Abstract
Background:
Many people with type 1 diabetes (T1D) do not achieve levels of exercise recommended by the American Diabetes Association, often due to unique barriers, including fear of hypoglycemia. This study aimed to broaden the understanding of barriers and facilitators to exercise among adults with T1D by exploring social media—specifically T1D-themed blogs—in addition to more traditional interviews and journals.
Methods:
Data sources included exercise-focused T1D blog posts (n = 67) and associated comments (n = 717), as well as interviews of and journals kept by adults with T1D (n = 10). Data were analyzed using a qualitative inductive thematic approach. Shared and unique themes were identified among the three data sources. Content mapping illustrates these relationships and interplay.
Results:
Three metathemes were identified: (1) exercise with T1D requires significant planning, (2) hypoglycemia often interrupts or causes alteration to exercise, and (3) “ordinary” activities can cause greater insulin sensitivity and hypoglycemia, much like planned exercise, but are often unrecognized as exercise. Unique themes found only in the blogs, only in interviews, or only in journals are also reported.
Conclusions:
Social media such as blogs can be a valuable addition to qualitative research, especially when combined with other sources of data. This study suggests a need for providing adults with T1D with more instruction on preventing hypoglycemia during exercise, as well as links to organized or online activities that can provide support and education. Health care providers may wish to consider strategies to help adults with T1D recognize glycemic impact from daily activities not typically recognized as exercise.
Keywords: blogs, exercise, self-management, social media, type 1 diabetes
Physical activity contributes to overall health and mental wellbeing in all adults,1 and for adults with type 1 diabetes (T1D) there are crucial incremental benefits compared to individuals without diabetes, such as decreased cardiovascular disease and mortality.2 The American Diabetes Association (ADA) recommends that adults with diabetes perform at least 150 minutes of moderate-to-vigorous activity and 2-3 sessions of resistance training per week, with no more than two consecutive days without exercise.3 A recent consensus statement provides recommendations including glucose targets, nutrition, and insulin adjustments in exercise management.4 Despite these recommendations and guidelines, most adults with T1D—like most adults in general—do not get the recommended amount of exercise.5-7 While there are multiple barriers to exercise in the general population (eg, lack of time and/or motivation, limited access to facilities, inclement weather, and unsafe neighborhoods),8-10 specific additional barriers exist for adults with T1D, such as fear of hypoglycemia.11-16
Qualitative research is “intended to generate knowledge grounded in human experience”17 and is an important methodology to better understand the barriers and facilitators that adults with T1D experience while attempting to exercise. Previous studies on barriers to exercise for people with T1D have employed traditional qualitative methods such as questionnaires with open-ended responses, focus groups, and interviews.14,15
Social media is a growing platform for conducting research,18-22 including for the study of diabetes. There is a vast and vibrant Diabetes Online Community (DOC)—a term widely used to encompass the people and their various online activities related to living with diabetes.23 Blogs (online journals usually maintained by one person, whereby people can leave comments to start meaningful conversations) are one part of the DOC that can represent a breadth of people living with T1D and that can help broaden understanding and identify barriers and facilitators to exercise in T1D that may not have been found previously. Blogs allow people to share their thoughts and experiences when and where they choose, unconstrained by time, geographic proximity to other participants, or a research environment. They allow for anonymous participation, if desired, and enable asynchronous interaction between bloggers, commenters, and noncommenting blog readers. This study adds to the growing literature on barriers and facilitators to exercise in adults with T1D by combining blogs with traditional qualitative data sources, thereby seeking to broaden understanding further. Such a complementary array of data sources allows representation from a broader population, through more diverse means of expression, thereby mitigating the limitations of each unique type of data source. To our knowledge, there have been no prior studies analyzing blogs to further explore challenges and successes in exercising with T1D.
Methods
This study was approved by the Penn State College of Medicine Institutional Review Board. Informed consent was obtained from all participants prior to participation. Three different types of data were utilized: blogs, individual interviews, and handwritten journals.
Data Sources, Participants, and Data Collection
Blogs
Blogs were selected through a combination of previous work analyzing the DOC23 and snowball sampling24 with a focus on well-known, sustained blogs with high volumes of usage. Snowball sampling began with the most visited and visible T1D blog, Six Until Me (www.sixuntilme.com), which serves as a gateway to other blogs. This yielded a group of four online blogs written by adults with T1D that also had available on them content tags for “exercise” and/or “fitness,” or whose blog owner was willing to add such tags. Based on viewable data from the blogs themselves (eg, pageview counters) and analytics supplied by the bloggers, the included blog sites were viewed approximately 90,000 times per month by 45,000 unique individuals. Blog authors were contacted via email, and each provided permission to retrospectively analyze the posts and comments on their blogs. All included data were publicly available online; all blogs could be found by internet search engine, did not require invitation, permission, or password to access content, and could therefore be viewed and have comments added by anyone with internet access via standard web browsers.
