Abstract
Objective:
Suicidal thoughts and behavior (STBs) have their peak period of onset in adolescence, but little is known about how such behavior is associated with later functioning. The aim of this study is to test whether childhood STBs are related to adult psychiatric, suicidal, and functional outcomes.
Method:
This is a prospective, population-based community study of 1,420 participants assessed with structured interviews up to 7 times in childhood/adolescence (ages 9 to 16; 6,674 observations) for STBs including passive and active ideation, plans and attempts. Participants were then assessed 4 times in young adulthood (ages 19, 21, 24, and 30; 4,556 observations of 1,273 participants) for psychiatric diagnoses, STBs, and functional outcomes.
Results:
By age 16, 7.0% of participants had reported some type of STBs with 3.9% reporting an attempt. Both ideation only and suicide attempts were associated with higher levels of anxiety disorders and STBs in adulthood, as well as poor functioning across financial, health, risky/illegal, and social domains. These observed effects generally were attenuated after adjusting for other psychiatric and psychosocial factors that predict childhood STBs (particularly maltreatment, depression, and disruptive behavior disorders). The exception was adult suicidal behavior, which was predicted by both childhood ideation and attempts, even in the fully adjusted model. Children and adolescents with STBs were more likely to have a disrupted transition to adulthood.
Conclusion:
Childhood STBs are a marker for a multitude of poor psychiatric and functional outcomes in adulthood, but these effects are largely accounted for by other factors. In contrast, childhood STBs are a robust risk factor for adult suicidal thoughts and behavior.
Keywords: Childhood, suicidal behavior, suicide, epidemiology, longitudinal
INTRODUCTION
During one of otherwise healthiest periods of the lifecycle (e.g.,1–3)—childhood/adolescence—suicidal behavior is one of the leading causes of death and disability.4 Suicidal thoughts and behaviors (STBs) have their peak period of onset in adolescence and are commonly associated with psychiatric problems.5,6 Extensive research efforts have been undertaken to identify which adolescents are at risk for STBs, when they are at risk, and how best to intervene.7–10 Although the primary clinical concern of STBs in the short-term is immediate safety, from a public health perspective, adolescents are at the beginning of the lifespan, and these experiences have the potential to be associated with functioning for years and even decades to come. STBs themselves are clearly grave outcomes, but for adolescents, they also have the potential to be associated with risk for further problems during the transition to adulthood and beyond.
Several longitudinal studies have tested associations of childhood STBs with adult functioning, particularly suicidal behavior and psychiatric functioning.11–16 Despite various study differences (e.g., period assessed, assessment measures, length of follow-up, focus on attempts or ideation), a few common findings are noteworthy. The strongest predictions are that childhood STBs are predictive of adult STBs with odds ratios (ORs) indicating a large effect (ORs > 5.0).17 Second, childhood STBs have generally been associated with some type of adult psychiatric problem, either anxiety or mood disorders. However, results for individual studies have been mixed, some supporting associations with later mood but not anxiety disorders,13 or vice versa.14 Associations of childhood STBs with adult substance disorders have been mixed (e.g., positive association,12 negative association11,14). Fewer studies have looked at functional outcomes such as educational attainment, occupational functioning, or adult physical health, but those that have tend to report some significant effects.13,16 Together, these studies suggest early STBs may be associated with increased risk for difficulties in adult functioning.
Nonetheless, it is not always clear whether risk associated with STBs in childhood and adolescence are primarily attributable to the STBs themselves, or to the other factors associated with STBs such as psychiatric functioning (e.g., depression, anxiety), low socioeconomic status (SES), or maltreatment. This is no small consideration given that a number of early experiences are risk factors for early suicidal behavior.7,8,18,19 When such factors are accounted for, many associations of early STBs are attenuated. For example, in the Christchurch Health and Development Study, there were relationships observed between childhood ideation and suicide attempts, and young adult suicidal behavior and psychiatric functioning; however, after adjustment for other risk factors, the only remaining significant associations were with adult suicide attempts and depression.20 This attenuation of significant association is most commonly seen for psychiatric outcomes and less so for adult STBs.11, 16
This study will use a prospective epidemiologic sample to build on the current literature in the following ways. First, we will test associations of prospectively measured STBs with a broad range of adult outcomes including STBs and psychiatric functioning, as well as often understudied functional outcomes. Next, we will look at the effect of both suicidal attempts and ideation to determine whether patterns of risk are specific to different suicidal behaviors, rather than grouping STBs. To clarify mixed findings on independent effects of childhood STBs, we will test whether observed associations are due to childhood STBs or whether the apparent associations are accounted for by child psychiatric functioning and other psychosocial adversities that predict STBs. While there is some evidence that STBs are more common in females,5 we will test whether observed effects are sex specific. Also, we will test whether childhood depression accounts for observed effects of childhood STBs, moderates such effects, or both. Finally, to understand the full public health burden of childhood STBs, it is necessary to account for effects across the lifespan. This study will address this issue by estimating what percent of children with STBs still struggle in some important domain in adulthood and how this compares to children without a history of STBs. This sample has already contributed to the literature on risk factors for childhood suicidal thoughts and behavior by identifying the importance of total symptom load and the specific psychiatric profile of comorbid depression and generalized anxiety disorder.7
METHOD
Participants
The Great Smoky Mountains Study (GSMS) is a longitudinal, representative study of children in 11 predominantly-rural counties of North Carolina (see 21). Three cohorts of children, ages 9, 11, and 13 years, were recruited from a pool of some 12,000 children using a two-stage sampling design, resulting in N = 1,420 participants (49% female; see also 21). The two-stage sampling design involved oversampling of participants at risk for psychopathology. In addition, American Indians, who make up 3% of the area population, were oversampled to constitute 25% of the sample. Of the 1,420 participants, 51.1% were female (unweighted n=630), 6.9% non-Hispanic African-American (n=88), and 3.7% American Indian (n=349). Sampling weights are applied to adjust for differential probability of selection.
