Abstract
Background:
Avascular necrosis (AVN) of the femoral head usually occurs in the third to fifth decade. The treatment options depend on the stage of disease varying from nonoperative treatment to surgical procedure including core decompression (CD) with or without nonvascularized or vascularized fibular graft, muscle pedicle bone grafting, osteotomies, and arthroplasty. Finite life of the total hip arthroplasty (THA) prosthesis limits its use in young adults or in middle aged. In this study, we envisage to evaluate the clinicoradiological outcomes of CD and nonvascularized fibular grafting in early stages of AVN femoral head.
Materials and Methods:
Our study is longitudinal observational study including 76 hips (46 patients) in the age group of 18–48 years (mean 30.07 years). Ficat and Arlet staging system was used and only early stages, that is, Stage 1 (n = 36 hips) and Stage 2 (n = 40 hips) were included in the study. The cases with traumatic AVN were excluded. All patients in Stage 1 underwent CD (Group 1) and those in Stage 2 underwent CD and fibular grafting (Group 2). Preoperative Harris Hip Score (HHS), visual analog score (VAS), plain radiographs, and magnetic resonance imaging (MRI) were compared with serial postoperative HHS, VAS, plain radiographs, and MRI taken at different intervals.
Results:
Average period of followup was 53.5 months (44–63 months). Radiological progression was not seen in 55 hips out of 76 hips (72.3%), whereas 21 hips (27.6%) demonstrated signs of progression and collapse. Failure of surgery was defined as progression of the disease, which was 25% (n = 9) in Group 1and 30% (n = 12) Group 2. Median values of HHS at the end of the followup in Group 1 was 77 and in Group 2 was 71.5 compared to the preoperative HHS of 48 and 62 in Group 1 and 2, respectively. Median values of VAS at the end of the followup in Stage 1 was 0 and in Stage 2 was 2 compared to the preoperative VAS of 6 and 8 in Group 1 and Group 2, respectively.
Conclusion:
CD with or without fibular grafting is effective in preserving the sphericity of the femoral head and to delay the progression of the AVN of femoral head in the early stages, that is, Stage 1 and Stage 2 and aids in the early revascularization of ischemic femoral head and is a useful modality to negate or delay the requirement of THA.
Keywords: Avascular necrosis femoral head, core decompression, nonvascularized fibular grafting
Introduction
Avascular necrosis (AVN) of the hip is a condition caused by interruption in the blood supply to the subchondral region of the head of the femur leading to death of the osteoblasts and osteocytes. It can be posttraumatic, alcohol or steroid induced, and idiopathic variety.1 It usually affects the young population (third to fifth decade) and has been found to be responsible for 5%–12% of hip replacements.2 Such a necrotic bone is not able to bear compressive stresses and if not treated, generally progress to collapse leading to loss of sphericity of the head and eventually secondary osteoarthritis. Various diagnostic modalities are now available to diagnose it early among which magnetic resonance imaging (MRI) stands out as the standard tool. Apart from being more sensitive and specific when compared to other diagnostic modalities, it also helps to diagnose the condition even in the presymptomatic stage when there are no changes on plain radiographs.3
There is a wide range of treatment modalities available but still the management of AVN of femoral head remains controversial. The medical treatment includes nonsteroidal anti-inflammatory drugs, bisphosphonates, hyperbaric oxygen therapy, and extracorporeal shock wave therapy, but their role has been shown to be ineffective.4 On the other hand, surgical options are femoral head preserving or hip salvaging procedures and hip replacement procedures.
Preservation of femoral head delays the replacement procedures which have finite lifespan. Hence, femoral head-preserving procedures should be considered for the management of properly selected patients in order to delay the arthroplasty. Nevertheless, preservation of head allows for floor level activities which are required for Indian population. Therefore, we envisage to analyze the clinical outcome and radiological outcomes after core decompression (CD) and CD with nonvascularized fibular grafting.
Materials and Methods
This prospective longitudinal observational study was carried out in our institute between November 2014 and December 2017.
