Abstract
Background
Recent clinical practice guidelines have suggested conservative treatment approaches, including physical therapy, are indicated as first-line treatment for patients with low back pain (LBP); however, LBP continues to be managed with opioids, despite decreases in function, morbidity, and insignificant improvements in pain.
Objective
The primary purpose was to compare characteristics and downstream medication use between patients with LBP with prior opioid exposure vs. those who were opioid-naïve. The secondary purpose was to explore the role of prior opioid use by LBP disability.
Methods
Seven hundred and nine participants in a LBP self-management class were evaluated utilizing self-report data at baseline and longitudinal claims data from the Military Health System Data Repository. Participants were dichotomized into opioid-naïve and prior opioid use groups and then further divided into low and high disability groups based on Oswestry Disability Index (ODI) scores. Patient characteristics, comorbidities, and medication use were compared between groups.
Results
Prior opioid users had significantly higher baseline ODI and Fear Avoidance Beliefs Questionnaire physical activity subscale and work subscale scores as well as pre-index instances of mental health disorders, chronic pain, and insomnia than opioid-naïve individuals. Prior opioid users filled significantly more pain medication prescriptions in the year after the index date than did opioid-naïve individuals. Prior opioid users were significantly more likely to be taking opioids at 1 year after the index date, regardless of disability level.
Conclusion
In patients presenting with LBP, prior opioid exposure appears to be related to increased analgesic use (opioid and non-opioid) and longitudinal analgesic utilization at 1 year after the index date.
Keywords: analgesics, opioid, back pain, low back pain, opioid analgesics, opioids
INTRODUCTION
Opioid prescription rates doubled in the previous decade and sales of prescriptions nearly quadrupled from 1999 to 2014.1 This increase in opioid prescription and sales rates is matched by a concomitant upsurge in opioid-related morbidity, mortality, overdose, and substance abuse treatment admissions, with prescription drug overdose deaths in the United States having quintupled since 1999.1–3 Low back pain (LBP) is a condition that is commonly managed with opioid medication.4 For conditions such as LBP, continued opioid use has been associated with decreased function5–8 and, in some instances, death.9 Although short-term trials have shown some evidence of benefit with opioids, the studies were not designed to weigh benefits and harms and contained notable methodological flaws.10
In response to the increase in opioid prescription rates and the resulting morbidity and mortality, in 2017 the American College of Physicians released a clinical practice guideline (CPG)11 on noninvasive treatments for acute, subacute, and chronic LBP. Included in the guidelines were the utilization of nonpharmacologic treatments for LBP, such as exercise, therapeutic modalities, stress reduction, and cognitive behavioral therapy. The CPG also states that exposure to opioids should only be considered for patients who have failed the aforementioned treatments, if the benefits outweigh the risks, and after a discussion on known risks and realistic benefits occurs with the patient prior to opioid prescription.11 Similarly, in 2017 the U.S. Department of Veterans Affairs and the U.S. Department of Defense (DoD) revised the 2010 CPG for the management of opioid therapy for chronic pain. Recommendations included reducing exposure to long-term opioid therapy for chronic pain and using self-management strategies and other nonpharmacologic treatments to manage pain.2
The initiation of prescription opioid care appears to influence downstream consequences associated with continued use, morbidity, and mortality.5–9 Opioid-naïve individuals are defined as those who have not been exposed previously to opioids or who are not chronically receiving opioid analgesics on a daily basis.12 One could argue that prior exposure to opioids should increase one’s risk of downstream opioid or analgesic use, but to our knowledge this has not been investigated in patients with LBP. Further, there may be key characteristics or health differences among opioid-naïve and prior users that may partially explain prior exposure and downstream use. For this study’s primary purpose, we endeavored to compare characteristics, health comorbidities, and downstream prescription medication use among opioid-naïve and prior users. A secondary purpose was to compare downstream prescription medication use between opioid-naïve and prior users after adjusting for the role of condition severity by splitting groups into high and low LBP disability categories. We hypothesized that regardless of LBP disability level, categorization by prior use of opioids (opioid-naïve vs. prior users) would result in significant differences in use of medications.
METHODS
Reporting Guidelines
The Reporting of Studies Conducted Using Observational Routinely Collected Health Data (RECORD) initiative13 was used to guide the reporting of this study. The Institutional Review Board at Madigan Army Medical Center gave ethical approval of the study.
