Abstract
Hip arthroscopy is widely utilized to treat femoroacetabular impingement syndrome (FAIS). In order to evaluate the postoperative clinical and functional outcomes at 2-year follow up in patients with and without benign joint hypermobility syndrome following hip arthroscopy with capsular plication for FAIS, consecutive female patients with generalized ligamentous laxity undergoing primary hip arthroscopy with complete T-capsulotomy closure via plication for FAIS were prospectively identified. Patients were matched in a 4:1 ratio based on Beighton-Horan joint mobility index (BHJMI) then classified into no generalized joint laxity (NGJL, Score<4) or generalized joint laxity cohort (GJL, Score=4). Patient and surgical-related factors were analyzed using univariate and paired analysis with statistical significance set at a = 0.05. A total of 125 female patients were included in the study: 25 generalized joint laxity (GJL) patients and 100 matched to age, sex and BMI (NGJL cohort). The results demonstrated that there were no significant differences between demographics, preoperative range of motion, or radiographic analysis on univariate analysis. There was no statistical difference in postoperative range of motion between groups, though both groups demonstrated significant increases in postoperative flexion and postoperative internal rotation following hip arthroscopy. Paired analysis demonstrated no significant difference in HOS-SS, HOS-ADL, mHHS or VAS-pain, while GJL patients reported significantly greater patient satisfaction score at 2-years follow-up (p=0.007). In summary, hip arthroscopy with capsular plication is a highly effective treatment for FAIS in patients with and without generalized joint laxity. In our analysis, patients with and without generalized joint laxity demonstrated statistically similar and significant improvement in outcomes.
INTRODUCTION
Hip arthroscopy is widely utilized to treat femoroacetabular impingement syndrome (FAIS). FAIS is recognized as an important source of hip pain in active patients and has been suggested to contribute to the development of hip osteoarthritis [1–5]. FAIS results from abnormal hip joint morphology and resulting pathologic contact between the acetabulum and the femoral head neck junction [1].
Generalized joint hypermobility is currently recognized as a common, multi-systemic pathology [6]. Hypermobility is a known risk factor for musculoskeletal injuries, including recurrent shoulder dislocation, patellar and ankle instability, anterior cruciate ligament tears and vertebral disc pathology [7–11]. Hip capsular laxity associated with systemic hypermobility may lead to trunk hyperflexion and increasing risk of acetabular labral tear [12, 13].
Patients with increased hip motion are able to place their hip in potentially impinging positions even in the setting of normal osseous anatomy, which may lead to a predisposition for impingement. The association between hypermobility and injury has been shown in dancers and gymnasts [14–16], whose sports require routinely placing the hip in damaging positions, leading to a combination of instability and impingement [17, 18]. Hip arthroscopy has been shown to be a beneficial treatment for these patients [19–21], and capsular repair can mitigate the potential for hip instability after hip arthroscopy [22–24].
Outcomes after hip arthroscopy in hypermobile patients have largely been studied in short-term trials, and there is a dearth of literature on longer-term outcomes in this population. These studies also inconsistently study patients undergoing capsular repair. Pontiff et al. [25] compared women with and without laxity as judged by the Beighton and Horan Joint Mobility Index (BHJMI) found no peri-operative differences in complications or outcomes at 6 months in patients undergoing capsular repair after hip arthroscopy. Naal et al. [26] found that generalized joint laxity (GJL) did not affect functional outcomes at 2-years post-operatively, but this study did not examine range of motion or specify capsular management and assessed patients only undergoing treatment via open surgical dislocation. Long-term outcomes and risks in this theoretically high-risk group remain undefined.
The purpose of this study was to evaluate the post-operative clinical and functional outcomes in patients with and without GJL following hip arthroscopy for FAIS and capsular plication. We hypothesized that there would be no significant differences in post-operative outcomes in a matched cohort of patients with and without joint hypermobility.
