Abstract
Human papillomaviruses (HPVs) infect the epithelia of skin or mucosa, where they can induce hyperproliferative lesions. More than 220 different HPV types have been characterized and classified into five different genera. Mucosal high-risk HPVs are causative for cancers of the anogenital region and oropharynx. Clinical data from patients with the rare genetic disorder epidermodysplasia verruciformis (EV) indicate that genus beta-HPVs cooperate with ultraviolet (UV) radiation in the development of cutaneous squamous cell carcinoma. In addition, epidemiological and biological findings indicate that beta-HPV types play a role in UV-mediated skin carcinogenesis also in non-EV individuals. However, the mechanisms used by these cutaneous viruses to promote epithelial carcinogenesis differ significantly from those of mucosal HPVs. Recent studies point to a delicate cross-talk of beta-HPVs with the cell-autonomous immunity of the host keratinocytes and the local immune microenvironment that eventually determines the fate of cutaneous HPV infection and the penetrance of disease. This review gives an overview of the critical interactions of genus beta-HPVs with the local immune system that allow the virus to complete its life cycle, to escape from extrinsic immunity, and eventually to cause chronic inflammation contributing to skin carcinogenesis.
This article is part of the theme issue ‘Silent cancer agents: multi-disciplinary modelling of human DNA oncoviruses’.
Keywords: beta-HPVs, immune system, inflammation, cutaneous squamous cell carcinoma, epidermodysplasia verruciformis, organ transplant recipients
1. Introduction
Human papillomaviruses (HPVs) are double-stranded DNA viruses that infect mucosal and cutaneous epithelia. They form a large family that includes more than 220 HPV types [1]. A subgroup of HPVs is clearly associated with the development of neoplasia in the anogenital and upper respiratory tracts. They are classified as mucosal high-risk (HR) HPV types and belong to the genus alpha of the HPV phylogenetic tree [1].
HPV types belonging to genus beta have a cutaneous tropism and are subdivided into five species (beta-1–5) [1]. Genetically, they differ from other HPV genera, in that they lack E5 or E8 open reading frames [2]. Genus beta-HPVs were detected in the skin of patients with the rare recessive genetic disorder epidermodysplasia verruciformis (EV) [3–5]. These individuals are permissive hosts for persistent beta-HPV infection in the skin. Persistent infection presents as disseminated pityriasis versicolor-like lesions and flat warts, starting in early childhood [6]. About 30–60% of EV patients develop cutaneous squamous cell carcinoma (cSCC) in skin areas exposed to sunlight [2,7]. Two beta-1 types, HPV5 and HPV8, were the first beta-HPVs identified, and the International Agency for Research on Cancer (IARC) classified them as ‘possibly carcinogenic’ (Group 2B) in EV patients [8]. Epidemiological studies suggest an association of beta-HPVs and keratinocyte carcinomas also in the general human population [9]. However, owing to their commensal nature, a final proof is still challenging.
2. Mucosal high-risk human papillomaviruses persist throughout carcinogenesis
In contrast to cutaneous HPVs, mucosal HR-HPVs have been extensively studied. The products of two mucosal HR-HPV early genes, E6 and E7, are the main viral oncoproteins. They subvert the regulation of pathways involved in key cellular events, such as the cell cycle, apoptosis, DNA repair, senescence and differentiation, thus promoting the immortalization and transformation of infected cells [10,11]. A major oncogenic activity of mucosal alpha HR-HPVs involves proteolytic degradation of p53 by the E6 protein, which forms a complex with the ubiquitin ligase E6-AP [12,13]. Therefore, in strong contrast to other cancers, including skin cancer, p53 mutations are rarely detected in HR-HPV-induced cancers.
The majority (70–90%) of HR-HPV infections remain asymptomatic and are efficiently cleared by the immune system within 1–2 years [14–16]. However, once these HPV types escape immune control, they can establish persistence, a prerequisite for carcinogenesis, and even the cancer cells maintain oncogene expression [17].
Genetic features and behavioural variables that impair the immune response significantly increase the risk of cancer development [18]. In addition, specific human leukocyte antigen polymorphisms are associated with the fate of HR-HPV infections [19,20].
Importantly, HR-HPV types can deregulate innate and adaptive immune responses, supporting immune escape and persistence [21,22]. Continuous deregulated expression of the viral oncogenes leads to accumulation of chromosomal alterations and transformation of the infected cell. Thus, in this scenario, it is evident why the establishment of chronic persistent HR-HPV infection is an essential condition for the development of high-grade premalignant and malignant lesions.
3. Cutaneous human papillomaviruses operate differently from mucosal human papillomaviruses
(a). The ‘hit and run’ hypothesis
Valuable animal models have demonstrated the transforming potential of beta-HPVs [23–26].
There is accumulating evidence that cutaneous beta-HPVs are involved in human epithelial skin carcinogenesis, albeit via mechanisms that differ from those used by alpha HR-HPVs [27–29]. Beta-HPVs can establish persistent infections in EV patients or in patients with certain immune deficiencies. However, cSCCs arising in the general population harbour only few HPV-DNA-positive nuclei, as shown by in situ hybridization [30], and transcriptome analysis indicates that HPV is not actively transcribed in non-EV cSCCs [31].
Based on recent observations in animal models using natural infection, conditional transgenic mice, and in human explant cultures, the postulate that the presence of cutaneous HPV is necessary throughout carcinogenesis has been challenged [26,32,33]. The proposed model is that beta-HPVs act at early stages of skin carcinogenesis, and later become dispensable for the maintenance of the malignant phenotype, compatible with a ‘hit and run’ mechanism [34].
As an initial key step in skin carcinogenesis in lesional skin of EV patients, beta-HPV8 infection expands the ΔNp63-positive progenitor/stem cell compartment by suppressing the stemness-repressing microRNA-203 [35]. This increases a keratinocyte population with a particular susceptibility to skin carcinogenesis [36]. Mechanistically, the major beta-HPV oncoprotein E6 [24] targets CCAAT/enhancer-binding protein alpha (C/EBPα), a novel regulator of microRNA-203. Apart from its role in epidermal differentiation, C/EBPα serves as a potent suppressor of ultraviolet (UV)-induced skin carcinogenesis [37,38]. Thus, targeting C/EBPα appears to be a critical early step in beta-HPV-mediated co-carcinogenesis with UV light. Furthermore, beta-HPV E6 interferes with another important regulator of keratinocyte differentiation, Notch, via binding to its upstream regulator Mastermind-like protein 1 (MAML1) [39,40]. As a second step, keratinocytes expressing beta-HPV E6 become more resistant to UV-induced apoptosis, i.e. by targeting the pro-apoptotic factor Bak [41,42]. Beta-HPV E6 interferes with the DNA damage response, thus facilitating the accumulation of UV-induced DNA mutations (summarized in [43]). These comprise p53 mutations, which are also common in cSCCs of EV patients [44]. With an increased burden of critical mutations, the lesion may then progress to cSCC, while the viral episome becomes dispensable and is lost, potentially owing to a hostile microenvironment in non-EV skin.
