Abstract
Labral pathology is seen in both dysplastic and borderline dysplastic hips. Periacetabular osteotomy (PAO) is the treatment of choice for dysplasia. However, some authors have suggested that borderline dysplastic hips with concurrent labral pathology should be treated arthroscopically. The purpose of this study was to investigate the frequency of labral pathology between dysplastic and borderline dysplastic hips, whether centre-edge (CE) angle is associated with labral pathology, and finally if pain and labral pathology are associated. Ninety-nine symptomatic patients (104 hips) scheduled for PAO were examined. Five patients were excluded due to complaints from multiple joints and four failed to show at 2-year follow-up. Five patients did not fill out questionnaires preoperatively. Hips were characterized as dysplastic (CE angle <20°) and borderline dysplastic (CE angle 20° ≤ 25°). A magnetic resonance arthrography was performed, and labral pathology was classified according to the Czerny classification. Association with the CE angle, the acetabular index (AI) and preoperative WOMAC pain score was tested by multiple linear regression. There was no significant difference in frequency of labral pathology when comparing the two groups. Across the cohort, 86 of 99 patients had labral pathology. The CE angle was associated with increasing severity of labral pathology, whereas the AI angle and preoperative pain were not associated with labral pathology. Decreased lateral coverage adversely loads the labrum, predisposing it to tears. We advocate reorienting the biomechanical forces through PAO, not arthroscopic treatment. Level of pain was not associated with labral pathology, suggesting that labral pathology may not alone explain the dysplastic pain complex.
INTRODUCTION
Wiberg [1] defined a dysplastic hip as definitively pathological with a centre-edge (CE) angle <20° and hips with borderline CE angles 20° ≤ 25° as potentially pathological. Further studies have confirmed the link between dysplasia and early osteoarthritis [2]. A number of patients with hip dysplasia experience pain and reduced function [3]. To treat these symptoms and to counteract the development of osteoarthritis at an early age, the periacetabular osteotomy (PAO) that reorients the acetabulum and increase the acetabular coverage may be performed [4]. Various authors have published follow-up results after adoption of the Bernese osteotomy [5–9]. Clohisy et al. [10] published a literature review in 2009 with a follow-up ranging from 3.2 to 12 years with 0–21% failure and conversion to total hip arthroplasty (THA).
A controversy still reigns around the best treatment of borderline dysplasia. Labral lesions are often seen in this group [11] and some clinicians advocate arthroscopy and labral repair. Lodhia et al. [12] performed a systematic review of the literature in 2016 suggesting that one can achieve good results in this patient group with arthroscopy but that in more severe deformities PAO is preferred. Due to the lack of data, no firm conclusion could be reached. When performing PAO using a modified Smith–Petersen approach a simultaneous arthrotomy and labral repair may be performed; however, complete visualization of the labrum may not be possible and labral pathology may be underdiagnosed [13]. An alternative is to perform arthroscopy after PAO and case series have reported no difference in outcome using this approach compared to the former [14]. At our institution, we first perform PAO using the minimally invasive transsartorial technique [15] to correct the bony malformation. If the patient shows symptoms despite postoperative rehabilitation, a decision is made whether to schedule the patient for an arthroscopy. Unfortunately, limited clinical benefit has been seen in arthroscopy after PAO [16]. The great majority of patients with hip dysplasia have labral pathology [13, 17]. In our view, after unloading the labrum through PAO, many patients have a clear regression in pain and discomfort and do not need labral repair.
The purpose of this study was to investigate whether there is a difference in the frequency of labral pathology in symptomatic patients with CE angles <20° and between 20° ≤ 25°. Furthermore, to investigate the association between the CE angle and labral lesions pathology graded according to the Czerny classification [18], and finally to investigate the association between pain and labral pathology.
