Abstract
Introduction:
Current evidence is controversial about the outcomes after the repair of the delaminated versus nondelaminated rotator cuff tears. The objective of this study was to evaluate the factors affecting delamination of the cuff and clinical and structural outcomes after en masse arthroscopic repair of delaminated versus nondelaminated cuff of varying sizes.
Materials and Methods:
A total of 233 patients with full-thickness posterosuperior cuff tears were divided in two groups: Group 1: Delaminated tears (n = 131) and Group 2: Nondelaminated tears (n = 102) of medium, large, and massive sizes. Both groups were evaluated by clinical scores (Constant–Murley [CM], American shoulder and elbow score [ASES]) and ultrasonography (USG), at a minimum followup of 2 years.
Results:
The mean followup was 45.47 months. There was a weak but statistically significant linear correlation (P = 0.02) between the increasing size of tear and delamination, whereas increasing age and duration of symptoms did not correlate with increasing tendency of delamination. Final followup USG analysis revealed that there was no significant difference (P = 0.55) between healing rates of Group 1 and Group 2. Further taking various tear sizes into account, USG revealed no significant difference between the healing rates of two groups. The mean overall final postoperative CM and ASES scores of two groups did not show any significant difference (CM; P = 0.36, ASES; P = 0.4). However, the clinical outcome was significantly better in the completely healed group as compared to partially healed or retear group.
Conclusions:
A weak linear correlation between delamination and increasing size of the tear was noted. Although overall structural and clinical outcome is no different between two groups, the clinical outcomes of completely healed tear are better than partially healed ones.
Level of Evidence:
Level III, Retrospective comparative.
Keywords: Clinical outcome, cuff healing, delamination, partially healed defect, rotator cuff tear, size of tear
Introduction
Delamination of rotator cuff tendons was first described by Sonnabend et al. as the horizontal splitting of the tendon along with its histology and suggested that the presence of end arteritis obliterans in rotator cuff, causing local ischemia, along with dissimilar stresses between the layers (due to different collagen fiber orientation in the rotator cuff) result in delamination.1 Chang-Wan Kim et al. further defined delamination as a horizontally retracted tear of both the articular and bursal sides of the tendon, with a distinguishable gap between the articular and bursal surfaces, and interstitial horizontal splitting.2 Gwak et al. suggested that delaminated tears could be both partial and complete.3 As knowledge about the rotator cuff tendons delamination improved, the incidence of these lesions has been picked up more frequently and has been quoted to be between 38% and 92%.2,4,5,6 Sonnabend et al. also advocated curettage of delaminated layers lined by synovial cells before repair, to promote healing.1
Once delaminated, the factors possibly associated with progression of delamination of the rotator cuff tear (age, size of tear, duration of tear) remain under investigation. Although few studies have found no difference in the occurrence of delamination with advancing age or size of the tear,7 it still remains unsettled whether the delamination increases with advancing age, duration of a symptom, or increasing size of the tear. Nevertheless, it seems plausible that the delaminated layer, if unrepaired, may lead to a poor outcome, as a substantial portion of the tendon would not heal to the footprint. Many studies have confirmed that the presence of delamination has little effect on healing and outcome, if the tear is repaired on to the footprint,2,8,9,10 whereas few studies have indicated the negative correlation of delamination with tendon healing and outcome after its arthroscopic repair.4,5,11 Regarding the type of repair of the delaminated layer, many authors have described various techniques of repair of delaminated rotator cuff tears, as en masse repair of delaminated layers,2,3 dual layer repair using suture bridge, or double row repair.10,11 However, most studies conducted in recent past focus on the type of repair in delaminated tears,3,10,12,13 rather than comparing the repair of delaminated versus nondelaminated tears.2,7 Further, most authors did not compare the effect of increasing size of the tear affecting the clinical and structural outcome, after repair of delaminated versus nondelaminated rotator cuff tears.7
With the controversy still existing about whether there is any clinical and structural outcome difference between delaminated and nondelaminated tears in varying sizes and associated factors, this study was conducted: (1) to comprehend if delamination increase in complete rotator cuff tears, with respect to the increasing age, duration of symptoms, and size of the cuff tear and (2) to compare the structural and clinical outcomes of patients who underwent arthroscopic en masse repair, in rotator cuff tears with and without delamination (in varying sizes of cuff tears – medium, large, and massive tears). Our working null hypothesis was that increasing age, duration of symptoms, and size of tear would not affect delamination, and the presence of delaminated tears would not result in a poor structural and clinical outcome in comparison to nondelaminated tears even if the size of tear increases.
