Abstract
Background:
All-suture fixation for the treatment of Neer's Type IIB lateral clavicle fractures by coracoclavicular (CC) ligament reconstruction has become popular in the past decade. Results of modified under-coracoid-around-clavicle (UCAC) technique are reported in this paper.
Methodology and Results:
Nineteen consecutive patients with minimum 6-month followup (FU) were identified. Average FU was 23 months (6–47 m), mean age was 38 years (16–81), and male-to-female ratio was 2:1. The time to surgery varied from 4 days to 12 weeks. Two patients had primary lateral end excision; of the rest, all but one healed fully. Average time to regain full range of motion was 4 weeks; postoperative Oxford Shoulder Score at 6 months was 43. All the patients returned to their previous occupation. One patient showed mild osteolysis on the last X-rays. There were no cases with infections or stiffness.
Discussion:
CC ligament reconstruction converts the unstable Type IIB fracture into stable Type I; therefore, it is unnecessary to fix the distal fragment separately. Standard plating procedures are technically challenging due to small lateral fragment and frequently require a second operation for implant removal. The cost of commercially available implants vary from ≤750 to ≤1450. This technique is quick, easy to perform, provides good primary stability, and comparable union rates with other techniques at an implant cost of <£120.
Conclusion:
This is a reproducible and efficient technique that provides comparable results with other established procedures at a fraction of the cost of the next cheapest implant. It is recommended for the treatment of displaced Type II clavicle fractures.
Level of Evidence:
Level IV.
Keywords: Coracoclavicular ligament rupture, lateral clavicle fracture, ligament reconstruction, Neer's Type II, parachute technique
Introduction
Lateral clavicle fractures account for nearly a quarter of all clavicle fractures.1,2,3 Epidemiologically, clavicle fractures have bipolar distribution, with a third occurring between 13 and 20 years; then, the incidence falls off and rises again in the old age. Various classifications have been published to describe the pattern of clavicle fracture;2,4,5,6 Neer's classification, described in 1982, is the most commonly used for distal clavicle fractures:5
Type I: Fracture lateral of coracoclavicular (CC) ligaments but no ligament damage, stable, minimally displaced
Type IIA: Fracture medial to CC ligaments which remain intact, unstable, displaced
Type II B: Fracture between CC ligaments with complete rupture of the conoid ligaments, very unstable, severely displaced
Type III: Intraarticular (stable).
Type IIB fractures being unstable are the most challenging to treat. Historically, these fractures were also treated conservatively such as Types I and III, and there are a few contemporary papers to support this approach. Robinson and Cairns published a paper in 2004,7 concluding that the outcomes of nonoperative treatment were not statistically different from surgical intervention for displaced lateral clavicle fractures in middle-aged and elderly patients. However, the degree of displacement and breakup of fracture pattern into specific subtypes was not specified. They also excluded patients with skin compromise. Some other contemporary papers3,8 show poor results with conservative treatment, with a quarter of patients complaining of pain at rest and one-third on activity. Almost half of the patients reported some symptoms at 6 months. The recent trend has, therefore, shifted to surgical management of these injuries.
Different surgical techniques have been described with some variations but follow the same underlying principle of bony fixation with some form of CC ligament reconstruction. Common problems encountered with traditional hardware include the prominence of metalwork necessitating removal, difficulty in surgical exposure of the clavicle and coracoid from the same approach, and variable CC ligament reconstruction techniques sometimes resulting in persistent instability of the acromioclavicular (AC) joint. Type IIB fracture can be essentially described as a soft-tissue injury to CC ligament. The remaining lateral clavicle is frequently comminuted and is not always strong enough to hold traditional hardware. Reconstructing the ligament provides sufficient indirect stability to the fracture itself, enabling union without the need for metallic plates and screws.
A modification of the under-coracoid-around-clavicle (UCAC) approach,9 the parachute technique, is described that includes primary repair or reconstruction of the ligament and anteroposterior stability provided by a separate synthetic ligament.
