Abstract
Objectives
To assess the knowledge and intake of folic acid among teachers of childbearing age and to identify barriers to folic acid intake.
Setting
Governmental schools, which included 14 primary models, 29 primary, 14 preparatory and 16 secondary schools. The proportion of teachers in each stratum was then determined, and a stratified random sampling design had been used with proportional allocation.
Study design
Cross-sectional study
Participants
A total of 406 non-pregnant teachers of childbearing age enrolled in the study. A validated questionnaire in the Arabic language was used.
Results
The overall response rate was 98%. About 34.6% reported the optimal period in which they should take folic acid, 28.3% reported the correct intake duration and only 29.5% could name food rich in folic acid. Friends and healthcare providers were the main sources of information for the participants; however, 44% said that they did not receive enough information from their healthcare providers.
Conclusion
There is a lack of knowledge and poor intake of folic acid among the participants. In particular, they lacked information about the appropriate time to start folic acid supplementations, the duration of intake and the folic acid-rich food. The most common reason being the limited advice given by their healthcare providers.
Awareness campaigns are recommended to emphasise the role of healthcare providers in counselling women about the proper use of folic acid before pregnancy.
Keywords: folic acid, pregnancy, neural tube defects, childbearing, knowledge
Strengths and limitations of this study.
This is the first population-based study among teachers assessing their knowledge and intake of folic acid in Qatar.
Teachers are considered role models by their students and they have a unique opportunity to reinforce thoughts and ideas among students and community. They are a well-defined group with reasonable socioeconomic status and accessible.
The level of awareness and knowledge about folic acid might be related to the selection of a highly educated subject group.
This is a cross-sectional study where temporality cannot be demonstrated.
With the self-reporting nature involved in gathering this data, there is the danger of recall bias and participants may have over-reported or under-reported their knowledge about or use of folic acid supplements. The teachers in this study may not represent all women of childbearing age and therefore, the generalisability of these results may be limited.
Introduction
Birth defects have so far been the leading cause of infant mortality for the past 25 years, causing 22% of all infant deaths. Infants with neural tube defects (NTDs) continue to be at increased risk of morbidity and mortality, resulting in approximately 88 000 deaths and 8.6 million disability-adjusted life years.1–5 NTDs are a serious group of heterogeneous and complex congenital birth defects of the brain and spine. They are considered to make up one of the highest incidence rates of all congenital malformations. NTDs rates differ from one population to another and have been found to vary according to geography, time and selected maternal demographic characteristics.6–8 According to the International Clearinghouse for Birth Defects Surveillance and Research, the prevalence rates of NTDs—including spina bifida, anencephaly and encephalocele—between 2007 and 2011 were 5.14 per 10 000 live births and stillbirths in Canada, 6.85 in Japan and 7.64 in the US state of Texas.9 The European Surveillance of Congenital Anomalies found the prevalence of NTDs in European countries between 2008 and 2012 to be 9.69 per 10 000 births.10 The incidence of NTDs in the United Arab Emirates (UAE) was 11.4 per 10 000 live births; with approximately 50 000 live births annually in the UAE, it is expected that around 57 babies are born with NTDs every year. If folic acid supplements can prevent half of these cases that would mean a reduction of about 30 cases of NTD annually.11 In Oman, national data retrieved from hospital records showed the incidence of NTDs to be 12.5 per 10 000.12
Folic acid reduces the risk of birth defects, including NTDs. It also decreases the risk of miscarriage and fetal death as well as folate-deficiency anaemia.13–15 Folate status is particularly important before conception and during the first 12 weeks of pregnancy. Despite the increasing awareness of the need for NTD prevention, studies have reported that folic acid intake by non-pregnant women, especially young women taking daily multivitamin supplements containing folic acid, is still low.16 17 Different reports show women who were aware of the need for folic acid were almost 40 times more likely to take it than women who did not know of its benefit.18
Food fortification has been undertaken in the Arab Gulf Region since the late 1970s. In the 1990s, several countries in the region began fortifying wheat flour with encouragement from international organisations, such as the WHO, the United Nations Children’s Fund and the Micronutrient Initiative. Fortification of wheat flour with iron and folic acid is mandatory in Kingdom of Saudi Arabia, Oman, Kuwait and Bahrain, and voluntary in Qatar. In the year 2000, Qatar started adding 30 mg of iodine and 1.5–2 mg of folic acid to wheat flour. Non-pregnant women of childbearing age reported an average daily consumption of 128 μg of folic acid, only 32% of the daily recommended amount. Investigations determined that at the present level of folic acid fortification most women still need to consume folic acid-containing dietary supplement daily to achieve the 400 micrograms per day as recommended. Thus, supporting the need for continuing the promotion of folic acid supplementation, especially in a developing country, such as Qatar.19
Female teachers are a well-defined group with good socioeconomic status, well-educated, they are accessible, and proposed target for intervention. They are role models for their students and could reinforce thoughts and ideas among them. There is a lack of data available about folic acid awareness or intake among teachers of childbearing age in the State of Qatar.
Objectives
This study aims to assess the knowledge and intake of folic acid among teachers of childbearing age and to identify barriers to folic acid intake.