Ethical clearance was obtained from the Ethical Committee of the institution.
Adults of age 18–50 years with Stage 1 and 2 of Ficat and Arlet classification were included for the study.
Hip diseases with local site infection, patients with traumatic etiology, psychiatric patients, and patients with comorbidities were excluded from the study. The diagnosis of AVN was made based on the clinical and radiological investigations, that is, X-ray and MRI [Figures 1–3].
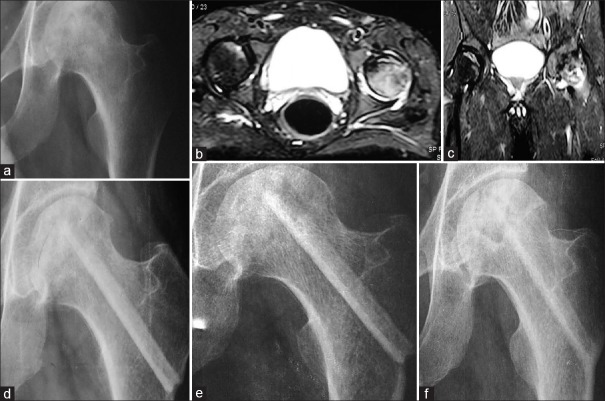
Figure 1.
(a) Preoperative X-ray of a 24-year-old male with bilateral steroid induced avascular necrosis, left side – Ficat and Arlet Stage 2. (b and c) T2 images of axial section and coronal section of magnetic resonance imaging showing bilateral disease. (d) Immediate postoperative X-ray after core decompression and fibular grafting procedure showing fibular graft. (e and f) Fifty eight months followup X-ray AP view and frog-legged lateral view demonstrating intact sphericity of the femoral head, that is, Ficat and Arlet Stage 2
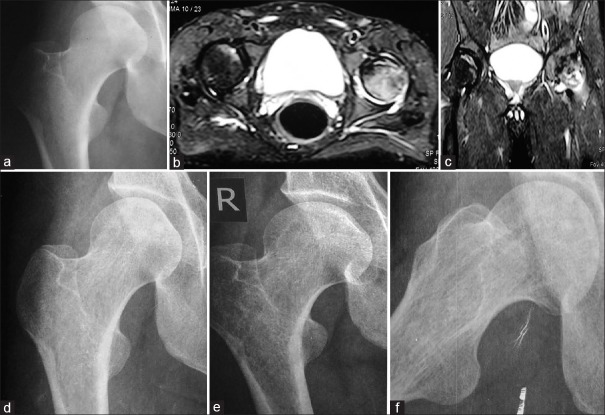
Figure 3.
A 44-year-old male with idiopathic avascular necrosis on the right side (unilateral disease) in Ficat and Arlet Stage 2. (b and c) T2 image of coronal section and axial section of magnetic resonance imaging showing hypointense lesion in the femoral head and edema. (d) Immediate postoperative X-ray after core decompression and fibular grafting showing the graft. (e) Ten months followup X-ray, AP view demonstrating intact sphericity of the femoral head. (f) Twenty two months followup X-ray frog-legged lateral view showing loss of sphericity of the femoral head, that is, Ficat and Arlet Stage 3
Figure 2.
(a) Preoperative X-ray of the right hip, Ficat and Arlet Stage 1 avascular necrosis in a steroid-induced patient. (b and c) T2 images of axial section and coronal section of magnetic resonance imaging showing bilateral disease hypointense lesion, edema, and collection. (d) Immediate postoperative X-ray following core decompression, showing tracts of core decompression. (e and f) Fifty eight months followup X-ray AP view and frog-legged lateral view demonstrating intact sphericity of the femoral head, that is, Ficat and Arlet Stage 1
A total of 76 hips (n = 46 patients) were identified as being eligible for the study. The average age of the patients was 30 years (range 18–48 years). 38 males with 64 hips (82.6%) and 8 female patients with 12 hips (17.3%) were included in the study and the sex ratio being 3:1. Out of 76 hips, 52 hips had involvement of the right side (68.4%). 30 patients (65.2%) had bilateral involvement out of which 26 patients (56.5%) presented with symptoms pertaining to only one hip the other hip was in Stage 1. Sixteen patients (34.7%) had unilateral involvement.