Interviews and Journals
To obtain interview and journal data, ten people with T1D between the ages of 18 and 65 years were recruited from the Penn State Hershey clinical population. A large age range was selected to include barriers and facilitators to exercise across a broad age distribution. To understand exercise barriers especially, those who did not meet current ADA recommendations for exercise3 were sought.
Data were collected via qualitative interviews conducted by two authors (TKO and GW) based on a topic guide that addressed exercise barriers that participants faced while trying to exercise, factors that made it easier to exercise, and the sources from which participants obtained information on exercising with diabetes. To study the experience of exercise in a longitudinal manner, participants completed three individual 30-minute interviews—one at baseline, after week 1, and after week 2—totaling 90 minutes for each of the ten participants.
To capture “real-time” thoughts and reduce the influence of recall bias relating to exercise in this population, journals were also mailed to participants prior to the study, with instructions to write in the journal any time they thought about exercise or participated in exercise, and how T1D affected their exercise experience during the 2-week study period.
Data Analysis
All qualitative data sources (blog posts including associated comments, interview transcripts, and exercise journals) were imported into qualitative data analysis management software (NVivo, QSR International; Burlington, MA). The study team employed an inductive thematic approach25-28 to construct themes represented in the data. Blog data were analyzed separately from interview and journal data to allow comparison of themes derived from each method, and especially from the traditional sources (interviews and journals), to the more novel approach of utilizing blogs. Primary coders (TKO, SMO) reviewed the data and noted initial impressions. For each of the three data source types, a preliminary codebook was created and revised through ongoing discussions among the study team, establishing a basis for coding procedures by all. After coding 10% of the datasets, Cohen’s kappa was calculated as one method to assess intercoder reliability; Cohen’s kappa is a measure that incorporates how frequently multiple coders agree that a given code applies to a segment of data and how frequently they agree that a given code does not apply to a segment of data.29 Kappa was calculated for each dataset and found to be high (0.911-0.958). With intercoder reliability established, the remainder of the datasets were coded, proceeding until saturation was established (when the primary coders determined that no new codes or themes were being uncovered, subsequently corroborated by the full study team). Undertaking an inductive approach to determine emergent themes, the team performed a detailed review of coded content to identify frequently utilized codes as well as pairs of codes frequently appearing together to construct themes occurring within the datasets. As themes were determined separately for each type of data source, any metatheme reported as existing in all data source types must have been present independently as a theme in each of those source types. In other words, a metatheme reported as existing across all source types must have been independently identifiable as a theme within the blog data, within the interview data, and within the journal data. Likewise, a theme from the blog data which was supported by only one or two comments in the interviews and the journals would not satisfy this criterion to be a metatheme.
Results
Data Sources and Participants
Table 1 summarizes characteristics of the study population. Sixty-seven blog posts and 717 associated comments were analyzed. Ten participants engaged in three 30-minute interviews each (totaling thirty 30-minute interviews) and provided 100 journal entries (mean 10.0, range 2-17, SD 5.75) over a 14-day period. Interview and journal participants ranged in age from 19-63 years (mean 36.9, SD 17.8). Average age at T1D diagnosis was 17.5 years (range 7-39). Participants were predominantly female (70%), with 50% using an insulin pump and 40% using a continuous glucose monitor (CGM) system. This information was not available for bloggers or commenters.
Table 1.
Characteristics of the Study Population.
| Blog and blogger characteristics | ||
|---|---|---|
| Blogger demographics | Female gender, n (%) | 3 (75) |
| Age in years, mean (SD), range | 39.5 (5.4), 35-47 | |
| Age at diagnosis, mean (SD), range | 7.3 (2.6), 5-11 | |
| Years blogging, mean (SD), range | 8.3 (2.8), 5-11 | |
| Blog characteristics | Exercise-related blog posts, n | 67 |
| Comments on blog posts, n (mean), range | 717 (10.7), 1-94 | |
| Interview, journal participant characteristics | ||
| Participant demographics | Female gender, n (%) | 7 (70) |
| Age in years, mean (SD), range | 36.9 (17.8), 19-63 | |
| Age at diagnosis, mean (SD), range | 17.5 (9.1), 7-39 | |
| Diabetes-related data | Insulin pump usage, n (%) | 5 (50) |
| CGM usage, n (%) | 4 (40) | |
| Self-reported A1c, n (%) | ||
| 6.0-6.4 | 1 (10) | |
| 6.5-6.9 | 2 (20) | |
| 7.0-7.4 | 2 (20) | |
| 7.5-7.9 | 0 (0) | |
| 8.0-8.4 | 1 (10) | |
| 8.5-8.9 | 0 (0) | |
| 9.0+ | 4 (40) | |
Data Analysis
Thematic analysis revealed metathemes shared across blogs, interviews, and journals, as well as themes unique to each data source type. Even where similar topics were discussed (ie, content coded to the same topic area), the nuanced meanings captured in the themes sometimes differed by data type. The metathemes and themes by data type are summarized in Table 2 and fully presented with representative quotes in Table 3.
