Abstract
Background:
Hip fractures in older adults often result from a fall in the lateral direction. While younger adults tend to recover balance from a lateral perturbation with a single lateral sidestep, older adults are prone to multistep responses which are associated with an increased fall risk. This study compared the stepping characteristics and stability of single and multistep responses to lateral perturbation in healthy older adults.
Methods:
Eighty-four older adults received lateral waist-pull perturbations to either side. Spatio-temporal stepping characteristics and balance stability were quantified.
Findings:
Fewer steps were taken to recover balance when the first step was a lateral sidestep. The stability margin of single lateral sidesteps was greater than medial sidesteps and cross-over steps to the back but not significantly different from single cross-over steps to the front at step termination. Single step responses were more stable than multistep responses at step termination and at step initiation for lateral sidesteps and cross-over steps to the front. The decreased stability of multistep responses was attributed to an increased center of mass velocity and a smaller distance between the center of mass and base-of-support at step termination.
Interpretation:
Although lateral sidesteps result in fewer steps than cross-over steps to the front, the stability margin was not significantly different at step termination. These results suggest difficulty terminating center of mass motion and/or inefficient center of mass control differentiates single and multistep responses. Future studies should investigate perturbation training and/or hip abductor muscle conditioning as a means of improving compensatory stepping reactions.
Keywords: Aging, Falls, Balance, Stepping, Rehabilitation, Perturbation
1. Introduction
Falls and their resulting injuries are among the major health problems among older adults where risk for hip fracture is six times greater during sideways falls than forward or backward falls (Nevitt and Cummings, 1993). Unsurprisingly, many older adults have difficulties stepping sideways as a protective response to a lateral loss of balance (Mille et al., 2005; Rogers and Mille, 2003). Older adults tend to recover balance with multiple steps where younger adults typically require only a single step (Mille et al., 2005). The multistep reactions of older adults are associated with an increased fall risk (Johnson Hilliard et al., 2008) and may be attributed to problems in the initial stepping strategy. However, the specific reasons for these differences in stepping performance are incompletely understood.
Following a lateral perturbation, the center of mass (CoM) is moved passively, relative to the base of support (BoS), such that the leg contralateral to the direction of the imposed CoM movement is passively unloaded (Maki et al., 1996; Mille et al., 2005; Yungher et al., 2012) while the ipsilateral leg is passively loaded. A step initiated with the passively loaded limb is called a lateral sidestep (LSS, Fig. 1A). A LSS requires the passively loaded limb to be actively and rapidly unloaded prior to step initiation. In contrast, stepping with the passively unloaded leg likely requires less effort to transfer weight before step initiation. When stepping with the unloaded leg, three different initial stepping strategies have been identified: a cross-over step to the front (CSF), a cross-over step to the back (CSB), or a medial sidestep (MSS, Fig. 1).
Fig. 1.
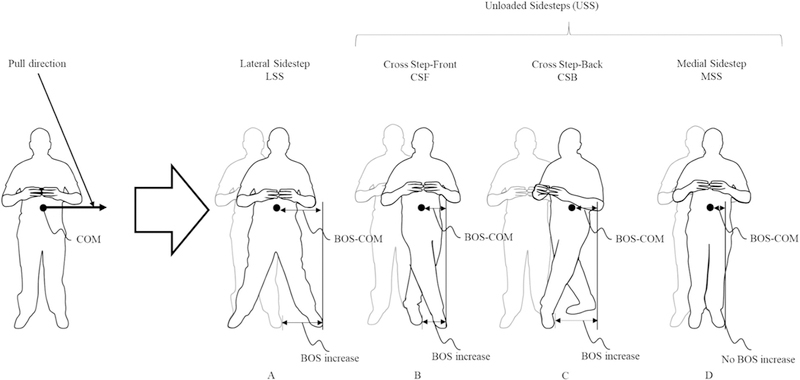
Illustration of loaded (A) and unloaded sidestep strategies (B, C, and D). Pull direction is indicated by the arrow at waist-level. The increase in base of support (BoS) boundary is shown for each step type. Note that in CSF and CSB, the swing foot must step beyond the stance foot to increase the BoS boundary. The distance between the CoM and BoS (BoS-CoM) is also shown.
Younger adults often respond with a single LSS, while older adults more often take multiple steps that are initiated with the unloaded limb when responding to lateral perturbations (Mille et al., 2005). In addition to being associated with multistep responses, stepping with the unloaded limb involves an increased risk of inter-limb collisions and more complex step trajectories (Maki et al., 2000). Stepping with the unloaded limb may be easier to execute due to passive unloading that facilitates a more rapid swing-foot lift off (Maki et al., 1996) and may allow more opportunities to make corrective adjustments during a series of preplanned steps (Luchies et al., 1994). However, responding to a lateral perturbation with multiple steps, as opposed to a single step, is associated with an increased risk of falls (Johnson Hilliard et al., 2008). Additionally, unloaded sidesteps (USS), which result in multistep reaction more frequently than LSS, are thought to be less stable (Maki et al., 1996; Patton et al., 2006). Therefore, identifying factors associated with multistep recovery strategies, e.g. diminished stability, may lead to insights in developing targeted interventions to enhance balance stability and prevent falls.
Reduced stability has been a consistent finding that differentiates single step versus multiple step reactions (Barrett et al., 2012; Carty et al., 2011; Carty et al., 2012). The CNS appears to alter the response in real time (Fujimoto et al., 2017) based on the evolving balance state, i.e. the central nervous system (CNS) monitors the current and future states of the CoM relative to the BoS (Maki and McIlroy, 1999; Rogers and Mille, 2016). Reduced dynamic stability at first step foot contact, and as early as first step lift off, has been linked with additional steps following lateral perturbations (Fujimoto et al., 2017), although only cross-over step types were analyzed. Reduced dynamic stability at first step foot contact following an anterior-posterior perturbation (Carty et al., 2011) has also been linked with additional steps.