Materials and Methods
Study design and patient selection
After institutional ethical committee approval (IEC 523/2014), we included 268 patients, between January 2010 and January 2015, with medium to massive sized full-thickness rotator cuff tears (delaminated and nondelaminated), who underwent arthroscopic rotator cuff repair, with a minimum followup of 2 years. The exclusion criteria were (1) partial and small cuff tears, (2) irreparable cuff tears or partial repair of cuff, (3) concomitant labral repair or associated fracture fixations, (4) concomitant Grade 2 or more glenohumeral arthritis, (5) concomitant Lafosse Type 4 and Type 5 subscapularis tear and repair, and (6) severe supra- and infraspinatus atrophy and Goutallier Grade 3 and 4 fatty infiltrated muscles.
Partial cuff tears were excluded because one, we had selected to analyze complete tears, with both delaminated layers being detached from the footprint, whereas, in partial tear, one layer is attached to the footprint, bursal, or articular. Second, still, usually, most partial rotator cuff repairs remain painful and stiff for a longer duration, and this could have affected the clinical outcome. Small cuff tears were also excluded as they mostly heal, irrespective of minor delamination.
The patients were further divided into two groups; delaminated tears (Group 1) and nondelaminated tears (Group 2). The size of the tear (medium–massive) was determined based upon arthroscopic findings, which were recorded in a standardized digital and video format. Thirty five patients (13%) were lost to followup. Finally, 233 patients, who completed a minimum of 2 years of followup, were evaluated.
Preoperative clinical and radiological evaluation
All patients with suspected rotator cuff tear underwent comprehensive standard clinical evaluation. After clinical evaluation, the patients underwent radiographic analysis using plain radiograph and ultrasound (USG) or magnetic resonance imaging (MRI) to confirm the diagnosis. USG was performed at our institute by trained musculoskeletal sonologist, using Philips iU22 xMATRIX machine (Amsterdam, The Netherlands) with a high resolution 12–5 MHz linear array transducers. There was no preoperative attempt to detect delamination of the cuff by a sonologist. Preoperative Constant–Murley (CM) and American shoulder and elbow (ASES) scores were calculated.
Surgical technique
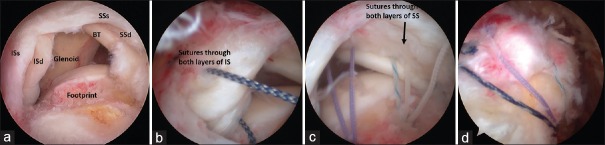
All arthroscopic repairs were done by a single senior surgeon, with the patient under general anesthesia or interscalene block, in lateral decubitus position. Standard posterior, anterior, lateral, and posterolateral portals were made. Diagnostic arthroscopy of the shoulder was performed from the posterior portal. The intraarticular lesions were treated as per the standard norm. Biceps tendon was left alone if there was no biceps lesion. If the biceps tendon was found to have degenerative features (fraying, splitting, or severe synovitis), a tenotomy was performed in elderly low demand patients, whereas open subpectoral biceps tenodesis was performed using bioabsorbable interference screw in young and/or demanding patients. Type 1 subscapularis tears were debrided, whereas Type 2 and 3 were repaired using a single anchor. Then, the scope was shifted to the subacromial space. Adequate subacromial bursectomy was performed. Bony acromioplasty was performed only if there was a spur. The number of torn tendons, size of tear, and retraction of posterosuperior rotator cuff tendons were also noted. The anteroposterior size of the cuff tear was determined using a graduated probe. The size of the tear was classified according to the Cofield classification as small (<1 cm), medium (1–3 cm), large (3–5 cm), or massive (>5 cm).14 The delamination in anterior and posterior parts of the cuff was noted from posterolateral and lateral portals. The delamination was further defined intraoperatively as horizontal split between two layers of the cuff, with horizontal split extending 5 mm medial to the tip of the split, and was measured by graduated probe. Han et al. concluded that delamination of the rotator cuff could be 100% confirmed through the posterolateral and lateral portal.6 We commonly used the posterolateral and lateral portals to identify delamination in each case and rarely the anterolateral portal. After confirming the size of the tear, the edges of the tear were pulled laterally to check the reducibility of the tendon over the footprint. Further, both superior and inferior delaminated layers were separately held with a suture retriever or tissue grasper, and their reducibility to the footprint was checked. Sometimes, both layers could be reduced equally on the footprint. However, more often, the inferior layer was found to be retracted more medially than the superior one, and it was difficult to reduce it anatomically on the footprint. In latter case, mobilization of the cuff was done as necessary by releasing the coracohumeral ligament, paralabral