Abstract
Cat-scratch disease (CSD) is usually a self-limiting infection that in the majority of cases occurs as lymphadenitis in children who have been scratched or bitten by a cat. Rarely, Bartonella henselae is cause of fever of unknown origin (FUO), with dissemination to various organs, mimicking an inflammatory rather than a lymphoproliferative disease. This manuscript will present a case of thoracic manifestations of CSD in an immunocompetent 2-years baby without history of cat contact, with fever of unknown origin, investigated by chest CT and MRI. (www.actabiomedica.it)
Keywords: Cat-scratch disease, pediatrics, magnetic resonance, Bartonella henselae, chest
A previously healthy 2-year-old girl was admitted to our hospital with a history of 6 weeks of intermittent fever and a pulmonary consolidation in the left lower lobe, treated with amoxicillin-clavulanic acid and antipyretics therapy at home. Any localising signs or symptoms were found during physical examination, in particular no enlarged palpable lymphnodes and no skin lesions were detected.
Complete blood count was normal, C-reactive protein (CRP) was 1,9 mg/dl, while the erythrocyte sedimentation rate (ESR) and fibrinogen values were in the normal ranges. She tested negative for Epstein–Barr virus, Pneumococcus, Staphilococcus aureus and Streptococcus pyogene, Mycobacterium Tubercolosis bacilli. Quantiferon test was negative and no tuberculosis bacilli were found in broncoalveolar lavage. Vanillylmandelic acid (VMA) test and other routine serum chemistries were performed with negative results.
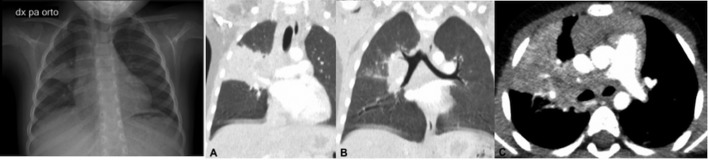
A chest radiograph demonstrated a large pulmonary consolidation in the upper right lobe associated with mediastinal bulging on the right side (Figure 1). Any consolidation was seen in the left lung. Bronchoscopy yielded normal findings. Ultrasonic examination of abdominal organs was negative too.
Figure 1.
On the left side, Chest X-Ray (anterior-posterior projection), shows a large pulmonary consolidation in the upper right lobe. Notice the widened mediastinum on the right. On the right side see coronal reformatted CT images (A,B) showing a large perilar consolidation involving the upper right lobe, without air bronchogram. C. Axial contrast-enhanced CT image reveals a large soft tissue attenuation mass occupying the mediastinal space
During the hospitalization the girl underwent a chest CT scan with contrast medium that confirmed the consolidation of the upper right lobe and revealed a large soft tissue attenuation mass occupying the mediastinum: it extended from the anterior to posterior mediastinum, occupying the pretracheal space, involving the right hilum and the space behind the heart (Figure 2). This mass was characterized by homogenous contrast enhancement without signs of necrosis inside. No pleural effusion was detected. Our first hypothesis was a pneumonia associated with a wide mediastinal lymphonode pack, but we were not able to exclude a lymphomatous mass.
Figure 2.
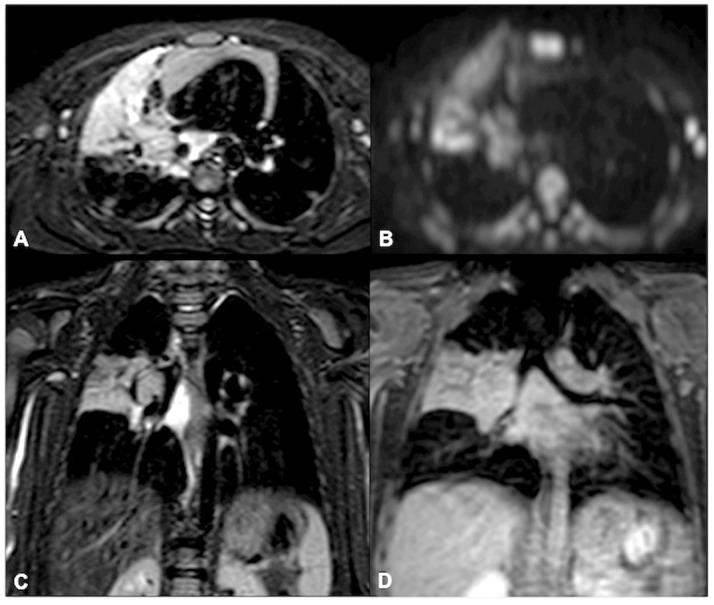
MR imaging shows a solid and homogenous mediastinal mass characterized by high signal intensity on T2-weighted (A) sequence, DWIBS (B) sequence and STIR images (C). D. Shows the enhancement of mediastinal mass after gadolinium injection on suppressed T1-weighted images
A chest MR was also performed confirming the presence of a solid and homogenous mediastinal mass, that was characterized by high signal intensity on STIR images and DWIBS sequences, and moderate enhancement after intravenous Gadolinium injection. Thymus presented normal appearance and signal intensity.