To further address these issues, the purposes of this study were to characterize: 1) the balance stability of the different evoked first step reactions; and 2) the stability of single and multistep strategies of older adults to lateral waist-pull perturbations. We hypothesized that a single LSS is more stable than a single USS which leads to additional compensatory steps. Furthermore, we hypothesized that the first step of a single step response is more stable than the first step of a multistep strategy.
2. Methods
2.1. Participants
Eighty-four community dwelling older adults (46 females and 38 males; 72.7 (5.6) years old; 166.0 (8.3) cm; 76.7 (15.9) kg) were recruited from the greater Baltimore area, and from the Geriatric Research, Education and Clinical Center of the Baltimore Veterans Affairs Medical Center. Exclusion criteria were: 1) Mini Mental State Examination ≤ 24 (Folstein et al., 1975); 2) centers for Epidemiological Studies Depression Survey ≥ 16 (Radloff, 1977); 3) sedative use; 4) any clinically significant functional impairment related to musculoskeletal, neurological, cardio-pulmonary, metabolic, or other general medical problems that limit functional activities; 5) non-ambulatory or use of walking device at home; 6) participating in vigorous exercises or muscle strengthening exercises; 7) advised not to exercise by primary care physician; and 8) received surgery in the past year. All participants provided written informed consent prior to participation and the study was approved by the Institutional Review Board at the University of Maryland School of Medicine and the Baltimore Veterans Affairs Medical Center.
The Berg Balance Scale short form (7 item) (Berg et al., 1989; Berg et al., 1992), timed up and go (Podsiadlo and Richardson, 1991), Physical Activity Scale for the Elderly (Washburn and Montoye, 1986), Falls Efficacy Scale (Tinetti et al., 1990), Activities-Specific Balance Confidence Scale (Powell and Myers, 1995), 4-item dynamic gait index (Marchetti and Whitney, 2006), and the four square step test (Dite and Temple, 2002) were taken prior to study participation as participant descriptors. The short-form Berg Balance Scale is a measure of balance for elderly individuals that yields scores between 0 and 28. Individuals scoring below 23 are considered at risk for falling (Chou et al., 2006) assuming a linear transformation of the original Berg Balance Scale (Chou et al., 2006). The timed up and go test measures the amount of time required for an individual to rise from a seated position, walk 3 m, turn around, walk back 3 m and sit down again (Podsiadlo and Richardson, 1991). Individuals requiring > 14 s are considered to be at risk for falls (Shumway-Cook et al., 2000). The Physical Activity Scale for the Elderly is a question-based assessment of fall risk yielding scores between 0 and 793 that are indicative of physical activity level (Washburn and Montoye, 1986). Correlational data suggests a minimum Physical Activity Scale for the Elderly Score of 140 and 120, for males and females respectively, predicted a favorable waist circumference (Logan et al., 2013). The Falls Efficacy Scale is a self-administered questionnaire to assess fear of falling (Tinetti et al., 1990). Respondents rate their fear of falling between 1 and 10 for 10 questions concerned with various activities of daily living. Total scores range between 10 and 100 with higher scores indicating a greater fear of falling. The Activities-Specific Balance Confidence Scale is a self-administered questionnaire to asses confidence in performing various ambulatory activities (Powell and Myers, 1995). Respondents rate their balance confidence on a scale from 0 to 100 for 16 items and the score is averaged. Scores below 50, between 50 and 80, and above 80 indicate low, moderate and highly functioning older adults (Myers et al., 1998). The dynamic gait index-4 item was developed to assess the likelihood of falling in older adults (Marchetti and Whitney, 2006). The dynamic gait index scores range from 0 to 12 with individual scoring <10 considered at risk for falls (Marchetti and Whitney, 2006). The four-square step test times individuals while stepping once in each of four squares arranged in a grid and then back (Dite and Temple, 2002). Individuals that take longer than 15 s are considered to be at risk for falls (Dite and Temple, 2002).
2.2. Testing protocol
Participants received 36 randomly applied, motor-driven lateral waist-pull perturbations (the system has been described in detail previously (Pidcoe and Rogers, 1998)). Trials were conducted at six, constant velocity, pull intensities (total displacement: 5, 8.6, 12.1, 15.7, 19.3, 22.8 cm; velocity: 9, 18, 27, 36, 45, 54 cm/s, and maximum acceleration: 180, 360, 540, 720, 900, 900 cm/s2). The mean rise time for the velocity is about 60 ms (Pidcoe and Rogers, 1998). Three trials at each intensity were performed in the left and right directions. Trials were presented in a random order to prevent anticipation and learning effects. Participants wore a safety harness to prevent contact with the ground. Participants stood in a self-selected, comfortable standing position and held a light cylindrical baton (to avoid arm contact with the pull mechanism) with both hands in front of the body. Prior to testing, foot position was traced on contact paper to ensure consistent foot placement. Participants were instructed to “relax and react naturally to prevent themselves from falling.”
2.3. Data collection
Analysis focused on the minimum pull intensity where multiple steps (mean number of steps > 1) were evoked. The minimum pull intensity where multiple steps occurred was defined as the balance tolerance limit (BTL) (Yungher et al., 2012). The BTL is a way of making the postural challenge consistent across participants by effectively normalizing perturbation magnitudes according to where participants transitioned to multiple stepping behavior (Yungher et al., 2012). Three-dimensional motion-capture (Vicon, Oxford, UK) was used to collect kinematic data (sampling rate = 120 Hz, low-pass filtered at 6 Hz using a dual-pass fourth-order digital filter).
