interview survey (NHIS) | 13732 | Functional difficulties (difficulty with IADLS) |
|
|
| 1st Author, pub year | Immigrant Group(s) | Data set used | Sample | Disability Measure: Name (Scale used) | Major results (Variable in review) | Factors (effect on disability) |
| (De Souza & Fuller-Thomson, 2013) | Filipino | 2006 ACS | 5192 | Function limitations (ADL limitations Y/N) |
|
|
| (Tran et al., 2014) | Vietnamese | 2000 Integrated Public Use Microdata Series IPUMS | 2610 | Functional disability (DIFFCARE- ADL limitations Y/N) |
|
|
| (Howrey et al., 2015) | Mexicans | 1993 – 2013 Hispanic EPESE | 2584, with subset of 2230 (no baseline ADL limitations) | Disability (Modified Katz ADL scale- 0-no help needed ,1-help needed) |
|
|
| (Garcia & Reyes, 2017) | Mexicans | (H-EPESE) 1993–94 1995–96, 1998–99, 2000–2001, 2004–2005, 2007, and 2010–2011 | 1,483 men 2,051 women | Disability (Independence in ADLs) |
|
|
Five factors were associated with decreased disability in immigrants (acculturation, migrating at a younger age, exercise, alcohol intake, and church attendance). Acculturation was protective of disability in one study [11], and younger age, alcohol intake, exercise and church attendance were reported as protective factors of disability in one study each as well [30, 45, 50].
Differences in Factors Associated with Disability
Factors associated with disability differed by immigrant group. Older age, female gender, low income, migration at an older age, limited education, and three medical conditions were associated with increased disability in studies of Hispanic/Latinos, Asian and two diverse immigrant samples. Being single was reported in studies of Filipinos immigrants only [29]. Chronic conditions associated with disability were reported in studies with Mexican immigrants only [47, 50]. Migration at an older age was associated with greater disability in two studies (one with a diverse sample and one with Mexican immigrants) [30, 51]. The opposite, migrating at a younger age was protective of disability in the same study of diverse immigrants [30]. Of the protective factors identified; exercise has been documented to be related to improved health outcomes in older adults [52, 53]. The other four were reported in one study each, limiting any further comparisons. Alcohol was reported to be associated with lower prevalence of disability in one study [45].
Study designs and findings were complex as some studies compared foreign born to U.S. born of the same ethnicity whereas others compared foreign born to U.S. born Whites only. And still others compared foreign born to those in their home countries. In a study that compared factors by birth place (i.e. U.S. born vs foreign born), differences by birth place were not statistically significant [29]. Another reported that Mexican immigrants had lower levels of education compared to their U.S. born White counterparts [28]. A third study included birth place as a covariate in the analyses but did not report on the differences in factors associated with disability by this variable [50]. Finally, one study reported that arthritis was a risk factor for disability in Mexican immigrants to the U.S. and in Mexico [47].
Discussion
This systematic review was conducted to synthesize the current evidence on the prevalence and factors associated with disability in older immigrants in the U.S. The majority of the studies were in Hispanic/Latino and Asian older adult immigrants. The prevalence of disability in a sample of U.S. immigrants from multiple countries was 19.3% [30]. Hispanic/Latinos (Mexicans) had the highest prevalent of disability at 58.1% [46], but this result was obtained from a 20-year old dataset and it may not reflect the current burden of disability in this population. This prevalence was lower than that of U.S. born older adults at 60% [3]. Immigration related factors associated with disability in this review included migration at older age, migration at a younger age and acculturation [11, 30, 51]. Medical factors associated with disability in these immigrant groups were similar to those for U.S. born older adults. A review of risk factors for disability in native born older adults includes obesity, arthritis, and diabetes [54]. Old age is consistently associated with disability across populations due to age-related loses in ability, medical conditions, and the social and physical environmental challenges [1].
We found that although immigration may be a risk factor for disability, the risk factors for disability in immigrant populations were the same as those universally found (female gender, limited education and low income)[4, 6–9]. Older adult immigrants are more likely to be female, have limited education and low income [17, 55]. These sociodemographic correlates of disability (female gender, single status, limited education and low income) were reported in Hispanic/Latino and Asian immigrants who make up the highest and second highest groups of immigrants in the U.S.[10, 11, 28, 29, 50]. However, migration selectivity, acculturation and other unique sociocultural factors may interact with medical and sociodemographic factors to impact disability in older adult immigrants. For example, due to economic hardship and preference for aging in place, older adult immigrants are more likely to live with family members, compared to their U.S. born counterparts [56, 57]. This likely provides social connections and caregiving resources for older immigrant that impact disability and further functional decline.
