Visual Abstract
Keywords: Blood microbiome; chronic kidney disease; Proteobacteria; DNA, Bacterial; DNA, Ribosomal; glomerular filtration rate; Enterobacteriaceae; Endotoxemia; Cross-Sectional Studies; Pilot Projects; Dysbiosis; Metagenomics; Microbiota; Pseudomonadaceae; Sequence Analysis, DNA; Polymerase Chain Reaction; Renal Insufficiency, Chronic; Permeability
Abstract
Background and objectives
The association between gut dysbiosis, high intestinal permeability, and endotoxemia-mediated inflammation is well established in CKD. However, changes in the circulating microbiome in patients with CKD have not been studied. In this pilot study, we compare the blood microbiome profile between patients with CKD and healthy controls using 16S ribosomal DNA sequencing.
Design, setting, participants, & measurements
Blood bacterial DNA was studied in buffy coat samples quantitatively by 16S PCR and qualitatively by 16S targeted metagenomic sequencing using a molecular pipeline specifically optimized for blood samples in a cross-sectional study comparing 20 nondiabetic patients with CKD and 20 healthy controls.
Results
There were 22 operational taxonomic units significantly different between the two groups. 16S metagenomic sequencing revealed a significant reduction in α diversity (Chao1 index) in the CKD group compared with healthy controls (127±18 versus 145±31; P=0.04). Proteobacteria phylum, Gammaproteobacteria class, and Enterobacteriaceae and Pseudomonadaceae families were more abundant in the CKD group compared with healthy controls. Median 16S ribosomal DNA levels did not significantly differ between CKD and healthy groups (117 versus 122 copies/ng DNA; P=0.38). GFR correlated inversely with the proportion of Proteobacteria (r=−0.54; P≤0.01).
Conclusions
Our pilot study demonstrates qualitative differences in the circulating microbiome profile with lower α diversity and significant taxonomic variations in the blood microbiome in patients with CKD compared with healthy controls.
Introduction
Complex assemblages of microorganisms unique to different human body sites are emerging as important modulators of human health and diseases (1). High-throughput sequencing methods have demonstrated that the human gut is symbiotically inhabited by thousands of bacterial species in diverse communities helping the host in digestion of complex carbohydrates, short-chain fatty acid generation, vitamin and amino acid synthesis, and shaping of the immune system (2,3). An imbalanced intestinal microbial community has been associated with various diseased states and is referred to as gut dysbiosis (4). Several studies have demonstrated an association between gut dysbiosis, inflammation, and CKD (5,6). Gut dysbiosis leading to disruption in intestinal barrier function in CKD permits translocation of gut-derived toxins, bacterial products, and intact bacteria into the circulation, resulting in inflammation (7,8). This circulating microbiome in CKD is indirectly evidenced by higher levels of endotoxins, LPS levels, and gut uremic toxins measured in blood (9,10). Recently, the existence of a highly diversified blood microbiome, including metagenomic profiles even in healthy human donors, has been found using 16S ribosomal DNA (rDNA) measurement (11). We hypothesized that patients with CKD would have a different quantitative and qualitative microbial profile in blood compared with controls. This deviation in the microbiome has the potential to provide an insight into the etiology and mechanisms of inflammation and associated outcomes in the CKD population. The aim of our pilot study was to measure the blood microbiome profile in nondialysis patients with CKD and compare them with healthy controls by comparing their quantitative 16S rDNA levels and qualitative metagenomic profiles.
Methods
Study Design
We conducted a cross-sectional pilot study including 20 patients with CKD and 20 healthy controls who had blood buffy coat samples in our hospital biobank.
Study Participants
Buffy coat samples of eligible patients were obtained from Partners Healthcare biobank. The Partners biobank comprises samples voluntarily obtained from individuals at any Partners-affiliated hospitals to foster research. Patients and healthy volunteers affiliated with the Partners Healthcare system can contribute their blood samples to the biobank after consenting and electronically filling out a health information survey. Their blood samples are drawn during a scheduled visit with a biobank staff or at the time of their clinic visit. These samples are made available to Partners Healthcare investigators with appropriate approval from the Partners Institutional Review Board (IRB protocol No. 2009P002312). They are linked to clinical data from the electronic medical record and categorized into healthy and various disease states as well as by other clinical characteristics enabling researchers to identify patients relevant to their study. The Partners ethics committee approved this study. The study adhered to the Declaration of Helsinki.
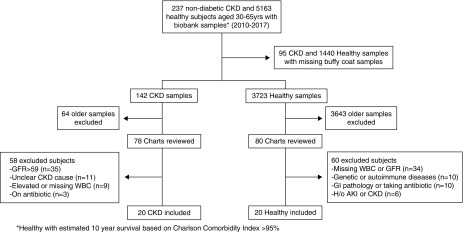
Patients with CKD of various nondiabetic etiologies, who were aged 30–65 years, with GFR 10–59 ml/min, and never on dialysis were eligible for inclusion. Patients with diabetes were excluded because of its ability to influence 16S rDNA levels, demonstrated by prior studies (12). Patients with clearly documented etiology were preferred. Healthy controls matched by age group 30–65 years and available buffy coat samples were randomly chosen using estimated 10-year survival >95%, determined by Charlson comorbidity index. Any patient with a white blood cell (WBC) count >109/L, evidence of active infection or on antibiotics during sample collection, or history of inflammatory bowel disease or prior intestinal surgery was excluded. Charts of eligible patients were reviewed preferring the latest available blood samples until 20 patients in each group were included (Figure 1). Demographics and covariates were obtained from electronic medical records.
Figure 1.
Enrollment of study participants. GI, gastrointestinal.