2.4. Data analysis
Analysis focused on the markers placed on the bilateral posterior iliac spine, medial malleoli, 5th metatarsophalangeal joints, the 1st metatarsal head, and heel. The CoM was approximated as the midpoint of the posterior iliac spine markers (Yang and Pai, 2014). Stability was quantified using the margin of stability (MoS) defined by Hof (Hof et al., 2005),
where BoS is the base of support and XCoM is the extrapolated center of mass. The XCoM is defined as,
where g is gravitational acceleration, L is the average CoM height prior to perturbation, and x and x˙ are the CoM displacement and CoM velocity respectively. Positive MoS values indicate a stable state while negative values imply instability. The BoS was determined using markers on the feet (1st metatarsal head, lateral malleolus, 5th metatarsophalangeal joint, and heel marker). The BoS boundary was assumed to exist at the most lateral aspect of the foot in the direction of the perturbation (depending on the orientation of the foot).
The MoS was calculated at step initiation and step termination. Step initiation was defined as the time that the lateral ankle marker vertical velocity exceeded 0.01 m/s and was verified by visual inspection. Step termination was defined as the time that the lateral ankle marker velocity was < 0.01 m/s in the downward direction. Step length, swing time, first step BoS increase (explained further below), distance between the CoM and BoS boundary (BoS-CoM), and CoM velocity were also calculated to assess first step characteristics.
Step length was defined, in the frontal plane, as the distance between the lateral malleolus at step initiation and step termination of the stepping leg. Swing time was defined as the time between step initiation and step termination. While step length defines the increase in BoS boundary for LSS (Fig. 1), the same is not true for CSF, CSB, and MSS. In MSS, the swing leg does not increase the BoS boundary and in CSF and CSB, the swing leg does not increase the BoS boundary until the swing leg moves laterally past the stance leg. Therefore, BoS boundary increase was included in the analysis to directly quantify the effect of step type on stability. Trials with obstructed markers between step initiation and step termination were excluded from analysis.
2.5. Statistical analyses
A linear mixed effects model with participants as a random factor, test number as a repeated within-participant factor, and step type as a fixed effect were used to compare step count between LSS with CSF, CSB, and MSS. Separate linear mixed effects models were used to compare dependent variables with participant as a random factor, test number as a repeated within-participant factor, and step type and step count (single or multistep) as fixed effects (including an interaction term). Estimated mean and standard error are reported from the fitted model. When step type was a significant main effect, post-hoc comparisons between single LSS and single CSF, single LSS and single CSB, and single LSS and single MSS were evaluated using Fisher’s least significant differences. When significant interaction effects were found post-hoc comparisons were performed between single and multistep responses within each step type using Fisher’s least significant differences. Statistical analysis was performed using SPSS v22 (IBM Corp, Armonk, NY).
3. Results
Participant demographics and clinical measures are shown in Table 1. Spatio-temporal stepping parameters were affected by step type and mostly unrelated to step count (single versus multistep). Table 2 shows the total number of steps taken, step initiation onset timing, and step length. Post-hoc analyses, performed following a significant main effect of step type (p < 0.001), showed that when a LSS was evoked as the first step it resulted in fewer recovery steps than when a CSF (p = 0.004), a CSB (p = 0.005), or a MSS (p < 0.001) was evoked. First step initiation was significantly affected by step type (p < 0.001) and the interaction of step type and step count (p = 0.002). LSS were initiated later than CSF (p < 0.001) and CSB (p < 0.001). Multi-step MSS were initiated earlier than single MSS (p 0.001) with CSF (p < 0.001) and CSB (p < 0.001) exhibiting longer swing times than LSS. Step length was significantly affected by step type (p < 0.001) with CSF (p < 0.001) and CSB (p < 0.001) having longer step lengths compared to LSS while MSS (p < 0.001) had shorter step lengths (Table 2).
Table 1.
Participant demographics.
| n | 84 |
| Females | 46 |
| Age | 72.7 (5.6) years |
| Height | 166.0 (8.3) cm |
| Weight | 76.7 (15.9) kg |
| Short-form berg balance scale-7 | 26.6 (2.0) |
| Timed up and go | 10.7 (2.0) s |
| Physical activity scale for the elderly | 118.2 (48.6) |
| Falls efficacy scale | 11.1 (2.0) |
| Activities-specific balance confidence scale y | 93.3 (6.5) |
| 4-item dynamic gait index | 10.9 (1.7) |
| Four square step test | 9.6 (2.5) s |
Table 2.
Estimated mean, standard error, and number of trials for each step based on first evoked step type.
| Step count (#) |
n | Step initiation (ms) |
Swing time (ms) |
Step length (% height) |
||
|---|---|---|---|---|---|---|
| LSS | 1.36 | Single | 66 | 408 (12)†,‡ | 471 (22)†,‡ | 23.7 (1.0)†,‡,§ |
| (0.07)†,‡,§ | Multi | 30 | 375 (17) | 470 (31) | 21.4 (1.3) | |
| CSF | 1.73 (0.11)† | Single | 16 | 290 (24)† | 834 (39)† | 32.6 (2.0)† |
| Multi | 24 | 326 (20) | 792 (35) | 30.0 (1.5) | ||
| CSB | 1.64 (0.07)‡ | Single | 46 | 340 (15)‡ | 825 (28)‡ | 30.9 (1.2)‡ |
| Multi | 57 | 372 (14) | 780 (28) | 28.7 (1.0) | ||
| MSS | 1.96 (0.06)§ | Single | 16 | 402 (23)* | 491 (39) | 7.2 (1.7)§ |
| Multi | 111 | 336 (10)* | 483 (21) | 8.4 (0.9) | ||
Significant post-hoc difference between LSS and CSF.