Table 2.
Overview of Metathemes and Themes by Type of Data Source.
| Metathemes shared across blogs, interviews, and journals | ||
|---|---|---|
| • T1D requires significant planning for exercise | ||
| • Hypoglycemia often interrupts or alters exercise | ||
| • Unrecognized exercise can result in hypoglycemia and/or greater insulin sensitivity | ||
| Themes unique to one type of data source | ||
| Blogs | Interviews | Journals |
| • Bringing diabetes supplies to exercise is a significant burden, but family can help by sharing the burden • Organized, group exercise activities are beneficial • Online peer support is encouraging; it facilitates and motivates exercise |
• Being outdoors and/or being with family facilitates exercise • Exercise barriers that are unrelated to diabetes are the greatest barriers • Exercise is understood to be essential, but there is little to no guidance from health care providers about how to exercise |
• Family and friends exercising together builds relationships and shared experiences • Adults with T1D routinely exercise without realizing it, through daily activities unrecognized as exercise • Glucose management during exercise is different and is learned by experience, not by instruction or guideline • Journaling is useful |
Table 3.
Metathemes and Themes With Representative Quotes.
| Metathemes shared across all data source types | |
|---|---|
| 1. Adults with T1D described the significant burden of planning for exercise | “I’d like to go but it takes me a good 10 or 15 minutes to do all the things that I need to do to get ready for a hike.” “And then depending on what time I’d get home from work it was time to eat dinner and I didn’t really want to go later after dinner because it’s not easy to exercise after you eat. And with the way my diabetes is I have to plan and turn my insulin pump a little bit and make sure my blood sugar’s okay before I go. And on any given day my blood sugar’s not the same.” “A lot of it is preparing for if you are doing an intense workout to load with carbs before you do anything like that.” “It’s always in the back of your mind. You’re always thinking about ‘What’s my blood sugar?’ or ‘How long am I gonna be gone for? What do I need to prepare for? What do I need to bring along?’” “It isn’t that it takes long, it’s just a lot to do. To try and think about how long I am going to be gone today, and how much I should eat before I leave. It’s the planning and everything.” “Trying to figure out how much I should eat and how much insulin to take kills my drive to exercise.” |
| 2. Hypoglycemia is a common barrier that causes interruption and/or cessation of workouts among adults with T1D; there is a need to check glucose levels “constantly” during workouts and plan exercise accordingly | “We’ve had to take breaks when we’re out hiking because I’ve had a low and I need to sit for a while and treat. So that’s something that’s always there and present.” “I’m not a bike rider but I knew that my legs shouldn’t have been as wobbly as they were. I was jittery and sweating madly, even though we’d been on the road for literally minutes: ‘I need to stop for a minute and have some more Gatorade.’” “But throughout the entire time I was at the gym it’s something that’s always in the back of your mind.” “And I guess that could be fear, like I don’t enjoy exercising if I know that I’m going to go low the whole time. I don’t know if that’s necessarily fear or more that I don’t want to have to deal with it.” |
| 3. Hypoglycemia and increased insulin sensitivity can occur with day-to-day activities that are not recognized or prepared for as exercise | “Like at the mall the other day (I should KNOW by now to do a temporary basal rate while shopping!) I was finding a spot to sit on the floor maybe just 2 minutes after saying, ‘Hmm, I don’t feel good’ and the CGM said 94. Then the very next reading it alarmed at 66.” “For the past couple of weeks I’ve been working hard on redoing our dining room. After some intense physical labor, it’s about 93% done and looking fantastic. But combine that extra activity with a monthly hormonal swing and a cold / flu thing that hit yesterday? Hello, epic lows.” “It’s finally above 30 degrees and I’m burning off buckets o’ carbs mulching and weeding the garden!” |
| Themes unique to blogs | |
| 1. Wearing and carrying diabetes technology and supplies is a burden, but the burden can be reduced when family helps | “I love when [my husband] and I run together because I totally strap all my diabetes crap to him and use him as a pack mule too. He’s younger than me anyway, so he should definitely carry all my stuff.” “The miles might be logged a little slower than when I’m by myself, but there’s nothing more convenient than making use of her bike basket to carry all my diabetes stuff, and I love sharing some outside play moments with my daughter.” “When I started the ride, I was at 168 mg/dL, which was high enough for me to feel comfortable exercising, but not so high that I felt like I was wearing lead boots. My daughter sat in the trailer with my backpack, with the CGM receiver sitting in the front zipper pocket.” |