(b). Determinants of disease penetrance
The potential of cutaneous beta-HPVs to act as co-carcinogens in UV-induced carcinogenesis has been clearly established in animal models. Nevertheless, the proof of their causal association with skin carcinogenesis in the general human population is still a challenge, because they are ‘ubiquitous and infect the skin of all people as a commensal flora’ [9, p. 291].
Critical questions remain: what determines the penetrance of disease, and how do beta-HPVs establish a state of infection that lasts long enough to catalyse all the necessary events, eventually leading to symptomatic disease and cancer? There are several lines of evidence that host cell-autonomous and extrinsic immunological conditions play an eminent role in the control of beta-HPVs in the general population. Studies in EV patients were seminal for this understanding [45]. Recent data strongly indicate that in these patients, the beta-HPV-specific keratinocyte-intrinsic restriction is lost owing to genetic mutation. As a consequence, EV patients apparently provide a host cell environment that is permissive for potent gene expression and viral replication.
In individuals with other distinct genetic disorders that result in deteriorated T-cell immunity, beta-HPV infection may clinically present as atypical EV, indicating a second line of beta-HPV control by adaptive T-cell immunity. The risk of cSCC development is also considerably higher in the skin of organ transplant recipients (OTRs) who receive immunosuppressive treatments [46], and in elderly people with decreasing immune function [47]. This further points to an important role of the extrinsic immune system, particularly adaptive T-cell immunity, for controlling these viruses.
Conversely, if cell-autonomous and/or extrinsic immunological control fails, the virus may be able to partially or fully complete its life cycle, and the levels of oncogene expression may be key to determine the probability and extent of stem/progenitor cell expansion and tumour initiation.
Interestingly, the beta-HPV life cycle also appears to be adapted to UV-light-induced inflammatory responses in the skin. Thus, beta-HPVs are activated by UV-mediated signalling [48,49], and they even have intrinsic properties to promote inflammatory responses [50,51]. It may be speculated that this fuels chronic inflammation, promoting progression to malignancy.
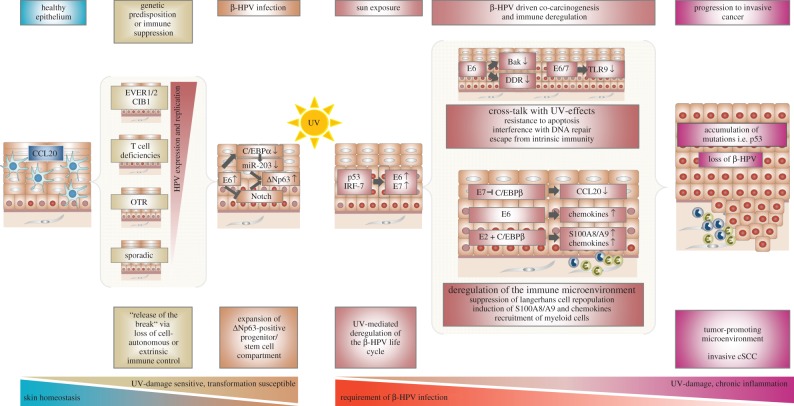
Thus, beta-HPVs show an intimate cross-talk with the immune system at various stages of infection. This review highlights the interactions of beta-HPVs with the host keratinocyte's cell-autonomous immunity and the local immune microenvironment during the establishment of cutaneous beta-HPV infection and during progression to cancer (summarized in figure 1).
Figure 1.
Schematic presentation of the cross-talk between beta-HPVs and the cell-autonomous or extrinsic immune system that may determine disease penetrance and progression to skin cancer. In healthy epithelium, Langerhans cells are present; during beta-HPV-driven co-carcinogenesis and progression to invasive cancer, the local immune system is deregulated and the stroma becomes infiltrated with myeloid cells. Red nuclei indicate ΔNp63-positive progenitor/stem cells. CCL20, CC-chemokine ligand 20; C/EBP, CCAAT/enhancer-binding protein; CIB1, calcium- and integrin-binding protein 1; cSCC, cutaneous squamous cell carcinoma; DDR, DNA damage response; HPV, human papillomavirus; IRF, interferon regulatory factor; OTRs, organ transplant recipients; TLR, Toll-like receptor; UV, ultraviolet.
4. Cell-autonomous and extrinsic immune control of beta-human papillomavirus infection
(a). Cell-autonomous control
(i). EVER proteins and CIB1
In consanguineous EV families, a susceptibility locus for EV was mapped to chromosome 17q25, which harbours two adjacent genes, EVER1 (TMC6) and EVER2 (TMC8), that are mutated in about 50% of EV cases [52]. EVER1 and EVER2 encode two highly conserved transmembrane channel-like proteins that are localized in the endoplasmic reticulum [53]. It is assumed that the keratinocyte-intrinsic functions of EVER proteins are most critical for beta-HPV control, because EV patients display no enhanced susceptibility to pathogens other than beta-HPVs [45] and EVER2 deficiency is associated only with mild changes in T lymphocytes [54]. To date, there are only few data on EVER function.
Initial studies suggested that both EVER1 and EVER2 are involved in the regulation of zinc levels in keratinocytes and potentially also in immune cells [55,56]. EVER1 and EVER2 are able to repress zinc-dependent transcription. However, in a different study, endogenous deficiencies of neither protein were found to be associated with overt disturbed zinc homeostasis [57].
Beta-HPV replication and viral transcription are regulated by the non-coding region (NCR), located upstream of the early gene region. The beta-HPV NCR differs from that of other HPVs in its small size of about 400 bp. EVER2-deficient cells were shown to activate the HPV5 NCR through a c-Jun N-terminal kinase (JNK)-dependent pathway [58]. Moreover, EVER2 induces tumour necrosis factor alpha (TNFα)- and TNF-related apoptosis-inducing ligand (TRAIL)-dependent apoptosis [59].
Recently, identification of a third EV susceptibility gene encoding the pleiotropic factor calcium- and integrin-binding protein 1 (CIB1) [60] has shed more light on the potential molecular basis underlying EV [57]. Notably, CIB1 protein levels were also found to be low in EVER1- or EVER2-mutated keratinocytes. In normal cells, CIB1 forms a complex with EVER1 and EVER2. The alpha HPV16 E5 and the gamma HPV4 E8 proteins were shown to interact with CIB1. Although there is no formal proof, it is assumed that these viral proteins interfere with CIB1-dependent restriction. The hypothesis drawn from these observations is that CIB1 may represent an intrinsic antiviral restriction factor specific for beta-HPVs, because these viruses do not encode a viral protein that can help to overcome CIB1-dependent restriction [57]. Thus, the beta-HPV life cycle may only be efficiently supported in the absence of functional CIB1.
(ii). Interferon regulatory factors
Further investigations support the notion that beta-HPVs are also under the control of innate immunity, particularly the interferon system. In the beta-HPV regulatory region, response elements for the interferon regulatory factors IRF-3 and IRF-7 were identified [49]. Both factors play an important role in the regulation of type I interferons and antiviral immunity [61].