Sample Collection
Microbiome in blood predominantly exists in the buffy coat (11). For analysis, samples were first thawed under sterile precautions. DNA extraction, 16S rDNA quantitative PCR, and qualitative 16S targeted metagenomic sequencing was performed by Vaiomer (Vaiomer, Toulouse, France). The testing laboratory was blinded to the two groups. The primary aim was to compare quantitative 16S rDNA levels and qualitative bacterial profiles between the two groups. The secondary aim was to look for any correlation between 16S rDNA levels and GFR.
16S DNA Extraction and Quantification
DNA was extracted from these samples using an optimized tissue-specific technique. Total genomic DNA was collected in a final 50 μl extraction volume. Total DNA concentrations were determined by ultraviolet spectroscopy. Total 16S rDNA present in the samples was measured by quantitative PCR in triplicates using 16S universal primers targeting the V3–V4 region of the bacterial 16S ribosomal gene and normalized using a plasmid-based standard scale, details of which have been described previously (11,13). In these experiments, the efficiency calculated from the standard curve was required to be between 80% and 120%, and the R2 of the standard curve was >0.980. After successful extraction and amplification, 16S rDNA was measured as 16S copy number per nanogram of DNA in triplicates and fell within the standard curve range.
16S Metagenomic Sequencing
Library preparation was performed by two-step PCR amplification using 16S universal primers targeting the V3–V4 region of the bacterial 16S ribosomal gene (Vaiomer universal 16S primers) as described previously (14). The resulting amplicon of approximately 467 base pairs (as in Escherichia coli 16S) was sequenced using 2×300 paired-end MiSeq kit V3. For each sample, a sequencing library was generated by addition of sequencing adapters. The detection of the sequencing fragments was performed using MiSeq Illumina technology.
The targeted metagenomic sequences from microbiota were analyzed using the bioinformatics pipeline established by Vaiomer from the Find, Rapidly, OTUs with Galaxy Solution guidelines (15). Briefly, after demultiplexing of the barcoded Illumina paired reads, single-read sequences are cleaned and paired for each sample independently into longer fragments. Operational taxonomic units (OTUs) are produced via single-linkage clustering using the Swarm algorithm and its adaptive sequence agglomeration (15). The taxonomic assignment is performed against the Silva v132 database to determine community profiles. The following specific filters were applied for this analysis to obtain the best results: (1) the last ten bases of reads R1 were removed; (2) the last 50 bases of reads R2 were removed; (3) amplicons with a length of <350 or >500 nucleotides were removed; (4) OTUs with abundance <0.1% of the whole dataset abundance and undetectable in half of the samples in both groups were removed.
α and β diversities were compared between the two groups (1). α diversity measures the richness of taxa within each sample. We used the Chao1 index which determines the diversity from the abundance data (observed taxa) and an estimation of the unobserved taxa (unobserved rare taxa) (16). β diversity allows for comparison of the taxonomic profiles between pairs of individual samples. We measured the β diversity looking at the OTU distribution of each sample using the weighted UniFrac technique, which calculates the distance between pairs of samples on the basis of the abundance and phylogenetic relatedness of observed taxa (17).
Statistical Analyses
SAS version 9.4 was used for statistical analysis to compare demographics and microbiome differences between groups. Demographic characteristics between CKD and healthy groups were compared by t test, Mann–Whitney U test, chi-squared test, and Fisher exact test, as appropriate. Variances in 16S rDNA levels were compared between groups using the F test. Total 16S rDNA levels and differences in α diversity were compared between groups using Mann–Whitney U test. Proportion differences between groups for the four major phyla (Proteobacteria, Bacteroidetes, Firmicutes, and Actinobacteria) were compared using Mann–Whitney U test, and P values were adjusted for multiple comparisons using the Benjamini–Hochberg method to control the false discovery rate (FDR) (18). Given the proportions of phyla varying between 0 and 1, multivariable β regression models were used to adjust for potential confounders, which included age, body mass index (BMI), WBC, hypertension, hyperlipidemia, and history of immunosuppressant intake. Linear discriminant analysis effect size (LEfSe) algorithm (R version 3.4.4) was used to measure OTU differences between groups (19). Because Proteobacteria was the only phylum significantly different between the two groups on the LEfSe, further testing for differences in OTU was only performed within this phylum by Mann–Whitney U test. For each group, correlations between GFR and 16S rDNA quantitative levels, proportion of Proteobacteria, age, and BMI were calculated using Spearman rank order correlation or Pearson correlation coefficients, as appropriate. Two-tailed P values (including FDR-adjusted P values) of <0.05 were deemed statistically significant.
Results
Baseline Characteristics
Baseline characteristics of the 40 patients are shown in Table 1. Although all patients were aged 30–65 years, the CKD cohort had a higher mean age. BMI and prevalence of hypertension and hyperlipidemia was higher in the CKD group, as expected. There was no significant difference in serum albumin levels, WBC count, or prior antibiotic use between groups. There was a higher prevalence of prior steroid or immunosuppressant use in the CKD group, as expected for treatment of underlying etiology, and three patients were on active treatment at the time of sample collection. This group included patients with glomerular etiologies such as lupus plus ANCA nephritis, collapsing FSGS, and rheumatoid arthritis–induced kidney amyloidosis. Prior antibiotic and immunosuppressant use was defined as more than 1 month prior but within 2 years of sample collection. Steroid and immunosuppression treatment in patients with CKD given primarily for kidney disease included patients with lupus nephritis, immune complex–mediated GN, IgG4-related kidney disease, antiphospholipid antibody, and two patients with interstitial cystitis with reflux nephropathy, about 6 months before sample collection. Two patients with CKD received immunosuppression unrelated to their kidney disease. This included use of Bacillus Calmette-Guerin for bladder cancer (last dose more than 1 month before sample collection) and chemotherapy for non-Hodgkin lymphoma (more than 1 year before sample collection). Among healthy controls, two patients had a history of receiving immunosuppression. This included oral prednisone for optic neuritis a year before sample collection and natalizumab for multiple sclerosis more than 2 months before sample collection.