Surgical approach
The procedure is done under general anesthesia (GA) in beach chair position, with the image intensifier positioned on the other side of the table. The fracture is approached through a 4–5-cm strap incision, centered slightly medial to the protruding medial end of the clavicle. Skin edges are undermined to make a mobile window.
A T-shaped flap is raised from deltotrapezial fascia [Figure 1], with base over the anterior end of the clavicle. It is subperiosteally elevated to expose the lateral third of the clavicle and fracture, up to the AC joint (ACJ). Coracoid process is exposed by blunt dissection along the vertical limb of T-flap, through the anterior deltoid. In fresh injuries, CC ligaments are easily identifiable and can be imbricated with stay sutures for primary repair to clavicle in the end.
Figure 1.
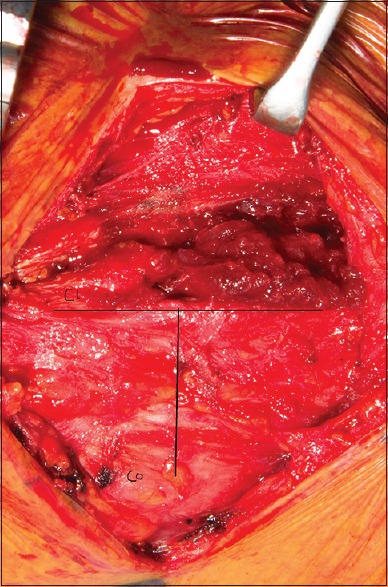
T-shaped deltotrapezial flap to expose coracoid
A long-curved hemostat is used for blunt dissection and creating a window on either side of the coracoid. No. 2 FiberTape and TigerTape (Arthrex, Naples, FL) are passed around the coracoid from medial to lateral using a coracoid passer or Lahey's forceps.
1.8-mm drill holes are made through the anatomical insertion of the conoid and trapezoid CC ligaments, pointing toward the coracoid [Figure 2]. The edges are beveled to minimize the risk of sharp bone edges cutting through the suture. In a fresh injury, usually, the ligament stump can be identified. Otherwise, the trapezoid tunnel is drilled around 2.5 cm and conoid tunnel 4.5 cm from the end of clavicle, as described by Rios et al.10 in their anatomical study. Both the ends of FiberTape (red in the figures) are delivered through the respective holes [Figure 3], along with the stay suture of the CC ligaments to be tied later. One end of the TigerTape (green in the figures) is delivered posterior to the clavicle. The fracture is now reduced under vision, and both ends of tape 1 are tied on top of the clavicle [Figure 4]. The suture through the CC ligaments can also be tied at this stage. Tape 2 is then tied to itself with slight overreduction of ACJ to protect the repair [Figure 4].
Figure 2.
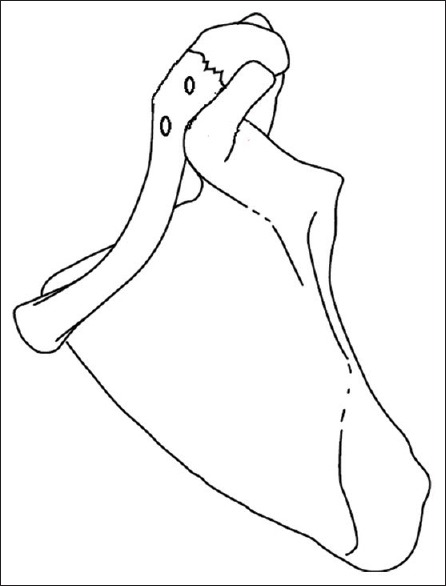
Drill holes
Figure 3.