MATERIALS AND METHODS
The design of this study is a prospective cohort study with a 2-year clinical and radiographic follow-up. The study was conducted on the same study-population as the study by Hartig-Andreasen et al. [19] but with different hypotheses. Ethical approval was not needed since all patients scheduled for PAO had magnetic resonance arthrography (MRA) during 20 months in 2010–11 as part of a quality assessment of PAO at our department. The Danish Data Protection Agency approved the study (journal number: 2012-58-006). Ninety-nine patients (104 hips) who were consecutively scheduled for PAO between January 2010 and August 2011 were included. Mean age of the patients were 34.1 years (range 14.5–58.9 years). Five patients had complaints from multiple joints and were excluded as they did not represent a typical PAO patient. Of the remaining patients, eight hips had previously undergone hip arthroscopy and one patient had been operated with a combined femur and pelvic osteotomy. Six patients failed to fill out preoperative patient-reported outcome measures (PROMs) and a further three patients failed to show up at 2-year follow-up. Hence, the study group consisted of 94 patients (99 hips, 87 female, and 56 right hips) with a complete radiographic data set, 88 patients (93 hips, 83 female, and 51 right hips) with complete preoperative questionnaires and 85 patients (90 hips, 80 female, and 49 right hips) whom had a complete data set including 2-year follow-up (Fig. 1).
Fig. 1.
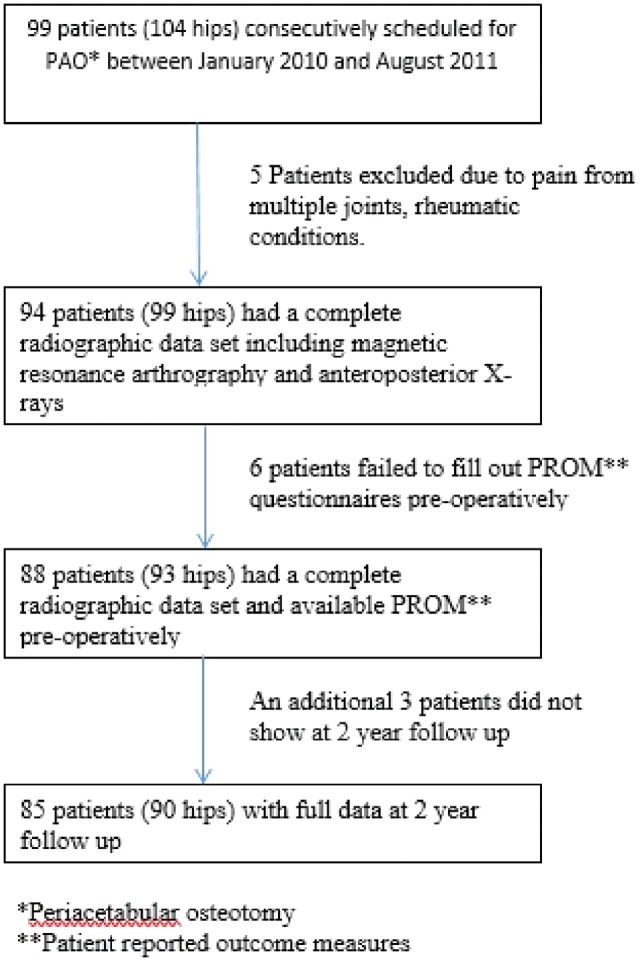
Flow diagram of patients with hip dysplasia included in this study.
Twenty-three patients underwent PAO surgery on the opposite hip within the 2-year study period, and three patients had screws removed following PAO. One complication among the 104 hips was observed in the form of an obturator nerve lesion resulting in pain and paralysis of the adductor muscles. Another hip developed osteoarthritis during the study period. Dysesthesia of the lateral thigh due to affection of the lateral cutaneous nerve was regarded as an expected postoperative affliction; two patients had painful dysesthesia at 2-year follow-up. No further intra- or postoperative complications were observed.
Preoperatively and at 2-year follow-up patients were requested to fill out the Western Ontario and McMaster Universities Osteoarthritis index (WOMAC) [20], the Oxford hip score (OHS) [21] and the general health questionnaire short form 36, version 1 [22]. The preoperative and postoperative scores from all PROMs were presented for the dysplasia group and the borderline dysplasia group. When collating the PROM scores for the patients who underwent bilateral PAO during the study period, only scores for the first operated hip was included in the analyses. To enhance the comparability with other studies, the summarized WOMAC total score was normalized to a scale of 0–100, and the OHS score was presented as 0–48, the highest value indicating the best possible score for both. Physical and mental component scores were calculated from the SF-36 data. Based on the literature, we divided the OHS into four groups [excellent (>41), good (34–40), fair (27–33), and poor (<27)] and the minimal clinically important change (MCID) was set at an increase by one category [23]. MCID for WOMAC has been reported to be 15–20 and 2.0–7.8 for SF-36 [24].