MATERIALS AND METHODS
Patient enrollment
After institutional review board approval, patients undergoing hip arthroscopy and labral repair for femoroacetabular impingement from January of 2015 through December 2015 were enrolled in a patient repository database. All clinical data were prospectively collected in a secure repository and patient-reported outcomes (PROs) were collected in a secure electronic outcome data collection database. Inclusion criteria consisted of diagnosis of FAIS and willingness to participate and complete required questionnaires. Exclusion criteria were patients under the age of 16 or above 50 at the time of surgery, functional illiteracy, patients with prior history of pediatric deformities (congenital hip dislocation, slipped capital femoral epiphysis or Perthes disease), osteoarthritis or joint space narrowing <2 mm (Tönnis grade > 0), hip dysplasia (lateral center edge angle [LCEA] < 20°), patients with concomitant arthroscopic procedures in addition to FAI correction (i.e. gluteus medius repair, trochanteric bursectomy, hamstring repair and psoas lengthening), interim lower extremity surgery, and history of previous bilateral hip arthroscopy. Guardian consent and minor assent were obtained for all minors (<18 years) enrolled in the study.
Generalized ligamentous laxity
To ensure consistency, the Beighton test for GJL assessment was performed by an independent observer (trained medical student or physician assistant) pre-operatively on the day of surgery, using established methods [27–29] (Table I). Patient classification into no GJL (NGJL) cohort or GJL cohort was based on the BHJMI [27]. A Beighton score of 0-3 was considered normal [27], while a score between 4 and 9 was considered an indication of GJL.
Table I.
Beighton test
| Right | Left | Max. points | |
|---|---|---|---|
| Active forward trunk flexion with the knees extended and palms flat on the floor | 1 | ||
| Hyperextension of the elbow beyond 10° | 1 | 1 | 2 |
| Hyperextension of the knee beyond 10° | 1 | 1 | 2 |
| Thumb touches flexor aspect of forearm | 1 | 1 | 2 |
| Hyperextension of fifth MCP joint beyond 90° | 1 | 1 | 2 |
MCP, metacarpophalangeal.
Matching
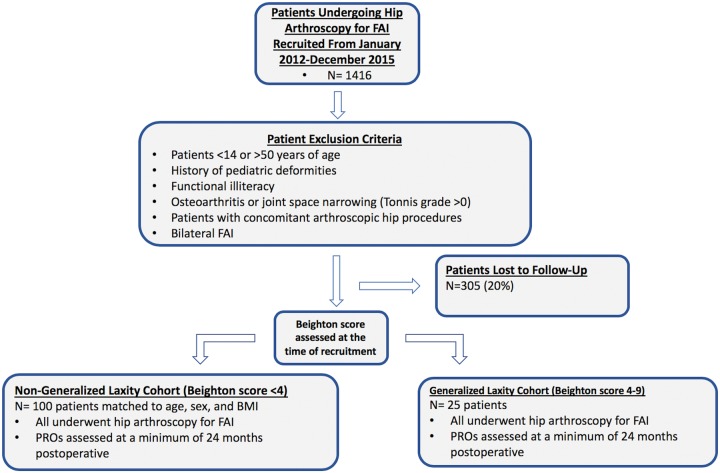
In a healthy college and graduate student population, using Beighton score ≥5 as a cutoff, Russek et al. [30] reported generalized joint hypermobility present in 26.2% (36.7% female and 13.7% male) of the population [30]. A retrospective analysis of the ratio of people without generalized hypermobility to people with generalized hypermobility was 4:1 in the author’s hip patient data repository. An a priori power analysis using a 4:1 matching ratio revealed that a sample size of 106 subjects (86 without hypermobility versus 21 with hypermobility) was required to obtain a power of 0.90 at an alpha level of 0.05 (Cohen, 1988). As such, 25 consecutive female patients were identified as having joint laxity (Beighton score ≥4) in the database and were matched by age, gender and body mass index (BMI) in a 4:1 ratio to patients with Beighton score < 4 (Fig. 1).
Fig. 1.
Flow chart diagram of patient study group recruitment.
Radiographic assessment
Pre- and post-operative weight-bearing anteroposterior (AP) pelvis, false profile and Dunn 90° lateral views were obtained for all participants. Tönnis grade and LCEA were assessed on the AP pelvis radiographs, and alpha angle (AA) was assessment on Dunn lateral radiographs. LCEA was measured from vertical to the lateral edge of the acetabular bone [31]. Hip joint space width (JSW) at superolateral, apical and superomedial positions was measured on AP view to assess for joint narrowing using the methods described by Lequesne et al. [32]. All patients underwent magnetic resonance imaging prior to surgery. All measurements and assessments were performed by a trained fourth year medical student, a sports fellow and a fellowship trained orthopedic surgeon.