Study Design and Sample
The study was an observational design that included a cross-sectional assessment of self-reported measures and a 24-month assessment of healthcare utilization for 709 individuals consecutively diagnosed with LBP who were referred to a self-management for LBP class in the physical therapy clinic. All enrolled participants were included in this study. The participation date in the self-management class was the index date for this analysis. To capture all person-level health interactions, we targeted patients within the military health system. This allowed us to evaluate pre- and post-LBP diagnosis medication use, and to categorize individuals as opioid-naïve or prior opioid users. All individuals were U.S. DoD beneficiaries being seen at Madigan Army Medical Center, Tacoma, Washington, U.S.A., between March 1, 2010, and December 4, 2012. Healthcare utilization was extracted for the period of 12 months before and 12 months after the index date (Figure 1).
Figure 1.
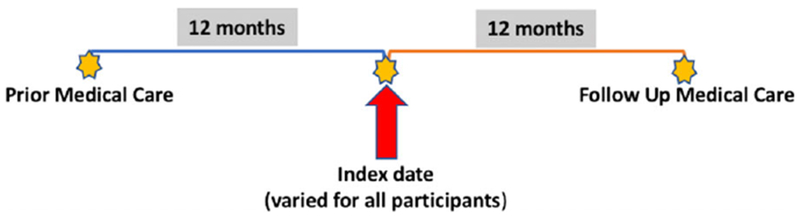
Study timeline.
Data Sourcing
Self-reported medical history and measures of pain, function, disability, and fear avoidance were captured at baseline. Healthcare utilization data were pulled from the Military Health System Data Repository (MDR). The MDR serves as the centralized data repository for all Defense Health Agency corporate healthcare data. MDR data are collected from a worldwide network of more than 260 DoD healthcare facilities and non-DoD entities. The MDR is unique as it functions as a single-payer data source and includes all person-level interactions, regardless of health-related reason. The MDR data processing is coordinated by the Defense Health Agency, updated monthly, and available to a select group of researchers with special data usage agreements.
Selection of Variables
Group Status: Opioid Use
Individuals were divided into 2 groups: opioid-naïve and prior users. This categorization was designated by examining opioid use in the 12 months prior to the index date (date of a self-management class). By definition, for opioid-naïve status we required no recorded prescription use of opioids in the 12 months prior to the index date. Conversely, individuals with an opioid prescription present prior to the self-management class were categorized as prior users. The self-management course was led by a physical therapist and was the same for everyone.
Outcome Variables
All outcome variables were captured in the 12-month period after the index date. These included total (1) opioid prescriptions, (2) nonsteroidal anti-inflammatory drug (NSAID) prescriptions, (3) muscle relaxer prescriptions, and (4) prescriptions for any other pain medications (acetaminophen and other non-represented prescription pain medications). In addition, we captured the proportion of individuals still taking opioids at 1 year after the index date.
Descriptive Variables
Patient characteristics were captured, including age, sex, and military beneficiary status. Beneficiary status was categorized as active duty service member, warrior in transition unit (medical management unit for more chronic injuries), retired service member, member of the Reserves or National Guard, and family member. Prior episodes of LBP were also captured, as were months of reported LBP before the self-management class. Disability status was captured with the Modified Oswestry Disability Index (ODI) at baseline, using a scale of 0 to 100. The modified ODI is a questionnaire divided into 10 sections assessing pain intensity, personal care, lifting, walking, sitting, standing, sleeping, social life, traveling, and the effect of LBP on employment and homemaking.14 The modified ODI has good content and construct validity and reliability for LBP.15 Fear of pain and consequent avoidance behaviors were evaluated using the Fear Avoidance Beliefs Questionnaire (FABQ) physical activity subscale and work subscale. The FABQ is a self-report measure that assesses patients’ beliefs about how work and physical activity affect LBP. The FABQ has high test-retest reproducibility and internal consistency for patients with LBP.16
Comorbidities
To better reflect the health status of the sample, we included data on several medical comorbidities within the MDR. In order to qualify as present, the patient was required to have been seen by a medical provider and diagnosed for that specific comorbidity at any time during the 12-month pre-index period. We captured proportional information on systemic arthropathy (eg, rheumatoid or psoriatic arthritis, ankylosing spondylitis), chronic pain, diabetes, traumatic brain injury, tobacco use, neoplasm, high blood pressure, obesity, substance abuse, insomnia, mental health problems, and post-traumatic stress disorder.
Missing Values
Data in the MDR are processed weekly and the processing involves encounter validation and replacement of missing values before release to researchers or policymakers. Within the dataset, 97.6% of cases had complete data and 99.8% of values were complete. Because these missing data were few and were mostly present in high-stakes outcomes, we opted not to impute data and instructed the statistical management tool to skip missing values. Because the self-reported data were captured cross-sectionally at baseline, there were no missing data for these variables.