Radiography
All patients underwent MRA and anteroposterior (AP) X-rays prior to PAO and a follow-up standing AP X-ray at 2 years. The majority of AP X-rays were standing (weight-bearing). However, some patients referred from other institutions had undergone supine AP X-rays. It has previously been reported that the CE angle is not affected by pelvic tilt [25, 26], in contrast to signs of retroversion [27]. One investigator (C.H.A.) assessed the following radiographic parameters: CE angle [1], the acetabular index (AI) angle [28] and the Tönnis grade of osteoarthritis. Hips were characterized dysplastic if the CE angle was below 20° and borderline dysplastic if CE was between 20° and/or equal to 25°. AI-angles were considered normal if within 0–10°.
The MRA were performed with a 1.5 T Scanner (Siemens Magnetom Symphony) preceded by guided injection of 10 ml of diluted gadolinium contrast medium (Gd-DTPA, 2 mmol/l) into the hip joint. The Czerny classification [18] was chosen to evaluate the labrum for tears and hypertrophy due to its high reproducibility and good intraobserver reliability (kappa coefficient = 0.96) [29]. One senior radiologist (J.G.) performed all intra-articular injections and analysis of MRA scans.
Sample size/power considerations
The sample size of this study is based on our previous study performed with magnetic resonance imaging (MRI) arthrography in patients with hip dysplasia [19]. We performed a sample size calculation prior to the initiation of this study. Based on a significance level of 5%, a power of 80%, and an estimated difference of 20% point in the frequency of labral pathology, we found that we had to include 34 patients in each group.
Statistics
Normal distribution was checked with histograms and probability plots. The frequency of labral pathology in groups of patients with CE angles <20° and between 20° ≤ 25° was described with absolute numbers and percentages and tested with the Fisher’s exact test. Multiple linear regression analysis was used to investigate the association between the CE angle and labral pathology graded according to the Czerny classification, with the CE angle as the independent variable and labral pathology as the dependent variable. Adjustments were made for age and gender. 99 hips were available for the statistical analysis of the radiographic data set after exclusion of hips with pain from multiple joints.
Furthermore, multiple linear regression analyses were used to estimate the associations between pain and labral pathology adjusted for age and gender. To assess preoperative pain, we used the pain subscale of the WOMAC score which was calculated with a range of 0–20, the latter being the most pain. The cohort was limited to 93 hips as six patients failed to fill out pain questionnaires preoperatively. Patients who underwent PAO bilaterally were asked rate each hip separately. Before performing the multiple regression analyses, it was investigated if the model assumptions were fulfilled, using QQ-plots, Scatter-plots and histograms. Whether any of the potential confounders were effect modificators was also investigated. The significance level was set at 0.05 and the STATA 13 (StataCorp, College Station, TX, USA) software package was used for data analysis.
RESULTS
Our primary aim was to investigate whether there is a difference in the frequency of labral pathology in symptomatic patients with dysplasia (CE <20°) and borderline dysplasia (CE 20 ≤ 25°). Table I shows the two study groups. No statistical difference concerning gender, age or preoperative Tönnis grade between the two groups were found. The Fisher’s exact test was applied and showed that the frequency of labral pathology is not significantly higher in patients with CE angles <20° than in patients with CE angles between 20° ≤ 25°, (P = 0.07); however, a clear trend was seen (Table II). The frequency of labral pathology was high in both the dysplasia group (93%) and the borderline dysplasia group (80%) (Fig. 2).
Table I.
Description of the Czerny classification [30]
| Czerny grade | Description |
|---|---|
| 0 | Normal triangular shaped labrum without hypertrophy. Intact recess between joint capsule and labrum |
| 1a | Increased signal intensity within labrum that does not extend to the margin. Triangular shape. Intact recess between joint capsule and labrum. |
| 1b | Increased signal intensity within labrum that does not extend to the margin. Thickened and deformed shape. Recess between joint capsule and labrum not visible |
| 2a | Extension of contrast material into the labrum. Triangular shape. Intact recess between joint capsule and labrum. |
| 2b | Extension of contrast material into the labrum. Thickened and deformed shape. Recess between joint capsule and labrum not visible |
| 3a | Detached labrum. Triangular shape. Intact recess between joint capsule and labrum. |
| 3b | Detached labrum. Thickened and deformed shape. Recess between joint capsule and labrum not visible |
Table II.