Clinical evaluation
Patients underwent comprehensive history and physical examination to assess if symptoms were consistent with FAIS or other hip pathology (gluteal pathology, athletic pubalgia or iliopsoas pathology). FAIS was clinically diagnosed by a fellowship-trained hip arthroscopy specialist based on clinical history, radiographic findings and physical findings [33]. Age, gender, BMI, smoking status, comorbidities and other demographics were recorded. Range of motion was assessed with a goniometer by the senior author to assess flexion, external rotation and internal rotation °with hip flexed 90°.
Operative technique
All hip arthroscopies were performed by a single fellowship-trained hip surgeon at a high-volume academic hospital and have been described in the literature [22, 34, 35]. A standard anterolateral portal was established under fluoroscopic guidance and anterior portal was established under direct visualization. The modified mid anterior portal was established via spinal needle localization under direct arthroscopic visualization. A 2–4 cm capsulotomy connecting the anterior to anterolateral port was performed. Central compartment pathology was then addressed in a standard fashion, including labral repair and acetabular rim trimming if pincer morphology was present. If required, a 5.5-mm burr was used to perform acetabular rim trimming as was deemed adequate based on pre-operative imaging and intraoperative appearance. Hip traction was then released, to allow for T-capsulotomy, access to the peripheral compartment and femoral osteochondroplasty of the cam lesion. The vertical limb of the T-capsulotomy is made perpendicular to the interportal cut, and is ∼2–4 cm without violating the zona orbicularis. Dynamic examination and fluoroscopic imaging was used to confirm that there was no further impingement and that head-neck offset was restored.
The vertical portion of the T-capsulotomy is closed first, beginning at the base of the iliofemoral ligament (IFL) using a capsule-closure device loaded with a No. 2 high–molecular weight polyethylene suture (shuttled with Slingshot, Stryker Sports Medicine, Greenwood Village, CO). The vertical portion of the T-capsulotomy is typically closed with three stitches, compared with two stitches in side-to-side repair. Full thickness (∼3 mm) bites are taken on the leaflet shifted over, with an additional 3 mm bite on the opposite side completing the capsular shift. The bite size is titrated according to overall laxity of the joint. The interportal capsulotomy is then repaired in a side-by-side fashion using a capsular closure device (Injector, Stryker Sports Medicine, Greenwood Village, CO). The Injector is placed through the AL portal to close the lateral aspect of the interportal capsulotomy by placing suture through the acetabular limb of the capsule and then through the lateral leaflet of the IFL. In the same fashion the Injector is used to close the medial aspect of the interportal capsulotomy by placing suture through the acetabular limb and then through the medial leaflet of the IFL utilizing the distal anterolateral accessory (DALA) portal. In total, two interrupted stiches are used to close the interportal limb of the T-capsulotomy.
Patient-reported outcomes
Activities of Daily Living (ADL) and Sport Subscale (SS) of the Hip Outcome Score (HOS) and modified Harris Hip Score (mHHS) surveys were assessed pre-operatively starting at a 2-year window time point (22–24 months). Patients also reported their Visual Analog Scale (VAS) for pain and satisfaction at the same time points.
Statistical analysis
All statistical analyses were performed using SPSS statistical software (IBM SPSS Statistics for Windows, v23.0. Armonk, NY: IBM Corp). Continuous data were analysed with independent and paired t-tests. Levine’s test for variance was performed. Post-hoc corrections were utilized as indicated. Categorical data were analysed using chi-squared tests. Pre- and post-operative PROs scores were compared across cohorts with repeated measures analysis as appropriate.
RESULTS
A total of 125 patients were included in the study with 25 consecutive GJL patients and 100 patients matched to age, sex and BMI (NGJL cohort). There were no significant differences between age (GJL = 21.7 ± 8.7 versus NGJL = 20.8; P = 0.218) or BMI (GJL = 22.4 + 3.3 versus NGJL = 23.1 + 4.7; P = 0.472).The mean Beighton score for patients with GJL was 6.04 ± 1.61, whereas the mean Beighton score of the NGJL cohort was 1.46 ± 1.09. Of note, there were two patients with Ehlers-Danlos syndrome (EDS), both of whom were included in the study. All patients were female and underwent primary hip arthroscopy for FAIS with capsular plication. The mean follow-up time was 29.3 months (SD: ± 8.0 months; range: 23–49 months). There were no significant differences between patient demographics, and univariate analysis did not demonstrate significant differences in history or activities (Table II).