Sensing of viral nucleic acids by pathogen recognition receptors causes activation of IRF-3, which is constitutively expressed in keratinocytes. Activated IRF-3 strongly suppresses beta-HPV8 NCR activity, thus inducing a state of cell-autonomous immunity against HPV8. Interestingly, the HPV8 E6 protein neither binds to IRF-3 nor blocks its activity, which is in strong contrast to the mucosal HR-HPV16 E6 oncoprotein [49,62]. Thus, IRF-3 remains an Achilles heel of beta-HPV, opening new avenues for IRF-3-activating compounds in antiviral immunotherapy. Treatment of keratinocytes with the IRF-3 activators poly(I:C) (a synthetic analogue of double-stranded RNA) or RNA bearing 5′ phosphates (5′pppRNA) [49] leads to potent suppression of beta-HPV NCR activity. Whether poly(I:C) can further lead to necroptosis, as observed in cervical cancer cells, remains to be determined [63,64].
In contrast to IRF-3, the related factor IRF-7 increases HPV8 NCR-driven promoter activity [49]. IRF-7 can be activated by UV light [65], and UV is known to be an activator of beta-HPVs [48]. Cutaneous beta-HPVs have adapted to UV-triggered signalling pathways, even if they are part of a previous defence response. It may be speculated that this subversion of IRF-7 may result in a pro-tumorigenic feed-forward loop, because enhanced beta-HPV expression may further increase or accelerate pro-carcinogenic UV responses.
This demonstrates that IRFs play a dual role in beta-HPV biology: whereas IRF-3 mediates suppression, IRF-7 activates the virus.
(b). Extrinsic immunity
(i). Common gamma-c or Jak3 deficiency
EV-like pathologies (termed ‘atypical EV’) have also been reported in patients with genetic deficiencies other than EVER1, EVER2 or CIB-1 [45]. Atypical EV has been observed in 50% of patients with severe combined immune deficiency (SCID) owing to gamma-c cytokine receptor subunit (gamma-c) or Jak3 mutations, as a late-onset disease many years after successful haematopoietic stem cell transplantation [66]. It was speculated that persistent natural killer (NK) cell deficiency may play a role, because EV-like disease is not observed in patients with other SCIDs who have normal NK cell activity after immune reconstitution. Alternatively, gamma-c or Jak3 mutations may cause a keratinocyte-intrinsic defect that accounts for the high susceptibility to EV-like disease.
(ii). Inherited T-cell defects
Atypical EV is also found in patients with distinct primary T-cell deficiencies (summarized in [45]). However, EV-like disease is of low penetrance in these patients, and most of them display an enhanced susceptibility not exclusively to beta-HPV but to a much broader spectrum of pathogens. NK cell numbers are apparently normal in these patients. This points to a specific contribution of T-cell immunity to beta-HPV control.
(iii). Organ transplant recipients and beta-human papillomaviruses
A large body of evidence supporting a role of adaptive T-cell immunity for the control of beta-HPV infection and disease also comes from molecular or serological epidemiological studies of OTRs who receive immunosuppressive treatments [46]. In such OTRs, the incidence of cSCCs is increased more than 100-fold, and infections with multiple beta-HPVs are observed with higher viral loads than in the general population [9,67]. Although OTRs generally do not present with symptoms of overt EV-like disease [45], actively replicating beta-HPV infection was demonstrated in actinic keratosis and epithelium adjacent to cSCCs of these patients [68].
Taken together, these studies strongly suggest that beta-HPVs are under strict control of host cell-autonomous as well as extrinsic, particularly T-cell-mediated, immunity.
(c). Immune escape during beta-human papillomavirus infection
In EV patients, beta-HPVs can efficiently replicate, probably owing to loss of cell-autonomous antiviral restriction. However, it was unclear how beta-HPVs can escape from innate and adaptive immune control, which appears to function normally in these patients. Several studies indicate that beta-HPV-encoded proteins, once sufficiently expressed, interact with distinct immune signalling pathways in the host cell that allow the virus to further escape from immune control, supporting its persistence. Several important examples are detailed below.
(i). Interference with TLR9 expression
UV irradiation and other cellular stress signals can induce Toll-like receptor 9 (TLR9) expression. This pattern-recognition receptor is activated by unmethylated CpG sequences in DNA molecules [69]. Beta-HPV38 E6 and E7 oncoproteins are able to inhibit the expression of TLR9, and they seem to share this function with mucosal HR-HPV [70,71]. In addition, HPV38 E6 and E7 oncoproteins are able to block the UV-mediated activation of TLR9 by preventing the recruitment of p53 and c-Jun to the TLR9 promoter [72].
(ii). Suppression of Langerhans cell recruitment
A striking observation in lesional epidermis of EV patients is the lack of Langerhans cells [73,74]. Langerhans cells are involved in skin immunosurveillance by cross-presenting antigens from neighbouring keratinocytes to CD8+ effector T lymphocytes [75].
In healthy individuals, UV light can cause transient immunosuppression by inducing the egress of Langerhans cells from the epidermis [76]. However, subsequent induction of the CC-chemokine ligand 20 (CCL20) in the uppermost epidermal layers will lead to a reconstitution of the epidermis with CD1a+ Langerhans cell precursors in a CCL20/CCR6-dependent manner [77,78]. Interestingly, the lesional epidermis of EV patients lacks not only Langerhans cells but also the Langerhans cell-attracting chemokine CCL20 [74].
The transcription factor C/EBPβ was identified as the key regulator of constitutive differentiation-specific CCL20 expression in the normal epidermis [74]. However, in the epidermis of EV patients, the beta-HPV E7 protein is expressed in the same granular layer where CCL20 is found in normal human skin [79]. HPV8 E7 specifically sequesters C/EBPβ and thereby interferes with its binding to the CCL20 promoter. This results in potent suppression of CCL20 expression and of Langerhans cell recruitment [74].
Thus, once expressed at a sufficient level, beta-HPV-encoded proteins are able to disrupt the epithelial immune barrier at different levels, eventually allowing viral persistence in EV patients.
(d). Stromal inflammation in beta-human papillomavirus infection and progression to cancer
A remaining question was whether beta-HPVs can alter the local microenvironment, promoting progression to cancer. Stromal inflammation, a hallmark of cancer, fuels immune deviation and progression of the disease [80].
It has recently been shown that EV lesions are strongly infiltrated with inflammatory immune cells, particularly myeloid cells, from productive infection to cancer [22,51]. There is increasing evidence that beta-HPVs can directly promote inflammation. This is in strong contrast to mucosal HR-HPVs, which potently suppress pro-inflammatory signalling [81–84]. Rather, in cervical carcinogenesis, where stromal inflammation occurs at later stages of the disease, HR-HPV-transformed cells instruct stromal fibroblasts and immune cells to produce inflammatory mediators, promoting disease progression [85–87].
