Preamble
Since 2010, as research evidence is ever-increasing regarding hypertension and related diseases worldwide, guidelines for hypertension have been successively developed or revised in many countries and regions. In China, new evidence from population studies and clinical trials are accumulating, including representative sampling survey on the population with hypertension in the 12th Five-Year Plan, FEVER study subgroup, Chinese Hypertension Intervention Efficacy study (CHIEF), China Stroke Primary Prevention Trial (CSPPT). These studies have provided further information and evidence for the revision of Chinese guidelines for hypertension.
In September 2015, supported by the former Disease Control Bureau of National Health and Family Planning Commission of China, the Chinese Hypertension League, in partnership with Chinese Society of Cardiovascular Disease of the Chinese Medical Association, Hypertension Branch of the China International Exchange and Promotion Association for Medical and Healthcare, Hypertension Branch of the Chinese Geriatrics Society, and the Hypertension Committee of Chinese Medical Doctor Association organized a committee for revising the 2010 Chinese Guidelines for the Management of Hypertension. Over the past two years, discussions have been conducted for many times with respect to guiding ideas and plans of guideline revision. In the survey on major problems for revision of the guideline, 20 issues have been proposed including: goal of blood pressure (BP) control for treatment of hypertension, management of hypertension among special populations, role of β-blocker in treatment of hypertension. In response to these survey results, document retrieval has been extensively performed. Document database include China Biology Medicine (CBM), Wanfang Data Knowledge Service Platform, CNKI Platform, PubMed, Excerpta Medica Database (EMBASE), and platform of Institute of Medical Information & Library, CMAS&PUMC. After writing the first draft of the revised guideline, nearly 30 symposiums had been held by the committee for revision of guidelines, in which in-depth discussions were made regarding problems and development trends of management of hypertension. For those controversial issues, the consensuses were made with anonymous electronic voting by committee members. In early 2018, the newly revised guideline was reviewed and revised by a special group consisting 10 members of the committee, including five cardiologists, two epidemiologists, one endocrinologist, and one nephrologist. Subsequently, “the 2018 exposure draft for Chinese guidelines for the management of hypertension” was released to collect peers comments, based on which the final draft was completed.
By referring to the guideline development processes of World Health Organization (WHO) and Chinese Medical Association (CMA), assessment had been performed regarding important content, level of evidence (Table 1), and class of recommendation in this revised Guidelines (Table 2), with considerations on recent scientific developments on related fields, and current reality of hypertension management in China, the 2018 guidelines provide guidance for prevention and intervention, diagnosis and evaluation, classification and stratification and treatment and management of hypertension.
Revision Committee of 2018 Chinese Guidelines for Hypertension
Table 1. Class of recommendation.
| Definition | Recommended expression | |
| Class I | Evidence and/or overall agreement that the treatment or method is beneficial, useful or effective | Recommended/indication |
| Class II | Inconsistent evidence and/or disagreement about the use/effect of the treatment or method | |
| Class IIa | Evidence/views tend to be useful/effective | Should be considered |
| Class IIb | Evidence/views are not sufficient to establish useful/effective | Can consider it |
| Class III | Evidence and/or expert agree that the treatment or method is useless/ineffective and may be harmful in some cases | Not recommended |
Table 2. Level of evidence.
| Level A | Data from multiple randomized controlled clinical trials or meta-analyses consisting of randomized controlled clinical trials |
| Level B | Data from a single randomized clinical trial or multiple large randomized controlled trials |
| Level C | Data from expert consensus and/or small-scale studies, retrospective studies or registration studies |
1. Prevalence of hypertension in Chinese population
Key point 1. Prevalence of hypertension in Chinese population
-
The prevalence of hypertension is still increasing in China.
There are two significant features of the population with hypertension in China: the prevalence of hypertension increases from the south to the north; the prevalence of hypertension varied among different ethnic groups.
The awareness, treatment and control (crude rate) of hypertension patients in China have increased significantly in recent years, reaching 51.6%, 45.8% and 16.8% respectively, but is overall at a low level.
The important risk factors for hypertension are high sodium intake, low potassium diet, overweight, and obesity in Chinese population.
1.1. Prevalence, incidence and epidemic trend of hypertension in Chinese population
The 2012–2015 national hypertension survey,[1] showed the overall crude prevalence of hypertension was 27.9% (weighted rate 23.2%) in Chinese residents aged 18 and over. Compared with the previous national surveys of hypertension conducted in 1958–1959, 1979–1980, 1991, 2002 and 2012,[2] the trend keeps on increasing, although the total participants, age and diagnostic criteria for each survey are not completely consistent (Table 3).
Table 3. Results of six prevalence rates surveys of hypertension in China.
| Year | No. of surveyed province/city/autonomous region | Age, yrs | Diagnostic criteria | No. of participants | No. of hypertension | Prevalence, % |
| 1958–1959 | 13 | ≥ 15 | Disunity | 739,204 | 37,773 | 5.1Δ |
| 1979–1980 | 29 | ≥ 15 | Diagnosis of hypertension: ≥ 160/95 mmHg | 4,012,128 | 310,202 | 7.7Δ |
| Critical hypertension: 140–159/90–95 mmHg | ||||||
| 1991 | 29 | ≥ 15 | ≥ 140/90 mmHg and (or) taking antihypertensive drugs within two weeks | 950,356 | 129,039 | 13.6Δ |
| 2002 | 29 | ≥ 18 | ≥ 140/90 mmHg and (or) taking antihypertensive drugs within two weeks | 272,023 | 51,140 | 18.8Δ |
| 2012 | 31 | ≥ 18 | ≥ 140/90 mmHg and (or) taking antihypertensive drugs within two weeks | - | - | 25.2¶ |
| 2015 | 31 | ≥ 18 | ≥ 140/90 mmHg and (or) taking antihypertensive drugs within two weeks | 451,755 | 125,988 | 27.9Δ |
ΔRough rate; ¶Comprehensive adjustment of prevalence.
The prevalence of hypertension increases significantly with age. According to the 2012–2015 national survey, the prevalence of hypertension in young people aged 18 to 24, 25 to 34, and 35 to 44 years old was 4.0%, 6.1%, and 15.0%, respectively.[1] It is higher in male than in female. The prevalence of hypertension in the north is still higher than that in the south. The pattern is gradually changing into a higher prevalence of hypertension in large and medium-sized cities, such as in Beijing (35.9%), Tianjin (34.5%) and Shanghai (29.1%),[1] respectively. The prevalence of hypertension in rural areas increased faster than that in urban areas. According to the national survey from 2012 to 2015, the prevalence rate in rural areas (crude rate 28.8%, standardized rate 23.4%) surpassed that of in urban areas (crude rate: 26.9%, standardized rate: 23.1%) for the first time. Compared with different ethnic groups, the prevalence of hypertension among Tibetans, Manchus and Mongolians is higher than that of Han, but is lower in Hui, Miao, Zhuang and Buyi.[3]
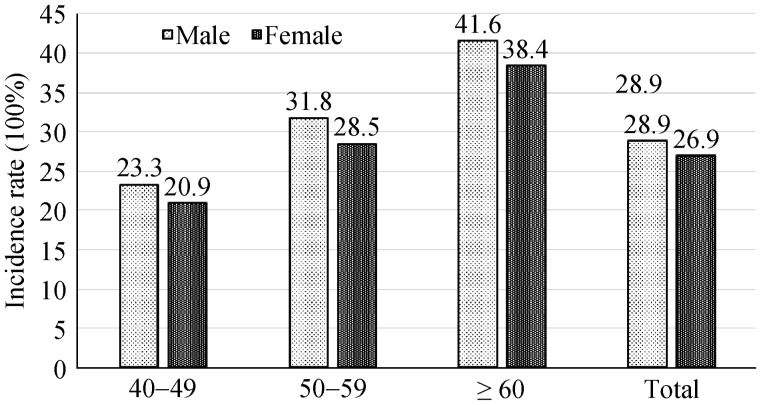
The research on the incidence of hypertension is relatively insufficient. One study with 10,525 non-hypertensive patients aged over 40 years of age showed: the cumulative incidence of hypertension in males and females was 28.9% and 26.9%, respectively, after follow up for an average of 8.2 years in 1991–2000,[4] the incidence increased with age (Figure 1).
Figure 1. Cumulative incidence of hypertension in different genders and baseline age groups from 1991 to 2000.
1.2. Awareness, treatment and control of hypertension in China
Awareness, treatment and control of hypertension are important parameters for reflecting status of the treatment and prevention of hypertension. According to the 2015 survey, the awareness, treatment, and control of hypertension in people over 18 years of age were 51.6%, 45.8%, and 16.8%, respectively, which were significantly higher than those in 1991 and 2002 (Table 4).[1] The prospective study of chronic diseases in China[5] from 2004 to 2009 showed that the rate of hypertension control was lower than that of 2002, which may be related to the sample method.
Table 4. Survey results of awareness, treatment and control (roughness rate) of hypertension in China.
| Year | Age, yrs | Awareness, % | Treatment, % | Control, % |
| 1991 | ≥ 15 | 26.3 | 12.1 | 2.8 |
| 2002 | ≥ 18 | 30.2 | 24.7 | 6.1 |
| 2012 | ≥ 18 | 46.5 | 41.1 | 13.8 |
| 2015 | ≥ 18 | 51.5 | 46.1 | 16.9 |
The awareness, treatment and control rate were higher in female than in male, and the treatment was significantly higher in urban than that in rural areas.[6] At the same time, these rates of residents in the southern region are higher than the north.[7],[8] With respect to ethnic groups, the treatment and control of hypertension is lower among ethnic minority than that of Han nationality.[1],[9]
1.3. Important risk factors for hypertension in Chinese population
Risk factors for hypertension include genetic factors, age, and unhealthy lifestyles. The clustering of risk factors is prevalent in the population. As the number and severity of hypertension risk factors increase, BP levels increase, and the risk of hypertension increases.[10]–[13]
1.3.1. High sodium, low potassium diet
High sodium and low potassium diets are important risk factors for hypertension in Chinese population. The INTERSALT study found that the median 24-h urinary sodium excretion increased by 2.3 g (100 mmol/day), and the median systolic blood pressure (SBP)/diastolic blood pressure (DBP) increased by an average of 5–7/2–4 mmHg. A survey found that the average cooking salt intake of residents aged 18 and over in China was 10.5 g in 2012, although it was lower than 12.9 g in 1992 and 12.0 g in 2002, but was still 75.0% higher than the recommended salt intake level,[15] while the Chinese population was generally sensitive to sodium.[14],[16]
1.3.2. Overweight and obesity
Overweight and obesity significantly increase the risk of all-cause mortality in the global population[17] and are also important risk factors for hypertension. For people aged 35–64, the overweight rate is 38.8%, and the obesity rate is 20.2%, which are higher in female than in male, in urban than in rural areas, and in north than south.[18] A follow-up study[19] on the relationship between overweight/obesity and hypertension in Chinese adults found that the risk of hypertension was 1.16 to 1.28 times higher in the overweight and obesity groups than in the normal weight group along with the increase of body mass index (BMI).[1]
Visceral obesity is closely related to hypertension. With the increase of visceral fat index, the risk of hypertension increases.[20] In addition, visceral obesity is closely related to metabolic syndrome, which can lead to abnormal glucose and lipid metabolism.[21]
1.3.3. Excessive drinking
Excessive drinking includes dangerous drinking (male: 41–60 g, female 21–40 g) and harmful drinking (more than 60 g for men and 40 g for women). Drinking is prevalent in China. The harmful drinking rate is 9.3%[15] among residents over 18 years old. Restricted drinking was significantly correlated with a drop in BP, with an average reduction in alcohol intake of 67%, a decrease in SBP of 3.31 mmHg and in DBP of 2.04 mmHg.[22] At present, there is insufficient evidence supports the correlation between cardiovascular health and less alcohol intake. However, some relevant research shows that even for people who drink a small amount of alcohol, reducing alcohol intake can improve cardiovascular health and reduce the risk of cardiovascular disease.[23]
1.3.4. Long-term nervousness
Long-term nervousness is a risk factor for hypertension, and mental stress can activate sympathetic nerves and increase BP.[24],[25] A meta-analysis of 13 cross-sectional studies and eight prospective studies[26] showed that the risk of hypertension was 1.18 times (95% CI: 1.02–1.37) and 1.55 times (95% CI: 1.24–1.94) among people with mental stress (defined as anxiety, stress, anger, panic or fear) than the normal population.
1.3.5. Other risk factors
In addition to the above risk factors for hypertension, other risk factors include age, family history of hypertension, lack of physical activity, and diabetes, etc. Studies have shown that exposure to PM2.5, PM10, SO2, and O3 is associated with increased risk of hypertension and increased mortality from cardiovascular disease.[27],[28]
2. Hypertension and cardiovascular risk
Key point 2. Hypertension and cardiovascular risk
BP is continuously, independently, directly and positively associated with cardiovascular risk.
Stroke is still the most important complication of hypertension in China by now, while the incidence of coronary events also increased evidently. Other complications include heart failure, left ventricular hypertrophy, atrial fibrillation and end-stage renal disease.
2.1. Relationship between BP and cardiovascular risk
There is a close causal relationship between BP and cardiovascular morbidity and mortality. A global prospective observational study of 61 populations (about 1 million people aged 40–89 years with the baseline BP ranging from 115/75 mmHg to 185/115 mmHg and with an average follow-up of 12 years)[29] showed that clinic SBP or DBP was continuously, independently, directly and positively associated with the risk of stroke, coronary heart disease (CHD) events and cardiovascular mortality. Each 20 mmHg increase in SBP or 10 mmHg increase in DBP was associated with doubled risk of cardiovascular and cerebrovascular morbidity.
In the Asia Pacific cohort study (APCSC) which consists of 13 Chinese populations,[30] clinic BP was closely associated with the risk of stroke and ischemic heart disease events, and the association between elevated BP and stroke or ischemic heart disease events in Asian populations was stronger than in Australia and New Zealand populations. For each 10 mmHg increase in SBP, the risk of stroke and fatal myocardial infarction increased by 53% and 31% respectively in Asian populations, while by 24% and 21% respectively in Australian and New Zealand populations.
There is also a causal relationship between BP level and heart failure. Clinical follow-up data showed that the incidence of heart failure increased with BP level.[31] Heart failure and stroke were the two complications most closely related to BP level. Chronic hypertension, left ventricular hypertrophy, heart failure constitute of an important chain of events. Hypertension mainly leads to heart failure with preserved ejection fraction, while if combined with CHD or myocardial infarction, it can also lead to heart failure with reduced ejection fraction.
Hypertension is an important cause of atrial fibrillation.[32] Hypertension-atrial fibrillation-cerebral embolism constitute of an important but easily overlooked chain of events.
Long-term clinical follow-up studies revealed that the incidence of end-stage renal disease (ESRD) also increased significantly with clinic BP.[33] The incidence of ESRD was 11 times higher in severe hypertension, and even 1.9 times higher in subjects with high normal BP compared to that in normotensive subjects.
The relationship between clinic BP and the above-mentioned complications and cardiovascular diseases has also been confirmed in studies on ambulatory or home BP monitoring.[34],[35] The 24-h ambulatory BP, nocturnal BP and morning BP were even more closely and significantly correlated with the risk of cardiovascular and cerebrovascular disease. Recent studies have also shown that long-term BP variation (BPV), which reflects BP fluctuations, may also be associated with cardiovascular risk.[35]
2.2. Cardiovascular risk characteristics of hypertension population in China
According to the population-based surveillance data in China,[36] cardiovascular and cerebrovascular diseases account for more than 40% of the total number of deaths. The annual incidence of stroke is 250/100,000, and the annual incidence of CHD events is 50/100,000. The incidence of stroke is five times higher than that of CHD events. In recent years, despite the ascending trend of the incidence of CHD events, the incidence difference between stroke and CHD events is still significant. In clinical trials, the incidence ratio of stroke/myocardial infarction is about 5:1–8:1 in hypertensives in China, while about 1: 1[37]–[41] in hypertensives in the Western countries. Therefore, stroke is still the major cardiovascular risk threatening the Chinese hypertensive population, and stroke prevention is an important goal of hypertension treatment in China.
3. Diagnostic evaluation
Diagnostic evaluation comprises the following three aspects: (1) to establish the diagnosis of hypertension, determine the stage of BP level; (2) to identify the etiology of hypertension, distinguish the primary or secondary hypertension; and (3) to search for other cardiovascular and cerebrovascular risk factors, target organ damage and their associated clinical conditions, so as to facilitate the differential diagnosis of hypertensive etiologies, assess the cardiovascular and cerebrovascular risk, and guide the diagnosis as well as the treatment.
3.1. Medical history
Patient's medical history should be comprehensively and thoroughly understood, including the following contents: (1) family history: the patients should be asked whether they have a family history of hypertension, stroke, diabetes mellitus, dyslipidemia, CHD or kidney disease, including the age at which cardiovascular and cerebrovascular events occur in first-degree relatives. (2) Clinical course: the time and place where hypertension was first detected or diagnosed the highest level of BP. If having been treated with anti-hypertensive drugs, type, dose, efficacy and side effects of anti-hypertensive drugs used in the past and at present should be recorded. (3) Symptoms and past history: inquire about the present and past history, symptoms and treatment of stroke or transient ischemic attacks, CHD, heart failure, atrial fibrillation, peripheral vascular disease, diabetes, gout, dyslipidemia, sexual dysfunction and kidney disease, etc. (4) Secondary hypertension clues: such as nephritis history or anemia history; muscle weakness, paroxysmal soft paralysis, etc; paroxysmal headache, palpitation, sweating; snoring with apnea; whether long-term use of drugs which can result in BP elevation. (5) Lifestyle: the dietary intake of salt, alcohol and fat, smoking status, physical activity, weight change, sleep habits, etc. (6) Socio-psychological factors: including patient's family situation, work environment, education background and history of psychological trauma.
3.2. Physical examination
Careful physical examinations are helpful in finding clues of secondary hypertension and target organ damages. Physical examinations include: BP measurement (see BP measurement section 3.5 for details), measurement of heart rate, BMI, and waist and hip circumference; observing whether there are features of Cushing's syndrome, skin stigmata of neurofibromatosis, eye signs suggestive of hyperthyroidism, or edema at the lower extremities; searching for murmurs via the auscultation at the carotid arteries, thoracic aorta, abdominal aorta and the femoral arteries; palpating the thyroid glands, examining thoroughly the heart and lungs, examining the abdomen to find out whether there is enlargement of kidneys (polycystic kidney) or masses, palpating the arterial pulses at the extremities, and performing neurological examinations.
3.3. Laboratory examinations
Routine examinations: blood chemistry (potassium, sodium, fasting blood glucose, lipids, uric acid and creatinine), blood routine test, urinalysis (urine protein, sugar, sedimentary microscopic examination), electrocardiogram, etc.
Recommended examinations include: echocardiography, carotid ultrasonography, oral glucose tolerance test, glycated hemoglobin, blood high-sensitivity C-reactive protein, urinary albumin/creatinine ratio, quantitative estimation of urinary protein, eye fundoscopy, chest X-ray, pulse wave velocity (PWV), and ankle-brachial BP index (ABI), etc.
Optional examinations include: blood homocysteine, for patients suspected of secondary hypertension. The following examinations might be performed if indicated: plasma renin activity or renin concentration, blood and urine aldosterone, blood and urine cortisol, blood free metanephrine and normetanephrine, blood or urine catecholamine, renal artery ultrasound and angiography, echogram, computed tomography (CT) or magnetic resonance imaging (MRI) of kidneys and adrenal glands, adrenal venous sampling, and polysomnography, etc. Hypertensives with comorbidity should be examined for relevant cardiac function, renal function and cognitive function.
3.4. Genetic analysis
Although genome-wide association studies (GWAS) of hypertension has reported a number of gene loci related to BP level or hypertension,[42] the current clinical genetic diagnosis is only applicable to Liddle syndrome,[43] glucocorticoid-remediable aldosteronism[44] and other monogenic inherited hypertension.
3.5. BP measurement
Key point 3A. Procedures for clinic BP measurement
Patient should be seated for at least 5 min in a quiet room before BP measurements, and keep the upper arm at the heart level.
Validated upper arm medical electronic sphygmomanometer is recommended, and mercury sphygmomanometer will be deprecated gradually.
Use a standard cuff (with a bladder of 12 cm wide and 22–26 cm long) for most patients, larger cuffs should be used for obese patients or those with large arm circumference (> 32 cm).
Measure BP on both arms at the first visit. Use the arm with higher value as the reference.
Two BP measurements should be taken 1–2 min apart and averaged for records. An additional measurement is required if the first two readings differ by > 5 mmHg, and the mean value of the three readings should be recorded.
Measure BP 1 min and 3 min after standing from a seated position in case of elderly patients, diabetic patients, and patients suspected orthostatic hypotension.
Heart rate should be measured together with BP.
Key point 3B: evaluation of various BP measurement methods
Clinic BP measurement is by now the common method to diagnose hypertension, grade the BP level category and observe the antihypertensive efficacy in China.
If possible, out-of-office BP measurement should be performed to diagnose white-coat hypertension and masked hypertension, evaluate the efficacy of antihypertensive therapy, and assist the diagnosis and treatment of resistant hypertension.[45]
Ambulatory BP monitoring can evaluate 24-h BP circadian rhythm, orthostatic hypotension, and postprandial hypotension, etc.
Home BP monitoring may assist in adjusting treatment regimens. Remote real-time BP monitoring based on internet is a new mode of BP management. Patients with high psychological anxiety are not recommended to have their BP checked frequently.
BP measurement is the fundamental means and method of evaluating BP level, diagnosing hypertension and observing antihypertensive efficacy. Clinic and out-of-office BP measurement are adopted frequently in clinical practice and population disease prevention and control, the latter refers to ambulatory BP monitoring (ABPM) and home BP monitoring (HBPM). Out-of-office BP measurement can provide large amount of BP data outside the medical environment, and its relationship with target organ damage is more significant than that of clinic BP, and it is better than clinic BP in predicting cardiovascular risk.[34],[46]
3.5.1. Clinic BP measurement
The clinic BP measurement is carried out by doctors or nurses, under standard conditions and unified guidelines. It is the common method to diagnose hypertension, grade the BP level category and observe the antihypertensive efficacy.
Upper arm medical electronic sphygmomanometer, which has been validated by international standardized protocols (ESH, BHS and AAMI) (electronic sphygmomanometer certification results are available in the following website: http://www.dableducational.org, http://www.bhsoc.org/default.stm), or mercury sphygmomanometer, which is up to the metrological standard (will be deprecated gradually), are used for the measurement. Automated office BP measurement (AOBP) can reduce the white-coat effect, which is worthy of further research and promotion.[47] See key point 3A for the measurement procedure. If mercury column sphygmomanometer is used for BP measurement, rapid inflation is required to let the inner pressure of the bladder go further up by 30 mmHg after the disappearance of the radial artery pulse downstream, and then deflate the bladder slowly at a speed of 2.0 mmHg per second. The deflation speed should be even slower if the heart rate is slow. Deflate the bladder quickly to zero after DBP reading is obtained; listen to the Korotkoff sound carefullly during the deflation of the bladder, watch the convex meniscus surface of the mercury column at its perpendicular height at the moment of Korotkoff phase I (the first sound) and phase V (the disappearance of the sound). Take the reading at Korotkoff phase I as SBP and the reading at Korotkoff phase V as DBP. In the case of children (< 12 years of age), pregnant women, patients with severe anemia, hyperthyroidism, aortic valve incompetence, or with the Korotkoff sound not disappearing, take the Korotkoff sound of phase IV (when the sound changes abruptly) as DBP. When reading the BP value, the last digit value can only be 0, 2, 4, 6, 8, and cannot be 1, 3, 5, 7, 9, and pay attention to avoiding the last digit preference. When measuring BP in patients with atrial fibrillation, there is often a long period of Korotkoff sound auscultation interval, which requires multiple measurements to obtain the mean value.
3.5.2. ABPM
ABPM with the use of automatic device can acquire multiple BP readings, avoid white-coat effect and there is no observer error. It is possible to measure BP during sleep at night, identify white-coat hypertension and masked hypertension, and diagnose isolated nocturnal hypertension. At present, the major clinical use of ABPM are: to diagnose white-coat hypertension, masked hypertension and isolated nocturnal hypertension; to observe abnormal BP rhythm and variation; to evaluate the efficacy of antihypertensive therapy and BP control over all time periods (including morning and sleep). (1) ABPM should be validated using international standardization protocols, and be calibrated regularly.[45] (2) Usually the monitors are programmed to measure BP every 15 to 20 min during the day and every 30 min during sleep at night. Ensure that BP is monitored effectively throughout 24-h, with at least one BP reading per hour, at least 70% of expected valid BP readings, and at least 20 measurements during the day and 7 measurements at night. (3) ABPM indices: 24-h, daytime (awakening), nighttime (sleep) SBP and DBP mean values.
3.5.3. HBPM
BP is measured by the person who is being measured, and can also be done with the help of family members, known as self-measured BP or HBPM. HBPM can be used to evaluate anti-hypertensive efficacy and long-term BP variation for days, weeks, months or even years, and can help to enhance patient's awareness of health participation, improve patient's compliance and adherence to treatment, and is suitable for long-term BP monitoring of patients.[48] With the development of BP telemonitoring technology and equipment, internet-based remote monitoring and management of HBP is expected to become a new model of BP management in the future, but more studies are needed to provide evidence of effectiveness and cost-effectiveness.
HBPM[48],[49] can be used for the BP monitoring of general hypertensive patients, so as to identify white-coat hypertension, masked hypertension and resistant hypertension, evaluate the long-term BP variation, assist in the assessment of anti-hypertensive efficacy, and predict cardiovascular risk and prognosis, etc. HBPM requires the selection of appropriate BP measurement devices, and patient education on BP self-measurement knowledge, skills and protocols. (1) Use upper-arm automatic electronic sphygmomanometer validated by international standardized protocols for home use. Wrist sphygmomanometer, finger sphygmomanometer, mercury column sphygmomanometer are not recommended for HBPM. Electronic sphygmomanometer should be calibrated regularly during use, at least once a year. (2) Monitoring protocol: for patients with firstly diagnosed hypertension or unstable hypertension, HBPM should be performed every morning and evening with 2–3 measurements each time and take the average; it is recommended to measure HBP for consecutive seven days and take the average BP of the last six days. Patients with stable and controlled BP are advised to have their BP measured one to two days a week, once in the morning and once in the evening. It is better to self-measure BP in the sitting position at fixed time after getting up in the morning, before taking antihypertensive medicines and breakfast, and after urination. (3) Keep a detailed record of the date and time of each BP measurement as well as all BP readings, not just the average. Complete BP records should be provided to the physician whenever possible. (4) HBPM is not recommended for patients with high psychological anxiety.
3.6. Evaluation of target organ damage
For patients with hypertension, the evaluation of target organ damage is an important part of the diagnostic evaluation of hypertension, especially the detection of asymptomatic subclinical target organ damage. Subclinical target organ damage can be reversed if detected early and treated timely. It is recommended to adopt methods, which are fit to individuals and local conditions, relatively simple, appropriate cost-effectiveness and easy to popularize, to screen and prevent subclinical target organ damage.
3.6.1. Heart
Left ventricular hypertrophy (LVH) is an independent risk factor for cardiovascular events. Routine examination methods include electrocardiogram and echocardiography. Electrocardiogram is simple and feasible, which can be used as a screening method for LVH. Commonly used parameters are: Sokolow-Lyon voltage (SV1+RV5) and Cornell voltage-duration product.[50] The sensitivity of echocardiography in the diagnosis of LVH is superior to that of electrocardiogram. Left ventricular mass index (LVMI) can be used to detect and diagnose LVH, and LVMI is a strong predictor of cardiovascular events. Other methods of assessing hypertensive cardiac damage include chest X-ray, exercise test, cardiac isotope imaging, computed tomography coronary angiography (CTA), cardiac magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA), coronary angiography, etc.
3.6.2. Kidney
Kidney damage is mainly characterized by elevated serum creatinine, reduced estimated glomerular filtration rate (eGFR), or increased urinary excretion of albumin. Microalbuminuria has been demonstrated as an independent predictor of cardiovascular events.[51] Hypertensive patients, especially those with diabetes mellitus, should be regularly monitored for urinary albumin excretion, 24-h urinary albumin excretion or urinary albumin/creatinine ratio. eGFR is a simple and sensitive indicator of renal function, which can be calculated by using “CKD-EPI formula”,[52] “MDRD formula”[53] or MDRD modified formula[54] proposed by Chinese researchers. Increased serum uric acid level may also have predictive value for cardiovascular risk.[55]
3.6.3. Large arteries
Carotid intima media thickness (IMT) can predict cardiovascular events,[56] and atherosclerotic plaques are more predictive than IMT.[57] There is growing evidence showing that increased large arterial stiffness predicts cardiovascular risk. Increased pulse wave velocity (PWV) is a strong predictor of cardiovascular events and all-cause mortality.[58] Carotid-femoral PWV (cfPWV) is the gold standard of arterial stiffness measurement.[59] Ankle-brachial index (ABI) is effective in screening and diagnosing peripheral arterial disease and predicting cardiovascular risk.[60]
3.6.4. Eye fundoscopy
Retinal arteriopathy can reflect small vascular lesions, and fundoscopy is particularly important for patients with both hypertension and diabetes mellitus. Among hypertensive fundus changes detected by conventional fundoscopy, according to Keith-Wagener and Barker four-grade taxonomies, Grade 3 or Grade 4 retinopathy in hypertensives is valuable for prognosis.[61] Recently, new fundoscopy techniques have been used to observe and analyze the remodeling of retinal arterioles.[62]
3.6.5. Brain
Cranial MRA or CTA can help to detect lacunar lesions, asymptomatic cerebrovascular lesions (such as intracranial arterial stenosis, calcification and plaque lesions, and hemangioma), and white matter lesions,[63] but it is not recommended for clinical screening of target organ damage. Transcranial doppler ultrasonography is helpful for the diagnosis of cerebral vasospasm, stenosis or occlusion. At present, the screening and evaluation of cognitive function mainly adopts the mini-mental state examination.
4. Classification and stratification of hypertension
Key point 4
Definition of hypertension: a clinic systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg without the use of anti-hypertensive medications. Hypertension is divided into grade 1, grade 2 and grade 3 based on the BP levels;
Cardiovascular risk was stratified according to BP level, cardiovascular risk factors, target organ damage, associated clinical complications and diabetes mellitus, which were divided into four levels: low risk, moderate risk, high risk and very high risk.
4.1. Classification by BP levels
At present, normal (SBP < 120 mmHg and DBP < 80 mmHg), high normal (SBP 120–139 mmHg and/or DBP 80–89 mmHg) and hypertension (SBP ≥140 mmHg and/or DBP ≥ 90 mmHg) are used to classify BP levels in China. The above classification applies to adults over 18 years of age.
In China, BP level of 120–139/80–89 mmHg is defined as ‘high normal’ mainly because our epidemiological studies have shown that the 10-year cardiovascular risk among this population is two times higher than those with BP < 110/75 mmHg. In addition, among the middle-aged population with a BP of 120–129/80–84 and of 130–139/85–89 mmHg, 45% and 64% respectively progressed to hypertension in ten years.[64]
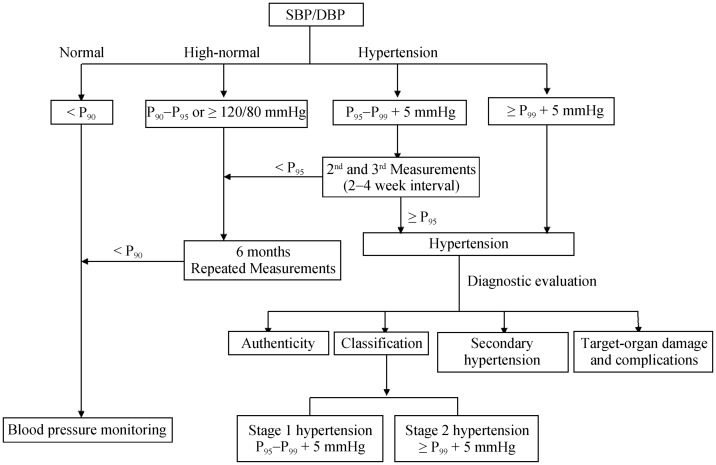
Hypertension is defined as a clinic systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg without the use of anti-hypertensive medications at three visits on different days. Systolic BP ≥ 140 mmHg and diastolic BP ≤ 90 mmHg is defined as isolated systolic hypertension. Subjects with a BP < 140/90 mmHg but having hypertensive history and currently are taking anti-hypertensive medication should also be diagnosed as hypertensives. Hypertension is divided into grade 1, grade 2 and grade 3 based on the levels of BP (Table 5). The diagnostic thresholds for hypertension based on ABPM is: 24-h mean SBP/DBP ≥ 130/80 mmHg; daytime SBP/DBP ≥ 135/85 mmHg; nighttime SBP/DBP ≥ 120/70 mmHg. The diagnostic thresholds of hypertension based on HBPM ≥ 135/85 mmHg, which is corresponding to 140/90 mmHg of clinic BP.
Table 5. Definitions and classification of BP levels.
| Category | SBP, mmHg | DBP, mmHg |
| Normal | < 120 | < 80 |
| High normal | 120–139 and (or) | 80–89 |
| Hypertension | ≥ 140 and (or) | ≥ 90 |
| Grade 1 (mild) | 140–159 and (or) | 90–99 |
| Grade 2 (moderate) | 160–179 and (or) | 100–109 |
| Grade 3 (severe) | ≥ 180 and (or) | ≥ 110 |
| Isolated systolic hypertension | ≥ 140 and | < 90 |
When a patient's systolic and diastolic BPs fall separately into different categories, the higher category should be taken. BP: blood pressure; DBP: diastolic blood pressure; SBP: systolic blood pressure.
Due to the low frequency of clinic BP measurement and the obvious fluctuation of BP, it is necessary to take multiple measurements within a few weeks to evaluate BP elevation, especially for grade 1 and grade 2 hypertension. If possible, 24-h ABPM or HBPM should be conducted.
4.2. Cardiovascular risk stratification
Although hypertension is an independent risk factor for the incidence and prognosis of cardiovascular events, it is not the only determinant. Most hypertensive patients have cardiovascular risk factors other than elevated BP. Therefore, the diagnosis and treatment of hypertension should base not only BP levels, but also comprehensive cardiovascular risk assessment and stratification. Cardiovascular risk stratification in hypertensive patients may help in determining appropriate time of starting antihypertensive therapy, optimizing antihypertensive therapy, establishing appropriate BP control target and conducting comprehensive management of patients.
For risk stratification, this guideline adopts the principle and basic contents of the 2005 and 2010 Chinese Hypertension Guidelines.[64],[65] Patients with hypertension are divided into four levels of cardiovascular risk: low risk, moderate risk, high risk and very high risk (Table 6). According to the implementation of the previous Chinese hypertension guidelines and relevant research progress, the contents affecting risk stratification have been partially modified (Table 7): BP range of 130–139/85–89 mmHg has been added; diagnostic criteria for hyperhomocysteinemia has been modified as ≥ 15 umol/L; inclusion of atrial fibrillation as a concomitant clinical disease; diabetes mellitus was divided into newly diagnosed and treated but not controlled according to the level of blood glucose (fasting and postprandial) and glycated hemoglobin, respectively.
Table 6. Cardiovascular risk stratification in patients with elevated BP.
| Other risk factors and medical history | BP, mmHg |
|||
| SBP 130–139 and (or) DBP 85–89 | SBP 140–159 and (or) DBP 90–99 | SBP 160–179 and (or) DBP 100–109 | SBP ≥ 180 and (or) DBP ≥ 110 | |
| No other risk factors | Low risk | Moderate risk | High risk | |
| 1–2 risk factors | Low risk | Moderate risk | Moderate to high risk | Very high risk |
| ≥ 3 risk factors, TOD or CKD grade 3 or diabetes mellitus without organ damage | Moderate/high risk | High risk | High risk | Very high risk |
| Clinical complications, or CKD grade ≥ 4, or diabetes mellitus with organ damage | High/very high risk | Very high risk | Very high risk | Very high risk |
BP: blood pressure; CKD: chronic kidney disease; DBP: diastolic blood pressure; SBP: systolic blood pressure; TOD: target organ damage.
Table 7. Important factors influencing cardiovascular prognosis in hypertensive patients.
| Cardiovascular risk factors | TOD | Concomitant clinical diseases |
|
|
|
|
Carotid ultrasonography (IMT ≥ 0.9 mm) or atherosclerotic plaque |
|
|
|
|
|
|
|
|
|
|
BMI: body mass index; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein; IMT: intima media thickness; LDL-C: low-density lipoprotein; LVMI: left ventricular mass index; TC: total cholesterol; TOD: Target organ damage.
5. Treatment of hypertension
5.1. Goal of hypertension treatment
Key point 5A
The fundamental goal of hypertension treatment is to reduce the overall risk of developing heart, brain, kidney and vascular complications and death.
The benefits of antihypertensive treatment derive primarily from the BP reduction per se.
On the basis of lifestyle improvement, antihypertensive drugs should be administered according to the overall risk level of hypertensive patients, while intervening in correctable risk factors, target organ damage and coexisting clinical diseases.
Intensive antihypertensive treatment strategy should be adopted to achieve maximum cardiovascular benefit if conditions allowed.
Goal of anti-hypertensive treatment: for general hypertensive patients, their BP should be reduced to < 140/90 mmHg (I, A),[1],[40],[66] and further lower level (< 130/80 mmHg) could also be applicable if patients can tolerant it or belongs to high-risk category (I, A).[37],[38],[67],[68]
The fundamental goal of hypertension treatment is to reduce the overall risk of developing heart, brain, kidney and vascular complications and the occurrence of death. Considering that hypertension is a cardiovascular syndrome, which is often combined with other cardiovascular risk factors, target organ damage and clinical disease, it is necessary to determine the timing and intensity of lifestyle improvement and antihypertensive drugs based on the BP level and overall risk level of hypertensive patients; meanwhile, it is also essential for intervening in other risk factors, target organ damage and coexisting clinical diseases that are detected. Given the unchanged situation in China that the major complication of hypertensive patients is still stroke,[36] intensive antihypertensive treatment strategy should therefore be adopted when conditions permit.