Frequency of labral pathology and patients’ characteristics in patients with CE angles ≤20° and in patients with CE angles between 20° and ≤25°
| CE angles <20° (n = 55) | CE angles 20< to <25° (n = 44) | P-value | |
|---|---|---|---|
| Labral pathology | 51 (93%) | 35 (80%) | 0.07 |
| 0 | 4 (7%) | 9 (20%) | |
| 1a | 1 (2%) | 2 (5%) | |
| 1b | 1 (2%) | 2 (5%) | |
| 2a | 7 (13%) | 7 (16%) | |
| 2b | 0 (0%) | 3 (7%) | |
| 3a | 31 (56%) | 16 (36%) | |
| 3b | 11 (20%) | 5 (11%) | |
| Gender male/female | 8/47 | 4/40 | 0.54 |
| Age (years)a | 34.8 ± 11.2 | 33.6 ± 12.55 | 0.61 |
| Hip side (right/left) | 32/23 | 24/20 | 0.84 |
| Centre edge angle (°)a | 14.13 ± 3.83 | 21.16 ± 1.29 | <0.00001 |
| Acetabular index angle (°)a | 17.36 ± 5.24 | 12.30 ± 2.61 | <0.00001 |
| Tönnis osteoarthritis gradea | 0.45 ± 0.50 | 0.59 ± 0.50 | 0.21 |
aValues are presented as mean ± standard deviation.
Fig. 2.
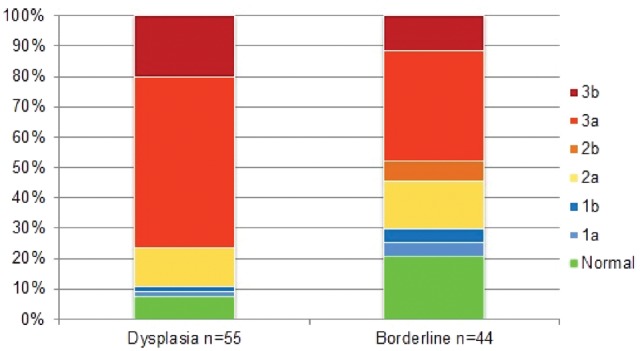
Frequency of labral pathology graded by the Czerny classification in the 99 hips that underwent MRA, subdivided into the dysplasia and borderline dysplasia subgroup.
A multiple linear regression analysis was performed with the CE angle as the independent variable and labral pathology as the dependent variable (Table III). There was a significant association between the CE angle and labral lesions pathology graded according to the Czerny classification (r2 = 0.11, P = 0.01). The higher the CE angle, the lower graded was the labral pathology. One degree increase in the preoperative CE angle was associated with a 0.10 point lower grading of severity on the Czerny classification. In a similar fashion, we investigated whether there was an association between AI angle and labral pathology according to the Czerny classification. A tendency to support this was seen but it did not reach statistical significance (r2 = 0.11, P = 0.06).
Table III.
Analysis of the linear association between the preoperative CE angle, the preoperative AI angle and labral lesions pathology graded according to the Czerny classification
| N | Change in labral lesions pathologya | 95% CI | P-value | R2 | |
|---|---|---|---|---|---|
| Preoperative CE angle (°) | 99 | −0.10 | −0.19 to −0.02 | 0.01 | 0.11 |
| Preoperative AI angle (°) | 99 | 0.08 | −0.003 to 0.15 | 0.06 | 0.11 |
aChange in labral lesions pathology graded according to the Czerny classification by one-point increase in preoperative CE angle or AI angle, adjusted for age and gender.
Finally, we investigated the association between pain and labral pathology (Table IV). There was no association between labral lesions pathology graded according to the Czerny classification and preoperative pain (r2 = 0.04, P = 0.95).
Table IV.
Analysis of the linear association between the preoperative WOMAC pain score and labral lesions pathology graded according to the Czerny classification
| N | Change in labral lesions pathologya | 95% CI | P-value | R2 | |
|---|---|---|---|---|---|
| Preoperative pain, WOMAC pain score | 93 | 0.004 | −0.11 to 0.11 | 0.95 | 0.04 |
aChange in labral lesions pathology graded according to the Czerny classification by one-point increase in preoperative pain, adjusted for age and gender.