(i). Potent induction of S100A8/A9 proteins by E2
In HPV8-positive skin of EV patients, infiltration with neutrophils starts in the stroma of productive lesions. This is paralleled by a dramatic upregulation of the differentiation-associated calprotectin complex, which consists of the Ca2+ and Zn2+ binding proteins S100A8 and S100A9, in the infected epithelium [51]. S100A8/A9 proteins serve as alarmins and induce immune cell chemotaxis, particularly of granulocytes [88].
S100A8/A9 expression is a direct consequence of viral infection. Notably, the viral transcription factor E2 has been identified as an inducer of this response, whereas HPV8 oncoproteins E6 and E7 suppress S100A8/A9 expression. HPV8 E2 is known to synergise with the differentiation-specific transcription factor C/EBPβ to induce keratinocyte differentiation [89]. HPV8 E2 exploits the same mechanism for S100A8/A9 induction, leading to neutrophil recruitment [51]. This function is not shared by the HPV16 E2 protein, potentially explaining the differences observed with mucosal HR-HPVs. In addition to S100A8/A9, keratinocytes co-expressing HPV8 E2 and C/EBPβ also produced other neutrophil-attracting chemokines, including interleukin 8 (IL-8), ENA-78, and NAP-2, which may further contribute to neutrophil attraction [51].
A role of HPV8 E2 in promoting chronic inflammation is consistent with observations in transgenic mice, where the HPV8 E2 protein expressed under control of the K14 promoter induces epidermal thinning, ulcerations and chronic inflammation [90]. Together, these observations strongly suggest that the property of beta-HPV E2 in enhancing inflammation appears to be intimately linked to its capability to promote differentiation [51,89,91,92].
In turn, infiltrating tumour-associated myeloid cells can provide factors like matrix metalloproteinase 9, promoting tumour growth and inducing vasculogenesis and matrix remodelling [85,93]. Thus, it can be assumed that beta-HPV infection enhances not only S100A8/A9-driven chronic inflammation but potentially also tumour progression, as has been observed in an animal model [94].
(ii). Beta-human papillomavirus oncoproteins and inflammation
An intrinsic property of activating tumour-promoting inflammation has also been demonstrated in mice expressing the complete early region (CER) or only the E6 protein of beta-HPV8 [23,24]. In HPV8 CER transgenic mice, the inflammatory signal transducer and activator of transcription 3 (STAT3) pathway are highly active, and keratinocyte-specific STAT3 heterozygosity impairs the development of skin tumours [95]. Potent activation of the STAT3 pathway has also been observed in cervical precancerous lesions [85,87]; it is thus a common trait of HPV-driven carcinogenesis and a potential target for immunotherapy.
Beta-HPV5 E6/E7 oncoproteins were shown to induce monocyte chemoattractant protein 1 (MCP1, CCL2) expression in keratinocytes [50]. The underlying mechanism remains to be clarified. However, this is in contrast to mucosal HR-HPV-encoded oncoproteins, which suppress CCL2 expression [81].
In beta-HPV38 oncoprotein immortalized cells, UVB leads to a much higher upregulation of cytokines, including IL-6, IL-8 and transforming growth factor beta (TGFβ), than in control keratinocytes [96]. Consistent with the findings for HPV8 oncoproteins [51], this was not the case for S100A8/A9. Also, TNFα upregulation was observed in the presence of HPV38 oncoproteins and relative control cells but not with mucosal HR-HPV16 [96]. Mechanistically, HPV38 was shown to activate NF-κB in human keratinocytes, supporting their survival under cytokine or UV exposure [97]. Both enhancement of UV-induced inflammation and prevention of cell death are believed to be implicated in the formation of premalignant skin lesions and subsequent cSCCs in UV-exposed HPV38 E6/E7 transgenic mice [25]. These studies showed that the presence of beta-HPV-encoded proteins can upregulate the basal levels of inflammatory cytokines and further increase inflammation upon UVB irradiation.
It is not clear how inflammation can positively affect the viral life cycle. It can be speculated that the active induction of inflammation may be part of an adaptation of beta-HPVs to a UV-activated microenvironment in the skin, in a way similar to the positive response of HPV8 to UV-activated IRF-7. However, as a side effect, the chronic inflammatory response in persistent beta-HPV infections in patients with EV or atypical EV may also promote skin carcinogenesis.
5. Conclusion and perspectives
Despite their commensalic nature in the general population, the evidence is accumulating that cutaneous genus beta-HPVs are important co-carcinogens with UV. Their biology is highly adapted to the skin, which is constantly at risk of UV exposure and damage. Thus, their life cycle and interplay with cell-autonomous immunity or the host microenvironment differ from those of mucosal HR-HPV in many aspects.
Beta-HPVs have the potential to promote the initial steps of UV-driven skin carcinogenesis. When sufficiently expressed, they expand the UV-sensitive stem/progenitor cell compartment, prolong local UV-induced immunosuppression by preventing the repopulation of the epidermis with Langerhans cells, promote the lifespan of their host cells through prevention of UV-induced apoptosis, lower the threshold to UV-induced DNA damage responses and enhance UV-induced tumour-promoting inflammation. Once critical genetic alterations are established, such as mutations in the tumour suppressor p53, beta-HPVs may become dispensable for the maintenance of the malignant phenotype (figure 1). This is compatible with a ‘hit and run’ mechanism of beta-HPV-supported skin carcinogenesis in the general population.
However, disease penetrance (i.e. EV or EV-like symptoms and development of skin cancer) is strongly controlled by host restriction factors and extrinsic immunity. Once these ‘brakes’ are released, viral expression and replication can occur, with all their deleterious consequences. This may happen occasionally in the general population, at a higher frequency in patients with acquired or inherited T-cell defects, and apparently on a regular basis in patients with classic EV.
In order to define novel strategies for therapeutic intervention against beta-HPVs beyond their sensitivity towards IRF-3-activating compounds, it is important to better understand their highly skin- and UV-light-adapted life cycle as well as their cross-talk with host cell-autonomous and extrinsic immunity.
Acknowledgements
The authors wish to thank all colleagues at their institutes and all collaborators for helpful discussions and would like to recognize all research studies that could not be considered in this review owing to space limitations. We are very grateful to Dr Karen Müller for editing this manuscript.
Data accessibility
This article has no additional data.
Authors' contributions
All authors contributed to drafting the article and revising it critically for important intellectual content, and all authors gave final approval for publication.
Competing interests
We have no competing interests. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Funding
M.T. and A.V. received funding from the Fondation ARC pour la recherche sur le cancer (no. PJA 20151203192) (https://www.fondation-arc.org/espace-chercheur) and the Institut National de la Santé et de la Recherche Médicale (no. ENV201610) (https://www.eva2.inserm.fr/EVA/jsp/AppelsOffres/CANCER/). S.L. received funding from the Deutsche Forschungsgemeinschaft (Lo 1853/1-2). S.S. received funding from the Deutsche Krebshilfe (grant no. 109752), the Saarland Staatskanzlei (grant no. WT/2 LFFP 14/15), and the Gemeinsamer Bundesausschuss (grant no. 01VSF16050).