| 2. Attending organized group exercise programs for adults with T1D facilitates exercise, while also providing peer support and diabetes education; these organized programs provide opportunities for adults with T1D to exercise with others who have T1D in a supervised environment | “But core to the camp (and the campers/athletes) is the education regarding the intricate physiology of the insulin, carbs, and exercise triangle. To eat, or not to eat? To bolus, or not to bolus? To train today, or not to train today? These and all the thousands of questions we ask ourselves 24×7 are explored, tested in training, and practiced at diabetes training camp in what quickly evolves into a tight-knit and supportive group of people with a common purpose – to develop to the next level.” “There are so many benefits to having friends around that can empathize and share their own feelings with you in return. The personal growth, through networking/coping like this, is infinitely more valuable than something you could buy.” “It is the place where I can totally relax where having diabetes is both the focus and the very last thing you are thinking about. It is a second home, no matter where the geographical location. It brings together a community that somehow becomes instantly tight-knit, caring and supportive, a community that understands all of those ‘little things’ that can really get to you as a type 1.” “There is always a funny thing that happens that weekend: diabetes feels easier when you’re dealing with it in the group.” |
| 3. Online peer support serves as a source of encouragement to exercise for adults with T1D | “I am crazy proud of you!!!!!!” “Glad you were able to crush the lows and rock the ride, it looks beautiful.” “Good for you, getting time in for exercise when you’re a mom with type 1.” “Congratulations on finishing your first race.” “This is the stuff that inspiration and motivation is made of. I think you’re doing a great job and you certainly don’t need to be so hard on yourself. Becoming an athlete is hard work for almost everybody. :) I’m so happy for your 12-week journey!” “Do NOT beat yourself up if you’re unable to meet a particular goal—in the case you mentioned here, running all segments of your workout. I’ve been doing endurance athletics for years, and still have problems with this sometimes!” “Very inspiring post! Well done on such an amazing achievement. I have just got into cycling recently and have not yet discovered exactly what it does to my blood glucose levels, every ride differs at the moment! After reading this I will definitely keep on going, only hope that one day I have the drive to manage what you have!” |
| Themes unique to interviews | |
| 1. Although adults with T1D face barriers to exercise unique to diabetes (eg, specific preparation needed before exercise), their greater barriers are shared by the general public, including comorbidities (especially mental health), being unmotivated, and lacking time | “That’s happened a couple times but I consider it more of a kind of depression sort of overall just the way of how I felt rather than diabetes-specific.” “And I’d say just it’s really my own psychology that is the big barrier to my exercising.” “I guess time. I just don’t have any time. Really the lack of energy and motivation is the big thing with me. It’s like I just don’t have any a lot; any motivation to do anything. It’s kind of hard sometimes.” “Well I just feel that physical exercise is a waste of time.” “If I don’t get up in the morning and I don’t do something and get it in. As the day goes on it’s harder to like fit it in.” “If I’m just not in the mood to exercise I won’t. But I feel like they’re all things that are normal and have nothing to do with diabetes.” |
| 2. Doing family activities outdoors is a facilitator | “I enjoy going out in the woods and hiking in particular the place that we’ve been going lately. I would rather go with [my husband], and our dog, and my daughter, than go out alone.” “My husband and I, and our daughters and our dog go out and we do that all together.” “And my daughter has been asking about going bike riding so she’s been motivating me.” |
| 3. While often told that exercise is essential, adults with T1D report receiving strikingly little guidance regarding how to exercise, including how to begin an exercise program or exercise safely with T1D | In response to interviewer asking “Have you gotten information about exercise from your endocrinologist or any physician?” 8 of 10 participants stated that they had not. Additional illustrative quotes follow: “I think when I was diagnosed, it was like 1992 or 1993. I remember talking about what’s going to happen when you go to gym class and you’re feeling shaky, but no—not in my adult life.” “It was just something they never mentioned or touched upon during normal appointments. It’s more ‘How are you?’ and ‘Let’s look at your bloodwork.’” “It’s never a topic of conversation, at least in my experience.” “Not within the last 10 years probably that anybody said anything about exercise.” “She keeps encouraging me to do exercise. We didn’t really have any further discussions.” “I don’t know a lot of providers who have a lot of valuable information. I think that sometimes it’s more effective when it comes from somebody who’s dealing with it themselves.” |
| Themes unique to journals | |
| 1. Family and friends provide motivation to exercise | “My daughter asked me about going for more bike rides soon. So this conversation has inspired me to do more bike riding with her to strengthen our mother-daughter relationship as well as exercise together.” “Wasn’t going to exercise, but my mom wanted to go so we went together.” “My husband and friends have been my motivators.” |