capsular releases, or other subacromial adhesions to make the inferior layer more mobile. However, no interval slides were performed. Again, the layers were held together to reduce it onto the footprint. If inferior layer could be brought 5–7 mm lateral to the articular cartilage margin, it was accepted for repair. However, if the inferior layer remained rigid even after releases, 2–5 mm medialization of the footprint was performed to provide healing area for the inferior layer without tension after fixation. In no case, we attempted to debride or curette the upper and lower surface of the delaminated layer as suggested by Sonnabend et al. to get rid of the synovial layer.1 Then, greater tuberosity was gently abraded to get a good bleeding bed of cancellous bone. All medium-sized tears were repaired with single row technique using one or two anchors, whereas large and massive tears were repaired by dual row suture bridge technique. Current literature supports single row repair for medium-sized tears and double row repair for large- and massive-sized tears.15 In single row technique, the anchors were placed in the middle of the greater tuberosity, en masse sutures were passed through the delaminated layers using the Mason Allen technique and were tied sequentially. In suture bridge technique, the medial row anchors were placed just lateral to the humeral head cartilage margin. En masse repair was performed by passing sutures through both inferior and superior layers in mattress fashion. Medial row knots were tied, and free limbs were anchored laterally 1 cm below the tuberosity using footprint anchors [Figure 1].
Figure 1.
Arthroscopic view of the right shoulder with complete SS and IS tear. (a) Delaminated tear of SS and IS; (b) en masse sutures through the IS; (c) en masse sutures through the SS; (d) completed double row suture bridge repair of delaminated tear. ISs: Superficial delaminated layer of infraspinatus; ISd: Deeper delaminated layer of infraspinatus; SSs: Superficial delaminated layer of supraspinatus; SSd: Deeper delaminated layer of supraspinatus; BT: Biceps tendon; SS: Supraspinatus; IS: Infraspinatus
Postoperative rehabilitation
All patients were started on structured rotator cuff rehabilitation protocol followed at our institute. They were advised to use arm sling for 4–6 weeks. During the first 4 weeks, all patients were encouraged for the elbow, wrist, finger mobilization and isometric scapular exercises. In the case of medium-sized tears repair, the gentle passive range of movement (ROM) was started on the 1st postoperative day with 30° forward flexion and 30° abduction, while rotations permitted up to neutral. However, large and massive tears were immobilized in an arm sling for 6 weeks with no flexion or abduction allowed. Medium-sized tears were further passively mobilized by the 5th week and active-assisted ROM was initiated by the 7th week. Large and massive tears were started on gentle passive movement at 7th week followed by an active-assisted movement from 9th week onward. At the end of 3 months, ultrasonography of the shoulder was performed in all the cases to ascertain the healing status of the cuff and footprint. The patients were then allowed a full-active ROM and isometric strengthening of the cuff. After 16 weeks, patients were started on advance strengthening exercises of the cuff with therabands. Return to full activity was allowed after 8–12 months after the restoration of strength and movements.
Final clinical and radiological evaluation
Patients underwent a standard clinical evaluation at 6 and 12 months and after that at yearly followup. Each patient was followed up for a minimum period of 2 years. The postoperative clinical outcomes were analyzed by CM and ASES scores. The range of motion was measured using a goniometer. The strength measurement was included in the CM scoring. The strength measurement was done keeping the patient in standing, with arm 90° elevation in scapular plane, with the elbow in full extension and forearm pronated. The spring balance was tied around the distal forearm of the patient. The patient was asked to maintain the position for 5 s, and three consecutive readings were taken. The average was noted in pounds. The structural outcome of healing tendons was analyzed by serial ultrasonographies, performed at 3 months and then yearly postoperatively, by a single musculoskeletal radiologist. The integrity of tendon healing was recorded in three grades; Grade 1: Healed cuff with normal thickness (>2 mm) and normal echotexture or with one or few echogenic areas with no tear; Grade 2: Healed cuff with bursal or articular side partial defect but no full-thickness discontinuity; Grade 3: Full-thickness tear, partial or complete anteroposterior width. A similar grading is suggested using computed tomography arthrography (CTA) at 6 months.16 However, we did not use CTA as it repetitive CTA would be high on radiation dose and expensive. Moreover, CTA cannot detect bursal defects.