References
- 1.Van Doorslaer K, et al. 2017. The Papillomavirus Episteme: a major update to the papillomavirus sequence database. Nucleic Acids Res. 45, D499–D506. ( 10.1093/nar/gkw879) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Orth G. 2006. Genetics of epidermodysplasia verruciformis: insights into host defense against papillomaviruses. Semin. Immunol. 18, 362–374. ( 10.1016/j.smim.2006.07.008) [DOI] [PubMed] [Google Scholar]
- 3.Lewandowsky F, Lutz W. 1922. Ein Fall einer bisher nicht beschriebenen Hauterkrankung (Epidermodysplasia verruciformis). Arch. Dermatol. Syph. 141, 193–203. ( 10.1007/BF01938833) [DOI] [Google Scholar]
- 4.Lutzner MA. 1978. Epidermodysplasia verruciformis. An autosomal recessive disease characterized by viral warts and skin cancer. A model for viral oncogenesis. Bull. Cancer 65, 169–182. [PubMed] [Google Scholar]
- 5.Rajagopalan K, Bahru J, Loo DS, Tay CH, Chin KN, Tan KK. 1972. Familial epidermodysplasia verruciformis of Lewandowsky and Lutz. Arch. Dermatol. 105, 73–78. ( 10.1001/archderm.1972.01620040045008) [DOI] [PubMed] [Google Scholar]
- 6.Orth G. 2008. Host defenses against human papillomaviruses: lessons from epidermodysplasia verruciformis. Curr. Top. Microbiol. Immunol. 321, 59–83. ( 10.1007/978-3-540-75203-5_3) [DOI] [PubMed] [Google Scholar]
- 7.Jablonska S, Majewski S. 1994. Epidermodysplasia verruciformis: immunological and clinical aspects. Curr. Top. Microbiol. Immunol. 186, 157–175. ( 10.1007/978-3-642-78487-3_9) [DOI] [PubMed] [Google Scholar]
- 8.Bouvard V, et al. 2009. A review of human carcinogens–part B: biological agents. The Lancet 10, 321–322. ( 10.1016/S1470-2045(09)70096-8) [DOI] [PubMed] [Google Scholar]
- 9.Howley PM, Pfister HJ. 2015. Beta genus papillomaviruses and skin cancer. Virology 479–480, 290–296. ( 10.1016/j.virol.2015.02.004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moody CA, Laimins LA. 2010. Human papillomavirus oncoproteins: pathways to transformation. Nat. Rev. Cancer 10, 550–560. ( 10.1038/nrc2886) [DOI] [PubMed] [Google Scholar]
- 11.Mittal S, Banks L. 2017. Molecular mechanisms underlying human papillomavirus E6 and E7 oncoprotein-induced cell transformation. Mutat. Res. Rev. Mutat. Res. 772, 23–35. ( 10.1016/j.mrrev.2016.08.001) [DOI] [PubMed] [Google Scholar]
- 12.Huibregtse JM, Scheffner M, Howley PM. 1991. A cellular protein mediates association of p53 with the E6 oncoprotein of human papillomavirus types 16 or 18. EMBO J. 10, 4129–4135. ( 10.1002/j.1460-2075.1991.tb04990.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huibregtse JM, Scheffner M, Howley PM. 1993. Cloning and expression of the cDNA for E6-AP, a protein that mediates the interaction of the human papillomavirus E6 oncoprotein with p53. Mol. Cell. Biol. 13, 775–784. ( 10.1128/MCB.13.2.775) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evander M, Edlund K, Gustafsson A, Jonsson M, Karlsson R, Rylander E, Wadell G. 1995. Human papillomavirus infection is transient in young women: a population-based cohort study. J. Infect. Dis. 171, 1026–1030. ( 10.1093/infdis/171.4.1026) [DOI] [PubMed] [Google Scholar]
- 15.Ho GY, Bierman R, Beardsley L, Chang CJ, Burk RD. 1998. Natural history of cervicovaginal papillomavirus infection in young women. N. Engl. J. Med. 338, 423–428. ( 10.1056/NEJM199802123380703) [DOI] [PubMed] [Google Scholar]
- 16.Moscicki AB, et al. 1998. The natural history of human papillomavirus infection as measured by repeated DNA testing in adolescent and young women. J. Pediatr. 132, 277–284. ( 10.1016/S0022-3476(98)70445-7) [DOI] [PubMed] [Google Scholar]
- 17.zur Hausen H. 2002. Papillomaviruses and cancer: from basic studies to clinical application. Nat. Rev. Cancer 2, 342–350. ( 10.1038/nrc798) [DOI] [PubMed] [Google Scholar]
- 18.Schiffman M, Doorbar J, Wentzensen N, de Sanjose S, Fakhry C, Monk BJ, Stanley MA, Franceschi S.. 2016. Carcinogenic human papillomavirus infection. Nat. Rev. Dis. Primers 2, 16086 ( 10.1038/nrdp.2016.86) [DOI] [PubMed] [Google Scholar]
- 19.Leo PJ, et al. 2017. Defining the genetic susceptibility to cervical neoplasia: a genome-wide association study. PLoS Genet. 13, e1006866 ( 10.1371/journal.pgen.1006866) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mehta AM, Mooij M, Brankovic I, Ouburg S, Morre SA, Jordanova ES. 2017. Cervical carcinogenesis and immune response gene polymorphisms: a review. J. Immunol. Res. 2017, 8913860 ( 10.1155/2017/8913860) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smola S, Trimble C, Stern PL. 2017. Human papillomavirus-driven immune deviation: challenge and novel opportunity for immunotherapy. Ther. Adv. Vaccines 5, 69–82. ( 10.1177/2051013617717914) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smola S. 2017. Immunopathogenesis of HPV-associated cancers and prospects for immunotherapy. Viruses 9, 254 ( 10.3390/v9090254) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schaper ID, Marcuzzi GP, Weissenborn SJ, Kasper HU, Dries V, Smyth N, Fuchs P, Pfister H. 2005. Development of skin tumors in mice transgenic for early genes of human papillomavirus type 8. Cancer Res. 65, 1394–1400. ( 10.1158/0008-5472.CAN-04-3263) [DOI] [PubMed] [Google Scholar]
- 24.Marcuzzi GP, Hufbauer M, Kasper HU, Weissenborn SJ, Smola S, Pfister H. 2009. Spontaneous tumour development in human papillomavirus type 8 E6 transgenic mice and rapid induction by UV-light exposure and wounding. J. Gen. Virol. 90, 2855–2864. ( 10.1099/vir.0.012872-0) [DOI] [PubMed] [Google Scholar]
- 25.Viarisio D, et al. 2011. E6 and E7 from beta HPV38 cooperate with ultraviolet light in the development of actinic keratosis-like lesions and squamous cell carcinoma in mice. PLoS Pathog. 7, e1002125 ( 10.1371/journal.ppat.1002125) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Viarisio D, et al. 2018. Beta HPV38 oncoproteins act with a hit-and-run mechanism in ultraviolet radiation-induced skin carcinogenesis in mice. PLoS Pathog. 14, e1006783 ( 10.1371/journal.ppat.1006783) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smola S. 2014. Human papillomaviruses and skin cancer. Adv. Exp. Med. Biol. 810, 192–207. [PubMed] [Google Scholar]