Data Analysis
Descriptive statistics were analyzed using t-tests and chi-square analyses (Fisher’s exact test when appropriate) on SPSS version 24.0 (IBM Corp., Armonk, NY, U.S.A.). Comorbidity proportions were analyzed using a chi-square analysis. For the full sample, drug use counts were analyzed using a Poisson log-linear regression, which accounts for non-negative count variables with significant skew. A chi-square analysis was used to measure proportional use of opioids at 1 year after the index date. For continuous outcome measures, we adjusted each analysis using demographic and comorbidity variables that were significantly different between groups. We also divided the entire cohort by disability severity levels using the ODI. To divide by disability level, we split the sample by median value of the ODI, with higher ODI scores being reflective of high levels of disability and lower scores associated with lower levels of disability.14 For both datasets (ODI < 17 and ODI ≥ 17), we re-ran Poisson log-linear analyses with control variables. For all analyses, a P value of <0.05 was used to discriminate statistical significance.
RESULTS
Of the 709 individuals diagnosed with LBP and referred to a self-management class, 224 (31.6%) were considered opioid-naïve, whereas 485 (68.4%) had documented prior opioid use (Table 1). No differences were noted between the opioid-naïve and prior opioid users in terms of age, months of reported LBP before the index date, or prior episodes of LBP. The proportion of males to females was greater in the opioid-naïve group than in the prior opioid users group (P = 0.02). The 2 groups also differed in their beneficiary statuses (P < 0.01). Furthermore, prior opioid users had higher baseline ODI scores (P < 0.01) as well as higher baseline FABQ physical activity subscale and work subscale scores than did the opioid-naïve group (P < 0.01), indicating higher pre-index levels of disability and pain avoidance behaviors, respectively.
Table 1.
Baseline Patient Characteristics and Incidence of Comorbidities Prior to Index Date
| Variables [Mean (SD)/Proportions] | Opioid Naïve (n = 224) | Prior Opioid Users (n = 485) | P Value* |
|---|---|---|---|
| Age, years | 33.87 (11.52) | 35.35 (12.00) | 0.12 |
| Sex | |||
| Female | 56 | 164 | 0.02 |
| Male | 168 | 321 | |
| Months of reported LBP before index date | 26.04 (50.21) | 22.64 (46.26) | 0.39 |
| Baseline ODI score | 15.73 (9.78) | 20.03 (12.72) | < 0.01 |
| FABQ physical activity score | 14.85 (5.20) | 15.93 (5.28) | 0.01 |
| FABQ work subscale score | 16.87 (10.39) | 20.48 (11.31) | < 0.01 |
| Beneficiary status | |||
| Active duty | 151 | 305 | < 0.01 |
| WTB | 6 | 49 | |
| Retired | 19 | 36 | |
| Res-NG | 8 | 9 | |
| FM | 40 | 86 | |
| Prior episodes of LBP | |||
| Yes | 123 | 292 | 0.37 |
| No | 97 | 183 | |
| Unknown | 4 | 10 | |
| Mental health disorder | |||
| Yes | 26 | 98 | < 0.01 |
| No | 198 | 387 | |
| Diabetes | |||
| Yes | 6 | 18 | 0.48 |
| No | 218 | 467 | |
| Obesity | |||
| Yes | 6 | 19 | 0.41 |
| No | 218 | 466 | |
| High blood pressure | |||
| Yes | 19 | 49 | 0.50 |
| No | 205 | 436 | |
| Chronic pain | |||
| Yes | 2 | 42 | < 0.01 |
| No | 222 | 443 | |
| Post-traumatic stress disorder | |||
| Yes | 2 | 8 | 0.43 |
| No | 222 | 477 | |
| Systemic arthropathy | |||
| Yes | 5 | 26 | 0.06 |
| No | 219 | 459 | |
| Insomnia | |||
| Yes | 19 | 93 | < 0.01 |
| No | 201 | 391 | |
| Missing | 4 | 1 | |
| Tobacco use | |||
| Yes | 9 | 31 | 0.20 |
| No | 215 | 454 |
Descriptive statistics and comorbidity proportions were analyzed using t-tests and chi-square analyses (Fischer’s exact test when appropriate). FABQ, Fear-Avoidance Beliefs Questionnaire; FM, family member; LBP, low backpain; ODI, Oswestry Disability Index; Res-NG, member of reserves or National Guard; SD, standard deviation; WTB, warrior in transition unit.
Bolded P values reflect statistical significance < 0.05.
Table 1 also details the prevalence of comorbidities prior to the index date of LBP. There was a relatively low prevalence of diabetes, obesity, post-traumatic stress disorder, systemic arthropathy, high blood pressure, and tobacco use, with no differences (P > 0.05) in frequencies between opioid-naïve and prior opioid users. Prior opioid users had higher incidences of mental health disorders (P < 0.01), chronic pain (P < 0.01), and insomnia (P < 0.01) than did the opioid-naïve group.