Significant post-hoc difference between LSS and CSB.
Significant post-hoc difference between LSS and MSS.
Significant post-hoc differences between single and multistep responses within step type.
3.1. Margin of stability
Although spatio-temporal stepping parameters were largely unrelated to step count, MoS at step initiation and step termination were significantly related to step type (p-values < 0.001), step count (p-values < 0.002), and the interaction of step type and step count (p-values < 0.037). Fig. 2A shows the MoS at first step initiation. The MoS of single CSF (8.3 (0.9) % height) was larger than single LSS (4.6 (0.5) % height). The MoS was significantly smaller for multistep versus single step LSS (single: 4.6 (0.5) % height; multistep: 2.3 (0.6) % height) and CSF (single: 8.3 (0.9) % height; multistep: 5.9 (0.7) % height).
Fig. 2.
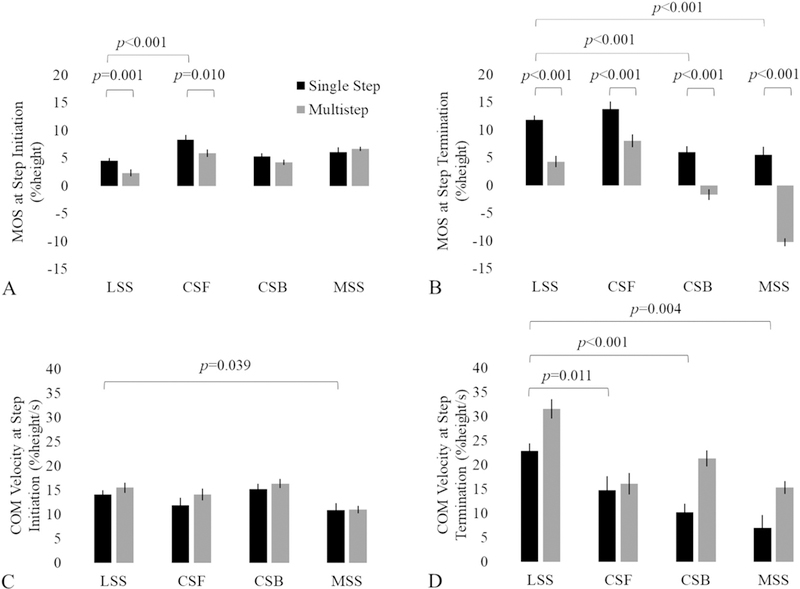
Estimated mean and standard error of the margin of stability of a lateral sidestep (LSS), cross-over step to the front (CSF), cross-over step to the back (CSB), and medial sidestep (MSS) at first step initiation (A) and step termination (B). Center of mass (CoM) velocity at step initiation (C) and step termination are also shown (D). Statistically significant differences are shown with brackets. A statistically significant step count main effect for CoM velocity at step termination is not shown in D (p < 0.001).
Fig. 2B shows the MoS at step termination. The MoS of single LSS (11.8 (0.8) % height) was significantly larger than single CSB (6.0 (1.0) % height) and single MSS (5.5 (1.4) % height) at step termination. The MoS was smaller for multistep responses compared to single step responses for LSS (single: 11.8 (0.8) % height; multistep: 4.3 (1.0) % height), CSF (single: 13.7 (1.4) % height; multistep: 8.0 (1.2) % height), CSB (single: 6.0 (1.0) % height; multistep: –1.7 (0.9) % height), and MSS (single: 5.5 (1.4) % height; multistep: –10.3 (0.8) % height).
3.2. Center of mass velocity
Fig. 2C and D show the CoM velocity at step initiation and step termination respectively. CoM velocity at step initiation was significantly affected by step type (p < 0.001, Fig. 2C). Post-hoc comparisons revealed single LSS CoM velocity (14.1 (0.8) % height/s) was larger than single MSS CoM velocity (10.9 (1.5) % height/s) at step initiation. CoM velocity at step termination was significantly affected by step type (p < 0.001) and step count (p < 0.001, Fig. 2D). At step termination single LSS CoM velocity (22.9 (1.6) % height/s) was larger than single CSF (14.7 (3.0) % height/s), single CSB (10.2 (1.9) % height/s), and single MSS (7.0 (2.7) % height/s). Across step types, CoM velocity at first step termination was lower for single step responses (13.7 (1.4) % height/s) compared to multistep responses (21.1 (1.2) % height/s).
3.3. BoS-CoM
Similar to MoS, the BoS-CoM at step initiation and step termination was significantly affected by step type (p-values < 0.001), step count (p-values < 0.001), and the interaction of step type and step count (p values < 0.024). Fig. 3A shows the BoS-CoM at step initiation. Post-hoc comparisons revealed that the CoM position was closer to the BoS boundary in single LSS (8.8 (0.3) % height) compared to single CSF (11.9 (0.7) % height) and single CSB (10.0 (0.4) % height) at step initiation. The CoM position was further from the BoS boundary in single step compared to multistep responses for LSS (single: 8.8 (0.3); multi: 7.0 (0.5) % height) and CSF (single: 11.9 (0.7); multi: 10.1 (0.5) % height) at step initiation.
Fig. 3.