Table II.
Patient demographics
| NGJL ± SD | GJL ± SD | P-value | |
|---|---|---|---|
| n | 100 | 25 | |
| Age | 22.7 ± 8.73 | 18.00 ± 6.25 | 0.059 |
| Gender (female) | 100% | 100% | |
| BMI | 23.1 ± 4.65 | 22.4 ± 3.25 | 0.722 |
| Routine physical exercise | 65 (86.7%) | 24 (96%) | 0.196 |
| Running as primary form of exercise | 54 (64.3%) | 13 (52%) | 0.268 |
| Current smoker | 3 (3.5%) | 1 (4%) | 0.9.04 |
| History of anxiety and/or depression | 8 (10.6%) | 4 (17.4%) | 0.389 |
Assessment of differences in range of motion
Range of motion (hip flexion, internal rotation and external rotation) was not significantly different between GJL and NGJL cohorts both pre- and post-operatively (Table III). Comparison of pre- and post-operative differences in range of motion demonstrated statistical differences in flexion and internal rotation in both patient groups. NGJL patients gained a mean of 7° in flexion (SD: ±13.5; P values: 0.003) and a mean of 5° in internal rotation (SD: 12.3, P values < 0.001). GJL patients gained a mean of 6° in flexion (SD: 12.8; P values: 0.025) and a mean of 8° in internal rotation (SD: 8.3, P values < 0.001).
Table III.
Pre- and post-operative physical exam scores
| NGJL cohort | GJL cohort | P-value | |
|---|---|---|---|
| Pre-operative | |||
| Flexion | 113 ± 13.6 | 118 ±10.7 | 0.286 |
| External rotation | 44.6 ± 10.5 | 50.0 ± 11.1 | 0.713 |
| Internal rotation | 17.3 ± 11.0 | 17.9 ± 9.8 | 0.270 |
| Post-operative | |||
| Flexion | 120 ± 6.60 | 124 ± 8.93 | 0.304 |
| External rotation | 45.2 ± 11.9 | 48.1 ± 13.3 | 0.596 |
| Internal rotation | 23.0 ± 6.10 | 25.5 ± 5.17 | 0.462 |
Measurements in degrees ± SD.
Assessment of radiological findings
To assess whether differences in radiological findings would influence differences in clinical outcomes, measurements were compared between the NGJL and GJL groups. The pre- and post-operative radiographic measurements including the AA, lateral and anterior center edge angles and the mean JSW did not differ between the two cohorts (Table IV). All patients that were in the GJL group were mixed FAI. In total 18 of the 100 matched NGJL cohorts only had cam impingement, with the rest having mixed type.
Table IV.
Changes in radiographic measures
| NGJL cohort | GJL cohort | P-value | |
|---|---|---|---|
| Pre-operative | |||
| AA (°) | 59.3±8.48 | 60.6±8.19 | 0.277 |
| Lateral center edge angle (°) | 31.2±4.77 | 30.6±6.17 | 0.072 |
| Anterior center edge angle (°) | 32.3±5.51 | 31.2±7.22 | 0.445 |
| JSW (mean, mm) | 12.1±1.68 | 13.2±1.21 | 0.056 |
| Post-operative | |||
| AA (°) | 42.7±4.58 | 41.1±5.03 | 0.504 |
| Lateral center edge angle (°) | 27.3±5.08 | 27.4±5.31 | 0.995 |
| Anterior center edge angle (°) | 30.3±5.13 | 29.7±5.14 | 0.684 |
| JSW (mean, mm) | 12.2±1.19 | 13.1±1.77 | 0.188 |
Change (Δ) in PROs between pre-operative and 2-year follow-up time points was compared between cohorts (Table V). The NGJL cohort demonstrated no significant change in HOS-SS, HOS-ADL, mHHS and pain from the GJL cohort. However, hypermobile patients reported, on average, greater patient satisfaction score at the 2-year follow-up (92.9 versus 80.2; P = 0.007). There was a high rate of minimal clinical important difference (MCID) achievement for HOS-ADL, HOS-SS and mHHS in both cohorts, although the difference between the cohorts was not statistically significant (Table VI).
Table V.