Tables 2 and 3 describe the unadjusted and adjusted bivariate differences between opioid-naïve and prior opioid users. After controlling for gender, beneficiary status, pre-index chronic pain, insomnia, mental health disorders, ODI score, and FABQ physical activity subscale and work subscale scores, there were differences between the opioid-naïve and prior opioid users in terms of total opioid prescriptions (P < 0.01), total NSAID prescriptions (P < 0.01), total muscle relaxers (P < 0.01), and total prescriptions for any other pain medication (P < 0.01) after the index date, with almost 2.5 times more prescriptions being provided to prior opioid users than to opioid-naïve individuals. Furthermore, the proportion of individuals still taking opioids at 1 year after the index date was higher (P < 0.01) in prior opioid users as compared to opioid-naïve individuals.
Table 2.
Unadjusted Bivariate Differences Using Poisson Analysis Overall and by Subsets Based on Disability Scores
| Pharmacology Prescription Variables After Index Date | Opioid Naïve (mean and 95% CI/Proportions) (n = 224) | Prior Opioid Users (mean and 95% CI/Proportions) (n = 485) | P value |
|---|---|---|---|
| Total opioid prescriptions | 2.16 (1.97, 2.36) | 10.06 (9.78, 10.34) | < 0.01 |
| Total NSAID prescriptions | 4.04 (3.79, 4.31) | 6.19 (5.97, 6.42) | < 0.01 |
| Total muscle relaxer prescriptions | 1.57 (1.41, 1.74) | 3.22 (3.07, 3.39) | < 0.01 |
| Total prescriptions for any other pain medication | 33.62 (32.87, 34.39) | 72.22 (71.47, 72.98) | < 0.01 |
| Proportion still taking opioids at 1 year after index date* | |||
| Yes | 101 | 290 | < 0.01 |
| No | 123 | 195 | |
| Oswestry Score of 16 or less (n = 358) | |||
| Total opioid prescriptions | 1.78 (0.04, 3.52) | 5.43 (4.04, 6.82) | < 0.01 |
| Total NSAID prescriptions | 3.86 (3.13, 4.59) | 4.97 (4.39, 5.55) | 0.02 |
| Total muscle relaxer prescriptions | 1.50 (1.04, 1.97) | 1.91 (1.54, 2.28) | 0.18 |
| Total prescriptions for any other pain medication | 31.69 (24.17, 39.21) | 47.74 (41.75, 53.73) | < 0.01 |
| Proportion still taking opioids at 1 year after index date* | |||
| Yes | 60 | 117 | 0.06 |
| No | 79 | 102 | |
| Oswestry score of 17 or greater (n = 351) | |||
| Total opioid prescriptions | 2.76 (−1.96, 7.49) | 13.87 (11.20, 16.54) | < 0.01 |
| Total NSAID prescriptions | 4.33 (3.00, 5.66) | 7.20 (6.44, 7.95) | < 0.01 |
| Total muscle relaxer prescriptions | 1.67 (0.41, 2.93) | 4.30 (3.59, 5.02) | < 0.01 |
| Total prescriptions for any other pain medication | 36.78 (17.18, 56.37) | 92.37 (81.29, 103.44) | < 0.01 |
| Proportion still taking opioids at 1 year after index date* | |||
| Yes | 41 | 173 | < 0.01 |
| No | 44 | 93 | |
No statistical control for covariates. CI, confidence interval; NSAID, nonsteroidal anti-inflammatory drug; ODI, Oswestry Disability Index.
Of those with ODI scores of 16 or less (n = 358), 139 were opioid naïve and 219 used opioids previously. Of those with ODI scores of 17 or greater (n = 351), 85 were opioid naïve and 266 used opioids previously.
Bolded P values reflect statistical significance < 0.05.
Table 3.