| 2. Despite not identifying themselves as “exercisers” most participants did exercise nearly every day through “ordinary” activities | “Thinking of walking later today. Spent 4+ hours in yard gardening-using shovel and digging fork- squatting and bending. Blood sugar then low so no walk today.” “I did not think about exercise . . . but shoveled snow as part of my job.” “I did not exercise . . . I did clean my house and washed the windows and it took most of the day.” |
| 3. Usefulness of journaling | “This study helps me be very aware of my diabetes thought process.” “I think I wrote that in the little journal. I wrote ‘Oh my God I need to get out there and do something.’ I haven’t actively moved in like 4 days.” “And I’d write what I should have exercised today. But because I’m writing in the book at 9 o’clock at night, I’m like I should have did this today.” “I can’t really tell you what but I guess I learned more about being diabetic and trying to be more aware of exercising and things like that.” |
| 4. Adults with T1D often manage blood sugars during exercise through learning that has occurred through life experiences rather than following guidelines or HCP directions, and often do not test prior to or during exercise | “How’s my BS [blood sugar]? Should I check it? Nah—I’m fine and it’s a short walk.” “Drank a juice box as we walked. Felt a little sluggish, but didn’t test though. Felt lazy for not having tested.” “My sugar remained high [after exercise] which created some issues regarding whether I would take insulin or let myself come down naturally into range which is what usually happens when I am active.” “I tend to have the bad habit of not taking insulin before exercise to prevent lows. But then all the negative effects of high blood sugar are draining on your energy and mood.” |
Analysis resulted in three metathemes present across all data source types: (1) adults with T1D feel that exercise requires significant planning, (2) hypoglycemia often interrupts exercise, or causes adults with T1D to have to alter their planned exercise, and (3) “ordinary” activities can cause greater insulin sensitivity and hypoglycemia, similar to planned exercise. These are discussed in greater detail below.
Adults With T1D Feel That Exercise Requires Significant Planning
In all three data sources, people describe the amount of planning that they must perform to feel that they can exercise, and how this can be a deterrent to exercising: “It’s always in the back of your mind. You’re always thinking about ‘what’s my blood sugar?’ or ‘How long am I gonna be gone for? What do I need to prepare for? What do I need to bring along?’” Participants identified that it is not the time needed to plan, but the emotional burden of having to plan: “It isn’t that it takes long, it’s just a lot to do. To try and think about how long I am going to be gone today, and how much I should eat before I leave. It’s the planning and everything.” As one participant succinctly summarized when discussing the emotional burden of preparation needed to exercise: “Trying to figure out how much I should eat and how much insulin to take kills my drive to exercise.”
Hypoglycemia Often Interrupts Exercise or Causes Adults With T1D to Have to Alter Their Planned Exercise
Through the incorporation of blogs, interviews, and journals, we found that participants did not describe fear of hypoglycemia as much as the burden of having exercise interrupted or changed due to hypoglycemia: “I had to not work out as hard as I wanted, to keep my blood sugar from dropping below 80 before class was over. It was very frustrating and agitating that I couldn’t do the workout I wanted because of my diabetes.” Even when asked directly about fear of hypoglycemia, one participant responded: “I don’t know if that’s necessarily fear or more that I don’t want to have to deal with it.” They described the impact of hypoglycemia on family activities (“We’ve had to take breaks when we’re out hiking because I’ve had a low and I need to sit for a while and treat. So that’s something that’s always there and present”), as well as the burden of constantly having to think about the possibility of low blood glucose (“Throughout the entire time I was at the gym it’s something that’s always in the back of your mind”).
“Ordinary” Activities Can Cause Greater Insulin Sensitivity and Hypoglycemia, Similar to Planned Exercise
This analysis of three data sources demonstrated that although adults with T1D may not exercise on a regular basis, they are often physically active: “I did not exercise—I did clean my house and wash windows (it took me most of the day).” Such activities unrecognized as “exercise” were also associated with unexpected hypoglycemia: “Like at the mall the other day (I should KNOW by now to do a temporary basal rate while shopping!) I was finding a spot to sit on the floor maybe just 2 minutes after saying, ‘Hmm, I don’t feel good’ and the CGM said 94. Then the very next reading it alarmed at 66.” At times, planned exercise was prevented by hypoglycemia resulting from other physical activity not recognized as exercise: “Thinking of walking later today. Spent 4+ hours in yard gardening—using shovel and digging fork—squatting and bending. Blood sugar then low so no walk today.”