Table 1.
Baseline characteristics of the microbiome study sample
| Variable | CKD Group, n=20 | Healthy Controls, n=20 |
|---|---|---|
| Age, yr | 56 (49, 61) | 44 (39, 53) |
| Men, n (%) | 11 (55) | 7 (35) |
| White, n (%) | 17 (85) | 20 (100) |
| Body mass index, kg/m2a | 31.2 (27.1, 32.9) | 24.7 (22.1, 27.1) |
| White blood cell, per μl | 6.5 (5.9, 8.6) | 6.3 (4.4, 8.1) |
| Hypertension, n (%) | 17 (85) | 3 (15) |
| Hyperlipidemia, n (%)a | 14 (18) | 7 (42) |
| Serum albumin g/dla | 4.3 (0.3) | 4.5 (0.4) |
| Prior antibiotic use, n (%)b | 10 (50) | 11 (55) |
| Prior or current steroid or immunosuppression use, n (%)b | 11 (55) | 2 (10) |
| eGFR, ml/min | 42 (35, 49) | 86 (80, 91) |
| 16S DNA, copies/ng DNA | 117 (84, 162) | 122 (114, 148) |
Significant differences between groups detected in age, body mass index, hypertension, hyperlipidemia, eGFR, and prior use of immunosuppression. Data are expressed as median (25th, 75th quartile), mean (SD), or n (%) as appropriate.
Missing values; eGFR determined using the CKD Epidemiology Collaboration equation.
Use within past 2 years but more than 1 month before sample collection.
Blood Bacterial 16S rDNA Concentration
Comparison of bacterial 16S rDNA quantity between the two groups of patients (Supplemental Figure 1) showed more variability within the CKD group (F statistic =4.30; degrees of freedom=[19, 19]; P=0.002). 16S levels significantly correlated with WBC (r=0.55; P=0.01). Median blood 16S rDNA concentration was similar between CKD and healthy groups (117 versus 122 copies/ng DNA; P=0.38). After adjusting for covariates (BMI, WBC, age, albumin, hypertension, hyperlipidemia, and immunosuppression), we found no significant difference in 16S levels between the two groups (P=0.16). We then performed a sensitivity analysis after excluding three participants who were on immunosuppressants. The overall adjusted model was still nonsignificant (P=0.16).
16S Metagenomic Sequencing
α and β Diversity.
There was a significant decrease in α diversity (richness of bacterial taxa) using Chao1 index (127±18 versus 145±31; P=0.04) in the CKD group compared with healthy controls (Figure 2A). We did not observe major separation in β diversity (bacterial community) between groups using the weighted UniFrac technique (Figure 2B).
Figure 2.
CKD group had a lower α diversity and similar β diversity compared to the healthy group. (A) α diversity (Chao1 index) measuring bacterial richness. (B) β diversity (Weighted UniFrac technique) showing distance between samples summarized in two dimensions, with individual points representing OTU distribution of each sample. Larger overlap indicating similar β diversity between groups.
Taxonomic Signature Analysis.
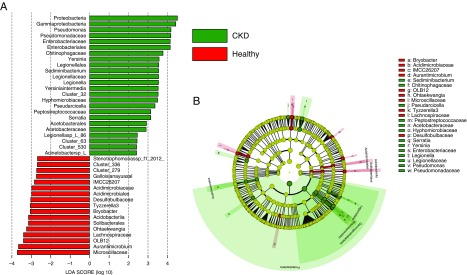
We performed a taxonomic assignment of the 16S rDNA bacterial sequences and analyzed for each patient’s taxonomic profile, using the LEfSe algorithm representing significant differences between groups at all taxonomic levels (Figure 3A). Cladogram represents these differences at various phylogenic levels starting from phylum level at the center to subphylum levels toward the periphery (Figure 3B). For clarity, taxa assigned to unknown and multiaffiliations are not shown in this figure. There were total 22 significant OTU differences between groups (Table 2). At the phylum level, microbiome in blood was composed primarily of Proteobacteria followed by Bacteroidetes, Actinobacteria, and Firmicutes, comprising approximately 98% of all phyla (Figure 4). We compared the differences in these four phyla between the CKD and healthy groups. The proportion of Proteobacteria was significantly higher in the CKD group compared with healthy controls (61% versus 54%; P values were 0.004 and 0.03 before and after multiple testing adjustment by FDR, respectively). No significant difference was observed in the Bacteroidetes (19% versus 21%; P=0.76), Actinobacteria (15% versus 18%; P=0.36), or Firmicutes (3% versus 4%; P=0.76) phyla between groups. On looking deeper within the Proteobacteria phylum, class Gammaproteobacteria was significantly higher in the CKD group (45% versus 38%; P=0.01). Within Gammaproteobacteria, families Enterobacteriaceae and Pseudomonadaceae were significantly higher in the CKD group compared with healthy controls (10% versus 7%; P=0.03 and 23% versus 18%; P=0.03, respectively). After adjusting for covariates (age, BMI, WBC, hypertension, hyperlipidemia and immunosuppression use), we found statistically significant differences in Proteobacteria phylum and Gammaproteobacteria class between groups, but not in families Enterobacteriaceae and Pseudomonadaceae (Table 3).
Figure 3.