- 28.Tommasino M. 2017. The biology of beta human papillomaviruses. Virus Res. 231, 128–138. ( 10.1016/j.virusres.2016.11.013) [DOI] [PubMed] [Google Scholar]
- 29.Wendel SO, Wallace NA. 2017. Loss of genome fidelity: beta HPVs and the DNA damage response. Front. Microbiol. 8, 2250 ( 10.3389/fmicb.2017.02250) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weissenborn SJ, Nindl I, Purdie K, Harwood C, Proby C, Breuer J, Majewski S, Pfister H, Wieland U. 2005. Human papillomavirus-DNA loads in actinic keratoses exceed those in non-melanoma skin cancers. J. Invest. Dermatol. 125, 93–97. ( 10.1111/j.0022-202X.2005.23733.x) [DOI] [PubMed] [Google Scholar]
- 31.Arron ST, Ruby JG, Dybbro E, Ganem D, Derisi JL. 2011. Transcriptome sequencing demonstrates that human papillomavirus is not active in cutaneous squamous cell carcinoma. J. Invest. Dermatol. 131, 1745–1753. ( 10.1038/jid.2011.91) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hasche D, et al. 2017. The interplay of UV and cutaneous papillomavirus infection in skin cancer development. PLoS Pathog. 13, e1006723 ( 10.1371/journal.ppat.1006723) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Borgogna C, et al. 2018. beta-HPV infection correlates with early stages of carcinogenesis in skin tumors and patient-derived xenografts from a kidney transplant recipient cohort. Front. Microbiol. 9, 117 ( 10.3389/fmicb.2018.00117) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hasche D, Vinzon SE, Rosl F. 2018. Cutaneous papillomaviruses and non-melanoma skin cancer: causal agents or innocent bystanders? Front. Microbiol. 9, 874 ( 10.3389/fmicb.2018.00874) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marthaler AM, et al. 2017. Identification of C/EBPα as a novel target of the HPV8 E6 protein regulating miR-203 in human keratinocytes. PLoS Pathog. 13, e1006406 ( 10.1371/journal.ppat.1006406) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Missero C, Antonini D. 2017. p63 in squamous cell carcinoma of the skin: more than a stem cell/progenitor marker. J. Invest. Dermatol. 137, 280–281. ( 10.1016/j.jid.2016.10.032) [DOI] [PubMed] [Google Scholar]
- 37.Thompson EA, Zhu S, Hall JR, House JS, Ranjan R, Burr JA, He YY, Owens DM, Smart RC. 2011. C/EBPα expression is downregulated in human nonmelanoma skin cancers and inactivation of C/EBPα confers susceptibility to UVB-induced skin squamous cell carcinomas. J. Invest. Dermatol. 131, 1339–1346. ( 10.1038/jid.2011.31) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schuster MB, Porse BT. 2006. C/EBPα: a tumour suppressor in multiple tissues? Biochim. Biophys. Acta 1766, 88–103. ( 10.1016/j.bbcan.2006.02.003) [DOI] [PubMed] [Google Scholar]
- 39.Tan MJ, White EA, Sowa ME, Harper JW, Aster JC, Howley PM. 2012. Cutaneous beta-human papillomavirus E6 proteins bind Mastermind-like coactivators and repress Notch signaling. Proc. Natl Acad. Sci. USA 109, E1473–E1480. ( 10.1073/pnas.1205991109) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meyers JM, Spangle JM, Munger K. 2013. The human papillomavirus type 8 E6 protein interferes with NOTCH activation during keratinocyte differentiation. J. Virol. 87, 4762–4767. ( 10.1128/JVI.02527-12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jackson S, Harwood C, Thomas M, Banks L, Storey A. 2000. Role of Bak in UV-induced apoptosis in skin cancer and abrogation by HPV E6 proteins. Genes Dev. 14, 3065–3073. ( 10.1101/gad.182100) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Underbrink MP, Howie HL, Bedard KM, Koop JI, Galloway DA. 2008. E6 proteins from multiple human betapapillomavirus types degrade Bak and protect keratinocytes from apoptosis after UVB irradiation. J. Virol. 82, 10 408–10 417. ( 10.1128/JVI.00902-08) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wallace NA, Galloway DA. 2014. Manipulation of cellular DNA damage repair machinery facilitates propagation of human papillomaviruses. Semin. Cancer Biol. 26, 30–42. ( 10.1016/j.semcancer.2013.12.003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Padlewska K, Ramoz N, Cassonnet P, Riou G, Barrois M, Majewski S, Croissant O, Jablonska S, Orth G. 2001. Mutation and abnormal expression of the p53 gene in the viral skin carcinogenesis of epidermodysplasia verruciformis. J. Invest. Dermatol. 117, 935–942. ( 10.1046/j.0022-202x.2001.01515.x) [DOI] [PubMed] [Google Scholar]
- 45.de Jong SJ, Imahorn E, Itin P, Uitto J, Orth G, Jouanguy E, Casanova JL, Burger B.. 2018. Epidermodysplasia verruciformis: inborn errors of immunity to human beta-papillomaviruses. Front. Microbiol. 9, 1222 ( 10.3389/fmicb.2018.01222) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Proby CM, et al. 2011. A case-control study of betapapillomavirus infection and cutaneous squamous cell carcinoma in organ transplant recipients. Am. J. Transplant. 11, 1498–1508. ( 10.1111/j.1600-6143.2011.03589.x) [DOI] [PubMed] [Google Scholar]
- 47.Garcovich S, Colloca G, Sollena P, Andrea B, Balducci L, Cho WC, Bernabei R, Peris K. 2017. Skin cancer epidemics in the elderly as an emerging issue in geriatric oncology. Aging Dis. 8, 643–661. ( 10.14336/AD.2017.0503) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Akgul B, Lemme W, Garcia-Escudero R, Storey A, Pfister HJ. 2005. UV-B irradiation stimulates the promoter activity of the high-risk, cutaneous human papillomavirus 5 and 8 in primary keratinocytes. Arch. Virol. 150, 145–151. ( 10.1007/s00705-004-0398-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Oldak M, et al. 2011. Differential regulation of human papillomavirus type 8 by interferon regulatory factors 3 and 7. J. Virol. 85, 178–188. ( 10.1128/JVI.00998-10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.De Andrea M, Mondini M, Azzimonti B, Dell'Oste V, Germano S, Gaudino G, Musso T, Landolfo S, Gariglio M.. 2007. Alpha- and betapapillomavirus E6/E7 genes differentially modulate pro-inflammatory gene expression. Virus Res. 124, 220–225. ( 10.1016/j.virusres.2006.09.010) [DOI] [PubMed] [Google Scholar]