Based on the evidence from previous studies,[2],[3],[15],[40] the goal of BP control should be managed below 140/90 mmHg in general patients; under tolerable and sustainable conditions, some patients with diabetes, proteinuria, etc. who belong to high-risk category can control their BP below 130/80 mmHg. Although evidence suggests lower or higher BP goal in special population exists,[37],[38] but this mainly depends on the patients' tolerance and the complexity of their treatment. If a patient can reduce BP to lower level without carrying out a complex treatment regimen and can tolerate it, then there is no need to change the regimen to get the BP restored.
When selecting the kind and the intensity of treatment regimen, it should be balanced between long-term benefits and patient tolerability, so as to reduce or avoid withdrawal due to the patients' intolerance. Intensive interventions for high-risk and very-high-risk patients are justified, as well as aggressive interventions to reverse target organ damage in patients with subclinical target organ damage without severe comorbidities. However, when antihypertensive drugs are administered to high-normal BP populations with low or moderate risk, there is still insufficient evidence from clinical trials with the prognostic endpoint as the research objective.
Although some studies[39],[69],[70] have shown that elderly hypertensive patients' BP have a higher goal than those general patients, recent subgroup analysis of some studies also showed that a lower BP goal (SBP < 130 mmHg) is beneficial to the elderly population.[38] It should be noted that age growth is not a sufficient condition for setting a higher goal for antihypertensive treatment. For elderly patients, based on the severity of patients' comorbidities, physicians should evaluate the compliance and the adherence to treatment comprehensively, and determine their treatment goals of BP.
5.2. Therapeutic strategies
Key point 5B
The way to achieve antihypertensive treatment target: in addition to hypertensive emergencies and hypertensive urgencies, most hypertensive patients' BP should be gradually reduced to the target level within 4 weeks or 12 weeks according to their condition (I, C).
Timing of antihypertensive drug therapy: on the basis of lifestyle improvement, patients with BP still ≥ 140/90 mmHg and/or above target BP should initiate drug therapy (I, A).
(1) Target of antihypertensive treatment: the purpose of antihypertensive treatment for hypertensive patients is to effectively prevent or delay the occurrence of complications such as stroke, myocardial infarction, heart failure and renal insufficiency by reducing their BP, and to effectively control hypertension's progression and prevent the occurrence of severe hypertension such as hypertensive emergencies and hypertensive urgencies. Earlier antihypertensive trials with the inclusion criteria of DBP (≥ 90 mmHg) showed that each 5 mmHg lowering in DBP (10 mmHg lowering in SBP) would result in a decrease of stroke risk by 40% and ischemic heart disease by 14%, respectively;[71] later trials of antihypertensive treatment for isolated systolic hypertension (SBP ≥ 160 mmHg, DBP < 90 mmHg) showed that each 10 mmHg lowering in SBP (4 mmHg lowering in DBP) would result in a decrease of stroke risk by 30% and ischemic heart disease by 23%, respectively.[72] Recent studies, such as Systolic Blood Pressure Intervention Trial (SPRINT), Action to Control Cardiovascular Risk in Diabetes (ACCORD) also showed that intensive BP control is beneficial for patients of different age groups and/or patients with heart, kidney or diabetes comorbidities.[37],[38]
(2) The way to achieve antihypertensive treatment target: reducing BP to the target level can significantly reduce the risk of cardio-cerebrovascular complications. In addition to hypertensive emergencies and hypertensive urgencies, most hypertensive patients' BP should be gradually reduced to the target level within 4 weeks or 12 weeks according to their condition. For the young and for patients with shorter course of hypertension, BP might be reduced faster, whereas for elderly patients with longer course of hypertension, poor tolerability and combined with comorbidities, BP might be reduced slightly slower. Subgroup analysis of the FEVER study suggested that after medication, patients who reach the target BP within one month may further reduce their risk of cardiovascular events than those who meet the criteria behind that time.
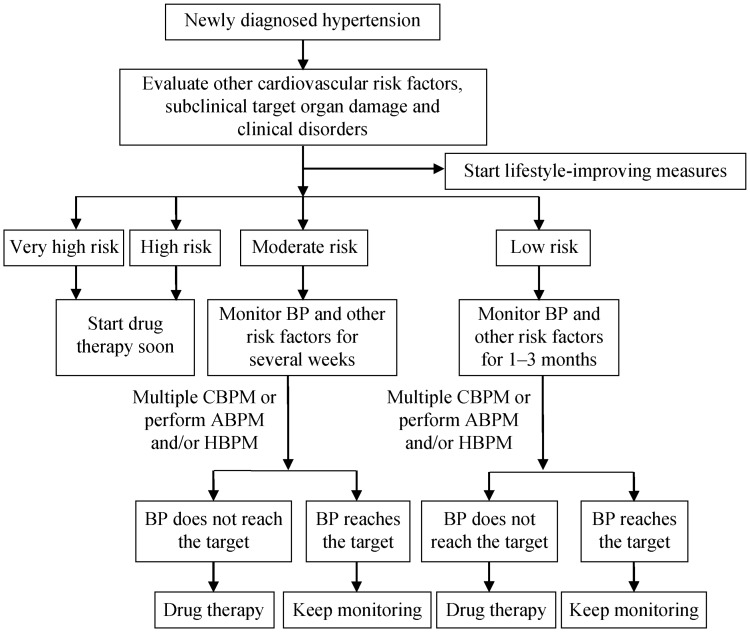
(3) Timing of antihypertensive drug therapy: the timing of antihypertensive drug therapy depends on the level of cardiovascular risk assessment. On the basis of lifestyle improvement, patients with BP still ≥ 140/90 mmHg and/or above target BP should initiate drug therapy. For patients with high and very high risk, drug therapy must be started soon, and comprehensive treatment should be performed for the associated risk factors and clinical conditions; patients with moderate risk can be observed for several weeks to assess target organ damage and improve lifestyle, if target BP is still not achieved, drug therapy ought to be started; patients with low risk, can be observed for one to three months with a close follow-up, performing out-of-office BP monitoring whenever possible, assessing target organ damage and improving lifestyle, if target BP could still not be achieved, drug therapy can be started.
This strategy should be followed especially for newly diagnosed hypertensive patients. The assessment and monitoring procedures are shown in Figure 2.
Figure 2. Evaluation and monitoring procedures for newly diagnosed hypertension.
Diagnostic criteria of hypertension for ABP is daytime mean SBP ≥ 135 mmHg or DBP ≥ 85 mmHg, nighttime mean SBP ≥ 120 mmHg or DBP ≥ 70 mmHg, or 24-h mean SBP ≥ 130 mmHg or DBP ≥ 80 mmHg; that criteria for home blood pressure is mean SBP ≥ 135 mmHg or DBP ≥ 85 mmHg. Moderate risk patients with BP ≥ 160/100 mmHg should start drug therapy immediately. ABPM: ambulatory blood pressure monitoring; BP: blood pressure; CBPM: clinic blood pressure monitoring; DBP: diastolic blood pressure; HBPM: home blood pressure monitoring; SBP: systolic blood pressure.
5.3. Lifestyle intervention
Key point 5C
Lifestyle interventions are reasonable and effective treatments for any hypertensive patients (including normal high-value patients and hypertensive patients requiring medication) at any time, aim to lower BP, control other risk factors and clinical conditions.
-
Lifestyle interventions have positive effects towards reducing BP and cardiovascular risk, [73]–[75] which should be used in all patients. The main measures include:
To reduce sodium intake, gradually reduce the daily salt intake to < 6 g, and increasing potassium intake (I, B)[74]–[79]
Reasonable meal, balanced diet (I, A)[80]–[83]
To control body weight to make BMI < 24, and to make waist circumference < 90 cm
for male and < 85 cm for female (I, B)[84]–[86]
Do not smoke, completely quit smoking, and avoid passive smoking (I, C).[87],[88]
Do not drink or restrict alcohol (I, B)[22],[89]–[91]
To increase exercise, medium intensity; 4–7 times per week; 30–60 min each time (I, A)[92]–[94]
To reduce mental stress and maintain psychological balance (IIa, C)[95]
Lifestyle interventions can reduce BP, prevent or delay the onset of high BP, and reduce the risk of cardiovascular disease.[96]–[99] In this guideline, lifestyle interventions include promoting healthy lifestyles and eliminating behaviors and habits that are unconducive to physical and mental health. Lifestyle interventions should be continued throughout the entire process of hypertension treatment, in combination with medication,[100] if necessary. The details are as follows.
5.3.1. Sodium intake reduction and potassium intake increase
Sodium salt can significantly increase BP and the risk of hypertension, and the moderate reduction of sodium intake can effectively lower BP.[75],[79] Excessive sodium intake and/or insufficient potassium intake, as well as a low ratio of potassium to sodium intake are important risk factors for hypertension in China.[101],[102]
Around 75.8% of the sodium in the diet of Chinese residents comes from household cooking salt, followed by high-salt seasoning. As dietary patterns change, sodium salt in processed foods will also become important pathways for sodium intake.[103] In order to prevent high BP and reduce BP in hypertensive patients, sodium intake should be reduced to 2400 mg/day (6 g sodium chloride). All hypertensive patients should take various measures to limit sodium intake. The main measures include: (1) reducing cooking salt and sodium-containing condiments (including monosodium glutamate, soy sauce); (2) avoiding or reducing processed foods with high sodium content, such as pickles, ham, all kinds of roasted seeds and vegetables; and (3) it is recommended to use a quantitative salt spoon as much as possible during cooking to serve as a warning.
Increasing potassium intake in the diet can reduce BP.[74] The main measures are: (1) increasing the intake of potassium-rich foods (fresh vegetables, fruits and beans); and (2) individuals with good kidney function can choose low-sodium potassium-rich alternative salts. It is not recommended to take potassium supplements (including drugs) to reduce BP. Patients with renal insufficiency should consult a doctor before potassium supplementation.
5.3.2. Reasonable diet
A reasonable diet mode can reduce the risk of hypertension and cardiovascular disease in the population.[80]–[83] Hypertensive patients and those with normal BP who are at risk of developing hypertension are recommended that the diet should be based on fruits, vegetables, low-fat dairy products, whole grains rich in dietary fiber, and protein derived from plants to reduce saturated fat and cholesterol intake. DASH (Dietary Approaches to Stop Hypertension) diet is rich in fresh vegetables, fruits, low-fat (or skim) dairy products, poultry, fish, soybeans and nuts, it has less sugar, sugary drinks and red meat, it also has low levels of saturated fat and cholesterol, and it is rich in trace elements such as potassium, magnesium and calcium, high quality protein and cellulose.[80] For hypertensives, DASH diet can reduce SBP 11.4 mmHg and DBP 5.5 mmHg respectively,[80] the general population can reduce SBP 6.74 mmHg and DBP 3.54 mmHg respectively. If hypertensives control caloric intake, BP drop will be greater.[81] Compliance with DASH diet can effectively reduce the risk of CHD and stroke.[82],[83]
5.3.3. Weight control
It is recommended to maintain weight in a healthy range (BMI: 18.5–23.9 kg/m2, waist circumference < 90 cm for male, < 85 cm for female).[104] All overweight and obese patients were recommended to lose weight. Weight control is an intervention that includes controlling calorie intake, increasing physical activity, and behavioral interventions. Firstly, calorie intake control should include reducing daily total calorie intake, controlling intake of high-calorie foods (high-fat foods, sugary drinks and alcohol), and proper control of carbohydrate intake, and they all base on dietary balance. Then, increasing physical activity is advancing regular moderate-intensity aerobic exercise and reducing sedentary time. In addition, behavior therapy, such as establishing diet awareness, making meal plans, recording the type and weight of food intake, and calculating calories, can help to reduce weight. For those who are not ideal for weight loss in comprehensive lifestyle interventions, it is recommended to use medication or surgery. For special individuals, such as lactating women and the elderly, individualized weight loss measures should be used as appropriate.[105] The weight loss plan should be adhered to in the long term, the speed varies from person to person, no quick results should be rushed for. It is recommended to make a target that losing 5% to 10% of the initial weight in a year.[106],[107]
5.3.4. Smoking cessation
Smoking is an unhealthy behavior and one of the major risk factors for cardiovascular disease and cancer. Passive smoking significantly increases the risk of cardiovascular disease.[108] Although smoking cessation does not help for controlling BP,[109] it can reduce the risk of cardiovascular disease.[88]
The benefits of quitting smoking are very positive, therefore, physicians should strongly recommend and urge patients with hypertension to quit smoking, they also should ask each patient about the daily amount and smoking habits, and then, advise them to quit smoking in a clear, strong, and personalized way. After assessing the smoker's willingness to quit, physicians should help the smoker to start smoking cessation with the “sudden stop method” after 1–2 week preparation period. At the same times, they should instruct patients to apply smoking cessation drugs for withdrawal symptoms, such as nicotine patches, nicotine chewing gum (over-the-counter), bupropion hydrochloride sustained-release tablets and varenicline. Above all, following up and supervising successful quitters to avoid relapse.
5.3.5. Restrict drinking
Excessive drinking significantly increases the risk of developing hypertension, and its risk increases with the increasing consumption of alcohol. Limiting drinking could reduce hypertension. Hypertension patients are not advised to drink alcohol. In case of drinking, better mild wine than strong wine. Daily alcohol intake does not exceed 25 g for men and 15 g for women. The weekly alcohol intake does not exceed 140 g for men and 80 g for women.[110] Liquor, wine, and beer intake are less than 50 mL, 100 mL, and 300 mL,[22] respectively.
5.3.6. More exercise
Exercise can improve BP levels. Aerobic exercise reduced SBP by 3.84 mmHg, DBP 2.58 mmHg on average.[94] Cohort studies have found that regular exercise in hypertensives reduces the risk of cardiovascular death and all-cause mortality.[93] Therefore, it is recommended that non-hypertensives who want to reduce the risk of high BP or hypertensive who is willing to reduce BP should execute moderate-intensity exercise with accumulated for 30 to 60 min per day, 4 to 7 days per week,[111] such as walking, jogging, cycling, swimming, etc. The types of exercise can be categorized under aerobic, impedance and stretching.[94] Aerobic exercise is the priority type, and anaerobic exercise as the supplementary type. Exercise intensity must vary from person to person. The maximum heart rate during exercise is used to assess exercise intensity. Medium-intensity exercise is an exercise about 60% to 70% of achieving maximum heart rate [maximum heart rate (times/min) = 220 – age]. High-risk patients need to be evaluated before exercise.
5.3.7. Reducing stress and maintain psychological balance
Mental stress can activate the sympathetic nerves which could raise hypertension,[24],[25] the main reasons of increasing mental stress include excessive work, life stress and morbid psychology. Morbid psychology covers depression, anxiety, Type A personality, social isolation, lack of social support and so on. Doctors should manage stress of hypertensives by guiding them to individualized cognitive behavioral interventions. If necessary, doctors could use psychotherapy combined with medication to relieve anxiety and stress in patients. Drugs that are primarily suitable for anxiety disorders include benzodiazepines which include alprazolam, lorazepam and selective 5-HT1A receptor agonists such as buspirone, tandospirone and so on. Patients can also be advised to visit a professional medical institution to avoid BP fluctuations due to mental stress.
5.4. Pharmacological therapy of hypertension
Key point 5D. Basic principles of anti-hypertensive treatment
All five classes of anti-hypertensive drugs commonly used are suitable for the initiation of anti-hypertensive therapy. It is recommended that the choice of specific drugs should be based on the type of special population and comorbidities so as to the individualized treatment.
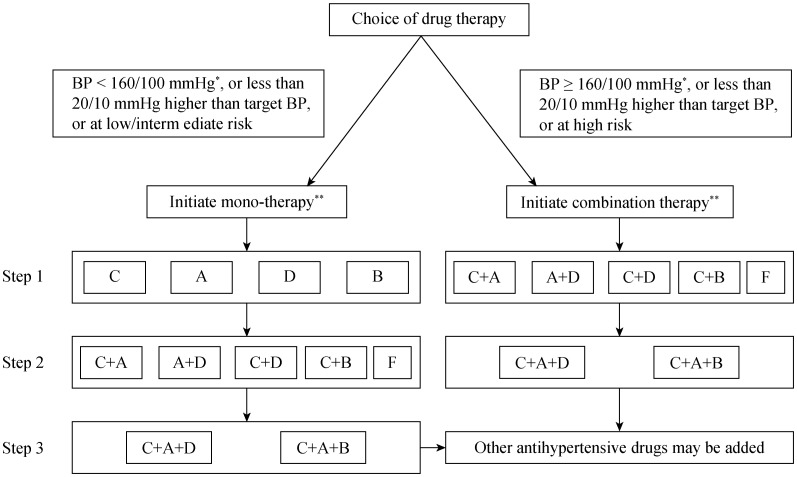
The intimal selection between mono-therapy and combination therapy should be based the baseline BP and the cardiovascular risk factors.
Ordinary patients start with regular dose, while the elderly is initiated with lower effective therapeutic dose. It can be considered to gradually titrate to the full dosage according to the treatment demand.[70],[112]–[115]
It is preferred to use long-acting agents to control 24-h BP, which can prevent cardio- and cerebrovascular complications more effectively.[40],[116]–[118]
It is recommended that high-risk group of patients with BP ≥ 160/100 mmHg or 20/10 mmHg higher than that of the target BP, or patients who receive mono-therapy and do not achieve the goal BP should be treated with combination therapy (I, C), including fixed combination preparations or a free combination of two or more agents.[119]
It is feasible to initiate with small dose combination therapy for patients with BP ≥ 140/90 mmHg (I, C).[67],[120]–[123]
5.4.1. Clinical trail basis of anti-hypertensive treatment
Since the 1950s, a series of randomized controlled trials of anti-hypertensive therapy which mainly targeted cardio- and cerebrovascular complications has established a theoretical basis for the treatment and management of hypertension.
These clinical trials can be divided into four types. (1) Early trials, which had a placebo control or untreated control, has demonstrated anti-hypertensive treatment can significantly reduce the risk factors of cardio- and cerebrovascular complications in various group of patients.[71],[72] These studies have established the most important theoretical basis for the treatment and management of hypertension.
(2) The compared trials involving different types of anti-hypertensive regimens mainly focus on the comparison between newer type of anti-hypertensive agents drugs (CCB, ACEI and ARB) and traditional ones (thiazide diuretics, β-blockers, etc.). The outcome reveals that reducing BP per se is the most important reason for these drugs to reduce cardio- and cerebrovascular complications.[124],[125] Differences between antihypertensive agents are generally small, but their effects on cause-specific outcomes still exist, and there are also differences in the results of different combination therapy trials.
(3) Trials taking hypertensive patients as the research subjects target to certain the most appropriate goal BP to treat hypertension by comparing the effect of intensive blood-pressure control and that of standard treatment.[37],[38],[126]
(4) Trials taking patients with moderate or high cardiovascular risk as the research subjects suggest that after BP is controlled under the target level of 140/90 mmHg, to further reduce BP should be tailored to individual conditions, which demands taking the patient's disease characteristics and the treatment plan including its composition and implementation method into full consideration.
China has also independently completed a series of clinical trials of antihypertensive therapy and contributed to several international multi-center clinical trials. Three early trials Syst-China,[39],[127] STONE[128] and CNIT[129] all confirmed that active anti-hypertensive treatment based on calcium channel blockers (CCBs, such as nitrendipine, nifedipine, etc.) can significantly reduce Chinese hypertensive patients' incidence and mortality of stroke. Furthermore, the FEVER trial showed that although the SBP/DBP decrease is as small as 4/2 mmHg induced by the add-on therapy of felodipine to hydrochlorothiazide, the incidence of fatal and non-fatal stroke was markedly reduced by 27%.[42] Further subgroup analysis of the FEVER revealed that the stroke, cardiac events and total mortality were lowest when the mean BP level was below 120/70 mmHg after treatment.[66] The elderly patients with SBP < 140 mmHg benefit more from anti-hypertensive therapy than those of higher BP. The study phase report of CHIEF documented that initial treatment of low-dose amlodipine combination with telmisartan or compound amiloride can significantly reduce the BP level in hypertensive patients, with the control rates reached about 80%, which suggests CCB-based combination therapy is one of the optimal antihypertensive medication for Chinese hypertensive patients.[120]
The Post-stroke Antihypertensive Treatment Study (PATS) completed by China independently was the first large-scale, placebo-controlled clinical trial of antihypertensive therapy for the post-stroke secondary prevention in the world. The results showed a decrease of 5/2 mmHg and 29% recurrence in the BP and stroke respectively induced by indapamide (2.5 mg/day) compared with the placebo.[130],[131] Thereafter, the result of the perindopril protection against recurrent stroke study (PROGRESS) in which China has cooperated showed that perindopril-based therapy reduced the recurrence of stroke by 28%, and the combination with indapamide produced larger reductions in BP than mono perindopril did.[132] The outcome of subgroup analysis showed that the risk of stroke reduction was larger in Asian participants such as the Chinese and the Japanese.[133] The post-hoc analysis determined that no “J-curve” phenomenon was observed even when the average BP fell to 112/72 mmHg after the treatment.[134] A further study was followed up in the 1560 enrolled Chinese patients and the average 6-year data confirmed that antihypertensive treatment significantly reduced the risk of stroke recurrence, total mortality and myocardial infarction.[135]
Chinese also participated in the three international multi-center clinical trials: “the Hypertension in the Very Elderly Trial” (HYVET),[70] “the Action in Diabetes and Vascular disease: preterAx and diamicroN-MR Controlled Evaluation” (ADVANCE)[122] and “the Heart Outcomes Prevention Evaluation” (HOPE-3).[67] The HYVET study showed that hypertension treatment based on indapamide (sustained release) in the very elderly (≥ 80 years old) with SBP above 160 mmHg, aimed to achieve a target BP of 150/80 mmHg, is beneficial and is associated with reduced risks of death from stroke and any cause.[70] The ADVANCE trial showed that compared to antihypertensive conventional treatment, a low-dose fixed combination of perindopril/indapamide produced a reduction of 5.6/2.2 mmHg and down to 135/75 mmHg in patients with diabetes, lowering the combined endpoints rate of major macrovascular or microvascular event by 9%.[122]
In the HOPE-3 trial, treatment with candesartan plus hydrochlorothiazide lowered BP by 6.0/3.0 mmHg as compared with placebo. Patients in the treatment group with SBP above 143.5 mmHg had significantly lower rates of cardiovascular risk than those in the placebo group. By contrast, no reduction of cardiovascular risk was observed among the patients in the active-treatment group who had an SBP below 131.5 mmHg.[67] The SPRINT study, mainly recruiting the US hypertensive patients, was a clinic trial conducted with a strategy of intensive blood-pressure control by using multiple antihypertensive drugs. Patients in the intensive-treatment group with the mean SBP reduced to 121 mmHg had lower incidence of cardio- and cerebrovascular complications, especially in the rates of heart failure, compared with those in the standard-treatment group with the mean SBP reduced to 135 mmHg.[38]
Hyperhomocysteinemia is positively associated with stroke risk.[136]–[138] Clinical trials conducted in China (such as multivitamin treatment trials,[139] meta-analysis of folic acid treatment trials[140] and CSPPT–China stroke primary prevention trial[41],[141],[142]) have shown that supplementation with folic acid can reduce plasma homocysteine concentration and reduce the risk of stroke. However, the role of folic acid in the prevention of stroke in hypertensive patients with high homocysteine still requires multi-center clinical trials for further validation.
5.4.2. Principles of drug treatment
(1) Initial dose: Ordinary patients start with regular dose, while the elderly is initiated with lower effective therapeutic dose. It can be considered to gradually titrate to the full dosage according to the treatment demand.[70],[113]–[116]
(2) Long-acting agents: it is preferred to use long-acting agents to control 24-h BP, which can prevent cardio- and cerebro-vascular complications more effectively.[40],[117]–[120] If intermediate-acting or short-acting agents are used, they should be administered two to three times per day in order to achieve a smooth BP control.
(3) Combination therapy: it is recommended that high-risk group of patients with BP ≥ 160/100 mmHg and 20/10 mmHg higher than that of the target BP, or patients who receive mono-therapy and do not achieve the goal BP should be treated with combination therapy, including fixed combination preparations or a free combination of two or more agents.[71] For patients with BP ≥ 140/90 mmHg, it is also feasible to initiate with small dose combination therapy.[67],[122]–[125]
(4) Individualized treatment: the choice of anti-hypertensive drugs should be based on the individual conditions of the patient, the patients' comorbidities, drug efficacy and tolerance, as well as the personal will and the long-term financial reach.
(5) Pharmacoeconomics: hypertension requires lifelong treatment and the cost/benefit should be taken into consideration.
5.4.3. Classes of anti-hypertensive drugs
Currently recommended anti-hypertensive drugs include five classes, i.e., calcium channel blockers (CCB), angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARB), diuretics, β-blockers, and fixed-ratio compound preparations composed of the above drugs.
All the 5 classes of anti-hypertensive drugs are suitable for the initiation and maintenance of anti-hypertensive therapy. Rational use of drugs should be based on patient risk factors as well as target organ subclinical damage plus clinical disease, and give preference to certain types of these drugs.[143],[144] (Tables 8 & 9). These clinical conditions can be referred to as strong indications (Table 10). Sometimes α-blockers and other types of antihypertensive drugs can also be used in certain hypertension populations. The selection criteria of these anti-hypertensive drugs for clinical practice are listed Table 11.
Table 8. Anti-hypertensive drugs commonly available.
| Oral agents | Does per day, mg (initiation–full) | Times per day | Major side effects |
| Dihydropyridines CCB | Ankle edema, headache and flushing | ||
| Nifedipine | 10–30 | 2–3 | |
| Slow release | 10–80 | 2 | |
| Control release | 30–60 | 1 | |
| Amlodipine | 2.5–10 | 1 | |
| Levamlodipine | 2.5–5 | 1 | |
| Felodipine | 2.5–10 | 2 | |
| Slow release | 2.5–10 | 1 | |
| Lacidipine | 4–8 | 1 | |
| Nicardipine | 40–80 | 2 | |
| Nitrendipine | 20–60 | 2–3 | |
| Benidipine | 4–8 | 1 | |
| Lercanidipine | 10–20 | 1 | |
| Manidipine | 5–20 | 1 | |
| Cinildipine | 5–10 | 1 | |
| Barnidipine | 10–15 | 1 | |
| Non-dihydropyridines CCB | A-V block and negative inotropic cardiac effect | ||
| Verapamil | 80–480 | 2–3 | |
| Slow release | 120–480 | 1–2 | |
| Diltiazem | 90–360 | 1–2 | |
| Thiazide diuretic | Hypokalemia, hyponatremia and hyperuricemia | ||
| Hydrochlorothiazide | 6.25–25 | 1 | |
| Chlorthalidone | 12.5–25 | 1 | |
| Indapamide | 0.625–2.5 | 1 | |
| Slow release | 1.5 | 1 | |
| Loop diuretics | Hypokalemia | ||
| Furosemide | 20–80 | 1–2 | |
| Torasemide; | 5–10 | 1 | |
| Potassium sparing diuretics | Hyperkalemia | ||
| Amiloride | 5–10 | 1–2 | |
| Triamterene | 25–100 | 1–2 | |
| Aldosterone receptor antagonists | |||
| Spirolactone | 20–60 | 1–3 | Hyperkalemia and gynecomastia |
| Eplerenone | 50–100 | 1–2 | |
| β-blockers | Bronchospasm and negative inotropic cardiac effect | ||
| Bisoprolol | 2.5–10 | 1 | |
| Metoprolol | 50–100 | 2 | |
| Slow release | 47.5–190 | 1 | |
| Atenolol | 12.5–50 | 1–2 | |
| Propranolol | 20–90 | 2–3 | |
| Betaxolol | 5–20 | 1 | |
| α- and β-blockers | Postural hypotension and bronchospasm | ||
| Labetalol | 200–600 | 2 | |
| Cavedilol | 12.5–50 | 2 | |
| Arotinolol | 10–20 | 1–2 | |
| ACEI | Coughing, hyperkalemia and angioedema | ||
| Captopril | 25–300 | 2–3 | |
| Enalapril | 2.5–40 | 2 | |
| Benazepril | 5–40 | 1–2 | |
| Lisinopril | 2.5–40 | 1 | |
| Ramipril | 1.25–20 | 1 | |
| Fosinopril | 10–40 | 1 | |
| Cilazapril | 1.25–5 | 1 | |
| Perindopril | 4–8 | 1 | |
| Imidapril | 2.5–10 | 1 | |
| ARB | Hyperkalemia and angioedema (rare) | ||
| Losartan | 25–100 | 1 | |
| Valsartan | 80–160 | 1 | |
| Irbesartan | 150–300 | 1 | |
| Telmisartan | 20–80 | 1 | |
| Candesartan | 4–32 | 1 | |
| Olmesartan | 20–40 | 1 | |
| Allisartan Isoproxil | 240 | 1 | |
| α-blockers | Postural hypotension | ||
| Doxazosin | 1–16 | 1 | |
| Prazosin | 1–10 | 2–3 | |
| Terazosin | 1–20 | 1–2 | |
| Centrally acting agents | |||
| Reserpine | 0.05–0.25 | 1 | Nasal congestion, depression, bradycardia, and digestive ulceration |
| Clonidipine | 0.1–0.8 | 2–3 | Hypotension, xerostomia, drowsiness |
| Clonidipine patch | 0.25 | 1/week | Skin allergy |
| Methyldopa | 250–1000 | 2–3 | Liver function damage and immune dysfunction |
| Vasodialatators | |||
| Minoxidila | 5–100 | 1 | Hypertrichosis |
| Hydralazineb | 25–100 | 2 | Lupus syndrome |
| Renin inhibitors | |||
| Aliskiren | 150–300 | 1 | Diarrhea and hyperkalemia |
aListed in Europe and the United States, unlisted in China; bApproved in China. ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blockers; CCB: calcium channel blockers.
Table 9. Single-pill combination preparations.
| Major components and single dose | Tablets per day | Times per day | Major side effects | |
| Losartan pot./Hydrochlorothiazide | Angioneurotic edema (occasional) and abnormal serum potassium | |||
| 50 mg/12.5 mg | 1 | 1 | ||
| 100 mg/12.5 mg | 1 | 1 | ||
| 100 mg/25 mg | 1 | 1 | ||
| Valsartan/Hydrochlorothiazide | Angioneurotic edema (occasional) and abnormal serum potassium | |||
| 80 mg/12.5 mg | 1–2 | 1 | ||
| Irbesartan/Hydrochlorothiazide | 1 | 1 | Angioneurotic edema (occasional) and abnormal serum potassium | |
| 150 mg/12.5 mg | ||||
| Telmisartan/Hydrochlorothiazide | 1 | 1 | Angioneurotic edema (occasional) and abnormal serum potassium | |
| 40 mg/12.5 mg | ||||
| 80 mg/12.5 mg | 1 | 1 | ||
| Olmesartan/Hydrochlorothiazide | 1 | 1 | Angioneurotic edema (occasional) and abnormal serum potassium | |
| 20 mg/12.5 mg | ||||
| Captopril/Hydrochlorothiazide | 1–2 | 1–2 | Coughing, angioneurotic edema (occasional), abnormal serum potassium | |
| 10 mg/6 mg | ||||
| Lisinopril/Hydrochlorothiazide | 1 | 1 | Coughing, angioneurotic edema (occasional), abnormal serum potassium | |
| 10 mg/12.5 mg | ||||
| Enalapril/Hydrochlorothiazide | 1 | 1 | Coughing, angioneurotic edema (occasional), abnormal serum potassium | |
| 5 mg/12.5 mg | ||||
| Benazepril/Hydrochlorothiazide | 1 | 1 | Coughing, angioneurotic edema (occasional), abnormal serum potassium | |
| 10 mg/12.5 mg | ||||
| Perindopril/Indapamide | 1 | 1 | Coughing, angioneurotic edema (occasional), abnormal serum potassium | |
| 4 mg/1.25 mg | ||||
| Perindopril/Amlodipine | 1 | 1 | Dizziness, headache and coughing | |
| 10 mg/5 mg | ||||
| Amlodipine/Valsartan | 1 | 1 | Headache, ankle edema, angioneurotic edema (occasional) | |
| 5 mg/80 mg | ||||
| Amlodipine/Telmisartan | 1 | 1 | Headache, ankle edema, angioneurotic edema (occasional) | |
| 5 mg/80 mg | ||||
| Amlodipine/Benazepril | 1 | 1 | Headache, ankle edema, angioneurotic edema (occasional) | |
| 5 mg/10 mg | ||||
| 2.5 mg/10 mg | 1 | 1 | Headache, ankle edema, angioneurotic edema (occasional) | |
| Amiloride/Hydrochlorothiazide | 1 | 1 | Abnormal serum potassium, hyperuricemia | |
| 2.5 mg/25 mg | ||||
| Nitrendipine/Atenolol | 1 | 1–2 | Headache, ankle edema, bronchospasm, bradycardia | |
| 10 mg/20 mg | ||||
| 5 mg/10 mg | 1–2 | 1–2 | ||
| Reserpine/Hydrochlorothiazide/Dihydralazine/Promethazine | 1–3 | 2–3 | Digestive ulceration and sleepiness | |
| 0.032 mg/3.1 mg/4.2 mg/2.1 mg | ||||
| Reserpine/Triamterene Hydrochlorothiazide/Dihydralazine | 1–2 | 1 | Digestive and headache | |
| 0.1 mg/12.5 mg/12.5 mg/12.5 mg | ||||
| Zhenjujiangya tablet | 1–3 | 2–3 | Hypotension and abnormal serum potassium | |
| Clonidipine 0.03 mg/Hydrochlorothiazide 5 mg | ||||
| Enalapril/Folic acid | 1–2 | 1–2 | Coughing, nausea, angioneurotic edema (occasional), headache, ankle edema, myalgia | |
| 10 mg/0.8 mg | ||||
| Amiloride/Atorvastatin | 1 | 1 | Transaminase elevation | |
| 5 mg/10 mg | ||||
| Candesartan/Hydrochlorothiazide | 1 | 1 | Upper respiratory tract infection, backache, abnormal serum potassium | |
| 16 mg/12.5 mg | ||||
For details on the usage of antihypertensive drugs, please refer to the relevant manual approved by China Food and Drug Administration.
Table 10. Strong indications for antihypertensive drugs commonly available.
| Indication | CCB | ACEI | ARB | diuretic | β-blockers |
| Left ventricular hypertrophy | + | + | + | ± | ± |
| Stable CAD | + | +a | +a | – | + |
| Post-myocardial infarction | –b | + | + | +c | + |
| Heart failure | –e | + | + | + | + |
| Prevention of atrial fibrillation | – | + | + | – | – |
| Cerebrovascular disease | + | + | + | + | ± |
| Carotid intima-media thickness | + | ± | ± | – | – |
| Proteinuria/Microproteinuria | – | + | + | – | – |
| Renal inadequacy | ± | + | + | +d | – |
| Elderly hypertension | + | + | + | + | ± |
| Diabetes | ± | + | + | ± | – |
| Dyslipidemia | ± | + | + | – | – |
aSecondary prevention of CHD; blong-acting CCB can be used to control hypertension in patients with a history of myocardial infarction; cspironolactone; dloop diuretics should be chosen when eGFR < 30 mL/min; eamlodipine and felodipine are also applicable. +: applicable; –: insufficient evidence or not applicable; ±: likely applicable. ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blockers; CCB: calcium channel blockers; eGFR: estimated glomerular filtration rate.
Table 11. Selection of principal anti-hypertensive drugs for clinical practice.
| Classes | Indications | Contraindications |
|
| Absolute | Relative | ||
| Dihydropyridines CCB | Elderly hypertension Peripheral vascular disease Isolated systolic hypertension Stable angina pectoris Carotid atherosclerosis Coronary atherosclerosis |
Tachydysrhythmia Heart failure |
|
| Non-dihydropyridines CCB | Angina pectoris Carotid atherosclerosis Supraventricular tachycardia |
A-V block (grade 2 or 3) Heart failure |
|
| ACEI | Heart failure Coronary heart disease Left ventricular hypertrophy Left ventricular dysfunction Prevention of atrial fibrillation Carotid atherosclerosis Non-diabetic nephropathy Diabetic nephropathy Proteinuria/Microproteinuria Metabolic syndrome |
Pregnancy Hyperkalemia Bilateral reno-arterial stenosis |
|
| ARB | Diabetic nephropathy Proteinuria/Microproteinuria Coronary heart disease Heart failure Left ventricular hypertrophy Prevention of atrial fibrillation ACE-inhibitor coughing Metabolic syndrome |
Pregnancy Hyperkalemia Bilateral reno-arterial stenosis |
|
| Diuretics (thiazides) | Heart failure Elderly Hypertension Old-aged Hypertension Isolated systolic hypertension |
Gout | Pregnancy |
| Diuretics (loop diuretics) | Renal insufficiency Heart failure |
||
| Diuretics (anti-aldosterone) | Heart failure Post-myocardial infarction |
Renal failure Hyperkalemia |
|
| β-blockers | Angina pectoris Post-myocardial infarction Tachydysrhythmia Chronic heart failure |
A-V block (grade 2 or 3) asthma |
COPD Peripheral vascular disease glucose intolerance Athletes |
| α-blockers | Prostatic hyperplasia Hyperlipidemia |
Orthostatic hypotension | Heart failure |
ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blockers; CCB: calcium channel blockers; COPD: chronic obstructive pulmonary disease.
(1) CCB: CCB mainly plays a role in dilating blood vessels and lowering BP by blocking calcium channel on vascular smooth muscle cells, which includes dihydropyridine CCB and non-dihydropyridine CCB. In previous large-scale clinical trials of antihypertensive therapy, dihydropyridine CCB was commonly used as the research agent, and it was confirmed that the antihypertensive treatment based on dihydropyridine CCB can significantly reduce the risk of stroke in hypertensives.[145]–[148] Dihydropyridine CCB can be combined with other four classes of drugs, especially suitable for patients with elderly hypertension, isolated systolic hypertension, stable angina pectoris, coronary or carotid atherosclerosis or peripheral vascular disease.[149] Common side effects include reflex sympathetic activation leading to rapid heartbeat, facial flushing, edema of the ankle, hyperplasia of the gums, and so on. Dihydropyridine CCB has no absolute contraindications, but patients with tachycardia and heart failure should be used with caution. Nifedipine is generally not recommended for patients with acute coronary syndrome, because it is a short-acting agent.