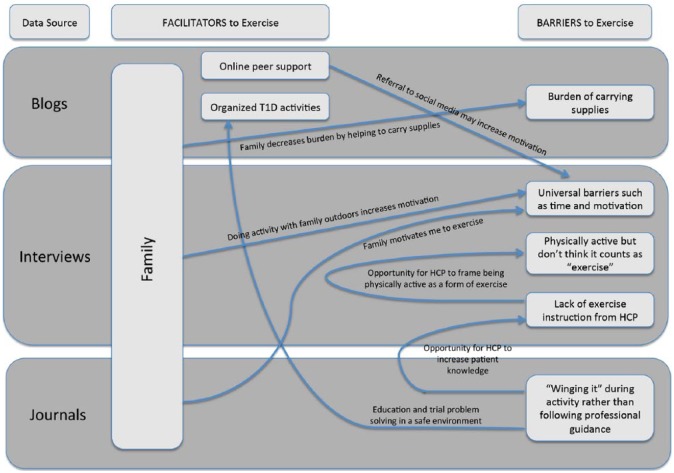
In addition to metathemes, each data source identified unique themes that were often interrelated, as demonstrated in Figure 1. For instance, family was identified as a facilitator to exercise among blogs, interviews, and journals, but the more specific way in which family was helpful differed among the sources: blogs identified family as helping to decrease the burden of carrying diabetes supplies during exercise; interviews identified family as facilitators through exercising together outside; and journals identified family as motivating to exercise. In addition, facilitators identified through one data source presented opportunities to decrease barriers identified by another source. For instance, interviews and journals respectively identified potential barriers in lack of exercise information from health care providers (HCPs) and “winging it” (improvising, making decisions and adjustments based on experience, intuition, trial, and error) with diabetes management during exercise, yet blogs identified a facilitator in organized T1D activities as a possible avenue to obtain education and practice problem solving in a safe environment.
Figure 1.
Concept map of themes relating to barriers and facilitators to exercise with type 1 diabetes, by data source.
Discussion
This qualitative study uses the addition of social media through the inclusion of blogs to supplement traditional methods such as interviews and journals. Through combining three sources of data, themes identified in this research add to the growing body of literature on barriers and facilitators to exercise in adults with T1D. Clear guidelines now exist for exercise management, including glucose targets, nutritional, and insulin dose adjustments to help prevent exercise-related glucose excursions.4 Yet many adults with T1D do not meet the ADA’s recommendations for exercise.3 This study agrees with others that hypoglycemia is a major barrier to exercise, yet unlike in our previous work involving caregivers to children with T1D22 and others who cite fear of hypoglycemia as a barrier,4,11,12 participants in this study seemed to be more burdened by the effect of low blood glucose on their ability to complete their exercise as planned. We agree with Campbell et al30 that many adults with T1D are active through daily living and recreational activities even though HCPs and adults with T1D alike may not identify this as exercise, and therefore unexpected hypoglycemia can occur. Like Kime et al,14 we found that adults were often “winging it” when exercising with T1D, with little to no guidance from HCPs. Family was found to be an important facilitator across all three data sources and helped not only to decrease burdens associated with diabetes (eg, carrying equipment while exercising), but also helped by participating in exercise together, as well as motivating adults with T1D to exercise. Consistent with prior studies,11,12 this study found that adults with T1D feel safer and more comfortable exercising when they are with a group of others who also have T1D, noting a sense of shared experience and knowledge that only comes from living with T1D.
This work supports the development of a model applying social and behavioral modification problem solving strategies31-33 to the barriers adults with T1D face in relation to exercise. HCPs can help increase adult with T1D preparedness and engagement in exercise through the steps of general orientation, problem definition and formulation, generation of alternatives, decision making, and verification.31-33 HCPs and adults with T1D share a mutual role in identifying and validating that there are issues related to exercise (general orientation). HCPs can then aid in identifying individualized problems facing the adult with T1D in relation to exercise engagement (problem definition and formulation), for example, becoming hypoglycemic on a family bike ride. Next, HCPs can help the adult with T1D brainstorm ways to be prepared for managing hypoglycemic events (generation of alternatives) and then help them examine several of the alternatives to identify which may be most effective and realistic (decision making). HCPs with ongoing patient relationships are perfectly poised to check in at follow-up visits, assess effectiveness of the strategies (verification), and negotiate how best to modify them for the future. Through problem solving, HCPs can better prepare adults with T1D for exercise by using their expertise to share a variety of response alternatives for dealing with potential problematic situations31 (eg, a handout listing specific foods and quantities to promptly treat hypoglycemia, a list of available online T1D social networking groups to learn from others’ experiences, or education about insulin dose adjustment), and thereby increase the likelihood that adults with T1D will select the most personally effective responses from among these alternatives.31 Implementing this model could increase activity in those who are inactive and reinforce persistence in those already exercising—a potential area for future research.
To our knowledge this is the first social media study to use blog analysis specifically to conduct a qualitative analysis of exercise habits among adults with T1D. Blog content is publicly available and freely shared and is not constrained by interview scripts, questionnaires, or other traditional methods of data collection. Bloggers and commenters are unaffected by researcher bias, as their content is not based on what they believe a researcher wants to know or hear. Nor are they asked to think back retrospectively, and somewhat artificially, to previous experiences. Instead, blogs provide a near real-time glimpse into the attitudes and emotions around a specific topic. In the blogs analyzed in this study, bloggers wrote about same-day or recent experiences they had while being physically active, and commenters responded as they read the blog posts. Since blogs are public and meant to be shared, perhaps this helps explain why some of the themes found in the blog analysis are more group-oriented, including the helpfulness of organized exercise activities, diabetes camps, and—especially online—peer support.