- 51.Podgorska M, et al. 2018. Chronic inflammatory microenvironment in epidermodysplasia verruciformis skin lesions: role of the synergism between HPV8 E2 and C/EBPβ to induce pro-inflammatory S100A8/A9 proteins. Front. Microbiol. 9, 392 ( 10.3389/fmicb.2018.00392) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ramoz N, Rueda LA, Bouadjar B, Montoya LS, Orth G, Favre M. 2002. Mutations in two adjacent novel genes are associated with epidermodysplasia verruciformis. Nat. Genet. 32, 579–581. ( 10.1038/ng1044) [DOI] [PubMed] [Google Scholar]
- 53.Keresztes G, Mutai H, Heller S. 2003. TMC and EVER genes belong to a larger novel family, the TMC gene family encoding transmembrane proteins. BMC Genomics 4, 24 ( 10.1186/1471-2164-4-24) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crequer A, et al. 2013. EVER2 deficiency is associated with mild T-cell abnormalities. J. Clin. Immunol. 33, 14–21. ( 10.1007/s10875-012-9749-1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lazarczyk M, Cassonnet P, Pons C, Jacob Y, Favre M. 2009. The EVER proteins as a natural barrier against papillomaviruses: a new insight into the pathogenesis of human papillomavirus infections. Microbiol. Mol. Biol. Rev. 73, 348–370. ( 10.1128/mmbr.00033-08) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lazarczyk M, Dalard C, Hayder M, Dupre L, Pignolet B, Majewski S, Vuillier F, Favre M, Liblau RS. 2012. EVER proteins, key elements of the natural anti-human papillomavirus barrier, are regulated upon T-cell activation. PLoS ONE 7, e39995 ( 10.1371/journal.pone.0039995) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.de Jong SJ, et al. 2018. The human CIB1-EVER1-EVER2 complex governs keratinocyte-intrinsic immunity to beta-papillomaviruses. J. Exp. Med. 215, 2289–2310. ( 10.1084/jem.20170308) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vuillier F, Gaud G, Guillemot D, Commere PH, Pons C, Favre M. 2014. Loss of the HPV-infection resistance EVER2 protein impairs NF-κB signaling pathways in keratinocytes. PLoS ONE 9, e89479 ( 10.1371/journal.pone.0089479) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gaud G, Guillemot D, Jacob Y, Favre M, Vuillier F. 2013. EVER2 protein binds TRADD to promote TNF-α-induced apoptosis. Cell Death Dis. 4, e499 ( 10.1038/cddis.2013.27) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leisner TM, Freeman TC, Black JL, Parise LV. 2016. CIB1: a small protein with big ambitions. FASEB J. 30, 2640–2650. ( 10.1096/fj.201500073R) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Takaoka A, Tamura T, Taniguchi T. 2008. Interferon regulatory factor family of transcription factors and regulation of oncogenesis. Cancer Sci. 99, 467–478. ( 10.1111/j.1349-7006.2007.00720.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ronco LV, Karpova AY, Vidal M, Howley PM. 1998. Human papillomavirus 16 E6 oncoprotein binds to interferon regulatory factor-3 and inhibits its transcriptional activity. Genes Dev. 12, 2061–2072. ( 10.1101/gad.12.13.2061) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Schmidt SV, et al. 2015. RIPK3 expression in cervical cancer cells is required for PolyIC-induced necroptosis, IL-1α release, and efficient paracrine dendritic cell activation. Oncotarget 6, 8635–8647. ( 10.18632/oncotarget.3249) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Smola S. 2016. RIPK3: a predictive marker for personalized immunotherapy? Oncoimmunology 5, e1075695 ( 10.1080/2162402X.2015.1075695) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim TK, Kim T, Kim TY, Lee WG, Yim J. 2000. Chemotherapeutic DNA-damaging drugs activate interferon regulatory factor-7 by the mitogen-activated protein kinase kinase-4-cJun NH2-terminal kinase pathway. Cancer Res. 60, 1153–1156. [PubMed] [Google Scholar]
- 66.Laffort C, et al. 2004. Severe cutaneous papillomavirus disease after haemopoietic stem-cell transplantation in patients with severe combined immune deficiency caused by common gammac cytokine receptor subunit or JAK-3 deficiency. Lancet 363, 2051–2054. ( 10.1016/S0140-6736(04)16457-X) [DOI] [PubMed] [Google Scholar]
- 67.Bouwes BJN, et al. 2018. Human papillomavirus and posttransplantation cutaneous squamous cell carcinoma: a multicenter, prospective cohort study. Am. J. Transplant. 18, 1220–1230. ( 10.1111/ajt.14537) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Borgogna C, et al. 2014. Improved detection reveals active beta-papillomavirus infection in skin lesions from kidney transplant recipients. Mod. Pathol. 27, 1101–1115. ( 10.1038/modpathol.2013.240) [DOI] [PubMed] [Google Scholar]
- 69.Wagner H. 2002. Interactions between bacterial CpG-DNA and TLR9 bridge innate and adaptive immunity. Curr. Opin Microbiol. 5, 62–69. ( 10.1016/S1369-5274(02)00287-4) [DOI] [PubMed] [Google Scholar]
- 70.Hasan UA, et al. 2007. TLR9 expression and function is abolished by the cervical cancer-associated human papillomavirus type 16. J. Immunol. 178, 3186–3197. ( 10.4049/jimmunol.178.5.3186) [DOI] [PubMed] [Google Scholar]
- 71.Pacini L, Savini C, Ghittoni R, Saidj D, Lamartine J, Hasan UA, Accardi R, Tommasino M. 2015. Downregulation of Toll-like receptor 9 expression by beta human papillomavirus 38 and implications for cell cycle control. J. Virol. 89, 11 396–11 405. ( 10.1128/JVI.02151-15) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pacini L, Ceraolo MG, Venuti A, Melita G, Hasan UA, Accardi R, Tommasino M. 2017. UV radiation activates Toll-like receptor 9 expression in primary human keratinocytes, an event inhibited by human papillomavirus type 38 E6 and E7 oncoproteins. J. Virol. 91, e01123–17. ( 10.1128/JVI.01123-17) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van Voorst Vader PC, de Jong MC, Blanken R, Kallenberg CG, Vermey A, Scheres JM.. 1987. Epidermodysplasia verruciformis: Langerhans cells, immunologic effect of retinoid treatment and cytogenetics. Arch. Dermatol. Res. 279, 366–373. ( 10.1007/BF00412621) [DOI] [PubMed] [Google Scholar]