Clinical and PROs
| NGJL cohort | GJL cohort | P-value | |
|---|---|---|---|
| ΔHOS-ADL | 27.3 ± 21.98 | 31.3 ± 23.88 | 0.618 |
| ΔHOS-SS | 37.0 ± 26.65 | 35.1 ± 27.31 | 0.944 |
| ΔmHHS | 23.7 ± 18.51 | 28.5 ± 14.77 | 0.913 |
| ΔVAS-pain | −51.5 ± 30.71 | −59.5 ± 29.28 | 0.512 |
| VAS-satisfaction | 80.2 ± 27.8 | 92.9 ± 17.87 | 0.007 |
HOS-ADL, hip outcome score-activities of daily living; HOS-SS, sports subscale; mHHS, modified Harris hip score; VAS, visual analog scale.
Table VI.
Percentage of MCID for PROs
| NGIL | GJL | Chi-square (P-value) | |
|---|---|---|---|
| HOS-ADL | 44 (57%) | 13 (68%) | 0.80 (0.37) |
| HOS-SS | 27 (39%) | 7 (41%) | 0.02 (0.89) |
| mHHS | 44 (66%) | 13 (68%) | 0.21 (0.89) |
DISCUSSION
The principle finding of our study is that no significant differences were found in post-operative outcomes between patients with and without GJL in patients undergoing hip arthroscopy for FAI Syndrome at 2-year follow-up. The matched cohort analysis for gender, age and BMI, patients with and without GJL demonstrated significantly improved objective and subjective outcomes after hip arthroscopy and capsular plication to correct FAIS. There was similarly no difference in pain outcome scores or percentage of patients MCID at 2 years post-operatively, but patient satisfaction was greater in the GJL group. No patients in either cohort sustained peri-operative complications or required revision surgery during the study period.
Supraphysiologic flexibility of the hip is thought to predispose dancers and gymnasts to impingement due to the frequency in which these athletes place their hip in impinging positions [17, 18]. As an increasingly recognized source of pain and injury, cross-sectional studies also have begun to demonstrate that hypermobility in general and FAIS populations is more prevalent than previously thought [30, 36].
Both short and long-term studies have demonstrated no significant difference in patient outcomes in hypermobile patients treated for FAI when compared with non-hypermobile cohorts. Pontiff et al. [25] examined women with and without generalized laxity and found no peri-operative and short-term differences in complications or outcomes at 6 months. Brennan et al showed that patients with GJL had worse outcomes at 6 weeks post-arthroscopy, but similar outcomes after 12 months compared with NGJL patients [21]. Naal et al. [26] showed no difference in patient-reported outcomes (PROs) between patients with and without GJL undergoing open surgery dislocation at a mean follow-up of 3.7 years post-operatively.
In this study, we show that patients with GJL demonstrate no difference in HOS-SS, HOS-ADL, mHHS and pain than NGJL patients at a mean follow-up of 29.3 months after hip arthroscopy, a time point that was not previously reported. Our results also present a more robust description of functional outcomes over time, as we analyse the change in PRO scores while other studies compare scores directly. Finally, we show that performing capsular plication alongside hip arthroscopy on hypermobile patients’ yields functionally similar outcomes to those of patients without hypermobility.
The importance of capsular management at the time of hip arthroscopy is increasingly recognized [37–45]. Iatrogenic instability, secondary to transection of the IFL, is a concern in hypermobile patients, and capsular repair may be crucial in preventing gross dislocation events in these patients. A recent systematic review investigating instability after hip arthroscopy identified 9 case reports (10 patients) describing post-operative dislocation [23]. Upon examination, the most common surgical factor, present in nearly 80% of dislocations, was an unrepaired capsulotomy [23]. The authors proposed female gender and generalized ligamentous laxity as patient-related risk factors for post-arthroscopy dislocation [23]. Outcomes such as these support the theory that neglecting capsular repair in the hypermobile population may increase the incidence of iatrogenic instability and subsequent complications. Our results demonstrate that capsular plication likely plays a role in managing supraphysiological movements in post-operative hypermobile patients, thus restoring their range of motion to be equal to that of non-hypermobile patients.
Routine capsular repair regardless of joint laxity is associated with improved outcomes [22, 34] and all patients in our cohort were treated with capsular repair. This strategy yielded optimal functional and clinical outcomes, with no significant difference from controls, supporting aforementioned literature in that capsular repair may help prevent micro-instability in all populations.