Annual assessments were completed on the 1,420 children until age 16. Of 7,910 possible interviews during this period, 6,674 (84.4%) were completed. Participants were then interviewed in young adulthood at ages 19, 21, 25, and 30. Of the 5,626 possible interviews during young adulthood, 4,395 (78.1%) were completed. Across all waves, 81.8% of all possible interviews were completed ranging from 74% - 94% at any particular wave. The maximum possible number of interviews per participant is 8 (oldest cohort), 10 (middle cohort), and 11 (youngest cohort). The median number of interviews to date is 8.
Interviews were completed by a parent figure and the participant to age 18, and by the participant only thereafter, as most participants had left their parent’s home. Before all interviews, parent and child signed informed consent/assent forms. The study protocol and consent forms have been approved by the Duke University Medical Center Institutional Review Board.
Childhood/Adolescent Suicidal Thoughts and Behavior
STBs including passive and active suicidal ideation, suicide plans, and suicide attempts were assessed as part of the depressive disorder module of the Child and Adolescent Psychiatric Assessment (CAPA) until age 16.22 The full operational definition of each suicidal behavior and the CAPA items used to assess construct and prevalence by age 16 are provided in Table 1. The definitions of constructs are consistent with those proposed by the Columbia Classification Algorithm of Suicide Assessment.23 Although assessed, thoughts of death and dying not related to the participant were not included as passive suicidal ideation. A behavior was counted as present if reported by either parent or child or both. To minimize recall bias and forgetting, the timeframe for determining the presence of STBs and related constructs, with the exception of suicide attempts, was the 3 months preceding the interview. Suicide attempts were assessed for lifetime occurrence given the likelihood that they would be remembered more accurately than less severe STBs. In addition to the presence/absence of the behavior, information was collected about the date of onset, duration, and intensity of each behavior. For suicide attempts, information was collected about the methods, intent, and lethality.
Table 1.
Definitions and Prevalence by Age 16 of Different Types of Suicidal Thoughts and Behaviors
| Construct | Definition | CAPA/YAP A Items | % (n) |
|---|---|---|---|
| Passive ideation | Thoughts about wanting to be dead or death. Include thoughts about not being able to go on any longer and life not being worth living. To code, thoughts must be intrusive into at least two activities. | CDC9I01 PDC9I01 |
4.1 (71) |
| Active ideation | Thoughts specifically about killing oneself, by whatever means, with some intention to carry them out. Do not include suicidal plans | CDD0I01 PDD0I01 |
2.5 (42) |
| Suicidal Plans | Suicidal thoughts that contain plans of a suicidal act and some intent to carry them out. If suicidal attempt has been made, determine whether a plan was present prior to the attempt. | CDD1I01 PDD1I01 |
1.2 (17) |
| Suicide Attempt | Episodes of deliberately self-harmful behavior involving some intention to die at the time of the attempt. Rate here, no matter how unlikely the attempt was to cause death, so long as the child's intention was to die. If parent unsure about intention to die, code if the parent can describe a clear self-harmful event. | CDD2E01 PDD2E01 CDD2I01 PDD2I01 |
3.9 (69) |
| Total | 7.0 (116) |
Note: All assessed 4 to 7 times between ages 9 and 16 by structured interview with the child and their parent. All constructs were assessed for the 3 months immediately preceding the interview to maximize recall except suicide attempts, which were assessed for both the 3-month primary period as well as lifetime. CAPA = Child and Adolescent Psychiatric Assessment; YAPA = Young Adult Psychiatric Assessment.
Adult Outcomes
Psychiatric Status and Suicidal Behavior.
All psychiatric and suicidal behavior outcomes were assessed through interviews with the young adults at ages 19, 21, 24–26, and 30 with the Young Adult Psychiatric Assessment. Scoring programs, written in SAS,24 combined information about the date of onset, duration, and intensity of each symptom to create diagnoses according to the DSM-IV.25 Diagnoses made included any DSM-IV anxiety disorder, depressive disorder, alcohol use disorder, and marijuana use disorder. Psychosis and bipolar disorder were not included in analyses as they were very rare in the community. Validity is well-established using multiple indices of construct validity.26 Finally, the same suicidal behaviors assessed in childhood/adolescence were also assessed in adulthood using the same interview items.