Methods
Study design
Cross-sectional study
Setting
The study was conducted in governmental schools. According to the Ministry of Education, there are four educational regions in Qatar, represented as follows: Doha Region, Dukhan Region, Al Shamal Region and Al Khor Region. These four areas included all the governmental schools with different educational levels (primary model, primary, preparatory and secondary levels). These levels are distributed in 73 schools, most of these schools (approximately 56) are located inside Doha city as it’s the largest city in Qatar with majority of the population (90%) living in it.
Sample size
The sample size was calculated by Open Epi Info software (V.10), based on 53.7% expected proportion (effect size) of folic acid awareness, 95% CI and 0.05 absolute precision on either side of the proportion p (d) were used.
Estimated sample (n)=338, after addition of 20% to compensate for non-response, the final sample (n)=406.
Sampling technique
A total number of 3757 teachers were employed in governmental schools and the eligible number of teachers were 2913. A stratified random sampling design was used with proportional allocation. First, the schools were divided into four different strata according to the educational level (primary model, primary, middle and high schools); the sample included 14 primary models, 29 primary, 14 preparatory and 16 secondary schools. The proportion of teachers in each stratum was then determined, and a simple random sampling was conducted to select the eligible teachers from each stratum.
Inclusion criteria
Teachers of childbearing age ≤49 years old working in the selected schools at different educational levels.
Exclusion criteria
Teachers who are pregnant and those who are on leave when the study is conducted.
Outcome variables
Knowledge of folic acid and its intake before pregnancy
Potential determinants
Sociodemographic factors including age, marital status and nationality, socioeconomic status including family income and educational level, and finally, the relationship between knowledge and intake of folic acid
Method of data collection tool
A self-administered questionnaire in the Arabic language was developed by the researchers after reviewing the literature.16 20–23 The questionnaire included sociodemographic data, such as age, nationality, marital status, educational level, place of work and family income. It also included questions concerning knowledge about folic acid as a vitamin, its role in the prevention of NTDs, the frequency, the duration and appropriate intake time. Other questions assessed their knowledge around the sufficiency of food as a source of folic acid and it also examined their intake of folic acid supplements in addition to food rich in folic acid as well as the participants’ source of information regarding these. There were also questions to determine their folic acid intake (400 μg as recommended daily) at the time when the survey was conducted even if they took it as a one-off on the day. The final questions assessed the barriers related to folic acid intake. The questionnaire was pretested with a convenient sample of the study population (n=41 female teachers), and some questions were modified based on the feedback from the pilot testing. Teachers who participated in the pilot were excluded from the sampling frame when selecting the study subjects.
The findings of this study are subject to certain bias as it’s based on self-reported information; therefore, findings might be overestimated or underestimated. However, we are convinced with the results since it’s unlikely that the participants spent time giving unreliable answers especially with full explanation of the importance and confidentiality of data here as well as anonymity of the survey.
Data management
The data were analysed using SPSS, Windows, V.20. Χ2 tests of significance and/or Fisher’s exact test were performed to test relationships between proportions. A value of p<0.05 was considered the cut-off value for significance.
Ethical consideration
Voluntary participation and confidentiality were assured.
Patient and public involvement
The research questions were developed utilising the published literature on the importance of folic acid, the level of awareness surrounding it and its intake. Teachers’ priorities, experiences and preferences were neither directly gathered nor involved in designing the study. There are no plans to disseminate results to the study participants directly. However, it is likely that the study participants will become more aware of it in the future.
Results
In total, 406 female teachers were surveyed about their folic acid knowledge and intake for a period of 3 months, 400 participants completed and returned the questionnaires, giving an overall response rate of 98%. Respondents’ mean age was 35±5.65 years. Of the teachers surveyed, Qatari female teachers constituted the majority (89%) and 79% of participants were married. Family income per month ranged between 20 001 and 30 000 QR for 47.3% of participants, with a median income of 22 000 QR (table 1). Of the respondents, 88% had heard of folic acid and more than half of them had heard of NTDs. Concerning participants’ knowledge about the timing of folic acid intake, 53.5% answered that they knew this but only 34.6% accurately reported the best time to take it, which is prior to conception and during the first trimester of pregnancy (table 2). Regarding the origins of their knowledge, 60% reported that they received this advice from the women’s hospital, while only 27% received advice from their primary healthcare and the remaining 13% from private health sectors. The majority of respondents (90.9%) were advised to take folic acid supplementation by their doctor who attended to them during their antenatal visits, 6.2% received advice from the nurses and very few respondents received this information from a dietician (2.9%). More than two-thirds of participants (72.5%) had been advised about folic acid supplementation before the survey (table 3), but only 29.5% of participants mentioned that they knew which foods are rich in folic acid. About 32% answered that dietary folate is a sufficient source for the daily requirement of folic acid. Approximately, 78% of participants reported that taking both folic acid supplementations and food items rich in folate are beneficial (table 4). It was found that 74.5% had received folic acid pills at some point in time and 52.5% were taking folic acid supplements at the time of the study. Among those who took folic acid at some point in their lives, 55.4% took it daily; 80.2% of them were taking supplements in response to medical advice and 11% were taking it based on the advice of family and friends (table 5).