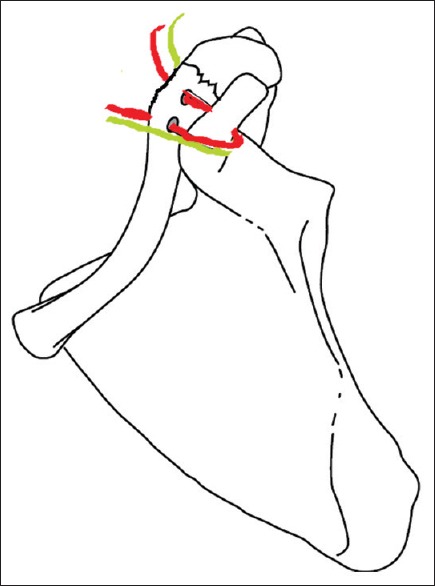
Passage of sutures under the coracoid. Red tape (tape 1) passed through the drill holes, and green tape (tape 2) passed behind the clavicle
Figure 4.
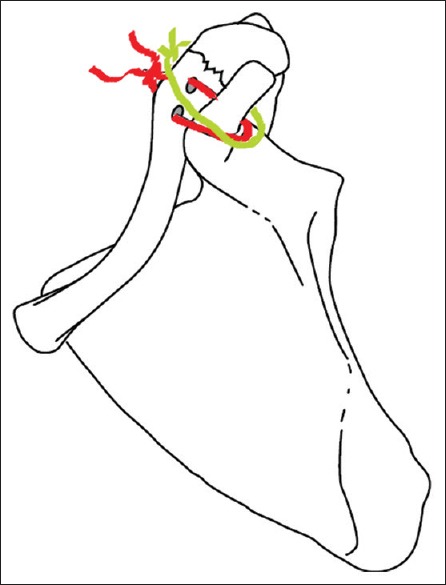
Sutures tied to stabilize the fracture
The lateral fragment is usually stable at this stage, and further stability can be achieved by using one of the tapes in tension band or cerclage configuration [Figures 5 and 6] or be excised if it is too small. The fascia and ACJ capsule are meticulously repaired, with subcuticular sutures used for skin.
Figure 5.
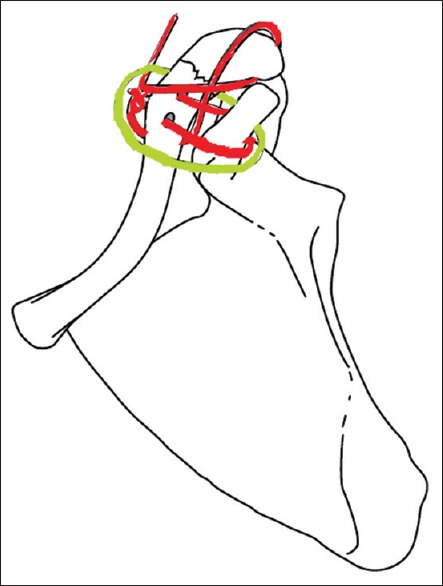
Optional cerclage fixation of the lateral fragment using the tape 1 after tying knot
Figure 6.
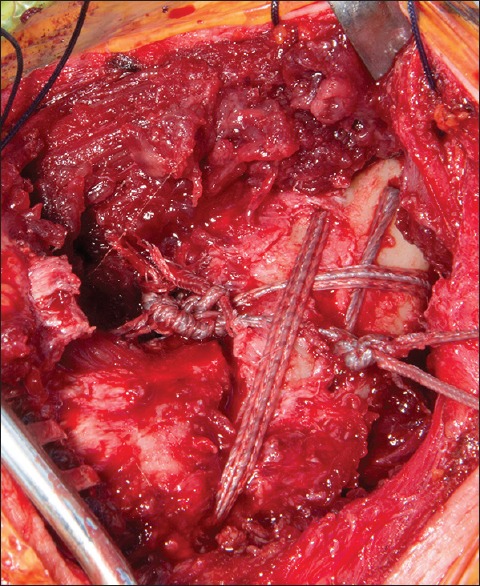
After completion of repair
Postoperatively, pendulum exercises can be started when comfortable, and full passive/active assisted range of motion (ROM) can be started as tolerated after 2 weeks. Sling is worn for 4 weeks. The aim is to regain full ROM by 6 weeks, and strengthening should be avoided in this period.