Adult Health, Legal, Financial, and Social Outcomes.
Risk scales for each functional domain were derived assessing multiple indicators of functioning. These scales were then standardized across the sample for ease of interpretation. The health scale included items like regular smoking, diagnosis with a physical illness, and obesity status. A full list description of each scale is provided in Supplement 1, available online.
Analytic Strategy
Childhood STBs were assessed in 6,674 interviews with the 1,420 GSMS participants between ages 9 and 16. Sampling weights were applied to adjust for differential probability of selection and to ensure that results represent unbiased estimates for the original population from which the sample was drawn. All reported prevalence estimates were weighted, and all sample sizes were unweighted. In addition, sandwich type variance corrections27 were applied to adjust for the parameter and variance effects induced by the sampling stratification. Weighted regression analyses were completed using PROC GENMOD in SAS 9.2.24 The present analysis aggregated outcomes across adult observations. Models based upon repeated measures of each outcome at 19, 21, 25, and 30 are available upon request from the first author. Finally, adjusted models accounted for demographics (sex, race) as well as other childhood psychosocial (low SES, family dysfunction, family instability, maltreatment) and psychiatric factors (childhood anxiety, depression, disruptive behavior disorders, and substance disorder; for full description see Supplement 1, available online).
RESULTS
Childhood Suicidal Behavior
In GSMS, STBs by age 16 were relatively uncommon, with 7.0% (95% CI, 4.8–9.2) reporting either passive or active ideation, plans, or a suicide attempt (see Table 1). Passive suicidal ideation was most common at 4.1% (95% CI, 2.4–5.8), followed by active ideation at 2.5% (95% CI, 1.3–3.8), and plans at 1.2% (95% CI, 0.2–2.1). Suicide attempts were more common at 3.9% (95%CI, 2.3–5.5), as attempts were assessed for lifetime occurrence, whereas other types of suicide behavior were assessed only in the 3 months immediately prior to the interview to maximize recall. All 1,420 participants completed at least one observation in childhood from ages 9 to 16, and 94.0% (or n=1,334) had 2 or more childhood observations. Having 2 or more childhood observations was associated with higher levels of STBs (p<.01), suggesting that including those with only one observation may be biased. Thus, all subsequent analyses will focus on this group with multiple childhood observations.
Of the 69 participants reporting a suicide attempt, 26 (37.7%) reported an attempted overdose, 8 (11.6%) reported hanging, 31 (44.9%) reported stabbing, 5 (7.3%) reported shooting, 4 (5.8%) reported running into traffic, and 26 (37.7%) reported another method. In terms of actual lethality, 4 (5.8%) reported need for serious medical attention (unconsciousness, blood loss, need for operative intervention), 18 (26.1%) reported moderate physical effects (i.e., need for stitches, stomach lavage), and 41 (or 59.4%) reported no need for medical attention.
For all primary analyses, childhood participants were categorized according to their highest level of reported STBs by age 16: none 93.0% (95% CI, 90.8–95.2), ideation (passive or active) or suicide plans 3.1% (95% CI, 1.6–4.7), and attempts 3.9% (95% CI, 2.3–5.5). Prevalence of different suicidal behavior groups did not differ by sex (despite a slight enrichment of attempts in females) or race/ethnicity (Table S1, available online). STBs were strongly associated with meeting criteria for a depressive disorder in childhood, and also with childhood anxiety, disruptive behavior, and substance disorders. The overlap with depression is of particular interest given that STBs are symptoms of depression. In this sample, only about 58.2% of those reporting mild/moderate suicide behavior and 35.4% of those with a suicide attempt met criteria for childhood depression (i.e., many children with either level of STBs did not meet criteria for a full diagnosis of major depression).
Associations With Young Adult Functioning
Of the 1,334 participants with multiple observations in childhood, 1,281 or 96.0% were assessed in adulthood. Participants with childhood STBs were neither more nor less likely to have an adult observation (p=.39).
Table 2 shows the prevalence estimates and associations between the childhood STB groups and measures of adult psychiatric (anxiety, depression, alcohol use disorder, and cannabis use disorder) and STB status (any adult STBs and adult suicide attempts). Both levels of childhood STB were significantly associated with three adult outcomes: adult anxiety, any adult STBs, and specifically adult suicide attempts. Childhood suicide ideation only was also associated with depression in adulthood and lower levels of both types of substance disorders, whereas suicide attempts were associated with increased risk for meeting criteria for multiple psychiatric disorders in adulthood. There was little evidence that having had a childhood suicide attempt predicted more adult psychiatric problems or suicidal behavior than childhood ideation only.
Table 2.