Table 1.
Sociodemographic characteristics of the study population (n=400)
| Characteristics | N | % |
| Age | ||
| ≤35 years | 202 | 50.5 |
| >35 years | 198 | 49.5 |
| Mean≠SD 35.59±5.654 | ||
| Nationality | ||
| Qatari | 356 | 89 |
| Non-Qatari | 40 | 10 |
| Missing | 4 | 1 |
| Marital status | ||
| Married | 316 | 79 |
| Non-married | 83 | 20.8 |
| Missing | 1 | 0.2 |
| Educational level | ||
| College level | 371 | 92.8 |
| Postgraduate education | 28 | 7 |
| Missing | 1 | 0.2 |
| Place of work | ||
| Model schools | 45 | 11.2 |
| Primary schools | 246 | 61.5 |
| Preparatory schools | 44 | 11 |
| Secondary schools | 65 | 16.3 |
| Family income | ||
| ≤20 000 | 165 | 41.3 |
| 20 001–30 000 | 189 | 47.3 |
| >30 000 | 46 | 11.4 |
| Median=22 000 | ||
Table 2.
Frequency distribution of participants according to awareness of folic acid (FA) and neural tube defects (NTDs)
| Knowledge | N | % |
| Ever heard of FA | ||
| Yes | 352 | 88 |
| No | 48 | 12 |
| Total | 400 | 100 |
| Ever heard of NTDs | ||
| Yes | 211 | 52.8 |
| No | 189 | 47.2 |
| Total | 400 | 100 |
| Awareness of preventive role of FA | ||
| Yes | 162 | 76.7 |
| No | 49 | 23.3 |
| Total | 211 | 100 |
| Do you know the time of FA intake | ||
| Yes | 214 | 53.5 |
| No | 186 | 46.5 |
| Total | 400 | 100 |
| Best time of FA intake | ||
| Yes | 74 | 34.6 |
| No | 140 | 65.4 |
| Total | 214 | 100 |
| Duration of FA intake | ||
| Yes | 113 | 28.3 |
| No | 287 | 71.7 |
| Total | 400 | 100 |
| Frequency of FA intake | ||
| Daily | 320 | 80 |
| Weekly | 60 | 15 |
| Monthly | 20 | 5 |
| Total | 400 | 100 |
Table 3.
Frequency distribution of participants who were advised about folic acid (FA), according to source and clarity of advice
| N | % | |
| Source of advice | ||
| Primary health care | 69 | 27 |
| Women’s hospital | 152 | 60 |
| Private hospital | 34 | 13 |
| Person who gave the advice | ||
| Doctors | 232 | 90.9 |
| Nurses | 16 | 6.2 |
| Dietitian | 7 | 2.9 |
| Clarity of advice | ||
| Clear | 188 | 73.7 |
| Unclear | 67 | 26.3 |
| Total | 255 | 100 |
| Ever advised about FA | ||
| Yes | 255 | 72.5 |
| No | 97 | 27.5 |
| Total | 352 | 100 |
Table 4.
Frequency distribution of participants according to their knowledge of food rich in folic acid (FA) (n=400)
| Knowledge | N | % |
| Knew some foods rich in FA | ||
| Yes | 118 | 29.5 |
| No | 282 | 70.5 |
| Thought folate in food is a sufficient source | ||
| Yes | 138 | 34.5 |
| No | 262 | 65.5 |
| Taking both food rich in folate and folic acid pills are beneficial | ||
| Yes | 311 | 77.8 |
| No | 89 | 22.2 |
| Source of information about folate-rich foods | ||
| Family | 30 | 7.6 |
| Friends | 183 | 45.7 |
| Healthcare providers | 183 | 45.7 |
| Media | 4 | 1 |
Table 5.
Frequency distribution of participants according to whether they had ever taken folic acid (FA), current users, and for what reason
| Folic acid intake | N | % |
| Currently taking folic acid supplements* | ||
| Yes | 210 | 52.5 |
| No | 190 | 47.5 |
| Have ever taken folic acid supplements† | ||
| Yes | 289 | 74.5 |
| No | 102 | 25.5 |
| Total | 400 | 100 |
| How frequently did you take folic acid supplements‡ | ||
| Daily | 165 | 55.4 |
| Weekly | 99 | 33.2 |
| Monthly | 34 | 11.4 |
| Reason for taking FA supplements | ||
| Medical advice | 223 | 80.2 |
| Family/friends advice | 33 | 11 |
| Self-initiation | 26 | 8.8 |
| Total | 298 | 100 |
*Currently using it.
†Took folic acid before.
†Frequency of using folic acid before.