Methodology and Results
Nineteen consecutive patients with a minimum 6-month followup (FU) were reviewed. Average FU was 23 months (6–47 m), mean age was 38 years (16–81), and male-to-female ratio was 2:1. The most common mode of injury was fall from bicycle (54%). The time to surgery varied from 4 days to 12 weeks. All the patients underwent CC ligament reconstruction as per the standardized technique described above. Two patients had primary lateral end excision; of the rest, all but one healed fully.
Average time to regain full ROM was 4 weeks [Figures 7–9]; at 6 months postoperatively, the average Oxford Shoulder Score was 43. All the patients returned to their previous occupation and two-thirds to preinjury leisure activity. Average time to radiological healing was 8.2 weeks (7–12 weeks). Figures 10 and 11 show the preoperative and 6-week postoperative radiological appearance, respectively. One patient showed partial loss of reduction (presented 8 weeks postinjury after developing skin ulcer and had poor compliance postop), but this did not result in any functional impairment. There were no complications such as nerve injury, coracoid or clavicle fracture, ligament failure, infection, or stiffness.
Figure 7.

Flexion at 6 weeks
Figure 9.

Internal rotation at 6 weeks
Figure 10.
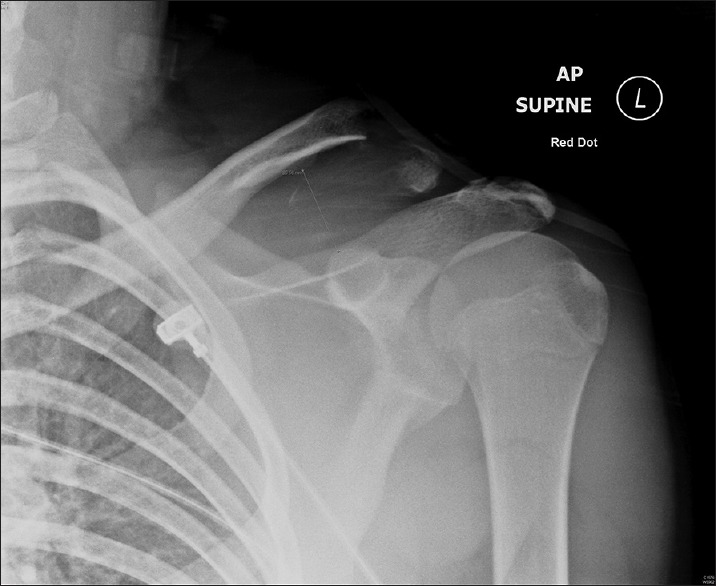
Preoperative X-ray
Figure 11.

X-ray at 6 weeks
Figure 8.

Abduction at 6 weeks
Discussion
Direct osteosynthesis in distal clavicle fractures can be technically challenging due to variable and usually inadequate bone stock of the distal fragment, which frequently precludes a strong enough fixation to enable early mobilization. It is also difficult to access the coracoid process through the direct horizontal approach usually needed for plate fixation. Inadequate exposure can, in turn, compromise the ligament reconstruction, which is in fact more critical toward a successful outcome than fracture healing alone. Persistent instability of lateral clavicle is a well-described complication if the fracture is addressed without ligament reconstruction. Numerous techniques have been devised over the years to deal with this challenge, but none can be called a gold standard.
Broadly, the fixation modalities can be divided in three groups:
Tension band and/or transarticular K-wire fixation through ACJ
Direct osteosynthesis using distal clavicle plates (±CC ligament augmentation) or hook plates
Indirect reduction using CC ligament reconstruction (Tightrope or Dog Bone technique, Surgilig, parachute technique etc) ± direct ligament repair.
Tension band and/or transarticular K-wire fixation
Transacromial fixation using K-wires has been used as a treatment modality for >70 years. It is technically easy and potentially less invasive than a plate but has been associated with high rates of hardware-related complications such as wire migration infection and postoperative ACJ arthritis.11 In addition, it did not address the CC ligament damage, resulting in persistent lateral clavicle instability even after fracture healing. This approach has been largely abandoned in modern-day practice.