Non-dihydropyridine CCB commonly used in clinic is also applicable for antihypertensive therapy, the major side effects include inhibition of cardiac systolic function and conduction function, second to third degree atrioventricular block. Heart failure patients are forbidden to use it. Gingival hyperplasia induced by non-dihydropyridine CCB sometimes occurs. Therefore, doctors should detail patients' medical history and perform electrocardiogram before prescription, and the patients should be reviewed within two to six weeks after using it.
(2) ACEI: the mechanism of ACEI is to inhibit angiotensin-converting enzyme, block the production of renin angiotensin II and the degradation of kininase, so it can play a role in antihypertensive treatment.Various large-scale clinical trials conducted in hypertensive patients of the United States and Europe have demonstrated their good protection on target organ and preventive effects in cardiovascular end points.[68],[150],[151] ACEI has a definite antihypertensive effect and has no adverse effects on glycolipid metabolism. Salt restriction diet or combination with diuretic can increase its antihypertensive effect. ACEI is especially suitable for patients with chronic heart failure, cardiac insufficiency after myocardial infarction, prevention of atrial fibrillation, diabetic nephropathy, non-diabetic nephropathy, metabolic syndrome, proteinuria or microalbuminuria. The most commonly seen side effect is dry cough which often occurs in the early stage of medication. Patients with mild symptoms can keep taking the drug, while those who cannot tolerate should switch to ARB. Other side effects include hypotension, rash, occasional angioedema and dysgeusia. Long-term administration may lead to hyperkalemia; therefore, serum potassium and creatinine levels should be monitored regularly. Patients with bilateral renal artery stenosis, hyperkalemia, and pregnancy are the contraindication of ACEI.
(3) ARB: ARB plays its antihypertension role by the mechanism of blocking angiotensin II type 1 receptor. Kinds of large-scale clinical trials conducted in hypertensives of the United States and Europe have demonstrated that ARB can reduce the incidence of cardiovascular complications[152] and risk of cardiovascular events[153] in patients with a history of cardiovascular disease (such as CHD, stroke or peripheral arterial disease). ARB can also reduce the level of proteinuria and microalbuminuria in patients with diabetes or kidney disease.[113],[115] It is especially suitable for patients with left ventricular hypertrophy, heart failure, diabetic nephropathy, CHD, metabolic syndrome, microalbuminuria/proteinuria, or patients who cannot tolerate ACEI. There is also a prevention effect of atrial fibrillation in ARB.[154],[155] This class of drugs has less side effects and only occasionally observed diarrhea. Long-term administration may lead to hyperkalemia, so it should be paid attention to monitoring changes of serum potassium and creatinine. ARB is forbidden used by pregnant women and patients with bilateral renal artery stenosis or hyperkalemia.
(4) Diuretics: diuretics mainly exert their antihypertensive effect by urinating sodium and reducing the capacity load. The diuretics used to control BP are mainly thiazide diuretics, which are divided into thiazide diuretics and thiazide-like diuretics. The former includes hydrochlorothiazide, benzfluorothiazide, etc., while the latter includes chlorthalidone, indapamide and so on. The PATS[130] study confirmed that indapamide treatment can significantly reduce the risk of stroke recurrence. Low-dose thiazide diuretics (such as hydrochlorothiazide 6.25–25 mg) have little effect on metabolism, and can significantly increase antihypertensive effect of the latter agent when combined with other antihypertensive drugs (especially ACEI or ARB). This class of drugs is especially suitable for elderly hypertension, isolated systolic hypertension and heart failure. They are also one of the basic drugs for treating refractory hypertension.[156] The side effects of diuretics are closely related to the dosage, so small doses should generally be prescribed. Thiazide diuretics can lead to hypokalemia, long-term users should regularly monitor serum potassium, and supply potassium salt appropriately. Patients with gout are forbidden to use. Patients with hyperuricemia and obvious renal insufficiency should be used with caution. If the latter requires diuretics, loop diuretics such as furosemide are preferred.
Potassium-sparing diuretics such as amiloride, aldosterone receptor antagonists such as spironolactone, etc., are also applicable for the control of refractory hypertension. They do not increase potassium excretion while urinating sodium. When combined with other antihypertensive drugs with potassium-sparing effect such as ACEI or ARB, it should be aware of the risk of hyperkalemia. Long-term administration of spironolactone may lead to some side effects such as gynecomastia.
(5) β-blockers: β-blockers play a role in antihypertensive treatment mainly by inhibiting over-activated sympathetic nerve activity and myocardial contractility, plus heart rate slowing. Highly selective β1 blockers have a high affinity for β1 receptor, thus fewer side effects are induced by blocking the β2 receptor, which not only can reduce BP, but also can protect target organs and reduce the risk of cardiovascular events.[157],[158] β-blockers are especially suitable for patients with tachyarrhythmia, CHD, chronic heart failure,[159],[160] increased sympathetic activation, and high-dynamic hypertension. β-blockers' side effect commonly include fatigue, cold limbs, agitation, gastrointestinal upset, etc., and it may also affect glucose and lipid metabolism. Patients with second/third degree atrioventricular block and asthma are banned to use. Athletes and patients with chronic obstructive pulmonary disease, peripheral vascular disease or abnormal glucose tolerance should be used with caution. β-blockers are generally not preferred when glucose and lipid metabolism is abnormal, if necessary, highly selective β-blockers can also be used with caution. Long-term users of β-blockers can exhibit rebound phenomenon when suddenly withdrawal, which means the original symptom is worsen or new performance (such as BP rebound, headache, anxiety, etc.) is appeared. That is so called “withdrawal syndrome”.
(6) α-blockers: α-blockers are not the first choice for the antihypertension treatment, and are mainly used for patients with hypertension and benign prostatic hyperplasia. It is also suitable for the treatment of refractory hypertension.[161] Initial medication should be administered before bedtime in order to prevent postural hypotension. The sitting and standing BP should be monitored during the application and the controlled release formulation is preferred. Patients with postural hypotension are banned to use while those with heart failure can be used with caution.
(7) Renin inhibitors: the mechanism of renin inhibitors is a direct inhibition of renin, to reduce the production of angiotensin II, which can significantly reduce BP levels in hypertensive patients.[162]–[165] Other effects of renin inhibitors may also be helpful in reducing BP and protecting tissues, such as lowering plasma renin activity, blocking renin/renin receptors, and reducing production of intracellular angiotensin II. These drugs are well tolerated. Rash and diarrhea are their most common side effects.
5.4.4. Combination therapy of antihypertensive drugs
Combination therapy has become the basic method to treat hypertension.[166] In most cases, it requires two or more drugs to have BP controlled below the target BP.
(1) Indications for combination therapy: high-risk group of patients with BP ≥ 160/100 mmHg or 20/10 mmHg higher than that of the target BP often require two drugs for initial treatment. It is also feasible to initiate with small dose combination therapy if the patient's BP exceeds 140/90 mmHg. If the target BP is still not achieved, the dosage may be increased on the basis of the original medication, sometimes three or more than three drugs may be needed for antihypertension treatment. CHIEF study shows that initial combination therapy has a good antihypertensive effect on the middle-aged and elderly patients with moderate or high risk of cardiovascular disease in Chinese population, and significantly improves BP control rate.[120]
(2) Method of combination therapy: when the two drugs are combined, their antihypertensive mechanism should be complementary; meanwhile, they should have an additive antihypertensive effect and can offset or alleviate the side effects of each other. For example, the addition of a small dose of thiazide diuretic to the medication of ACEI or ARB can reach or exceed the antihypertensive effect which doubles the original ACEI or ARB did. Equally, the addition of dihydropyridine CCB has a similar effect of that.
(3) The regimen of combination therapy (Figure 3).
Figure 3. Flowchart for the choice of initial single versus combination antihypertensive therapy.
A: ACEI or ARB; B: β-blockers; C: dihydropyridines CCB; D: thiazide-type diuretics; F: fixed-dose combination drugs. *For those with BP ≥ 140/90 mmHg and at high risk, initial low-dose combination therapy can also be recommended; **Including dosage titration and sequential addition of other agents to achieve BP target. ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blockers; BP: blood pressure; CCB: calcium channel blockers.
a. ACEI/ARB+thiazide diuretic: ACEI and ARB can increase serum potassium slightly, and can antagonize side effects such as hypokalemia caused by long-term administration of thiazide diuretics. The combination of ACEI or ARB plus thiazide diuretics has a synergistic effect, which is beneficial to improve the antihypertensive effect.
b. Dihydropyridine CCB+ACEI/ARB: CCB has the function of directly dilating the arteries, while ACEI or ARB can dilate both the arteries and the veins, thus the combination of the two drugs has a synergistic antihypertensive effect. A common side effect that dihydropyridine CCB has is ankle edema, which can be alleviated or offset by ACEI or ARB. The CHIEF study showed that low-dose long-acting dihydropyridine CCB preparation plus ARB used in hypertensive patients newly diagnosed can significantly improve the control rate of BP.[122] In addition, ACEI or ARB can also partially block the adverse reactions induced by CCB to increase patients' reflex sympathetic tone and heart rate.
c. Dihydropyridine CCB+Thiazide diuretic: the FEVER study[40] has confirmed that combination therapy of dihydropyridine CCB plus thiazide diuretic can reduce the risk of stroke in hypertensive patients.
d. Dihydropyridine CCB+β-blockers: CCB has the effect of dilating blood vessels and slightly increasing heart rate, which can offset the vasoconstriction and reduction of heart rate induced by β-blockers. The combination of the two drugs can alleviate their side effects.
The combination therapy below is optimized and recommended in China: dihydropyridine CCB+ARB; dihydropyridine CCB+ACEI; ARB+thiazide diuretic; ACEI+ thiazide diuretic; dihydropyridine CCB+thiazide diuretic; dihydropyridine CCB+β-blockers.
The combination therapy below can be taken into consideration: thiazide diuretic+β-blockers; α-blockers+β-blockers; dihydropyridine CCB+potassium-sparing diuretics; Thiazide diuretic+Potassium-sparing diuretics.
The combination therapy below that is not regularly recommended but can be used with caution if necessary: ACEI+β-blockers; ARB+β-blockers; ACEI+ARB; centrally acting agents+β-blockers.
The combination of multiple drugs: combination therapy of three drugs, the medication based on the combination of two drugs above plus another antihypertensive drug. One of the most commonly used combination is dihydropyridine CCB+ACEI (or ARB) + thiazide diuretics. Combination therapy of four drugs: on the basis of combination three drugs above, the fourth drug (such as β-blockers, aldosterone receptor antagonists, triamterene, Clonidine or α-blockers, etc.) is added. This medication is mainly for patients with refractory hypertension.
(4) Single-pill combination (SPC): SPC is a group of agents commonly used for antihypertension treatment, usually composed of two or more antihypertensive drugs with different mechanism.[167] Compared with the freely combined use of various drugs, the advantage of it is convenient to use and may help improve curative effect patient compliance, which is the new trend of combination therapy. It should be paid attention to the contraindications or possible side effects of their corresponding components when SPC is administrated.
Traditional combination preparations in China, such as “Fu-fang-jiang-ya-pian (Composite hypotensor)”, “Fu-fang-li-xue-ping-an-ben-die-ding-pian”, “Zhen-ju-jiang-ya-yin” and so on, included reserpine, hydralazine, and hydrochlorothiazide as the main components wildly used at that time. These compound preparations are still wildly used in grass-root clinical practice, long-acting “Fu-fang-li-xue-ping-an-ben-die-ding-pian” is one of the representatives.
New single-pill combinations are generally composed of two drugs with different mechanisms. Most of them are taken orally once per day, which is convenient to use and can improve patient compliance. These agents available in China mainly include ACEI plus thiazide diuretics, ARB plus thiazide diuretics; dihydropyridine CCB plus ARB, dihydropyridine CCB plus ACEI, dihydropyridine CCB plus β-blockers, thiazide diuretics plus potassium-sparing diuretics and so on.
5.5. Advance in device-based hypertension treatment
Key point 5E
Renal denervation (RDN) is not recommended for the routine treatment of resistant hypertension outside of the framework of clinical trials until enough evidence regarding safety and efficacy of such therapy becomes available.
RDN is a novel BP-lowering technique. Although the result from SYMPLICITY HTN-3 study is negative, the technique should not be denied. The study raised many issues, such as screening criteria for appropriate patient, operating skill and improvement of RDN device, etc., which all should be considered in clinical research.[168] In recent years, novel RDN devices are emerging, which will be hopeful to achieve more effective renal denervation.[169] Interim data from two recent RCTs (SPYRAL HTN-OFF MED and SPYRAL HTN-ON MED) with a sham procedure control showed that renal denervation is effective and safe in lowing BP in patients with grade I –II hypertension.[170],[171] Further RCT studies are needed before RDN can be recommended for the routine treatment of hypertension outside of the framework of clinical trials.
Other device-based therapies for hypertension, such as carotid baroreceptor stimulation,[172] central iliac arteriovenous anastomosis,[173] carotid body ablation, deep brain stimulation and device-guided breathing exercise are all undergoing early stages of investigation, whose safety and efficacy are unclear. So far, we do not know which approach in them will be accepted in clinical practice in the future.
5.6. Treatment of associated risk factors
5.6.1. Lipid treatment
Key point 5F
Patients with hypertension and dyslipidemia should be actively treated with antihypertensive therapy and moderate lipid-lowering therapy based on changes in therapeutic lifestyle.
For patients with low and intermediate risk of atherothrombotic cardiovascular disease (ASCVD), when the blood lipid level cannot reach the target value after strict implementation of lifestyle intervention for six months, drug lipid-lowering therapy should be considered.
For patients with hypertension at risk of ASCVD, statin therapy should be initiated immediately. Moderate-strength statins (IA) can be used, if cholesterol-lowering drugs can be combined with when necessary.[173]
Hypertension and dyslipidemia are important risk factors for atherosclerotic cardiovascular and cerebrovascular diseases. Hypertension associated with dyslipidemia significantly increases the risk of cardiovascular events. The Guidelines for the Prevention and Treatment of Dyslipidemia in Chinese Adults (Revised 2016)[174] for the first time clarified that the ideal cholesterol level in the primary prevention population of Chinese ASCVD is LDL-C < 2.6 mmol/L (non-HDL-C < 3.4 mmol/L).
A large number of randomized controlled clinical trials (including China's completed CCSPS study[174]–[182]) have shown that statin lipid-lowering therapy can significantly reduce the risk of all-cause mortality and cardiovascular events in patients with hypertension and dyslipidemia. It suggests low-medium-strength statins are safe and effective for primary prevention in patients with hypertension and dyslipidemia. However, as a primary prevention strategy for cardiovascular events, not all hypertensive patients require statin therapy. Analysis of existing data shows that low- and medium-intensity statin therapy can significantly reduce cardiovascular risk in patients with intermediate or high-risk cardiovascular disease including hypertensive patient.[183],[184] The therapy is safe and tolerable.
Hypertensive patients should consider applying statins under the following conditions: hypertension with more than one metabolic risk factor or with target organ damage. Statins should be used as primary prevention for cardiovascular disease. Hypertension with clinical disease (including heart, brain, kidney, blood vessels, etc.) should use statins as secondary prevention. In patients with hypertension, statins can be used as primary prevention. Low-intensity statins can be used. If multiple risk factors are combined (≥ 3) or target organ damage is severe, moderate-intensity statins can be used. Hypertensive patients use statins as secondary prevention. They can choose a moderate-intensity statin for initial treatment and high-intensity statins or statins in combination with other lipid-lowering drugs (specific intestinal cholesterol absorption inhibitors) if necessary.
In patients with hypertension and dyslipidemia, lipid-lowering therapy is treated according to the Guidelines for Prevention and Treatment of Dyslipidemia in Chinese Adults (2016 Revision).
5.6.2. Antiplatelet therapy
Key point 5G
The role of anti-platelet therapy in secondary prevention of cardiovascular and cerebrovascular diseases has been confirmed by a large number of clinical trials, which can effectively reduce the risk of cardiovascular events by 19%–25%, including 1/3 of nonfatal myocardial infarction, 1/4 of nonfatal stroke, and 1/6 of fatal vascular events.[187],[188]
The following hypertensive patients should be actively treated with antiplatelet therapy: (1) patients of hypertension complicated with ASCVD should be treated with low-dose aspirin (ASA) (100 mg/day) for long-term secondary prevention;[185],[186] and (2) in the case of acute episodes of thrombosis, such as acute coronary syndrome, ischemic stroke, transient ischemia, or occlusive peripheral atherosclerosis, ASA should be used in combination with a P2Y12 receptor inhibitor according to relevant guidelines. P2Y12 receptor inhibitor includes clopidogrel and ticagrelor, usually administered in the acute phase at a loading dose (ASA: 300 mg, clopidogrel: 300–600 mg or ticagrelor 180 mg), ASA (100 mg/day) was combined with clopidogrel (75 mg/d) or ticagrelor 180 mg/day for 3 to 12 months, followed by low-dose ASA (100 mg/day) for long-term secondary prevention.
The benefits of antiplatelet therapy on primary prevention of cardiovascular and cerebrovascular diseases are mainly reflected in high-risk groups, such as hypertension with diabetes, hypertension with chronic kidney disease, people aged 50–69 years with high cardiovascular risk (10-year total cardiovascular risk ≥ 10% or hypertension with three or more risk factors), so primary prevention can be carried out with small dose ASA (75–150 mg/day).[189]–[192] Patients with ASA intolerance can take clopidogrel (75 mg/day) as a replacement. Long-term use of ASA in patients with hypertension should be noted:[193],[194] (1) it should be taken after BP well controlled (< 150/90 mmHg). ASA may increase the risk of cerebral hemorrhage in uncontrolled hypertensive patients. (2) Aspirin enteric-coated tablets are recommended on an empty stomach to reduce gastrointestinal reactions. (3) Among patients with high risk factor of gastrointestinal bleeding, such as digestive tract disease (ulcer disease and its complications), more than 65-years-old, taking corticosteroids, anticoagulants or non steroidal anti-inflammatory drugs, preventive measures should be taken, including screening and treatment of helicobacter pylori infection, the prophylactic use of proton pump inhibitors, and adopting the reasonable scheme of combination of antithrombotic drugs. (4) Patients with active gastric ulcer, severe liver disease, renal failure, hemorrhagic disease should taking ASA with caution or stopping taking. (5) Patients with severe gastrointestinal bleeding after taking ASA should stop taking, and treatment should be conducted according to the related path of hemorrhage, and proton pump inhibitor treatment should be added for mild cases.
5.6.3. Blood glucose control
Key point 5H
Target of blood glucose control: HbA1c < 7%; fasting blood glucose (FBG) 4.4–7.0 mmol/L; two hours postprandial blood glucose or high peak blood glucose < 10.0 mmol/L. Target of blood glucose control could be more relaxed for patients prone to hypoglycemia, with long course of disease, elder, with comorbidity or various complications.
It's common for hypertensive patients to have hyperglycemia, who are often combined with a variety of other metabolic cardiovascular risk factors, such as obesity, dyslipidemia, fatty liver, proteinuria, hyperuricemia, etc., which would promote and aggravate the pathogenesis and development of cardiovascular risk. Therefore, it requires comprehensive control of multiple factors including healthy lifestyles and drugs against various metabolic cardiovascular risks, to achieve blood glucose control.
Target of blood glucose control: HbA1c < 7%; FBG 4.4–7.0 mmol/L; two hours postprandial blood glucose or high peak blood glucose < 10.0 mmol/L. Target of blood glucose control could be more relaxed for patients prone to hypoglycemia, with long course of disease, elder, with comorbidity or various complications, which also applies to patients with type 1 diabetes mellitus complicated with kidney disease and fundus disease. The basic principle is no hypoglycemia or hyperglycemia occurrence.
The principle of dietary adjustment: control total calorie, and carbohydrates should account for 55% to 65% of total calories; protein should be no more than 15% of total calories. Try best to control the body weight within the normal range. Eat little and often with the total calories being the same.
Principles of exercise and activity: the exercise and activity should be moderate, regular and individualized. It is recommended to take skeletal muscle isotonic exercises, such as walking, swimming, etc., whereas heavy sports and heavy exercise should be restricted. Hours should be regular for patients receiving insulin therapy, for example, meals and exercise should be regular with a fixed quantity.
Main principles of drug treatment:[189],[195]
(1) For most patients with type 2 diabetes mellitus, metformin is preferred.
(2) Light-weight petients and patients whose blood sugar cannot be effectively controlled with metformin alone should switch to or add sulfonylurea or glinide-type hypoglycemic agent or dipeptidyl peptidase-4 inhibitor, α-glycoside enzyme inhibitor.
(3) The novel sodium-glucose cotransporter 2 (SGLT2) inhibitor or glucagon-like peptide-1 (GLP-1) receptor ago-nist, could reduce blood glucose effectively as well as re-duce SBP and weight slightly. It was shown in recent clini-cal trials that the SGLT2 drugs, empagliflozin and canagliflozin and the GLP-1 receptor agonist, liraglutide, can reduce cardiovascular mortality, and dapagliflozin can reduce the risk of cardiovascular death or hospitalization for heart failure.[196]–[198]
(4) If it is difficult to control blood glucose after two kinds of medium-dose hypoglycemic drugs have been used, hypoglycemic agents can be administrated orally during daytime, and intermediate-acting or super-long-acting insulin treatment can be injected before bedtime; if blood glucose is still not controlled effectively, multiple insulin injections can be adopted everyday.
(5) For new-onset diabetes with fasting blood glucose above 11 mmol/L or HbA1c over 9%, short-term intensive insulin therapy could be adopted so as to control blood glucose and preserve islet β-cell function as soon as possible.
(6) In the process of antihypertensive treatment, the effect of antihypertensive drugs on glycemic control should be taken into consideration. For instance, long-term application of thiazide diuretics with large doses could result in blood glucose elevating; β-recepter blockers may mask hypoglycemia responses including heart rate increase, etc..
For detailed guidance on diabetes prevention and treatment, or precautions for insulin application, see China Guidelines for Diabetes Prevention and Treatment (Edition 2017).[199]
5.6.4. Treatment of hypertension complicated with atrial fibrillation (AF)
Key point 5I
In hypertensive patients with risk of atrial fibrillation (such as left atrial enlargement, left ventricular hypertrophy or reduced cardiac function), it is recommended to use renin-angiotensin aldosterone system (RAS) inhibition drugs (especially ARB) to reduce the occurrence of atrial fibrillation (IIA, B).[200]
Patients with atrial fibrillation and risk factors for thromboembolism should be treated with anticoagulant therapy in accordance with the current guidelines (I, A).[201]
Hypertension is an important risk factor for atrial fibrillation.[202] In hypertensive patients with risk of atrial fibrillation, such as left atrial enlargement, left ventricular hypertrophy, or reduced cardiac function, It is recommended to use RAS inhibition drugs (especially ARB) to reduce the occurrence of atrial fibrillation.[200] A common important complication of hypertension and AF is stroke. Hypertension is one of the risk factors for stroke and systemic embolism in non-valvular AF patients. Uncontrolled hypertension is also a risk factor for bleeding in patients with atrial fibrillation. All hypertensive patients with non-valvular AF should be assessed for risk of thromboembolism based on CHADS2 or CHA2DS2-VASc scores and risk assessment of bleeding.
Anticoagulant therapy should be given in accordance with the current guidelines for patients with hypertension complicated with AF who have risk factors for thromboembolism.[201] Oral anticoagulant warfarin can be used under the guidance of the international standardized ratio (INR) to control the INR in 2.0–3.0. Because of the metabolic gene characteristics of warfarin metabolism in Chinese population, special consideration and attention should be given in the dose of initial or adjustment of warfarin treatment in order to ensure the efficacy and avoid bleeding side effect. The novel oral anticoagulants were compared with warfarin in clinical trials in patients with non-valvular AF with the results of non-inferior or superior efficacy in stroke and systemic embolism prevention with no more than or less bleeding complications than warfarin,[203]–[206] and all drugs significantly reduced intracranial hemorrhage. It is recommended to follow the recommendations in indication and contraindication in relevant guidelines to use and follow up appropriately. Rate or rhythm control should be given in patients with symptomatic atrial fibrillation in accordance with the current guidelines.[201]
It is recommended to use the average value of three BP measurements for the potential measurement error by the irregular rhythm in AF. If possible an electronic sphygmomanometer with the function of detecting atrial fibrillation can be used.
5.6.5. Management of hypertension with multiple risk factors
Key point 5J
Lifestyle intervention is the basis of cardiovascular disease prevention in hypertensive patients with multiple risk factors. It is suggested that hypertensive patients with elevated homocysteine level should be supplemented with fresh vegetables, fruits and folic acid (IIa, B),[41],[137] if necessary.
Lifestyle intervention is the basis of cardiovascular disease prevention in hypertensive patients with multiple risk factors. The management of hypertensive patients is an important approach for intervention of the multiple risk factors.
Studies showed that intervention of multiple risk factors with health education, lifestyle intervention and drug treatment may significantly improve the individual risk factor control[207]–[210] and risk factor aggregation status[211] of high-risk population of cardiovascular disease in community. Lifestyle interventions are detailed in 5.3. The fixed-proportion combination of antihypertensive drugs and other cardiovascular drugs includes dihydropyridine CCB+statin, etc. The use of such drugs should be based on the risk factors and concurrent clinical diseases of the patient, the indications and contraindications of antihypertensive drugs and non-antihypertensive drugs should be grasped.
Treatment of hypertension with elevation in homocysteine (HCY) level: nutrition intervention study in Lin County[137] and CSPPT study[41] suggest supplement of folic acid could reduce the risk of first stroke. Appropriate supplement of fresh vegetables and fruits is recommended in hypertensive patients with elevation of HCY level, and the supplement of folic acid should be conducted as necessary.
5.7. Follow-up, referral and medical record of anti-hypertensive therapy
5.7.1. Purpose of follow-up
The purpose of follow-up are to assess the treatment response, to investigate the patient's tolerance to the drug, to analyze whether or not the BP treat to target stably and the status of other risk factors, and to establish the good relationship of reciprocal trust between physician and patient.
5.7.2. Contents of follow-up
During the follow-up, office BP measurement and/or ambulatory BP monitoring are recommended, the numerical value of BP and the status of BP targeting are mastered and the adherence to drug therapy are inquired. According to the fluctuation of BP and the adverse effect of drug, the drug of hypertensive treatment will be modified. Order the patient to take medicine on time, direct the patient to improve the lifestyle and persistent long-term treatment, not to stop taking drugs at will.
5.7.3. Interval of follow-up
The interval of follow-up will be determined by total cardiovascular risk along with BP level. Patients with high–normal BP or grade 1 hypertension, with low- or moderate-risk, or taking only one kind of anti-hypertensive agent, should be visited for follow-up every two to three months. The interval of follow-up of patients with new-defined high-risk and complicated case should be shortened, and for high-risk patients whose BP not at goal or with clinical symptoms, a shorter interval (2–4 weeks) should be considered. The patient with targeting BP stably should be follow-up every month or a longer interval. The patient, whose BP could not reach the target after taking at least three kinds of anti-hypertensive agents, should be transferred to hypertensive specialist clinics for further diagnosis and treatment.
5.7.4. Medical record
Every follow-up should be recorded formally, the follow-up case should be created and community-based hospital should create patient's follow-up file. At every visit, the numerical values of BP and heart rate, together with the symptom related with BP, dosage, category and adverse effect of drugs, should be recorded in the follow-up case.
6. Treatment of hypertension for special populations
6.1. Hypertension in the elderly
Key point 6A
In the general population aged 65 to 79 years with BPs ≥ 150 mmHg systolic and 90 mm Hg diastolic, drug therapy is recommended (IA), and when BPs is ≥ 140 mmHg systolic and 90 mmHg diastolic, pharmacologic treatment should be considered (IIa, B); for the elderly ≥ 80 years of age with SBP ≥ 160 mmHg, initiate the pharmacologic treatment (IIa, B).[110],[212]
In the elderly population aged 65 to 79 years, initiate pharmacologic treatment to lower BP at SBP of 150 mmHg and DBP of 90 mmHg. If the treatment is well tolerated, BP can be lowered to < 140 mmHg systolic and 90 mmHg (IIa, B), and for the elderly ≥ 80 years of age, BP should be lowered to < 150 mmHg systolic and 90 mmHg (IIa, B).[213]
In 2012, the prevalence of hypertension among rural and urban population aged ≥ 60 years in China was 60.6% and 57.0%, respectively, and the awareness, treatment, and control rates of hypertension were 53.7%, 48.8% and 16.1%,[2] respectively. It is uniformly accepted that ≥ 65 years of age is defined as elderly hypertension, and when SBP is more than 140 mmHg, and DBP is less than 90 mmHg it is defined isolated systolic hypertension (ISH).
6.1.1. Clinical Features
(1) Increase of SBP and high pulse pressure: ISH is the most common type of elderly hypertension, accounting for 60%–80% of elderly hypertension,[214] and reaching to 80%–90% in elderly population aged 70 years and over.[215] Elevation in SBP increases the risk of stroke, CHD and end stage renal disease.
(2) BP fluctuation: number of hypertensive patients with postural BP variability and postprandial hypotension has been increasing, including orthostatic hypotension and supine hypertension. Fluctuation in BP affects treatment results and remarkably increases the risk of cardiovascular events.
(3) The incidence of abnormal circadian rhythm of BP is high: with high presence of nocturnal hypotension and hypertension as well as the high occurrence of morning hypertension.
(4) There is an increasing number of patients with white-coat hypertension and pseudohypertension.[216]
(5) It is generally accepted that hypertension commonly coexists with other chronic diseases such as CHD, heart failure, cerebrovascular disease, renal insufficiency and diabetes, etc. Such condition makes the treatment more difficult.
6.1.2. Lifestyle modification
For more information on lifestyle modification, please refer to 5.3 lifestyle intervention
6.1.3. Drug therapy for the elderly hypertension
(1) Research evidence: a meta-analysis showed that drug treatment could significantly reduce the risk of stroke, CHD and all-cause mortality.[217] HYVET study (≥ 80 years) showed a reduction in the rate of stroke 30%, all-cause 21%, heart failure 64% and cardiovascular events 34%, respectively.[70] The results of clinical trials in China have proved that elderly and even very elderly can benefit greatly from the antihypertensive drug treatment.[39],[70],[127]
(2) BP thresholds for initiating treatment: drug therapy should be instituted for the elderly aged 65 to 79 years with BPs ≥ 150 mmHg systolic and 90 mmHg diastolic, and drug therapy should be considered when BPs is ≥ 140 mmHg systolic and 90 mmHg diastolic; and it should be initiated when the elderly turn ≥ 80 years of age with SBP ≥ 160 mmHg.[110],[212]
(3) Thresholds and goals for BP treatment: the primary goal of hypertension treatment is to attain and maintain SBP treatment goals. The decision to lower BP targets and to set BP treatment goals should be on an individual basis after comprehensive assessment of comorbidities and frailty among the adult group. For the elderly aged 65 to 79 years of age, first step is to lower BP to < 150/90 mmHg, and the target BP should be maintained at < 140/90 mmHg if it is tolerated, and be lowered to < 150/90 mmHg for the elderly aged 80 years or over. If pharmacologic treatment results in SBP lower than130 mm Hg and is well tolerated, the treatment for hypertension should be maintained and does not need to be adjusted. When patients have > 75% bilateral carotid stenosis, central perfusion pressure is decreased, and intensive blood-pressure lowering may increase the risk of cerebral ischemia. Antihypertensive treatment should be based on the inhibition for the avoidance of cerebral ischemia symptoms. It is however, common to lose control of BP targets.[218] The BP of frail and elderly patients on medication to lower BP, should be regularly monitored. It is also advisable not to lower the BP excessively and at a high pace.
6.1.4. Drug application
Drug selection for optimal treatment of hypertension in the elderly: current recommended drugs to be considered as initial therapy or combination therapy for BP lowering are diuretics, calcium channel blockers (CCB), angiotensin-converting-enzyme inhibitors (ACEI), and angiotensin II receptor blocking (ARB),[69],[70],[219]–[223] which should be initiated at a low dose and be increased gradually up to the maximum dose. β-blockers are usually not the first choice for the elderly hypertensive patients without commodity disease. Diuretics may reduce glucose tolerance, induce hypokalemia, hypeluricemia and dyslipidemia. Therefore, they should be used in small doses. Alpha-adrenergic receptor antagonists (α-blockers) are drugs of second line (adjuvant drugs) which can be used for patients with benign prostatic hyperplasia or refractory hypertension. When given to the very elderly patients with postural BP variations, α-blockers should be used with caution and they may cause postural hypotension.
Drug therapy for elderly patients with isolated systolic hypertension (ISH): for patients with DBP < 60 mmHg, when SBP is < 150 mmHg, no medication is recommended. If SBP is 150–179 mmHg, small dose of antihypertensive drugs can be initiated, and when SBP is ≥ 180 mmHg, antihypertensive drugs should be used, but observation for adverse effects and altering BP is recommended.
6.2. Hypertension in children and adolescents
Key point 6B
Routine blood pressure measurement should begin at three years of age; appropriate cuff size is important for accurate blood pressure measurement, and most children aged ≥ 12 years can use adult cuffs;
The diagnosis of hypertension in children is based on blood pressure measurements on three occasions. Childhood hypertension is defined as SBP and/or DBP ≥ 95% on three occasions. A child can be diagnosed with hypertension when SBP and/or DBP reach stage 2 hypertension even one time;
Lifestyle interventions are recommended for all children with stage 1 hypertension. Medication treatment for stage 2 hypertension begins with low-dose single medication, and treatment regimen and course should be adjusted individually.
6.2.1. Clinical features and epidemiology of hypertension
6.2.1.1. Clinical features
Primary hypertension is more common among children and adolescents < 18 years (referred to as “children”). Children with primary hypertension often are asymptomatic with only slightly increased BP. Thus, diagnosis of childhood hypertension is difficult without regular BP measurement. The proportion of primary hypertension increases with age, and hypertension that occurs during puberty is mostly primary.[224],[225]
6.2.1.2. Epidemiology
Data from the Chinese National Surveys on Students' Constitution and Health in 2010 showed that the prevalence of hypertension among children was 14.5% (16.1% for boys versus 12.9% for girls).[226] Studies have shown that the prevalence after multiple separate occasions is around 4%–5%.[227],[228] A variety of risk factors for childhood primary hypertension has been identified. Obesity is the most important risk factor with approximately 30%–40% of children with primary hypertension being obese.[226] Other risk factors include parental hypertension history, low birth weight, premature birth, high salt intake, sleep insufficiency, and physical inactivity.
6.2.1.3. Secondary hypertension in children
Secondary hypertension in children is usually characterized by dramatical increase in BP but sometimes characterized by mild or moderate increase. Secondary hypertension usually has definite causes, including as kidney disease, renal artery stenosis, aortic coarctation, endocrine diseases, and drugs. Renal disease is the most common cause accounting for about 80% of secondary hypertension.[229]
6.2.2. Short- or long-term impacts of childhood hypertension
Early target-organ damages have occurred among approximately 30% to 40% of hypertensive children.[230]–[232] Abnormal left ventricular geometry is the most common target-organ damage, and other damages include increased vascular intima-media thickness, reduced arterial elasticity, reduced renal function, and fundus arteriosclerosis.[233]–[235]
Childhood hypertension can continue into adulthood, and about 40% of hypertensive children still have hypertension in adulthood without intervention[236],[237] Hypertensive children have significantly increased risks of cardiovascular and kidney diseases in adulthood.[238]–[241]
6.2.3. BP measurement and diagnostic evaluation in children
6.2.3.1. BP Measurement
The methods, operations and sphygmomanometer selection for childhood BP measurement are described in office BP section in this guideline (i.e., 3.5.1).
Selecting appropriate cuff size is important for accurate BP measurement in children. Table 12 shows commonly used cuff sizes and the corresponding upper arm circumference and age. In order to be consistent with method of BP measurement in the criteria, BP at the radial artery of right upper arm should be measured in routine examinations.[242],[243] For children having first BP measurement, all four limbs should be measured to exclude aortic stenosis and should be measured in different positions (sitting, lying, and standing) to detect orthostatic hypertension.
Table 12. Arm circumference and age for cuff size model.
| Cuff size model | Arm circumference, cm | Age group, yrs |
| XS | 12–18 | 3–5 |
| S | 18–22 | 6–11 |
| M | 22–32 | ≥ 12 |
| L | 32–42 | - |
| XL | 42–50 | - |
Childhood hypertension is identified based on three or more separate occasions with at least 2-week time intervals. Multiple BP measurements on the first instance can significantly reduce the rate of false positive and the burden of measurements on second occasion.[228] Three BP measurements on each occasion are recommended and the average value of the last two readings or the lowest value is recommended to be used for diagnosis. Children ≥ 3 years old should have their BP measured and physical development evaluated annually if possible.
6.2.3.2. Childhood hypertension criteria
Given the influence of height on BP in children, we established sex-, age- and height-specific BP reference standard for Chinese children aged 3 to 17 years old (referred to Supplement Tables) based on the 2010 standard.[243] Childhood hypertension can be categorized according to the age- and height-specific 50th, 90th, 95th, and 99th percentile values in boys and girls: hypertension is classified as having SBP and/or DBP ≥ 95th percentile; high-normal BP as having SBP and/or DBP 90th–95th percentile or ≥ 120/80 mmHg. The standard has been shown to have a good predictive value for adult subclinical cardiovascular damage,[244] and can be used for childhood hypertension diagnosis in the epidemiological and clinical settings.
In order to facilitate the clinician's rapid diagnosis of hypertension in children, it is recommended to use the simplified “Formula Standard” (Table 13) when making preliminary diagnosis. The consistency rates for diagnosing hypertension between “Formula Standard” and “Table Standard” is up to 95%, and childhood hypertension defined by “Formula Standard” performs well in predicting the risk of adult hypertension and subclinical cardiovascular target-organ damage.[245],[246] Children who have been diagnosed suspected hypertension by “Formula Standard” needs definite diagnosis by “Table Standard”.