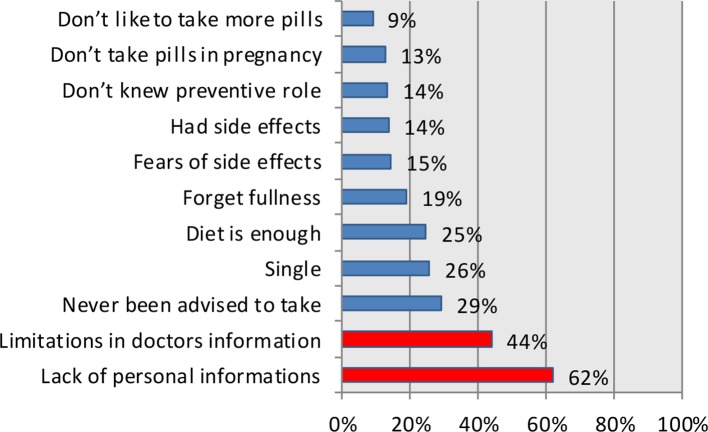
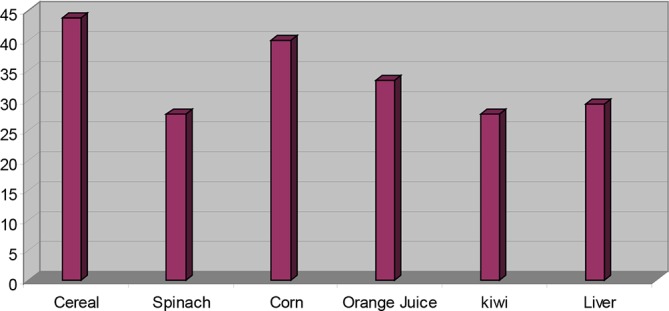
Marital status was the only statistically significant sociodemographic characteristic of the study population affecting their awareness (p=0.025; see table 6) and use of folic acid, with 81.6% of married women stating that they took folic acid pills (p=0.001; see table 7). A statistically significant relationship was established between folic acid awareness and its intake, whereby 81.8% of participants who were aware of folic acid took it as a supplement, and 88.9% of those who knew of its preventative role took folic acid supplements as a result. Of the teachers surveyed, 91% knew when to take folic acid, while 94.6% and 87.6% of those who knew the best time and the ideal duration of folic acid intake, respectively, had taken folic acid as a supplement at some point in time. Only 82% of teachers who knew the ideal frequency of folic acid intake had ever taken folic acid supplements. There is a statistically significant relationship (p<0.05) between knowledge about folic acid and being a current user of folic acid supplements; current use was particularly related to awareness of it, its preventive role, when to take it and the ideal duration of use (table 8). Concerning participants’ intake of folate-rich food, the highest proportion (43.8%) included cereals in their regular diet, followed by corn and spinach, kiwi was consumed the least (27.8% each; see figure 1). The most common barrier to folic acid intake (for 62% of respondents) was limitation of personal information about folate, while 9.2% of participants mentioned that because they were already taking many pills, they did not want to take additional supplements. About 44% said that they did not get enough information from their healthcare providers (figure 2).
Table 6.
Relation between sociodemographic characteristics and awareness about folic acid (n=400)
| Ever heard of folic acid | |||
| Characteristics | Yes | No | P value |
| N (%) | N (%) | ||
| Age | |||
| ≤35 years | 183 (90.6) | 19 (9.4) | 0.10* |
| >35 years | 169 (85.4) | 29 (14.6) | |
| Nationality | |||
| Qatari | 311 (87.4) | 45 (12.6) | 0.15† |
| Non-Qatari | 38 (95.0) | 2 (5.0) | |
| Marital status | |||
| Married | 284 (89.9) | 32 (10.1) | 0.025* |
| Non-married | 68 (81.0) | 15 (19.0) | |
| Educational level | |||
| College | 327 (88.1) | 44 (11.9) | 0.86† |
| Postgraduate education | 25 (89.3) | 3 (10.7) | |
| Place of work | |||
| Model schools | 43 (95.6) | 2 (4.4) | 0.32† |
| Primary schools | 200 (88.1) | 46 (11.9) | |
| Preparatory schools | 38 (86.4) | 6 (13.6) | |
| Secondary schools | 55 (84.5) | 10 (15.5) | |
| Family income | |||
| ≤20 000 | 151 (91.5) | 14 (8.4) | 0.18† |
| 20 001–30 000 | 161 (85.2) | 28 (14.8) | |
| >30 000 | 43 (93.5) | 3 (6.5) | |
*Χ2test.
†Fisher’s exact test.
Table 7.
Relation between sociodemographic characteristics and folic acid intake (n=400)
| Have ever taken folic acid supplements | |||
| Characteristics | Yes | No | P value |
| N (%) | N (%) | ||
| Age | |||
| ≤35 years | 152 (75.2) | 50 (24.8) | 0.72 |
| >35 years | 146 (73.7) | 52 (26.3) | |
| Nationality | |||
| Qatari | 267 (75.0) | 89 (25.0) | 0.73 |
| Non-Qatari | 29 (72.5) | 11 (27.5) | |
| Marital status | |||
| Married | 258 (81.6) | 58 (18.4) | 0.001 |
| Non-married | 40 (47.6) | 43 (52.4) | |
| Educational level | |||
| College | 278 (74.9) | 93 (25.1) | 0.68 |
| Postgraduate education | 20 (71.4) | 8 (28.6) | |
| Place of work | |||
| Model schools | 37 (82.2) | 8 (17.8) | |
| Primary schools | 169 (68.7) | 77 (31.3) | 0.58 |
| Preparatory schools | 31 (70.5) | 13 (29.5) | |
| Secondary schools | 61 (93.8) | 4 (6.1) | |
| Family income | |||
| ≤20 000 | 104 (63) | 61 (36.9) | 0.60 |
| 20 001–30 000 | 140 (74.1) | 49 (25.9) | |
| >30 000 | 37 (80.4) | 9 (19.6) | |
Table 8.