Linear discriminant analysis Effect Size (LEfSe) showing microbiome differences between groups at various taxonomic levels. (A) LEfSe analysis with linear discriminant analysis (LDA) score representing statistical and biological differences in phyla between groups. (B) LEfSe cladogram demonstrating microbiome differences at various phylogenic levels.
Table 2.
Major taxonomic differences between CKD and healthy groups
| Higher in Group | Phylum | Class | Order | Family | Genus | No. of Speciesa |
|---|---|---|---|---|---|---|
| CKD | Proteobacteria | Gammaproteobacteria | Legionellales | Legionellaceae | Legionella | 1 |
| Enterobacteriales | Enterobacteriaceae | Serratia | 1 | |||
| Enterobacteriales | Enterobacteriaceae | Yersinia | 1 | |||
| Pseudomonadales | Moraxellaceae | Acinetobacter | 3 | |||
| Pseudomonadales | Pseudomonadaceae | Pseudomonas | 2 | |||
| Xanthomonadales | Xanthomonadaceae | Lysobacter | 1 | |||
| Alphaproteobacteria | Rhizobiales | Hyphomicrobiaceae | Hyphomicrobium | 1 | ||
| Firmicutes | Bacilli | Bacillales | Bacillaceae | Bacillus | 2 | |
| Bacteroidetes | Bacteroidia | Chitinophagales | Chitinophagaceae | Sediminibacterium | 2 | |
| Bacteroidia | Cytophagales | Spirosomaceae | Pseudarcicella | 1 | ||
| Healthy | Proteobacteria | Gammaproteobacteria | Xanthomonadales | Xanthomonadaceae | Stenotrophomonas | 1 |
| Alphaproteobacteria | Rhodobacterales | Rhodobacteraceae | Paracoccus | 2 | ||
| Sphingomonadales | Sphingomonadaceae | Sphingomonas | 1 | |||
| Firmicutes | Clostridia | Clostridiales | Lachnospiraceae | Tyzzerella | 1 | |
| Actinobacteria | Actinobacteria | Corynebacteriales | Corynebacteriaceae | Corynebacterium | 1 | |
| Actinobacteria | Micrococcales | Microbacteriaceae | Candidatus | 1 |
Exact species difficult to identify because of clustering and multiple affiliations of species.
Figure 4.
Relative proportion of taxa at phylum levels demonstrating a higher proportion of Proteobacteria phylum in the CKD group.
Table 3.
Distribution of Proteobacteria phylum and its major subphyla between CKD and healthy groups
| Taxonomic Level | Taxon | CKD, n=20; Median, % (IQR) | Healthy, n=20; Median, % (IQR) | P Value Raw | P Value Adjusteda |
|---|---|---|---|---|---|
| Phylum | Proteobacteria | 61 (57, 65) | 54 (49, 57) | 0.004 | 0.002 |
| Class | Gammaproteobacteria | 45 (43, 47) | 38 (32, 44) | 0.01 | 0.03 |
| Family | Enterobacteriaceae | 10 (8,12) | 7 (3, 11) | 0.03 | 0.09 |
| Pseudomonadaceae | 23 (17, 25) | 18 (15, 21) | 0.03 | 0.17 |
IQR, interquartile range.
Adjusted for age, body mass index, white blood cell count, hypertension, hyperlipidemia, and immunosuppressant intake history.
Correlation Analysis
GFR did not significantly correlate with 16S rDNA quantitative levels (r=−0.002; P=0.98) or α diversity on the basis of Chao index (r=0.25; P=0.11). However, GFR had a strong inverse correlation with the Proteobacteria phylum, with a higher proportion of Proteobacteria detected in patients with lower GFR (r=−0.54; P ≤0.01). When correlated separately between groups, it remained significant in the healthy group (r=−0.56; P=0.009) but not in the CKD group (r=−0.15; P=0.52). There was no significant correlation of age or BMI with GFR or Proteobacteria in either groups (Supplemental Figure 2).
Discussion
Previous studies have reported significant alterations in gut microbiome profiles in patients with CKD (20). Although previous studies have used circulating levels of bacterial LPS and serum endotoxin levels as a surrogate for blood microbiome, our study successfully compares the blood microbiome between patients with CKD and healthy controls for the first time by quantitative 16S PCR and qualitative 16S targeted metagenomic sequencing (21). We observed that patients with CKD had a significantly lower α diversity and 22 major taxonomic differences compared with healthy controls. Although β diversity and median 16S rDNA levels remained similar between the two groups, Proteobacteria phylum, Gammaproteobacteria class, and Enterobacteriaceae and Pseudomonadaceae families were more abundant in the CKD group.
The gut microbiome is involved in numerous physiologic processes, including nutrient extraction, metabolism, and immune regulation (22,23). Gut dysbiosis is frequently characterized by decreased α diversity and relative abundance of selected microbial taxa (24). Pathologic features of gut dysbiosis include generation of adverse metabolites, higher endotoxin release, augmentation of proinflammatory signals, and higher permeability to gut-derived molecules, permitting them to enter the systemic circulation (25,26). Higher intestinal permeability has been associated with CKD, metabolic syndrome, and cardiovascular diseases (8,27). High urea levels in CKD is converted to ammonia, resulting in the disruption of intestinal tight junctions and translocation of gut toxins into blood (28,29). α diversity is a measure of richness in bacterial taxa within a sample. α diversity has been observed to be decreased in a dysbiotic gut and is associated with various chronic disease states such as autoimmune diseases, diabetes, metabolic syndrome, autism, and colorectal cancer (30). Low α diversity has also been associated with higher arterial stiffness (31). Analogous to this, our study also shows a lower α diversity in the blood of patients with CKD, suggesting a possible association of diseased state with lower bacterial richness.