A detailed history regarding pain and visual analog score (VAS), drug history of steroid intake, smoking and alcohol intake, and history suggestive of coagulation disorders were taken. General examination and systemic examination in detail were done. Local examination of both the hip joints for gait abnormality and restriction of movements were assessed. Blood investigations such as complete blood count and peripheral smear, liver function tests, kidney function tests, random blood sugar, and coagulation profile were done.
X-rays of the pelvis with bilateral hip of anteroposterior view and frog-leg lateral view was obtained. We used Ficat and Arlet classification system for staging.5 Baseline HHS and VAS were recorded. CD was done in Stage 1 (n = 36) and CD with fibular grafting was done in Stage 2 (n = 40). All the surgeries were done by two senior orthopedic consultants and X-rays and MRI were read by the same two senior orthopedic consultants (AKJ and IKD).
Operative procedure
The surgeries were done under spinal anesthesia, in supine position on a fracture table and under image intensifier. The lateral femoral cortex was exposed through a short linear incision. Fascia lata and vastus lateralis muscle was divided in line with their fibers and identify the flare of the greater trochanter. A small drill hole was placed in the mid-lateral cortex and entry point was just proximal to the level of lesser trochanter to avoid stress fractures. Small guidewire was inserted through this hole into the center of the lesion in the femoral head. With the help of the triple reamer (8 mm) of dynamic hip screw which is slowly advanced into the lesion and necrosed bone was removed and sample was sent for biopsy. Autograft of fibula was obtained with the help of curette, proximal end was tapered and distal end was rounded, and multiple drill holes were made in the graft. The appropriate length of the graft was measured from the reverse measuring device. Graft was passed through the lateral cortex to place up into the head with the proximal end just underneath the subchondral bone within 5 mm from the outer cortex, in the area of the lesion. Closure was done in layers.
Check X-ray was obtained on postoperative day 1 and VAS was recorded. In postoperative period, absolute nonweight bearing regimen was followed with traction of 2 kg throughout the day for first 1 week and during night times for next 2 weeks. Active assisted range of motion exercises were started after 1 week.
Clinicoradiological followup was done at 1 week, 2 weeks, 4 weeks, 12 weeks, 6th month, and subsequently every 6 months. One week after discharge, patient was evaluated for surgical site infection and VAS score was recorded. Serial X-rays were obtained at the interval of 2 weeks, 4 weeks, 12 weeks and 6 months and at every 6 months and MRI was done after 3 years in all cases, which was compared with the preoperative plain radiographs and MRI for signs of revascularization and preservation of sphericity of the femoral head. Outcome in terms of functional improvement was assessed with the comparison of the serial VAS scores and Harris Hip Scores (HSSs).
The average followup was 53.5 months (range 44–63 months).
Statistical analysis
The information collected on the questionnaires were entered into Microsoft Excel and after data cleaning, the data were transferred and further analyzed using SPSS software version 20.0 (IBM, Chicago, USA). These outcome variables were found to be skewed, hence median values were considered and statistical analysis was done using nonparametric test. The preoperative HSSs and VAS scores were compared with that of HSSs and VAS scores at serial intervals of followup using Friedman's two-way analysis of variance by ranks.