Relation between knowledge and practice of folic acid (FA) intake
| Currently taking FA supplementation | Have ever taken FA supplementations | ||||
| Knowledge | Yes (%) | No (%) | Yes(%) | No (%) | P value |
| Ever heard FA | 201 (57.1) | 151 (42.9) | 288 (81.8) | 64 (18.2) | <0.05 |
| Knew FA preventive role | 109 (67.3) | 53 (32.7) | 144 (88.9) | 18 (11.1) | <0.05 |
| Knew when to take FA | 134 (62.6) | 80 (37.4) | 195 (91.1) | 19 (8.9) | <0.05 |
| Knew the best time to take FA | 44 (59.5) | 30 (40.5) | 70 (94.6) | 4 (5.4) | <0.05 |
| Knew duration to take FA | 76 (67.3) | 37 (32.7) | 99 (87.6) | 14 (12.4) | <0.05 |
| Knew frequency | 191 (59.9) | 129 (40.1) | 264 (82.8) | 56 (17.2) | <0.05 |
Figure 1.
Distribution of participants according to the intake of folate-rich food items (n=400).
Figure 2.
Barriers related to folic acid intake.
Discussion
Periconceptional folic acid supplementation is effective in the prevention of NTDs and other congenital abnormalities and can assist in the reduction of infant morbidity and mortality. It is, therefore, important to estimate knowledge and intake of folic acid among women of childbearing age.24 25 The current study showed that the overall awareness about folic acid was relatively high; 88% of participants reported that they had heard of folic acid at some point. This may be as a result of the participants’ education level (almost all of them were college educated and higher) and three-quarters of them were married (approximately 75% were married); this comes in agreement with results from previous studies that showed that there was a direct association between educational level of women of childbearing age and their knowledge and intake of folic acid, where fortification strategies were found to offer the most cost-effective route to improve folic acid intakes and status.26 27
There’s a clear contrast here to a study conducted in Saudi Arabia among female college students, which showed that a much lower percentage (12%) were aware of the importance of folic acid.28 Our findings are consistent with the findings of Hassan’s study (2008), which was conducted in Qatar to assess folic acid intake among pregnant Qataris, of whom 94.0% were aware of folic acid.29 The current study showed that slightly more than half of the participants had heard about NTDs at some time and of these, only 23.3% of the participants lacked awareness of its preventative role in reducing these birth defects. This is in contrast with a survey undertaken in the USA, which indicated that 75% of reproductive-aged women had heard of folic acid, but only 14% knew that it prevented birth defects.30 The study by Chacko et al found that half of the young women knew the role of folic acid in the prevention of birth defects.31
The current study shows that around one-third of the participants could identify the correct time to start taking folic acid and the duration of intake, with half of them currently using folic acid. This finding comes in agreement with a retrospective hospital-based cohort study, which was done to determine the trends of NTD over a period of 25 years. The study reported NTD in 1.09 per 1000 births, with high rates of consanguinity and lack of correct intake of folic acid among mothers being major factors contributing to NTD in Qatar.32
This study’s findings were less than the results from the survey conducted in New Zealand, which showed that among women with planned pregnancies, 98.0% had heard of folic acid, 63.6% knew that folic acid could prevent birth defects and 77.4% knew the appropriate time to take folic acid.33 Intake of food rich in folic acid as part of the weekly regular diet was assessed among the participants, 43.8% included cereal in their regular diet; these results support those of Chacko et al, who found that cereal was the most frequently consumed folate-rich food, but only 37% reported adequate frequency of cereal intake.31
A comparative analysis of strategies to improve folic acid intake concluded that dietary education to change dietary habits is difficult, and often food sources of individual micronutrients are limited. Encouraging use of nutritional supplements is plagued by low adherence rates and fortification strategies were found to offer the most cost-effective route to improve folic acid intake and status.34
Fortification of cereal grain products with folic acid began in the USA, contributing to a 36% reduction in NTDs between 1996 and 2006: preventing an estimated 10 000 NTD-affected pregnancies in a decade.35 The same founded that the prevalence of NTDs declined from 2.6 per 1000 live births to 0.9 per 1000 live births.36
In this study, the younger teachers aged 35 years or below were more aware about the effects of folic acid than the older teachers. This agrees with the findings from the study by Bonin, which showed that knowledge was highest among the same younger age group.23
According to the results of our study, being married was significantly associated with better knowledge about folic acid, which can be due to the married women’s previous experiences of pregnancy. This is similar to the findings of Sen et al, which found that majority of women of childbearing age (91%) who are aware of folic acid were married.37 Our study’s results are also similar to those of a survey conducted among Irish women of childbearing age, which showed no statistical association between age, education level and family income in relation to folic acid intake.30 A comparison of our results with a survey conducted in the USA shows that there are statistically significant differences regarding knowledge of folic acid and folic acid supplement consumption, and that these differences are observed more among the age group between 25 and 34 years, women with the highest incomes and those with higher levels of education.38