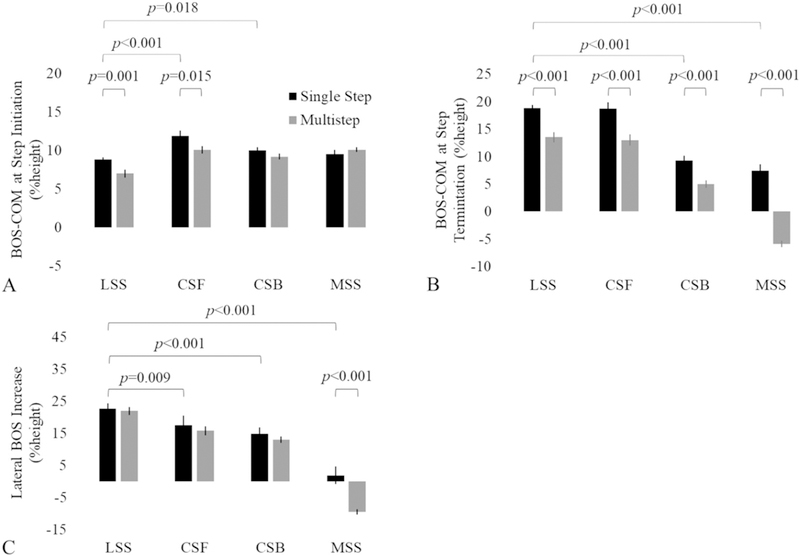
Estimated mean and standard error of the distance between the center of mass (CoM) and base of support (BoS) of a lateral sidestep (LSS), cross-over step to the front (CSF), cross-over step to the back (CSB), and medial sidestep (MSS) at first step initiation (A) and step termination (B). The lateral increase in the BoS resulting from compensatory stepping is shown in C. Statistically significant differences are shown with brackets.
Fig. 3B shows the BoS-CoM at step termination. The CoM position was further from the BoS boundary in single LSS (18.8 (0.6) % height) compared to single CSB (9.3 (0.8) % height) and single MSS (7.4 (1.2) % height) at step termination. The CoM position was closer to the BoS boundary in multistep responses compared to single steps for all step types (LSS-single: 18.8 (0.6); LSS-multi: 13.5 (0.9); CSF-single: 18.7 (1.2); CSF-multi: 13.0 (1.0); CSB-single: 9.3 (0.8); CSB-multi: 5.0 (0.7); MSS-single: 7.4 (1.2); MSS-multi: −5.9 (0.6) % height).
3.4. BoS increase
Fig. 3C shows the lateral BoS increase resulting from each step type. Lateral BoS increase was significantly affected by step type (p < 0.001), step count (p < 0.001), and the interaction of step type and step count (p < 0.001). Although, the step length associated with LSS was only larger than MSS, the lateral BoS boundary increased more in single LSS (22.6 (1.0) % height) than single CSF (17.5 (1.8) % height), single CSB (14.8 (1.2) % height), and single MSS (1.8 (1.7) % height). The BoS boundary decreased in multistep responses of MSS (−9.6 (0.8) % height) compared to single step responses (1.8 (1.7) % height). No significant differences were found between single and multistep responses in LSS, CSF, or CSB.
4. Discussion
We hypothesized that a single LSS would be more stable than a single USS and that the first step of a single step response would be more stable than the first step of a multistep strategy. The results did not entirely support our hypotheses. A single LSS was more stable at step termination than a single CSB and single MSS but not significantly different than a single CSF. At step initiation, a single CSF was more stable than a single LSS. Single step responses were more stable than multistep responses at step termination and step initiation with the exception of CSB and MSS at step initiation, which were not significantly different. Of note, the MoS of single LSS and single CSF were not significantly different at step termination despite the fact that LSS resulted in fewer steps on average than CSF.
Although participants were able to recover balance with a single step following a lateral perturbation using either a USS or a LSS, the mean number of recovery steps was greater when the first step was an USS. A decreased MoS at first step termination provided a possible explanation for the increased number of steps required to recover balance when the first step was a CSB or MSS. However, a decreased MoS does not explain the increase in protective steps required when the first evoked step was a CSF. The difference in mean step count may be explained by the difference in stepping characteristics of LSS and CSF.
LSS are characterized by a significantly larger CoM velocity, larger BoS increase at step termination, and a more rapid step (shorter swing time) than CSF. Although the BoS increase associated with CSF was not as large as LSS, the step length was significantly larger, and the swing time is nearly twice that of a LSS. The decreased CoM velocity at step termination and longer swing time of CSF, compared to LSS, imply a more gradual acceleration and deceleration of the CoM. Inefficient or impaired control of the CoM motion state are possible explanations for the differences in total step count between CSF and LSS. However, the stepping characteristics suggest that inefficient CoM control may not be as critical in CSF compared to LSS because of the gradual acceleration and deceleration of the CoM. Age-related impairment of the hip abductor-adductor muscles engaged in medio-lateral stepping, however, may preclude the use of LSS as a protective stepping response and limit an individual’s ability to accelerate/decelerate the CoM and exacerbate inefficient CoM control.
Age-related declines in hip abductor muscle composition and torque generation have been shown to affect evoked step type (Addision et al., 2017). LSS require a rapid medial-lateral weight shift from the passively loaded limb to the unloaded limb prior to step initiation. Older adults have been shown to have difficulty rapidly developing a hip abductor torque (Mille et al., 2005) and decreased hip abductor and adductor strength (Addision et al., 2017; Inacio et al., 2014; Johnson et al., 2004). Furthermore, older adults have been shown to exhibit delayed weight shifting prior to step initiation (Arampatzis et al., 2008). Delayed weight shifting may result in unintended USS. Declines in hip abductor performance limit the use of LSS and may also cause further difficulties stopping CoM motion at step termination leading to additional compensatory steps when USS are evoked.