Although the presence of bacterial DNA in blood is well recognized, its source remains a topic of considerable deliberation. Contrary to Louis Pasteur’s monomorphic germ theory, bacteria in blood was described by Antoine Béchamp and Günther Enderlein as pleomorphic organisms developing into pathogenic or apathogenic forms, depending on the environmental conditions (32,33). Several other studies have also proposed the hypothesis of pleomorphism of bacteria in healthy blood (34). With the discovery of L-forms (cell wall–deficient nonculturable bacterial forms that reproduce asexually) (35) and advanced DNA sequencing techniques to detect bacterial DNA from blood (11), it has been proven that the microbiome can exist in dormant, viable, or nonviable forms and undergo pleomorphism in response to the environmental conditions (36). Molecular studies have shown that bacterial cytosine–guanosine dinucleotides exist in nonstimulatory methylated forms in vertebrate DNA, and their epigenetic unmethylation under inflamed conditions can stimulate the immune system in an analogous manner to bacterial LPS (37). We hypothesize that analogous to stem cells, primitive bacterial L-forms may be undergoing pleomorphic changes and developing into different bacterial forms depending on the ecosystem of the body site, which explains why specific microbial communities tend to adapt to specific body sites. A shift in the microbiome can occur if there is a change in the ecosystem. In our case, the microbiome in blood may be undergoing pleomorphic changes in response to the ecosystem in blood formed from translocation of gut toxins, retention of uremic toxins, and decreased GFR, as well as other lifestyle-related factors, medications, and comorbid conditions. This change in ecosystem causes a shift in the microbiome resulting in qualitative differences between groups as well as individual variations within groups.
The intestinal membrane, liver, and the immune system also act as filters responsible for differences in the microbiome (38). In our study, the quantity of 16S rDNA significantly correlated with the WBC count but was similar between the two groups, suggesting that it possibly depends on the immune system function. Significantly higher 16S levels in blood have been observed in patients with liver disease, possibly due to decreased clearance and diminished compensation of the immune system (13). Large individual variations in quantitative 16S levels within the CKD group may be due to varying levels of WBC, differing levels of immune system compensation, or other potential confounders.
Although microbiome profiles vary between individuals, the human microbiome project has shown more variations between different body sites within an individual compared with similar body sites between individuals, suggesting that it tends to specifically adapt to the host body site (1,39). Similarly, our results show a significant difference in the blood microbiome compared with the gut microbiome, demonstrating higher Proteobacteria and Actinobacteria predominance in the blood in contrast to Bacteroidetes and Firmicutes, which normally dominate the gut (13,40). Although one of the possible reasons is a leak in the intestinal membrane barrier, we hypothesize that this is from bacterial pleomorphic adaptation to the ecosystem of gut and blood as explained above. Because β diversity measures the interindividual differences in taxa distribution within a specific body site, it tends to be relatively similar within that specific body site, blood in this case. Therefore, despite high interindividual variations in blood bacterial profiles observed at the OTU level, overall proportions of different bacteria in the blood at the phylum level are relatively constant, making them genetically closely related and less β diverse.
Proteobacteria is a major phylum of Gram-negative bacteria, which includes a wide variety of pathogens, such as Escherichia, Salmonella, Vibrio, Yersinia, Pseudomonas, and many other genera (41). Proteobacteria has been found to be higher both in the gut and blood in many chronic inflammatory diseases, including inflammatory bowel disease, metabolic syndrome, cardiovascular diseases, and chronic lung diseases, and has also been detected in atherosclerotic plaques (42−44). We noticed a similar rise in Proteobacteria in CKD in our study, likely an effect of increasing severity of CKD. The correlation of all these diseases with gut dysbiosis, intestinal bacterial translocation, and endotoxemia-related inflammation, as well as their clinical association with each other, suggests a common mechanism underlying these diseases associated with inflammation, arising from the gut. Interestingly, evolution of mitochondria has been linked to Proteobacteria on the basis of their striking similarities and widely accepted endosymbiotic theory of evolution, which hypothesizes that mitochondria evolved from endosymbiosis of Proteobacteria inside host cells, forming mitochondria (45,46). It is possible that the Proteobacteria increase in chronic inflammatory diseases could be an effect of being released into blood after cell death in the above organs. Further studies are needed to explore this.
Our pilot study has successfully showed variations in the blood microbiome profile between nondiabetic patients with CKD and healthy controls. With the increasing importance of epigenetic influences on human health and diseased states, the blood microbiome may serve as a personalized biomarker for CKD etiology and prognosis as well as provide potential therapeutic interventional targets aimed at restoring a healthier microbiome state. So far, various therapeutic strategies with prebiotics, probiotics, and synbiotics have been attempted to restore gut dysbiosis in CKD, with encouraging results, but longitudinal studies measuring kidney outcomes are lacking (47,48). Feeding high amylose-resistant, fiber-rich starch diet in CKD mouse models has ameliorated inflammation by mitigating gut dysbiosis, and correlated with improved kidney function (49,50). Understanding the microbiome in blood and correlating with gut may help in developing targeted probiotic drugs and interventions aimed at restoring the intestinal membrane barrier.