Median WOMAC score and WOMAC pain score decreased by 24 and seven for the dysplasia group and 21 and three for the borderline group at 2-year follow-up. The changes observed were substantially larger than the MCID. The median OHS score decreased by 14 in the dysplasia group and by 11 in the borderline dysplasia group. Both the dysplasia and borderline median increased by two categories from fair (27–33) to excellent (>41). Concerning SF-36, we saw a change of 9.5 and 6.6 in the physical component and 2.3 and 3.9 in the mental component for the dysplasia group and the borderline dysplasia group at 2-year follow-up, respectively. The SF-36 showed a tendency towards improvement, but only the physical component for the two groups exceeded the MCID suggested previously (Table V).
Table V.
Difference in median PROM values for the two groups preoperatively and at 2-year follow-up
| PROM | CE angles <20° (n = 47) |
CE angles 20°≤ to <25° (n = 38) |
||||
|---|---|---|---|---|---|---|
| Preoperative | At 2 years | Change | Preoperative | At 2 years | Change | |
| WOMAC (0–100)a | 69 (56–79) | 93 (77–98) | 24 | 69 (57–80) | 90 (78–99) | 21 |
| WOMAC pain (0–20)a | 12 (10–15) | 19 (15–20) | 7 | 13 (11–15) | 16 (14–20) | 3 |
| OHS (0–48)a | 29 (23–34) | 43 (35–46) | 14 | 31 (27–35) | 40 (30–47) | 9 |
| SF-36 physical componentb | 37.0 ± 8.8 | 46.5 ± 9.2 | 9.5 | 38.9 ± 7.9 | 45.5 ± 12.2 | 6.6 |
| SF-36 mental componentb | 54.2 ± 9.1 | 56.5 ± 7.1 | 2.3 | 49.5 ± 10.4 | 53.4 ± 10.7 | 3.9 |
aValues are presented as median (interquartile range).
bValues are presented as mean ± standard deviation.
As reported in the previous paper concerning this cohort, 22 hips had hip arthroscopy after PAO within the 2-year study period. Preoperatively, 14 patients had Type 3a tears, one patient had Type 3b tears and one patient had a Type 1 tear. Four patients were preoperatively classified as Type 0, but upon arthroscopy, the labrum was found to be affected in three patients and was treated accordingly (Table VI). One hip was converted to total hip arthroplasty. With THA as endpoint the hip joint survival rate was 99% at 2 years, which is similar to data published earlier from our institution [15, 31].
Table VI.
A table depicting preoperative Czerny grade on MRA and subsequent treatment by arthroscopy within the 2-year study period
| Preoperative Czerny grade | Arthroscopic treatment |
|---|---|
| 3a | Labral refixation |
| 3a | Labral refixation |
| 1a | Rim trimming, cheilectomy, partial synovectomy |
| 0 | Rim trimming, cheilectomy |
| 3a | Rim trimming, cheilectomy, labral refixation, partial synovectomy |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 0 | Rim trimming, cheilectomy, labral refixation, partial synovectomy |
| 3a | Rim trimming, cheilectomy |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 3a | Internal snapping hip |
| 3a | Rim trimming cheilectomy, partial synovectomy |
| 0 | Synovectomy, capsulotomy |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 3b | Rim trimming, cheilectomy, labral refixation |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 3b | Rim trimming, cheilectomy, labral refixation |
| 3a | Rim trimming, cheilectomy, labral refixation |
| 0 | Rim trimming, cheilectomy, labral refixation |
| 3a | Labral refixation |
| 3a | Rim trimming, cheilectomy, labral refixation |
DISCUSSION
We found an overall high frequency of labral pathology in hips with dysplasia and in borderline dysplasia with no statistically significant difference between the two groups. The high prevalence of labral pathology in the borderline dysplasia group was far beyond what one would expect in a non-dysplastic symptomatic hip [32]. This lends credibility to the notion that borderline dysplasia is a pathological condition. However, we could not demonstrate an association between the severity of labral pathology and pain upon presentation. As such, our study indicates that there is more to the dysplastic pain complex than a sole structure. For example, recent evidence has shown an association between iliopsoas and gluteus medius tendon pathology and pain in dysplasia patients [33]. Furthermore, microinstability and rim overload are also possible pain generators [34].