The majority of participants in the current study recall hearing about folic acid from their doctors (90.9%) and their intake of folic acid supplements was dependent on medical advice, with 80.2% reporting that their intake was a result of a doctor’s advice. Both friends (45.7%) and healthcare providers (45.7%) were the most frequent sources of participants’ knowledge on folate-rich foods. This is higher than that found in the study by Chacko et al, which showed that the health sector in general (44%) and doctors in particular (27%) were the most common sources of information about folic acid.31 This shows that healthcare systems still have an opportunity to reach more women with advice surrounding the intake of folic acid in the periconceptional period, which is supported by the study of Sayers et al, where only a few women (8.7%) had received advice on taking folic acid before becoming pregnant.39
Our study showed that folic acid intake among participants was related in a statistically significant fashion with their awareness; 81.8% of participants who knew the recommended frequency of folic acid intake reported that they had used folic acid, and 49.3% of these were taking folic acid daily. This contrasts the results of the study by Chacko et al, which found that only 9% of young women reported taking a daily multivitamin, and a very small number took daily multivitamins to prevent birth defects.31
The rate of adequate supplement frequency was much higher in our study compared with that of Robert, which found that among the 77% of women who had heard about the benefits of folic acid only 26% reported that they took it daily as recommended.39 This agrees with the survey conducted among Irish women of childbearing age, which showed that despite a high level of knowledge about folic acid, the current daily intake of folic acid was still very low30 40. Another study showed that even though women aware of folic acid knew that they had to start taking it before conception, the majority still did not use it in the correct period.41
One of the limitations of the current study that planning for pregnancy, parity and history of a previous baby with anomalies (NTDs) were not studied, which might affect women knowledge and practice regarding folic acid.42
Despite that the participants in the current study were well-educated and well-off population, the right knowledge and intakes of folic acid supplementation including doses and duration still were not sufficient, which came in agreement with findings from a previous study that showed half of the studied group had correct knowledge whereas only 27% of women reached the recommended 0.4 mg/day.27 This suggests that there are still opportunities for more comprehensive patient education.
In the current study self-reported nature of the data, there is also the danger of recall bias, and participants may have over-reported or under-reported either their knowledge about or use of folic acid supplements. The teachers may not be representative of all reproductive-aged women; therefore, the generalisability of results is limited.
In addition to these knowledge gaps, this study also identified the participants’ stated barriers to folic acid intake; the most frequent barrier (62%) being the limitation of the participant’s information about folic acid, while 44% mentioned that they did not take folic acid pills specifically because they had not received enough information from their doctor. Similar results were found in a survey of women aged 18–45 years, who reported that they did not take a vitamin supplement containing folic acid because they felt that they did not need to or rather that they did not receive information about folic acid from their healthcare provider. A study by Coll et al concerning NTDs in the Mediterranean region in 2000 determined that there are three barriers related to poor intake of folic acid: low awareness of the need to take folic acid, folic acid not being prescribed in time and lack of information concerning the advantages of folic acid intake during counselling prior to conception.43
Recommendation from large community intervention trial included 247 831 women of reproductive age confirmed that periconceptional supplementation with only 0.4 mg of folic acid per day can reduce NTD risk by as much as 81%.44 The Chinese government had launched a programme that provides folic acid supplements free for eight women showed that prevalence of NTDs decreased by 22.4%.45 So improving folic acid knowledge is an essential step in promoting the use of folic acid to prevent NTDs.46 47
Supplementary Material
Acknowledgments
The authors thank all the teachers who took part in this study, and the admin staff and data collectors for their support and guidance.
Footnotes
Contributors: LA-M, NAAS and MGA-K designed the study, wrote the primary proposal, managed the data collection, review the literature, fieldwork data management and revised the manuscript. MFS updated the literature review and the discussion and results interpretation, drafted and revised the manuscript, and finalised and submitted the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Ethics approval: IRB was obtained from Hamad Medical Corporation.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
Patient consent for publication: Obtained.
References
- 1. Sharp GF, Naylor LA, Cai J, et al. Assessing awareness, knowledge and use of folic acid in kansas women between the ages of 18 and 44 years. Matern Child Health J 2009;13:814–21. 10.1007/s10995-008-0414-5 [DOI] [PubMed] [Google Scholar]
- 2. Farley TF, Hambidge SJ, Daley MF. Association of low maternal education with neural tube defects in Colorado, 1989-1998. Public Health 2002;116:89–94. 10.1016/S0033-3506(02)00509-7 [DOI] [PubMed] [Google Scholar]
- 3. Rajab A, Vaishnav A, Freeman NV, et al. Neural tube defects and congenital hydrocephalus in the Sultanate of Oman. J Trop Pediatr 1998;44:300–3. 10.1093/tropej/44.5.300 [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization. Global health estimates (GHE)–Cause-specific mortality. 2015. http://www.who.int/healthinfo/global_burden_disease/estimates/en/ (Accessed 14th Apr 2015).