Despite the similarity in outcomes between GJL and NGJL cohorts, we found that hypermobile patients were more satisfied following hip arthroscopy than those without hypermobility. This finding was surprising as Philipon et al. [46] found that higher mHHS score was predictive of greater patient’s satisfaction 5–7 years after hip arthroscopy for FAIS. Our result is likely related to the fact that hypermobile patients were symptomatic with sporting activities but otherwise highly functional, and with return to sports they maintained high functional status and thus achieved greater satisfaction. It is also possible that hip arthroscopy afforded GJL patients a faster rate of recovery than NGJL patients, allowing them to return to sports and activities sooner while reaching equivalent outcomes at 2 years. GJL patients could also have had lower expectations pre-operatively due to pain or other psychological factors (16% of our GJL cohort had a history of anxiety or depression) and outperformed their expected outcome. Further investigation of predictors of satisfaction after hip arthroscopy in a hypermobile cohort could elucidate these specific factors that allow GJL patients to be more satisfied with their outcome.
LIMITATIONS
There are a number of limitations that should be noted. First, all the patients in the hypermobile cohort were female. Although males can show symptoms of hypermobility, it is a pathology which affects females disproportionally [47]. Next, while the power analysis indicated that a sample size of 106 subjects (86 without hypermobility versus 21 with hypermobility), our statistical associations may have been stronger with a larger sample size. Furthermore, there are other possible forms of diagnosing benign joint hypermobility that were not used, which could have improved identification of patients for the study.
Although all patients underwent capsular plication, we did not randomize patients to capsular closure versus capsular plication, which could obscure the effect of capsular management on outcomes. We did not differentiate the etiology of GJL (e.g. idiopathic versus EDS), or identify specific items within Beighton criteria that may have had stronger associations with outcomes. Patients with GJL were also not blinded to their condition, which has the potential to introduce performance bias as they may be more motivated due to their theoretical risk for complications. Additionally, disorders related to hypermobility (e.g. EDS) were self-reported, and may have been underreported in the GJL group. However, the integrity of the analysis is enhanced by 4:1 matching with consecutive patients to minimize the above biases. Last, femoral version was not measured pre-operatively, which can affect internal rotation.
CONCLUSION
Hip arthroscopy with capsular plication is a highly effective treatment for FAIS in patients with and without GJL. In our matched cohort analysis, both cohorts demonstrated statistically similar and significant improvement in outcomes and range of motion regardless of their joint laxity. Those with GJL reported significantly greater satisfaction at 2-year follow-up.
CONFLICT OF INTEREST STATEMENT
B.R.W. is a board/committee member of AAOS, Arthroscopy Association of North America and Society of Military Orthopaedic Surgeons; he is on the editorial/governing board of American Journal of Orthopedics and Arthroscopy; he receives publishing royalties and financial/material support from Elsevier; he is a paid consultant for Genzyme. S.J.N. receives research support from Allosource, Arthrex, Inc., Athletico, DJ Orthopaedics, Linvatec, Miomed, Smith & Nephew and Stryker; education payments from Arthrex, Inc.; IP royalties from Ossur; consulting fees and hospitality payments from Stryker; and publishing royalties and financial/material support from Springer. He is a paid consultant for Ossur and Stryker; he is on the editorial/governing board of American Journal of Orthopedics; he is the board/committee member of American Orthopaedic Society for Sports Medicine and Arthroscopy Association of North America. A.V.S. receives research support from Smith & Nephew.