In order to exclude lymphoproliferative disease, the girl underwent a bone marrow aspiration but any abnormal results were found. Finally a CT-guided biopsy of the mediastinal mass was performed and the polymerase chain reaction (PCR) effectively provided laboratory diagnosis of Bartonella henselae.
Discussion
Bartonella henselae, is a gram-negative bacillus, acquired from a bite or a scratch of a cat, that causes typical manifestations of the Cat-Scratch Disease (CSD) as fever and regional lymphadenitis of the region of inoculation (1-5). The majority of cases presents painful but self-limited lymphadenopathies, especially of the neck, axillary region or upper extremities. Just in few cases Bartonella h. may cause only prolonged fever of unknown origin, without lymphadenopathies (5-25% of patients) (6-11).
More rarely (5-14%) this infection may have atypical manifestations caused by hematogenous spread of the germ leading to systemic disease (4-7). In these cases Bartonella h. may present atypical manifestations as hepatic and splenic abscess, endocarditis, encephalopathy osteomyelitis, Perinaud oculoglandular disease, neuroretinitis (6).
In our case, the patient presented prolonged fever of unknown origin and a large solid mass of mediastinum diagnosed as lymphnodes pack, associated with pulmonary consolidation, without pleural effusion.
The diagnostic process included the evaluation of systemic infectious and non infectious disease causing mediastinal lymphadenopathy, as tuberculosis (TB), sarcoidosis, lymphoma or metastatic disease (12-17).
In the 44% of patients with TB, mediastinal lymphnodes are enlarged with evidence of caseous necrosis (13, 14). Sarcoidosis, especially the juvenile type, is a multisystem granulomatous disease characterized by mediastinal non-caseating lymph nodes enlargement (18, 19).
Lymphoma is a systemic disease that may be easily confused with tuberculosis or sarcoidosis in case of mediastinal lymphadenopathies (13, 14).
Pathologically lymph nodes affected by Bartonella h. present a granuloma with central avascular necrosis and cortical thickening and germinal hypertrophy (1), so they may be easily mistaken for metastasis. Conversely, neoplastic lymphadenopathy shows central necrosis only after radiotherapy or chemotherapy (16, 17, 20).
Therefore lymphadenopathy associated with persistent fever is a nonspecific finding because it may be associated with variable etiologies, so the diagnosis is not easy cause the overlapping of clinical and imaging findings.
In our case imaging showed a nonspecific mediastinal mass, the etiology of which was demonstrated by laboratory after biopsy.
In conclusion, the definitive diagnosis in a patient with mediastinal lymphadenopathy needs of an extensively investigation by a detailed history, an accurate physical and laboratory examination and a good reading of Imaging.
Informed consent:
informed consent was obtained from all individual participants included in the study.