Direct osteosynthesis using distal clavicle plates (±coracoclavicular ligament augmentation) or hook plates
The hook plate was introduced as an alternative to K-wire fixation around 25 years ago. Numerous publications over the years highlight the success, as well as potential problems with the use of this plate. It offers the advantage of a familiar surgical approach for general orthopedic or trauma surgeons and application of standard plating principles. A study in 2002 reported similar union rates after hook plate and K-wire fixation, but the former had significantly lower complication rates (6% vs. 55%).12 In 2006, Flinkkilä et al. reported 91% healing of fractures using hook plate in unstable lateral clavicle fractures.13 Numerous other contemporary studies have confirmed excellent union rates varying from 91% to 100% with the use of hook plates but also reported complication rates of 8% to 18%14,15,16,17 and a very high reoperation rate.
Acromion erosion and painful subacromial impingement are inevitable, and plate removal is recommended in all patients after the fracture has healed. This necessitates another GA and added expenses for another surgery.
Direct osteosynthesis of the distal clavicle using specialized angular stable plates that allow multiple locking screws to be placed in the small distal clavicle fragment has shown excellent union rates, while avoiding trauma to the ACJ and acromion.18,19 Unfortunately, these plates also have a high removal rate up to 40%–50% of cases20 and do not address the problem of CC ligament instability unless supplemented with some form of CC ligament reconstruction. Any surgical approach primarily directed toward plating also makes it difficult to access the coracoid through the same incision for ligament repair.
Indirect reduction using only coracoclavicular ligament reconstruction (synthetic ligaments or tendon grafts)
These techniques are based on the principle of indirect reduction and stabilization of fracture by CC ligament reconstruction, in effect converting the unstable Type II into a stable Type I pattern. Once stabilized in this manner, secondary fracture healing can be expected to proceed naturally. It is not a new concept – originally proposed in the 1990s, there is a lot of contemporaneous literature showing good results.8,9,21,22,23,24 Union rates in excess of 90% have been reported in most papers. A wide variety of nonabsorbable materials such as Dacron graft, polyethylene, and polyglactin or tendon grafts using palmaris longus or hamstrings have been used. The fixation technique is fairly consistent, by passing the graft Under Coracoid around clavicle (UCAC). Other soft-tissue repair techniques use suture anchors or buttons in the base of coracoid.
It works on the principle of reduced shearing forces at the fracture site by stabilizing proximal clavicle. A meta-analysis of 21 studies in 2013 by Stegeman et al.25 revealed fracture union rate of 98% after suture-only fixation. It also showed a 24-fold increased risk of complications after using hook plate, when compared with suture anchor-based methods. Reported complications with suture-only technique include knot slippage, loss of reduction, and suture prominence,26,27 along with the risk of coracoid fracture or loss of fixation from the suture anchor if used.
A recent biomechanical analysis comparing suture-only fixation, distal clavicle plates with or without CC ligament augmentation, and hook plates was published by Bishop et al.28 It did not show a significant difference in ultimate load to failure among all these groups. However, they showed that fixation failure with a plate construct was more likely to result in the need for additional surgery than failure of a suture-only construct.