Results
Out of 76 hips, 42 hips (55.26%) were in Stage 2 signifying that Stage 2 is the most common stage in which patient presents to the clinician followed by 34 hips in Stage 1 (44.73%). Median values of HHS at the end of the followup in Group 1 [Table 1] was 77 and in Group 2 [Table 2] was 71.5 compared to the preoperative HHS of 48 and 62 in Group 1 and 2, respectively. Median values of VAS at the end of the followup in Stage 1 was 0 and in Stage 2 was 2 compared to the preoperative VAS of 6 and 8 in Group 1 [Table 1] and Group 2 [Table 2], respectively. Combined HSS was found to be excellent (<90) in 6 hips, good (80–89) in 24 hips, fair (70–79) in 32 hips, and poor (<69) in 14 hips [Table 3]. Fifty-five hips (71%) out of 76 hips showed no signs of progression of the disease or signs of collapse, whereas 21 hips (27.6%) demonstrated signs of progression and collapse. Out of 21 hips, 12 were in Stage 2 and 9 were in Stage 1 on initial assessment. Among the 9 hips that failed in Group 1, 6 hips progressed to Stage 2, 2 hips progressed to Stage 3, and 1 hip to Stage 4. Whereas among the 12 hips that failed in Group 2, 8 hips progressed to Stage 3 and 4 hips progressed to Stage 4, at an average followup of 53.5 months. Fifty percentage of the total steroid induced cases showed progression the disease as compared to 11.4% of the idiopathic cases whereas no failure was seen among the alcohol-induced group [Table 4]. Among the type of surgical procedure done, CD and fibular grafting have higher number of failures, that is, 30% followed by CD 25% [Table 5].
Table 1.
Median values of Harris Hip score and visual analog score of patients in Group 1
| Clinical parameters | Preoperative | Postoperative | P |
|---|---|---|---|
| HHS | 48 (44-60) | 77 (61-88) | 0.007 |
| VAS | 6 (3-7) | 0 (0-2.75) | 0.008 |
HHS=Harris Hip Score, VAS=Visual analog score
Table 2.
Median values of Harris Hip Score and visual analog score of patients in group 2
| Clinical parameters | Preoperative | Postoperative | P |
|---|---|---|---|
| HHS | 63 (54.25-65) | 71.5 (61-88) | 0.0013 |
| VAS | 8 (0-10) | 2 (0-6) | 0.067 |
HHS=Harris Hip Score, VAS=Visual analog score
Table 3.
Combined Harris Hip Score of all the patients
| Harris Hip Score | No. of hips |
|---|---|
| Excellent (>90) | 6 hips |
| Good (80-89) | 24 hips |
| Fair (70-79) | 32 hips |
| Poor (<69) | 14 hips |
Table 4.
Etiological distribution of cases of avascular necrosis of femoral head
| Etiology | Total patients | Total hips | Percentage | Failures (%) |
|---|---|---|---|---|
| Idiopathic | 25 patients | 35 hips | 46 | 4 hips (11.4) |
| Steroid-induced AVN | 12 patients | 30 hips | 39.4 | 15 hips (50) |
| Alcohol-induced AVN | 9 patients | 11 hips | 14.4 | 0 hips |
AVN=Avascular necrosis
Table 5.
Distribution of cases that showed progression
| Stage | Surgical procedure | Total hips | Total failure | Percentage of failure |
|---|---|---|---|---|
| Stage 1 | Core decompression | 36 hips (47.3) | 9 hip | 25 |
| Stage 2 | Core decompression with fibular grafting | 40 hips (52.6) | 12 hips | 30 |
Discussion
It has been established in the literature that early diagnosis and treatment leads to better outcome in AVN of the femoral head.3 Various diagnostic modalities are now available to diagnose it early among which MRI stands out as the standard tool. Apart from being more sensitive and specific when compared to other diagnostic modalities, it also helps to diagnose the condition even in the presymptomatic stage when there are no changes on plain radiographs.3
Frequency of the type of surgery done for AVN of the femoral head is not uniform in the literature which means that there is no consensus on which is the best surgery to delay the progression of the disease. In our study, CD was done in 36 hips (Stage 1) whereas CD with fibular grafting (Stage 2) was done in 40 hips.Babhulkar5 (n = 345) reported 88.4% of the patients underwent CD with bone grafting for Stage 1, Stage 2, and Stage 3 and 7.2% of the patients underwent CD alone for Stage 0 and 1. Whereas in a study by Tsai et al.6 (1153 hips), CD procedure was done for Stage 1 and Stage 2 whereas Stage 3 and Stage 4 arthroplasty was done and CD with bone grafting was not done at all.