Differences in Adult Psychiatric Status and Suicide Behavior by Childhood Suicidal Thoughts and Behavior (STBs)
| None (0) | Ideation/ plans (1) | Attempts (2) | Any STBs (1, 2) | 2 vs. 0 | 1 vs. 0 | 1,2 vs. 0 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 79.7 (1304) | 15.5 (47) | 4.8 (69) | 7.0 (116) | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Psychiatric | |||||||||||||
| Depressive | 9.3 (120) | 24.1 (10) | 12.9 (16) | 18.0 | 1.4 | 0.7–3.1 | .34 | 3.1 | 1.0–11.0 | .04 | 2.1 | 0.9–4.9 | .07 |
| Anxiety | 14.2 (160) | 38.3 (16) | 31.5 (23) | 34.6 | 2.8 | 1.1–7.0 | .03 | 3.8 | 1.3–10.8 | .01 | 3.2 | 1.6–6.6 | .002 |
| AUD | 20.2 (218) | 4.1 (6) | 24.1 (15) | 15.0 | 1.3 | 0.5–3.4 | .65 | 0.2 | 0.1–0.5 | <.001 | 0.7 | 0.3–1.6 | .40 |
| CUD | 16.8 (201) | 6.1 (8) | 30.8 (63) | 19.5 | 2.2 | 0.9–5.4 | .08 | 0.3 | 0.1–0.8 | .02 | 1.2 | 0.6–2.5 | .63 |
| Any dx | 40.1 (458) | 43.4 (23) | 55.6 (38) | 50.0 | 1.9 | 0.8–4.5 | .17 | 1.1 | 0.4–3.1 | .79 | 1.5 | 0.8–2.9 | .24 |
| Any 2 disorders | 16.9 (201) | 24.9 (10) | 31.9 (25) | 28.7 | 2.3 | 1.0–5.5 | .05 | 1.6 | 0.5–5.4 | .43 | 2.0 | 1.0–4.1 | .04 |
| Any suicide behavior | 8.1 (110) | 35.0 (16) | 34.8 (29) | 34.9 | 6.1 | 2.5–15.1 | <.001 | 6.1 | 2.1–18.2 | .001 | 6.1 | 2.9–12.8 | <.001 |
| Suicide attempts | 7.2 (98) | 33.3 (13) | 33.2 (27) | 33.2 | 6.4 | 2.6–16.3 | <.001 | 6.5 | 2.1–19.7 | .001 | 6.5 | 3.0–13.8 | <.001 |
Note: Bolded values are significant at the p < .05 level. AUD = alcohol use disorder; CUD = cannabis use disorder; dx = diagnosis.
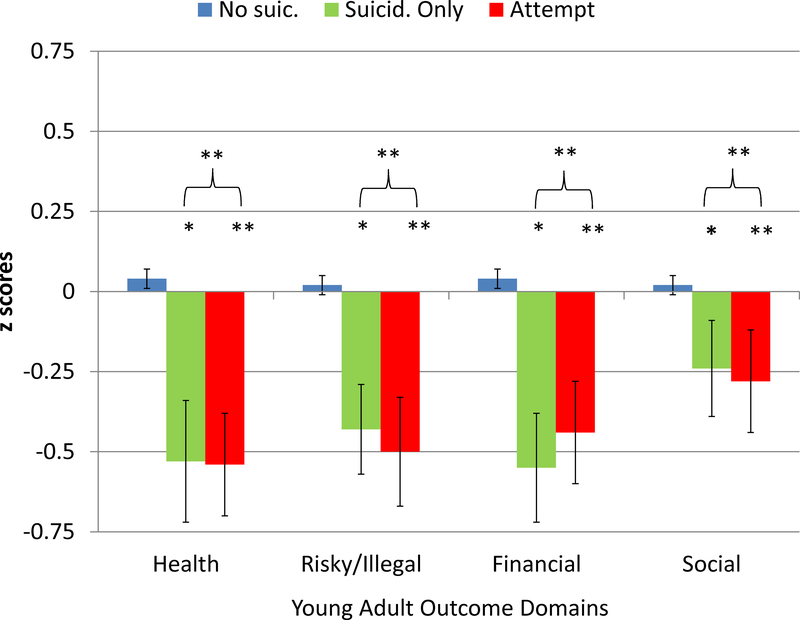
Beyond clinical status, we tested associations between childhood STBs and scales of health, risky behavior, financial/educational, and social functioning. These scales were standardized to allow for comparability (Figure 1). The pattern of findings was similar across all domains: those with any history of childhood STBs had poorer functioning, and there was little difference based on the severity of the STBs. There were no scales where those with a childhood suicide attempt were significantly worse off than those with mild/moderate STBs.
Figure 1.
Associations of childhood suicidal thoughts and behavior (STB) groups with adult functional scales for health, risky behavior, financial/educational, and social functioning. Note: Suicide behavior groups were compared to no childhood suicide behavior group. *p < .05; ** p< .01.