References
- 1.Reddy AK, Morriss MC, Greg I. Utility of MR imaging in cat-scratch neuroretinitis. Pediatr Radiol. 2007;37:840–3. doi: 10.1007/s00247-007-0514-1. [DOI] [PubMed] [Google Scholar]
- 2.Margileth AM. Recent advances in diagnosis and treatment of cat scratch disease. Curr Infect Dis Rep. 2000;2:141–6. doi: 10.1007/s11908-000-0026-8. [DOI] [PubMed] [Google Scholar]
- 3.Massei F, Messina F, Talini I, et al. Widening of the clinical spectrum of Bartonella henselae infection as recognized through serodiagnostics. Eur. J. Pediatr. 2000;159:416–9. doi: 10.1007/s004310051298. [DOI] [PubMed] [Google Scholar]
- 4.Rolain JM, Brouqui P, Koehler JE, et al. Recommendations for treatment of human infections caused by bartonella species. Antimicrob Agents Chemother. 2004;48:1921–33. doi: 10.1128/AAC.48.6.1921-1933.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang C-W, Chang W-C, Chao T-K, et al. Computed tomography and magnetic resonance imaging of cat-scratch disease: a report of two cases. Clinical Imaging. 2009;33:31–21. doi: 10.1016/j.clinimag.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Conrad DA. Treatment of cat-scratch disease. Curr Opin Pediatr. 2001;13:56–9. doi: 10.1097/00008480-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Mafee MF. Ocular manifestations of cat-scratch disease: role of MR imaging. AJNR. 2005;26:1303–4. [PMC free article] [PubMed] [Google Scholar]
- 8.Verdon R, Geffray L, Collet T, et al. Vertebral ostemyelitis due to Bartonella henselae in adults: a report of 2 cases. Clin Infect Dis. 2002;35:e141–2. doi: 10.1086/344791. [DOI] [PubMed] [Google Scholar]
- 9.Modi S, Epphes S, Klein J. Cat-scratch disease presenting as multifocal osteomyelitis with toracic abscess. Pediatr Infect Dis J. 2001;20:1006–7. doi: 10.1097/00006454-200110000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Hipp S, O’Shields A, Fordham L, Blatt J, Hamrick H, Henderson F. Multifocal bone marrow involvement in cat-scratch disease. Pediatr Infect Dis J. 2005;24:472–4. doi: 10.1097/01.inf.0000160993.52059.3a. [DOI] [PubMed] [Google Scholar]
- 11.Walls T, Moshal K, Trounce J, Hartley J, Harris K, Davies G. Broad-range polymerase chain reaction for the diagnosis of Bartonella henselae endocarditis. J Pediatr Child Health. 2006;42:469–71. doi: 10.1111/j.1440-1754.2006.00900.x. [DOI] [PubMed] [Google Scholar]
- 12.Göknar N, Çakır E, Çakır FB, Kasapcopur O, Yegen G, Gedik AH, Oktem F. A Difficult Case of Hodgkin Lymphoma with Differential Diagnosis of Tuberculosis and Sarcoidosis. Hematol Rep. 2015 Jun 8;7(2):5644. doi: 10.4081/hr.2015.5644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta D, Agarwal R, Aggarwal AN, Jindal SK. Sarcoidosis and tuberculosis: the same disease with different manifestations or similar manifestations of different disorders. Curr Opin Pulm Med. 2012 Sep;18(5):506–16. doi: 10.1097/MCP.0b013e3283560809. [DOI] [PubMed] [Google Scholar]
- 14.Gobbi PG, Ferreri AJ, Ponzoni M, Levis A. Hodgkin lymphoma. Crit Rev Oncol Hematol. 2013 Feb;85(2):216–37. doi: 10.1016/j.critrevonc.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 15.Dong PR, Seeger LL, Yao L. Uncomplicated cat-scratch disease: findings at CT, MR imaging, and radiography. Musculoskelet Radiol. 1995;195:837–9. doi: 10.1148/radiology.195.3.7754017. [DOI] [PubMed] [Google Scholar]
- 16.Fox BC, Guttler RA. Cat-scratch disease mimicking rhabdomyosarcoma. Orthop Rev. 1993;22:1148–9. [PubMed] [Google Scholar]
- 17.Bracke P, Vanhoenacker F, Schepper AM. Berlin: Springer Co; 2001. Soft tissue lymphoma. Imaging of soft tissue tumors; pp. 427–32. [Google Scholar]
- 18.Lazarus A. Sarcoidosis: epidemiology, etiology, pathogenesis, and genetics. Dis Mon. 2009 Nov;55(11):649–60. doi: 10.1016/j.disamonth.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Fretzayas A, Moustaki M, Vougiouka O. The puzzling clinical spectrum and course of juvenile sarcoidosis. World J Pediatr. 2011 May;7(2):103–10. doi: 10.1007/s12519-011-0261-0. [DOI] [PubMed] [Google Scholar]
- 20.Rohr A, Saettele MR, et al. Spectrum of radiological manifestations of paediatric cat-scratch disease. Pediatr Radiol. 2012;42:1380–4. doi: 10.1007/s00247-012-2451-x. [DOI] [PubMed] [Google Scholar]