There was no statistically significant change between preoperative HSS and scores of 3-month followup (P = 0.673). This finding can be substantiated by the fact that the patient was given complete bed rest for initial 3 months in the postoperative period and hence the patient is functionally inactive. However, a statistically significant change was noted in both scores of 3 months versus 6 months (P = 0.024) and preoperative versus 6 months (P = 0.010) as the patient was allowed to mobilize after 3 months of operation and was allowed to do household activities as well as occupational activities. The functional improvement is directly correlated with the length of followup.
Babhulkar5 (n = 345 hips) reported the results of femoral head preserving surgeries based on HSS to be very good in 95 hips (27.5%), good in 135 hips (39.1%), medium in 36 hips (10.3%), fair in 65 hips (18.8%), and poor results in 14 hips (4%). Marker et al.7 (n = 52 patients) reported the outcome of CD to be excellent results in 48%, good results in 13%, fair results in 1%, and poor outcome in 38% and similar results were found by Shah et al.8
To best of our knowledge, there is no long term study that compares the results of CD with that of CD with nonvascularized fibular graft. However, there are numerous studies comparing the effectiveness of CD with that of the conservative therapy and studies with followup results of CD alone. Despite numerous studies, assessment of success rate of CD is difficult to determine because of differences among studies with regard to selection of patients (i.e., differences in patient diagnoses), classification systems, operative procedures, postoperative management, and evaluation of clinical outcome.9
Stulberg et al.10 (n = 55 hips) did an RCT comparing the results of CD with conservative treatment, using HHS. CD was successful in 70% in Ficat Stage 1, 2, or 3 whereas the results of the cases managed conservatively was only 20% successful in Ficat Stage 1, 0% in Stage 2, and 10% in Stage 3 and concluded that CD is effective than conservative therapy. His result was also supported by Smith et al.11 (n = 702), in which he reviewed 12 articles published between 1979 and 1991 with mean followup of 38 months and reported that cases treated with CD had 78% success in Stage 1, 62% in Stage 2, and 41% in Stage 3 in comparison with that of the cases treated with conservative therapy. Similar results were also seen by Mont et al.12 (n = 1206 hips) with 71% success rate in Ficat Stage 1 and 2 as compared to that of the conservative therapy with 35% success rate. These results are consistent with the result of our study, that is, 75% success with CD alone and proves that the CD modality of treatment for AVN of the femoral head is effective in the precollapse stage of the femoral head.
Steinberg13 did a retrospective study (n = 297) on patients treated with CD with bone grafting, they used University of Pennsylvania classification and with an average followup of 24 months. They reported 78% success in Stage 1A and 2A and 60% success in Stage 1B, 2B, and 2C. This result is similar to our study, that is, with a success rate of 70% in Ficat Stage 2. Similar results were seen in study by Stulberg et al.14 (n = 36) where the results of CD was documented to be 70% in Stage 1, 71% in Stage 2, and 73% in Stage 3.83% success rate was seen in study by Mont et al.15 (n = 30 hips) and in a similar study by Boettcher et al.16 (n = 55 hips) where 79% of success was seen with followup of 8 years.
Contrary to our results was reported by Smith et al.17 (n = 114 hips) where 66.5% of failure was seen in Stage 2 and 100% failure in Stage 3. The reason for the poor results by Smith et al. can be explained by the fact that, CD was done even in Stage 3 where the femoral head has already collapsed. CD procedure delays the femoral head collapse and subsequent arthritis, but it does not completely stops the progression of the disease, as the length of followup increases the number of failures also increases.2
Conclusion
CD with or without fibular grafting in early stages, that is, Stage 1 and Stage 2 of AVN of femoral head is an effective modality to delay the progression of the disease, postpone the femoral head collapse and eventual arthritis, and also helps in revascularization of the femoral head. However, it requires a long term, multicentric, level I studies to confirm the results.
Limitations of the study
Long term results are to be evaluated to assess the outcome of the procedure and multicentric level I studies are required in order to reach the final conclusion. Further, large sample size is required.