Acculturation was identified as a protective factor of disability in one study in this review, which is different from what is typically noted in other acculturation studies. In this study, acculturation was measured with language proficiency and naturalization status [11]. High English language proficiency has been associated with better self-rated health in immigrants [58]. Also, English language proficiency is linked to the ability to access healthcare and other social services [17]. However, the majority of older immigrants in the U.S have limited English proficiency, and improving English language proficiency may offer an avenue for interventions towards the goal of improving disability and health in older adult immigrants.
In the context of the Heathy Immigrant Effect, differences in the prevalence of disability between U.S. born and immigrant older adults are more nuanced. This hypothesis suggest that immigrants are healthier than their U.S. born counterparts [51, 59]. The Healthy Immigrant Effect is often explained by healthy self-selection at migration, extensive screening of immigrants before and upon arrival into the U.S., and heathier lifestyles in their home countries [51]. Broadly, this review shows that immigrants had a lower prevalence of disability compared to U.S. born older adults. However, Yang et.al reported that Asian immigrants had higher prevalence of disability than in U.S born Whites [44]. Dallo and colleagues reported that Asian immigrants had higher prevalence of disability than U.S born Asians but not Whites, Blacks or Hispanic/Latinos [60]. Additionally, Melvin and colleagues [46], reported similar proportions of disability across Asian immigrants and all U.S. born older adults. This suggest that older immigrants may not have a complete health advantage over their U.S. born counterparts as it is suggested by the Healthy Immigrant Effect hypothesis.
Another concept related to the Healthy Immigrant Effect, the “Salmon Bias” was not supported in this review. This concept which suggests that immigrants will return to their home countries once their health begins to fail is used to explain why the remaining immigrant population is healthier [61, 62]. Mexican immigrants had a higher prevalence of disability, when compared to their counterparts in Mexico [63]. Current research suggests that with increasing age, the prevalence of disability in foreign-born older adults also increases [46]. Therefore, more research is needed to determine accurate rates of disability and examine how migratory patterns are related to disability in immigrant older adults.
Knowledge gained from this study can contribute to the tailoring of interventions to improve the health of older adult immigrants. Identification of factors associated with disability in immigrants is vital to inform these interventions. Many older immigrants immigrate with health problems or may develop them soon after migration [31, 32]. Identifying migration at an older age as a factor associated with increasing disability highlights an important consideration for disability interventions in older immigrants. This suggests that early intervention for older adults who migrate in later adulthood might decrease disability and improve quality of life later in older age. Also, older immigrants may have low income and limited education [29, 49, 55], which should be considered when developing interventions to improve disability in older immigrants.
This review has some limitations. The results do not include all immigrant groups and many of the datasets analyzed are relatively old. Most studies were on Asian and Hispanic/Latinos older immigrants, and only one study included European immigrants. There were no studies on the prevalence of disability among older African and Afro Caribbean immigrants, some of the fastest growing groups of U.S. immigrants [64]. Many of datasets analyzed for the prevalence results are old. For example, the study with the highest prevalence was from the 1993–1994 Hispanic EPESE study. Although the years are not reported for some studies, the most recent data was collected in 2011, which is 7 years old [28, 46]. The concept of disability is described and measured differently by different researchers. While the search terms incorporated the most frequently used terminology for the study concepts, it is possible that some articles may have been missed in this review if they contain other terminology for basic and instrumental activities of daily living.
There are some limitations of the studies included in this review. Several studies had small sample sizes [40, 42] or included limited number of older adults[10, 29, 30, 32, 42, 44]. Research shows that minority elders have negative attitudes and distrust of the medical and research community [65]. While some studies translated its instruments to the immigrant language, this alone might not be enough to overcome this barrier and results presented may not reflect that entire immigrant group. Also, culture and gender norms influence ADLs and IADLs. In certain cultures, activities of daily living are divided by gender (e.g. women are engaged activities such as meal preparation, and laundry, while men manage the money). Research has shown that when gender roles are accounted for, the prevalence of limitations in activities of daily living decreases [66]. The measurement of disability without consideration and adjustments for gender and cultural norms might lead to an over or underestimation of disability rates.