Table 13. Simplified formula standard for screening hypertension in Chinese children and adolescents aged 3 to 17 years.
| Sex | SBP, mmHg | DBP, mmHg |
| Male | 100 + 2 × Age | 65 + Age |
| Female | 100 + 1.5 × Age | 65 + Age |
The unit of age is ‘years’. The formula is established based on 95th percentile values of BP from “Table Standard”, which can be used for rapid screen for childhood hypertension. DBP: diastolic blood pressure; SBP: systolic blood pressure.
6.2.3.3. Diagnostic evaluation
The process of diagnostic evaluation for primary hypertension in children includes:[224] (1) evaluating BP authenticity and classifying hypertension; (2) excluding secondary hypertension; (3) evaluating degree of target-organ damage; and (4) assessing comorbidities as diabetes. Clinicians can make treatment strategy based on above evaluation results.
Repeated BP measurements on three consecutive occasions with at least two week intervals are required to make individual hypertension diagnosis. Hypertension is diagnosed when SBP and/or DBP ≥ 95th percentile for sex, age, and height on all three occasions. Childhood hypertension can be categorized into two stages: stage 1 hypertension is defined as SBP and/or DBP ranging from 95th to 99th + 5 mmHg; stage 2 hypertension is defined as SBP and/or DBP ≥ 99th + 5 mmHg (Figure 4).[224],[225]
Figure 4. Flow chart for diagnostic evaluation of hypertension in children.
DBP: diastolic blood pressure; SBP: systolic blood pressure.
“White-coat hypertension” and “Orthostatic hypertension” in children are common and can be identified using ambulatory BP monitoring and head-up tilt table test, respectively.
6.2.4. Treatment
6.2.4.1. Target for BP treatment
The treatment goal for children with primary hypertension should be reduction of BP to below 95th percentile. For hypertensive children combined with kidney disease, diabetes or target-organ damage, BP should be reduced to below 90th percentile to reduce target-organ damage and long-term risk of cardiovascular disease.[224]
6.2.4.2. Etiology treatment
Etiology treatment is preferred for children with secondary hypertension.
6.2.4.3. Lifestyle intervention
Children with hypertension should improve their lifestyles initially and throughout the whole treatment process: (1) obese children should control their body weight, delay the rising trend of BMI and reduce body fat without damaging normal development; (2) increase aerobic and resistance exercise and reduce sedentary time; (3) improve the dietary patterns and diversity, and limit total and fat-sourced energy; control salt and sugar intake and develop healthy dietary habits according to WHO recommendations for children; (4) avoid persistent mental stress; and (5) ensure sufficient sleep. Most hypertensive children can acquire optimal BP after lifestyle interventions.[75],[247]–[250]
Hypertensive children should have BP monitored annually. For children with persistently high BP, ambulatory BP monitoring is recommended to identify white coat hypertension and obtain the circadian rhythm of BP.
6.2.4.4. Pharmacological therapy
Pharmacological therapy should be started in children who have stage 2 hypertension or hypertensive patients combined with one or more of the following conditions: (1) clinical symptoms; (2) diabetes; (3) secondary hypertension; and (4) target-organ damage.
Children should receive pharmacological therapy when failing to achieve target BP after lifestyle interventions for about six months and when developing stage 2 hypertension or clinical symptoms during the period of lifestyle interventions.
Pharmacologic therapy of childhood hypertension should be initiated using a low-dose and single drug and needs to be considered individually. The treatment strategy and course should be adjusted according to effect and BP levels, and combination therapy should be implemented if possible. See Practical Pediatrics for detailed operations.
At present, the China Food and Drug Administration (CFDA) has apporved limited antihypertensive drugs applied in children, as follows:
(1) ACEI: ACEI is one of the most commonly used antihypertensive drugs for children. Captopril is the only CFDA-approved ACEI drug.
(2) Diuretics: CFDA-approved diuretics include triamterene, chlorthalidone, hydrochlorothiazide, and furosemide.
(3) Dihydropyridine CCB: amlodipine is the only CFDA-approved dihydropyridine CCB.
(4) Adrenergic receptor blockers: CFDA-approved medications include propranolol, atenolol and prazosin.
(5) ARB: None ARB drug has been approved by CFDA.
Note: Refer to the package inserts or medication guides to confirm whether or not antihypertensive medicine is appropriate in children.
6.3. Hypertensive disorders in pregnancy
Key point 6C
For patients with hypertension in pregnancy, the threshold for the initiation of antihypertensive drug treatment is BP ≥ 150/100 mmHg. The target of treatment is 150/100 mmHg (IIb, C).[251],[252]
The drug treatment for hypertension can be withheld until BP ≥ 160/110 mmHg if the patient has no proteinuria or other target organ damage.[253]
In pregnant women with mild hypertension, non-pharmacologic intervention should be emphasized, with simultaneous monitoring of BP, proteinuria/target organ damage, and so on.
The prevalence of hypertensive disorders accounts for 5%–10% of pregnant women. Seventy percent of hypertensive disorders in pregnancy develop 20 weeks after gestation, while 30%, predate pregnancy.[254],[255] Hypertension in pregnancy is associated with increased risk of placental abruption, cerebral hemorrhage, disseminated intravascular coagulation, acute hepatic failure, acute renal failure, and intrauterine growth retardation. It is also an important factor associated with maternal and fetal mortality.
6.3.1. Classification of hypertensive disorders in pregnancy
Hypertensive disorders in pregnancy can be divided into four categories: gestational hypertension, preeclampsia/eclampsia, chronic hypertension and chronic hypertension with superimposed preeclampsia. Gestational hypertension develops after 20 weeks of gestation without any manifestations of target organ damage and recovers within the first 12 weeks after delivery. Chronic hypertension predates pregnancy or develops within the first 20 weeks of gestation, and/or persists after delivery. Preeclampsia is pregnant hypertension in association with proteinuria (≥ 300 mg/day) or established organ damage (heart, lung, liver or renal) but no proteinuria. Severe eclampsia is diagnosed as hypertension (≥ 160/110 mmHg) in association with clinical proteinuria and/or cerebral malfunction, blurred vision, pulmonary edema, renal failure, thrombocytopenia (platelet count < 100 × 109/L), hepatic failure, abnormal placental circulatory failure, etc.
6.3.2. Treatment strategy
The primary objective of antihypertensive treatment is to maintain maternal-fetal safety, support a smooth delivery and reduce perinatal mortality. The threshold for the initiation of antihypertensive drug treatment is BP ≥ 150/100 mmHg. The target of treatment is 150/100 mmHg.[251],[252] The drug treatment can be withheld until BP ≥ 160/110 mmHg if the patient has no proteinuria or other target organ damage.[253],[256] BP should not be lower than 130/80 mmHg, in order to avoid placental hypoperfusion.
6.3.3. Management of hypertension in pre-pregnancy women
It is highly recommended that women with chronic hypertension should be clinically evaluated before pregnancy to identify the cause of hypertension and the severity of BP elevation. The treatment includes non-pharmacological interventions, and antihypertensive drug treatment, if necessary. Some patients can have their BP reduced to less than 150/100 mmHg under non-pharmacological interventions to minimize the duration and intensity of drug treatment. Patients with uncontrolled BP (≥ 160/110 mmHg) need to be advised to avoid conception.
6.3.4. Non-pharmacologic treatment of hypertension in pregnancy
Non-pharmacological treatment of hypertension in Pregnancy includes salt restriction, regular exercise, emotional relaxing, weight controlling, adequate sleep, and so on. Salt intake can be reduced to about 6 g/day, while excessive salt restriction may lead to hypovolemia and placental hypoperfusion and should be avoided.[253]
6.3.5. The management of mild hypertension in pregnancy
Non-pharmacological treatment should be emphasized in uncomplicated mild hypertension, with BP, proteinuria, and blood cell counts closely monitored. In hypertensive patients treated with multi-drug or complicated by target organ damage, dosage and number of drugs used should be as less as possible.
Patients with mild hypertension complicated by preeclampsia, since the probability of developing eclampsia is only about 0.5%, routine use of magnesium sulfate is not recommended. However, maternal BP and proteinuria, state of the fetus need to be monitored carefully.[253]
6.3.6. The management of severe hypertension in pregnancy
The primary objective of the treatment is to reduce maternal-fetal morbidity and mortality. The persistence of treatment, the target of BP, drug selection, and the indication for pregnancy termination should be prespecified. In patients with severe eclampsia, intravenous magnesium sulfate should be administrated if no contraindication exists. Patients with very high BP (≥ 180/120 mmHg) should be treated as a hypertensive emergency.
6.3.7. Drug treatment of hypertension in pregnancy
The most commonly used oral antihypertensive drugs in pregnant women include labetalol, methyldopa, and nifedipine. Low dose thiazides can also be considered in necessary (Table 14). Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are contraindicated in pregnant as well as in pre-pregnancy hypertensive women.
Table 14. Commonly used oral antihypertensive drugs in pregnant women.
| Name | Mode of action | Dosage | Categories** | Side effects |
| Methyldopa | Decreasing sympathetic tone of the brain stem | 200–500 mg, 2–4 times/day | B | Depression, Extremely sedation, Hypotension |
| Labetalol | Blocking α- and β-receptors | 50–200 mg q12h, max. 600 mg/day | C | Fetal bradycardia, Pruritus |
| Nifedipine | Inhibiting calcium influx of arteriolar smooth muscle cells | 5–20 mg q8h or sustained release preparation 10–20 mg q12h or controlled release preparation 30–60 mg q.d. | C | Hypotension |
| Hydrochloro-thiazide* | Diuresis and natriuresis | 6.25–12.5 mg/day | B | Placenta bloodstream reduction with high dose diuretics |
*Diuretics should be avoided in patients with reduced placenta bloodstream (preeclampsia or fetal growth retardation). **Pregnancy Risk Categories: A, Adequate and well-controlled studies have failed to demonstrate a risk to the fetus in the first trimester of pregnancy; B, Animal reproduction studies have failed to demonstrate a risk to the fetus, and there are no adequate and well-controlled studies in pregnant women; C, Animal reproduction studies have shown an adverse effect on the fetus, and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks.
In patients with previous gestational hypertension, chronic renal disease, autoimmune diseases, diabetes, chronic hypertension, complicated by ≥ 1 risk factors of preeclampsia (uniparas, > 40 years old, BMI > 35, family history of preeclampsia, multifetation), low dose aspirin can be prescribed from the twelfth week of the gestation until one week before delivery.[257]
6.4. Hypertension with stroke
Key point 6D
For patients with stable stroke, antihypertensive therapy should be initiated if BP ≥ 140/90 mmHg, and the target of lowering BP is < 140/90 mmHg (IIa, B).
For patients with acute ischemic stroke, the BP should be controlled at < 180/110 mmHg if thrombolysis is planned.
Antihypertensive therapy for acute intracerebral hemorrhage: Aggressively intravenous antihypertensive agents are recommended if SBP > 220 mmHg. Intravenous antihypertensive agents are recommended if SBP > 180 mmHg. The reference goal for lowering BP is 160/90 mmHg (IIb, B).
6.4.1. BP management in stable stroke
Systematic analysis showed that antihypertensive agents significantly reduced the risk of stroke recurrence by 22%.[131] For stable stroke patients, the goal for lowering BP should be < 140/90 mmHg. For patients with stroke or TIA attributable to intracranial atherosclerotic stenosis (stenosis degrees 70%–99%) the recommended BP would be < 140/90 mmHg. For stroke or TIA patients due to hemodynamic reasons, the speed of lowering BP and the range to be maintained should be based on the tolerance and hemodynamics conditions of each patient. Selection of the type and dosage of antihypertensive drugs and BP targets should be individualized after fully considering these three factors: drugs, characteristics of stroke and patient conditions.
6.4.2. Antihypertensive therapy for acute intracerebral hemorrhage
For patients with acute ischemic stroke, the BP should be controlled at < 180/110 mmHg if thrombolysis is planned. Patients with elevated BP within 24 h after ischemic stroke should be carefully treated. Anxiety, pain, nausea, vomiting, and elevated intracranial pressure should be treated in priority. For patients with continuous elevation of BP, SBP ≥ 200 mmHg or DBP ≥ 110 mmHg, or with severe cardiac insufficiency, aortic dissection or hypertensive encephalopathy, antihypertensive agents should be given. Intravenous agents, such as Lorol or Nicardia, could be administered, as well as agents of lowering BP rapidly should be avoided.
Antihypertensive therapy for acute intracerebral hemorrhage: the BP of patients should be evaluated comprehensively and the causes of BP escalation should be investigated. Antihypertensive therapy for acute intracerebral hemorrhage: aggressively intravenous antihypertensive agents are recommended if SBP > 220 mmHg. Intravenous antihypertensive agents are recommended if SBP > 180 mmHg. The reference goal for lowering BP is 160/90 mmHg. Early aggressive antihypertension is safe, but the effectiveness of improving prognosis needs to be further investigated. The BP should be closely monitored during antihypertension therapy. BP should be monitored every 15 min.
6.5. Hypertension with coronary artery disease (CAD)
Key point 6E
In patients with CAD, it is recommended: the target BP is to < 140/90 mmHg (I, A), if tolerated, the target BP is to < 130/80 mmHg (IIa, B).[38], [68] It should be noted that DBP should not be too low (IIb, C).[258]–[263]
In patients with stable angina pectoris, beta-blocker or CCB should be recommended first (I, A).
6.5.1. Target BP
In patients with CAD, the target BP is to < 140/90 mmHg, if tolerated, the target BP is to < 130/80 mmHg.[38],[68] It should be noted that DBP should not be lower than 60 mmHg.[254] In elderly patients or patients with severe coronary stenosis, BP should not be too low.
6.5.2. Selection of antihypertensive drugs for patients with stable angina pectoris
The β-blocker and CCB can reduce myocardial oxygen consumption and angina pectoris attack, so they should be the first choice. If BP control is not ideal, ACEI/ARB and diuretics can be used together.
6.5.3. Selection of antihypertensive drugs for patients with non-ST-segment elevation acute coronary syndrome
The β-blocker and CCB are still the first choice for patients with worsening exertional angina pectoris. If BP control is not ideal, RAS blocker and diuretic can be used together. In addition, when considering the existence of vasospasm factors, large doses of beta-blocker should be avoided as it may induce coronary spasm.
6.5.4. Selection of antihypertensive drugs for patients with acute ST-segment elevation myocardial infarction
Long-term use of β-blocker and RAS blocker can significantly improve the prognosis of patients with myocardial infarction as secondary prevention. They should be used early and without contraindications. CCB and diuretic can be used in combination when BP control is not ideal.
6.6. Hypertension with heart failure
Key point 6F
For patients with both hypertension and heart failure the recommended BP goal is < 130/80 mmHg (I, C).
For patients with heart failure and reduced ejection fraction (HFrEF) the antihypertensives of choice are ACEIs (or an ARB for patients intolerant to ACEIs), β-receptor blockers and aldosterone receptor blockers (I, A).
6.6.1. Epidemiology and mechanism
In China, the incidence of hypertension among heart failure patients is 54.6%.[258] The incidence of heart failure in patients with hypertension is 28.9%, stroke (30.0%). Chronic and continuous hypertension eventually leads to heart failure with preserved ejection fraction or heart failure with reduced ejection fraction.[259]
6.6.2. Clinical benefits of antihypertensive therapy
A review of large scale meta-analysis suggests a 10 mmHg reduction in SBP can reduce the incidence of heart failure by 28%.[260] Recent studies among hypertensive patients show that compared to standard BP management (SBP < 140 mmHg), an aggressive BP management strategy (SBP < 120 mmHg) can reduce the incidence of heart failure by 38%, and stroke by 43%.[38]
6.6.3. Antihypertensive goals
The recommended target BP is < 130/80 mmHg, this recommendation is supported by randomized controlled studies. For patients with hypertension and left ventricular hypertrophy, but without heart failure, the BP may be lowered to < 140/90 mmHg,. A target of < 130/80 mmHg has the added advantage of preventing heart failure, in patients with high tolerance levels.
6.6.4. The management of hypertension with chronic heart failure
Hypertension with chronic HFrEF: The drug of choice is ACEI (or ARB in intolerant patients), β-receptor blockers and aldosterone receptor blockers. The concomitant use of these three classes of drugs also forms the basis of the treatment of HFrEF, and can reduce mortality and improve the prognosis, aside from having excellent antihypertensive efficacy. Most of these heart failure patients need to regularly use loop diuretics and thiazide diuretics, which also have good antihypertensive activity. If the above cannot effectively control BP, the use of amlodipine and felodipine are recommended.
Hypertension with HFpEF: the pathogenesis most often involves hypertension, hypertension may be present even after the appearance of symptoms of heart failure. The three drugs mentioned above cannot reduce the mortality and improve the prognosis of these patients. However, these drugs are safe and still recommended for their antihypertensive effect. If the BP still cannot be controlled, the administration of amlodipine or felodipine is recommended. The use of αblockers, centrally acting antihypertensive agents (such as moxonidine) are not recommended. Negatively chronotropic CCBs such as diltiazem and verapamil cannot be used in HFrEF, however can be safely used in HFpEF patients.
6.6.5. Management of hypertensive with acute heart failure
The clinical characteristics include hypertension, primarily left heart failure, rapid progressive, and most often HFpEF. BP needs to be controlled while concomitantly controlling heart failure, primarily by the administration of intravenous diuretics and vasodilators, including nitroglycerin, sodium nitroprussideand urapidil. When mild, BP can be gradually reduced over 24–48 h.When severe with concomitant acute pulmonary edema the reduction in BP should not exceed 25% of baseline in the initial one hour, and may be further reduced to 160/100–110 mmHg in the proceeding 2–6 h, and gradually reduced to normal in 24–48 h.[261],[262]
6.7. Hypertension in chronic kidney disease (CKD)
Key point 6G
We recommend that in CKD and urine albumin excretion < 30 mg/24 h (or equivalence), the goal of treatment with anti hypertension drugs is < 140/90 mmHg (I, A), with albuminuria ≥ 30 mg/24 h (or equivalence) the goal is < 130/80 mmHg (IIA, B).
We suggest 18–60 years old of hypertension in patients with CKD in ≥ 140/90 mmHg should be evaluated and initiate anti-hypertensive drug treatment (I, A)
The initial antihypertensive therapy for hypertension in CKD patients should include one ACEI (IIa) or ARB (IIb) alone or in combination with other antihypertensive drugs, but the combination of ACEI and ARB is not recommended (A).[263],[264]
6.7.1. The relationship between hypertension and CKD
Hypertension and kidney disease are closely related to each other as etiology and aggravating factors. Hypertension caused by various CKD, which is called renal hypertension, is mainly divided into renal vascular hypertension and renal parenchyma hypertension. The prevalence of hypertension in non-dialysis CKD patients in China is 67.3%–71.2%.[265],[266] while the prevalence of hypertension in dialysis patients is as high as 91.7%.[267]
6.7.2. The goal of lowering BP in CKD patients
Drug antihypertensive therapy was initiated in patients with CKD complicated with hypertension when SBP ≥ 140 mmHg or DBP ≥ 90 mmHg. The target of antihypertensive therapy is < 140/90 mmHg when urine albumin excretion < 30mg/24 h (or equivalence), and < 130/80 mmHg when albuminuria ≥ 30 mg/24 h (or equivalence). The antihypertensive target can be appropriately relaxed for patients over 60 years old.
Proteinuria is a risk factor for renal dysfunction and CVD disease and CVD death in CKD patients. This guideline recommends a more stringent target of 130/80 mmHg BP reduction for patients with proteinuria.
6.7.3. Principles of antihypertensive drugs in CKD patients
ACEI/ARB, CCB, α-receptor blocker, β-blockers, and diuretics can all be used as initial drug choices.
ACEI/ARB not only has antihypertensive effect, but also can reduce proteinuria, delay the decline of renal function, and improve the renal prognosis of CKD patients.[263],[264] Initial antihypertensive therapy should include an ACEI or ARB, either alone or in combination with other antihypertensive drugs, the combination of the two drugs is not recommended. ACEI/ARB can be used cautiously even if the serum creatinine increased is less than 30% of basic value, and the dosage reduction or withdrawal can be considered if the serum creatinine increased-exceeds 30% of basic value.
Dihydropyridine and non-dihydropyridine long-acting CCB can be used in the treatment of hypertension in CKD and its renal protection ability mainly depends on its antihypertensive effect.
Thiazide diuretics were effective in patients with GFR > 30 mL/min per 1.73 m2) (CKD stage 1–3), patients with GFR < 30 mL/min per 1.73 m2) (stage 4–5 CKD) can use loop diuretics. Diuretics should be given in low dose, excessive diuresis can lead to insufficient blood volume, hypotension, or a decrease in GFR. The combination of aldosterone antagonists with ACEI or ARB may accelerate the risk of renal function deterioration and hyperkalemia.[268]
β-blockers can play a hypotensive role against the excessive activation of the sympathetic nervous system, and alpha beta blockers have a better advantage to play a cardio-renal protective role and can be applied to the hypotensive treatment of patients with CKD at different stages.
Other antihypertensive drugs, such as α-receptor blocker and central alpha receptor agonists, may be used in combination with other antihypertensive drugs as appropriate.
6.7.4. Antihypertensive therapy in dialysis patients with end-stage renal diseases (stage 5 CKD)
Resistant hypertension in CKD5D is an important clinical issue and the blood control needs a combination of more than three antihypertensive medications in most cases. The serum, potassium and creatinine levels should be monitored when receiving RAAS blockers in dialysis patients. Antihypertensive drugs should be avoided at the stage of rapid decrease of dialysis blood volume to avoid severe hypotension. The dosage of antihypertensive drugs should be adjusted to take into account the hemodynamic changes and the clearance of drugs by dialysis. BP measured before dialysis or in the clinic cannot reflect the average BP of dialysis patients very well, so it is recommended to measure the BP of patients at home. BP variation in dialysis patients should not be too large. The ideal target of blood post dialysis is 120–140 mmHg.[269]
6.8. Concomitant hypertension and diabetes mellitus
Key point 6H
The recommended target BP in patients with diabetes mellitus is less than 130/80 mmHg (II a, B).
Nonpharmacologic methods lasting less than three months can be instituted in diabetic patients with systolic BP 130–139 mmHg or diastolic BP 80–89 mmHg. If the target BP cannot be achieved by rational nonpharmacologic methods, antihypertensive medication is indicated.
Patients with confirmed BP ≥ 140/90 mmHg should, in addition to lifestyle therapy, have prompt initiation of pharmacologic therapy to achieve BP targets. In patients also present with established microalbuminuria, pharmacologic therapy should be started directly (I, A).
Initial choices of medication include ACEI or ARB therapy. When combination therapy is needed, ACEI or ARB is recommended to remain as one of the antihypertensive agents (I, A).
Diabetes mellitus and hypertension often coexist. In Chinese patients with hypertension followed up in out-patient clinic, 24.3% of them also suffered from diabetes.[270] Patients with both diabetes and hypertension are at increased risk for cardio-cerebrovascular morbidity. Studies have showed that antihypertensive therapy significantly reduced the rates of all-cause mortality, cardio-cerebrovascular morbidity, and some other adverse clinical outcomes.[271],[272]
6.8.1. The BP target level for patients with diabetes
Analysis of the previous studies showed that every 10 mmHg reduction in systolic BP is associated with a 12% reduction in the risk of any diabetes-related complications, and a 15% reduction in the risk of death. Studies also suggested that the lowest incidence of major cardiovascular events occurred at a mean achieved DBP of 82.6 mmHg.[273],[274] Currently, the recommended target BP level is 130/80 mmHg for patients with diabetes. For elder diabetic patients and those with severe cardiovascular diseases, BP should be reduced gradually to a slightly higher target of 140/90 mmHg.
6.8.2. The choice and application of antihypertensive agents in patients with diabetes
Nonpharmacologic methods, lasting less than three months, can be instituted in diabetic patients with systolic BP 130–139 mmHg or diastolic BP 80–89 mmHg. If the target BP cannot be achieved by rational nonpharmacologic methods, antihypertensive medication is indicated. Patients with confirmed BP ≥ 140/90 mmHg should, in addition involve themselves in lifestyle therapy and have prompt initiation of pharmacologic therapy to achieve BP targets. In patients, also present with established microalbuminuria, pharmacological treatment should be started directly. Initial choices of antihypertensive agents include ACEI or ARB therapy.[113]–[115] When combination therapy is needed, diuretics or CCB can be added on ACEI or ARB therapy. For those patients with angina, β-blockers are recommended. Diuretics should be used with caution in diabetic patients with coexisting hyperuricemia. β-blockers should be used with caution in those who are prone to recurrent hypoglycemia, since patients' symptoms of hypoglycemia can be masked by β-blockers. Diuretics and β-blockers should be started in low dosage if prescribed. In patients with BP which cannot be controlled satisfactorily or with prostate hypertrophy, α-blockers might be considered. In general, multiple-drug therapy is often required to achieve BP targets.
6.9. Metabolic syndrome
The prevalence of metabolic syndrome in Chinese adults has increased from 13.8% in 2002 to 18.2% in 2009.[273] The prevalence increases with aging and peaks at 60 to 69 years.[275]
6.9.1. Diagnosis
Metabolic syndrome can be diagnosed with at least three of the following: (1) abdominal obesity, waist circumference 90 cm in male and 85 cm in female or greater; (2) elevated BP: BP 130/85 mmHg or greater, or diagnosed as hypertension and treated; (3) dyslipidemia: fasting triglycerides 1.7 mmol/L (150 mg/dL) or greater, or HDL-cholesterol < 1.04 mmol/L (40 mg/dL), or diagnosed with dyslipidemia and treated; and (4) hyperglycemia: fasting glucose 6.1 mmol/L (100 mg/dL) or greater, or postprandial glucose 2 h after sugar loading 7.8 mmol/L (100 mg/dL) or greater, or diagnosed with diabetes and treated.
Among the components of the metabolic syndrome, hypertension has the highest incidence of 65.4%, followed by dyslipidemia (53.6% in male with hypertriglyceridemia, 49.4% in female with decreased HDL, respectively).[275],[276]
6.9.2. Cardiovascular risks
Chinese population studies showed that patients with metabolic syndrome had a 1.85-fold increased risk of 10-year cardiovascular events compared with non-metabolic syndrome patients, and the risk of ischemic and hemorrhagic stroke increased by 2.41 and 1.63 times, respectively. Among the combinations of metabolic syndrome components, abdominal obesity accompanied by hypertension and low HDL-C had the highest cardiovascular risk (increased by 5.25 times), and the risk is further increased by 16.58 times if hyperglycemia is added in.[189],[275]–[277]
6.9.3. Management
Early and comprehensive intervention is crucial in reducing cardiovascular risk and prevents target organ damages for patients with metabolic syndrome.
Treatment lifestyle changes such as healthy diet and regular exercise, are fundamental and effective for metabolic syndrome management. Chinese community studies showed that exercise reduced the risk of metabolic syndrome by 10% to 20%.[278]
ACEI and ARB are recommended as the first-line anti-hypertensive drugs, especially for patients with diabetes or obesity. Dihydropyridine CCB is also the alternative. Thiazide diuretics and beta-blockers can be used in patients with cardiac dysfunction or CHD.
6.10. Antihypertensive treatment for peripheral arterial disease (PAD)
Key point 6I
The BP of the patients with lower extremity arterial disease with hypertension should be controlled at < 140/90 mmHg.
CCB, ACEI or ARB should be adopted first. The application of selective β1 receptor blockers treating PAD can be considered in condition. Generally, diuretics are not recommended.
PAD is a common manifestation of systemic atherosclerosis. It was shown via epidemiological investigation abroad that the prevalence rate of the same is 3%–10% in the general population, and 15%–20% in the seniors over 70 years old.[279],[280] It is 2%–4% in the general population in China, which is as high as 16.4% in the population over 60 years old. It is even higher in patients with risk factors, such as hypertension, diabetes and metabolic syndrome.[281] Approximately half of PAD patients are suffering from hypertension, which also increases the risk of cardiovascular diseases and even death.[282]
BP of the patients with lower extremity arterial disease with hypertension should be controlled at < 140/90 mmHg. The BP targeting not only reduces the incidence of cardiovascular and cerebrovascular events in these patients, but also slows down the progression of the lesion, as well as reduces the amputation rate of the patients.[283],[284] The blood flow of the affected limb may reduce during the BP control process, which could be tolerated by most patients.
Drug selection: CCB and RAS inhibitors including ACEI or ARB can improve the endothelial function of the affected blood vessels while reducing BP.[283],[285] Generally, selective β1 receptor blockers can be considered in condition, for they are effective for treating PAD with hypertension, and do not increase the resistance of the affected blood vessels, which has a certain preventive effect on CHD events. Generally, diuretics are not recommended due to their reduction of blood volume and increase of blood viscosity.
6.11. Refractory hypertension
Key point 6J
Out-of-office BP measurements are often used to determine whether patients are refractory hypertension.
It is necessary to find out the causes of poor BP control and the coexisting disease factors.
Conventional dosage of RAS inhibitor + CCB + thiazide diuretics is recommended, and the dosage of each drug should be increased according to patient's characteristics and tolerance and should reach the full dose.
6.11.1. Definition and cause screening of refractory hypertension
On the basis of improved lifestyle when the application of the three reasonable and tolerable dose of antihypertensive drugs including thiazide diuretics at least four weeks after treatment, the inadequate control of BP is confirmed by the office and out-of-office (including home BP or ambulatory BP monitoring), or at least four drugs are needed to achieve the BP standard, called refractory hypertension. The prevalence of refractory hypertension is unknown, and there is no exact epidemiological data in China.
To determine whether a patient has refractory hypertension, out-of-office BP measurements (home BP measurements and dynamic BP monitoring) are usually required to exclude the effects of White-coat phenomenon and pseudo-resistant hypertension.
Look for causes that affect poor BP control and coexisting disease factors: (1) the more common reason is that patients have poor treatment compliance (failure to adhere to medication). (2) Improper selection and use of antihypertensive drugs (unreasonable drug combination and insufficient drug dose). (3) The substances antagonizing hypertension drugs were used, including oral contraceptives, cyclosporine, erythropoietin, glucocorticoids, non-steroidal anti-inflammatory drugs, antidepressants, cocaine and some traditional chinese medicines (such as licorice, ephedra). (4) Other influencing factors are: unhealthy lifestyle, obesity, volume overload (inadequate diuretic treatment, excess salt intake, progressive renal insufficiency); or some coexisting diseases, such as diabetes, dyslipidemia, chronic pain, long-term insomnia, anxiety, etc. Patients may have more than one cause that can be corrected or difficult to correct. (5) After eliminating the above factors, we should be alert to the possibility of secondary hypertension and start the screening of secondary hypertension.
6.11.2. Therapeutic principles of refractory hypertension[287]–[290]
(1) It is recommended that the patient should refer to a hypertensive specialist. The diagnosis of refractory hypertension should be made by a qualified hypertension specialist.
(2) Advocate out-of-office BP measurements (home BP and ambulatory BP) and effective communication with patients. Pay attention to patient compliance with long-term medication.
(3) Nearly possible elimination of influencing factors. They are mainly obesity, metabolic disorders, excessive sodium intake and other unhealthy habits.
(4) Adjust the antihypertensive treatment combined scheme. First, check whether the composition of the multi-drug combination scheme is reasonable. It is recommended to choose the conventional dose of RAS inhibitor+CCB+thiazide diuretics. The dosage of each drug should be increased according to patient's characteristics and tolerance, and the total dose should be reached.
(5) The fourth antihypertensive drug can be added according to the characteristics of patients with unsatisfactory results. The choice can be made between aldosterone receptor antagonists, beta receptor blockers, alpha receptor blockers or sympathetic nerve inhibitors (clonidine), but the principle of individualized therapy is still required.
6.11.3. Device-based hypertension treatment
Details can be found in 5.5. Advances in Device Intervention.
6.12. Hypertensive emergencies and hypertensive urgencies
Key point 6K
Treatment of hypertensive emergencies: The target of BP reduction in the initial phase (within 1 h) is to reduce MAP by no more than 25% of the untreated level. Reduce BP to a safer level in the next 2 to 6 h, typically around 160/100 mmHg. Reduce BP to normal levels gradually in the next 24 to 48 h if such BP levels can be tolerated.
Treatment of hypertensive urgencies: Slowly reduce BP to 160/100 mmHg in 24 to 48 h. There is no evidence that acute BP lowering management will improve prognosis. The BP reduction of many patients with hypertension urgencies can be achieved with oral medication.
6.12.1. Definition and evaluation
Hypertensive emergencies are situations in which the BP suddenly and severely increases (generally over 180/120 mmHg) in patients with primary or secondary hypertension, with progressive target organ damage such as the heart, brain, and kidney. Including hypertensive encephalopathy, hypertensive intracranial hemorrhage (cerebral hemorrhage and subarachnoid hemorrhage), cerebral infarction, heart failure, acute coronary syndrome (unstable angina, acute myocardial infarction), aortic dissection, pheochromocytoma crisis, using drugs such as amphetamine, cocaine, hallucinogen, etc., perioperative hypertension, pre-eclampsia or eclampsia, etc.[110],[291]
It should be noted that the level of BP is not directly proportional to the extent of acute target organ damage. Some hypertensive emergencies are not accompanied by severe increased BP level, such as acute pulmonary edema, aortic dissection, myocardial infarction, etc., while BP is just moderately elevated, but they should also be considered as hypertension emergencies as this kind of situations have a significant impact on target organ function
The term ‘hypertensive urgencies’ is used to describe patients with severe hypertension in whom there is no acute target organ damage. Symptoms such as headache, chest tightness, nosebleeds, irritability, etc. caused by severe elevated BP level may be associated with these patients. Most patients' medication compliance may be poor and have inadequate treatments.
The only criterion to distinguish between hypertensive emergencies and hypertensive urgencies is not the degree of elevated BP level, it is that whether there is occurring a new acute progressive target organ damage. Patients with suspected hypertensive emergencies should be thoroughly evaluated to determine if they are hypertensive emergencies while the initial treatment can not be delayed due to the overall evaluation process.
6.12.2. Treatment of hypertensive emergencies[110], [292]
(1) Therapeutic principles: blood pressure and vital signs should be continuously monitored; the causes and incentives of elevated BP should be eliminated or corrected promptly; the fear can be removed by appropriate usage of effective sedatives; the intravenous antihypertensive drugs should be administrated as soon as possible to control blood pressure in order to prevent further damage to target organs, and the damaged ones can be treated accordingly; and finally, complications should be reduced to improve outcomes.
(2) Choice of treatment drugs: the choice of treatment drugs should be based on the conditions of target organ involved and the patients' hepatorenal functions. The ideal drug should be able to predict the strength and speed of antihypertension, preserve target organ function, and adjust conveniently. The commonly used drugs for hypertensive emergencies are shown in Table 15. When the blood pressure tends to level off through initial intravenous administration, oral medication can be started and the intravenous drug should be gradually reduced until it can be stopped.
Table 15. Intravenous or intramuscular anti-hypertensive drugs for hypertensive emergencies.
| Drug name | Dosage | Onset time | Duration | Side effects |
| Nitroprusside | The intravenous infusion dose stars from 6.25–12.5 µg/min and adjusts it according to blood pressure (perioperative hypertension). 0.25–10 µg/kg per minute, IV (hypertension emergencies) Initial dose: 0.3–0.5 g/kg per minute. The dose can be gradually increased according to the blood pressure response; the maximum dose is 10 g/kg per minute (pregnancy-induced hypertension; safety level: C). |
Immediately | 2–10 min | Hypotension, tachycardia, headache, muscle spasms. Continuous use for more than 48 to 72 h or administration doses > 2 g/kg per minute may induce cyanide poisoning. |
| Nitroglycerine | 5–100 µg/min, IV (hypertensive emergency with myocardial ischemia). | 2–5 min | 5–10 min | Headache and vomiting. |
| Phentolamine | 2.5–5 mg, IV (used to diagnose pheochromocytoma and to treat hypertensive episodes caused by it, including hypertension occurred during surgical resection, and can also be used to assist in the diagnosis of pheochromocytoma based on the BP response to it). | 1–2 min | 10–30 min | Tachycardia, headache and flushing. |
| Nicardipine | 0.5–10 µg/kg per minute, IV, (perioperative hypertension, hypertension emergencies). The initial dose is 5 mg/h, and is gradually increased to 15 mg/h according to blood pressure response (pregnancy-induced hypertension, safety level C). |
5–10 min | 1–4 h | Tachycardia, headache, peripheral edema, angina pectoris, nausea, dizziness, inhibition of uterine contraction (combined with magnesium sulfate). |
| Esmolol | 0.15–0.3 mg/kg per minute, IVI (perioperative hypertension). 250–500 µg/kg, IV Followed by 50–300 µg/kg per minute, IV, (hypertension emergencies). |
1–2 min | 10–20 min | Hypotension and nausea. |
| Metoprolol | 3–5 mg, IV, repeated every 5 min, the maximum dose is 15 mg (hypertension emergencies). | 5–10 min | 5–10 h | Hypotension, heart failure, heart block, dizziness, fatigue, depression, bronchospasm. |
| Labetalol | 25–50 mg, IV, repeat every 15min is permitted, and the total dose can be used up to 200 mg. Intravenous infusion is also feasible, 1–4 mg/min, IV (perioperative hypertension). 20–80 mg IV, 0.5–2.0 mg/min IVI (hypertensive emergency). |
5–10 min | 3–6 min | Nausea, vomiting, cephalic anesthesia, bronchospasm, conduction block, orthostatic hypotension. |
| Urapidil | 10–50 mg IV 6–24 mg/h |
5 min | 2–8 h | Hypotension, dizziness, nausea, and fatigue. |
| Enalaprilat | 1.25–5 mg IV q6 h | 15–30 min | 6–12 h | Blood pressure has a steep drop in high renin status, and the variation is high. |
| Diltiazem | 5–10 mg IV, or 5–15 µg/kg per minute IVI (perioperative hypertension, hypertension emergencies). | 5 min | 30 min | Tachycardia, AV block, hypotension, cardiac failure, peripheral edema, headache, constipation, hepatotoxicity. |
| Dralzine | 10–20 mg IV 10–40 mg IM |
10–20 min 20–30 min |
1–4 h 4–6 h |
Tachycardia, flushing, headache, vomiting and angina aggravated. |
| Fenoldopam | 0.03–1.6 µg/kg per minute, IV | < 5 min | 30 min | Tachycardia, flushing, headache and vomiting. |
| Magnesium sulphate* | Dilute 5 g magnesium sulphate to 20 mL and inject slowly for 5 min, followed by 1 to 2 g/h IVI for maintenance; or dilute 5 g magnesium sulphate to 20 mL and deep intramuscular injection every 4 h. The total dosage can be used to 25–30 g/d (pregnancy-induced hypertension, severe pre-eclampsia). | The drug should be stopped when urine volume < 600 mL/day, respiration < 16 times/min and tendon reflex disappeared. |
*Non-hypertensive drugs. The use of emergency anti-hypertensive drugs is detailed as per the instructions. IV: intravenous injection; IM: intramuscular injection; IVI: intravenous infusion.