Consistent with previous studies following forward loss of balance, a reduced first step MoS was found for multistep responses compared to single step responses (Arampatzis et al., 2008; Barrett et al., 2012; Carty et al., 2011; Carty et al., 2012) and in cross-over steps following a lateral loss of balance (Fujimoto et al., 2017). Additionally, the stability limit was not reached at first step termination in many cases despite additional steps being taken, a finding consistent with previous reports that steps are frequently taken before the stability limit is reached (Pai et al., 1998). Differences in MoS between multistep and single step responses, in the present study, were attributable to differences in CoM velocity at step termination and the BoS-CoM relationship. There were no significant differences in BoS boundary as a result of multistep responses compared to single step responses, which is consistent with anteroposterior perturbations (Arampatzis et al., 2008; Carty et al., 2012) and previous work in cross-over steps (Fujimoto et al., 2017). These results indicate efficient CoM control is an important factor in achieving a sufficient MoS to avoid additional protective steps. As such, CoM control appears to be important as early as step initiation in LSS and CSF (Fujimoto et al., 2015).
4.1. Clinical implications
Perturbation-based balance training has been shown to improve CoM control (Dijkstra et al., 2015; Liu et al., 2016) and balance stability (Lee et al., 2016), and to reduce the incidence of falls during a 12 month follow-up period (Kurz et al., 2016; Rosenblatt et al., 2013). Hip abductor-adductor power training has been shown to increase the prevalence of LSS over USS in older adults (Bair et al., 2016). However, it is not clear if perturbation-based training and/or muscle strength/conditioning provides the most effective improvement in balance outcomes such as number of steps following loss-of-stability. For example, no difference in leg-extensor muscle strength or tendon stiffness in the ankle plantar flexors and knee extensors between single and multistep responders following forward stepping responses have been reported, and practicing dynamic stability control was proposed to be a possible mechanism to reduce the number of protective steps following postural perturbations (Arampatzis et al., 2008). While this view supports perturbation-based training, single session changes from multistep responses to single step responses have been observed to not be sustainable because multistep responders were operating near their performance capacity and reverted to multistep responses after a few trials (Carty et al., 2012). Implications that limited neuromotor performance capacity underlies multiple step responses is supported by reports of hip abductor strength differentiating fallers and non-fallers in community dwelling older adults (Inacio et al., 2014) and is associated with significantly more steps following lateral waist pulls (Addision et al., 2017). While the relative importance of practice-based motor learning (possibly through perturbation-based training) and muscle capacity in improving balance stability is not known, it is likely that both play a role in the ability to recover balance following an unexpected perturbation. Although perturbation training appears to have potential as a fall prevention intervention, maintaining and/or improving functional neuromotor capacity is an accessible means of fall prevention and may further enhance the effects of perturbation training when the approaches are combined.
4.2. Limitations
Among the limitations of the study is our method of defining the CoM and BoS. The CoM was approximated as the midpoint of the posterior iliac spine markers. Yang et al. found that CoM positions were highly correlated with those of the sacrum for walking and slip (R’s > 0.90) (Yang and Pai, 2014). In a study of feet-in-place lateral perturbations, a simplified estimate of the CoM based on the pelvis alone was found to be sufficiently accurate compared to a full-body estimate of the CoM (Inkol et al., 2018). In studies of cable-pull lateral perturbations which evoked stepping reactions, the trunk was tilted away from the perturbation direction at step initiation and toward the perturbation direction at step termination (Bair et al., 2016; Hurt et al., 2011; Mille et al., 2005) with LSS exhibiting this characteristic to a lesser degree. The net effect would be an increased MoS at step initiation and a decreased MoS at step termination with LSS being affected to a lesser degree.
Additionally, the BoS was assumed to exist at the lateral edge of the foot. While this is a commonly used approximation in studies of lateral balance (e.g. (Hurt et al., 2011; Inkol et al., 2018)), this represents a best-case scenario for the BoS and assumes that the center of pressure is at the limit of the boundary defined by the foot. Other studies have shown that the area functionally used for center of pressure movement is smaller than the total BoS (Fujimoto et al., 2013; King et al., 1994). Therefore, the functional BoS would be more accurately defined by the center of pressure location, as reduced functional center of pressure limits have been shown to discriminate between fallers and non-fallers (Fujimoto et al., 2015). However, no difference in the functional base of support in single versus multistep responses was identified in a study of lateral stepping (Fujimoto et al., 2017). Based on results of previous work (Fujimoto et al., 2017), the relative differences in MoS between single and multistep response would likely be similar to those found if functional BoS were reported in this study.
5. Summary
Although lateral balance recovery using a single step was possible with different types of steps, lateral sidesteps more frequently resulted in balance recovery with a single step. Age-related declines in hip abductor muscle performance capacity may preclude older individuals from using lateral sidesteps and limit their ability to reduce the CoM motion on step termination potentially requiring additional steps. CoM control, as early as step initiation, was found to be an important factor in achieving a margin of stability sufficient to recover lateral stability in a single step. Rapid hip abductor torque generation (muscle power) is likely an important factor in controlling early and late CoM position/velocity during a perturbation evoked lateral stepping reaction. Future studies should target investigating the effect of combined hip abductor conditioning and perturbation-based step training on reducing the number of protective steps taken through improved balance stability following lateral imbalance.