Despite these limitations, this literature review has several strengths and implications. The understanding of disability among older immigrants from multiple ethnic groups and countries can help identify areas for program development in this population. Many Asians and some Europeans immigrants migrated to the U.S. as refugees following political turmoil in their countries [44, 49]. For some Hispanic/Latinos, political issues in Cuba led to migration, while some Mexicans migrated as laborers during the Bracero period [10]. These histories create conditions for differing health trajectories and make comparisons across immigrant groups somewhat challenging. However, this review adds to the state of the science about disability and the health of older immigrants in the U.S. It also highlights areas for future research in this population: Future research in disability in immigrants should: 1) examine the trajectory of disability in all immigrant groups including African, European, and Afro Caribbean immigrants; 2) validate measures of disability in immigrant populations; and 3) examine other forms of disability including cognitive disability in older immigrants.
Future research on disability in immigrants should also examine how the immigration process influences disability and other health outcomes in immigrants. Some of this work has begun with the PINE (The Population Study of Chinese Elderly in Chicago) study [67] in Chinese older adults and the Hispanic/Latino EPESE in Hispanic/Latino older adults. Also, some nationally representative cohort and cross-sectional surveys like the NHIS have updated its sampling approach to account for these aspects of immigrant health [68]. Despite these, more comprehensive studies of disability are needed to inform interventions for older immigrants.
Activities of daily living limitations in older adults can be treated with behavioral interventions [69]. Interventions such as the Community Aging in Place Advancing Better Living for Elders (CAPABLE) [70] have been shown to decrease disability in U.S. born older adults. Although some immigrants have benefited from CAPABLE and other interventions, these interventions may benefit from adaptation to work with the culturally diverse older adult immigrants in the United States. Research that is tailored to older adult immigrants’ experiences, goals, and cultural contexts will allow them to thrive in the United States.
Acknowledgments
This publication was made possible by the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by Grant Number TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Ruth-Alma Turkson-Ocran was supported by training grants under the National Institute of Nursing Research (NINR) and National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) of the National Institutes of Health under award numbers T32NR012704 and 3T32DK062707 respectively.
Funding: N/A
Footnotes
Conflict of Interest:
Manka Nkimbeng, Joycelyn Cudjoe, Ruth-Alma Turkson-Ocran, Yvonne Commodore-Mensah, Roland J. Thorpe Jr, and Sarah L. Szanton declare that they have no conflict of interest.
Compliance with Ethical Standards: N/A
Ethical Approval: This article does not contain any studies with human participants performed by any of the authors.
References
- 1.World Health Organization. Summary: World Report on Ageing and Health 2015. [Google Scholar]
- 2.Disability and Health Fact sheet. Available at: http://www.who.int/mediacentre/factsheets/fs352/en/. Accessed 01/17, 2017.
- 3.Disability and Functioning (Noninstitutionalized Adults 18 Years and Over). Available at: http://www.cdc.gov/nchs/fastats/disability.htm.
- 4.Millan-Calenti JC, Tubio J, Pita-Fernandez S, et al. Prevalence of Functional Disability in Activities of Daily Living (ADL), Instrumental Activities of Daily Living (IADL) and Associated Factors, as Predictors of Morbidity and Mortality. Arch Gerontol Geriatr 2010; 50:306–10 doi: 10.1016/j.archger.2009.04.017 [doi]. [DOI] [PubMed] [Google Scholar]
- 5.Taş Ü, Verhagen AP, Bierma-Zeinstra SMA, et al. Incidence and Risk Factors of Disability in the Elderly: The Rotterdam Study. Prev Med 2007; 44:272–8 [DOI] [PubMed] [Google Scholar]