Statistical analysis
Descriptive analysis was used for frequencies and means of various variables. Chi-square test was performed to analyze and compare categorical variables using contingency tables. Bivariate Spearman correlation was used to assess the correlation between delamination and age, duration of symptoms, and size of the tear. Paired sample t-test was used to analyze the difference in the means of clinical scores of the same group (delaminated and nondelaminated) at pre- and postoperative followup. Independent sample t-test was utilized to analyze the difference between the clinical scores of delaminated and nondelaminated groups. A comparison of clinical scores among the delaminated and nondelaminated group layered with anatomic healing group, partial defect group, and full-thickness tear group was performed using one-way ANOVA analysis or Kruskal–Wallis H-test. Statistical analysis was performed using SPSS 16.0 (IBM, Armonk, NY, USA), and the significance level was kept at P < 0.05.
Results
The overall mean (±standard deivaiton [SD]; range) followup of 233 patients was 45.47 months (±12.6; 24–78). There were 131 patients (56%) in delaminated (Group 1) and 102 patients (44%) in nondelaminated category (Group 2). The mean age, sex, duration of symptoms, size of the tear, preoperative CM and ASES score, and mean followup were comparable in two groups [Table 1]. Although the two groups remain comparable on baseline statistics, the prevalence of delamination increases as the size of tear increases from medium to massive (medium: large: massive = 47.2%:57.3%:70.8%). Even though weak, there was a statistically significant linear correlation between the increasing size of tear and prevalence of delamination (P = 0.02; Spearman correlation coefficient = 0.14). However, there was no significant correlation of delaminated cuff with advancing age (P = 0.76; Spearman correlation coefficient = 0.02) or duration of symptoms (P = 0.97; Spearman correlation coefficient = 0.002).
Table 1.
Baseline characteristics of patients in two groups
| Group characteristics | Delaminated (n=131), n (%) | Nondelaminated (n=102), n (%) | P |
|---|---|---|---|
| Age (years), mean±SD | 59.4±9 | 58.5±10 | 0.46 |
| Sex | |||
| Male | 82 (62.6) | 69 (67.6) | 0.49 |
| Female | 49 (37.4) | 33 (32.4) | |
| Duration of symptoms in months±SD | 10.98±14.05 | 10.21±12.01 | 0.66 |
| Size of tear | |||
| Medium (n=72) | 34 (47.2) | 38 (52.8) | 0.08 |
| Large (n=117) | 67 (57.3) | 50 (47.2) | |
| Massive (n=44) | 30 (70.8) | 14 (29.2) | |
| Preoperative clinical scores | |||
| CM score | 31.48±6.8 | 30.87±5.6 | 0.46 |
| ASES score | 28.6±4.2 | 30.2±6.2 | 0.37 |
| Mean followup in months±SD | 44.38±12.4 | 46.92±12.8 | 0.27 |
CM=Constant–Murley, ASES=American shoulder elbow society, SD=Standard deviation
Structural healing of tendon over footprint based upon ultrasonographic assessment
Final followup USG revealed that there was no significant difference (P = 0.55) between the healing rates of delaminated and nondelaminated groups [Table 2]. 75% (n = 175) patients revealed complete healing, while 15.5% (n = 36) showed partial defects on articular or bursal surfaces. 9.5% (n = 22) of the tears had full-thickness retear. Amid 36 patients with a partial defect, there were 29 patients (80.5%) with an articular sided partial defect, and seven patients with a bursal-sided partial defect (19.5%) [Table 3]. There was more articular-sided defect in both groups, but the difference between the two groups was not significant (P = 0.67).
Table 2.
Tendon healing rate in delaminated and nondelaminated group
| Delaminated or nondelaminated | Intact, normally healed (n=175; 75%) | Partial defect (n=36; 15.45%) | Retear (n=22; 9.55%) | P |
|---|---|---|---|---|
| Group 1 - Delaminated (n=131) | 95 (72.5) | 23 (17.6) | 13 (9.9) | 0.55 |
| Group 2 - Nondelaminated (n=102) | 80 (78.4) | 13 (12.7) | 9 (8.8) |
Table 3.
Location of partial defect (bursal or articular) in 36 patients with partial defect healed tendons over the footprint
| Type of tear | Partial articular side defect | Partial bursal side defect | P |
|---|---|---|---|
| Delaminated tears (n=23) | 19 | 4 | 0.67 |
| Nondelaminated tear (n=13) | 10 | 3 |
Individually, when healing rates of medium to massive-sized tear were compared amid two groups, there was no difference between the healing patterns “within the tear size group” [Table 4].