(3) The degree and speed of blood pressure reduction: the blood pressure should be gradually adjusted to the appropriate level without the effect to organ perfusion. The target of BP reduction in the initial phase (within 1 h) is to reduce MAP by no more than 25% of the untreated level. Reduce BP to a safer level in the next 2 to 6 h, typically around 160/100 mmHg. Reduce BP to normal levels gradually in the next 24 to 48 h if such BP levels can be tolerated. For pregnant patients with hypertensive emergencies, blood pressure should be controlled steadily to a relatively safe range (< 150/100 mmHg) as soon as possible, and sudden drop in blood pressure should be avoided lest it affects placental blood circulation.
The degree and speed of blood pressure reduction varies from different target organ damaged in hypertensive emergencies. For patients with acute coronary syndrome and acute left heart failure, it is necessary to reduce blood pressure to the level that can improve cardiac blood supply, reduce myocardial oxygen consumption and improve cardiac function as soon as possible. For patients accompanied with aortic dissection, it is necessary to rapidly reduce blood pressure to the lowest level required to maintain the basic perfusion of tissues and organs. Generally, it is necessary to use antihypertensive drugs in combination and pay attention to the sufficient dose of β-blockers. If not applicable (such as increased airway resistance), it is feasible to consider switching to non-dihydropyridine CCB.
Notice: Blood pressure control in hypertensive emergencies is to rapidly lowering blood pressure based on ensuring perfusion of important organs. For patients with existed target organ damage, excessively lowering blood pressure can easily lead to the reduction of tissue perfusion pressure and induce ischemic events, which should be avoided.
6.12.3. Treatment of hypertensive urgencies
BP should be slowly reduced to 160/100 mmHg in 24 to 48 hours. There is no evidence that acute BP lowering management will improve prognosis. The BP reduction of many patients with hypertension urgencies can be achieved with oral medication, such as CCBs, ACEIs, ARBs, β-blockers, α-blockers, etc., and loop diuretics can also be used if applicable. The initial therapy can be treated in the outpatient service or emergency department, with an observation of 5 to 6 hours after medication. The dose should be adjusted after 2 to 3 days in the clinic, after which long-acting preparation may be used to control blood pressure to the final target level. Patients attended in the emergency department should adjust their regimen of oral medication under the blood pressure is basically controlled, and then adjust their treatment regularly in the outpatient service afterwards. Patients in hypertensive urgencies associated with high risk factors such as cardiovascular disease can also be hospitalized for treatment.
6.13. Perioperative management of hypertension
Key point 6L
Continuation of beta-blockers or CCB is recommended in hypertensive patients, while ACEI and ARB should be discontinued.
Target BP for patients under 60 years old should be < 140/90 mmHg. For patients 60 years old or above without diabetes or chronic kidney diseases, SBP should be lowered < 150 mmHg. For patients over 80 years old without diabetes or chronic kidney diseases, SBP should be targeted between 140 and 150 mmHg and < 140/90 mmHg when combined with diabetes or chronic kidney diseases.[110],[213],[293]
6.13.1. Definition of perioperative hypertension and risk factors[65],[294],[295]
(1) Definition: perioperative hypertension refers to an elevation of BP (SBP, DBP or PP) over 30% of baseline between the decision of operation and the end of its related therapy, or SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg during this period. Perioperative hypertensive crisis refers to transient elevation of BP over 180/110 mmHg at this period.
(2) Risk factors: patients with hypertension history, uncontrolled BP before operation, secondary hypertension or intracranial hypertension, psychological factors such as stress, anxiety, fearness or sleeping disorder, especially those with DBP > 110 mmHg, are prone to develop perioperative BP fluctuation.
(3) Operations: perioperative hypertension often occurs in operation of carotid artery, abdominal aorta, peripheral blood vessels, abdominal cavity and thoracic cavity. Severe hypertension may occur in cardiac surgery, large artery operation including carotid endarterectomy and aortic surgery, nervous system operation, head and neck operation, kidney transplantation and severe trauma like empyrosis or head trauma.
6.13.2. Principles of perioperative hypertensive control and BP targets[296]
(1) Principles: basic principle is to ensure perfusion of important organs, reduce cardiac afterload and protect cardiac function. Continuation of β-blockers or CCB is recommended in hypertensive patients, while ACEI and ARB should be discontinued.
(2) BP targets: BP should be controlled < 140/90 mmHg for patients under 60 years old. For patients of 60 years old or above without diabetes or chronic kidney diseases, SBP should be < 150 mmHg. For patients over 80 years old without diabetes or chronic kidney diseases, SBP should be targeted 140 mmHg and 150 mmHg and < 140/90 mmHg when combined with diabetes or chronic kidney diseases.[110],[213],[293] For selective operation patients with SBP/DBP > 180/110 mmHg when entering operation room, deferring the intervention is recommended. If operation is necessary, such as tumor with hemorrhage, the operation could be performed with family members' approval. Considering possible ischemia of important target organ and side effect of antihypertensive pharmacological therapy, it is not recommended to lower blood pressure in few hours for patients with preoperative SBP/DBP > 180/110 mmHg. In patients with mild to moderate hypertension (SBP/DBP < 180/110 mmHg), there is no evidence of benefit from delaying surgery to optimize therapy.[100],[297],[298] Emergency operation should be performed for those with life-threatening emergencies without consulting the level of BP. For severe hypertension combined with life-threatening target organ damage or complications, such as those with left heart failure, unstable angina or variant angina pectoris, oliguric renal failure and severe hypokalemia (< 2.9 mmol/L), vital organs function improvement is recommended in the beginning for a brief period.
6.13.3. Drug therapy of perioperative hypertension
Intravenous administration of antihypertensive drugs is usually recommended. Immediate target is to lower DBP to 110 mmHg in 30 to 60 min or reduce 10%–15% of DBP (but no more than 25%). Lowering BP to 160/100 mmHg in the following 2 to 6 h is recommended, if tolerated. BP should be lowered faster in patients with aortic dissection and reached the bottom line for maintaining organ perfusion within 24 to 48 h. Highly reactive drugs are recommended (Table 15).
7. Hypertension prevention, treatment measures and strategies
Key point 7
Incorporate hypertension prevention into the local medical and health service system and develop corresponding policies, including supervision and evaluation system, resource allocation and personnel arrangement plan.
Community hypertension prevention and treatment should combine “all populations” and “high-risk groups”.
Hypertension needs lifelong management. Modern information technology (‘Internet +’ and electronic digital technology) should be applied to aid disease management, and expert services should be facilitated in places where conditions permit.
7.1. Prevention and treatment policy and health service system
It can be prevented and controlled for most of the hypertension pressure, whereas it is not easy to cure. To prevent hypertension effectively, detecting and diagnosing individuals with elevated BP timely, maintaining healthy BP, and managing BP control continuously and systematically, are critical measures to prevent the occurrence of cardiovascular and cerebrovascular diseases, nephrosis, and death in the whole population. Therefore, it requires policy support of the government and involvement of the whole society (those with the disease and those without) to prevent and control hypertension effectively. Prevention and treatment policies should be feasible, cost-effective, and sustainable.
7.1.1. Healthy lifestyles
It requires healthy lifestyles to prevent the pathogenesis of hypertension as well as to control the risk level of it in patients effectively. Departments of the government play a leading role in the improvement of health, which is implemented by the whole society. It's of great value to implement tobacco control measurements, restrict excessive drinking, reduce salt intake, and increase exercise and healthy eating. Except for public education, it needs the support of relevant laws and regulations. Additionally, appropriate sports facilities should be equipped in workplaces, schools and communities. Food choices should be safe and healthy, whereas tobacco and alcohol consumption should be controlled via price and taxation. Relevant departments of cultural and educational media should publicize healthy lifestyles widely, establish role models fulfilling a healthy lifestyle, and guide the public, especially the youth, to have healthy lifestyles. Medical and health service institutions should provide healthy lifestyle guidance for patients as well as medical interventions for those with severe alcohol and tobacco dependence.
7.1.2. Systematic hypertension management
Generally, systematic hypertension management (providing fair and continuous screening, diagnosis, treatment, referral and long-term follow-up for the whole population) is a responsibility shared by the health service system and the whole population, which includes the following four aspects:
(1) Include the prevention and treatment of hypertension into medical and health service policies. (a): Detection and management protocol should be supported based on local hypertension prevalence and economic conditions and preferential policies should be provided for drug treatment in terms of funding. (b): Regular training should be provided for community doctors according to the service areas. (c): Non-clinical doctors, nurses and pharmacists should be allowed to participate in the screening and lifestyle guiding of hypertensive patients after being trained. (d): Smooth two-way referral channels should be provided for patients with complicated or refractory hypertension; and prevention and treatment quality and effect of hypertension should be taken as the main evaluation indicators for medical and health service at all levels regarding their performance indicators.
(2) Once hypertension occurs, it requires lifelong management. Effective management is the key to preventing complications, such as severe cardiovascular and cerebrovascular diseases. The grassroots medical service is the frontier of hypertension prevention and treatment, which ought to be responsible for the detection, recording, treatment and long-term systematic management of hypertension.
(3) Establish and strengthen the unified electronic cardiovascular and cerebrovascular disease management and expert service network in places where conditions permit. A unified electronic information management network in medical and health service system can significantly improve the efficiency of treatment and management of hypertension. In addition, the expert service network regarding cardiovascular and cerebrovascular diseases can provide further education for the grassroots health care providers as well as immediate guidance and advice for patients to improve the management hypertension.
(4) Establish and implement supervision and evaluation system based on medical investigating evidence, with service quality and outcome as the index and cardiovascular and cerebrovascular health as the target of the whole community, as well as health service policies on resource allocation and personnel arrangements guided by assessment results.
7.2. Community hypertension prevention and treatment strategy
The community should adopt comprehensive prevention and treatment strategies for the whole population, hypertension susceptible (high risk) population and patients in terms of hypertension prevention and treatment, and integrated interventions combining primary, secondary and tertiary prevention.
7.2.1. Strategy for the whole population
Health improvement theory is applied in the strategy for the whole population mainly adopts, with focus on the following aspects: (1) policy development and environment support: healthy lifestyles are called for, with particular focus on reducing salt intake, controlling body weight, promoting early detection and treatment of hypertension, developing policies and creating a supportive environment; (2) Health education: teachers in charge of community health education should strive for the support and cooperation from the local government, and carry out publicity and education on hypertension prevention and control for the whole population in various forms; (3) Community involvement: different departments should cooperate and the whole community should be encouraged to participate in the prevention and treatment of hypertension based on the current health care network; and (4) Facilities intervention: facilities to improve health are divided into five categories: first is the whole city, second is hospitals, third is communities, fourth is workplaces; and fifth is schools. Develop and implement intervention plans on hypertension based on the characteristics of different facilities.
7.2.2. Strategy for population of high-risk (susceptible) to hypertension
It requires early detection of risk factors that may lead to hypertension and effective intervention to prevent the pathogenesis of hypertension in terms of the intervention of high-risk population in the community.
(1) Screening of population susceptible to hypertension: susceptible factors for hypertension include high-normal BP values, overweight and obesity, alcoholism and high salt diet.
(2) Prevention and treatment strategies for population susceptible to hypertension: (a) physical examination: physical examination should include general enquiry, height, weight, BP measurement, routine urinalysis, blood glucose, blood lipids, renal function, electrocardiogram, etc; and (b) control of risk factors level: similar to the strategy for general population, perform followed up for management and lifestyle guidance for individuals susceptible to hypertension based on physical examination.
8. Community-based standardized management of hypertension
Key point 8
Timely detection of hypertension is the first step in prevention and treatment. If there is no condition for the screening of hypertension, the system of “office BP monitoring for first-time visit” should be established. Other opportunities for BP measurement should also be provided.
Integrate the management of hypertension into the daily medical work of general practitioners. Establish the hierarchical medical system of hypertension with general practitioners as the main body and maintain two-way referral unobstructed. Where conditions permit, a grid information management system should be established step by step.
Improve patients' knowledge of disease prevention and self-care awareness in various ways. Where conditions permit, the technology of home BP measurement should be properly promoted.
Community-based standardized management of hypertension can improve patients' awareness rate, treatment rate and control rate.[299] As the control rate of hypertension is low at present, it is necessary to standardize and rationalize the use of antihypertensive drugs to improve the status of routine drug treatment of hypertension in China, and then improve the control rate of hypertension.[300]
8.1. Screening and registration of hypertension
BP should be measured in both adult general outpatients for first-time visit and hypertensive patients. Newly diagnosed hypertensive patients need to be registered for the scope of hypertension management.
8.2. Management of first-time visit hypertensive patients
| First-time visit | Follow-up |
| Determine whether there is atarget organ damage | BP and related symptoms and signs |
| Evaluate the possibility of secondary hypertension | Side effects of treatment |
| Comprehensive cardiovascular risk assessment and determine whether to intervene in other cardiovascular risk factors. | Obstacles affecting lifestyle changes and drug treatment compliance |
| Provide lifestyle guidance and medication. Determine the next follow-up date. Recommend home BP monitoring. Registered for the scope of hypertension management. | |
8.3. Hierarchical long-term follow-up for hypertension management
According to the conditions of primary health service institutions and doctors, it is suggested that, in the long-term follow-up for hypertension patients, the management should be divided into I and II levels. Management levels are determined according to whether the patients reach target BP. The main content of follow-up is to observe BP, medication, adverse reactions. Other risk factors should also be paid attention to, such as heart rate, blood lipid, blood sugar, target organ damage and clinical diseases. Hierarchical management can effectively utilize existing resources so as to focus on the management of patients with uncontrolled hypertension, and improve the BP control rate. The contents of hierarchical follow-up management are shown in Table 16.
Table 16. The contents of hierarchical follow-up for hypertension management.
| Items | Management level I | Management level II |
| Management object | Patients with controlled hypertension | Patients with uncontrolled hypertension |
| Non-drug therapy | Long-term adherence | Strengthen lifestyle interventions for a long time |
| Follow-up frequency | Once every three months | Once every 2–4 weeks |
| Drug therapy | Maintenance drug therapy Keep BP up to standard |
Adjust treatment regimen according to guidelines |
Follow-up content: BP level, treatment measures, adverse reactions, intervention of other risk factors, treatment of clinical situation, etc.
According to the risk factors, target organ damage and concomitant clinical diseases, blood sugar, blood lipid, renal function, urine routine and electrocardiogram can be examined regularly or irregularly.
The main methods of follow-up for hypertension are outpatient follow-up and telephone follow-up. Follow-up can be also carried out online especially for young and middle-aged people.
8.4. Health education for hypertensive patients[301]
The hypertension management team is responsible for the health education of hypertensive patients. The main contents include:
| Normal population | High-risk population of hypertension | Diagnosed hypertensive patients |
|
|
|
8.5. Remote management of hypertensive patients
According to local conditions, each region can actively establish a clinical information system and a chronic disease management information system including hypertension.
Where conditions permit, a remote management platform for hypertension and related diseases can be further established. Patients can measure BP outside hospital by using electronic sphygmomanometer with remote transmission function. Doctors can monitor patients' BP data remotely. So that patients can get doctor's guidance and suggestions without leaving home. The dynamic management of patients' BP outside hospital between outpatient service and follow-up can also be realized. So as to improve patients' treatment compliance and enhance the quality of hypertension management in primary health service institutions.
8.6. Team building
Community health service centers should set up hypertension management teams consisting of doctors, nurses and health accountants (or physician assistant). The team members should receive regular training, and share the responsibility of hypertension management. Team members should have a clear division of labor and responsibilities, and develop team workflow.
8.7. Hierarchical medical system of hypertensive patients
With the advancement of hierarchical medical system reform, the functional orientation of hypertension diagnosis and treatment in medical institutions at all levels should be gradually clarified. General practitioners are the main force of hypertension prevention and treatment. The management of hypertension should be integrated into the daily medical work of general practitioners. The two-way referral channels should be opened to further improve the control rate of hypertension.
8.7.1. Transfer conditions for hypertension in community first-visit
(1) Complicated with severe clinical condition or target organ damage, further evaluation and treatment are needed;
(2) The result of multiple BP measurements is up to grade 3 and further evaluation and treatment are needed;
(3) Suspected patients with secondary hypertension;
(4) Pregnant and lactating women;
(5) Hypertensive emergencies and sub-emergencies;
(6) Further examination is needed in upper hospitals for diagnosis.
8.7.2. Transfer conditions for hypertension in community follow-up
(1) BP of patients which has still not reached the target after being treated with more than two antihypertensive drugs; (2) patients with previously stable BP control, the BP rises again and is difficult to control; (3) the BP fluctuates greatly and the clinical treatment is difficult; (4) new serious clinical diseases or worsening of original diseases occurred during follow-up; (5) unexpected or intractable adverse reactions occurred after taking antihypertensive drugs; and (6) patients with multiple hypertension risk factors or target organ damage and difficult to deal with.
8.7.3. Transfer conditions for patients from superior hospitals to communities
(1) The diagnosis of hypertension is clear; (2) the treatment regimen has been determined; and (3) BP and its accompanying clinical conditions have been controlled and stabilized.
8.8. Self-management of hypertensive patients
All hypertensive patients should participate in self-management to varying degrees. (1) Improving compliance: General practitioners should use their knowledge, skills and resources to help patients in their preferred ways. In order to enhance their initiative in preventing and treating hypertension and compliance with antihypertensive drugs. (2) Patient self-management group: By combining with the neighborhood committee or village committee, the patient self-management group should carry out education for hypertensive patients. (3) Family BP measurement: Guide patients to carry out family self-measurement of BP. It is recommended that patients use the upper arm automatic sphygmomanometer qualified by international standards to measure BP when conditions permit. Guide patients to master measurement technology and standardize operation, record BP measurement results truthfully. Provide the BP data to medical staff for treatment reference during follow-up.
9. Secondary hypertension
Key point 9
Conventional Secondary hypertension screening should be performed in patients with newly diagnosed hypertension.
Patients with Resistant hypertension should be considered as having the possibility of secondary hypertension and should be advised to the relevant specialist when necessary.
Secondary hypertension, also known as symptomatic hypertension, is one of the symptoms of some diseases in their developments. When the primary disease is cured, BP will also drop or go back to normal. In addition to the harm caused by hypertension itself, the electrolyte disturbance, endocrine imbalance, hypoxemia that associated with secondary hypertension can also lead to the cardiovascular damage independent of BP, which is more harmful than primary hypertension. Therefore, early identification and treatment are particularly important. Conventional secondary hypertension screening should be performed in patients with newly diagnosed hypertension. Patients with resistant hypertension should be considered as the possibility of secondary hypertension and should be advised to the hypertension specialty or endocrine and nephropathy specialty when necessary.
9.1. Renal parenchymal hypertension
Common diseases that leads to renal parenchymal hypertension include various primary glomerulonephritis (IgA nephropathy, focal segmental glomerular sclerosis, membranoproliferative glomerulonephritis, etc.); polycystic kidney disease; tubulointerstitial disease (chronic pyelonephritis, obstructive nephropathy, reflux nephropathy, etc.); metabolic disease and renal damage (diabetic nephropathy, etc.); systemic or connective tissue disease. Renal damage by systemic or connective tissue diseases (lupus nephritis, scleroderma, etc.); monoclonal immunoglobulin-related kidney disease (light chain deposition disease); hereditary kidney disease (Liddle syndrome, etc.).
The diagnosis of renal parenchymal hypertension depends on: history of kidney disease; proteinuria and hematuria; abnormal renal function; decreased eGFR; abnormal size and shape of kidney; and should take pathological biopsy of kidney when necessary. At the same time, it should be differentiated from the kidney damage caused by hypertension, the former often occurs before or at the same time with hypertension with high and uncontrollable BP; proteinuria/hematuria occurs early and severely, and the renal function is significantly damaged.
Patients with renal parenchymal hypertension should be given a low-salt diet (NaCl < 6.0 g/day, Na < 2.3 g/day). For patients with renal insufficiency, it is advisable to choose high-quality protein with high biological value (0.3–0.6 g/kg per day) to ensure adequate energy intake and plus alpha-ketoacid therapy. The target BP is 130/80 mmHg. The first choice for patients with proteinuria should be ACEI or ARB. Long-acting CCB, diuretics, beta-receptor blockers and alpha-receptor blockers can be used as combined therapy drugs.
9.2. Hypertension caused by renal artery stenosis and other vascular diseases
9.2.1. Renal artery stenosis
The main characteristic of renal artery stenosis is the stenosis at the main trunk or branch of renal artery, which leads to renal ischemia, significant increase of renin-angiotensin system activity thereby causing hypertension and renal hypofunction. Renal artery stenosis is one of the most important causes of hypertension and/or renal insufficiency. The prevalence of renal artery stenosis is about 1%–3% of in hypertensive patients. In China, atherosclerosis is the most common cause of renal artery stenosis, accounting for about 82%, followed by arteritis (about 12%), fibromuscular dysplasia (about 5%) and other causes accounting for 1%.
The purposes of diagnosing renal artery stenosis include: (1) defining the causes; (2) defining lesion site and degree; (3) hemodynamic significance; and (4) whether can benefit from vascular reconstruction. Transarterial angiography is still the gold standard for the diagnosis of renal artery stenosis. Antihypertensive drugs treatment is the basic treatment for renal vascular hypertension. CCB is safe and effective. ACEI or ARB is the most targeted drug, but it should be cautiously used in patients with unifunctional or bilateral renal artery stenosis. For severe renal artery stenosis with pathophysiological significance (diameter stenosis > 70%), for example: if BP is poorly controlled, kidney atrophy or renal dysfunction occurred, revascularization is recommended.[309] Endovascular therapy is the first choice for vascular reconstruction. Open surgery is recommended for failed lesions.
9.2.2. Stenosis of aorta
Aortic stenosis includes congenital and acquired aortic stenosis. Congenital aortic stenosis manifests as limited stenosis or atresia at the aorta, the onset site is usually near the orifice of the original ductus arteriosus in the isthmus of the aorta, while some of which may occur in other parts of the aorta. Acquired aortic stenosis includes Takayasu arteritis, atherosclerosis, and aortostenosis causes by Aortic dissection. The basic pathophysiological changes of the disease are blood flow redistribution caused by stenosis, water and sodium retention and RAS activation caused by renal ischemia, which results in left ventricular hypertrophy, heart failure, cerebral hemorrhage and other important organ damages. Aortic stenosis manifests as hypertension in upper limbs, weak or no arteries in lower limbs. The BP of both lower limbs was significantly lower than that of upper limbs (ABI < 0.9). There was obvious vascular murmur around stenosis vessels during auscultation. There was obvious vascular murmur around stenosis vessels during auscultation. Endovascular therapy or open surgery was selected according to the specific condition. Active Takayasu arteritis should be treated with glucocorticoids and immunosuppressive agents.
9.3. Obstructive sleep apnea syndrome
Obstructive Sleep Apnea Syndrome (OSAS) includes muscle collapse in upper respiratory tract during sleep, apnea or significant reduction of oronasal airflow, resulting in intermittent hypoxia, sleep fragmentation, sympathetic hyperexcitability, neurohumoral dysregulation and so on. The incidence of hypertension in these patients ranges from 35% to 80%.[310]
Polysomnographic breathing monitor (PSG) is the “golden standard” for diagnosing OSAS. Apnea hypopnea index (AHI) refers to the average number of sleep apnea hypopnea in per hour. According to AHI, it can be divided into mild, moderate and severe degrees, mild: AHI 5–15 times/h; moderate: AHI 15–30 times/hour; severe: AHI more than 30 times/h.
Improving life style is the basis of treatment, which includes losing weight, proper exercise, smoking cessation, alcohol restriction, lateral sleeping, etc. For patients with mild OSAS, oral appliance is recommended; for patients with mild OSAS with obvious symptoms (such as daytime sleepiness, cognitive impairment, depression), cardio-cerebrovascular diseases and diabetes mellitus, and for patients with moderate to severe OSAS (AHI > 15 times/h), non-invasive ventilation (CPAP) is recommended.
9.4. Primary aldosteronism and other endocrine hypertension
9.4.1. Primary aldosteronism
Primary aldosteronism is a clinical syndrome characterized by hyperaldosterone secretion in the globular zone of the adrenal cortex, which leads to hypertension, hypokalemia and renin activity inhibition. Common types of primary aldosteronism include aldosteronism (35%) and idiopathic aldosteronism (60%). Other rare types are adrenal cortical carcinoma and familial aldosteronism, such as glucocorticoid-inhibiting aldosteronism (GRA). Primary aldosteronism accounts for about 5%–10% of hypertensive patients and only a small percentage of them have hypokalemia, which accounts for about 20% of refractory hypertension. It can increase the risk of metabolic syndrome, arteriosclerosis and cardiovascular and cerebrovascular diseases.[311],[312]
The clinical diagnosis process of primary aldosteronism includes three steps: screening, diagnosis and classification. Serum aldosterone/renin ratio (ARR) was used for screening.[301] The screening subjects were refractory hypertension, hypertension with spontaneous or diuretic-induced hypokalemia, or adrenal accidental tumors, primary aldosteronism in first-degree relatives, sleep apnea syndrome, early onset hypertension or family history of cardiovascular events (< 40 years old). The confirmation tests include high sodium diet test, intravenous saline test, fluorocortisone inhibition test and captopril test. The classification diagnostic method includes adrenal imaging examination and lateral adrenal venous sampling (AVS). Patients with surgical indication and intention should undergo AVS. While, for those younger than 35 years of age and have typical manifestations (hyperaldosterone, PRA depression, hypokalemia, unilateral adrenal space–occupying lesions), AVS can be avoided. Treatment includes surgery and drug therapy. Patients younger than 35 years of age with unilateral adenomas or large nodules (> 1 cm) or unilateral dominant secretory adenomas or nodules confirmed by AVS were should take surgical treatment.
Drug therapy should be taken for those who have no surgical indication, intention or intolerance. The first-line drug is salt corticosteroid receptor antagonist, and spironolactone is recommended as the first choice.
9.4.2. Pheochromocytoma/paraganglioma
Pheochromocytoma is a neoplasm originating from adrenal medulla or pheochromocyte of extra adrenal nerve chain. Tumor can secrete excessive catecholamine (CA), which can cause persistent or paroxysmal hypertension, functional and metabolic disorders on some organs. It is a clinically curable secondary hypertension. The clinical features of pheochromocytoma appeared to be paroxysmal, persistent or paroxysmal severe hypertension. Hypertension is often accompanied by headache, palpitation and hyperhidrosis, also abnormal glucose and lipid metabolism.
The main method of qualitative diagnosis of pheochromocytoma is determination of catecholamines and its metabolites. Enhanced CT is recommended as the preferred locational method for thoracic, abdominal and pelvic lesions. MRI is recommended as the preferred locational method for skull base and neck lesions. Besides, metaiodobenzylguanidine (MIBG), 18F-FDG PET and somatostatin imaging can be used to make function and image localization for metastatic and extraadrenal tumors. Surgical treatment is important for patients with pheochromocytoma. Alpha-receptor blockers can be administered before surgery. Using beta-blockers before using alpha-blockers is not recommended. Lifelong follow-up should be taken after surgery.
9.4.3. Cushing's syndrome
Cushing's syndrome (CS) that is hypercortisolism. Hypercortisolism can be accompanied by various complications, leading to the syndrome with typical manifestations like centripetal obesity, hypertension, abnormal glucose metabolism, hypokalemia and osteoporosis.
As Qualitative and locational diagnosis of CS and its treatment is more complicated, it is suggested to communicate and cooperate with doctors in hypertension specialty or endocrinology department actively. ACEI or ARB antihypertensive drugs are preferred to use in the initial treatment of Cushing's syndrome-related hypertension.
If BP is still higher than 130/80 mmHg, they can be combined with mineralocorticoids receptor antagonists or CCB according to the severity of the disease and the presence or absence of hypokalemia. If BP is still higher than 130/80 mmHg, the alpha-receptor blocker or nitric acid can be added. If BP still cannot reach the standard, beta-blocker and diuretic can be carefully selected and used.
9.5. Other rare types of secondary hypertension
According to the present epidemiological data, there are still some rare causes of elevated BP, which account for less than 1% of the causes of hypertension, mainly includes thyroid dysfunction, hyperparathyroidism, renin tumors and so on.
9.6. Drug-induced hypertension
Drug-induced hypertension is caused by the drug itself in a conventional dose or its interactions with other drugs, and when BP exceeds 140/90 mmHg, it should be considered as drug-induced hypertension (Table 17). The drugs involved mainly include: (1) hormone drugs; (2) central nervous drugs; (3) non-steroidal anti-inflammatory drugs; (4) Chinese herbal medicine; and (5) other drugs.
Table 17. Drugs, mechanisms and treatment of drug-induced hypertension.
| Category | Common drugs | Mechanism | Treatment and notes | |
| Hormones | ||||
| Estrogen | Estradiol, ilestriol | (1) Water-sodium retention | Diuretic | |
| premarin, desogestreland ethinylestradiol | (2) RAS activation (3) Insulin resistance |
ACEI (ARB) β-blocker |
||
| Progestogen | Medroxyprogesterone 17-acetate, nore-thindrone, medroxyprogesterone acetate | Corticosteroid responses induced by | High doses of drugs | |
| Androgen | MethyltestosteroneNandroloniPhenylPropionas, stanozolol | (1) Induce polycythemia (2) Affecting the regulation of potassium channels and androgen receptors, leading to retention of nitrogen, sodium, potassium and phosphorus and insulin resistance |
||
| Oxytocin | Antidiuretic effects will occur in large doses | |||
| Pituitrin | (1) Arterioles contraction (2) Increased water reabsorption |
|||
| Glucocorticoid | Hydrocortisone, Prednisone, Dexamethasone | Both cortisol and corticosterone have salt corticosteroid activity | Pay attention to the change of serum potassium Diuretic CCB ACEI (ARB) |
|
| Mineralocor-ticoid | 9α-Fludrocortisone, Deoxycortone Acetate | Increase sodium reabsorption and Promote potassium excretion | Diuretic Pay attention to the change of serum potassium |
|
| Thyroxine Sodium | Euthyrox | Increase the excitability of sympathetic nervous system | ||
| Affecting sympathetic excitation | ||||
| Anesthetics | Ketamine, desflurane, sevoflurane, naloxone hydrochloride, | Increased sympathetic excitability | α receptor blockers, clonidine, diltiazem, | |
| ritali, amphetamine, cocaine | Promote the release of dopamine and NE from nerve endings and block their recovery, increase synaptic sites and prolong the action time | α receptor blockers, verapamil, nitroglycerin | ||
| Antiparkinsonian drug | L-DOPA | Stimulate dopamine receptors at the postsynaptic membrane to play the role of antiparkinsonian and elevate BP at the same time | ||
| Diet pills | Sibutramine | Inhibit the re-uptake of 5-hydroxytryptamine and NE, increase the content of synaptic space and the excitability of sympathetic nerve | Lose weight in other ways ACEI (ARB) β-blocker | |
| Adrenaline β2-agonist | Salbutamol sulfate, bambuterol hydrochloride, terbutaline sulfate, clorprenaline | Activate the adenylate cyclase and increase the synthesis of adenosine cyclophosphate in cells | Should be used with caution for pheochromocytoma or hyperthyroidism | |
| Methylxanthines | Aminophylline, doxofylline,dyphylline | Increased the release of endogenous epinephrine and norepinephrine | ||
| Nonsteroidal anti-inflammatory drugs | ||||
| Indomethacin, indomethacin,ibuprofen, phenylbutazone celebrex, arthrotec, antine | (1) Water-sodium retention, (2) reduce the prostaglandins in circulation, (3) renal damage | CCB ACEI (ARB) |
||
| Chinese herbal medicine | ||||
| Glycyrrhizin | Glycyrrhizin, cholic acid, carbenoxolone | (1) Inhibits the activity of 11beta-hydroxysteroid dehydro-genas, increase the production of cortisol-mediated mineral corticoid and elevate BP (2) Inhibit the synthesis of prostaglandin (3) Inhibit the synthesis and release of histamine |
Diuretics CCB ACEI (ARB) |
|
| Ephedrines | Ephedrine nasal drops, ephedrine and chlorphenamine, diphenhydramine | (1) Directly activate adrenaline α and β2 receptors (2) Indirectly promote the release of NE neurotransmitters (3) Significant central stimulating |
α receptor blocker β receptor blocker |
|
| Others | ||||
| Monoamine oxidase inhibitor | Isoniazid, furazolidone, ketoconazole; Reserpine; TCA | Antagonize monoamine oxidase and other enzymes, it is not beneficial to the inactivation of catecholamines both inside and outside the cell, therefore enhances vasoconstriction. | α receptor blocker | |
| TZDs | Rosiglitazone maleate, pioglitazone | Water-sodium retention | Use cautiously in patients with severe heart failure | |
| Recombinant human erythropoietin | (1) Vasoconstriction and intracellular calcium homeostasis and increase sympathetic excitability (2) Stimulate the synthesis of endothelin in vascular endothelial cells (3) Polycythemia (4) Genetic mechanisms |
Preferred CCB or αreceptor blocker, Diuretics and ACEI are not sensitive for antihyper-tensive effects | ||
| Ciclosporin and immuno-suppressant | Cyclosporin Tacrolimus | (1) Activation of sympathetic nervous system (2) Diuretic response is unresponsive when dilatation of blood volume happen (3) NO-mediated vasodilation is impaired and endothelin release increased (4) Afferent nerve of renal sympathetic nerve is activated after neurocalcin was blocked |
CCB (may increase in serum cyclosporin concentration) Combination of multiple antihypertensive drugs (Clonidine) |
|
ACEI: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blockers; CCB: calcium channel blockers.
9.7. Monogenic inherited hypertension
The mutations of monogenic inherited hypertension are mostly associated with gene mutations on renal unit ion transporters or RAS components causing dysfunction. It can be divided into the following categories: (1) Gene mutations directly affect the function of related proteins in renal tubu-lar ion channel transport system: Liddle syndrome, Gordon syndrome, apparent mineralocortixoid excess, pregnancy-I resistancenduced hypertension caused by corticosteroid receptor mutations (2) abnormal steroid synthesis in the adrenal gland caused by Gene mutations: familial hyperaldosteronism (I, II, III), congenital adrenal hyperplasia (11β-hydroxylase deficiency, 7 α-hydroxylase/17, 20-lyase deficiency, 17OHD), familial glucocorticoid resistance (3) Various neuroendocrine tumors, such as pheochromocytoma, hypertension with brachydactylia, multipleendocrineneoplasm (MEN) and Von Hippel-Lindau (VHL).
10. Research prospection
In 2015, researchers from Chinese Center for Disease Control and Prevention published an article focusing on the burden of disease in China, showing that from 1990 to 2013 the age-standardized death rate of stroke decreased by 21% and that rate of hemorrhagic stroke decreased by 38% respectively.[313] Stroke, especially hemorrhagic stroke, is a major complication of hypertension, therefore the results reflects the hypertension prevention and treatment has achieved some effect in terms of cardiac outcomes. Presently, the important ongoing hypertension researches in China include Study of Antihypertensive Treatment in Patients with High-normal Blood Pressure and Risk Factors (CHINOM), Optimal Blood Pressure and Cholesterol Targets for Preventing Recurrent Stroke in Hypertensives (SHOT), Strategy of Blood Pressure Intervention in the Elderly Hypertensive Patients (STEP), Systolic hypertension in the elderly: Chinese Trial-2 (Syst-China-2), Intervention Study of Blood Pressure in People with High Normal or Borderline Hypertension and Type 2 Diabetes (IPAD), China Stroke Primary Prevention Trial-2 (CSPPT-2) and so on. The report of Comparative Effect Study of L-amlodipine Maleate and Amlodipine Besylate in the Hypertensive Patients (LEADER Study), supported by the National Science and Technology Major Project for Drug Discovery, is being summarized, and important results will be released for clinical reference. The CHIEF study will also continue to summarize data on cardiovascular events.
Supplement 1. Blood pressure references for children and adolescents aged 3 to 17 years old in China by sex and height.