The severity of labral pathology according to the Czerny classification is associated with decreasing CE angle. In the clinical setting, few studies have assessed the association between CE angle and labral pathology. Garabekyan et al. [35] reported an association between CE angle and labral length. They found significantly larger values of labral length, indicating a hypertrophic labrum, in dysplastic and borderline dysplastic hips. Both this study and our result indicate that borderline dysplasia is a structural pathologic condition with a high prevalence of labral pathology.
It is interesting to note that a linear regression analysis with focus on the AI angle did not show a significant association. However, a clear trend was seen supporting the results regarding the CE angle mentioned previously. This may be due to the fact that the AI angle is only a measure of the inclination of the sourcil and does not take into account the femoral head’s position in relation to the lateral acetabular margin. As such, it is not a direct indicator of acetabular coverage but rather of acetabular morphology.
At 2 years we saw a substantial improvement in both WOMAC and OHS scores and in the physical component of SF-36. Pain at presentation was not statistically associated with grade of labral pathology. Some authors have argued that labral hypertrophy and tearing causes the pain associated with pre-osteoarthritic dysplasia. Our results suggest the aetiology of pain is multifactorial and cannot be attributed to a single structure. Investigating labral pathology with MRA may be superfluous in the diagnostic algorithm of dysplasia in the young. MRA or MRI may add value in a more mature patient category where one wishes to identify patients with poor cartilage and insipient osteoarthritis.
The approach to treatment varies in the literature. Recently, Domb et al. have published promising results concerning arthroscopic treatment of labral lesions in borderline dysplasia. The study group consisted of 24 patients and 19% required secondary arthroscopic procedures. They emphasize the need for lateral preservation and capsular plication as essential to retaining hip stability [36].
However, in the normal ball and socket hip joint, little load is placed on the capsule and the labrum is a secondary supporting structure. Theoretical studies using finite element analysis have proven severe increase in load superolaterally in dysplastic hips and a decrease in the lateral load after re-orientation of the acetabulum through PAO [37]. A 2.8–4-fold increase in the load supported by the labrum in hips with a CE angle of <25° [38] has been showed. Considering the increased anterolateral stress and increased load on the labrum in borderline dysplasia, we prefer to reorient the acetabulum rather than focus on secondary structures such as the labrum or capsule to compensate the load. In this way, we believe that we create a foundation for a stable hip joint. The literature supports this approach as multiple studies have shown poor results through arthroscopy alone and in some cases postoperative subluxation of the joint and quick progression to osteoarthritis [39–42].
The results of this study have shown that labral pathology and pain are not associated. Through arthroscopy alone, one may not address other pain generators such as rim overload and tendinopathy. In this cohort only 27% of patients went on to require arthroscopy after unloading the labrum through PAO although 87% had labral pathology. Furthermore, only one patient required conversion to THA.
This study is limited as the study group is not representative of the population as a whole. All patients have been through thorough investigation before referral to our institution. Our cohort represents an example of clinical practice at a tertiary hip preservation institution. Furthermore, the dysplastic joint has a wide and diverse morphology. The CE angle only represents the lateral coverage in respect to the centre of the femoral head. Acetabular version and femoral morphology are important factors to take into account when performing PAO. We did not compensate for pelvic tilt as studies have showed negligible effect on the CE angle between supine and standing radiographs [26, 43, 44].