Table 4.
Healing pattern in various size of tear in two groups, delaminated versus nondelaminated
| Size of tear | Delaminatedornondelaminated | Intact, normally healed (n=175), n (%) | Partially healed (n=36), n (%) | Retear (n=22), n (%) | P |
|---|---|---|---|---|---|
| Medium size tear (n=72) | Delaminated (n=34) | 29 (85.3) | 4 (11.8) | 1 (2.9) | 0.27 |
| Nondelaminated (n=38) | 30 (78.9) | 3 (7.9) | 5 (13.2) | ||
| Column total | 59 (81.9) | 7 (9.7) | 6 (8.3) | ||
| Large size tear (n=117) | Delaminated (n=67) | 51 (76.1) | 10 (14.9) | 6 (9) | 0.29 |
| Nondelaminated (n=50) | 41 (82) | 8 (16) | 1 (2) | ||
| Column total | 92 (78.6) | 18 (15.4) | 7 (6) | ||
| Massive size tear (n=44) | Delaminated (n=30) | 15 (50) | 9 (30) | 6 (20) | 0.52 |
| Nondelaminated (n=14) | 9 (64.3) | 2 (14.3) | 3 (21.4) | ||
| Column total | 24 (54.5) | 11 (25) | 9 (20.45) |
Clinical outcome based on Constant–Murley and American shoulder and elbow scores
The overall mean CM and ASES (±SD) score improved significantly from 31.48 (±6.8) to 82.23 (±7.8) and 42.6 to 86.17 (±7.8) (P < 0.0001) at a minimum of 2 years followup. However, the mean final postoperative CM and ASES scores of delaminated and nondelaminated groups revealed no significant difference [Table 5].
Table 5.
Mean Constant–Murley and American shoulder elbow society scores of two groups
| Type of tear | CM score±SD | ASES score±SD |
|---|---|---|
| Delaminated tear (Group 1) | 81.8±7.5 | 85.8±7.8 |
| Nondelaminated tear (Group 2) | 82.7±8.1 | 86.6±8.1 |
| P | 0.36 | 0.4 |
CM=Constant–Murley, ASES=American shoulder elbow society, SD=Standard deviation
Further, when clinical scores were compared in healed, partial defect, and complete retear group, the CM and ASES scores were significantly superior in the completely healed group in comparison to cuffs with a partial defect or retear group (P < 0.0001) [Table 6]. However, there was no difference in clinical scores between partial defect and retear group (P = 0.98).
Table 6.
Constant–Murley and American shoulder elbow society scores in patients with completely healed, with partial defect and complete retear
| Scores | Completely healed | Partial defect in tendon | Complete tear |
|---|---|---|---|
| Mean CM score±SD | 84.1±6.7 | 76.5±7.1 | 76.4±10.1 |
| Mean ASES score±SD | 88.0±6.7 | 80.3±7.1 | 80.7±10.7 |
CM=Constant–Murley, ASES=American shoulder elbow society, SD=Standard deviation
Discussion
The most important finding of our study is that, in comparison to nondelaminated cuff, repair of a delaminated cuff does not affect the clinical and structural outcomes even if the tear size increases from medium to massive. Furthermore, slightly higher tendency of delamination was noted with increasing size of the tear.
The presence of delamination in rotator cuffs and its effect on healing over the footprint after the repair has been a topic of debate in recent years. It may be presumed that factors such as increasing age, longer duration of a symptom, or larger size of tear may increase the chance of delamination. Despite multiple published studies, fewer authors have looked into these facts. MacDougal and Todhunter suggested that there is no correlation between age or size of tear and delamination.7 Choo et al. concluded in an MRI-based study that age is similar in delaminated versus nondelaminated group.17 However, no author established any correlation between size of tear and delamination. In our study, the occurrence of delamination was not affected by advancing age or duration of symptoms. However, there was a positive linear correlation between occurrence of delamination and size of the tear. The increasing occurrence of delamination with increasing size of tear could be perhaps understood by the anatomical variation in different fibers of supraspinatus and infraspinatus, explained by Mochizuki et al.18 The supraspinatus has anterior long and thick and posterior short and thin fibers, whereas infraspinatus has long and thick superior fibers and short and thin inferior fibers, each running in a different direction. Hence, this may explain why delamination increases when more tendons are involved (increased size) with delaminated layers running in different directions.