Supplement Table 1-1. Blood pressure references for children and adolescents aged 3 to 17 years old in China, male.
| Age, year | Height percentile | Height range, cm | SBP, mmHg |
DBP, mmHg |
||||||
| 50th | 90th | 95th | 99th | 50th | 90th | 95th | 99th | |||
| 3 | P5 | < 96 | 88 | 99 | 102 | 108 | 54 | 62 | 65 | 72 |
| P10 | 96–97 | 88 | 100 | 103 | 109 | 54 | 63 | 65 | 72 | |
| P25 | 98–100 | 89 | 101 | 104 | 110 | 54 | 63 | 66 | 72 | |
| P50 | 101–103 | 90 | 102 | 105 | 112 | 54 | 63 | 66 | 73 | |
| P75 | 104–106 | 91 | 103 | 107 | 113 | 55 | 63 | 66 | 73 | |
| P90 | 107–108 | 92 | 104 | 107 | 114 | 55 | 63 | 66 | 73 | |
| P95 | ≥ 109 | 93 | 105 | 108 | 115 | 55 | 63 | 66 | 73 | |
| 4 | P5 | < 102 | 89 | 101 | 104 | 111 | 55 | 64 | 67 | 74 |
| P10 | 102–104 | 90 | 102 | 105 | 111 | 55 | 64 | 67 | 74 | |
| P25 | 105–107 | 91 | 103 | 106 | 113 | 55 | 64 | 67 | 74 | |
| P50 | 108–110 | 92 | 104 | 108 | 114 | 56 | 64 | 67 | 74 | |
| P75 | 111–113 | 93 | 106 | 109 | 115 | 56 | 64 | 67 | 74 | |
| P90 | 114–116 | 94 | 107 | 110 | 117 | 56 | 65 | 68 | 75 | |
| P95 | ≥ 117 | 95 | 107 | 111 | 117 | 56 | 65 | 68 | 75 | |
| 5 | P5 | < 109 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 75 |
| P10 | 109–110 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 75 | |
| P25 | 111–113 | 93 | 105 | 109 | 115 | 56 | 65 | 68 | 75 | |
| P50 | 114–117 | 94 | 106 | 110 | 117 | 57 | 65 | 69 | 76 | |
| P75 | 118–120 | 95 | 108 | 111 | 118 | 57 | 66 | 69 | 76 | |
| P90 | 121–123 | 96 | 109 | 112 | 119 | 58 | 67 | 70 | 77 | |
| P95 | ≥ 124 | 97 | 110 | 113 | 120 | 58 | 67 | 70 | 77 | |
| 6 | P5 | < 114 | 93 | 105 | 109 | 115 | 57 | 66 | 69 | 76 |
| P10 | 114–116 | 94 | 106 | 110 | 116 | 57 | 66 | 69 | 76 | |
| P25 | 117–119 | 95 | 107 | 111 | 117 | 58 | 66 | 69 | 77 | |
| P50 | 120–123 | 96 | 108 | 112 | 119 | 58 | 67 | 70 | 78 | |
| P75 | 124–126 | 97 | 110 | 113 | 120 | 59 | 68 | 71 | 78 | |
| P90 | 127–129 | 98 | 111 | 115 | 121 | 59 | 69 | 72 | 79 | |
| P95 | ≥ 130 | 99 | 112 | 116 | 123 | 60 | 69 | 73 | 80 | |
| 7 | P5 | < 118 | 94 | 106 | 110 | 117 | 58 | 67 | 70 | 77 |
| P10 | 118–120 | 95 | 107 | 111 | 118 | 58 | 67 | 70 | 78 | |
| P25 | 121–123 | 96 | 108 | 112 | 119 | 59 | 68 | 71 | 78 | |
| P50 | 124–127 | 97 | 110 | 113 | 120 | 59 | 68 | 72 | 79 | |
| P75 | 128–131 | 98 | 112 | 115 | 122 | 60 | 70 | 73 | 81 | |
| P90 | 132–135 | 100 | 113 | 117 | 124 | 61 | 71 | 74 | 82 | |
| P95 | ≥ 136 | 100 | 114 | 117 | 125 | 62 | 71 | 74 | 82 | |
| 8 | P5 | < 121 | 95 | 108 | 111 | 118 | 59 | 68 | 71 | 78 |
| P10 | 121–123 | 95 | 108 | 112 | 119 | 59 | 68 | 71 | 79 | |
| P25 | 124–127 | 97 | 110 | 113 | 120 | 60 | 69 | 72 | 80 | |
| P50 | 128–132 | 98 | 111 | 115 | 122 | 61 | 70 | 73 | 81 | |
| P75 | 133–136 | 99 | 113 | 117 | 124 | 62 | 71 | 74 | 82 | |
| P90 | 137–139 | 101 | 114 | 118 | 125 | 62 | 72 | 75 | 83 | |
| P95 | ≥ 140 | 102 | 115 | 119 | 127 | 63 | 73 | 76 | 84 | |
| 9 | P5 | < 125 | 96 | 109 | 112 | 119 | 60 | 69 | 72 | 80 |
| P10 | 125–128 | 96 | 109 | 113 | 120 | 60 | 69 | 73 | 80 | |
| P25 | 129–132 | 98 | 111 | 115 | 122 | 61 | 71 | 74 | 82 | |
| P50 | 133–137 | 99 | 113 | 117 | 124 | 62 | 72 | 75 | 83 | |
| P75 | 138–142 | 101 | 115 | 119 | 126 | 63 | 73 | 76 | 84 | |
| P90 | 143–145 | 102 | 116 | 120 | 128 | 64 | 73 | 77 | 85 | |
| P95 | ≥ 146 | 103 | 117 | 121 | 129 | 64 | 74 | 77 | 85 | |
| 10 | P5 | < 130 | 97 | 110 | 114 | 121 | 61 | 70 | 74 | 81 |
| P10 | 130–132 | 98 | 111 | 115 | 122 | 62 | 71 | 74 | 82 | |
| P25 | 133–137 | 99 | 113 | 116 | 124 | 62 | 72 | 75 | 83 | |
| P50 | 138–142 | 101 | 115 | 119 | 126 | 63 | 73 | 77 | 85 | |
| P75 | 143–147 | 102 | 117 | 120 | 128 | 64 | 74 | 77 | 85 | |
| P90 | 148–151 | 104 | 118 | 122 | 130 | 64 | 74 | 77 | 86 | |
| P95 | ≥ 152 | 105 | 119 | 123 | 131 | 64 | 74 | 77 | 86 | |
| 11 | P5 | < 134 | 98 | 111 | 115 | 122 | 62 | 72 | 75 | 83 |
| P10 | 134–137 | 99 | 112 | 116 | 124 | 63 | 72 | 76 | 84 | |
| P25 | 138–142 | 100 | 114 | 118 | 126 | 64 | 73 | 77 | 85 | |
| P50 | 143–148 | 102 | 116 | 120 | 128 | 64 | 74 | 78 | 86 | |
| P75 | 149–153 | 104 | 119 | 123 | 130 | 64 | 74 | 78 | 86 | |
| P90 | 154–157 | 106 | 120 | 124 | 132 | 64 | 74 | 78 | 86 | |
| P95 | ≥ 158 | 106 | 121 | 125 | 133 | 64 | 74 | 78 | 86 | |
| 12 | P5 | < 140 | 100 | 113 | 117 | 125 | 64 | 73 | 77 | 85 |
| P10 | 140–144 | 101 | 115 | 119 | 126 | 64 | 74 | 78 | 86 | |
| P25 | 145–149 | 102 | 117 | 121 | 128 | 65 | 75 | 78 | 86 | |
| P50 | 150–155 | 104 | 119 | 123 | 131 | 65 | 75 | 78 | 86 | |
| P75 | 156–160 | 106 | 121 | 125 | 133 | 65 | 75 | 78 | 86 | |
| P90 | 161–164 | 108 | 123 | 127 | 135 | 65 | 75 | 78 | 87 | |
| P95 | ≥ 165 | 108 | 124 | 128 | 136 | 65 | 75 | 78 | 87 | |
| 13 | P5 | < 147 | 102 | 116 | 120 | 128 | 65 | 75 | 78 | 86 |
| P10 | 147–151 | 103 | 117 | 121 | 129 | 65 | 75 | 78 | 87 | |
| P25 | 152–156 | 104 | 119 | 123 | 131 | 65 | 75 | 79 | 87 | |
| P50 | 157–162 | 106 | 121 | 125 | 133 | 65 | 75 | 79 | 87 | |
| P75 | 163–167 | 108 | 123 | 128 | 136 | 65 | 75 | 79 | 87 | |
| P90 | 168–171 | 110 | 125 | 130 | 138 | 66 | 76 | 79 | 87 | |
| P95 | ≥ 172 | 110 | 126 | 130 | 139 | 66 | 76 | 79 | 88 | |
| 14 | P5 | < 154 | 103 | 118 | 122 | 130 | 65 | 75 | 79 | 87 |
| P10 | 154–157 | 104 | 119 | 124 | 132 | 65 | 75 | 79 | 87 | |
| P25 | 158–162 | 106 | 121 | 125 | 133 | 65 | 75 | 79 | 87 | |
| P50 | 163–167 | 108 | 123 | 128 | 136 | 65 | 75 | 79 | 87 | |
| P75 | 168–172 | 109 | 125 | 130 | 138 | 66 | 76 | 79 | 88 | |
| P90 | 173–176 | 111 | 127 | 131 | 140 | 66 | 76 | 80 | 88 | |
| P95 | ≥ 177 | 112 | 128 | 133 | 141 | 67 | 77 | 80 | 89 | |
| 15 | P5 | < 158 | 105 | 120 | 124 | 132 | 65 | 76 | 79 | 87 |
| P10 | 158–161 | 106 | 121 | 125 | 133 | 65 | 76 | 79 | 87 | |
| P25 | 162–166 | 107 | 122 | 127 | 135 | 66 | 76 | 79 | 88 | |
| P50 | 167–170 | 109 | 124 | 128 | 137 | 66 | 76 | 80 | 88 | |
| P75 | 171–174 | 110 | 126 | 131 | 139 | 66 | 77 | 80 | 89 | |
| P90 | 175–178 | 112 | 128 | 132 | 141 | 67 | 77 | 81 | 89 | |
| P95 | ≥ 179 | 113 | 129 | 133 | 142 | 67 | 77 | 81 | 90 | |
| 16 | P5 | < 161 | 105 | 121 | 125 | 133 | 66 | 76 | 79 | 88 |
| P10 | 161–164 | 106 | 121 | 126 | 134 | 66 | 76 | 79 | 88 | |
| P25 | 165–168 | 107 | 123 | 127 | 136 | 66 | 76 | 80 | 88 | |
| P50 | 169–172 | 109 | 125 | 129 | 138 | 66 | 76 | 80 | 88 | |
| P75 | 173–176 | 111 | 126 | 131 | 140 | 67 | 77 | 80 | 89 | |
| P90 | 177–179 | 112 | 128 | 133 | 141 | 67 | 77 | 81 | 90 | |
| P95 | ≥ 180 | 113 | 129 | 134 | 142 | 67 | 78 | 81 | 90 | |
| 17 | P5 | < 163 | 106 | 121 | 126 | 134 | 66 | 76 | 80 | 88 |
| P10 | 163–165 | 107 | 122 | 126 | 135 | 66 | 76 | 80 | 88 | |
| P25 | 166–169 | 108 | 124 | 128 | 136 | 66 | 76 | 80 | 88 | |
| P50 | 170–173 | 109 | 125 | 130 | 138 | 67 | 77 | 80 | 89 | |
| P75 | 174–177 | 111 | 127 | 131 | 140 | 67 | 77 | 81 | 89 | |
| P90 | 178–180 | 112 | 129 | 133 | 142 | 67 | 78 | 81 | 90 | |
| P95 | ≥ 181 | 113 | 129 | 134 | 143 | 68 | 78 | 82 | 90 | |
Supplement Table 1-2. Blood pressure references for children and adolescents aged 3 to 17 years old in China, female.
| Age, year | Height percentile | Height range, cm | SBP, mmHg |
DBP, mmHg |
||||||
| 50th | 90th | 95th | 99th | 50th | 90th | 95th | 99th | |||
| 3 | P5 | < 95 | 87 | 99 | 102 | 108 | 55 | 63 | 67 | 74 |
| P10 | 95–96 | 88 | 99 | 103 | 109 | 55 | 63 | 67 | 74 | |
| P25 | 97–99 | 88 | 100 | 103 | 110 | 55 | 64 | 67 | 74 | |
| P50 | 100–102 | 89 | 101 | 104 | 111 | 55 | 64 | 67 | 74 | |
| P75 | 103–105 | 90 | 102 | 105 | 112 | 55 | 64 | 67 | 74 | |
| P90 | 106–107 | 91 | 103 | 106 | 113 | 55 | 64 | 67 | 75 | |
| P95 | ≥ 108 | 91 | 103 | 107 | 113 | 56 | 64 | 67 | 75 | |
| 4 | P5 | < 101 | 89 | 101 | 105 | 111 | 56 | 64 | 67 | 75 |
| P10 | 101–103 | 89 | 101 | 105 | 111 | 56 | 64 | 67 | 75 | |
| P25 | 104–106 | 90 | 102 | 106 | 112 | 56 | 64 | 67 | 75 | |
| P50 | 107–109 | 91 | 103 | 107 | 113 | 56 | 64 | 67 | 75 | |
| P75 | 110–112 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 75 | |
| P90 | 113–114 | 93 | 105 | 109 | 115 | 56 | 65 | 68 | 76 | |
| P95 | ≥ 115 | 93 | 105 | 109 | 115 | 56 | 65 | 68 | 76 | |
| 5 | P5 | < 108 | 91 | 103 | 106 | 113 | 56 | 65 | 68 | 76 |
| P10 | 108–109 | 91 | 103 | 107 | 113 | 56 | 65 | 68 | 76 | |
| P25 | 110–112 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 76 | |
| P50 | 113–116 | 93 | 105 | 109 | 115 | 57 | 65 | 68 | 76 | |
| P75 | 117–119 | 93 | 106 | 109 | 116 | 57 | 66 | 69 | 77 | |
| P90 | 120–122 | 94 | 107 | 111 | 117 | 58 | 66 | 70 | 77 | |
| P95 | ≥ 123 | 95 | 108 | 111 | 118 | 58 | 67 | 70 | 78 | |
| 6 | P5 | < 113 | 92 | 104 | 108 | 115 | 57 | 65 | 69 | 76 |
| P10 | 113–114 | 92 | 105 | 108 | 115 | 57 | 66 | 69 | 77 | |
| P25 | 115–118 | 93 | 106 | 109 | 116 | 57 | 66 | 69 | 77 | |
| P50 | 119–121 | 94 | 107 | 110 | 117 | 58 | 67 | 70 | 78 | |
| P75 | 122–125 | 95 | 108 | 112 | 118 | 58 | 67 | 71 | 79 | |
| P90 | 126–128 | 96 | 109 | 113 | 119 | 59 | 68 | 71 | 79 | |
| P95 | ≥ 129 | 97 | 110 | 114 | 121 | 59 | 69 | 72 | 80 | |
| 7 | P5 | < 116 | 93 | 105 | 109 | 115 | 57 | 66 | 69 | 77 |
| P10 | 116–118 | 93 | 106 | 109 | 116 | 57 | 66 | 69 | 77 | |
| P25 | 119–122 | 94 | 107 | 110 | 117 | 58 | 67 | 70 | 78 | |
| P50 | 123–126 | 95 | 108 | 112 | 119 | 59 | 68 | 71 | 79 | |
| P75 | 127–130 | 96 | 109 | 113 | 120 | 59 | 69 | 72 | 80 | |
| P90 | 131–133 | 97 | 111 | 114 | 122 | 60 | 69 | 73 | 81 | |
| P95 | ≥ 134 | 98 | 112 | 115 | 122 | 61 | 70 | 73 | 82 | |
| 8 | P5 | < 120 | 94 | 106 | 110 | 116 | 58 | 67 | 70 | 78 |
| P10 | 120–122 | 94 | 107 | 111 | 117 | 58 | 67 | 71 | 79 | |
| P25 | 123–126 | 95 | 108 | 112 | 119 | 59 | 68 | 71 | 79 | |
| P50 | 127–131 | 96 | 109 | 113 | 120 | 60 | 69 | 72 | 80 | |
| P75 | 132–135 | 98 | 111 | 115 | 122 | 61 | 70 | 73 | 82 | |
| P90 | 136–138 | 99 | 112 | 116 | 123 | 61 | 71 | 74 | 83 | |
| P95 | ≥ 139 | 100 | 113 | 117 | 124 | 62 | 71 | 75 | 83 | |
| 9 | P5 | < 124 | 95 | 108 | 111 | 118 | 59 | 68 | 71 | 79 |
| P10 | 124–127 | 95 | 108 | 112 | 119 | 59 | 68 | 72 | 80 | |
| P25 | 128–132 | 97 | 110 | 113 | 120 | 60 | 69 | 73 | 81 | |
| P50 | 133–136 | 98 | 111 | 115 | 122 | 61 | 71 | 74 | 82 | |
| P75 | 137–141 | 100 | 113 | 117 | 124 | 62 | 72 | 75 | 84 | |
| P90 | 142–145 | 101 | 114 | 118 | 125 | 63 | 72 | 76 | 84 | |
| P95 | ≥ 146 | 102 | 115 | 119 | 126 | 63 | 73 | 76 | 85 | |
| 10 | P5 | < 130 | 96 | 109 | 113 | 120 | 60 | 69 | 73 | 81 |
| P10 | 130–133 | 97 | 110 | 114 | 121 | 61 | 70 | 73 | 82 | |
| P25 | 134–138 | 99 | 112 | 116 | 123 | 62 | 71 | 75 | 83 | |
| P50 | 139–143 | 100 | 113 | 117 | 124 | 63 | 72 | 76 | 84 | |
| P75 | 144–147 | 101 | 115 | 119 | 126 | 63 | 73 | 76 | 85 | |
| P90 | 148–151 | 103 | 116 | 120 | 128 | 63 | 73 | 77 | 85 | |
| P95 | ≥ 152 | 103 | 117 | 121 | 129 | 64 | 73 | 77 | 86 | |
| 11 | P5 | < 136 | 98 | 112 | 115 | 122 | 62 | 71 | 75 | 83 |
| P10 | 136–139 | 99 | 113 | 116 | 123 | 62 | 72 | 75 | 84 | |
| P25 | 140–144 | 101 | 114 | 118 | 125 | 63 | 73 | 76 | 85 | |
| P50 | 145–149 | 102 | 116 | 120 | 127 | 64 | 73 | 77 | 86 | |
| P75 | 150–154 | 103 | 117 | 121 | 128 | 64 | 74 | 77 | 86 | |
| P90 | 155–157 | 104 | 118 | 122 | 129 | 64 | 74 | 77 | 86 | |
| P95 | ≥ 158 | 104 | 118 | 122 | 130 | 64 | 74 | 77 | 86 | |
| 12 | P5 | < 142 | 100 | 113 | 117 | 124 | 63 | 73 | 76 | 85 |
| P10 | 142–145 | 101 | 114 | 118 | 125 | 63 | 73 | 77 | 85 | |
| P25 | 146–150 | 102 | 116 | 120 | 127 | 64 | 74 | 77 | 86 | |
| P50 | 151–154 | 103 | 117 | 121 | 129 | 64 | 74 | 78 | 86 | |
| P75 | 155–158 | 104 | 118 | 122 | 130 | 64 | 74 | 78 | 87 | |
| P90 | 159–162 | 105 | 119 | 123 | 130 | 64 | 74 | 78 | 87 | |
| P95 | ≥ 163 | 105 | 119 | 123 | 131 | 64 | 74 | 78 | 87 | |
| 13 | P5 | < 147 | 101 | 115 | 119 | 126 | 64 | 74 | 77 | 86 |
| P10 | 147–149 | 102 | 116 | 120 | 127 | 64 | 74 | 78 | 87 | |
| P25 | 150–153 | 103 | 117 | 121 | 128 | 64 | 74 | 78 | 87 | |
| P50 | 154–157 | 104 | 118 | 122 | 129 | 65 | 74 | 78 | 87 | |
| P75 | 158–161 | 105 | 119 | 123 | 130 | 65 | 74 | 78 | 87 | |
| P90 | 162–164 | 105 | 119 | 123 | 131 | 65 | 74 | 78 | 87 | |
| P95 | ≥ 165 | 105 | 119 | 123 | 131 | 65 | 75 | 78 | 87 | |
| 14 | P5 | < 149 | 102 | 116 | 120 | 127 | 65 | 74 | 78 | 87 |
| P10 | 149–152 | 103 | 117 | 121 | 128 | 65 | 75 | 78 | 87 | |
| P25 | 153–155 | 104 | 118 | 122 | 129 | 65 | 75 | 78 | 87 | |
| P50 | 156–159 | 104 | 118 | 122 | 130 | 65 | 75 | 78 | 87 | |
| P75 | 160–163 | 105 | 119 | 123 | 130 | 65 | 75 | 78 | 87 | |
| P90 | 164–166 | 105 | 119 | 123 | 131 | 65 | 75 | 79 | 87 | |
| P95 | ≥ 167 | 106 | 120 | 124 | 131 | 65 | 75 | 79 | 88 | |
| 15 | P5 | < 151 | 103 | 116 | 120 | 128 | 65 | 75 | 79 | 87 |
| P10 | 151–152 | 103 | 117 | 121 | 128 | 65 | 75 | 79 | 88 | |
| P25 | 153–156 | 104 | 118 | 122 | 129 | 65 | 75 | 79 | 88 | |
| P50 | 157–160 | 105 | 119 | 123 | 130 | 65 | 75 | 79 | 88 | |
| P75 | 161–163 | 105 | 119 | 123 | 131 | 65 | 75 | 79 | 88 | |
| P90 | 164–166 | 105 | 120 | 124 | 131 | 65 | 75 | 79 | 88 | |
| P95 | ≥ 167 | 106 | 120 | 124 | 131 | 65 | 75 | 79 | 88 | |
| 16 | P5 | < 151 | 103 | 117 | 121 | 128 | 65 | 75 | 79 | 88 |
| P10 | 151–153 | 103 | 117 | 121 | 129 | 65 | 75 | 79 | 88 | |
| P25 | 154–157 | 104 | 118 | 122 | 130 | 65 | 75 | 79 | 88 | |
| P50 | 158–160 | 105 | 119 | 123 | 130 | 65 | 75 | 79 | 88 | |
| P75 | 161–164 | 105 | 119 | 123 | 131 | 66 | 76 | 79 | 88 | |
| P90 | 165–167 | 106 | 120 | 124 | 131 | 66 | 76 | 79 | 88 | |
| P95 | ≥ 168 | 106 | 120 | 124 | 132 | 66 | 76 | 79 | 88 | |
| 17 | P5 | < 152 | 103 | 117 | 121 | 129 | 66 | 76 | 79 | 88 |
| P10 | 152–154 | 104 | 118 | 122 | 129 | 66 | 76 | 79 | 89 | |
| P25 | 155–157 | 104 | 118 | 122 | 130 | 66 | 76 | 80 | 89 | |
| P50 | 158–161 | 105 | 119 | 123 | 130 | 66 | 76 | 80 | 89 | |
| P75 | 162–164 | 105 | 119 | 124 | 131 | 66 | 76 | 80 | 89 | |
| P90 | 165–167 | 106 | 120 | 124 | 132 | 66 | 76 | 80 | 89 | |
| P95 | ≥ 168 | 106 | 120 | 124 | 132 | 66 | 76 | 80 | 89 | |
Footnotes
Announcement of conflict of interest (This list is in no particular order.): During the revision of this guideline, AstraZeneca Investment (China) Co., Ltd., Bayer Health Care Co., Ltd., Beijing Double-Crane Pharmaceutical Co., Ltd., Sinopharm Holding Distribution Co., Ltd., Hanhui Pharmaceutical Co., Ltd., Hangzhou MSD Pharmaceutical Co., Ltd., Lepu Pharmaceutical Technology Co., Ltd., Merck Serono Co., Ltd., Sanofi (Hangzhou) Pharmaceutical Co., Ltd., Shenzhen Salubris Pharmaceutical Co., Ltd., Servier (Tianjin) Pharmaceutical Co., Ltd., Tianjin Tanabe Pharmaceutical Co., Ltd., Tibet Kangzhe Pharmaceutical Development Co., Ltd., Nanjing Chia Tai Tianqing Pharmaceutical Co., Ltd., Jiangsu Simcere Pharmaceutical Co., Ltd., Beijing Nuohe Xinkang Gene Technology Co., Ltd., and Beijing Precision Health Management of Hypertension & Angiocardiopathy Co., Ltd. supported the conferences of revision, but did not participate in or influence the guideline's academic content and evidence review. The guideline remains independent.
References
- 1.Wang Z, Chen Z, Zhang L, et al. Status of Hypertension in China: results from the China hypertension survey, 2012–2015. Circulation. 2018;137:2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 2.Li LM, Rao KQ, Kong LZ, et al. [Survey on Nutrition and Health Status of Chinese Residents in 2002] Chin J Epidemiol. 2005;26:478–484. [In Chinese] [PubMed] [Google Scholar]
- 3.Hu YS, Yao CH, Wang WZ, et al. [Prevalence of hypertension in some ethnic groups in China in 2002] Wei Sheng Yan Jiu. 2006;35:573–575. [In Chinese] [PubMed] [Google Scholar]
- 4.Gu D, Wildman RP, Wu X, et al. Incidence and predictors of hypertension over 8 years among Chinese men and women. J Hypertens. 2007;25:517–523. doi: 10.1097/HJH.0b013e328013e7f4. [DOI] [PubMed] [Google Scholar]
- 5.Lewington S, Lacey B, Clarke R, et al. The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176:524–532. doi: 10.1001/jamainternmed.2016.0190. [DOI] [PubMed] [Google Scholar]
- 6.Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–2686. doi: 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 7.Fan GH, Wang ZW, Zhang LF, et al. [Survey of prevalence, awareness, treatment rate and control rate of hypertension in rural areas in four northern districts in 2013] Chine J Med. 2015;95:616–620. [In Chinese] [PubMed] [Google Scholar]
- 8.Yang L, Yan J, Tang X, et al. Prevalence, awareness, teatment, control and risk factors associated with hypertension among adults in Southern China, 2013. PLoS One. 2016;11:e0146181. doi: 10.1371/journal.pone.0146181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gu H, Li W, Yang J, et al. Hypertension prevalence, awareness, treatment and control among Han and four ethnic minorities (Uygur, Hui, Mongolian and Dai) in China. J Hum Hypertens. 2015;29:555–560. doi: 10.1038/jhh.2014.123. [DOI] [PubMed] [Google Scholar]
- 10.Wang G, Li LM, Hu YH, et al. [Study on the relationship between risk factors and risk of hypertension in community population in Shanghai] Chin J Epidemiol. 2013;34:307–310. [In Chinese] [Google Scholar]
- 11.Gu D, Gupta A, Muntner P, et al. Prevalence of cardiovascular disease risk factor clustering among the adult population of China: results from the International Collaborative Study of Cardiovascular Disease in Asia (InterAsia) Circulation. 2005;112:658–665. doi: 10.1161/CIRCULATIONAHA.104.515072. [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Feng X, Zhang M, et al. Clustering of cardiovascular behavioral risk factors and blood pressure among people diagnosed with hypertension: a nationally representative survey in China. Sci Rep. 2016;6:27627. doi: 10.1038/srep27627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ying CQ, Fu SB, Xu Q, et al. Multiple risk factor clustering and risk of hypertension in the Mongolian ethnic population of China. Biomed Environ Sci. 2007;20:381–385. [PubMed] [Google Scholar]
- 14.Elliott P, Stamler J, Nichols R, et al. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996;312:1249–1253. doi: 10.1136/bmj.312.7041.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Health and Family Planning Commission Disease Prevention and Control Bureau. [Report on Nutrition and Chronic Disease Status of Chinese Residents (2015)] Beijing: People's Medical Publishing House; 2015. pp. 33–50. [In Chinese] [Google Scholar]
- 16.Liu Z. Dietary sodium and the incidence of hypertension in the Chinese population: a review of nationwide surveys. Am J Hypertens. 2009;22:929–933. doi: 10.1038/ajh.2009.134. [DOI] [PubMed] [Google Scholar]
- 17.Global BMIMC. Di Angelantonio E, Bhupathiraju Sh N, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–786. doi: 10.1016/S0140-6736(16)30175-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang ZW, Hao G, Wang X, et al. [Aggregation analysis of overweight/obesity and cardiovascular risk factors in middle-aged population in China] Chin J Hypertens. 2014;35:1000. [In Chinese] [Google Scholar]
- 19.Feng BY, Chen JC, Li Y, et al. [A follow-up study on the relationship between overweight and obesity and hypertension in Chinese adults] Chin J Epidemiol. 2016;37:606–611. [In Chinese] [Google Scholar]
- 20.Wang Z, Zeng X, Chen Z, et al. Association of visceral and total body fat with hypertension and prehypertension in a middle-aged Chinese population. J Hypertens. 2015;33:1555–1562. doi: 10.1097/HJH.0000000000000602. [DOI] [PubMed] [Google Scholar]
- 21.Fox CS, Massaro JM, Hoffmann U, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007;116:39–48. doi: 10.1161/CIRCULATIONAHA.106.675355. [DOI] [PubMed] [Google Scholar]
- 22.Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–1127. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 23.Holmes MV, Dale CE, Zuccolo L, et al. Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data. BMJ. 2014;349:g4164. doi: 10.1136/bmj.g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lambert E, Dawood T, Straznicky N, et al. Association between the sympathetic firing pattern and anxiety level in patients with the metabolic syndrome and elevated blood pressure. J Hypertens. 2010;28:543–550. doi: 10.1097/HJH.0b013e3283350ea4. [DOI] [PubMed] [Google Scholar]
- 25.Bajko Z, Szekeres CC, Kovacs KR, et al. Anxiety, depression and autonomic nervous system dysfunction in hypertension. J Neurol Sci. 2012;317:112–116. doi: 10.1016/j.jns.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 26.Pan Y, Cai W, Cheng Q, et al. Association between anxiety and hypertension: a systematic review and meta-analysis of epidemiological studies. Neuropsychiatr Dis Treat. 2015;11:1121–1130. doi: 10.2147/NDT.S77710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dong GH, Qian ZM, Xaverius PK, et al. Association between long-term air pollution and increased blood pressure and hypertension in China. Hypertension. 2013;61:578–584. doi: 10.1161/HYPERTENSIONAHA.111.00003. [DOI] [PubMed] [Google Scholar]
- 28.Shang Y, Sun Z, Cao J, et al. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ Int. 2013;54:100–111. doi: 10.1016/j.envint.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 29.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 30.Lawes CM, Rodgers A, Bennett DA, et al. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003;21:707–716. doi: 10.1097/00004872-200304000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Lloyd-Jones DM, Larson MG, Leip EP, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 32.Conen D, Tedrow UB, Koplan BA, et al. Influence of systolic and diastolic blood pressure on the risk of incident atrial fibrillation in women. Circulation. 2009;119:2146–2152. doi: 10.1161/CIRCULATIONAHA.108.830042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klag MJ, Whelton PK, Randall BL, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334:13–18. doi: 10.1056/NEJM199601043340103. [DOI] [PubMed] [Google Scholar]
- 34.Dolan E, Stanton A, Thijs L, et al. Superiority of ambulatory over clinic blood pressure measurement in predicting mortality: the Dublin outcome study. Hypertension. 2005;46:156–161. doi: 10.1161/01.HYP.0000170138.56903.7a. [DOI] [PubMed] [Google Scholar]
- 35.Johansson JK, Niiranen TJ, Puukka PJ, et al. Prognostic value of the variability in home-measured blood pressure and heart rate: the Finn-Home Study. Hypertension. 2012;59:212–218. doi: 10.1161/HYPERTENSIONAHA.111.178657. [DOI] [PubMed] [Google Scholar]
- 36.Chen WW, Gao RL, Liu LS, et al. [Summary of China Cardiovascular Disease Report 2016] Chin J Circulation. 2017;32 [In Chinese] [Google Scholar]
- 37.ACCORD Study Group. Cushman WC, Evans GW, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.SPRINT Research Group. Wright JT, Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang JG, Staessen JA, Gong L, et al. Chinese trial on isolated systolic hypertension in the elderly. Systolic Hypertension in China (Syst-China) Collaborative Group. Arch Intern Med. 2000;160:211–220. doi: 10.1001/archinte.160.2.211. [DOI] [PubMed] [Google Scholar]
- 40.Liu L, Zhang Y, Liu G, et al. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens. 2005;23:2157–2172. doi: 10.1097/01.hjh.0000194120.42722.ac. [DOI] [PubMed] [Google Scholar]
- 41.Huo Y, Li J, Qin X, et al. Efficacy of folic acid therapy in primary prevention of stroke among adults with hypertension in China: the CSPPT randomized clinical trial. JAMA. 2015;313:1325–1335. doi: 10.1001/jama.2015.2274. [DOI] [PubMed] [Google Scholar]
- 42.Kato N, Takeuchi F, Tabara Y, et al. Meta-analysis of genome-wide association studies identifies common variants associated with blood pressure in East Asians. Nat Genet. 2011;43:531–538. doi: 10.1038/ng.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gao PJ, Zhang KX, Zhu DL, et al. Diagnosis of Liddle syndrome by genetic analysis of β and γ subunits of epithelial sodium channel-a report of five affected family members. J Hypertens. 2001;19:885–889. doi: 10.1097/00004872-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Mulatero P, Morello F, Veglio F, et al. Genetics of primary aldosteronism. J Hypertens. 2004;22:663–670. doi: 10.1097/00004872-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 45.Parati G, Stergiou G, O'Brien E, et al. European Society of Hypertension practice guidelines for ambulatory blood pressure monitoring. J Hypertens. 2014;32:1359–1366. doi: 10.1097/HJH.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 46.Stergiou GS, Siontis KC, Ioannidis JP, et al. Home blood pressure as a cardiovascular outcome predictor: it's time to take this method seriously. Hypertension. 2010;55:1301–1303. doi: 10.1161/HYPERTENSIONAHA.110.150771. [DOI] [PubMed] [Google Scholar]
- 47.Myers MG, Godwin M. Automated office blood pressure. Can J Cardiol. 2012;28:341–346. doi: 10.1016/j.cjca.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 48.Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension guidelines for blood pressure monitoring at home: a summary report of the Second International Consensus Conference on Home Blood Pressure Monitoring. J Hypertens. 2008;26:1505–1526. doi: 10.1097/HJH.0b013e328308da66. [DOI] [PubMed] [Google Scholar]
- 49.Chinese Medical Association Hypertension Professional Committee. [Family blood pressure monitoring Chinese expert consensus] Chin Clin. 2012:69–72. [In Chinese] [Google Scholar]
- 50.Schillaci G, Battista F, Pucci G, et al. A review of the role of electrocardiography in the diagnosis of left ventricular hypertrophy in hypertension. J Electrocardiol. 2012;45:617–623. doi: 10.1016/j.jelectrocard.2012.08.051. [DOI] [PubMed] [Google Scholar]
- 51.Agrawal B, Berger A, Wolf K, et al. Microalbuminuria screening by reagent strip predicts cardiovascular risk in hypertension. J Hypertens. 1996;14:223–228. doi: 10.1097/00004872-199602000-00011. [DOI] [PubMed] [Google Scholar]
- 52.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 54.Ma YC, Zuo L, Chen JH, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–2944. doi: 10.1681/ASN.2006040368. [DOI] [PubMed] [Google Scholar]
- 55.Bos MJ, Koudstaal PJ, Hofman A, et al. Uric acid is a risk factor for myocardial infarction and stroke: the Rotterdam study. Stroke. 2006;37:1503–1507. doi: 10.1161/01.STR.0000221716.55088.d4. [DOI] [PubMed] [Google Scholar]
- 56.O'Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14–22. doi: 10.1056/NEJM199901073400103. [DOI] [PubMed] [Google Scholar]
- 57.Polak JF, Pencina MJ, Pencina KM, et al. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. 2011;365:213–221. doi: 10.1056/NEJMoa1012592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vlachopoulos C, Aznaouridis K, Stefanadis C, et al. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol. 2010;55:1318–1327. doi: 10.1016/j.jacc.2009.10.061. [DOI] [PubMed] [Google Scholar]
- 59.Laurent S, Cockcroft J, Van Bortel L, et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254. [DOI] [PubMed] [Google Scholar]
- 60.Murabito JM, Evans JC, Larson MG, et al. The ankle-brachial index in the elderly and risk of stroke, coronary disease, and death: the Framingham Study. Arch Intern Med. 2003;163:1939–1942. doi: 10.1001/archinte.163.16.1939. [DOI] [PubMed] [Google Scholar]
- 61.Breslin DJ, Gifford RW, Jr, Fairbairn JF, et al. Prognostic importance of ophthalmoscopic findings in essential hypertension. JAMA. 1966;195:335–338. [PubMed] [Google Scholar]
- 62.Lehmann MV, Schmieder RE. Remodeling of retinal small arteries in hypertension. Am J Hypertens. 2011;24:1267–1273. doi: 10.1038/ajh.2011.166. [DOI] [PubMed] [Google Scholar]
- 63.Longstreth WT, Jr, Manolio TA, Arnold A, et al. Clinical correlates of white matter findings on cranial magnetic resonance imaging of 3301 elderly people. The Cardiovascular Health Study. Stroke. 1996;27:1274–1282. doi: 10.1161/01.str.27.8.1274. [DOI] [PubMed] [Google Scholar]
- 64.[Guidelines for the Prevention and Treatment of Hypertension in China] Revised 2005. Beijing: People's Medical Publishing House; 2006. Revision Committee of the Guidelines for the Prevention and Treatment of Hypertension in China. [In Chinese] [Google Scholar]
- 65.Committee on Prevention and Treatment of Hypertension in China. [China's Guidelines for the Prevention and Treatment of Hypertension] Revised 2010. Beijing: People's Medical Publishing House; 2012. [In Chinese] [Google Scholar]
- 66.Zhang Y, Zhang X, Liu L, et al. Is a systolic blood pressure target < 140 mmHg indicated in all hypertensives? Subgroup analyses of findings from the randomized FEVER trial. Euro Heart J. 2011;32:1500–1508. doi: 10.1093/eurheartj/ehr039. [DOI] [PubMed] [Google Scholar]
- 67.Lonn EM, Bosch J, Lopez-Jaramillo P, et al. Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374:2009–2020. doi: 10.1056/NEJMoa1600175. [DOI] [PubMed] [Google Scholar]
- 68.Fox KM. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study) Lancet. 2003;362:782–788. doi: 10.1016/s0140-6736(03)14286-9. [DOI] [PubMed] [Google Scholar]
- 69.Staessen JA, Fagard R, Thijs L, et al. Randomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertension. The Systolic Hypertension in Europe (Syst-Eur) Trial Investigators. Lancet. 1997;350:757–764. doi: 10.1016/s0140-6736(97)05381-6. [DOI] [PubMed] [Google Scholar]
- 70.Beckett NS, Peters R, Fletcher AE, et al. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 71.Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2, Short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet. 1990;335:827–838. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 72.Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet. 2000;355:865–872. doi: 10.1016/s0140-6736(99)07330-4. [DOI] [PubMed] [Google Scholar]
- 73.Elliott P, Stamler J, Nichols R, et al. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996;312:1249–1253. doi: 10.1136/bmj.312.7041.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. doi: 10.1136/bmj.f1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 76.Zhao Q, Gu D, Chen J, et al. Blood pressure responses to dietary sodium and potassium interventions and the cold pressor test: the GenSalt replication study in rural North China. Am J Hypertens. 2014;27:72–80. doi: 10.1093/ajh/hpt163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–634. doi: 10.1056/NEJMoa1304127. [DOI] [PubMed] [Google Scholar]
- 78.CSSSC G. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007;25:2011–2018. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 79.ICR G. Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ. 1988;297:319–328. doi: 10.1136/bmj.297.6644.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–1124. doi: 10.1056/NEJM199704173361601. [DOI] [PubMed] [Google Scholar]
- 81.Saneei P, Salehi-Abargouei A, Esmaillzadeh A, et al. Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. NMCD. 2014;24:1253–1261. doi: 10.1016/j.numecd.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 82.Struijk EA, May AM, Wezenbeek NL, et al. Adherence to dietary guidelines and cardiovascular disease risk in the EPIC-NL cohort. Inter J Cardiol. 2014;176:354–359. doi: 10.1016/j.ijcard.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 83.Fung TT, Chiuve SE, McCullough ML, et al. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008;168:713–720. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 84.Neter JE, Stam BE, Kok FJ, et al. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–884. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 85.China Obesity Working Group Data Summary Analysis Collaborative Group. [Predictive value of adult body mass index and waist circumference for risk factors associated with disease: a study of appropriate body mass index and waist circumference] Chin J Epidemiol. 2002;23:5–10. [In Chinese] [Google Scholar]