Our study has several limitations. Our study sample is small and not powered to detect a clear association between CKD etiology and blood microbiome profiles. The patients with CKD heterogenous with various etiologies are not a clear representative of CKD overall. Confounding cannot be excluded because of the cross-sectional observational design of the study. Our study lacked associated measurement of stool microbiome, inflammatory markers, rate of CKD progression, and environmental epigenetic factors such as food habits and stress, which are all known to influence the microbiome. Concurrent stool microbiome measurement would have helped compare the diversity and dysbiosis of gut microbes with blood microbes and understand the crosstalk between them. Prior use of antibiotics and immunosuppression more than a month before sample collection date was determined on the basis of chart review, assuming patients did not get any prescriptions from out of network providers. The effect of immunosuppressant drugs on the microbiome is unclear. However, the primary goal of our pilot study was to demonstrate that a varied blood microbiome exists in patients with CKD. In this context, our study is a first, promising proof of concept and opens a novel pathway for using the blood microbiome as a potential diagnostic and therapeutic tool in CKD. The above limitations should be addressed in future studies.
In summary, our study successfully demonstrates variations in blood microbiome profiles between patients with CKD and healthy controls. We show a reduction in α diversity and distinct variations in taxonomic profiles between the two groups, with a significant rise in the Proteobacteria phylum in patients with CKD. Such a rise in Proteobacteria has been observed in other chronic diseases such as metabolic syndrome and cardiovascular diseases, indicating that inflammation originating from gut bacterial translocation into blood is the common underlying mechanism in these diseases, resulting in pleomorphic shifts in microbial profile in blood. Although therapeutic interventions aimed at restoring intestinal membrane and bacterial flora may be future targets, current blood microbiome studies are limited, necessitating further research. Our findings are based on a small study of 20 patients with CKD. Further large-scale studies correlating blood microbiome with gut microbiome, intestinal permeability markers, inflammatory markers, epigenetic factors, and various etiologies of CKD are needed to better interpret the blood microbiome as a potential diagnostic biomarker, and to identify therapeutic targets in these patients.
Disclosures
Dr. Fasano reports personal fees from AbbVie, other funding from Alba Therapeutics, personal fees from Innovate Biopharmaceuticals, personal fees from Mead Johnson Nutrition, personal fees from Takeda, and personal fees from uBiome, outside the submitted work. Dr. Allegretti, Dr. Kalim, Dr. Lelouvier, Dr. Nigwekar, Dr. Raj, Dr. Serena, Dr. Servant, Dr. Shah, Dr. Thadhani, and Dr. Zhao have nothing to disclose.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.12161018/-/DCSupplemental.
Supplemental Figure 1. Distribution of 16S copies per ng of DNA among CKD and healthy groups.
Supplemental Figure 2. Correlation in CKD and healthy groups between (A) Proteobacteria versus eGFR, (B) age versus eGFR, and (C) BMI versus eGFR.
Supplementary Material
Acknowledgments
We thank Partners Healthcare Biobank for providing samples, genomic data, and health information data.
All authors contributed to the study. Dr. Shah designed the study and drafted the manuscript. Dr. Nigwekar and Dr. Kalim helped with data acquisition and manuscript revision. Dr. Zhao helped with statistical analysis. Dr. Serena assisted with sample transfer. Dr. Lelouvier and Dr. Servant ran the blood microbiome analysis, generated output, and helped with interpretation. Dr. Thadhani helped with study design and participated in conference calls. Dr. Raj helped with literature content and revision of the manuscript and Dr. Fasano helped with interpretation and approval of the final version.
This study was internally funded by Massachusetts General Hospital Kidney divisional funds.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
See related editorial, “Blood Microbiome in CKD: Should We Care?,” on pages 648–649.
References
- 1.Human Microbiome Project Consortium : Structure, function and diversity of the healthy human microbiome. Nature 486: 207–214, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hooper LV, Gordon JI: Commensal host-bacterial relationships in the gut. Science 292: 1115–1118, 2001 [DOI] [PubMed] [Google Scholar]
- 3.Hooper LV, Bry L, Falk PG, Gordon JI: Host-microbial symbiosis in the mammalian intestine: Exploring an internal ecosystem. BioEssays 20: 336–343, 1998 [DOI] [PubMed] [Google Scholar]
- 4.Wang B, Yao M, Lv L, Ling Z, Li L: The human microbiota in health and disease. Engineering 3: 71–82, 2017 [Google Scholar]
- 5.Evenepoel P, Poesen R, Meijers B: The gut-kidney axis. Pediatr Nephrol 32: 2005–2014, 2017 [DOI] [PubMed] [Google Scholar]
- 6.Vaziri ND, Wong J, Pahl M, Piceno YM, Yuan J, DeSantis TZ, Ni Z, Nguyen TH, Andersen GL: Chronic kidney disease alters intestinal microbial flora. Kidney Int 83: 308–315, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Brenchley JM, Douek DC: Microbial translocation across the GI tract. Annu Rev Immunol 30: 149–173, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaziri ND, Zhao YY, Pahl MV: Altered intestinal microbial flora and impaired epithelial barrier structure and function in CKD: The nature, mechanisms, consequences and potential treatment. Nephrol Dial Transplant 31: 737–746, 2016 [DOI] [PubMed] [Google Scholar]