The biggest challenge with the presence of delamination is to accurately identify the delamination, followed by its anatomic repair on the footprint. Cha et al. identified different patterns of retraction of both superior and inferior layers of supraspinatus and infraspinatus and posteromedial and anteromedial retraction.10 We did not attempt to classify such patterns in our study as the fundamental strategy to repair any “repairable” cuff remains the same whether it is retracted antero- or posteromedial.
Earlier studies quoted delamination as a negative prognostic factor in clinical outcome,4,5 whereas recent studies find no influence of delamination on clinical outcome.2,7 Recently published studies have discussed “repair of full-thickness delaminated cuff” and its outcome.10,13 Kim et al. compared the results after en masse and double row repair,13 whereas Cha et al. discussed the outcomes after the repair of delaminated cuff utilizing dual layer suture bridge and standard double row technique.10 Gwak et al. compared the outcomes after en masse suture bridge repair of full-thickness and partial-thickness delaminated cuff tears.3
Only Chang-Wan Kim et al. and MacDougal and Todhunter compared the results after repair of delaminated versus nondelaminated cuff tears.2,7 Further, Chang-Wan Kim et al. included “only small- and medium-sized tears” in their study and they did not compare the outcomes of two sizes, concerning delamination and nondelamination.2 They reported “no-different” clinical outcomes at 2 years between the two groups, but structural healing was reported at 6 months using CT arthrogram. However, they concluded that the degree of tissue healing after repair “differed” between the delaminated and nondelaminated rotator cuff tear groups. The delaminated group had more partial defect healing, and nondelaminated ones had a full thickness retear. On the other hand, MacDougal and Todhunter included “all sizes of tears” in their study and reported that the clinical outcomes at 2 years (WORC score) were similar amid all sizes of both groups. However, they performed miniopen repair of the cuff and did not report any structural healing or failure by any radiological methods.
Our study is the first to report both clinical and structural outcomes at a minimum of 2-year followup, comparing both delaminated and nondelaminated rotator cuff tears, in medium to massive tear size. We did not find any difference, clinical or structural between the two groups amid all sizes of the tear. Our clinical outcomes are similar to one reported by Kim et al. However, Kim et al. reported significantly different structural healing between the two groups, wherein delaminated ones showed more tendency of partial defects and nondelaminated cuff showed a more retear tendency, whereas our study had no such trend noted. Further, they evaluated the radiological outcomes at just six months postoperatively, whereas we followed up patients for a minimum of 2 years and more. Cha et al. suggested that delamination disappeared in 89% of their cases on followup MRI.10 We too believe that cuff continues to heal gradually, and smaller partial defects which persist initially may heal completely over the years, and an early MRI or CTA at 6 months may overestimate postoperative partial defects, reducing the rate of the completely healed cuff.
Various authors describe a different method to repair the delaminated layer; en masse repair wherein both layers are taken together,2,3,9,13 separate suture for inferior layer via placing a separate medial anchor,10,11,19 or only bursal side if the articular side cannot be reduced over the footprint without tension.12 Proponents for individual layer repair suggest that individual layer repair ensures that there is lesser tension, and this leads to lesser pain and lesser chance of retear. On the contrary, defenders of en masse repair suggest that repairing the layers together leads to better healing between the two layers due to decreased shear force. Recently, Cheon et al. conducted an experimental study in rabbits and concluded that en masse repair of the delaminated cuff in comparison to individual layer repair leads to a narrow gap between layers and higher yield load at three weeks.20 Kim et al. conducted a randomized controlled trial between en masse repair versus separate dual layer repair and found no difference in clinical and structural outcomes, except better pain score in separate dual layer repair.13 On the other hand, Kim et al. suggested that if the articular or inferior layer cannot be reduced without tension, one should not repair it, as there is no structural or clinical difference between the results between en masse or only bursal side repair.12 Furthermore, all layer suturing may produce undue tension on the articular layer as it is pulled onto the footprint, resulting in its failure. Hence, they suggest a bursal layer only repair in delaminated cuff tears. We preferred to use en masse repair as the similar results are reported by various authors, with complete healing rate varying between 45% and 70%.2,13
The overall complete healing rate in our series was 75%, which was marginally higher than reported in other studies. A possible reason why healing rate is reported slightly higher in our series is that we have used USG finding of the last followup at a minimum of 2 years and further, whereas others have done the CTA at 6 months.2,3 Further, the use of USG also helped us in estimating the site of partial defect on the bursal side too, which was 19.6%. This finding of persistent bursal defect has not been reported in any other study.