Associations With Young Adult Functioning Adjusted for Childhood Covariates
All models predicting adult psychiatric, suicidal, and functional outcomes were retested accounting for demographics as well as other childhood psychosocial and psychiatric factors associated with childhood suicidality and adult outcomes (see Table 2). All significant associations between childhood STBs and adult psychiatric outcomes were attenuated—both in terms of p values and ORs—in these adjusted models. In contrast, childhood STBs—either ideation only or attempts—predicted adult suicide-related outcomes, and the effects were moderate to large (ORs > 4). Models were rerun for outcomes at ages 19 and 21 (Table S2, available online) and ages 25 and 30 (Table S3, available online) separately. The pattern of findings was the same as when aggregating across all adult observations. Like psychiatric outcomes, all models predicting adult functional outcomes were attenuated after inclusion of covariates (see Table S4, available online).
Moderation by Race/Ethnicity, Sex, and Childhood Depression
All analyses predicting adult psychiatric, suicide, and functional outcomes were rerun, testing whether the pattern of associations varied by sex or race/ethnicity by inclusion of an interaction term. The effect of child STBs on adult STBs was significantly moderated by sex. Figure S1, available online, shows the results for (a) any adult STBs, and (b) adult attempt. In both cases, child STBs was a risk factor for adult suicidal STBs for females but not for males. There was no evidence of moderation by race/ethnicity for any adult outcomes studied.
As noted above, childhood STBs were strongly associated with depression in childhood. At the same time, many individuals reporting either ideation only (41.8%; n=23) or suicide attempts (64.6%; n=34) did not meet criteria for depression in childhood. This degree of overlap allowed us to compare adult outcomes based upon childhood depression status. Analyses for all significant adult outcomes were rerun including childhood depression as a predictor as well as an interaction term between childhood suicide behavior and depression to test for differential prediction. These analyses were run using the 3 childhood STB groups. A significant interaction was detected among childhood depression, childhood ideation/plans only, and adult STBs. Figures S2a and S1b, available online, show the effect of childhood depression status on the association between ideation only and these adult outcomes. In both cases, childhood ideation only was a risk factor for later STBs only when the child also had a history of depression.
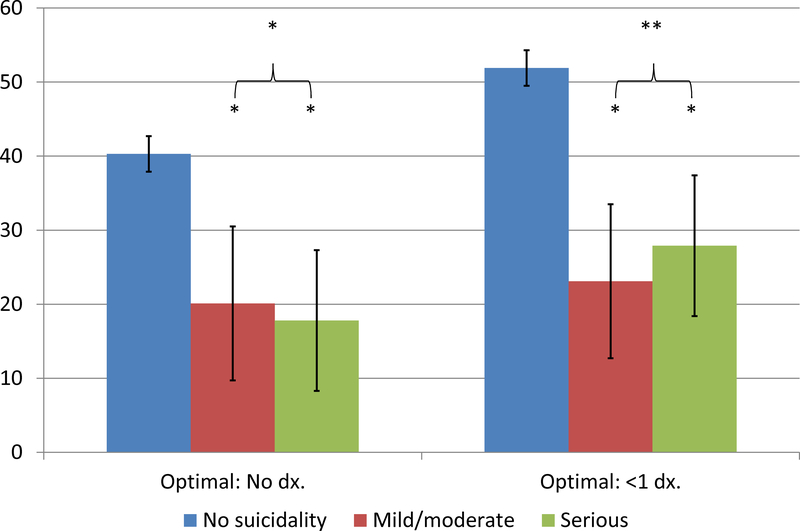
Childhood Suicide Behavior and a Successful Transition to Adulthood
Both levels of childhood STBs were associated with poor psychiatric and functional outcomes even if these associations were accounted for by other factors. This raises the question of just how many participants with childhood suicidal behavior successfully transitioned to adulthood. To estimate this, we derived two definitions of a successful transition to adulthood using the variables studied here: 1) No adult psychiatric disorder, no adult suicide behavior, and top 50% functioning in each functional domain; 2) same definition except 1 or fewer adult psychiatric disorders. Figure 2 shows the prevalence of these outcomes in the childhood suicide behavior groups. For those with no history of suicide behavior, only approximately 40% and 50% met these thresholds, respectively. Both STB groups were significantly less likely to have this successful transition than the no suicide behavior group, and there was no evidence that those with a childhood attempt had less successful transitions to adulthood than those with ideation/plans only.
Figure 2.
Associations of childhood suicidal thoughts and behavior (STB) groups with measures of optimal adult functioning. Note: dx = diagnosis. *p < .05; ** p< .01.
DISCUSSION
Childhood STBs are relatively common, distressing, and associated with significant impairment within childhood.5,11,19,28 This study followed children with STBs into adulthood to look at its associations with long-term functioning. Childhood STBs were associated with higher levels of adult anxiety and STBs as well as poor functioning across financial, health, risky/illegal and social domains. Notably, there was little evidence that children who reported ideation only fared any better than those with a suicide attempt. The predictive effects of childhood STBs seemed to be largely attributable to the other risk factors associated with the STBs. The only exception was adult suicidal behavior where both childhood ideation only and attempts continued to predict increased risk even in the fully adjusted model. Overall, childhood STBs were a strong risk factor for adult STBs and a marker of children who would struggle to make a successful transition to adulthood.