- 5. World Health Organization. Global health estimates (GHE)–Disease burden. 2015. http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (Accessed 14th Apr 2015).
- 6. Behrooz A. Prevalence of neural tube defect and its relative factors in south-west of Iran. Pak J Med Sci 2007;23:654–6. [Google Scholar]
- 7. Ryan M. Folic acid to prevent neural tube defects: a potential pharmacy initiative with public health implications. Hosp Pharm 2004;39:962–9. 10.1177/001857870403901007 [DOI] [Google Scholar]
- 8. Cho S. Folic acid for the prevention of neural tube defects. Pediatrics 1999;104:325–7. [DOI] [PubMed] [Google Scholar]
- 9. International Clearinghouse for Birth Defects Surveillance and Research. International clearinghouse for birth defects surveillance and research. Annual report 2013. Rome: International Clearinghouse for Birth Defects Surveillance and Research, 2013. [Google Scholar]
- 10. European Surveillance of Congenital Anomalies. Prevalence tables. Ispra: European Surveillance of Congenital Anomalies, 2015. [Google Scholar]
- 11. Yen J, Zoumas-Morse C, Pakiz B, et al. Folate intake assessment: validation of a new approach. J Am Diet Assoc 2003;103:991–1000. 10.1016/S0002-8223(03)00471-1 [DOI] [PubMed] [Google Scholar]
- 12. Pawlak R, Brown D, Meyer MK, et al. Theory of planned behavior and multivitamin supplement use in Caucasian college females. J Prim Prev 2008;29:57–71. 10.1007/s10935-008-0127-y [DOI] [PubMed] [Google Scholar]
- 13. Krishnaswamy K, Madhavan Nair K. Importance of folate in human nutrition. Br J Nutr 2001;85:S115–24. 10.1079/BJN2000303 [DOI] [PubMed] [Google Scholar]
- 14. Toriello HV. Professional Practice and Guidelines Committee, American College of Medical Genetics. Folic acid and neural tube defects. Genet Med 2005;7:283–4. 10.1097/00125817-200504000-00009 [DOI] [PubMed] [Google Scholar]
- 15. Ren A. The prevention of neural tube defects with folic acid. World J Clin Pediatr 2015;4:41–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Unusan N. Folic acid: Protection against neural tube defects Engels JV, Focus on birth defects research. New York, NY: Nova Science Publisher, 2006:223–32. [Google Scholar]
- 17. Kurtzweil P. How folate can help prevent birth defects. Rockville, MD: Dept. of Health and Human Services, Public Health Service, Food and Drug Administration, 1996. [Google Scholar]
- 18. Perry CA, Renna SA, Khitun E, et al. Ethnicity and race influence the folate status response to controlled folate intakes in young women. J Nutr 2004;134:1786–92. 10.1093/jn/134.7.1786 [DOI] [PubMed] [Google Scholar]
- 19. Middle East Global Leadership in Wheat Flour Fortification. Flour fortification initiative middle east report. 2012. http://www.ffinetwork.org/regional_activity/middle_east.php
- 20. Bener A, Al Maadid MG, Al-Bast DA, et al. Maternal knowledge, attitude and practice on folic acid intake among Arabian Qatari women. Reprod Toxicol 2006;21:21–5. 10.1016/j.reprotox.2005.07.004 [DOI] [PubMed] [Google Scholar]
- 21. de Jong-Van den Berg LT, Hernandez-Diaz S, Werler MM, et al. Trends and predictors of folic acid awareness and periconceptional use in pregnant women. Am J Obstet Gynecol 2005;192:121–8. 10.1016/j.ajog.2004.05.085 [DOI] [PubMed] [Google Scholar]
- 22. de Jong-van den Berg LT, de Walle HE, van der Pal-de Bruin KM, et al. Increasing awareness of and behaviour towards periconceptional folic acid consumption in The Netherlands from 1994 to 1995. Eur J Clin Pharmacol 1998;54:329–31. 10.1007/s002280050468 [DOI] [PubMed] [Google Scholar]
- 23. Bonin MM. Knowledge of periconceptional folic acid for the prevention of neural tube defects: the missing links. Arch Fam Med 1998;7:438–42. 10.1001/archfami.7.5.438 [DOI] [PubMed] [Google Scholar]
- 24. Pérez-Escamilla R. Periconceptional folic acid and neural tube defects: public health issues. Bull Pan Am Health Organ 1995;29:250–63. [PubMed] [Google Scholar]
- 25. Kilker KP. Is knowing half the battle? An examination of the relationship between folic acid knowledge and awareness and daily supplementation with folic acid among 18 to 24 year old women who are not contemplating pregnancy. [Master’s Thesis] Atlanta, GA: Georgia State University, 2007. [Google Scholar]