- 6.Martin LG, Schoeni RF. Trends in Disability and Related Chronic Conditions among the Forty-And-Over Population: 1997–2010. Disability and Health Journal 2014; 7: S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cigolle CT, Langa KM, Kabeto MU, et al. Geriatric Conditions and Disability: The Health and Retirement Study. Ann Intern Med 2007; 147:156–64. [DOI] [PubMed] [Google Scholar]
- 8.Ervin RB. Prevalence of Functional Limitations among Adults 60 Years of Age and Over: United States, 1999–2002. Adv Data 2006:1–7. [PubMed] [Google Scholar]
- 9.Holmes J, Powell-Griner E, Lethbridge-Cejku M, et al. Aging Differently: Physical Limitations among Adults Aged 50 Years and Over: United States, 2001–2007. NCHS data brief 2009;20. [PubMed] [Google Scholar]
- 10.Mendes de Leon Carlos F., Eschbach K Markides KS. Population Trends and Late-Life Disability in Hispanics from the Midwest. J Aging Health 2011; 23:1166–88 doi: 10.1177/0898264311422100. [DOI] [PubMed] [Google Scholar]
- 11.Tran TV, Nguyen T, Chan KT. Acculturation and Functional Disability among Older Vietnamese-Americans. Journal of Ethnic & Cultural Diversity in Social Work: Innovation in Theory, Research & Practice 2014;23:20–35 doi: 10.1080/15313204.2013.871996. [DOI] [Google Scholar]
- 12.Reichard A, Stolzle H, Fox MH. Health Disparities Among Adults with Physical Disabilities or Cognitive Limitations Compared to Individuals with No Disabilities in the United States. Disability and Health Journal 2011; 4:59–67 [DOI] [PubMed] [Google Scholar]
- 13.Freedman VA, Schoeni RF, Martin LG, et al. Chronic Conditions and the Decline in Late-Life Disability. Demography 2007; 44:459–77 doi: 10.1353/dem.2007.0026. [DOI] [PubMed] [Google Scholar]
- 14.Egede LE. Major Depression in Individuals with Chronic Medical Disorders: Prevalence, Correlates and Association with Health Resource Utilization, Lost Productivity and Functional Disability. Gen Hosp Psychiatry 2007; 29: 409–16 [DOI] [PubMed] [Google Scholar]
- 15.Immigrants in the United States. Available at: https://www.americanimmigrationcouncil.org/research/immigrants-in-the-united-states. Accessed 12/08, 2017.
- 16.Population Reference Bureau. Elderly Immigrants in the United States. Today’s Research on Aging 2013. [Google Scholar]
- 17.Scommegna P Elderly Immigrants in the United States. Immigration and America’s Cities: A Handbook on Evolving Services 2016:33. [Google Scholar]
- 18.Older Immigrants in the United States. Available at: http://www.migrationpolicy.org/article/older-immigrants-united-states. Accessed 06/30, 2016.
- 19.Baugh R, Witsman K. U.S. Lawful Permanent Residents: 2015. DHS Office of Immigration Statistics 2017. [Google Scholar]
- 20.Vincent GK, Velkoff VA. The Next Four Decades: The Older Population in The United States: 2010 To 2050: US Department of Commerce, Economics and Statistics Administration, US Census Bureau 2010. [Google Scholar]
- 21.Mather M Fact Sheet: Aging in the United States 2016. [Google Scholar]
- 22.Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in The United States. Washington, DC: US Census Bureau; 2014:25–1140. [Google Scholar]
- 23.Congressional Budget Office Projections of Expenditures for Long-Term Care Services for The Elderly 1999. [Google Scholar]
- 24.Willink A, Davis K, Schoen C, et al. Physical and/or Cognitive Impairment, Out-of-Pocket Spending, and Medicaid Entry among Older Adults. Journal of Urban Health 2016; 93:840–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koroukian SM, Schiltz N, Warner DF, et al. Combinations of Chronic Conditions, Functional Limitations, and Geriatric Syndromes that Predict Health Outcomes. Journal of general internal medicine 2016; 31: 630–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bentley JP, Brown CJ, McGwin G Jr, et al. Functional Status, Life-Space Mobility, and Quality of Life: A Longitudinal Mediation Analysis. Quality of Life Research 2013; 22:1621–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Department of Health and Human Services. Long-Term Services and Supports for Older Americans: Risks and Financing Research Brief 2016. [Google Scholar]
- 28.Garcia MA, Reyes AM. Physical Functioning and Disability Trajectories by Age of Migration Among Mexican Elders in the United States. J Gerontol B Psychol Sci Soc Sci 2017. doi: gbw167 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Souza L, Fuller-Thomson E. Acculturation and Disability Rates Among Filipino-Americans. J IMMIGRANT MINORITY HEALTH 2013; 15:471 10p doi: 10.1007/s10903-012-9708-1. [DOI] [PubMed] [Google Scholar]