- 9.Aronov PA, Luo FJ, Plummer NS, Quan Z, Holmes S, Hostetter TH, Meyer TW: Colonic contribution to uremic solutes. J Am Soc Nephrol 22: 1769–1776, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andersen K, Kesper MS, Marschner JA, Konrad L, Ryu M, Kumar Vr S, Kulkarni OP, Mulay SR, Romoli S, Demleitner J, Schiller P, Dietrich A, Müller S, Gross O, Ruscheweyh HJ, Huson DH, Stecher B, Anders HJ: Intestinal dysbiosis, barrier dysfunction, and bacterial translocation account for CKD-related systemic inflammation. J Am Soc Nephrol 28: 76–83, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Païssé S, Valle C, Servant F, Courtney M, Burcelin R, Amar J, Lelouvier B: Comprehensive description of blood microbiome from healthy donors assessed by 16S targeted metagenomic sequencing. Transfusion 56: 1138–1147, 2016 [DOI] [PubMed] [Google Scholar]
- 12.Amar J, Serino M, Lange C, Chabo C, Iacovoni J, Mondot S, Lepage P, Klopp C, Mariette J, Bouchez O, Perez L, Courtney M, Marre M, Klopp P, Lantieri O, Doré J, Charles M, Balkau B, Burcelin R; D.E.S.I.R. Study Group : Involvement of tissue bacteria in the onset of diabetes in humans: Evidence for a concept. Diabetologia 54: 3055–3061, 2011 [DOI] [PubMed] [Google Scholar]
- 13.Lelouvier B, Servant F, Païssé S, Brunet AC, Benyahya S, Serino M, Valle C, Ortiz MR, Puig J, Courtney M, Federici M, Fernández-Real JM, Burcelin R, Amar J: Changes in blood microbiota profiles associated with liver fibrosis in obese patients: A pilot analysis. Hepatology 64: 2015–2027, 2016 [DOI] [PubMed] [Google Scholar]
- 14.Lluch J, Servant F, Païssé S, Valle C, Valière S, Kuchly C, Vilchez G, Donnadieu C, Courtney M, Burcelin R, Amar J, Bouchez O, Lelouvier B: The characterization of novel tissue microbiota using an optimized 16S metagenomic sequencing pipeline. PLoS One 10: e0142334, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Escudié F, Auer L, Bernard M, Mariadassou M, Cauquil L, Vidal K, Maman S, Hernandez-Raquet G, Combes S, Pascal G: FROGS: Find, rapidly, OTUs with galaxy solution. Bioinformatics 34: 1287–1294, 2018 [DOI] [PubMed] [Google Scholar]
- 16.Hughes JB, Hellmann JJ, Ricketts TH, Bohannan BJ: Counting the uncountable: Statistical approaches to estimating microbial diversity. Appl Environ Microbiol 67: 4399–4406, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lozupone CA, Hamady M, Kelley ST, Knight R: Quantitative and qualitative beta diversity measures lead to different insights into factors that structure microbial communities. Appl Environ Microbiol 73: 1576–1585, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glickman ME, Rao SR, Schultz MR: False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J Clin Epidemiol 67: 850–857, 2014 [DOI] [PubMed] [Google Scholar]
- 19.Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, Huttenhower C: Metagenomic biomarker discovery and explanation. Genome Biol 12: R60, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Anders HJ, Andersen K, Stecher B: The intestinal microbiota, a leaky gut, and abnormal immunity in kidney disease. Kidney Int 83: 1010–1016, 2013 [DOI] [PubMed] [Google Scholar]
- 21.McIntyre CW, Harrison LE, Eldehni MT, Jefferies HJ, Szeto CC, John SG, Sigrist MK, Burton JO, Hothi D, Korsheed S, Owen PJ, Lai KB, Li PK: Circulating endotoxemia: A novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin J Am Soc Nephrol 6: 133–141, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cho I, Blaser MJ: The human microbiome: At the interface of health and disease. Nat Rev Genet 13: 260–270, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Levy M, Kolodziejczyk AA, Thaiss CA, Elinav E: Dysbiosis and the immune system. Nat Rev Immunol 17: 219–232, 2017 [DOI] [PubMed] [Google Scholar]
- 24.Le Chatelier E, Nielsen T, Qin J, Prifti E, Hildebrand F, Falony G, Almeida M, Arumugam M, Batto JM, Kennedy S, Leonard P, Li J, Burgdorf K, Grarup N, Jørgensen T, Brandslund I, Nielsen HB, Juncker AS, Bertalan M, Levenez F, Pons N, Rasmussen S, Sunagawa S, Tap J, Tims S, Zoetendal EG, Brunak S, Clément K, Doré J, Kleerebezem M, Kristiansen K, Renault P, Sicheritz-Ponten T, de Vos WM, Zucker JD, Raes J, Hansen T, Bork P, Wang J, Ehrlich SD, Pedersen O; MetaHIT consortium : Richness of human gut microbiome correlates with metabolic markers. Nature 500: 541–546, 2013 [DOI] [PubMed] [Google Scholar]
- 25.Levy M, Thaiss CA, Zeevi D, Dohnalová L, Zilberman-Schapira G, Mahdi JA, David E, Savidor A, Korem T, Herzig Y, Pevsner-Fischer M, Shapiro H, Christ A, Harmelin A, Halpern Z, Latz E, Flavell RA, Amit I, Segal E, Elinav E: Microbiota-modulated metabolites shape the intestinal microenvironment by regulating NLRP6 inflammasome signaling. Cell 163: 1428–1443, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Org E, Blum Y, Kasela S, Mehrabian M, Kuusisto J, Kangas AJ, Soininen P, Wang Z, Ala-Korpela M, Hazen SL, Laakso M, Lusis AJ: Relationships between gut microbiota, plasma metabolites, and metabolic syndrome traits in the METSIM cohort. Genome Biol 18: 70, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jie Z, Xia H, Zhong S-L, Feng Q, Li S, Liang S, Zhong H, Liu Z, Gao Y, Zhao H, Zhang D, Su Z, Fang Z, Lan Z, Li J, Xiao L, Li J, Li R, Li X, Li F, Ren H, Huang Y, Peng Y, Li G, Wen B, Dong B, Chen JY, Geng QS, Zhang ZW, Yang H, Wang J, Wang J, Zhang X, Madsen L, Brix S, Ning G, Xu X, Liu