Sonnabend et al. also emphasized that the presence of synovial lining (5 out of 17 cases) between the layers of delamination can be suggestive of chronicity of the tear.1 Many authors suggested that the opposing layers should be curetted before the repair, as the presence of synovial lining may hinder the healing process.1,3,7 MacDougal and Todhunter curetted the layers but did not perform any postoperative radiological investigations to confirm the healing of tear or cleavage.7 Gwak et al. performed the curettage of opposing layers but detected the presence of cleavage in 25.7%–48.6% of his patients, on CTA at 6-month postoperatively, done in partial delaminated and complete delaminated cuff tears respectively.3 It may suggest that, despite curettage, the layers may not heal with each other and cleavage may persist. Many authors did not report any negative influence on repair integrity without curettage.2,10 Similarly, we did not perform curettage of the layers and this did not have any negative influence on the clinical or structural outcomes of our study. Such results were comparable with other studies.
Limitation of the study
We have certain limitations in our study design. One, only one author has decided upon the presence and absence of delamination during arthroscopy. Even though the operating surgeon is a quite experienced surgeon, interobserver variation might exist, especially when the 5 mm medial split between superior and inferior layers has to be taken into account. Two, we have not taken fatty infiltration and atrophy into postoperative outcomes assessment, because primary mode of postoperative radiological investigation was ultrasonography. It was difficult to ask for MRI or CTA in every patient at repeated intervals due to longer waiting time, financial constraints, and concerns of radiation (in CTA). Although studies suggest that there is a good correlation between USG and MRI for the assessment of atrophy and fatty infiltration,21 the inter- and intraobserver reliability is only fair to good between the two modes of investigation.22 Although our sonologist reported the fatty infiltration and atrophy in the report, lack of standardization precluded us from taking that into account. Third, not all patients underwent similar repair method as medium-sized tear underwent single row and large to massive-sized tear underwent double row transosseous equivalent suture bridge repair. However, the current literature supports single row repair for medium-sized tears as it does not affects the outcome as compared to double row repair.15 Fourth, even though the healing of the delaminated tendons of the footprint remained unaffected without curettage of opposing layers, it remains unclear whether the presence of cleavage in postoperative scans would improve with intraoperative curettage or not. However, in most cases, our sonologist was not able to detect the cleavage between the healed layers. Probably, an MRI would be a better investigation to detect such subtle changes between the two layers.
Conclusions
The fundamental conclusion of our study is that increasing age or longer duration of symptom does not correlate with delamination. However, a weak linear correlation between delamination and increasing size of the tear exists. In comparison to nondelaminated tears, the presence of delamination does not affect the clinical or structural outcomes after en masse arthroscopic rotator cuff repair, while the size of tear increases from medium to massive. However, the clinical outcomes are significantly better in the completely healed group as compared to partially healed or retear group. We also conclude that not curreting the opposing layers may not have any effect on healing over the footprint. However, prospective randomized studies must be conducted to study the effect of curettage on the healing of cleavage.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sonnabend DH, Yu Y, Howlett CR, Harper GD, Walsh WR. Laminated tears of the human rotator cuff: A histologic and immunochemical study. J Shoulder Elbow Surg. 2001;10:109–15. doi: 10.1067/mse.2001.112882. [DOI] [PubMed] [Google Scholar]
- 2.Chang-Wan Kim JH, Gwak HC, Park JH. The comparison of outcomes between delaminated and nondelaminated rotator cuff tear repair: Is delamination a negative prognostic factor? J Shoulder Elbow Surg. 2017;26:216–24. [Google Scholar]
- 3.Gwak HC, Kim CW, Kim JH, Choo HJ, Sagong SY, Shin J, et al. Delaminated rotator cuff tear: Extension of delamination and cuff integrity after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2015;24:719–26. doi: 10.1016/j.jse.2014.09.027. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG, et al. Arthroscopic repair of full-thickness tears of the supraspinatus: Does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229–40. doi: 10.2106/JBJS.D.02035. [DOI] [PubMed] [Google Scholar]