Adjusted Bivariate Differences Using Poisson Analysis Overall and by Subsets Based on Disability Scores. Control Variables Include Gender, Beneficiary Status, Pre-index Chronic Pain, Insomnia, Mental Health Disorder, Oswestry Score, FABQ-PA, and FABQ-W
| Pharmacology Prescription Variables After Index Date | Opioid Naïve (Mean and 95% CI/proportions) (n = 224) | Prior Opioid Users (Mean and 95% CI/proportions) (N = 485) | P Value |
|---|---|---|---|
| Total opioid prescriptions | 2.42 (2.21, 2.64) | 7.42 (7.17, 7.68) | < 0.01 |
| Total NSAID prescriptions | 4.32 (4.05, 4.62) | 5.85 (5.63, 6.07) | < 0.01 |
| Total muscle relaxer prescriptions | 1.73 (1.56, 1.93) | 2.69 (2.54, 2.84) | < 0.01 |
| Total prescriptions for any other pain medication | 37.70 (36.85, 38.56) | 61.48 (60.76, 62.22) | < 0.01 |
| Proportion still taking opioids at 1 year after index date* | |||
| Yes | 101 | 290 | < 0.01 |
| No | 123 | 195 | |
| Oswestry score of 16 or less (n = 358) | |||
| Total opioid prescriptions | 1.66 (1.47, 1.89) | 4.29 (4.01, 4.58) | < 0.01 |
| Total NSAID prescriptions | 3.98 (3.65, 4.34) | 4.75 (4.47, 5.06) | < 0.01 |
| Total muscle relaxer prescriptions | 1.48 (1.29, 1.71) | 1.69 (1.52, 1.87) | 0.15 |
| Total prescriptions for any other pain medication | 33.26 (23.28, 34.27) | 44.29 (43.40, 45.20) | < 0.01 |
| Proportion still taking opioids at 1 year after index date* | |||
| Yes | 60 | 117 | 0.06 |
| No | 79 | 102 | |
| Oswestry score of 17 or greater (n = 351) | |||
| Total opioid prescriptions | 5.05 (0.47, 9.63) | 13.14 (10.58, 15.69) | < 0.01 |
| Total NSAID prescriptions | 4.53 (3.18, 5.87) | 7.13 (6.38, 7.88) | < 0.01 |
| Total muscle relaxer prescriptions | 2.08 (0.81, 3.35) | 4.17 (3.47, 4.88) | < 0.01 |
| Total prescriptions for any other pain medication | 48.02 (29.05, 66.98) | 88.78 (78.21, 99.35) | < 0.01 |
| Proportion still taking opioids at 1 year after index date* | |||
| Yes | 41 | 173 | < 0.01 |
| No | 44 | 93 | |
No statistical control for covariates. CI, confidence interval; FABQ, Fear-Avoidance Beliefs Questionnaire; NSAID, nonsteroidal anti-inflammatory drug; ODI, Oswestry Disability Index.
Of those with ODI scores of 16 or less (n = 358), 139 are opioid naïve and 219 used opioids previously. Of those with ODI scores of 17 or greater (n = 351), 85 are opioid naïve and 266 used opioids previously.
Bolded P values reflect statistical significance < 0.05.
Table 3 also details the adjusted bivariate differences by subsets based on disability scores and indicates that even when classified by level of disability, prior use of opioids leads to higher rates of overall pain medication usage. Among individuals with an ODI score of <17, after controlling for gender, beneficiary status, pre-index chronic pain, insomnia, mental health disorder, and FABQ physical activity subscale and work subscale scores, prior opioid users had higher rates of pain medication use after the index date, including total opioid prescriptions (P < 0.01), total NSAID prescriptions (P < 0.01), and total prescriptions for any other pain medication (P < 0.01). Among individuals with an ODI score of ≥17, after controlling for the same covariates, prior opioid users had greater rates of analgesic use, including total opioid prescriptions (P < 0.01), total NSAID prescriptions (P < 0.01), total muscle relaxer prescriptions (P < 0.01), and total prescriptions for any other pain medication (P < 0.01). A higher proportion of prior opioid users were still taking opioids at 1 year after the index date than were opioid-naïve individuals (P < 0.01).
DISCUSSION
Of the 709 individuals diagnosed with LBP included in this analysis, 485 were prior opioid users (68.4%). This finding is slightly higher than most recorded prescribing patterns, which show that 1 out of every 5 patients with pain-related diagnoses receives an opioid prescription.17 What we feel is an important finding is that continued opioid use at 1 year after the index date is associated with prior opioid use. This finding is consistent with those of others18 who have used a single-payment format (workers’ compensation claimants) with a cohort of patients who had acute disabling LBP. Early prescription of opioids (within 15 days of the claim) and the amount of opioids prescribed were positively associated with late opioid use.18 Additional studies have demonstrated similar results of prior opioid use leading to long-term use,19,20 and, worth noting, all have shown little to no positive effects in increasing function or decreasing pain levels long-term.19,20
Prior opioid users were significantly more likely to have previous incidences of mental health disorders, chronic pain, and insomnia. This finding is consistent with others who have found that mental health disorders, including anxiety and major depression, are very common among persons with chronic pain,21,22 opioid dependency,23–25 and long-term opioid use.26–28 Furthermore, individuals with increased levels of depression are at an increased risk for being prescribed and taking higher doses of opioids,29 and for receiving stronger classes of opioids for longer periods of time.28 Similarly, patients with chronic pain diagnoses receive higher doses of long-acting opioids on a long-term basis than those without chronic pain,30 and rates of opioid dependence have been reported as higher in chronic pain patients as compared to the general population,31 despite limited efficacy for chronic pain management.32 Additionally, in a cross-sectional study of over 8,000 community members, insomnia was 42% more likely among those who reported using prescription opioids compared to those who did not.33 Sleep quality has also been found to be poorer among opioid-dependent individuals on methadone maintenance therapy as compared to opioid-naïve individuals.34 Interestingly, insomnia and short sleep duration have also been found to be significant risk factors for onset of chronic pain,35,36with poor sleep increasing anxiety and hyperalgesia to heat, blunt pressure, cold, and pinprick stimuli.37,38 These findings indicate that there may be a bidirectional relationship between sleep and pain, with those who have trouble sleeping being more likely to be in pain and those who are in pain being less able to sleep.