- 86.Aucott L, Rothnie H, McIntyre L, et al. Long-term weight loss from lifestyle intervention benefits blood pressure?: a systematic review. Hypertension. 2009;54:756–762. doi: 10.1161/HYPERTENSIONAHA.109.135178. [DOI] [PubMed] [Google Scholar]
- 87.Chen Z, Peto R, Zhou M, et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. 2015;386:1447–1456. doi: 10.1016/S0140-6736(15)00340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Clair C, Rigotti NA, Porneala B, et al. Association of smoking cessation and weight change with cardiovascular disease among adults with and without diabetes. JAMA. 2013;309:1014–1021. doi: 10.1001/jama.2013.1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Peng M, Wu S, Jiang X, et al. Long-term alcohol consumption is an independent risk factor of hypertension development in northern China: evidence from Kailuan study. J Hypertens. 2013;31:2342–2347. doi: 10.1097/HJH.0b013e3283653999. [DOI] [PubMed] [Google Scholar]
- 90.Zhao J, Stockwell T, Roemer A, et al. Alcohol consumption and mortality from coronary heart disease: an updated meta-analysis of cohort studies. J Stud Alcohol Drugs. 2017;78:375–386. doi: 10.15288/jsad.2017.78.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Cushman WC, Cutler JA, Hanna E, et al. Prevention and Treatment of Hypertension Study (PATHS): effects of an alcohol treatment program on blood pressure. Arch Intern Med. 1998;158:1197–1207. doi: 10.1001/archinte.158.11.1197. [DOI] [PubMed] [Google Scholar]
- 92.Tanasescu M, Leitzmann MF, Rimm EB, et al. Exercise type and intensity in relation to coronary heart disease in men. JAMA. 2002;288:1994–2000. doi: 10.1001/jama.288.16.1994. [DOI] [PubMed] [Google Scholar]
- 93.Engstrom G, Hedblad B, Janzon L, et al. Hypertensive men who exercise regularly have lower rate of cardiovascular mortality. J Hypertens. 1999;17:737–742. doi: 10.1097/00004872-199917060-00003. [DOI] [PubMed] [Google Scholar]
- 94.Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 95.Landsbergis PA, Dobson M, Koutsouras G, et al. Job strain and ambulatory blood pressure: a meta-analysis and systematic review. Am J Public Health. 2013;103:e61–e71. doi: 10.2105/AJPH.2012.301153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Elmer PJ, Obarzanek E, Vollmer WM, et al. Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med. 2006;144:485–495. doi: 10.7326/0003-4819-144-7-200604040-00007. [DOI] [PubMed] [Google Scholar]
- 97.Cook NR, Cutler JA, Obarzanek E, et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP) BMJ. 2007;334:885–888. doi: 10.1136/bmj.39147.604896.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dickinson HO, Mason JM, Nicolson DJ, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–233. doi: 10.1097/01.hjh.0000199800.72563.26. [DOI] [PubMed] [Google Scholar]
- 99.He J, Whelton PK, Appel LJ, et al. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35:544–549. doi: 10.1161/01.hyp.35.2.544. [DOI] [PubMed] [Google Scholar]
- 100.Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich) 2014;16:14–26. doi: 10.1111/jch.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.The Hypertension Group in Chinese Society of Cardiology. [2015 Chinese expert guidance on the management of salt intake to control hypertension] Chin J Hypertens. 2015;23:1028–1034. [In Chinese] [Google Scholar]
- 102.Chen X, Guo X, Ma J, et al. Urinary sodium or potassium excretion and blood pressure in adults of Shandong province, China: preliminary results of the SMASH project. JASH. 2015;9:754–762. doi: 10.1016/j.jash.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 103.Anderson CA, Appel LJ, Okuda N, et al. Dietary sources of sodium in China, Japan, the United Kingdom, and the United States, women and men aged 40 to 59 years: the INTERMAP study. J Am Diet Assoc. 2010;110:736–745. doi: 10.1016/j.jada.2010.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.China Obesity Working Group Data Summary Analysis Collaborative Group. [Predictive value of Chinese adult body mass index and waist circumference for risk factors of related diseases: a study of appropriate body mass index and waist cut point] Chin J Epidemiol. 2003;23:5–10. [In Chinese] [Google Scholar]
- 105.Department of Disease Control, Ministry of Health of the People's Republic of China. [Guidelines for Prevention and Control of Overweight and Obesity in Adults in China] Beijing: People's Medical Publishing House; 2006. [In Chinese] [Google Scholar]
- 106.Douketis JD, Macie C, Thabane L, et al. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. Int J obes (Lond) 2005;29:1153–1167. doi: 10.1038/sj.ijo.0802982. [DOI] [PubMed] [Google Scholar]
- 107.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes Care. 2011;34:1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Malek AM, Cushman M, Lackland DT, et al. Secondhand Smoke Exposure and Stroke: The Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Prev Med. 2015;49:e89–e97. doi: 10.1016/j.amepre.2015.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Primatesta P, Falaschetti E, Gupta S, et al. Association between smoking and blood pressure: evidence from the health survey for England. Hypertension. 2001;37:187–193. doi: 10.1161/01.hyp.37.2.187. [DOI] [PubMed] [Google Scholar]
- 110.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31:1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 111.Leung AA, Nerenberg K, Daskalopoulou SS, et al. Hypertension Canada's 2016 Canadian Hypertension Education Program Guidelines for Blood Pressure Measurement, Diagnosis, Assessment of Risk, Prevention, and Treatment of Hypertension. Can J Cardiol. 2016;32:569–588. doi: 10.1016/j.cjca.2016.02.066. [DOI] [PubMed] [Google Scholar]
- 112.Okin PM, Oikarinen L, Viitasalo M, et al. Prognostic value of changes in the electrocardiographic strain pattern during antihypertensive treatment: the Losartan Intervention for End-Point Reduction in Hypertension Study (LIFE) Circulation. 2009;119:1883–1891. doi: 10.1161/CIRCULATIONAHA.108.812313. [DOI] [PubMed] [Google Scholar]
- 113.Parving HH, Lehnert H, Brochner-Mortensen J, et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med. 2001;345:870–878. doi: 10.1056/NEJMoa011489. [DOI] [PubMed] [Google Scholar]
- 114.Zong WZ, Yang WY, Xiang HD, et al. [Efficacy and safety of irbesartan in the treatment of type 2 diabetes with albuminuria: a multicenter randomized double-blind controlled study] Chin J Endocrinol Metabol. 2008;24:55–58. [In Chinese] [Google Scholar]
- 115.Lewis EJ, Hunsicker LG, Clarke WR, et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345:851–860. doi: 10.1056/NEJMoa011303. [DOI] [PubMed] [Google Scholar]
- 116.Department of Hypertension, Chinese Medical Association Cardiovascular Disease Branch. [Chinese expert guidance for early morning blood pressure clinical management] Chin J Cardiovasc Diseases. 2014;42:721–725. [In Chinese] [Google Scholar]
- 117.Brown MJ, Palmer CR, Castaigne A, et al. Morbidity and mortality in patients randomised to double-blind treatment with a long-acting calcium-channel blocker or diuretic in the International Nifedipine GITS study: Intervention as a Goal in Hypertension Treatment (INSIGHT) Lancet. 2000;356:366–372. doi: 10.1016/S0140-6736(00)02527-7. [DOI] [PubMed] [Google Scholar]
- 118.Kario K, Saito I, Kushiro T, et al. Home blood pressure and cardiovascular outcomes in patients during antihypertensive therapy: primary results of HONEST, a large-scale prospective, real-world observational study. Hypertension. 2014;64:989–996. doi: 10.1161/HYPERTENSIONAHA.114.04262. [DOI] [PubMed] [Google Scholar]
- 119.Weber MA, Julius S, Kjeldsen SE, et al. Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet. 2004;363:2049–2051. doi: 10.1016/S0140-6736(04)16456-8. [DOI] [PubMed] [Google Scholar]
- 120.Wang W, Ma LY, Liu MB, et al. [Phase report on the effect of initial low-dose amlodipine plus telmisartan or compound amiloride on blood pressure control rate in patients with hypertension] Chin J Cardiovasc Diseases. 2009;25:701–707. [In Chinese] [Google Scholar]
- 121.Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. New Engl J Med. 2008;359:2417–2428. doi: 10.1056/NEJMoa0806182. [DOI] [PubMed] [Google Scholar]
- 122.Patel A, MacMahon S, Chalmers J, et al. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370:829–840. doi: 10.1016/S0140-6736(07)61303-8. [DOI] [PubMed] [Google Scholar]
- 123.Wang W, Ma L, Zhang Y, et al. The combination of amlodipine and angiotensin receptor blocker or diuretics in high-risk hypertensive patients: rationale, design and baseline characteristics. J Hum Hypertens. 2011;25:271–277. doi: 10.1038/jhh.2010.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Staessen JA, Wang JG, Thijs L, et al. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet. 2001;358:1305–1315. doi: 10.1016/S0140-6736(01)06411-X. [DOI] [PubMed] [Google Scholar]
- 125.Neal B, MacMahon S, Chapman N, et al. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet. 2000;356:1955–1964. doi: 10.1016/s0140-6736(00)03307-9. [DOI] [PubMed] [Google Scholar]
- 126.Ogihara T, Saruta T, Rakugi H, et al. Target blood pressure for treatment of isolated systolic hypertension in the elderly: valsartan in elderly isolated systolic hypertension study. Hypertension. 2010;56:196–202. doi: 10.1161/HYPERTENSIONAHA.109.146035. [DOI] [PubMed] [Google Scholar]
- 127.Liu L, Wang JG, Gong L, et al. Comparison of active treatment and placebo in older Chinese patients with isolated systolic hypertension. Systolic Hypertension in China (Syst-China) Collaborative Group. J Hypertens. 1998;16:1823–1829. doi: 10.1097/00004872-199816120-00016. [DOI] [PubMed] [Google Scholar]
- 128.Gong L, Zhang W, Zhu Y, et al. Shanghai trial of nifedipine in the elderly (STONE) J Hypertens. 1996;14:1237–1245. doi: 10.1097/00004872-199610000-00013. [DOI] [PubMed] [Google Scholar]
- 129.Zhang TJ. [Hypertensive intervention trial a randomized controlled trial of nifedipine and placebo] Chin J Cardiovasc Diseases. 1994;201–5 [In Chinese] [Google Scholar]
- 130.PATS Collaborating Group. Post-stroke antihypertensive treatment study. A preliminary result. Chin Med J. 1995;108:710–717. [PubMed] [Google Scholar]
- 131.Liu L, Wang Z, Gong L, et al. Blood pressure reduction for the secondary prevention of stroke: a Chinese trial and a systematic review of the literature. Hypertens Res. 2009;32:1032–1040. doi: 10.1038/hr.2009.139. [DOI] [PubMed] [Google Scholar]
- 132.PROGRESS Collaborative Group. Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet. 2001;358:1033–1041. doi: 10.1016/S0140-6736(01)06178-5. [DOI] [PubMed] [Google Scholar]
- 133.Arima H, Anderson C, Omae T, et al. Perindopril-based blood pressure lowering reduces major vascular events in Asian and Western participants with cerebrovascular disease: the PROGRESS trial. J Hypertens. 2010;28:395–400. doi: 10.1097/HJH.0b013e328333b009. [DOI] [PubMed] [Google Scholar]
- 134.Arima H, Anderson C, Omae T, et al. Degree of blood pressure reduction and recurrent stroke: the PROGRESS trial. J Neurol Neurosurg Psychiatry. 2014;85:1284–1285. doi: 10.1136/jnnp-2014-307856. [DOI] [PubMed] [Google Scholar]
- 135.Liu LS, Gong LS, Wang W, et al. [A multicenter randomized, double-blind, controlled clinical trial of antihypertensive therapy for stroke recurrence in Chinese patients with cerebrovascular disease] Chin J Cardiovasc Diseases. 2005;33:613–617. [In Chinese] [Google Scholar]
- 136.Bostom AG, Rosenberg IH, Silbershatz H, et al. Nonfasting plasma total homocysteine levels and stroke incidence in elderly persons: the Framingham Study. Ann Intern Med. 1999;131:352–355. doi: 10.7326/0003-4819-131-5-199909070-00006. [DOI] [PubMed] [Google Scholar]
- 137.Zhou XL, Hu AH, Hui YT, et al. [Relationship between MTHFR gene polymorphism and plasma homocysteine levels and stroke] Chin J Cardiovasc Disease. 1999;27:121–123. [In Chinese] [Google Scholar]
- 138.Zhang W, Sun K, Chen J, et al. High plasma homocysteine levels contribute to the risk of stroke recurrence and all cause mortality in a large prospective stroke population. Clin Sci (Lond) 2010;118:187–194. doi: 10.1042/CS20090142. [DOI] [PubMed] [Google Scholar]
- 139.Mark SD, Wang W, Fraumeni JF, Jr, et al. Lowered risks of hypertension and cerebrovascular disease after vitamin/mineral supplementation: the Linxian Nutrition Intervention Trial. Am J Epidemiol. 1996;143:658–664. doi: 10.1093/oxfordjournals.aje.a008798. [DOI] [PubMed] [Google Scholar]
- 140.Zhao M, Wu G, Li Y, et al. Meta-analysis of folic acid efficacy trials in stroke prevention: Insight into effect modifiers. Neurology. 2017;88:1830–1838. doi: 10.1212/WNL.0000000000003909. [DOI] [PubMed] [Google Scholar]
- 141.Xu X, Qin X, Li Y, et al. Efficacy of folic acid therapy on the progression of chronic kidney disease: the renal substudy of the China stroke primary prevention trial. JAMA Intern Med. 2016;176:1443–1450. doi: 10.1001/jamainternmed.2016.4687. [DOI] [PubMed] [Google Scholar]
- 142.Qin X, Li Y, He M, et al. Folic acid therapy reduces serum uric acid in hypertensive patients: a substudy of the China Stroke Primary Prevention Trial (CSPPT) Am J Clin Nutr. 2017;105:882–889. doi: 10.3945/ajcn.116.143131. [DOI] [PubMed] [Google Scholar]
- 143.Cooper-DeHoff RM, Gong Y, Handberg EM, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304:61–68. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Wang W, Wang JG, Zhang YQ, et al. [To formulate strategies and programs for prevention and treatment of hypertension in China according to the characteristics of hypertension in China] Chin J Hypertens. 2010;904–907 [In Chinese] [Google Scholar]
- 145.Wang JG, Li Y, Franklin SS, et al. Prevention of stroke and myocardial infarction by amlodipine and Angiotensin receptor blockers: a quantitative overview. Hypertension. 2007;50:181–188. doi: 10.1161/HYPERTENSIONAHA.107.089763. [DOI] [PubMed] [Google Scholar]
- 146.Wang JG, Kario K, Lau T, et al. Use of dihydropyridine calcium channel blockers in the management of hypertension in Eastern Asians: a scientific statement from the Asian Pacific Heart Association. Hypertensi Res. 2011;34:423–430. doi: 10.1038/hr.2010.259. [DOI] [PubMed] [Google Scholar]
- 147.Mancia G, Parati G, Bilo G, et al. Blood pressure control by the nifedipine GITS-telmisartan combination in patients at high cardiovascular risk: the TALENT study. J Hypertens. 2011;29:600–609. doi: 10.1097/HJH.0b013e328342ef04. [DOI] [PubMed] [Google Scholar]
- 148.Nissen SE, Tuzcu EM, Libby P, et al. Effect of antihypertensive agents on cardiovascular events in patients with coronary disease and normal blood pressure: the CAMELOT study: a randomized controlled trial. JAMA. 2004;292:2217–2225. doi: 10.1001/jama.292.18.2217. [DOI] [PubMed] [Google Scholar]
- 149.Elliott HL, Meredith PA. Preferential benefits of nifedipine GITS in systolic hypertension and in combination with RAS blockade: further analysis of the ‘ACTION’ database in patients with angina. J Hum Hypertens. 2011;25:63–70. doi: 10.1038/jhh.2010.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Experts Association of Angiotensin-Converting Enzyme Inhibitors Correctly Applied in Kidney Diseases. [Expert consensus on the correct application of angiotensin-converting enzyme inhibitors in kidney disease] Chin J Nephrol. 2006:57–58. [In Chinese] [Google Scholar]
- 151.Danchin N, Cucherat M, Thuillez C, et al. [Angiotensin-converting enzyme inhibitors in patients with coronary artery disease and absence of heart failure or left ventricular systolic dysfunction: an overview of long-term randomized controlled trials. Arch Intern Med. 2006;166:787–796. doi: 10.1001/archinte.166.7.787. [DOI] [PubMed] [Google Scholar]
- 152.Yusuf S, Teo KK, Pogue J, et al. Telmisartan, ramipril, or both in patients at high risk for vascular events. N Engl J Med. 2008;358:1547–1559. doi: 10.1056/NEJMoa0801317. [DOI] [PubMed] [Google Scholar]
- 153.Lindholm LH, Ibsen H, Dahlof B, et al. Cardiovascular morbidity and mortality in patients with diabetes in the losartan intervention for endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:1004–1010. doi: 10.1016/S0140-6736(02)08090-X. [DOI] [PubMed] [Google Scholar]
- 154.Coyle D, Rodby R, Soroka S, et al. Cost-effectiveness of irbesartan 300 mg given early versus late in patients with hypertension and a history of type 2 diabetes and renal disease: a Canadian perspective. Clin Ther. 2007;29:1508–1523. doi: 10.1016/j.clinthera.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 155.Park HC, Choi HY, Kim BS, et al. Antiproteinuric effect of losartan in non-diabetic renal disease is not dependent on ACE insertion/deletion polymorphism. Blood Press Res. 2006;29:216–224. doi: 10.1159/000095736. [DOI] [PubMed] [Google Scholar]
- 156.Al Badarin FJ, Abuannadi MA, Lavie CJ, et al. Evidence-based diuretic therapy for improving cardiovascular prognosis in systemic hypertension. Am J Cardiol. 2011;107:1178–1184. doi: 10.1016/j.amjcard.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 157.Cleland JG, Coletta AP, Lammiman M, et al. Clinical trials update from the European Society of Cardiology meeting 2005: CARE-HF extension study, ESSENTIAL, CIBIS-III, S-ICD, ISSUE-2, STRIDE-2, SOFA, IMAGINE, PREAMI, SIRIUS-II and ACTIVE. Eur J Heart Fail. 2005;7:1070–1075. doi: 10.1016/j.ejheart.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 158.Bisoprolol Center Research Collaboration Group. [Effect of domestic bisoprolol on glucose metabolism in patients with type 2 diabetes mellitus] Chin J Intern Med. 2005;503–505 [In Chinese] [Google Scholar]
- 159.Castagno D, Jhund PS, McMurray JJ, et al. Improved survival with bisoprolol in patients with heart failure and renal impairment: an analysis of the cardiac insufficiency bisoprolol study II (CIBIS-II) trial. Eur J Heart Fail. 2010;12:607–616. doi: 10.1093/eurjhf/hfq038. [DOI] [PubMed] [Google Scholar]
- 160.Wikstrand J, Warnold I, Tuomilehto J, et al. Metoprolol versus thiazide diuretics in hypertension. Morbidity results from the MAPHY Study. Hypertension. 1991;17:579–588. doi: 10.1161/01.hyp.17.4.579. [DOI] [PubMed] [Google Scholar]
- 161.Haenni A, Lithell H. Moxonidine improves insulin sensitivity in insulin-resistant hypertensives. J Hypertension Suppl. 1999;17:S29–S35. [PubMed] [Google Scholar]
- 162.Brown MJ, McInnes GT, Papst CC, et al. Aliskiren and the calcium channel blocker amlodipine combination as an initial treatment strategy for hypertension control (ACCELERATE): a randomised, parallel-group trial. Lancet. 2011;377:312–320. doi: 10.1016/S0140-6736(10)62003-X. [DOI] [PubMed] [Google Scholar]
- 163.Oparil S, Yarows SA, Patel S, et al. Efficacy and safety of combined use of aliskiren and valsartan in patients with hypertension: a randomised, double-blind trial. Lancet. 2007;370:221–229. doi: 10.1016/S0140-6736(07)61124-6. [DOI] [PubMed] [Google Scholar]
- 164.Yarows A, Oparil S, Pate S, et al. Aliskiren and valsartan in stage 2 hypertension: subgroup analysis of a randomised, double-blind study. Adv Ther. 2008;25:1288–1302. doi: 10.1007/s12325-008-0123-x. [DOI] [PubMed] [Google Scholar]
- 165.Duprez DA, Munger MA, Botha J, et al. Aliskiren for geritric lowering of systolic hypertension: a randomized controlled trial. J Hum Hypertens. 2010;24:600–608. doi: 10.1038/jhh.2009.107. [DOI] [PubMed] [Google Scholar]
- 166.Franklin SS, Lopez VA, Wong ND, et al. Single versus combined blood pressure components and risk for cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119:243–250. doi: 10.1161/CIRCULATIONAHA.108.797936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Wang HY, Sun NL, Jing S, et al. [Efficacy and safety of compound reserpine triamterene tablets (Bump No. 0) and indapamide in the treatment of patients with essential hypertension Randomized controlled clinical study] Chin J Hypertens. 2016;857–862 [In Chinese] [Google Scholar]
- 168.Jiang XJ, Gao RL. Post-study era of SIMPLICITY HTN 3: The status and challenges of denervation for the treatment of refractory hypertension. Chin J Med. 2014;1761–1763 [Google Scholar]
- 169.White WB, Galis ZS, Henegar J, et al. Renal denervation therapy for hypertension: pathways for moving development forward. J Am Soc Hypertens. 2015;9:341–350. doi: 10.1016/j.jash.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 170.Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet. 2017;390:2160–2170. doi: 10.1016/S0140-6736(17)32281-X. [DOI] [PubMed] [Google Scholar]
- 171.Kandzari DE, Bohm M, Mahfoud F, et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet. 2018;391:2346–2355. doi: 10.1016/S0140-6736(18)30951-6. [DOI] [PubMed] [Google Scholar]
- 172.Bisognano JD, Bakris G, Nadim MK, et al. Baroreflex activation therapy lowers blood pressure in patients with resistant hypertension: results from the double-blind, randomized, placebo-controlled rheos pivotal trial. J Am Coll Cardiol. 2011;58:765–773. doi: 10.1016/j.jacc.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 173.Lobo MD, Sobotka PA, Stanton A, et al. Central arteriovenous anastomosis for the treatment of patients with uncontrolled hypertension (the ROX CONTROL HTN study): a randomised controlled trial. Lancet. 2015;385:1634–1641. doi: 10.1016/S0140-6736(14)62053-5. [DOI] [PubMed] [Google Scholar]
- 174.Zhu JR, Gao RL, Zhao L, et al. [Guidelines for prevention and treatment of dyslipidemia in Chinese adults (revised 2016)] Chin J Circ. 2016;937–953 [In Chinese] [Google Scholar]
- 175.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–1389. [PubMed] [Google Scholar]
- 176.Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 177.Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 178.Serruys PW, de Feyter P, Macaya C, et al. Fluvastatin for prevention of cardiac events following successful first percutaneous coronary intervention: a randomized controlled trial. JAMA. 2002;287:3215–3222. doi: 10.1001/jama.287.24.3215. [DOI] [PubMed] [Google Scholar]
- 179.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22. doi: 10.1016/S0140-6736(02)09327-3. [DOI] [PubMed] [Google Scholar]
- 180.Colhoun HM, Betteridge DJ, Durrington PN, et al. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial. Lancet. 2004;364:685–696. doi: 10.1016/S0140-6736(04)16895-5. [DOI] [PubMed] [Google Scholar]
- 181.LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352:1425–1435. doi: 10.1056/NEJMoa050461. [DOI] [PubMed] [Google Scholar]
- 182.Amarenco P, Bogousslavsky J, Callahan A, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–559. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 183.Taylor F, Ward K, Moore TH, et al. Statins for the primary prevention of cardiovascular disease. The Cochrane database of systematic reviews. 2011;Cd004816 doi: 10.1002/14651858.CD004816.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.[China Cholesterol Education Program Experts Group on Prevention and Treatment of Dyslipidemia] Chin J Cardiovasc Diseases. 2016;661–664 [In Chinese] [Google Scholar]
- 185.Kernan WN, Ovbiagele B, Black HR, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45:2160–2236. doi: 10.1161/STR.0000000000000024. [DOI] [PubMed] [Google Scholar]
- 186.Fowkes FG, Price JF, Stewart MC, et al. Aspirin for prevention of cardiovascular events in a general population screened for a low ankle brachial index: a randomized controlled trial. JAMA. 2010;303:841–848. doi: 10.1001/jama.2010.221. [DOI] [PubMed] [Google Scholar]
- 187.Baigent C, Blackwell L, Collins R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373:1849–1860. doi: 10.1016/S0140-6736(09)60503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Smith SC, Jr, Benjamin EJ, Bonow RO, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–2473. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 189.[Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2013 Edition)] Chin J Diabete. 2014:2–42. [In Chinese] [Google Scholar]
- 190.Guirguis-Blake JM, Evans CV, Senger CA, et al. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164:804–813. doi: 10.7326/M15-2113. [DOI] [PubMed] [Google Scholar]
- 191.Halvorsen S, Andreotti F, ten Berg JM, et al. Aspirin therapy in primary cardiovascular disease prevention: a position paper of the European Society of Cardiology working group on thrombosis. J Am Coll Cardiol. 2014;64:319–327. doi: 10.1016/j.jacc.2014.03.049. [DOI] [PubMed] [Google Scholar]
- 192.Bibbins-Domingo K. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive services task force recommendation statement. Ann Intern Med. 2016;164:836–845. doi: 10.7326/M16-0577. [DOI] [PubMed] [Google Scholar]
- 193.Whitlock EP, Burda BU, Williams SB, et al. Bleeding risks with aspirin use for primary prevention in adults: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164:826–835. doi: 10.7326/M15-2112. [DOI] [PubMed] [Google Scholar]
- 194.[Clinical application of aspirin in atherosclerotic cardiovascular disease: Chinese expert consensus (2016)] Chin J Intern Med. 2017:68–80. [In Chinese] [Google Scholar]
- 195.Standards of medical care in diabetes-2014. Diabetes Care. 2014;37:S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 196.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in Type 2 Diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 197.Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in Type 2 Diabetes. N Engl J Med. 2017;377:644–657. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
- 198.Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in Type 2 Diabetes. N Engl J Med. 2016;375:311–322. doi: 10.1056/NEJMoa1603827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Diabetes Branch of Chinese Medical Association. [Guidelines for the prevention and treatment of type 2 Diabetes in China (2017 Edition)] Chin J Diabetes. 2018;10:4–67. [In Chinese] [Google Scholar]
- 200.Wachtell K, Hornestam B, Lehto M, et al. Cardiovascular morbidity and mortality in hypertensive patients with a history of atrial fibrillation: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) study. J Am Coll Cardiol. 2005;45:705–711. doi: 10.1016/j.jacc.2004.06.080. [DOI] [PubMed] [Google Scholar]
- 201.Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50:e1–e88. doi: 10.1093/ejcts/ezw313. [DOI] [PubMed] [Google Scholar]
- 202.Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015;386:154–162. doi: 10.1016/S0140-6736(14)61774-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 204.Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 205.Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 206.Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–2104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 207.Yu EY, Wan EY, Chan KH, et al. Evaluation of the quality of care of a multi-disciplinary Risk Factor Assessment and Management Programme for Hypertension (RAMP-HT) BMC Fam Pract. 2015;16:71. doi: 10.1186/s12875-015-0291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wang HHX, Wong MCS, Tang JL, et al. Primary care-based lifestyle interventions on blood pressure and lipid profiles among Chinese subjects: a meta-analysis. World Congress of Cardiology Scientific Sessions. 2012 [Google Scholar]
- 209.Wang HHX, Wong MCS, Yan BP, et al. Effectiveness of lifestyle interventions in reducing cardiovascular risk factors among Chinese subjects in primary care setting: a systematic review. Intern J Cardiol. 2011;147:S32. [Google Scholar]
- 210.Wang HH, Wang JJ, Xu L, et al. 12 Effect of cardiovascular risk-based approach in primary care physician-led management for 19,400 hypertensive patients in southern China. J Hypertens. 2012;30:e4. [Google Scholar]
- 211.Zhou ZY, Pan YZ, Yi WD, et al. [Comparative analysis of multiple risk factors for metabolic syndrome in community population in Guiyang City] Chin J Hypertens. 2008;937–940 [In Chinese] [Google Scholar]
- 212.Zheng L, Li J, Sun Z, et al. Relationship of blood pressure with mortality and cardiovascular events among hypertensive patients aged >/= 60 years in rural areas of China: a strobe-compliant study. Medicine (Baltimore) 2015;94:e1551. doi: 10.1097/MD.0000000000001551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents. Circulation. 2011;123:2434–2506. doi: 10.1161/CIR.0b013e31821daaf6. [DOI] [PubMed] [Google Scholar]
- 214.Franklin SS, Jacobs MJ, Wong ND, et al. Predominance of isolated systolic hypertension among middle-aged and elderly US hypertensives: analysis based on National Health and Nutrition Examination Survey (NHANES) III. Hypertension. 2001;37:869–874. doi: 10.1161/01.hyp.37.3.869. [DOI] [PubMed] [Google Scholar]
- 215.Kim NR, Kim HC. Prevalence and trends of isolated systolic hypertension among Korean adults: the Korea national health and nutrition examination survey, 1998–2012. Korean Circ J. 2015;45:492–499. doi: 10.4070/kcj.2015.45.6.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self-measurement in elderly treated hypertensive patients. JAMA. 2004;291:1342–1349. doi: 10.1001/jama.291.11.1342. [DOI] [PubMed] [Google Scholar]
- 217.Insua JT, Sacks HS, Lau TS, et al. Drug treatment of hypertension in the elderly: a meta-analysis. Ann Intern Med. 1994;121:355–362. doi: 10.7326/0003-4819-121-5-199409010-00008. [DOI] [PubMed] [Google Scholar]
- 218.Franklin SS, Wilkinson IB, McEniery CM, et al. Unusual hypertensive phenotypes: what is their significance? Hypertension. 2012;59:173–178. doi: 10.1161/HYPERTENSIONAHA.111.182956. [DOI] [PubMed] [Google Scholar]
- 219.SHEP Cooperative Research Group. Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP) JAMA. 1991;265:3255–3264. [PubMed] [Google Scholar]
- 220.Dahlof B, Lindholm LH, Hansson L, et al. Morbidity and mortality in the Swedish Trial in Old Patients with Hypertension (STOP-Hypertension) Lancet. 1991;338:1281–1285. doi: 10.1016/0140-6736(91)92589-t. [DOI] [PubMed] [Google Scholar]
- 221.Coope J, Warrender TS. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J (Clin Res Ed) 1986;293:1145–1151. doi: 10.1136/bmj.293.6555.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Hansson L, Lindholm LH, Ekbom T, et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet. 1999;354:1751–1756. doi: 10.1016/s0140-6736(99)10327-1. [DOI] [PubMed] [Google Scholar]
- 223.Lithell H, Hansson L, Skoog I, et al. The Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trial. J Hypertens. 2003;21:875–886. doi: 10.1097/00004872-200305000-00011. [DOI] [PubMed] [Google Scholar]
- 224.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:555–576. [PubMed] [Google Scholar]
- 225.Lurbe E, Agabiti-Rosei E, Cruickshank JK, et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J Hypertens. 2016;34:1887–1920. doi: 10.1097/HJH.0000000000001039. [DOI] [PubMed] [Google Scholar]
- 226.Dong B, Ma J, Wang HJ, et al. The association of overweight and obesity with blood pressure among Chinese children and adolescents. Biomed Environ Sci. 2013;26:437–444. doi: 10.3967/0895-3988.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 227.Lo JC, Sinaiko A, Chandra M, et al. Prehypertension and hypertension in community-based pediatric practice. Pediatrics. 2013;131:e415–e424. doi: 10.1542/peds.2012-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Koebnick C, Mohan Y, Li X, et al. Failure to confirm high blood pressures in pediatric care-quantifying the risks of misclassification. J Clin Hypertens (Greenwich) 2018;20:174–182. doi: 10.1111/jch.13159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Hu YM, Zhu FT. [Practical Pediatrics] Beijing: People's Medical Publishing House; 2002. [In Chinese] [Google Scholar]