- 74.Sperling T, et al. 2012. Human papillomavirus type 8 interferes with a novel C/EBPβ-mediated mechanism of keratinocyte CCL20 chemokine expression and Langerhans cell migration. PLoS Pathog. 8, e1002833 ( 10.1371/journal.ppat.1002833) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stoitzner P, Tripp CH, Eberhart A, Price KM, Jung JY, Bursch L, Ronchese F, Romani N. 2006. Langerhans cells cross-present antigen derived from skin. Proc. Natl Acad. Sci. USA 103, 7783–7788. ( 10.1073/pnas.0509307103) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dandie GW, Clydesdale GJ, Jacobs I, Muller HK. 1998. Effects of UV on the migration and function of epidermal antigen presenting cells. Mutat. Res. 422, 147–154. ( 10.1016/S0027-5107(98)00186-9) [DOI] [PubMed] [Google Scholar]
- 77.Charbonnier AS, Kohrgruber N, Kriehuber E, Stingl G, Rot A, Maurer D. 1999. Macrophage inflammatory protein 3alpha is involved in the constitutive trafficking of epidermal Langerhans cells. J. Exp. Med. 190, 1755–1768. ( 10.1084/jem.190.12.1755) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Le Borgne M, et al. 2006. Dendritic cells rapidly recruited into epithelial tissues via CCR6/CCL20 are responsible for CD8+ T cell crosspriming in vivo. Immunity 24, 191–201. ( 10.1016/j.immuni.2006.01.005) [DOI] [PubMed] [Google Scholar]
- 79.Haller K, Stubenrauch F, Pfister H. 1995. Differentiation-dependent transcription of the epidermodysplasia verruciformis-associated human papillomavirus type 5 in benign lesions. Virology 214, 245–255. ( 10.1006/viro.1995.0028) [DOI] [PubMed] [Google Scholar]
- 80.Hanahan D, Weinberg RA. 2011. Hallmarks of cancer: the next generation. Cell 144, 646–674. ( 10.1016/j.cell.2011.02.013) [DOI] [PubMed] [Google Scholar]
- 81.Kleine-Lowinski K, Rheinwald JG, Fichorova RN, Anderson DJ, Basile J, Munger K, Daly CM, Rosl F, Rollins BJ. 2003. Selective suppression of monocyte chemoattractant protein-1 expression by human papillomavirus E6 and E7 oncoproteins in human cervical epithelial and epidermal cells. Int. J. Cancer 107, 407–415. ( 10.1002/ijc.11411) [DOI] [PubMed] [Google Scholar]
- 82.Karim R, Meyers C, Backendorf C, Ludigs K, Offringa R, van Ommen GJ, Melief CJ, van der Burg SH, Boer JM.. 2011. Human papillomavirus deregulates the response of a cellular network comprising of chemotactic and proinflammatory genes. PLoS ONE 6, e17848 ( 10.1371/journal.pone.0017848) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Karim R, et al. 2013. Human papillomavirus (HPV) upregulates the cellular deubiquitinase UCHL1 to suppress the keratinocyte's innate immune response. PLoS Pathog. 9, e1003384 ( 10.1371/journal.ppat.1003384) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Smola-Hess S, Pfister HJ. 2006. Immune evasion in genital papillomavirus infection and cervical cancer: role of cytokines and chemokines. In Papillomavirus research: from natural history to vaccines and beyond (ed. Campo MS.). Glasgow, UK: Caister; Academic Press. [Google Scholar]
- 85.Schroer N, Pahne J, Walch B, Wickenhauser C, Smola S. 2011. Molecular pathobiology of human cervical high-grade lesions: paracrine STAT3 activation in tumor-instructed myeloid cells drives local MMP-9 expression. Cancer Res. 71, 87–97. ( 10.1158/0008-5472.CAN-10-2193) [DOI] [PubMed] [Google Scholar]
- 86.Walch-Ruckheim B, Mavrova R, Henning M, Vicinus B, Kim YJ, Bohle RM, Juhasz-Boss I, Solomayer EF, Smola S. 2015. Stromal fibroblasts induce CCL20 through IL6/C/EBPβ to support the recruitment of Th17 cells during cervical cancer progression. Cancer Res. 75, 5248–5259. ( 10.1158/0008-5472.CAN-15-0732) [DOI] [PubMed] [Google Scholar]
- 87.Walch-Ruckheim B, et al. 2016. STAT3/IRF1 pathway activation sensitizes cervical cancer cells to chemotherapeutic drugs. Cancer Res. 76, 3872–3883. ( 10.1158/0008-5472.CAN-14-1306) [DOI] [PubMed] [Google Scholar]
- 88.Ryckman C, Vandal K, Rouleau P, Talbot M, Tessier PA. 2003. Proinflammatory activities of S100: proteins S100A8, S100A9, and S100A8/A9 induce neutrophil chemotaxis and adhesion. J. Immunol. 170, 3233–3242. ( 10.4049/jimmunol.170.6.3233) [DOI] [PubMed] [Google Scholar]
- 89.Hadaschik D, Hinterkeuser K, Oldak M, Pfister HJ, Smola-Hess S. 2003. The Papillomavirus E2 protein binds to and synergizes with C/EBP factors involved in keratinocyte differentiation. J. Virol. 77, 5253–5265. ( 10.1128/JVI.77.9.5253-5265.2003) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pfefferle R, Marcuzzi GP, Akgul B, Kasper HU, Schulze F, Haase I, Wickenhauser C, Pfister H. 2008. The human papillomavirus type 8 E2 protein induces skin tumors in transgenic mice. J. Invest. Dermatol. 128, 2310–2315. ( 10.1038/jid.2008.73) [DOI] [PubMed] [Google Scholar]
- 91.Oldak M, Maksym RB, Sperling T, Yaniv M, Smola H, Pfister HJ, Malejczyk J, Smola S. 2010. Human papillomavirus type 8 E2 protein unravels JunB/Fra-1 as an activator of the beta4-integrin gene in human keratinocytes. J. Virol. 84, 1376–1386. ( 10.1128/JVI.01220-09) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Oldak M, Smola H, Aumailley M, Rivero F, Pfister H, Smola-Hess S. 2004. The human papillomavirus type 8 E2 protein suppresses beta4-integrin expression in primary human keratinocytes. J. Virol. 78, 10 738–10 746. ( 10.1128/JVI.78.19.10738-10746.2004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Coussens LM, Werb Z. 2002. Inflammation and cancer. Nature 420, 860–867. ( 10.1038/nature01322) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gebhardt C, et al. 2008. RAGE signaling sustains inflammation and promotes tumor development. J. Exp. Med. 205, 275–285. ( 10.1084/jem.20070679) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.De Andrea M, et al. 2010. Keratinocyte-specific stat3 heterozygosity impairs development of skin tumors in human papillomavirus 8 transgenic mice. Cancer Res. 70, 7938–7948. ( 10.1158/0008-5472.CAN-10-1128) [DOI] [PubMed] [Google Scholar]
- 96.Dell'oste V, et al. 2008. Altered expression of UVB-induced cytokines in human papillomavirus-immortalized epithelial cells. J. Gen. Virol. 89, 2461–2466. ( 10.1099/vir.0.83586-0) [DOI] [PubMed] [Google Scholar]
- 97.Hussain I, et al. 2011. NF-kappaB protects human papillomavirus type 38 E6/E7-immortalized human keratinocytes against tumor necrosis factor alpha and UV-mediated apoptosis. J. Virol. 85, 9013–9022. ( 10.1128/JVI.00002-11) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This article has no additional data.