CONCLUSION
Our results support the position that borderline dysplasia is a pathological condition. Decreased lateral coverage adversely loads the labrum, with consequent hypertrophy and tears predisposing the hip to early osteoarthritis. The lack of association between pain and labral pathology suggests that the dysplastic pain complex is multifactorial and not attributable to a single structure. MRA may be of limited value in the diagnostic work-up in the young dysplasia patient. The authors advocate treatment of this patient group with PAO to optimize the biomechanics of the dysplastic hip joint before one considers specific arthroscopic treatment of labral lesions.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand 1939; 83: 7–135. [Google Scholar]
- 2. Reijman M, Hazes JM, Pols HA. et al. Acetabular dysplasia predicts incident osteoarthritis of the hip: the Rotterdam study. Arthritis Rheum 2005; 52: 787–93. [DOI] [PubMed] [Google Scholar]
- 3. Jacobsen JS, Nielsen DB, Sorensen H. et al. Joint kinematics and kinetics during walking and running in 32 patients with hip dysplasia 1 year after periacetabular osteotomy. Acta Orthop 2014; 85: 592–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mechlenburg I, Nyengaard JR, Rømer L. et al. Changes in load-bearing area after Ganz periacetabular osteotomy evaluated by multislice CT scanning and stereology. Acta Orthop Scand 2004; 75: 147–53. [DOI] [PubMed] [Google Scholar]
- 5. Wells J, Millis M, Kim YJ. et al. Survivorship of the bernese periacetabular osteotomy: what factors are associated with long-term failure? Clin Orthop Relat Res 2017; 475: 396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mechlenburg I, Nyengaard JR, Gelineck J. et al. Cartilage thickness and cyst volume are unchanged 10 years after periacetabular osteotomy in patients without hip symptoms. Clin Orthop Relat Res 2015; 473: 2644–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buchler L, Beck M.. Periacetabular osteotomy: a review of swiss experience. Curr Rev Musculoskelet Med 2014; 7: 330–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dahl LB, Dengso K, Bang-Christiansen K. et al. Clinical and radiological outcome after periacetabular osteotomy: a cross-sectional study of 127 hips operated on from 1999-2008. Hip Int 2014; 24: 369–80. [DOI] [PubMed] [Google Scholar]
- 9. Albers CE, Steppacher SD, Ganz R. et al. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res 2013; 471: 1602–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clohisy JC, Schutz AL, St John L. et al. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res 2009; 467: 2041–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hartig-Andreasen C, Soballe K, Troelsen A.. The role of the acetabular labrum in hip dysplasia. A literature overview. Acta Orthop 2013; 84: 60–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lodhia P, Chandrasekaran S, Gui C. et al. Open and arthroscopic treatment of adult hip dysplasia: a systematic review. Arthroscopy 2016; 32: 374–83. [DOI] [PubMed] [Google Scholar]
- 13. Redmond JM, Gupta A, Stake CE. et al. The prevalence of hip labral and chondral lesions identified by method of detection during periacetabular osteotomy: arthroscopy versus arthrotomy. Arthroscopy 2014; 30: 382–8. [DOI] [PubMed] [Google Scholar]
- 14. Domb BG, LaReau JM, Hammarstedt JE. et al. Concomitant hip arthroscopy and periacetabular osteotomy. Arthroscopy 2015; 31: 2199–206. [DOI] [PubMed] [Google Scholar]
- 15. Troelsen A, Elmengaard B, Soballe K.. A new minimally invasive transsartorial approach for periacetabular osteotomy. J Bone Joint Surg Am 2008; 90: 493–8. [DOI] [PubMed] [Google Scholar]
- 16. Hartig-Andreasen C, Nielsen TG, Lund B. et al. Outcome after arthroscopic labral surgery in patients previously treated with periacetabular osteotomy: a follow-up study of 43 patients. J Hip Preserv Surg 2017; 4: 67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ginnetti JG, Pelt CE, Erickson JA. et al. Prevalence and treatment of intraarticular pathology recognized at the time of periacetabular osteotomy for the dysplastic hip. Clin Orthop Relat Res 2013; 471: 498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Czerny C, Hofmann S, Neuhold A. et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology 1996; 200: 225–30. [DOI] [PubMed] [Google Scholar]
- 19. Hartig-Andreasen C, Troelsen A, Thillemann TM. et al. Risk factors for the need of hip arthroscopy following periacetabular osteotomy. J Hip Preserv Surg 2015; 2: 374–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bellamy N, Buchanan WW, Goldsmith CH. et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988; 15: 1833–40. [PubMed] [Google Scholar]