This study contributes to this literature on adult association of childhood STBs by: 1) studying a broad range of adult suicidal, psychiatric, and functional outcomes; 2) following participants for multiple assessments in both childhood and adulthood; 3) assessing a broad range of other childhood psychiatric and psychosocial factors that might account for observed associations including peer victimization; 4) parsing different levels of childhood suicidal behavior; 5) testing moderation of the effect of childhood STBs by childhood depression; and 6) testing whether the cumulative effect of outcomes suggested a compromised transition to adulthood. Our findings are consistent with some aspect of this accumulating literature. In terms of psychiatric outcomes, significant unadjusted associations diminish or attenuate completely after accounting for childhood risk factors for STBs.13–16,18,19 The studies that have accounted for the broadest range of such factors have seen the most attenuation (e.g., 12,16). While there are some exceptions (e.g., 12 for depression), the preponderance of the evidence is too mixed or null for childhood STBs to be considered an independent risk factor for adult psychiatric outcomes. In the case of substance outcomes, the literature has already been mixed or null, and our study suggested little evidence of association of childhood STBs with later DSM alcohol or cannabis disorders. Fewer studies have looked at a broad range of functional outcomes, and there is not enough evidence to support childhood STBs as a risk factor for specific educational or health outcomes. Even if childhood STBs are unlikely to be causal factor in predicting these adult outcomes, it is still a highly salient factor that can be assessed in primary care and school setting and is associated with a broad range of poor adult outcomes. As such, it may still be an efficient marker in risk assessment for broad adult functioning in addition to being an independent risk factor for adult STBs.
Both childhood ideation and attempts had independent association with adult STBs of similar magnitude. There was no evidence that children who reported ideation only fared any better than those with a suicide attempt. Some studies have chosen to focus on ideation11, 14 or attempts,13 but it does not appear that the findings vary systematically in the small group of studies available. Our study also provided an explanation for why a lower level of severity was associated with similar long-term risk. In this study, childhood ideation alone predicted adult STBs, but only when the child had also been diagnosed with depression. One in two children with ideation and depression went on to have adult STBs, whereas only 1 in 10 children with ideation but no depression displayed long-term problems. For clinicians, this supports the importance of assessing a history of both ideation and attempts in completing a risk assessment for adult suicidal behavior, but also suggests that those with ideation only should be assessed for history of depression. Future studies need to attend to the role of sex and depression status as factors that might identify high-risk subgroups.
Finally, previous work has demonstrated a variety of risk pathways to adult STBs. Our analysis suggested a particularly potent pathway for children with ideation or plans that never attempt suicide. For this group, a diagnosis of depression is a significant risk factor for adult STBs and suicide attempts such that 1 in 2 participants with a history of both depression and intent/plans only went on to have adult STBs or a suicide attempt. In contrast, among those with intent/plans only without depression, it was only about 1 in 10 participants that had adult STBs. Two things should be kept in mind when considering this finding. First, childhood depression may have good sensitivity (or true positive rate) when predicting which children with intent or plans only that will go on to have adult STBs, but it also has poor true negative rates or low sensitivity. Second, most individuals with adult suicidality had neither childhood STBs nor childhood depression. Thus while depression may be a good marker of children with intents/plans only that require monitoring, it addresses only a small portion of the total public health burden of adult STBs.
The study leveraged a community-based, representative sample that was recruited prior to the typical onset of suicidal behavior. The participants were then followed prospectively to assess multiple levels of suicidal behavior through childhood and adolescence. Assessments were repeated up to 7 times from ages 9 to 16. Participants were then followed up to 4 times between ages 19 and 30 to assess multiple features of their functioning. Response rates have remained high (>80%) over almost 20 years of study. At the same time, a number of caveats are noteworthy. The current sample is representative of children from the area sampled, which has high levels of childhood poverty and a substantial American Indian population, but it is not nationally representative and may not be generalizable to other populations or samples. Perhaps more importantly, suicidal ideation was only assessed in the 3 months immediately preceding the interview. A shorter assessment window goal can maximize recall and diminish forgetting,29–31 but it is also one reason why our reported rates of ideation for this study are lower than those of other studies that assessed lifetime occurrence of ideation.5,19,20 To the extent that the shorter assessment window might misclassify some children who did experience ideation into the no suicidal behavior group, our reported effects would underestimate the true associations. Finally, analyses attempted to statistically adjust for known independent risk factors of childhood suicidal thoughts and behavior, but not all such risk factors were assessed (e.g., family history of suicide).