- 26. Aronsson CA, Vehik K, Yang J, et al. Use of dietary supplements in pregnant women in relation to sociodemographic factors - a report from The Environmental Determinants of Diabetes in the Young (TEDDY) study. Public Health Nutr 2013;16:1390–402. 10.1017/S1368980013000293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pouchieu C, Lévy R, Faure C, et al. Socioeconomic, lifestyle and dietary factors associated with dietary supplement use during pregnancy. PLoS One 2013;8:e70733 10.1371/journal.pone.0070733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kari JA, Bardisi ES, Baitalmal RM, et al. Folic acid awareness among female college students. Saudi Med J 2008;29:1749–51. [PubMed] [Google Scholar]
- 29. Hassan AS, Al-Kharusi BM. Knowledge and use of folic acid among pregnant arabian women residing in Qatar and Oman. Int J Food Sci Nutr 2008;59:70–9. 10.1080/09637480701668770 [DOI] [PubMed] [Google Scholar]
- 30. Byrne J, Byrne Y. A population-based survey of knowledge and use of folic acid among Irish women. Drogheda, Ireland: Boyne Research Institute, 2006. [Google Scholar]
- 31. Chacko MR, Anding R, Kozinetz CA, et al. Neural tube defects: knowledge and preconceptional prevention practices in minority young women. Pediatrics 2003;112:536–42. 10.1542/peds.112.3.536 [DOI] [PubMed] [Google Scholar]
- 32. Kurdi B, Bener A, Hoffmann G, et al. The pattern of neural tube defects in a highly endogamous society: a 25-year incidence trends. Journal of Pediatric Neurology 2012;10:193–8. 10.3233/JPN-2012-0567 [DOI] [Google Scholar]
- 33. Mallard SR, Houghton LA. Folate knowledge and consumer behaviour among pregnant New Zealand women prior to the potential introduction of mandatory fortification. Asia Pac J Clin Nutr 2012;21:440–9. [PubMed] [Google Scholar]
- 34. de Lourdes Samaniego-Vaesken M, Alonso-Aperte E, Varela-Moreiras G, et al. Vitamin food fortification today. Food Nutr Res 2012;56:5459 10.3402/fnr.v56i0.5459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Flour Fortification Initiative. Newsletter dec 2012 anemia and neural tube birth defects decline in Bahrain. 2012. http://www.ffinetwork.org/about/stay_informed/newsletters/Q4_21012.html
- 36. Centers for Disease Control and Prevention (CDC). Ten great public health achievements-United States, 2001-2010. MMWR Morb Mortal Wkly Rep 2011;60:619–23. [PubMed] [Google Scholar]
- 37. Sen S, Manzoor A, Deviasumathy M, et al. Maternal knowledge, attitude and practice regarding folic acid intake during the periconceptional period. Public Health Nutr 2001;4:909–12. 10.1079/PHN2001123 [DOI] [PubMed] [Google Scholar]
- 38. Centers for Disease Control and Prevention (CDC). Prevalence of neural tube defects and folic acid knowledge and consumption-Puerto Rico, 1996-2006. MMWR Morb Mortal Wkly Rep 2008;57:10–13. [PubMed] [Google Scholar]
- 39. Sayers GM, Hughes N, Scallan E, et al. A survey of knowledge and use of folic acid among women of child-bearing age in Dublin. J Public Health Med 1997;19:328–32. 10.1093/oxfordjournals.pubmed.a024639 [DOI] [PubMed] [Google Scholar]
- 40. Meyer RE, Wall A, Morgan A, et al. Knowledge and use of folic acid among north Carolina women. N C Med J 2002;63:18–22. [PubMed] [Google Scholar]
- 41. de Walle HE, de Jong-van den Berg LT. Growing gap in folic acid intake with respect to level of education in the Netherlands. Community Genet 2007;10:93–6. 10.1159/000099086 [DOI] [PubMed] [Google Scholar]
- 42. Anzaku A. Assessing folic acid awareness and its usage for the prevention of neural tube defects among pregnant women in Jos, Nigeria. Journal of Basic and Clinical Reproductive Sciences 2013;2:13–17. 10.4103/2278-960X.112574 [DOI] [Google Scholar]
- 43. Coll O, Pisa S, Palacio M, et al. Awareness of the use of folic acid to prevent neural tube defects in a mediterranean area. Eur J Obstet Gynecol Reprod Biol 2004;115:173–7. 10.1016/j.ejogrb.2003.12.009 [DOI] [PubMed] [Google Scholar]
- 44. Berry RJ, Li Z, Erickson JD, et al. Prevention of neural-tube defects with folic acid in China. China-U.S. Collaborative project for neural tube defect prevention. N Engl J Med 1999;341:1485–90. 10.1056/NEJM199911113412001 [DOI] [PubMed] [Google Scholar]
- 45. Ministry of Health. Birth defects prevention and control in China. http://www.gov.cn/gzdt/att/att/site1/20120912/1c6f6506c7f811bacf9301.pdf (Accessed 18th Apr 2014).
- 46. Murphy BL, Dipietro NA, Kier KL. Knowledge and use of folic acid among college women: a pilot health promotion program led by pharmacy students and faculty. Pharm Pract 2010;8:220–5. 10.4321/S1886-36552010000400003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Cena ER, Joy AB, Heneman K, et al. Learner-centered nutrition education improves folate intake and food-related behaviors in nonpregnant, low-income women of childbearing age. J Am Diet Assoc 2008;108:1627–35. 10.1016/j.jada.2008.07.017 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.