This study also revealed that blogs themselves provide support and encouragement for adults with T1D to be physically active. One reason people with T1D turn to the DOC is to receive much-needed peer support that is traditionally missing from their diabetes care.23,34-35 With this information, HCPs can encourage adults with T1D to find a T1D-dedicated exercise group or to join the DOC and read blogs. The use of social media, such as blogs, can be an important source of information in research studies such as this, but can also provide HCPs with a lens through which to learn what the daily life of those living with T1D encompasses and thereby to deliver more highly personalized patient-centered care.
Also evident from this work is the advantage to using a combination of source types to form a more complete picture of the issues faced by the target population. Specifically, the findings of metathemes found across blogs, interviews, and journals strengthens the use of each modality as a qualitative data source. And the finding of unique themes from each, whether highly different or whether resembling each other but with important nuance in the differences, highlights the utility of employing multiple modalities to complement each other.
Limitations of this research include a relatively small sample size and lack of generalizability—but these are common limitations in qualitative research.25 We tried to balance the impact of sample size by including the broader array of source types: blogs (including blog posts as well as comments), interviews, and journals. Blogger participants were motivated to publicly share their successes and challenges, and thus may not represent the general population of adults living with T1D. It is also impossible to know many characteristics of the people who contributed to the blog content, such as demographics and insulin pump use or CGM use; this is an inherent limitation of anonymous online sampling and of blogs as a medium. The participants that were interviewed were recruited from one hospital system and their views may not represent those of the broader adult T1D population. However, including both groups should reduce concerns about generalizability compared to including only one or the other.
Future research is needed to develop and evaluate interventions to help adults with T1D overcome the barriers identified in this and earlier studies so that they can achieve the recommended amount of exercise. Such future interventions could target efforts to involve family, peer-led initiatives, and HCP delivery of information not only about the importance of exercise, but also recommendations about how to exercise safely with diabetes, as well as what constitutes exercise (including activities not typically recognized as exercise but which can still result in hypoglycemia).
Conclusions
This study demonstrates that the use of technology in the form of social media (blogs), in addition to interviews and real-time journaling, can provide a fuller understanding of the barriers and facilitators associated with exercising with T1D. This information can contribute to supporting and educating people with T1D by providing them with recommendations for safe exercise practice and preventing hypoglycemia during exercise. These findings also support the need for future research to continue to study this population, as the themes yielded from the qualitative data analysis present various opportunities for improvement in exercise management for adults with T1D.
Footnotes
Abbreviations: ADA, American Diabetes Association; CGM, continuous glucose monitor; DOC, Diabetes Online Community; HCP, health care provider; T1D, type 1 diabetes.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under Award Number DP3DK104054. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
ORCID iDs: Tamara K. Oser  https://orcid.org/0000-0002-0405-3420
https://orcid.org/0000-0002-0405-3420
Sean M. Oser  https://orcid.org/0000-0002-9640-3087
https://orcid.org/0000-0002-9640-3087
References
- 1. Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity—a systematic review of longitudinal studies. BMC Public Health. 2013;13:813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bohn B, Herbst A, Pfeifer M, et al. Impact of physical activity on glycemic control and prevalence of cardiovascular risk factors in adults with type 1 diabetes: a cross-sectional multicenter study of 18,028 patients. Diabetes Care. 2015;38:1536-1543. [DOI] [PubMed] [Google Scholar]
- 3. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065-2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Riddell MC, Gallen IW, Smart CE, et al. Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol. 2017;5:377-390. [DOI] [PubMed] [Google Scholar]
- 5. Makura CB, Nirantharakumar K, Girling AJ, Saravanan P, Narendran P. Effects of physical activity on the development and progression of microvascular complications in type 1 diabetes: retrospective analysis of the DCCT study. BMC Endocr Disord. 2013;13:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McCarthy MM, Funk M, Grey M. Cardiovascular health in adults with type 1 diabetes. Prev Med. 2016;91:138-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hayes C, Kriska A. Role of physical activity in diabetes management and prevention. J Am Diet Assoc. 2008;108(suppl 1):S19-S23. [DOI] [PubMed] [Google Scholar]