Childhood suicide behavior is rightly viewed as a serious, destructive childhood experience that requires immediate attention and treatment. The National Institute of Mental Health has put significant funds toward the development of programs to treat children that have a suicide attempt and to help to avoid further attempts. The attention is often rightfully directed to stabilizing the child, avoiding further ideation or attempts, and ameliorating childhood distress/dysfunction. With the immediacy of these goals, little attention has been paid to how suicide behavior can disrupt the successful transition to adulthood. This study suggests that for many, childhood suicide behavior is a marker for long-term, pervasive problems, problems that have the potential to derail functioning in adulthood for years to come. This work requires retesting in other samples, but it also should initiate work understanding the mechanism by which this childhood experience can disrupt functioning in many areas of functioning years after the suicide behavior. Many children with a history of STBs functioned well in adulthood, and such individuals should be studied to better understand characteristics and processes associated with resilience. Person-centered analyses have the potential to clarify the factors that portend such long-term problems and those that may allow for optimal functioning in the face of this risk.
Supplementary Material
Table 3.
Differences in Adult Psychiatric Status and Suicide Behavior by Childhood Suicidal Thoughts and Behavior (STBs) Adjusted for Childhood Psychiatric Status and Psychosocial Risk Factors
| 2 vs. 0 | 1 vs. 0 | 1,2 vs. 0 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | Sig. Covariates | OR | 95% CI | p | Sig. Covariates | OR | 95% CI | P | Sig. Covariates | |
| Psychiatric | ||||||||||||
| Depressive | 0.6 | 0.3–1.5 | .30 | 1, 2, 7, 10 | 1.6 | 0.4–6.6 | .48 | 1, 2, 7, 10 | 1.0 | 0.4–2.4 | .99 | 1, 2,6, 7, 10 |
| Anxiety | 1.2 | 0.4–3.7 | .73 | 1, 2, 3, 7, 8, 9, 10 | 1.2 | 0.4–3.5 | .81 | 1, 2, 3, 7, 8, 9, 10 | 1.2 | 0.5–2.8 | .70 | 1, 2, 3, 7, 8, 9, 10 |
| AUD | 1.0 | 0.4–2.5 | .96 | 1, 3 | 0.5 | 0.2–1.5 | .24 | 1, 3 | 0.5 | 0.2–1.2 | .12 | 1, 3 |
| CUD | 1.1 | 0.4–3.4 | .87 | 1, 2, 11 | 0.6 | 0.2–1.6 | .30 | 1, 2, 11 | 0.6 | 0.2–1.6 | .31 | 1, 2, 11 |
| Any dx | 0.8 | 0.3–2.3 | .72 | 1, 2, 7, 8, 11 | 0.5 | 0.2–1.2 | .9 | 1, 2, 7, 8, 11 | 0.6 | 0.3–1.3 | .20 | 1, 2, 7, 8, 11 |
| Any 2 disorders | 0.9 | 0.3–2.6 | .87 | 2, 7, 8, 10 | 0.4 | 0.2–1.7 | .23 | 2, 7, 8, 10 | 0.7 | 0.3–1.6 | .40 | 1, 7, 8, 10 |
| Any suicide behavior | 4.4 | 1.8–11.1 | .001 | 4.8 | 1.6–14.1 | .005 | 4.6 | 2.2–9.7 | <.001 | |||
| Suicide attempts | 5.3 | 2.0–13.6 | <.001 | 5.1 | 1.7–15.6 | .004 | 5.2 | 2.4–11.3 | <.001 | |||
Note: Bolded values are significant at the p < .05 level. Covariates include the following: 1 = sex; 2 = race; 3 = low socioeconomic status (SES); 3 = maltreatment; 4 = family instability; 5 = family dysfunction; 6 = peer victimization; 7 = childhood depression; 8 = childhood anxiety; 9 = childhood disruptive behavior disorder; and 10 = childhood substance disorder. AUD = alcohol use disorder; CUD = cannabis use disorder; dx = diagnosis.
Acknowledgments:
The authors would like to thank the participants of the Great Smoky Mountains Study and their families for their longstanding involvement in this study.
Funding: This work was supported by the following NIH grants: DA036523, DA023026, MH104576, DA011301. Dr. Copeland had full access to all the data in the study, performed all statistical analyses, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Disclosures:
Dr. Copeland has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse.
Dr. Goldston has received research support from the National Institute of Mental Health, the National Institute on Alcohol Abuse and Alcoholism, the Department of Defense (via subcontract from the Henry Jackson Foundation), the Substance Abuse and Mental Health Services Administration, and the American Foundation for Suicide Prevention.