- 21. Dawson J, Fitzpatrick R, Carr A. et al. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br 1996; 78: 185–90. [PubMed] [Google Scholar]
- 22. Bjorner JB, Thunedborg K, Kristensen TS. et al. The Danish SF-36 health survey: translation and preliminary validity studies. J Clin Epidemiol 1998; 51: 991–9. [DOI] [PubMed] [Google Scholar]
- 23. van der Wees PJ, Wammes JJ, Akkermans RP.. Patient-reported health outcomes after total hip and knee surgery in a Dutch University Hospital Setting: results of twenty years clinical registry. BMC Musculoskelet Disord 2017; 18: 97.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Angst F, Aeschlimann A, Stucki G.. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum 2001; 45: 384–91. [DOI] [PubMed] [Google Scholar]
- 25. Tannast M, Fritsch S, Zheng G. et al. Which radiographic hip parameters do not have to be corrected for pelvic rotation and tilt? Clin Orthop Relat Res 2015; 473: 1255–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Troelsen A, Jacobsen S, Rømer L. et al. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res 2008; 466: 813–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wassilew GI, Heller MO, Diederichs G. et al. Standardized AP radiographs do not provide reliable diagnostic measures for the assessment of acetabular retroversion. J Orthop Res 2012; 30: 1369–76. [DOI] [PubMed] [Google Scholar]
- 28. Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res 1976; 119: 39–47. [PubMed] [Google Scholar]
- 29. Freedman BA, Potter BK, Dinauer PA. et al. Prognostic value of magnetic resonance arthrography for Czerny stage II and III acetabular labral tears. Arthroscopy 2006; 22: 742–7. [DOI] [PubMed] [Google Scholar]
- 30. Czerny C, Hofmann S, Urban M. et al. MR arthrography of the adult acetabular capsular-labral complex: correlation with surgery and anatomy. AJR Am J Roentgenol 1999; 173: 345–9. [DOI] [PubMed] [Google Scholar]
- 31. Troelsen A, Elmengaard B, Soballe K.. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am 2009; 91: 2169–79. [DOI] [PubMed] [Google Scholar]
- 32. Heerey JJ, Kemp JL, Mosler AB. et al. What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. Br J Sports Med 2018; 52: 581–93. [DOI] [PubMed] [Google Scholar]
- 33. Jacobsen JS, Bolvig L, Holmich P.. Muscle-tendon-related abnormalities detected by ultrasonography are common in symptomatic hip dysplasia. Arch Orthop Trauma Surg 2018; 138: 1059–67. [DOI] [PubMed] [Google Scholar]
- 34. Klaue K, Durnin CW, Ganz R.. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 1991; 73: 423–9. [DOI] [PubMed] [Google Scholar]
- 35. Garabekyan T, Ashwell Z, Chadayammuri V. et al. Lateral acetabular coverage predicts the size of the hip labrum. Am J Sports Med 2016; 44: 1582–9. [DOI] [PubMed] [Google Scholar]
- 36. Domb BG, Chaharbakhshi EO, Perets I. et al. Hip arthroscopic surgery with labral preservation and capsular plication in patients with borderline hip dysplasia: minimum 5-year patient-reported outcomes. Am J Sports Med 2018; 46: 305–13. [DOI] [PubMed] [Google Scholar]
- 37. Liechti EF, Ferguson SJ, Tannast M.. Protrusio acetabuli: joint loading with severe pincer impingement and its theoretical implications for surgical therapy. J Orthop Res 2015; 33: 106–13. [DOI] [PubMed] [Google Scholar]
- 38. Henak CR, Abraham CL, Anderson AE. et al. Patient-specific analysis of cartilage and labrum mechanics in human hips with acetabular dysplasia. Osteoarthritis Cartilage 2014; 22: 210–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hatakeyama A, Utsunomiya H, Nishikino S. et al. Predictors of poor clinical outcome after arthroscopic labral preservation, capsular plication, and cam osteoplasty in the setting of borderline hip dysplasia. Am J Sports Med 2018; 46: 135–43. [DOI] [PubMed] [Google Scholar]
- 40. Yeung M, Kowalczuk M, Simunovic N. et al. Hip arthroscopy in the setting of hip dysplasia: a systematic review. Bone Joint Res 2016; 5: 225–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Kirsch JM, Khan M, Bedi A.. Does hip arthroscopy have a role in the treatment of developmental hip dysplasia? J Arthroplasty 2017; 32: S28–31. [DOI] [PubMed] [Google Scholar]
- 42. Parvizi J, Bican O, Bender B. et al. Arthroscopy for labral tears in patients with developmental dysplasia of the hip: a cautionary note. J Arthroplasty 2009; 24: 110–3. [DOI] [PubMed] [Google Scholar]
- 43. Tannast M, Zheng G, Anderegg C. et al. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res 2005; 438: 182–90. [DOI] [PubMed] [Google Scholar]
- 44. Siebenrock KA, Kalbermatten DF, Ganz R.. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 2003; 407: 241–8. [DOI] [PubMed] [Google Scholar]