One of our key findings was that compared to opioid-naïve individuals, prior opioid users utilized both higher levels of opioids and other pain medications. This finding is consistent with others who have found that opioid users with recurrent back pain were more likely to increase medication use on days of higher pain than were non-opioid users with back pain.39 Similarly, a study of long-term opioid use in long-stay nursing home residents found that opioid users were more commonly prescribed pain adjuvants and other pain medications than were nonusers.40 Investigators of opioid use before and after total knee arthroplasty41 and upper extremity surgical procedures42 have found that patients taking opioids preoperatively were more likely to continue to use opioids postoperatively and potentially become chronic users than were opioid-naïve individuals,41,42 further supporting our finding that prior opioid exposure increases opioid use after the index date.
Categorization of prior opioid use was found to influence downstream use of opioids, with a significantly higher proportion of prior opioid users still taking opioids at 1 year after the index date than opioid-naïve individuals. Others have found that individuals who previously used/abused opioids had a nearly 10-fold increase in risk for long-term opioid prescription receipt (hazard ratio = 9.70, 95% confidence interval 8.20 to 9.24) compared to those who were opioid-naïve.43 Further, the amount (quantity of prescriptions) of prior use might be a contributing factor to increased use after the index date. For example, among chronic opioid users undergoing total knee arthroplasty, an opioid dose of ≥12 mg/d over the 3 months leading up to surgery had an increased risk for persistent chronic opioid use by a factor of 6.44 Unfortunately, our dataset does not provide data on daily dosage, so we cannot comment on these findings as they relate to our sample.
Interestingly, when we classified by disability level (≥17 on the ODI), a significantly higher proportion of prior opioid users took opioids at 1 year. Others have reported that baseline severity of disability is significantly related to and predictive of long-term opioid use. Franklin et al.19 demonstrated that severe perceived disability on the Roland-Morris Disability Questionnaire at baseline was significantly associated with and predictive of long-term opioid use in a cohort of workers with LBP.45 However, it should be noted that the researchers did not consider prior opioid use as a confounder in the relationship between disability and long-term opioid use.19 To our knowledge, our study is the first that demonstrates the potential confounding impact of a prior history of opioid exposure in the relationship between disability severity and long-term opioid use.
Limitations
There are several limitations to this study. First, despite our ability to capture all person-level health interactions over a 24-month period, the cross-sectional study design did not permit causal associations to be made about the identified subgroups. Similarly, our self-reported outcome measures were captured cross-sectionally and we do not know whether they changed over time. Furthermore, this study includes patients within a military health system with LBP, and we cannot speak to the generalizability to other conditions, nonmilitary settings, or other clinical settings such as primary care. Lastly, the nature of the database is such that we could not determine why participants received opioids, only that they received them prior to or after the index date. Therefore, we do not know whether the opioid prescriptions are related to LBP or a different surgical procedure or injury. Additionally, we do not know if the participants actually used the opioids they received.
CONCLUSION
Clinicians treating LBP should be aware of the apparent associations between mental health disorders, insomnia, chronic pain, and opioid use, as these patients may be at increased risk for using and potentially abusing these medications. Similarly, clinicians should recognize the relationship between prior opioid exposure and increased opioid and non-opioid use in this population, as it underscores the importance of nonpharmacologic first-line treatment for the management of LBP. The results of this study emphasize the importance of the provision of specific, tailored pain management education to prior opioid users with LBP as these individuals may be more likely to utilize analgesics long-term, regardless of LBP disability severity level and despite a lack of medication efficacy. Future research is needed to confirm the relationship between prior opioid use, disability severity, and longitudinal opioid use in patients with LBP, and studies are needed to validate these relationships in patients presenting with other pain diagnoses to see if these relationships persist outside of patients with LBP.
Acknowledgments
FUNDING
Dr. Chad Cook acknowledges funding from the National Center for Complementary and Integrative Health (UG3AT009790).