Commercially available kits such as TightRope technique, double Endobutton technique (Arthrex Inc., Naples, Fl, USA),29 and Surgilig technique (Lockdown Medical, UK) enable secure fixation without traditional hardware. All these techniques have the advantage of minimal or no metalwork; as a result, there is minimal skin irritation and the rate of reoperation is reduced to almost zero. Endobutton technique needs limited dissection, can be done arthroscopically, and is more resistant to rotational forces by virtue of having four suture limbs. However, all the techniques described above are nonanatomical repair (linear fixation as opposed to the two limbs of natural ligament with separate insertion). The double Endobutton fixation may also be potentially compromised if the clavicle fracture extends medially.29 Moreover, it involves drilling through the coracoid, which can result in additional complications. The UCAC technique9 avoids this by looping the ligament around the coracoid rather than through it. Surgilig synthetic ligament is a type of UCAC repair providing very strong fixation but is also a nonanatomical repair as the ligament overreduces the clavicle anteroinferiorly, and there is a reported risk of osteolysis.30
The parachute technique has all the advantages of UCAC described above, and the modification allows a more anatomical repair. It supplements UCAC with a second more anatomical insertion of the ligaments through the native ligament footprint, thus providing a secure repair that restores a stable CC interval to enable early rehabilitation. Very small drill holes minimize the risk of stress fracture and anatomic repair of the CC ligaments where possible also allows biological healing of the native ligament and further reinforces the repair. As opposed to the use of strong sutures such as FiberWire,31 this technique uses suture tape, which has a wider surface area, thereby minimizing the risk of cutting through bone. Avoiding any button or similar hardware also minimizes risk of complications such as hardware prominence or osteolysis sometimes associated with other techniques. The same technique can also be modified for pure ACJ dislocations without fracture. There were no major complications in the current cohort, which compares favorably with other similar papers.
Financially, the parachute technique is considerably cheaper than any other modality. Commercially available implants mentioned above cost £750–£1450 in the UK. All the consumables in parachute technique taken together cost under £120. This is more than six times cheaper than the nearest commercially available kit and ten times cheaper than some plate + ligament constructs. The average surgical time was around 1 h, which is comparable or less than other techniques. The use of strap incision is also cosmetically better compared to the horizontal incision needed for the plate fixation. Furthermore, none of the patients needed to go back to theater for implant removal or loss of fixation, which compares very well with plating procedures that have relatively high reoperation rate for implant removal. Potential contraindications for this procedure include a fractured coracoid, patient unfit for surgery, and fracture extending beyond the insertion of the conoid ligament.
Limitations of the study
One disadvantage of this study is the relatively short FU with an average period of 2 years. However, it is long enough to assess the fracture healing rates and assess early complications if any. Second, it is a small sample of nonrandomized prospective study, therefore prone to selection bias and unsuitable for multivariate analysis. The sample size is, however, comparable or larger than many published papers.20,29,32,33,34 It is very encouraging that all the fractures healed by 3 months, and no short term complications such as ligament rupture, nerve injury, joint instability, or bone erosion have been seen. However, there is a learning curve to the procedure, and long term FU will be needed to conclusively prove its efficacy and assess delayed complications such as osteolysis.
Conclusion
Parachute technique is a reproducible and efficient procedure that provides comparable results with other established procedures, at a fraction of the cost. It is recommended for the treatment of displaced Type II clavicle fractures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
Help from the following individuals is gratefully acknowledged: (1) Mr. Sanjay Sinha MRCS – help with data collection, (2) Mr. Christian Butaliu MRCS – help with data collection, and (3) Mr. Amr Elseehy MRCS – help with data collection.