REFERENCES
- 1. Beck M, Kalhor M, Leunig M, Ganz R.. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 2. Ganz R, Leunig M, Leunig-Ganz K, Harris WH.. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008; 466: 264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ganz R, Parvizi J, Beck M. et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20. [DOI] [PubMed] [Google Scholar]
- 4. Philippon MJ, Maxwell RB, Johnston TL. et al. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc 2007; 15: 1041–7. [DOI] [PubMed] [Google Scholar]
- 5. Shindle MK, Voos JE, Heyworth BE. et al. Hip arthroscopy in the athletic patient: current techniques and spectrum of disease. J Bone Joint Surg Am 2007; 89(Suppl 3): 29–43. [DOI] [PubMed] [Google Scholar]
- 6. Fikree A, Aziz Q, Grahame R.. Joint hypermobility syndrome. Rheum Dis Clin North Am 2013; 39: 419–30. [DOI] [PubMed] [Google Scholar]
- 7. Bilsel K, Ceylan HH, Yildiz F. et al. Acetabular dysplasia may be related to global joint hyperlaxity. Int Orthop 2016; 40: 885–9. [DOI] [PubMed] [Google Scholar]
- 8. Bin Abd Razak HR, Bin Ali N, Howe TS.. Generalized ligamentous laxity may be a predisposing factor for musculoskeletal injuries. J Sci Med Sport 2014; 17: 474–8. [DOI] [PubMed] [Google Scholar]
- 9. Huang B, Kim YT, Kim JU. et al. Modified brostrom procedure for chronic ankle instability with generalized joint hypermobility. Am J Sports Med 2016; 44: 1011–6. [DOI] [PubMed] [Google Scholar]
- 10. Niedzielski KR, Malecki K, Flont P, Fabis J.. The results of an extensive soft-tissue procedure in the treatment of obligatory patellar dislocation in children with ligamentous laxity: a post-operative isokinetic study. Bone Joint J 2015; 97-B: 129–33. [DOI] [PubMed] [Google Scholar]
- 11. Vaishya R, Hasija R.. Joint hypermobility and anterior cruciate ligament injury. J Orthop Surg (Hong Kong) 2013; 21: 182–4. [DOI] [PubMed] [Google Scholar]
- 12. Groh MM, Herrera J.. A comprehensive review of hip labral tears. Curr Rev Musculoskelet Med 2009; 2: 105–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kelly BT, Weiland DE, Schenker ML, Philippon MJ.. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy 2005; 21: 1496–504. [DOI] [PubMed] [Google Scholar]
- 14. Duthon VB, Charbonnier C, Kolo FC. et al. Correlation of clinical and magnetic resonance imaging findings in hips of elite female ballet dancers. Arthroscopy 2013; 29: 411–9. [DOI] [PubMed] [Google Scholar]
- 15. Charbonnier C, Kolo FC, Duthon VB. et al. Assessment of congruence and impingement of the hip joint in professional ballet dancers: a motion capture study. Am J Sports Med 2011; 39: 557–66. [DOI] [PubMed] [Google Scholar]
- 16. Kolo FC, Charbonnier C, Pfirrmann CW. et al. Extreme hip motion in professional ballet dancers: dynamic and morphological evaluation based on magnetic resonance imaging. Skeletal Radiol 2013; 42: 689–98. [DOI] [PubMed] [Google Scholar]
- 17. Reid DC. Prevention of hip and knee injuries in ballet dancers. Sports Med 1988; 6: 295–307. [DOI] [PubMed] [Google Scholar]
- 18. Weber AE, Bedi A, Tibor LM. et al. The hyperflexible hip: managing hip pain in the dancer and gymnast. Sports Health 2015; 7: 346–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Scheper MC, de Vries JE, de Vos R. et al. Generalized joint hypermobility in professional dancers: a sign of talent or vulnerability? Rheumatology (Oxford) 2013; 52: 651–8. [DOI] [PubMed] [Google Scholar]
- 20. Pacey V, Nicholson LL, Adams RD. et al. Generalized joint hypermobility and risk of lower limb joint injury during sport: a systematic review with meta-analysis. Am J Sports Med 2010; 38: 1487–97. [DOI] [PubMed] [Google Scholar]
- 21. Brennan K, Spencer-Smith C, Villar R.. The influence of ligamentous laxity on the outcome of hip arthroscopy for femoroacetabular impingement. Arthroscopy 2013; 29. [Google Scholar]
- 22. Harris JD, Slikker W, Gupta AK. et al. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech 2013; 2: e89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yeung M, Memon M, Simunovic N. et al. Gross instability after hip arthroscopy: an analysis of case reports evaluating surgical and patient factors. Arthroscopy 2016; 32: 1196–204.e1. [DOI] [PubMed] [Google Scholar]