- 30.Gubernskaya Z, Bean FD, Van Hook J. (Un)Healthy Immigrant Citizens: Naturalization and Activity Limitations in Older Age. J Health Soc Behav 2013; 54:427–43 doi: 10.1177/0022146513504760 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lum TY, Vanderaa JP. Health Disparities Among Immigrant and Non-Immigrant Elders: The Association of Acculturation and Education. Journal of immigrant and minority health 2010; 12:743–53. [DOI] [PubMed] [Google Scholar]
- 32.Ro A, Gee GC. Disability Status Differentials Among Asian Immigrants in The United States: The Added Dimensions of Duration and Age. Race and Social Problems 2012; 4:83–92 doi: 10.1007/s12552-012-9069-3. [DOI] [Google Scholar]
- 33.Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino Health in the United States: A Review of the Literature and its Sociopolitical Context. Annu.Rev. Public Health 2005;26:367–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sadarangani TR, Jun J. Newly Arrived Elderly Immigrants: A Concept Analysis of “Aging Out of Place”. J Transcult Nurs 2015; 26:117 8p doi: 10.1177/1043659614549074. [DOI] [PubMed] [Google Scholar]
- 35.Szanton SL, Thorpe RJ, Boyd C, et al. Community Aging in Place, Advancing Better Living for Elders: A Bio‐Behavioral‐Environmental Intervention to Improve Function and Health‐Related Quality of Life in Disabled Older Adults. J Am Geriatr Soc 2011; 59:2314–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim BJ, Choi Y. The Relationship Between Activities of Daily Living (ADL), Chronic Diseases, and Depression Among Older Korean Immigrants. EDUC GERONTOL 2015; 41:417–27 doi: 10.1080/03601277.2014.982006. [DOI] [Google Scholar]
- 37.KATZ S, FORD AB, MOSKOWITZ RW, et al. Studies of Illness in The Aged. The Index Of ADL: A Standardized Measure of Biological and Psychosocial Function. JAMA 1963; 185:914–9. [DOI] [PubMed] [Google Scholar]
- 38.Lawton MP, Brody EM. Assessment of Older People: Self-Maintaining and Instrumental Activities Of Daily Living. Gerontologist 1969; 9:179–86. [PubMed] [Google Scholar]
- 39.Immigrant. Available at: http://www.merriam-webster.com/dictionary/immigrant. Accessed May 13, 2016.
- 40.Ceria-Ulep CD, Dalusung-Angosta A, Magday-Asselstine RT, et al. Assessing Physical Activity and Function in the Filipino Older Adults. J Cult Divers 2013; 20:30–9. [PubMed] [Google Scholar]
- 41.Wong R, Díaz JJ, Higgins M. Health Care Use Among Elderly Mexicans in the United States and Mexico: The Role of Health Insurance. Res Aging 2006; 28:408 16p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sorkin D, Tan AL, Hays RD, et al. Self-Reported Health Status of Vietnamese And Non-Hispanic White Older Adults in California. J Am Geriatr Soc 2008; 56:1543–8 doi: 10.1111/j.1532-5415.2008.01805.x [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Howrey BT, Al Snih S, Jana KK, et al. Stability and Change in Activities of Daily Living Among Older Mexican Americans. J Gerontol A Biol Sci Med Sci 2015. doi: glv172 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yang MS, Burr JA, Mutchler JE. The Prevalence of Sensory Deficits, Functional Limitations, and Disability Among Older Southeast Asians in the United States. J Aging Health 2012; 24:1252–74 doi:0898264312457413 [pii]. [DOI] [PubMed] [Google Scholar]
- 45.Son J Are Immigrants from Asia Healthier than Immigrants from other Regions? Self-reported Health Status and Functional Difficulties of Immigrants in the USA. Journal of International Migration and Integration 2013; 14:19–38 [Google Scholar]
- 46.Melvin J, Hummer R, Elo I, et al. Age Patterns of Racial/Ethnic/Nativity Differences in Disability and Physical Functioning in the United States. Demogr Res 2014; 31:497–510 doi: 10.4054/DemRes.2014.31.17 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Al Snih S, Ray L, Markides KS. Prevalence of Self-Reported Arthritis Among Elders from Latin America and the Caribbean and among Mexican Americans from the Southwestern United States. J Aging Health 2006; 18:207–23 doi:18/2/207 [pii]. [DOI] [PubMed] [Google Scholar]
- 48.Lum TY, Vanderaa JP. Health Disparities among Immigrant and Non-Immigrant Elders: The Association of Acculturation and Education. J Immigr Minor Health 2010; 12:743–53 doi: 10.1007/s10903-008-9225-4 [doi]. [DOI] [PubMed] [Google Scholar]