Dr. Costello has received research support from the National Institute of Mental Health and the National Institute on Drug Abuse. She is co-author of the following assessment tools: Child and Adolescent Psychiatric Assessment (CAPA), Young Adult Psychiatric Assessment (YAPA), Child and Adolescent Impact Assessment (CAIA), Child and Adolescent Services Assessment (CASA), and Mood and Feelings Questionnaire (MFQ). No personal income is derived from any of these measurements.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Erskine H, Moffitt T, Copeland W, et al. A heavy burden on young minds: the global burden of mental and substance use disorders in children and youth. Psychol Med. 2015;45:1551–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- 3.Harhay MO, King CH. Global burden of disease in young people aged 10–24 years. The Lancet. 2012;379(9810):27–28. [DOI] [PubMed] [Google Scholar]
- 4.Gore FM, Bloem PJN, Patton GC, et al. Global burden of disease in young people aged 10–24 years: a systematic analysis. The Lancet. 2011;377:2093–2102. [DOI] [PubMed] [Google Scholar]
- 5.Nock MK, Green J, Hwang I, et al. Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the national comorbidity survey replication adolescent supplement. JAMA Psychiatry. 2013;70:300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. [DOI] [PubMed] [Google Scholar]
- 7.Foley D, Goldston DB, Costello EJ, Angold A. Proximal psychiatric risk factors for suicidality in youth: the great smoky mountains study. Archive of General Psychiatry. 2006;63:1017–1024. [DOI] [PubMed] [Google Scholar]
- 8.Goldston DB, Reboussin BA, Daniel SS. Predictors of suicide attempts: state and trait components. Journal of Abnormal Psychology. 2006;115(4):842. [DOI] [PubMed] [Google Scholar]
- 9.Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR. Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54(2):97–107.e102. [DOI] [PubMed] [Google Scholar]
- 10.Gould M, Greenberg T, Velting D, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. [DOI] [PubMed] [Google Scholar]
- 11.Herba CM, Ferdinand RF, van der Ende JAN, Verhulst FC. Long-Term Associations of Childhood Suicide Ideation. J Am Acad Child Adolesc Psychiatry. 2007;46(11):1473–1481. [DOI] [PubMed] [Google Scholar]
- 12.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Suicidal behaviour in adolescence and subsequent mental health outcomes in young adulthood. Psychol Med. 2005;35(07):983–993. [DOI] [PubMed] [Google Scholar]
- 13.Goldman-Mellor SJ, Caspi A, Harrington H, et al. Suicide attempt in young people: A signal for long-term health care and social needs. JAMA Psychiatry. 2014;71:119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reinherz HZ, Tanner JL, Berger SR, Beardslee WR, Fitzmaurice GM. Adolescent suicidal ideation as predictive of psychopathology, suicidal behavior, and compromised functioning at age 30. American Journal of Psychiatry. 2006;163:1226–1232. [DOI] [PubMed] [Google Scholar]
- 15.Dhossche D, Ferdinand R, van der Ende J, Hofstra M, Verhulst FC. Diagnostic outcome of adolescent self-reported suicidal ideation at 8-year follow-up. J Affect Disord. 2002;72:273–279. [DOI] [PubMed] [Google Scholar]
- 16.Brière FN, Rohde P, Seeley JR, Klein D, Lewinsohn PM. Adolescent suicide attempts and adult adjustment. Depress Anxiety. 2015;32:270–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat Simul Comput. 2010;39:860–864. [Google Scholar]
- 18.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry. 2008;192(2):98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goldston DB, Erkanli A, Daniel SS, Heilbron N, Weller BE, Doyle O. Developmental Trajectories of Suicidal Thoughts and Behaviors From Adolescence Through Adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2016;55(5):400–407.e401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fergusson DM, Lynskey MT. Suicide attempts and suicidal ideation in a birth cohort of 16-year-old New Zealanders. J Am Acad Child Adolesc Psychiatry. 1995;34:1308–1317. [DOI] [PubMed] [Google Scholar]
- 21.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. [DOI] [PubMed] [Google Scholar]
- 22.Angold A, Costello EJ. The Child and Adolescent Psychiatric Assessment (CAPA). Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. [DOI] [PubMed] [Google Scholar]
- 23.Posner K, Oquendo MA, Gould M, Stanley B, Davies M. Columbia Classification Algorithm of Suicide Assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164:1035–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.SAS/STAT® Software: Version 9 [computer program]. Cary, NC: SAS Institute, Inc.; 2004. [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Fourth Edition Text Revision. Washington D.C: American Psychiatric Press; 2000. [Google Scholar]
- 26.Angold A, Costello E. The Child and Adolescent Psychiatric Assessment (CAPA). Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:39–48. [DOI] [PubMed] [Google Scholar]
- 27.Pickles A, Dunn G, Vazquez-Barquero J. Screening for stratification in two-phase (‘two-stage’) epidemiological surveys. Statistical Methods in Medical Research. 1995;4(1):73–89. [DOI] [PubMed] [Google Scholar]
- 28.Goldston DB, Daniel SS, Erkanli A, et al. Suicide attempts in a longitudinal sample of adolescents followed through adulthood: Evidence of escalation. Journal of Consulting and Clinical Psychology. 2015;83(2):253–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cannell CF, Miller PV, Oksenberg L. Research on interviewing techniques. Sociological Methodology. 1981;12:389–437. [Google Scholar]
- 30.Cannell CF, Marquis KH, Laurent A. A summary of studies of interviewing methodology: 1959–1970. Vital and Health Statistics. 1977;2:1–78. [PubMed] [Google Scholar]
- 31.Angold A, Erkanli A, Costello EJ, Rutter M. Precision, reliability and accuracy in the dating of symptom onsets in child and adolescent psychopathology. J Child Psychol Psychiatry. 1996;37:657–664. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.