Footnotes
Publisher's Disclaimer: Disclaimer: The view(s) expressed herein are those of the author(s) and do not reflect the official policy or position of Madigan Army Medical Center, the U.S. Army Medical Department, the U.S. Army Office of the Surgeon General, the Department of the Army, Department of Defense, Defense Health Agency, or the U.S. Government.
INSTITUTIONAL REVIEW BOARD
The Institutional Review Board at Madigan Army Medical Center gave ethical approval of the study.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Centers for Disease Control and Prevention. Vital signs: overdoses of prescription opioid pain relievers—United States, 1999–2008. MMWR. 2011;60:1487–1492. [PubMed] [Google Scholar]
- 2.Rosenberg JM, Bilka BM, Wilson SM, Spevak C. Opioid therapy for chronic pain: overview of the 2017 US Department of Veterans Affairs and US Department of Defense clinical practice guideline. Pain Med. 2017;1–14. [DOI] [PubMed] [Google Scholar]
- 3.Seth P, Rudd RA, Noonan RK, Haegerich TM. Quantifying the epidemic of prescription opioid overdose deaths. Am J Public Health. 2018;108:500–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jeffery MM, Hooten WM, Hess EP, et al. Opioid prescribing for opioid-naïve patients in emergency departments and other settings: characteristics of prescriptions and association with long-term use. Ann Emerg Med. 2017;166:514–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashworth J, Green DJ, Dunn KM, Jordan KP. Opioid use among low back pain patients in primary care: is opioid prescription associated with disability at 6-month follow-up? Pain. 2013;154:1038–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Deyo RA, Smith DH, Johnson ES, et al. Opioids for back pain patients: primary care prescribing patterns and use of services. J Am Board Fam Med. 2011;24:717–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ. 2015. January;350:g6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah A, Hayes CJ, Martin BC. Characteristics of initial prescription episodes and likelihood of long term opioid use—United States, 2006–2015. MMWR. 2017;66:265–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ray WA, Chung CP, Murray KT, Cooper WO, Hall K, Stein CM. Out-of-hospital mortality among patients receiving methadone for noncancer pain. JAMA Intern Med. 2015;175:420–427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chou R, Deyo R, Friedly J, et al. Systemic pharmacologic therapies for low back pain: a systematic review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med. 2017;166:480–492. [DOI] [PubMed] [Google Scholar]
- 11.Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166:514–530. [DOI] [PubMed] [Google Scholar]
- 12.Jeffery MM, Hooten WM, Hess EP, et al. Opioid prescribing for opioid-naïve patients in emergency departments and other settings: characteristics of prescriptions and association with long-term use. Ann Emerg Med. 2017;71:326.e19–336.e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Langan SM, Cook C, Benchimol EI. Improving the reporting of studies using routinely collected health data in physical therapy. J Orthop Sports Phys Ther. 2016;46:126–127. [DOI] [PubMed] [Google Scholar]
- 14.Fairbank J, Pynsent PB. The Oswestry disability index. Spine (Phila Pa 1976). 2000;25:2940–2953. [DOI] [PubMed] [Google Scholar]
- 15.Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther. 2002;82:8–24. [DOI] [PubMed] [Google Scholar]
- 16.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. [DOI] [PubMed] [Google Scholar]
- 17.Daubresse M, Chang H, Yu Y, et al. Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010. Med Care. 2013;51:870–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Webster BS, Verma SK, Gatchel RJ. Relationship between early opioid prescribing for acute occupational low back pain and disability duration, medical costs, subsequent surgery, and late opioid use. Spine (Phila Pa 1976). 2007;32:2127–2132. [DOI] [PubMed] [Google Scholar]
- 19.Franklin GM, Rahman EA, Turner JA, Daniel WE, Fulton-Kehoe D. Opioid use for chronic low back pain: a prospective, population-based study among injured workers in Washington state, 2002–2005. Clin J Pain. 2009;25:743–751. [DOI] [PubMed] [Google Scholar]
- 20.Martell BA, O’Connor PG, Kerns RD, et al. Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–127. [DOI] [PubMed] [Google Scholar]
- 21.Olfson M, Wall M, Wang S, Crystal S, Blanco C. Service use preceding opioid-related fatality. Am J Psychiatry. 2018;175:538–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manchikanti L, Giodano J, Boswell MV, Fellows B, Manchukonda R, Pampati V. Psychological factors as predictors of opioid abuse and illicit drug use in chronic pain patients. J Opioid Manag. 2007;3:89–100. [DOI] [PubMed] [Google Scholar]
- 23.Boscarino JA, Rukstalis M, Hoffman SN, et al. Risk factors for drug dependence among out-patients on opioid therapy in a large US health-care system. Addiction. 2010;105:1776–1782. [DOI] [PubMed] [Google Scholar]