Acknowledgements
The assistance of the Baltimore Veterans Affairs Medical Center, and the Geriatric Research, Education and Clinical Center is gratefully acknowledged. The assistance of Woei-Nan Bair, Brock Beamer, Alexandra Cirillo, Masahiro Fujimoto, Hao-Yuan Hsiao, Valentina Graci, Chen-Chieh Lin, Kaitlin Riddle, and Tricia Young is gratefully acknowledged.
Funding
NIH/NIA grant R01AG033607, the University ofMaryland Claude D Pepper-OAIC NIH/NIA grant P30AG028747, the UMANRRT Program (NIDRR 90AR50280, NIDILRR 90AR5004 formerly H133P100014).
Abbreviations:
- BoS
base of support
- BTL
balance tolerance limit
- CoM
center of mass
- CSF
cross-over step to the front
- CSB
cross-over step to the back
- LSS
lateral sidestep
- MoS
margin of stability
- MSS
medially directed sidestep
- USS
unloaded sidestep
Footnotes
Declarations of interest
None.
References
- Addision O, Inacio M, Bair W, Beamer B, Ryan A, Rogers M, 2017. Role of hip abductor muscle composition and torque in protective stepping for lateral balance recovery in older adults. Arch. Phys. Med. Rehabil. 98, 1223–1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arampatzis A, Karamanidis K, Mademli L, 2008. Deficits in the way to achieve balance related to mechanisms of dynamic stability control in the elderly. J. Biomech. 41 (8), 1745–1761. [DOI] [PubMed] [Google Scholar]
- Bair W, Prettyman M, Beamer B, Rogers M, 2016. Kinematics and behavioral analyses of protective stepping strategies and risk for falls among community living older adults. Clin. Biomech. 36, 74–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrett R, Cronin N, Lichtwark G, Mills P, Carty C, 2012. Adaptive recovery responses to repeated forward loss of balance in older adults. J. Biomech. 45 (1), 183–187. [DOI] [PubMed] [Google Scholar]
- Berg K, Wood-Dauphinee S, Williams J, Gayton D, 1989. Measuring balance in the elderly: preliminary development of an instrument. Physiother. Can. 41 (6), 304–311. [Google Scholar]
- Berg K, Wood-Dauphinee S, Williams J, Maki B, 1992. Measuring balance in the elderly: validation of an instrument. Can. J. Public Health 83 (Suppl. 2), S7–S11. [PubMed] [Google Scholar]
- Carty C, Mills P, Barrett R, 2011. Recovery from forward loss of balance in young and older adults using the stepping strategy. Gait Posture 33 (2), 261–267. [DOI] [PubMed] [Google Scholar]
- Carty C, Cronin N, Lichtwark G, Mills P, Barrett R, 2012. Mechanisms of adaptation from a multiple to a single step recovery strategy following repeated exposure to forward loss of balance in older adults. PLoS One 7 (3), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou C, Chien C, Hsueh I, Sheu C, Wang C, Hsieh C, 2006. Developing a short form of the Berg balance scale for people with stroke. Stroke 86 (2), 195–204. [PubMed] [Google Scholar]
- Dijkstra B, Horak F, Kamsma Y, Peterson D, 2015. Older adults can improve compensatory stepping with repeated postural perturbations. Front. Aging Neurosci. 7 (201), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dite W, Temple V, 2002. A clinical test of stepping and chnage of direction to identify multiple falling older adults. Arch. Phys. Med. Rehabil. 83 (11), 1566–1571. [DOI] [PubMed] [Google Scholar]
- Folstein M, Folstein S, McHugh P, 1975. Mini-mental state: a practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12 (3), 189–198. [DOI] [PubMed] [Google Scholar]
- Fujimoto M, Hsu W, Woollacott M, Chou L, 2013. Ankle dorsiflexor strength relates to the ability to restore balance during a backward support surface translation. Gait Posture 38 (4), 812–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto M, Bair W, Rogers M, 2015. Center of pressure control for balance maintenance during lateral waist-pull perturbations in older adults. J. Biomech. 48, 963–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujimoto M, Bair W, Rogers M, 2017. Single and multiple step balance recovery responses can be different at first step lift-off following lateral waist-pull perturbations in older adults. J. Biomech. 55, 41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hof A, Gazendam M, Sinke W, 2005. The condition for dynamic stability. J. Biomech. 38, 1–8. [DOI] [PubMed] [Google Scholar]
- Hurt C, Rosenblatt N, Grabiner M, 2011. Form of the compensatory stepping response to repeated laterally directed postural disturbances. Exp. Brain Res. 214, 557–566. [DOI] [PubMed] [Google Scholar]
- Inacio M, Ryan A, Bair W, Prettyman M, Beamer B, Rogers M, 2014. Gluteal muscle composition differentiates fallers from non-fallers in community dwelling older adults. BMC Geriatr. 14 (37), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inkol K, Huntley A, Vallis L, 2018. Modeling margin of stability with feet in place following a postural perturbation: effect of altered anthropometric models for estimated extrapolated Centre of mass. Gait Posture 62, 434–439. [DOI] [PubMed] [Google Scholar]
- Johnson Hilliard M, Martinez K, Janssen I, Edwards B, Mille M, Zhang Y, Rogers M, 2008. Lateral balance factors predict future falls in community-living older adults. Arch. Phys. Med. Rehabil. 89 (9), 1708–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson M, Mille M, Martinez K, Crombie G, Rogers M, 2004. Age-related changes in hip abductor and adductor joint torques. Arch. Phys. Med. Rehabil. 85 (5), 593–597. [DOI] [PubMed] [Google Scholar]