Declaration of patient consent
We certify that we have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Protection of patients’ rights to privacy
This study does not contain any information or data such as written descriptions, photographs, sonograms, computed tomography scans, and pedigrees that reveals the identity of a patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Dr. MP Singhm, professor, Department of Orthopaedics, UCMS and GTB hospital for expert guidance in interpretation of the data. Dr Rehan-Ul-Haq, professor, Department of Orthopaedics, UCMS and GTB hospital for help as a part of the surgical team.
References
- 1.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: Ten years later. J Bone Joint Surg Am. 2006;88:1117–32. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 2.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, et al. Osteonecrosis of the hip: Management in the 21st century. Instr Course Lect. 2003;52:337–55. [PubMed] [Google Scholar]
- 3.Nam KW, Kim YL, Yoo JJ, Koo KH, Yoon KS, Kim HJ, et al. Fate of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 2008;90:477–84. doi: 10.2106/JBJS.F.01582. [DOI] [PubMed] [Google Scholar]
- 4.Tripathy SK, Goyal T, Sen RK. Management of femoral head osteonecrosis: Current concepts. Indian J Orthop. 2015;49:28–45. doi: 10.4103/0019-5413.143911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babhulkar S. Osteonecrosis: Early diagnosis, various treatment options and outcome in young adults. Indian J Orthop. 2006;40:138–46. [Google Scholar]
- 6.Tsai SW, Wu PK, Chen CF, Chiang CC, Huang CK, Chen TH, et al. Etiologies and outcome of osteonecrosis of the femoral head: Etiology and outcome study in a Taiwan population. J Chin Med Assoc. 2016;79:39–45. doi: 10.1016/j.jcma.2015.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008;466:1093–103. doi: 10.1007/s11999-008-0184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah SN, Kapoor CS, Jhaveri MR, Golwala PP, Patel S. Analysis of outcome of avascular necrosis of femoral head treated by core decompression and bone grafting. J Clin Orthop Trauma. 2015;6:160–6. doi: 10.1016/j.jcot.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mont MA, Jones LC, Sotereanos DG, Amstutz HC, Hungerford DS. Understanding and treating osteonecrosis of the femoral head. Instr Course Lect. 2000;49:169–85. [PubMed] [Google Scholar]
- 10.Stulberg BN, Davis AW, Bauer TW, Levine M, Easley K. Osteonecrosis of the femoral head. A prospective randomized treatment protocol. Clin Orthop Relat Res. 1991;268:140–51. [PubMed] [Google Scholar]
- 11.Smith SW, Fehring TK, Griffin WL, Beaver WB. Core decompression of the osteonecrotic femoralhead. J Bone Joint Surg Am. 1995;77:674–80. doi: 10.2106/00004623-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Mont MA, Carbone JJ, Fairbank AC. Core decompression versus nonoperative management for osteonecrosis of the hip. Clin Orthop Relat Res. 1996;324:169–78. doi: 10.1097/00003086-199603000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg ME. Core decompression. Semin Arthroplasty. 1998;9:213–20. [Google Scholar]
- 14.Stulberg BN, Singer R, Goldner J, Stulberg J. Uncemented total hip arthroplasty in osteonecrosis: A 2- to 10-year evaluation. Clin Orthop Relat Res. 1997;334:116–23. [PubMed] [Google Scholar]
- 15.Mont MA, Einhorn TA, Sponseller PD, Hungerford DS. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br. 1998;80:56–62. doi: 10.1302/0301-620x.80b1.7989. [DOI] [PubMed] [Google Scholar]
- 16.Boettcher WG, Bonfiglio M, Smith K. Non-traumatic necrosis of the femoral head. II. Experiences in treatment. J Bone Joint Surg Am. 1970;52:322–9. [PubMed] [Google Scholar]
- 17.Smith KR, Bonfiglio M, Montgomery WJ. Non-traumatic necrosis of the femoral head treated with tibial bone-grafting. A followup note. J Bone Joint Surg Am. 1980;62:845–7. [PubMed] [Google Scholar]