- 24.Back SE, Payne RL, Simpson AN, Brady KT. Gender and prescription opioids: findings from the National Survey on Drug Use and Health. Addict Behav. 2010;35:1001–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Becker WC, Sullivan LE, Tetrault JM, Desai RA, Fiellin DA. Non-medical use, abuse and dependence on prescription opioids among U.S. adults: psychiatric, medical, and substance use correlates. Drug Alcohol Depend. 2008;94:38–47. [DOI] [PubMed] [Google Scholar]
- 26.Hoffman EM, Watson JC, St Sauver J, Staff NP, Klein CJ. Association of long-term opioid therapy with functional status, adverse outocmes, and mortality among patients with polyneuropathy. JAMA Neurol. 2017;74:773–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thielke SM, Simoni-Wastila L, Edlund MJ, et al. Age and sex trends in long-term opioid use in two large American health systems between 2000 and 2005. Pain Med. 2010;11:248–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braden JB, Sullivan MD, Ray GT, et al. Trends in long-term opioid therapy for noncancer pain among persons with a history of depression. Gen Hosp Psychiatry. 2009;31:564–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grattan A, Sullivan MD, Saunders KW, Campbell CI, Von Korff MR. Depression and prescription opioid misuse among chronic opioid therapy recipients with no history of substance abuse. Ann Fam Med. 2012;10:304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sehgal N, Colson J, Smith HS. Chronic pain treatment with opioid analgesics: benefits versus harms of long-term therapy. Exert Rev Neurother. 2013;13:1201–1220. [DOI] [PubMed] [Google Scholar]
- 31.Turk DC, Swanson KS, Gatchel RJ. Predicting opioid misuse by chronic pain patients: a systematic review and literature synthesis. Clin J Pain. 2008;24:497–508. [DOI] [PubMed] [Google Scholar]
- 32.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—2016. JAMA. 2016;315:1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serdarevic M, Osborne V, Striley CW, Cottler LB. The association between insomnia and prescription opioid use: results from a community sample in Northeast Florida. Sleep Health. 2017;3:368–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zahari Z, Inrahim MA, Tan SC, Mohamad N, Ismail R. Sleep quality in opioid-naïve and opioid-dependent patients on methadone maintenance therapy in Malaysia. Turk J Med Sci. 2016;46:1743–1748. [DOI] [PubMed] [Google Scholar]
- 35.Generaal E, Vogelzangs N, Penninx BW, Dekker J. Insomnia, sleep duration, depressive symptoms, and the onset of chronic multisite musculoskeletal pain. Sleep. 2017;40:1–10. [DOI] [PubMed] [Google Scholar]
- 36.Vanini G Sleep deprivation and recovery sleep prior to a noxious inflammatory insult influence characteristics and duration of pain. Sleep. 2016;39:133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schuh-Hofer S, Wodarski R, Pfau DB, et al. One night of total sleep deprivation promotes a state of hyperalgesia: a surrogate pain model to study the relationship of insomnia and pain. Tain. 2013;154:1613–1621. [DOI] [PubMed] [Google Scholar]
- 38.Zahari Z, Lee CS, Tan SC, Mohamad N, Lee YY, Ismail R. Relationship between cold pressor pain-sensitivity and sleep quality in opioid-dependent males on methadone treatment. PeerJ. 2015;3:e839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sturgeon JA, Hah JM, Sharifzadeh Y, et al. Predictors of daily pain medication use in individuals with recurrent back pain. Int J Behav Med. 2018;25:252–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hunnicutt JN, Chrysanthopoulou SA, Ulbricht CM, Hume AL, Lapane KL. Prevalence of long-term opioid use in long-stay nursing home residents. J Am Geriatr Soc. 2018;66:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Politzer CS, Kildow BJ, Goltz DE, Green CL, Bolognesi MP, Seyler TM. Trends in opioid utilization before and after total knee arthroplasty. J Arthroplasty. 2018;3:S147.e1–S153.e1. [DOI] [PubMed] [Google Scholar]
- 42.Waljee JF, Zhong L, Hou H, Sears E, Brummett C, Chung KC. The use of opioid analgesics following common upper extremity surgical procedures: a national, population-based study. Plast Reconstr Surg. 2016;137: 355e–364e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quinn PD, Hur K, Chang Z, et al. Incident and long-term opioid therapy among patients with psychiatric conditions and medications: a national study of commercial health care claims. Pain. 2017;158:140–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim KY, Anoushiravani AA, Chen KK, Roof M, Long WJ, Schwarzkopf R. Preoperative chronic opioid users in total knee arthroplasty—which patients persistently abuse opiates following surgery? J Arthroplasty. 2018;33:107–112. [DOI] [PubMed] [Google Scholar]
- 45.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976). 1983;8:141–144. [DOI] [PubMed] [Google Scholar]