- King M, Judge J, wolfson L, 1994. Functional base of support decreases with age. J. Gerontol. 49 (6), M258–M263. [DOI] [PubMed] [Google Scholar]
- Kurz I, Gimmon Y, Shapiro A, Debi R, Snir Y, Melzer I, 2016. Unexpected perturbations training improves balance control and voluntary stepping times in older adults - a double blind randomized control trial. BMC Geriatr. 16 (58), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee A, Bhatt T, Pai Y, 2016. Generalization of treadmill perturbation to overground slip during gait: effect of different perturbation distances on slip recovery. J. Biomech. 49 (2), 149–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Bhatt T, Pai Y, 2016. Intensity and generalization of treadmill slip training: high or low, progressive increase or decrease? J. Biomech. 49 (2), 135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan S, Gottlieb B, Maitland S, Meegan D, Spriet L, 2013. The physical activity scale for the Edlerly (PASE) questionairre; does it predict physical health. Int. J. Environ. Res. Public Health 10 (9), 3967–3986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchies C, Alexander N, Schultz A, Ashton-Miller J, 1994. Stepping responses of young and old adults to postural disturbances: kinematics. J. Am. Geriatr. Soc. 42 (5), 506–512. [DOI] [PubMed] [Google Scholar]
- Maki B, McIlroy W, 1999. Control of compensatory stepping reactions: age-related impairment and the potential for remedial intervention. Physiother. Theory Pract. 15 (2), 69–90. [Google Scholar]
- Maki B, McIlroy W, Perry S, 1996. Influence of lateral destabilization on compensatory stepping responses. J. Biomech. 29 (3), 343–353. [DOI] [PubMed] [Google Scholar]
- Maki B, Edmondstone M, McIlroy W, 2000. Age-related differences in laterally directed compensatory stepping behavior. J. Gerontol., Ser. A 55 (5), M270–M277. [DOI] [PubMed] [Google Scholar]
- Marchetti G, Whitney S, 2006. Construction and validation of the 4-item dynamic gait index. Phys. Ther. 86 (12), 1651–1660. [DOI] [PubMed] [Google Scholar]
- Mille M, Johnson M, Martinex K, Rogers M, 2005. Age-dependent differences in lateral balance recovery through protective stepping. Clin. Biomech. 20, 607–616. [DOI] [PubMed] [Google Scholar]
- Myers A, Fletcher P, Myers A, Sherk W, 1998. Discriminative and evaluative properties of the Activities-specific Balance Confidence (ABC) scale. J. Gerontol. 53A (4), M287–M294. [DOI] [PubMed] [Google Scholar]
- Nevitt M, Cummings S, 1993. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The study of osteoporotic fractures research group. J. Am. Geriatr. Soc. 41 (11), 1226–1234. [DOI] [PubMed] [Google Scholar]
- Pai Y, Rogers M, Patton J, Cain T, Hanke T, 1998. Static versus dynamic predictions of protective stepping following waist-pull perturbations in youg and older adults. J. Biomech. 31 (12), 1111–1118. [DOI] [PubMed] [Google Scholar]
- Patton J, Johnson Hilliard M, Martinez K, Mille M, Rogers M, 2006. A simple model of stability limits applied to sidestepping in young, elderly and elderly fallers. In: IEEE Engineering in Medicine and Biology Conference, New York. [DOI] [PubMed] [Google Scholar]
- Pidcoe P, Rogers M, 1998. A closed-loop stepper motor waist-pull system for inducing protective stepping in humans. J. Biomech. 31, 377–381. [DOI] [PubMed] [Google Scholar]
- Podsiadlo D, Richardson S, 1991. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 39 (2), 142–148. [DOI] [PubMed] [Google Scholar]
- Powell L, Myers A, 1995. The activities-specific balance confidence (ABC) scale. J. Gerontol. A Biol. Sci. Med. Sci. 50A (1), M28–M34. [DOI] [PubMed] [Google Scholar]
- Radloff L, 1977. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 (3), 385–401. [Google Scholar]
- Rogers M, Mille M, 2003. Lateral stability and falls in older people. Exerc. Sport Sci. Rev. 31 (4), 182–187. [DOI] [PubMed] [Google Scholar]
- Rogers M, Mille M, 2016. Timing paradox of stepping and falls in ageing: not so quick and quick(er) on the trigger. J. Physiol. 594 (16), 4537–4547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt N, Marone J, Grabiner M, 2013. Preventing trip-related falls by community-dwelling adults: a prospective study. J. Am. Geriatr. Soc. 61 (9), 1629–1631. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Brauer S, Woollacott M, 2000. Predicting the probability for falls in community-dwelling older adults using the timed up & go test. Phys. Ther. 80 (9), 896–903. [PubMed] [Google Scholar]
- Tinetti M, Richman D, Powell L, 1990. Falls efficacy as a measure of fear of falling. J. Gerontol. Psychol. Sci. 45 (6), 239–243. [DOI] [PubMed] [Google Scholar]
- Washburn R, Montoye H, 1986. The assessment of physical activity by questionnaire. Am. J. Epidemiol. 123 (4), 563–576. [DOI] [PubMed] [Google Scholar]
- Yang F, Pai Y, 2014. Can sacral marker approximate center of mass during gait and slip-fall recovery among community-dwelling older adults? J. Biomech. 47 (16), 3807–3812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yungher D, Morgia J, Bair W, Inacio M, Beamer B, Prettyman M, Rogers M, 2012. Short-term changes in protective stepping for lateral balance recovery in older adults. Clin. Biomech. 27 (2), 151–157. [DOI] [PMC free article] [PubMed] [Google Scholar]