- 5.Flurin PH, Landreau P, Gregory T, Boileau P, Brassart N, Courage O, et al. Arthroscopic repair of full-thickness cuff tears: A multicentric retrospective study of 576 cases with anatomical assessment. Rev Chir Orthop Reparatrice Appar Mot. 2005;91:31–42. doi: 10.1016/s0035-1040(05)84503-9. [DOI] [PubMed] [Google Scholar]
- 6.Han Y, Shin JH, Seok CW, Lee CH, Kim SH. Is posterior delamination in arthroscopic rotator cuff repair hidden to the posterior viewing portal? Arthroscopy. 2013;29:1740–7. doi: 10.1016/j.arthro.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 7.MacDougal GA, Todhunter CR. Delamination tearing of the rotator cuff: Prospective analysis of the influence of delamination tearing on the outcome of arthroscopically assisted mini open rotator cuff repair. J Shoulder Elbow Surg. 2010;19:1063–9. doi: 10.1016/j.jse.2009.12.020. [DOI] [PubMed] [Google Scholar]
- 8.Charousset C, Grimberg J, Duranthon LD, Bellaïche L, Petrover D, Kalra K, et al. The time for functional recovery after arthroscopic rotator cuff repair: Correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008;24:25–33. doi: 10.1016/j.arthro.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 9.Park JY, Lhee SH, Oh KS, Moon SG, Hwang JT. Clinical and ultrasonographic outcomes of arthroscopic suture bridge repair for massive rotator cuff tear. Arthroscopy. 2013;29:280–9. doi: 10.1016/j.arthro.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 10.Cha SW, Lee CK, Sugaya H, Kim T, Lee SC. Retraction pattern of delaminated rotator cuff tears: Dual-layer rotator cuff repair. J Orthop Surg Res. 2016;11:75. doi: 10.1186/s13018-016-0407-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mori D, Funakoshi N, Yamashita F. Arthroscopic lamina-specific double-row fixation for large delaminated rotator cuff tears. Arthrosc Tech. 2014;3:e667–71. doi: 10.1016/j.eats.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim SJ, Choi YR, Lee HH, Chun YM. Surgical results of delaminated rotator cuff repair using suture-bridge technique with all-layers or bursal layer-only repair. Am J Sports Med. 2016;44:468–73. doi: 10.1177/0363546515615573. [DOI] [PubMed] [Google Scholar]
- 13.Kim YS, Lee HJ, Jin HK, Kim SE, Lee JW. Conventional en masse repair versus separate double-layer double-row repair for the treatment of delaminated rotator cuff tears. Am J Sports Med. 2016;44:1146–52. doi: 10.1177/0363546516628869. [DOI] [PubMed] [Google Scholar]
- 14.DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563–7. [PubMed] [Google Scholar]
- 15.Spiegl UJ, Euler SA, Millett PJ, Hepp P. Summary of meta-analyses dealing with single-row versus double-row repair techniques for rotator cuff tears. Open Orthop J. 2016;10:330–8. doi: 10.2174/1874325001610010330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Charousset C, Bellaïche L, Kalra K, Petrover D. Arthroscopic repair of full-thickness rotator cuff tears: Is there tendon healing in patients aged 65 years or older? Arthroscopy. 2010;26:302–9. doi: 10.1016/j.arthro.2009.08.027. [DOI] [PubMed] [Google Scholar]
- 17.Choo HJ, Lee SJ, Kim JH, Kim DW, Park YM, Kim OH, et al. Delaminated tears of the rotator cuff: Prevalence, characteristics, and diagnostic accuracy using indirect MR arthrography. AJR Am J Roentgenol. 2015;204:360–6. doi: 10.2214/AJR.14.12555. [DOI] [PubMed] [Google Scholar]
- 18.Mochizuki T, Sugaya H, Uomizu M, Maeda K, Matsuki K, Sekiya I, et al. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008;90:962–9. doi: 10.2106/JBJS.G.00427. [DOI] [PubMed] [Google Scholar]
- 19.Sugaya H, Maeda K, Matsuki K, Moriishi J. Functional and structural outcome after arthroscopic full-thickness rotator cuff repair: Single-row versus dual-row fixation. Arthroscopy. 2005;21:1307–16. doi: 10.1016/j.arthro.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Cheon SJ, Kim JH, Gwak HC, Kim CW, Kim JK, Park JH, et al. Comparison of histologic healing and biomechanical characteristics between repair techniques for a delaminated rotator cuff tear in rabbits. J Shoulder Elbow Surg. 2017;26:838–45. doi: 10.1016/j.jse.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: Sonography versus MRI. AJR Am J Roentgenol. 2008;190:1105–11. doi: 10.2214/AJR.07.2835. [DOI] [PubMed] [Google Scholar]
- 22.Okoroha KR, Mehran N, Duncan J, Washington T, Spiering T, Bey MJ, et al. Characterization of rotator cuff tears: Ultrasound versus magnetic resonance imaging. Orthopedics. 2017;40:e124–30. doi: 10.3928/01477447-20161013-04. [DOI] [PubMed] [Google Scholar]