- 8. Allender S, Cowburn G, Foster C. Understanding participation in sport and physical activity among children and adults: a review of qualitative studies. Health Educ Res. 2006;21:826-835. [DOI] [PubMed] [Google Scholar]
- 9. Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: a review. Am J Prev Med. 2002;22:188-199. [DOI] [PubMed] [Google Scholar]
- 10. Brownson RC, Kelly CM, Eyler AA, et al. Environmental and policy approaches for promoting physical activity in the United States: a research agenda. J Phys Act Health. 2008;5:488-503. [DOI] [PubMed] [Google Scholar]
- 11. Lascar N, Kennedy A, Hancock B, et al. Attitudes and barriers to exercise in adults with type 1 diabetes (T1DM) and how best to address them: a qualitative study. PLOS ONE. 2014;9:e108019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Brazeau AS, Rabasa-Lhoret R, Strychar I, Mircescu H. Barriers to physical activity among patients with type 1 diabetes. Diabetes Care. 2008;31:2108-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Dube MC, Valois P, Prud’homme D, Weisnagel SJ, Lavoie C. Physical activity barriers in diabetes: development and validation of a new scale. Diabetes Res Clin Pract. 2006;72:20-27. [DOI] [PubMed] [Google Scholar]
- 14. Kime NH, Pringle A, Rivett MJ, Robinson PM. Physical activity and exercise in adults with type 1 diabetes: understanding their needs using a person-centered approach. Health Educ Res. 2018;33:375-388. [DOI] [PubMed] [Google Scholar]
- 15. Kennedy A, Narendran P, Andrews RC, Daley A, Greenfield SM. Attitudes and barriers to exercise in adults with a recent diagnosis of type 1 diabetes: a qualitative study of participants in the Exercise for Type 1 Diabetes (EXTOD) study. BMJ Open. 2018;8:e017813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yardley J, Mollard R, MacIntosh A, et al. Vigorous intensity exercise for glycemic control in patients with type 1 diabetes. Can J Diabetes. 2013;37:427-432. [DOI] [PubMed] [Google Scholar]
- 17. Sandelowski M. Using qualitative research. Qual Health Res. 2004;14:1366-1386. [DOI] [PubMed] [Google Scholar]
- 18. Greene JA, Choudhry NK, Kilabuk E, Shrank WH. Online social networking by patients with diabetes: a qualitative evaluation of communication with Facebook. J Gen Intern Med. 2011;26:287-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Balkhi AM, Reid AM, McNamara JP, Geffken GR. The diabetes online community: the importance of forum use in parents of children with type 1 diabetes. Pediatr Diabetes. 2014;15:408-415. [DOI] [PubMed] [Google Scholar]
- 20. Litchman ML, Lewis D, Kelly LA, Gee PM. Twitter analysis of #OpenAPS DIY artificial pancreas technology use suggests improved A1C and quality of life. J Diabetes Sci Technol. 2018:1932296818795705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. White K, Gebremariam A, Lewis D, et al. Motivations for participation in an online social media community for diabetes. J Diabetes Sci Technol. 2018;12:712-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Oser TK, Oser SM, McGinley EL, Stuckey HL. A novel approach to identifying barriers and facilitators in raising a child with type 1 diabetes: qualitative analysis of caregiver blogs. JMIR Diabetes. 2017;2:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hilliard ME, Sparling KM, Hitchcock J, Oser TK, Hood KK. The emerging diabetes online community. Curr Diabetes Rev. 2015;11:261-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Johnson TP. Snowball Sampling: Introduction. Wiley StatsRef: Statistics Reference Online; 2014. doi: 10.1002/9781118445112.stat05720. [DOI] [Google Scholar]
- 25. Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. Int J Qual Methods. 2017;16:1-13. [Google Scholar]
- 26. Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 27. Creswell JW, Creswell JD. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Thousand Oaks, CA: Sage; 2017. [Google Scholar]
- 28. Fereday J, Muir-Cochrane E. Demonstrating rigor using thematic analysis: a hybrid approach of inductive and deductive coding and theme development. Int J Qual Methods. 2006;5:80-92. [Google Scholar]
- 29. Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37-46. [Google Scholar]
- 30. Campbell MD, Kime N, McKenna J. Exercise and physical activity in patients with type 1 diabetes. Lancet Diabetes Endocrinol. 2017;5:493. [DOI] [PubMed] [Google Scholar]
- 31. D’Zurilla TJ, Goldfried MR. Problem solving and behavior modification. J Abnorm Psychol. 1971;78:107-126. [DOI] [PubMed] [Google Scholar]
- 32. Nezu AM. Problem solving and behavior therapy revisited. Behav Ther. 2004;35:1-33. [Google Scholar]
- 33. Nezu AM, Nezu CM. Problem solving therapy. J Psychother Integr. 2001;11:187-205. [Google Scholar]
- 34. Litchman ML, Rothwell E, Edelman LS. The diabetes online community: older adults supporting self-care through peer health. Patient Educ Couns. 2018;101:518-523. [DOI] [PubMed] [Google Scholar]
- 35. O’Kane AA, Park SY, Mentis H, Blandford A, Chen Y. Turning to peers: integrating understanding of the self, the condition, and others’ experiences in making sense of complex chronic conditions. CSCW. 2016;25:477-501. [DOI] [PMC free article] [PubMed] [Google Scholar]