- 230.McNiece KL, Gupta-Malhotra M, Samuels J, et al. Left ventricular hypertrophy in hypertensive adolescents: analysis of risk by 2004 National High Blood Pressure Education Program Working Group staging criteria. Hypertension. 2007;50:392–395. doi: 10.1161/HYPERTENSIONAHA.107.092197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Brady TM, Redwine KM, Flynn JT, et al. Screening blood pressure measurement in children: are we saving lives? Pediatr Nephrol. 2014;29:947–950. doi: 10.1007/s00467-013-2715-1. [DOI] [PubMed] [Google Scholar]
- 232.Litwin M, Niemirska A, Sladowska J, et al. Left ventricular hypertrophy and arterial wall thickening in children with essential hypertension. Pediatr Nephrol. 2006;21:811–819. doi: 10.1007/s00467-006-0068-8. [DOI] [PubMed] [Google Scholar]
- 233.Sinha MD, Reid CJ. Evaluation of blood pressure in children. Curr Opin Nephrol Hypertens. 2007;16:577–584. doi: 10.1097/MNH.0b013e3282f0d107. [DOI] [PubMed] [Google Scholar]
- 234.Assadi F. Relation of left ventricular hypertrophy to microalbuminuria and C-reactive protein in children and adolescents with essential hypertension. Pediatr Cardiol. 2008;29:580–584. doi: 10.1007/s00246-007-9153-4. [DOI] [PubMed] [Google Scholar]
- 235.Mitchell P, Cheung N, de Haseth K, et al. Blood pressure and retinal arteriolar narrowing in children. Hypertension. 2007;49:1156–1162. doi: 10.1161/HYPERTENSIONAHA.106.085910. [DOI] [PubMed] [Google Scholar]
- 236.Chen X, Wang Y, Appel LJ, et al. Impacts of measurement protocols on blood pressure tracking from childhood into adulthood: a metaregression analysis. Hypertension. 2008;51:642–649. doi: 10.1161/HYPERTENSIONAHA.107.102145. [DOI] [PubMed] [Google Scholar]
- 237.Zhang MM, Mi J, Wang W, et al. [A longitudinal control survey of blood pressure in 412 children in Beijing after 18 years] Chinese Journal of Evidence-Based Pediatrics. 2006;187–192 [In Chinese] [Google Scholar]
- 238.Sundstrom J, Neovius M, Tynelius P, et al. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643. doi: 10.1136/bmj.d643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Yan Y, Hou D, Liu J, et al. Childhood body mass index and blood pressure in prediction of subclinical vascular damage in adulthood: Beijing blood pressure cohort. J Hypertens. 2017;35:47–54. doi: 10.1097/HJH.0000000000001118. [DOI] [PubMed] [Google Scholar]
- 240.Liang Y, Hou D, Shan X, et al. Cardiovascular remodeling relates to elevated childhood blood pressure: Beijing Blood Pressure Cohort Study. Int J Cardiol. 2014;177:836–839. doi: 10.1016/j.ijcard.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 241.Gray L, Lee IM, Sesso HD, et al. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study) J Am Coll Cardiol. 2011;58:2396–2403. doi: 10.1016/j.jacc.2011.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140 doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 243.Fan H, Yan YK, Mi J, et al. [Reference standards for gender, age and height in Chinese children aged 3 to 17 years] Chin J Hypertens. 2017;428–435 [In Chinese] [Google Scholar]
- 244.Fan H, Hou D, Liu J, et al. Performance of 4 definitions of childhood elevated blood pressure in predicting subclinical cardiovascular outcomes in adulthood. J Clin Hypertens. 2018;20 doi: 10.1111/jch.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Fan H, Yan YK, Mi J, et al. [Development of a simplified blood pressure standard for children aged 3 to 17 years in China] Chin J Hypertens. 2017;436–440 [In Chinese] [Google Scholar]
- 246.Li S, Chen W. Identifying elevated blood pressure and hypertension in children and adolescents. J Clin Hypertens (Greenwich) 2018;20:515–517. doi: 10.1111/jch.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Geleijnse JM, Hofman A, Witteman JC, et al. Long-term effects of neonatal sodium restriction on blood pressure. Hypertension. 1997;29:913–917. doi: 10.1161/01.hyp.29.4.913. [DOI] [PubMed] [Google Scholar]
- 248.Rocchini AP, Katch V, Anderson J, et al. Blood pressure in obese adolescents: effect of weight loss. Pediatrics. 1988;82:16–23. [PubMed] [Google Scholar]
- 249.McCambridge TM, Benjamin HJ, Brenner JS, et al. Athletic participation by children and adolescents who have systemic hypertension. Pediatrics. 2010;125:1287–1294. doi: 10.1542/peds.2010-0658. [DOI] [PubMed] [Google Scholar]
- 250.Simons-Morton DG, Hunsberger SA, Van Horn L, et al. Nutrient intake and blood pressure in the Dietary Intervention Study in Children. Hypertension. 1997;29:930–936. doi: 10.1161/01.hyp.29.4.930. [DOI] [PubMed] [Google Scholar]
- 251.Magee LA, Pels A, Helewa M, et al. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can. 2014;36:416–441. doi: 10.1016/s1701-2163(15)30588-0. [DOI] [PubMed] [Google Scholar]
- 252.Cantwell R, Clutton-Brock T, Cooper G, et al. Saving Mothers' Lives: Reviewing maternal deaths to make motherhood safer: 2006-2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG. 2011;118:1–203. doi: 10.1111/j.1471-0528.2010.02847.x. [DOI] [PubMed] [Google Scholar]
- 253.Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–1131. doi: 10.1097/01.AOG.0000437382.03963.88. [DOI] [PubMed] [Google Scholar]
- 254.Sibai BM. Chronic hypertension in pregnancy. Obstet Gynecol. 2002;100:369–377. doi: 10.1016/s0029-7844(02)02128-2. [DOI] [PubMed] [Google Scholar]
- 255.Gilbert WM, Young AL, Danielsen B, et al. Pregnancy outcomes in women with chronic hypertension: a population-based study. J Reprod Med. 2007;52:1046–1051. [PubMed] [Google Scholar]
- 256.Magee LA, von Dadelszen P, Rey E, et al. Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372:407–417. doi: 10.1056/NEJMoa1404595. [DOI] [PubMed] [Google Scholar]
- 257.Bujold E, Roberge S, Lacasse Y, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116:402–414. doi: 10.1097/AOG.0b013e3181e9322a. [DOI] [PubMed] [Google Scholar]
- 258.Lubsen J, Wagener G, Kirwan BA, et al. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with symptomatic stable angina and hypertension: the ACTION trial. J Hypertens. 2005;23:641–648. doi: 10.1097/01.hjh.0000160223.94220.29. [DOI] [PubMed] [Google Scholar]
- 259.Zhang J, Zhang YH. [Multi-center, prospective Chinese heart failure registration study – preliminary analysis of etiology, clinical features and treatment] Chin J Circ. 2015;30:413–416. [In Chinese] [Google Scholar]
- 260.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 261.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 262.Chinese Medical Association Cardiovascular Branch, Editorial Board of Chinese Journal of Cardiovascular Diseases. [Guidelines for the diagnosis and treatment of heart failure in China 2014] Chin J Cardiovasc Diseases. 2014;98–122 [In Chinese] [Google Scholar]
- 263.Hollenberg NK. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic. Curr Hypertens Rep. 2003;5:183–185. doi: 10.1007/s11906-003-0018-9. [DOI] [PubMed] [Google Scholar]
- 264.Leenen FH, Nwachuku CE, Black HR, et al. Clinical events in high-risk hypertensive patients randomly assigned to calcium channel blocker versus angiotensin-converting enzyme inhibitor in the antihypertensive and lipid-lowering treatment to prevent heart attack trial. Hypertension. 2006;48:374–384. doi: 10.1161/01.HYP.0000231662.77359.de. [DOI] [PubMed] [Google Scholar]
- 265.Zhang W, Shi W, Liu Z, et al. A nationwide cross-sectional survey on prevalence, management and pharmacoepidemiology patterns on hypertension in Chinese patients with chronic kidney disease. Sci Rep. 2016;6:38768. doi: 10.1038/srep38768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Zheng Y, Cai GY, Chen XM, et al. Prevalence, awareness, treatment, and control of hypertension in the non-dialysis chronic kidney disease patients. Chin Med J (Engl) 2013;126:2276–2280. [PubMed] [Google Scholar]
- 267.Lin J, Ding JJ, Fu CS, et al. [A cross-sectional survey of hypertension in patients with chronic kidney disease] Chin J Nephrol. 2009;11:827–831. [In Chinese] [Google Scholar]
- 268.Dhaybi OA, Bakris G. Mineralocorticoid antagonists in chronic kidney disease. Curr Opin Nephrol Hypertens. 2017;26:50–55. doi: 10.1097/MNH.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 269.Robinson BM, Tong L, Zhang J, et al. Blood pressure levels and mortality risk among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2012;82:570–580. doi: 10.1038/ki.2012.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Liu J, Zhao D, Liu J, et al. Prevalence of diabetes mellitus in outpatients with essential hypertension in China: a cross-sectional study. BMJ Open. 2013;3:e003798. doi: 10.1136/bmjopen-2013-003798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.de Boer IH, Bangalore S, Benetos A, et al. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017;40:1273–1284. doi: 10.2337/dci17-0026. [DOI] [PubMed] [Google Scholar]
- 272.Emdin CA, Rahimi K, Neal B, et al. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313:603–615. doi: 10.1001/jama.2014.18574. [DOI] [PubMed] [Google Scholar]
- 273.Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351:1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 274.Gu D, Reynolds K, Wu X, et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet. 2005;365:1398–1405. doi: 10.1016/S0140-6736(05)66375-1. [DOI] [PubMed] [Google Scholar]
- 275.Xi B, He D, Hu Y, et al. Prevalence of metabolic syndrome and its influencing factors among the Chinese adults: the China Health and Nutrition Survey in 2009. Prev Med. 2013;57:867–871. doi: 10.1016/j.ypmed.2013.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Zhu ZM. [Metabolic Syndrome---Etiology Exploration and Clinical Practice. Prevention and Treatment of Metabolic Syndrome] Beijing: People's Military Medical Press; 2005. [In Chinese] [Google Scholar]
- 277.Liu J, Zhao D, Wang W, et al. [The relationship between different components and combinations of metabolic syndrome and cardiovascular disease in 11 provinces of China] Chin J Epidemiol. 2008;652–625 [In Chinese] [Google Scholar]
- 278.Xiao J, Wu C, Xu G, et al. Association of physical activity with risk of metabolic syndrome: findings from a cross-sectional study conducted in rural area, Nantong, China. J Sports Sci. 2016;34:1839–1848. doi: 10.1080/02640414.2016.1140221. [DOI] [PubMed] [Google Scholar]
- 279.Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999-2000. Circulation. 2004;110:738–743. doi: 10.1161/01.CIR.0000137913.26087.F0. [DOI] [PubMed] [Google Scholar]
- 280.Norgren L, Hiatt WR, Dormandy JA, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II) Eur J Vasc Endovasc Surg. 2007;33:S1–S75. doi: 10.1016/j.ejvs.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 281.Kong LZ, Hu SS. China Cardiovascular Disease Report 2010. Beijing: China Encyclopedia Publishing House; 2010. pp. 112–113. [In Chinese] [Google Scholar]
- 282.Lip GY, Makin AJ. Treatment of hypertension in peripheral arterial disease. Cochrane Database Syst Rev. 2003;CD003075 doi: 10.1002/14651858.CD003075. [DOI] [PubMed] [Google Scholar]
- 283.Singer DR, Kite A. Management of hypertension in peripheral arterial disease: does the choice of drugs matter? Eur J Vasc Endovasc Surg. 2008;35:701–708. doi: 10.1016/j.ejvs.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 284.European Stroke O, Tendera M, Aboyans V, et al. ESC Guidelines on the diagnosis and treatment of peripheral artery diseases: Document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteries: the Task Force on the Diagnosis and Treatment of Peripheral Artery Diseases of the European Society of Cardiology (ESC) Eur Heart J. 2011;32:2851–2906. doi: 10.1093/eurheartj/ehr211. [DOI] [PubMed] [Google Scholar]
- 285.Anderson JL, Halperin JL, Albert NM, et al. Management of patients with peripheral artery disease (compilation of 2005 and 2011 ACCF/AHA guideline recommendations): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:1425–1443. doi: 10.1161/CIR.0b013e31828b82aa. [DOI] [PubMed] [Google Scholar]
- 286.Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation, and treatment. A scientific statement from the American Heart Association Professional Education Committee of the Council for High Blood Pressure Research. Hypertension. 2008;51:1403–1419. doi: 10.1161/HYPERTENSIONAHA.108.189141. [DOI] [PubMed] [Google Scholar]
- 287.Denolle T, Chamontin B, Doll G, et al. Management of resistant hypertension: expert consensus statement from the French Society of Hypertension, an affiliate of the French Society of Cardiology. J Hum Hypertens. 2016;30:657–663. doi: 10.1038/jhh.2015.122. [DOI] [PubMed] [Google Scholar]
- 288.Williams B, MacDonald TM, Morant S, et al. Spironolactone versus placebo, bisoprolol, and doxazosin to determine the optimal treatment for drug-resistant hypertension (PATHWAY-2): a randomised, double-blind, crossover trial. Lancet. 2015;386:2059–2068. doi: 10.1016/S0140-6736(15)00257-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Oliveras A, Armario P, Clara A, et al. Spironolactone versus sympathetic renal denervation to treat true resistant hypertension: results from the DENERVHTA study—a randomized controlled trial. J Hypertens. 2016;34:1863–1871. doi: 10.1097/HJH.0000000000001025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Wu ZS, Zhu DL, Jiang XJ, et al. [The position and recommendations of the Chinese Hypertension League on percutaneous transluminal radiofrequency ablation of renal sympathetic nerve for the treatment of refractory hypertension] Chin J Hypertens. 2013;419:22–23. [In Chinese] [Google Scholar]
- 291.Ogihara T, Kikuchi K, Matsuoka H, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009) Hypertens Res. 2009;32:3–107. [PubMed] [Google Scholar]
- 292.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 293.Wright JT, Jr, Fine LJ, Lackland DT, et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014;160:499–503. doi: 10.7326/M13-2981. [DOI] [PubMed] [Google Scholar]
- 294.Ezzati M, Oza S, Danaei G, et al. Trends and cardiovascular mortality effects of state-level blood pressure and uncontrolled hypertension in the United States. Circulation. 2008;117:905–914. doi: 10.1161/CIRCULATIONAHA.107.732131. [DOI] [PubMed] [Google Scholar]
- 295.Aronson S. Perioperative hypertensive emergencies. Curr Hypertens Rep. 2014;16:448. doi: 10.1007/s11906-014-0448-6. [DOI] [PubMed] [Google Scholar]
- 296.Getsios D, Wang Y, Stolar M, et al. Improved perioperative blood pressure control leads to reduced hospital costs. Expert Opin Pharmacother. 2013;14:1285–1293. doi: 10.1517/14656566.2013.798646. [DOI] [PubMed] [Google Scholar]
- 297.Hanada S, Kawakami H, Goto T, et al. Hypertension and anesthesia. Curr Opin Anaesthesiol. 2006;19:315–319. doi: 10.1097/01.aco.0000192811.56161.23. [DOI] [PubMed] [Google Scholar]
- 298.Marik PE, Varon J. Perioperative hypertension: a review of current and emerging therapeutic agents. J Clin Anesth. 2009;21:220–229. doi: 10.1016/j.jclinane.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 299.Wang ZW, Yan H, Wang X, et al. [Comparative study on the effects of hypertension management in rural communities] J Med Res. 2015;25–28 [In Chinese] [Google Scholar]
- 300.Wang Z, Wang X, Chen Z, et al. Hypertension control in community health centers across China: analysis of antihypertensive drug treatment patterns. Am J Hypertens. 2014;27:252–259. doi: 10.1093/ajh/hpt186. [DOI] [PubMed] [Google Scholar]
- 301.Wu ZS, Huo Y, Wang W, Zhao LY, Zhu DL, on behalf of the “China High Blood Pressure Education Guide” Compilation Committee [Chinese Hypertension Patients Education Guide] Chin J Hypertens. 2013:1123–1149. [In Chinese] [Google Scholar]
- 302.Li N, Cheng WP, Yan ZT, et al. [Investigation and analysis of target organ damage in sleep apnea-related hypertension] Chin J Hypertens. 2011;642–646 [In Chinese] [Google Scholar]
- 303.Li NF, Li HJ, Wang HM, et al. [Study of left ventricular structural damage in patients with primary aldosteronism] Chin J Endocrinol Metabol. 2012:117–120. [In Chinese] [Google Scholar]
- 304.Li N, Ma X, Wang HM, et al. [Analysis of proteinuria in patients with primary aldosteronism] Chin J Hypertens. 2013;249–252 [In Chinese] [Google Scholar]
- 305.LI Nan-fang, W-pC, YAN Zhi-tao, et al. Prevalence of target organ damage in patients with obstructive sleep apnea-related hypertension. Am J Hypertens. 2011;24:1345. [Google Scholar]
- 306.Wang L, Li NF, Zhou KM, et al. [Analysis of 628 cases of uncontrollable hypertension] Chin J Cardiol. 2009;138–141 [In Chinese] [Google Scholar]
- 307.Peng M, Jiang XJ, Dong H, et al. Etiology of renal artery stenosis in 2047 patients: a single-center retrospective analysis during a 15-year period in China. J Hum Hypertens. 2016;30:124–128. doi: 10.1038/jhh.2015.40. [DOI] [PubMed] [Google Scholar]
- 308.[Expert Consensus Drafting Group of Vascular Diseases and Hypertension Branch of China International Exchange and Promotive Association for Medical and Health Care Chinese expert consensus on diagnosis and treatment of renal artery stenosis] Chin J Circ. 2017;835–844 [In Chinese] [Google Scholar]
- 309.Jiang X, Peng M, Li B, et al. The efficacy of renal artery stent combined with optimal medical therapy in patients with severe atherosclerotic renal artery stenosis. Curr Med Res Opin. 2016;32:3–7. doi: 10.1080/03007995.2016.1218833. [DOI] [PubMed] [Google Scholar]
- 310.Li NF, Zhang LL, Yan ZT, et al. [Study on the detection rate of sleep apnea hypopnea syndrome in hypertensive patients with different body mass index] Chin J Cardiovasc Diseases. 2012;40:120–124. [In Chinese] [PubMed] [Google Scholar]
- 311.Yao X, Li N, Zhang Y, et al. Plasma aldosterone concentration is positively associated with pulse pressure in patients with primary hypertension. Medicine (Baltimore) 2015;94:e614. doi: 10.1097/MD.0000000000000614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Ma X, Wang HM, Li J, et al. [The prevalence of metabolic syndrome in patients with primary aldosteronism] Chin J Endocrinol Metab. 2011;724–728 [In Chinese] [Google Scholar]
- 313.Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387:251–272. doi: 10.1016/S0140-6736(15)00551-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement Table 1-1. Blood pressure references for children and adolescents aged 3 to 17 years old in China, male.
| Age, year | Height percentile | Height range, cm | SBP, mmHg |
DBP, mmHg |
||||||
| 50th | 90th | 95th | 99th | 50th | 90th | 95th | 99th | |||
| 3 | P5 | < 96 | 88 | 99 | 102 | 108 | 54 | 62 | 65 | 72 |
| P10 | 96–97 | 88 | 100 | 103 | 109 | 54 | 63 | 65 | 72 | |
| P25 | 98–100 | 89 | 101 | 104 | 110 | 54 | 63 | 66 | 72 | |
| P50 | 101–103 | 90 | 102 | 105 | 112 | 54 | 63 | 66 | 73 | |
| P75 | 104–106 | 91 | 103 | 107 | 113 | 55 | 63 | 66 | 73 | |
| P90 | 107–108 | 92 | 104 | 107 | 114 | 55 | 63 | 66 | 73 | |
| P95 | ≥ 109 | 93 | 105 | 108 | 115 | 55 | 63 | 66 | 73 | |
| 4 | P5 | < 102 | 89 | 101 | 104 | 111 | 55 | 64 | 67 | 74 |
| P10 | 102–104 | 90 | 102 | 105 | 111 | 55 | 64 | 67 | 74 | |
| P25 | 105–107 | 91 | 103 | 106 | 113 | 55 | 64 | 67 | 74 | |
| P50 | 108–110 | 92 | 104 | 108 | 114 | 56 | 64 | 67 | 74 | |
| P75 | 111–113 | 93 | 106 | 109 | 115 | 56 | 64 | 67 | 74 | |
| P90 | 114–116 | 94 | 107 | 110 | 117 | 56 | 65 | 68 | 75 | |
| P95 | ≥ 117 | 95 | 107 | 111 | 117 | 56 | 65 | 68 | 75 | |
| 5 | P5 | < 109 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 75 |
| P10 | 109–110 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 75 | |
| P25 | 111–113 | 93 | 105 | 109 | 115 | 56 | 65 | 68 | 75 | |
| P50 | 114–117 | 94 | 106 | 110 | 117 | 57 | 65 | 69 | 76 | |
| P75 | 118–120 | 95 | 108 | 111 | 118 | 57 | 66 | 69 | 76 | |
| P90 | 121–123 | 96 | 109 | 112 | 119 | 58 | 67 | 70 | 77 | |
| P95 | ≥ 124 | 97 | 110 | 113 | 120 | 58 | 67 | 70 | 77 | |
| 6 | P5 | < 114 | 93 | 105 | 109 | 115 | 57 | 66 | 69 | 76 |
| P10 | 114–116 | 94 | 106 | 110 | 116 | 57 | 66 | 69 | 76 | |
| P25 | 117–119 | 95 | 107 | 111 | 117 | 58 | 66 | 69 | 77 | |
| P50 | 120–123 | 96 | 108 | 112 | 119 | 58 | 67 | 70 | 78 | |
| P75 | 124–126 | 97 | 110 | 113 | 120 | 59 | 68 | 71 | 78 | |
| P90 | 127–129 | 98 | 111 | 115 | 121 | 59 | 69 | 72 | 79 | |
| P95 | ≥ 130 | 99 | 112 | 116 | 123 | 60 | 69 | 73 | 80 | |
| 7 | P5 | < 118 | 94 | 106 | 110 | 117 | 58 | 67 | 70 | 77 |
| P10 | 118–120 | 95 | 107 | 111 | 118 | 58 | 67 | 70 | 78 | |
| P25 | 121–123 | 96 | 108 | 112 | 119 | 59 | 68 | 71 | 78 | |
| P50 | 124–127 | 97 | 110 | 113 | 120 | 59 | 68 | 72 | 79 | |
| P75 | 128–131 | 98 | 112 | 115 | 122 | 60 | 70 | 73 | 81 | |
| P90 | 132–135 | 100 | 113 | 117 | 124 | 61 | 71 | 74 | 82 | |
| P95 | ≥ 136 | 100 | 114 | 117 | 125 | 62 | 71 | 74 | 82 | |
| 8 | P5 | < 121 | 95 | 108 | 111 | 118 | 59 | 68 | 71 | 78 |
| P10 | 121–123 | 95 | 108 | 112 | 119 | 59 | 68 | 71 | 79 | |
| P25 | 124–127 | 97 | 110 | 113 | 120 | 60 | 69 | 72 | 80 | |
| P50 | 128–132 | 98 | 111 | 115 | 122 | 61 | 70 | 73 | 81 | |
| P75 | 133–136 | 99 | 113 | 117 | 124 | 62 | 71 | 74 | 82 | |
| P90 | 137–139 | 101 | 114 | 118 | 125 | 62 | 72 | 75 | 83 | |
| P95 | ≥ 140 | 102 | 115 | 119 | 127 | 63 | 73 | 76 | 84 | |
| 9 | P5 | < 125 | 96 | 109 | 112 | 119 | 60 | 69 | 72 | 80 |
| P10 | 125–128 | 96 | 109 | 113 | 120 | 60 | 69 | 73 | 80 | |
| P25 | 129–132 | 98 | 111 | 115 | 122 | 61 | 71 | 74 | 82 | |
| P50 | 133–137 | 99 | 113 | 117 | 124 | 62 | 72 | 75 | 83 | |
| P75 | 138–142 | 101 | 115 | 119 | 126 | 63 | 73 | 76 | 84 | |
| P90 | 143–145 | 102 | 116 | 120 | 128 | 64 | 73 | 77 | 85 | |
| P95 | ≥ 146 | 103 | 117 | 121 | 129 | 64 | 74 | 77 | 85 | |
| 10 | P5 | < 130 | 97 | 110 | 114 | 121 | 61 | 70 | 74 | 81 |
| P10 | 130–132 | 98 | 111 | 115 | 122 | 62 | 71 | 74 | 82 | |
| P25 | 133–137 | 99 | 113 | 116 | 124 | 62 | 72 | 75 | 83 | |
| P50 | 138–142 | 101 | 115 | 119 | 126 | 63 | 73 | 77 | 85 | |
| P75 | 143–147 | 102 | 117 | 120 | 128 | 64 | 74 | 77 | 85 | |
| P90 | 148–151 | 104 | 118 | 122 | 130 | 64 | 74 | 77 | 86 | |
| P95 | ≥ 152 | 105 | 119 | 123 | 131 | 64 | 74 | 77 | 86 | |
| 11 | P5 | < 134 | 98 | 111 | 115 | 122 | 62 | 72 | 75 | 83 |
| P10 | 134–137 | 99 | 112 | 116 | 124 | 63 | 72 | 76 | 84 | |
| P25 | 138–142 | 100 | 114 | 118 | 126 | 64 | 73 | 77 | 85 | |
| P50 | 143–148 | 102 | 116 | 120 | 128 | 64 | 74 | 78 | 86 | |
| P75 | 149–153 | 104 | 119 | 123 | 130 | 64 | 74 | 78 | 86 | |
| P90 | 154–157 | 106 | 120 | 124 | 132 | 64 | 74 | 78 | 86 | |
| P95 | ≥ 158 | 106 | 121 | 125 | 133 | 64 | 74 | 78 | 86 | |
| 12 | P5 | < 140 | 100 | 113 | 117 | 125 | 64 | 73 | 77 | 85 |
| P10 | 140–144 | 101 | 115 | 119 | 126 | 64 | 74 | 78 | 86 | |
| P25 | 145–149 | 102 | 117 | 121 | 128 | 65 | 75 | 78 | 86 | |
| P50 | 150–155 | 104 | 119 | 123 | 131 | 65 | 75 | 78 | 86 | |
| P75 | 156–160 | 106 | 121 | 125 | 133 | 65 | 75 | 78 | 86 | |
| P90 | 161–164 | 108 | 123 | 127 | 135 | 65 | 75 | 78 | 87 | |
| P95 | ≥ 165 | 108 | 124 | 128 | 136 | 65 | 75 | 78 | 87 | |
| 13 | P5 | < 147 | 102 | 116 | 120 | 128 | 65 | 75 | 78 | 86 |
| P10 | 147–151 | 103 | 117 | 121 | 129 | 65 | 75 | 78 | 87 | |
| P25 | 152–156 | 104 | 119 | 123 | 131 | 65 | 75 | 79 | 87 | |
| P50 | 157–162 | 106 | 121 | 125 | 133 | 65 | 75 | 79 | 87 | |
| P75 | 163–167 | 108 | 123 | 128 | 136 | 65 | 75 | 79 | 87 | |
| P90 | 168–171 | 110 | 125 | 130 | 138 | 66 | 76 | 79 | 87 | |
| P95 | ≥ 172 | 110 | 126 | 130 | 139 | 66 | 76 | 79 | 88 | |
| 14 | P5 | < 154 | 103 | 118 | 122 | 130 | 65 | 75 | 79 | 87 |
| P10 | 154–157 | 104 | 119 | 124 | 132 | 65 | 75 | 79 | 87 | |
| P25 | 158–162 | 106 | 121 | 125 | 133 | 65 | 75 | 79 | 87 | |
| P50 | 163–167 | 108 | 123 | 128 | 136 | 65 | 75 | 79 | 87 | |
| P75 | 168–172 | 109 | 125 | 130 | 138 | 66 | 76 | 79 | 88 | |
| P90 | 173–176 | 111 | 127 | 131 | 140 | 66 | 76 | 80 | 88 | |
| P95 | ≥ 177 | 112 | 128 | 133 | 141 | 67 | 77 | 80 | 89 | |
| 15 | P5 | < 158 | 105 | 120 | 124 | 132 | 65 | 76 | 79 | 87 |
| P10 | 158–161 | 106 | 121 | 125 | 133 | 65 | 76 | 79 | 87 | |
| P25 | 162–166 | 107 | 122 | 127 | 135 | 66 | 76 | 79 | 88 | |
| P50 | 167–170 | 109 | 124 | 128 | 137 | 66 | 76 | 80 | 88 | |
| P75 | 171–174 | 110 | 126 | 131 | 139 | 66 | 77 | 80 | 89 | |
| P90 | 175–178 | 112 | 128 | 132 | 141 | 67 | 77 | 81 | 89 | |
| P95 | ≥ 179 | 113 | 129 | 133 | 142 | 67 | 77 | 81 | 90 | |
| 16 | P5 | < 161 | 105 | 121 | 125 | 133 | 66 | 76 | 79 | 88 |
| P10 | 161–164 | 106 | 121 | 126 | 134 | 66 | 76 | 79 | 88 | |
| P25 | 165–168 | 107 | 123 | 127 | 136 | 66 | 76 | 80 | 88 | |
| P50 | 169–172 | 109 | 125 | 129 | 138 | 66 | 76 | 80 | 88 | |
| P75 | 173–176 | 111 | 126 | 131 | 140 | 67 | 77 | 80 | 89 | |
| P90 | 177–179 | 112 | 128 | 133 | 141 | 67 | 77 | 81 | 90 | |
| P95 | ≥ 180 | 113 | 129 | 134 | 142 | 67 | 78 | 81 | 90 | |
| 17 | P5 | < 163 | 106 | 121 | 126 | 134 | 66 | 76 | 80 | 88 |
| P10 | 163–165 | 107 | 122 | 126 | 135 | 66 | 76 | 80 | 88 | |
| P25 | 166–169 | 108 | 124 | 128 | 136 | 66 | 76 | 80 | 88 | |
| P50 | 170–173 | 109 | 125 | 130 | 138 | 67 | 77 | 80 | 89 | |
| P75 | 174–177 | 111 | 127 | 131 | 140 | 67 | 77 | 81 | 89 | |
| P90 | 178–180 | 112 | 129 | 133 | 142 | 67 | 78 | 81 | 90 | |
| P95 | ≥ 181 | 113 | 129 | 134 | 143 | 68 | 78 | 82 | 90 | |
Supplement Table 1-2. Blood pressure references for children and adolescents aged 3 to 17 years old in China, female.
| Age, year | Height percentile | Height range, cm | SBP, mmHg |
DBP, mmHg |
||||||
| 50th | 90th | 95th | 99th | 50th | 90th | 95th | 99th | |||
| 3 | P5 | < 95 | 87 | 99 | 102 | 108 | 55 | 63 | 67 | 74 |
| P10 | 95–96 | 88 | 99 | 103 | 109 | 55 | 63 | 67 | 74 | |
| P25 | 97–99 | 88 | 100 | 103 | 110 | 55 | 64 | 67 | 74 | |
| P50 | 100–102 | 89 | 101 | 104 | 111 | 55 | 64 | 67 | 74 | |
| P75 | 103–105 | 90 | 102 | 105 | 112 | 55 | 64 | 67 | 74 | |
| P90 | 106–107 | 91 | 103 | 106 | 113 | 55 | 64 | 67 | 75 | |
| P95 | ≥ 108 | 91 | 103 | 107 | 113 | 56 | 64 | 67 | 75 | |
| 4 | P5 | < 101 | 89 | 101 | 105 | 111 | 56 | 64 | 67 | 75 |
| P10 | 101–103 | 89 | 101 | 105 | 111 | 56 | 64 | 67 | 75 | |
| P25 | 104–106 | 90 | 102 | 106 | 112 | 56 | 64 | 67 | 75 | |
| P50 | 107–109 | 91 | 103 | 107 | 113 | 56 | 64 | 67 | 75 | |
| P75 | 110–112 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 75 | |
| P90 | 113–114 | 93 | 105 | 109 | 115 | 56 | 65 | 68 | 76 | |
| P95 | ≥ 115 | 93 | 105 | 109 | 115 | 56 | 65 | 68 | 76 | |
| 5 | P5 | < 108 | 91 | 103 | 106 | 113 | 56 | 65 | 68 | 76 |
| P10 | 108–109 | 91 | 103 | 107 | 113 | 56 | 65 | 68 | 76 | |
| P25 | 110–112 | 92 | 104 | 107 | 114 | 56 | 65 | 68 | 76 | |
| P50 | 113–116 | 93 | 105 | 109 | 115 | 57 | 65 | 68 | 76 | |
| P75 | 117–119 | 93 | 106 | 109 | 116 | 57 | 66 | 69 | 77 | |
| P90 | 120–122 | 94 | 107 | 111 | 117 | 58 | 66 | 70 | 77 | |
| P95 | ≥ 123 | 95 | 108 | 111 | 118 | 58 | 67 | 70 | 78 | |
| 6 | P5 | < 113 | 92 | 104 | 108 | 115 | 57 | 65 | 69 | 76 |
| P10 | 113–114 | 92 | 105 | 108 | 115 | 57 | 66 | 69 | 77 | |
| P25 | 115–118 | 93 | 106 | 109 | 116 | 57 | 66 | 69 | 77 | |
| P50 | 119–121 | 94 | 107 | 110 | 117 | 58 | 67 | 70 | 78 | |
| P75 | 122–125 | 95 | 108 | 112 | 118 | 58 | 67 | 71 | 79 | |
| P90 | 126–128 | 96 | 109 | 113 | 119 | 59 | 68 | 71 | 79 | |
| P95 | ≥ 129 | 97 | 110 | 114 | 121 | 59 | 69 | 72 | 80 | |
| 7 | P5 | < 116 | 93 | 105 | 109 | 115 | 57 | 66 | 69 | 77 |
| P10 | 116–118 | 93 | 106 | 109 | 116 | 57 | 66 | 69 | 77 | |
| P25 | 119–122 | 94 | 107 | 110 | 117 | 58 | 67 | 70 | 78 | |
| P50 | 123–126 | 95 | 108 | 112 | 119 | 59 | 68 | 71 | 79 | |
| P75 | 127–130 | 96 | 109 | 113 | 120 | 59 | 69 | 72 | 80 | |
| P90 | 131–133 | 97 | 111 | 114 | 122 | 60 | 69 | 73 | 81 | |
| P95 | ≥ 134 | 98 | 112 | 115 | 122 | 61 | 70 | 73 | 82 | |
| 8 | P5 | < 120 | 94 | 106 | 110 | 116 | 58 | 67 | 70 | 78 |
| P10 | 120–122 | 94 | 107 | 111 | 117 | 58 | 67 | 71 | 79 | |
| P25 | 123–126 | 95 | 108 | 112 | 119 | 59 | 68 | 71 | 79 | |
| P50 | 127–131 | 96 | 109 | 113 | 120 | 60 | 69 | 72 | 80 | |
| P75 | 132–135 | 98 | 111 | 115 | 122 | 61 | 70 | 73 | 82 | |
| P90 | 136–138 | 99 | 112 | 116 | 123 | 61 | 71 | 74 | 83 | |
| P95 | ≥ 139 | 100 | 113 | 117 | 124 | 62 | 71 | 75 | 83 | |
| 9 | P5 | < 124 | 95 | 108 | 111 | 118 | 59 | 68 | 71 | 79 |
| P10 | 124–127 | 95 | 108 | 112 | 119 | 59 | 68 | 72 | 80 | |
| P25 | 128–132 | 97 | 110 | 113 | 120 | 60 | 69 | 73 | 81 | |
| P50 | 133–136 | 98 | 111 | 115 | 122 | 61 | 71 | 74 | 82 | |
| P75 | 137–141 | 100 | 113 | 117 | 124 | 62 | 72 | 75 | 84 | |
| P90 | 142–145 | 101 | 114 | 118 | 125 | 63 | 72 | 76 | 84 | |
| P95 | ≥ 146 | 102 | 115 | 119 | 126 | 63 | 73 | 76 | 85 | |
| 10 | P5 | < 130 | 96 | 109 | 113 | 120 | 60 | 69 | 73 | 81 |
| P10 | 130–133 | 97 | 110 | 114 | 121 | 61 | 70 | 73 | 82 | |
| P25 | 134–138 | 99 | 112 | 116 | 123 | 62 | 71 | 75 | 83 | |
| P50 | 139–143 | 100 | 113 | 117 | 124 | 63 | 72 | 76 | 84 | |
| P75 | 144–147 | 101 | 115 | 119 | 126 | 63 | 73 | 76 | 85 | |
| P90 | 148–151 | 103 | 116 | 120 | 128 | 63 | 73 | 77 | 85 | |
| P95 | ≥ 152 | 103 | 117 | 121 | 129 | 64 | 73 | 77 | 86 | |
| 11 | P5 | < 136 | 98 | 112 | 115 | 122 | 62 | 71 | 75 | 83 |
| P10 | 136–139 | 99 | 113 | 116 | 123 | 62 | 72 | 75 | 84 | |
| P25 | 140–144 | 101 | 114 | 118 | 125 | 63 | 73 | 76 | 85 | |
| P50 | 145–149 | 102 | 116 | 120 | 127 | 64 | 73 | 77 | 86 | |
| P75 | 150–154 | 103 | 117 | 121 | 128 | 64 | 74 | 77 | 86 | |
| P90 | 155–157 | 104 | 118 | 122 | 129 | 64 | 74 | 77 | 86 | |
| P95 | ≥ 158 | 104 | 118 | 122 | 130 | 64 | 74 | 77 | 86 | |
| 12 | P5 | < 142 | 100 | 113 | 117 | 124 | 63 | 73 | 76 | 85 |
| P10 | 142–145 | 101 | 114 | 118 | 125 | 63 | 73 | 77 | 85 | |
| P25 | 146–150 | 102 | 116 | 120 | 127 | 64 | 74 | 77 | 86 | |
| P50 | 151–154 | 103 | 117 | 121 | 129 | 64 | 74 | 78 | 86 | |
| P75 | 155–158 | 104 | 118 | 122 | 130 | 64 | 74 | 78 | 87 | |
| P90 | 159–162 | 105 | 119 | 123 | 130 | 64 | 74 | 78 | 87 | |
| P95 | ≥ 163 | 105 | 119 | 123 | 131 | 64 | 74 | 78 | 87 | |
| 13 | P5 | < 147 | 101 | 115 | 119 | 126 | 64 | 74 | 77 | 86 |
| P10 | 147–149 | 102 | 116 | 120 | 127 | 64 | 74 | 78 | 87 | |
| P25 | 150–153 | 103 | 117 | 121 | 128 | 64 | 74 | 78 | 87 | |
| P50 | 154–157 | 104 | 118 | 122 | 129 | 65 | 74 | 78 | 87 | |
| P75 | 158–161 | 105 | 119 | 123 | 130 | 65 | 74 | 78 | 87 | |
| P90 | 162–164 | 105 | 119 | 123 | 131 | 65 | 74 | 78 | 87 | |
| P95 | ≥ 165 | 105 | 119 | 123 | 131 | 65 | 75 | 78 | 87 | |
| 14 | P5 | < 149 | 102 | 116 | 120 | 127 | 65 | 74 | 78 | 87 |
| P10 | 149–152 | 103 | 117 | 121 | 128 | 65 | 75 | 78 | 87 | |
| P25 | 153–155 | 104 | 118 | 122 | 129 | 65 | 75 | 78 | 87 | |
| P50 | 156–159 | 104 | 118 | 122 | 130 | 65 | 75 | 78 | 87 | |
| P75 | 160–163 | 105 | 119 | 123 | 130 | 65 | 75 | 78 | 87 | |
| P90 | 164–166 | 105 | 119 | 123 | 131 | 65 | 75 | 79 | 87 | |
| P95 | ≥ 167 | 106 | 120 | 124 | 131 | 65 | 75 | 79 | 88 | |
| 15 | P5 | < 151 | 103 | 116 | 120 | 128 | 65 | 75 | 79 | 87 |
| P10 | 151–152 | 103 | 117 | 121 | 128 | 65 | 75 | 79 | 88 | |
| P25 | 153–156 | 104 | 118 | 122 | 129 | 65 | 75 | 79 | 88 | |
| P50 | 157–160 | 105 | 119 | 123 | 130 | 65 | 75 | 79 | 88 | |
| P75 | 161–163 | 105 | 119 | 123 | 131 | 65 | 75 | 79 | 88 | |
| P90 | 164–166 | 105 | 120 | 124 | 131 | 65 | 75 | 79 | 88 | |
| P95 | ≥ 167 | 106 | 120 | 124 | 131 | 65 | 75 | 79 | 88 | |
| 16 | P5 | < 151 | 103 | 117 | 121 | 128 | 65 | 75 | 79 | 88 |
| P10 | 151–153 | 103 | 117 | 121 | 129 | 65 | 75 | 79 | 88 | |
| P25 | 154–157 | 104 | 118 | 122 | 130 | 65 | 75 | 79 | 88 | |
| P50 | 158–160 | 105 | 119 | 123 | 130 | 65 | 75 | 79 | 88 | |
| P75 | 161–164 | 105 | 119 | 123 | 131 | 66 | 76 | 79 | 88 | |
| P90 | 165–167 | 106 | 120 | 124 | 131 | 66 | 76 | 79 | 88 | |
| P95 | ≥ 168 | 106 | 120 | 124 | 132 | 66 | 76 | 79 | 88 | |
| 17 | P5 | < 152 | 103 | 117 | 121 | 129 | 66 | 76 | 79 | 88 |
| P10 | 152–154 | 104 | 118 | 122 | 129 | 66 | 76 | 79 | 89 | |
| P25 | 155–157 | 104 | 118 | 122 | 130 | 66 | 76 | 80 | 89 | |
| P50 | 158–161 | 105 | 119 | 123 | 130 | 66 | 76 | 80 | 89 | |
| P75 | 162–164 | 105 | 119 | 124 | 131 | 66 | 76 | 80 | 89 | |
| P90 | 165–167 | 106 | 120 | 124 | 132 | 66 | 76 | 80 | 89 | |
| P95 | ≥ 168 | 106 | 120 | 124 | 132 | 66 | 76 | 80 | 89 | |