References
- 1.Nordqvist A, Petersson C, Redlund-Johnell I. The natural course of lateral clavicle fracture 15 (11-21) year followup of 110 cases. Acta Orthop Scand. 1993;64:87–91. doi: 10.3109/17453679308994539. [DOI] [PubMed] [Google Scholar]
- 2.Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80:476–84. doi: 10.1302/0301-620x.80b3.8079. [DOI] [PubMed] [Google Scholar]
- 3.Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: A prospective study of 222 patients. Acta Orthop. 2005;76:496–502. doi: 10.1080/17453670510041475. [DOI] [PubMed] [Google Scholar]
- 4.Craig E, editor. Philadelphia, USA: 1990. The Shoulder: WB Saunders and Co. [Google Scholar]
- 5.Neer CS., 2nd Fractures of the distal third of the clavicle. Clin Orthop Relat Res. 1968;58:43–50. [PubMed] [Google Scholar]
- 6.Allman FL., Jr Fractures and ligamentous injuries of the clavicle and its articulation. J Bone Joint Surg Am. 1967;49:774–84. [PubMed] [Google Scholar]
- 7.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am. 2004;86-A:778–82. doi: 10.2106/00004623-200404000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Webber MC, Haines JF. The treatment of lateral clavicle fractures. Injury. 2000;31:175–9. doi: 10.1016/s0020-1383(99)00276-4. [DOI] [PubMed] [Google Scholar]
- 9.Soliman O, Koptan W, Zarad A. Under-coracoid-around-clavicle (UCAC) loop in type II distal clavicle fractures. Bone Joint J. 2013;95-B:983–7. doi: 10.1302/0301-620X.95B7.31316. [DOI] [PubMed] [Google Scholar]
- 10.Rios CG, Arciero RA, Mazzocca AD. Anatomy of the clavicle and coracoid process for reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2007;35:811–7. doi: 10.1177/0363546506297536. [DOI] [PubMed] [Google Scholar]
- 11.Lee YS, Lau MJ, Tseng YC, Chen WC, Kao HY, Wei JD, et al. Comparison of the efficacy of hook plate versus tension band wire in the treatment of unstable fractures of the distal clavicle. Int Orthop. 2009;33:1401–5. doi: 10.1007/s00264-008-0696-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flinkkilä T, Ristiniemi J, Hyvönen P, Hämäläinen M. Surgical treatment of unstable fractures of the distal clavicle: A comparative study of kirschner wire and clavicular hook plate fixation. Acta Orthop Scand. 2002;73:50–3. doi: 10.1080/000164702317281404. [DOI] [PubMed] [Google Scholar]
- 13.Flinkkilä T, Ristiniemi J, Lakovaara M, Hyvönen P, Leppilahti J. Hook-plate fixation of unstable lateral clavicle fractures: A report on 63 patients. Acta Orthop. 2006;77:644–9. doi: 10.1080/17453670610012737. [DOI] [PubMed] [Google Scholar]
- 14.Shin SJ, Ko YW, Lee J, Park MG. Use of plate fixation without coracoclavicular ligament augmentation for unstable distal clavicle fractures. J Shoulder Elbow Surg. 2016;25:942–8. doi: 10.1016/j.jse.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 15.Yoon JP, Lee BJ, Nam SJ, Chung SW, Jeong WJ, Min WK, et al. Comparison of results between hook plate fixation and ligament reconstruction for acute unstable acromioclavicular joint dislocation. Clin Orthop Surg. 2015;7:97–103. doi: 10.4055/cios.2015.7.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kashii M, Inui H, Yamamoto K. Surgical treatment of distal clavicle fractures using the clavicular hook plate. Clin Orthop Relat Res. 2006;447:158–64. doi: 10.1097/01.blo.0000203469.66055.6a. [DOI] [PubMed] [Google Scholar]
- 17.Muramatsu K, Shigetomi M, Matsunaga T, Murata Y, Taguchi T. Use of the AO hook-plate for treatment of unstable fractures of the distal clavicle. Arch Orthop Trauma Surg. 2007;127:191–4. doi: 10.1007/s00402-006-0284-5. [DOI] [PubMed] [Google Scholar]