- 49.Mehta NK, Elo IT. Migrant Selection and The Health of U.S. Immigrants from the Former Soviet Union. Demography 2012; 49:425–47 doi: 10.1007/s13524-012-0099-7 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Howrey BT, Al Snih S, Jana KK, et al. Stability and Change in Activities of Daily Living Among Older Mexican Americans. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 2015; 71:780–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wakabayashi C Effects of Immigration and Age on Health of Older People in the United States. Journal of Applied Gerontology 2010; 29:697–719. [Google Scholar]
- 52.Rejeski WJ, Mihalko SL. Physical Activity and Quality of Life in Older Adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2001; 56:23–35. [DOI] [PubMed] [Google Scholar]
- 53.Beswick AD, Rees K, Dieppe P, et al. Complex Interventions to Improve Physical Function and Maintain Independent Living in Elderly People: A Systematic Review and Meta-Analysis. The Lancet 2008; 371:725–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stuck AE, Walthert JM, Nikolaus T, et al. Risk Factors for Functional Status Decline in Community-Living Elderly People: A Systematic Literature Review. Soc Sci Med 1999; 48:445–69 [DOI] [PubMed] [Google Scholar]
- 55.Batalova J Senior Immigrants in the United States 2012;2016. [Google Scholar]
- 56.Rote S, Markides K. Aging, Social Relationships, and Health Among Older Immigrants. Generations 2014; 38:51–7. [Google Scholar]
- 57.Angel JL, Angel RJ, Markides KS. Late-Life Immigration, Changes in Living Arrangements, And Headship Status among Older Mexican-Origin Individuals. Social Science Quarterly 2000:389–403. [Google Scholar]
- 58.Okafor MT, Carter-Pokras OD, Picot SJ, et al. The Relationship of Language Acculturation (English Proficiency) to Current Self-Rated Health Among African Immigrant Adults. J Immigr Minor Health 2013; 15:499–509 doi: 10.1007/s10903-012-9614-6 [doi]. [DOI] [PubMed] [Google Scholar]
- 59.Dupre ME, Gu D, Vaupel JW. Survival Differences among Native-Born and Foreign-Born Older Adults in the United States. PLoS ONE 2012; 7: e37177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dallo FJ, Booza J, Nguyen ND. Functional Limitations and Nativity Status among Older Arab, Asian, Black, Hispanic, and White Americans. J Immigr Minor Health 2015; 17:535–42 doi: 10.1007/s10903-013-9943-0 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Palloni A, Arias E. Paradox Lost: Explaining the Hispanic Adult Mortality Advantage. Demography 2004; 41:385–415. [DOI] [PubMed] [Google Scholar]
- 62.Thomson EF, Nuru-Jeter A, Richardson D, et al. The Hispanic Paradox and older adults’ disabilities: is there a healthy migrant effect? Int J Environ Res Public Health 2013; 10:1786–814 doi: 10.3390/ijerph10051786 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mejía S, Miguel A, Gutiérrez LM, et al. Comparative Analysis of Cognitive Impairment Among Mexicans and Spanish-Speaking Immigrant’s Elders. J Aging Health 2006; 18:292–314. [DOI] [PubMed] [Google Scholar]
- 64.Anderson M African Immigrant Population in U.S. Steadily Climbs. Pew Research Center 2017. [Google Scholar]
- 65.Yancey AK, Ortega AN, Kumanyika SK. Effective Recruitment and Retention of Minority Research Participants. Annu Rev Public Health 2006; 27:1–28 doi: 10.1146/annurev. publhealth.27.021405.102113 [doi]. [DOI] [PubMed] [Google Scholar]
- 66.Allen SM, Mor V, Raveis V, et al. Measurement of Need for Assistance with Daily Activities: Quantifying the Influence of Gender Roles. Journal of Gerontology 1993; 48: S211 doi: 10.1093/geronj/48.4. S204. [DOI] [PubMed] [Google Scholar]
- 67.Dong X, Wong E, Simon MA. Study Design and Implementation of the PINE Study. J Aging Health 2014; 26:1085–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention, (CDC). About the National Health Interview Survey 2017. [Google Scholar]
- 69.Gitlin L, Czaja S. Behavioral Intervention Research: Designing, Evaluating, and Implementing: Springer Publishing Company; 2015. [Google Scholar]
- 70.Szanton SL, Leff B, Wolff JL, et al. Home-Based Care Program Reduces Disability and Promotes Aging in Place. Health Affairs 2016; 35:1558–63 doi: 10.1377/hlthaff.2016.0140. [DOI] [PubMed] [Google Scholar]