X, Hou Y, Jia H, He K, Kristiansen K: The gut microbiome in atherosclerotic cardiovascular disease. Nat Commun 8: 845, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ramezani A, Massy ZA, Meijers B, Evenepoel P, Vanholder R, Raj DS: Role of the gut microbiome in uremia: A potential therapeutic target. Am J Kidney Dis 67: 483–498, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaziri ND, Yuan J, Rahimi A, Ni Z, Said H, Subramanian VS: Disintegration of colonic epithelial tight junction in uremia: A likely cause of CKD-associated inflammation. Nephrol Dial Transplant 27: 2686–2693, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mosca A, Leclerc M, Hugot JP: Gut microbiota diversity and human diseases: Should we reintroduce key predators in our ecosystem? Front Microbiol 7: 455, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Menni C, Lin C, Cecelja M, Mangino M, Matey-Hernandez ML, Keehn L, Mohney RP, Steves CJ, Spector TD, Kuo CF, Chowienczyk P, Valdes AM: Gut microbial diversity is associated with lower arterial stiffness in women. Eur Heart J 39: 2390–2397, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Manchester KL: Antoine Béchamp: Pere de la biologie. Oui ou non? Endeavour 25: 68–73, 2001 [DOI] [PubMed] [Google Scholar]
- 33.Kritschewski IL, Ponomarewa IW: On the pleomorphism of bacteria: I. On the pleomorphism of B. Paratyphi B. J Bacteriol 28: 111–126, 1934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McLaughlin RW, Vali H, Lau PC, Palfree RG, De Ciccio A, Sirois M, Ahmad D, Villemur R, Desrosiers M, Chan EC: Are there naturally occurring pleomorphic bacteria in the blood of healthy humans? J Clin Microbiol 40: 4771–4775, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Errington J, Mickiewicz K, Kawai Y, Wu LJ. L-form bacteria, chronic diseases and the origins of life. Philos Trans R Soc B Biol Sci 371, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Potgieter M, Bester J, Kell DB, Pretorius E: The dormant blood microbiome in chronic, inflammatory diseases. FEMS Microbiol Rev 39: 567–591, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Häcker H, Vabulas RM, Takeuchi O, Hoshino K, Akira S, Wagner H: Immune cell activation by bacterial CpG-DNA through myeloid differentiation marker 88 and tumor necrosis factor receptor-associated factor (TRAF)6. J Exp Med 192: 595–600, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hand TW, Vujkovic-Cvijin I, Ridaura VK, Belkaid Y: Linking the microbiota, chronic disease, and the immune system. Trends Endocrinol Metab 27: 831–843, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lloyd-Price J, Abu-Ali G, Huttenhower C: The healthy human microbiome. Genome Med 8: 51, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schierwagen R, Alvarez-Silva C, Madsen MSA, Kolbe CC, Meyer C, Thomas D, Uschner FE, Magdaleno F, Jansen C, Pohlmann A, Praktiknjo M, Hischebeth GT, Molitor E, Latz E, Lelouvier B, Trebicka J, Arumugam M: Circulating microbiome in blood of different circulatory compartments [published online ahead of print March 26, 2018]. Gut 2018 [DOI] [PubMed] [Google Scholar]
- 41.Stackebrandt E, Murray RGE, Truper HG: Proteobacteria classis nov., a name for the phylogenetic taxon that includes the “purple bacteria and their relatives.”. Int J Syst Bacteriol 38: 321–325, 1988 [Google Scholar]
- 42.Rizzatti G, Lopetuso LR, Gibiino G, Binda C, Gasbarrini A: Proteobacteria: A common factor in human diseases. BioMed Res Int 2017: 9351507, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amar J, Lange C, Payros G, Garret C, Chabo C, Lantieri O, Courtney M, Marre M, Charles MA, Balkau B, Burcelin R; D.E.S.I.R. Study Group : Blood microbiota dysbiosis is associated with the onset of cardiovascular events in a large general population: The D.E.S.I.R. Study. PLoS One 8: e54461, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Calandrini CA, Ribeiro AC, Gonnelli AC, Ota-Tsuzuki C, Rangel LP, Saba-Chujfi E, Mayer MP: Microbial composition of atherosclerotic plaques. Oral Dis 20: e128–e134, 2014 [DOI] [PubMed] [Google Scholar]
- 45.Degli Esposti M, Chouaia B, Comandatore F, Crotti E, Sassera D, Lievens PM, Daffonchio D, Bandi C: Evolution of mitochondria reconstructed from the energy metabolism of living bacteria. PLoS One 9: e96566, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Degli Esposti M: Bioenergetic evolution in proteobacteria and mitochondria. Genome Biol Evol 6: 3238–3251, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Koppe L, Mafra D, Fouque D: Probiotics and chronic kidney disease. Kidney Int 88: 958–966, 2015 [DOI] [PubMed] [Google Scholar]
- 48.Rossi M, Johnson DW, Morrison M, Pascoe EM, Coombes JS, Forbes JM, Szeto CC, McWhinney BC, Ungerer JP, Campbell KL: Synbiotics easing renal failure by improving gut microbiology (SYNERGY): A randomized trial. Clin J Am Soc Nephrol 11: 223–231, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vaziri ND, Liu SM, Lau WL, Khazaeli M, Nazertehrani S, Farzaneh SH, Kieffer DA, Adams SH, Martin RJ: High amylose resistant starch diet ameliorates oxidative stress, inflammation, and progression of chronic kidney disease. PLoS One 9: e114881, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kieffer DA, Piccolo BD, Vaziri ND, Liu S, Lau WL, Khazaeli M, Nazertehrani S, Moore ME, Marco ML, Martin RJ, Adams SH: Resistant starch alters gut microbiome and metabolomic profiles concurrent with amelioration of chronic kidney disease in rats. Am J Physiol Renal Physiol 310: F857–F871, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.