- 18.Fleming MA, Dachs R, Maqungo S, du Plessis JP, Vrettos BC, Roche SJ, et al. Angular stable fixation of displaced distal-third clavicle fractures with superior precontoured locking plates. J Shoulder Elbow Surg. 2015;24:700–4. doi: 10.1016/j.jse.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 19.Herrmann S, Schmidmaier G, Greiner S. Stabilisation of vertical unstable distal clavicular fractures (Neer 2b) using locking T-plates and suture anchors. Injury. 2009;40:236–9. doi: 10.1016/j.injury.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 20.Largo RD, Rudin MA, Hotz TK, Valderrabano V, Käch KK. Anatomic reconstruction of unstable lateral clavicular fractures. J Trauma. 2011;71:1348–51. doi: 10.1097/TA.0b013e3182095dd1. [DOI] [PubMed] [Google Scholar]
- 21.Othman A. Internal fixation of lateral clavicle fractures with vicryl tape. Eur J Orthop Surg Traumatol. 2002;12:129–31. doi: 10.1007/s00590-002-0034-5. [DOI] [PubMed] [Google Scholar]
- 22.Robinson CM, Akhtar MA, Jenkins PJ, Sharpe T, Ray A, Olabi B, et al. Open reduction and endobutton fixation of displaced fractures of the lateral end of the clavicle in younger patients. J Bone Joint Surg Br. 2010;92:811–6. doi: 10.1302/0301-620X.92B6.23558. [DOI] [PubMed] [Google Scholar]
- 23.Chen CH, Chen WJ, Shih CH. Surgical treatment for distal clavicle fracture with coracoclavicular ligament disruption. J Trauma. 2002;52:72–8. doi: 10.1097/00005373-200201000-00013. [DOI] [PubMed] [Google Scholar]
- 24.Goldberg JA, Bruce WJ, Sonnabend DH, Walsh WR. Type 2 fractures of the distal clavicle: A new surgical technique. J Shoulder Elbow Surg. 1997;6:380–2. doi: 10.1016/s1058-2746(97)90006-9. [DOI] [PubMed] [Google Scholar]
- 25.Stegeman SA, Nacak H, Huvenaars KH, Stijnen T, Krijnen P, Schipper IB, et al. Surgical treatment of neer type-II fractures of the distal clavicle: A meta-analysis. Acta Orthop. 2013;84:184–90. doi: 10.3109/17453674.2013.786637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Flinkkilä T, Heikkilä A, Sirniö K, Pakarinen H. TightRope versus clavicular hook plate fixation for unstable distal clavicular fractures. Eur J Orthop Surg Traumatol. 2015;25:465–9. doi: 10.1007/s00590-014-1526-9. [DOI] [PubMed] [Google Scholar]
- 27.Takase K, Kono R, Yamamoto K. Arthroscopic stabilization for neer type 2 fracture of the distal clavicle fracture. Arch Orthop Trauma Surg. 2012;132:399–403. doi: 10.1007/s00402-011-1455-6. [DOI] [PubMed] [Google Scholar]
- 28.Bishop JY, Roesch M, Lewis B, Jones GL, Litsky AS. A biomechanical comparison of distal clavicle fracture reconstructive techniques. Am J Orthop (Belle Mead NJ) 2013;42:114–8. [PubMed] [Google Scholar]
- 29.Struhl S, Wolfson TS. Closed-loop double endobutton technique for repair of unstable distal clavicle fractures. Orthop J Sports Med. 2016;4(7):2325967116657810. doi: 10.1177/2325967116657810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sarda P, Richards AM, Corbett SA. Bone osteolysis following acromioclavicular joint reconstruction using synthetic ligament (Surgilig™) Shoulder Elbow. 2014;6:40–3. doi: 10.1111/sae.12035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kanchanatawan W, Wongthongsalee P. Management of acute unstable distal clavicle fracture with a modified coracoclavicular stabilization technique using a bidirectional coracoclavicular loop system. Eur J Orthop Surg Traumatol. 2016;26:139–43. doi: 10.1007/s00590-015-1723-1. [DOI] [PubMed] [Google Scholar]
- 32.Cho CH, Jung JH, Kim BS. Coracoclavicular stabilization using a suture button device for neer type IIB lateral clavicle fractures. J Shoulder Elbow Surg. 2017;26:804–8. doi: 10.1016/j.jse.2016.09.048. [DOI] [PubMed] [Google Scholar]
- 33.Levy O. Simple, minimally invasive surgical technique for treatment of type 2 fractures of the distal clavicle. J Shoulder Elbow Surg. 2003;12:24–8. doi: 10.1067/mse.2003.128564. [DOI] [PubMed] [Google Scholar]
- 34.Bezer M, Aydin N, Guven O. The treatment of distal clavicle fractures with coracoclavicular ligament disruption: A report of 10 cases. J Orthop Trauma. 2005;19:524–8. doi: 10.1097/01.bot.0000164593.04348.e5. [DOI] [PubMed] [Google Scholar]