- 24. Kuhns BD, Weber AE, Levy DM. et al. Capsular management in hip arthroscopy: an anatomic, biomechanical, and technical review. Front Surg 2016; 3: 13.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pontiff M, Ithurburn MP, Ellis T. et al. Pre- and post-operative self-reported function and quality of life in women with and without generalized joint laxity undergoing hip arthroscopy for femoroacetabular impingement. Int J Sports Phys Ther 2016; 11: 378–87. [PMC free article] [PubMed] [Google Scholar]
- 26. Naal FD, Muller A, Varghese VD. et al. Outcome of hip impingement surgery: does generalized joint hypermobility matter? Am J Sports Med 2017; 45: 1309–14. [DOI] [PubMed] [Google Scholar]
- 27. Biro F, Gewanter HL, Baum J.. The hypermobility syndrome. Pediatrics 1983; 72: 701–6. [PubMed] [Google Scholar]
- 28. Morlino S, Dordoni C, Sperduti I. et al. Refining patterns of joint hypermobility, habitus, and orthopedic traits in joint hypermobility syndrome and Ehlers-Danlos syndrome, hypermobility type. Am J Med Genet A 2017; 173: 914–29. [DOI] [PubMed] [Google Scholar]
- 29. Morris SL, O’Sullivan PB, Murray KJ. et al. Hypermobility and musculoskeletal pain in adolescents. J Pediatr 2017; 181: 213–21.e1. [DOI] [PubMed] [Google Scholar]
- 30. Russek LN, Errico DM.. Prevalence, injury rate and, symptom frequency in generalized joint laxity and joint hypermobility syndrome in a “healthy” college population. Clin Rheumatol 2016; 35: 1029–39. [DOI] [PubMed] [Google Scholar]
- 31. Hanson JA, Kapron AL, Swenson KM. et al. Discrepancies in measuring acetabular coverage: revisiting the anterior and lateral center edge angles. J Hip Preserv Surg 2015; 2: 280–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lequesne M, Malghem J, Dion E.. The normal hip joint space: variations in width, shape, and architecture on 223 pelvic radiographs. Ann Rheum Dis 2004; 63: 1145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Griffin DR, Dickenson EJ, O'Donnell J. et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016; 50: 1169–76. [DOI] [PubMed] [Google Scholar]
- 34. Frank RM, Lee S, Bush-Joseph CA. et al. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med 2014; 42: 2634–42. [DOI] [PubMed] [Google Scholar]
- 35. Slikker W 3rd, Van Thiel GS, Chahal J, Nho SJ.. The use of double-loaded suture anchors for labral repair and capsular repair during hip arthroscopy. Arthrosc Tech 2012; 1:e213–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Naal FD, Hatzung G, Muller A. et al. Validation of a self-reported Beighton score to assess hypermobility in patients with femoroacetabular impingement. Int Orthop 2014; 38: 2245–50. [DOI] [PubMed] [Google Scholar]
- 37. Benali Y, Katthagen BD.. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy 2009; 25: 405–7. [DOI] [PubMed] [Google Scholar]
- 38. Dierckman BD, Guanche CA.. Anterior hip capsuloligamentous reconstruction for recurrent instability after hip arthroscopy. Am J Orthop (Belle Mead NJ) 2014; 43: E319–23. [PubMed] [Google Scholar]
- 39. Ferguson SJ, Bryant JT, Ganz R, Ito K.. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech 2003; 36: 171–8. [DOI] [PubMed] [Google Scholar]
- 40. Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy 2009; 25: 400–4. [DOI] [PubMed] [Google Scholar]
- 41. Mei-Dan O, McConkey MO, Brick M.. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy 2012; 28: 440–5. [DOI] [PubMed] [Google Scholar]
- 42. Philippon MJ, Schenker ML, Briggs KK. et al. Revision hip arthroscopy. Am J Sports Med 2007; 35: 1918–21. [DOI] [PubMed] [Google Scholar]
- 43. Ranawat AS, McClincy M, Sekiya JK.. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am 2009; 91: 192–7. [DOI] [PubMed] [Google Scholar]
- 44. Sansone M, Ahlden M, Jonasson P. et al. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc 2013; 21: 420–3. [DOI] [PubMed] [Google Scholar]
- 45. Shu B, Safran MR.. Hip instability: anatomic and clinical considerations of traumatic and atraumatic instability. Clin Sports Med 2011; 30: 349–67. [DOI] [PubMed] [Google Scholar]
- 46. Philippon MJ, Skendzel JG, Herzog M. et al. Hip arthroscopy for FAI: predictors of patient satisfaction and conversion to total hip arthroplasty 5 to 7 years following arthroscopy. Orthop J Sports Med 2013; 1(4 Suppl). [Google Scholar]
- 47. Scher DL, Owens BD, Sturdivant RX, Wolf JM.. Incidence of joint hypermobility syndrome in a military population: impact of gender and race. Clin Orthop Relat Res 2010; 468: 1790–5. [DOI] [PMC free article] [PubMed] [Google Scholar]