Abstract
Background and Aim: Applying fractional flow reserve (FFR) recently helped to assess borderline coronary defects and also facilitates assessment of these lesions. The present study aimed to assess cost-effectiveness of FFR in detection of these borderline lesions. Methods: This cross-sectional study was conducted on140 consecutive patients with 219 diseased arteries who underwent coronary angiography and suffered intermediate coronary lesions. Results: Of 18 patients who candidate for CABG before FFR, only one patient underwent CABG after determining FFR (P-value<0.05), while 15 patients were scheduled for PCI and 2 patients for medical treatment. Of 122 patients who candidate for PCI, 59 were programmed to underwent PCI after FFR determination (P-value<0.05), while the strategy in 63 patients (47 with one-vessel disease, 15 with two vessel diseases, and 1 with three vessel diseases) was modified to medical treatment. Considering strategy modifying from PCI to medical treatment, 101 stents were saved (P-value<0.05). Also, in change of strategy from CABG to PCI, spending has decreased as much as 77.3% (P-value<0.05). Furthermore, the change of treatment approach from PCI on much number of coronary vessels to PCI on less number of coronary lesions led to saving of 52.2% of costs (P-value<0.05). Conclusions:In patients with an intermediate coronary lesion, measuring FFR to guide the decision to determine treatment strategy may lead to significant cost savings. (www.actabiomedica.it)
Keywords: fractional flow reserve, myocardial, coronary vessels, cost-benefit analysis, percutaneous coronary intervention, coronary artery bypass
Introduction
Management of moderate coronary lesions in coronary angiography which is defined as coronary stenosis between 50 to 70 percent by eyeball estimation is a challenging issue. Recently, applying fractional flow reserve (FFR) helped to assess moderate coronary stenosis and also facilitate assessment of these lesions in catheterization laboratory (1-3). This parameter is defined as the ratio of pressure distal to stenosis to aortic pressure (4, 5). Different studies have shown that the FFR lower than 0.75 can predict cardiac ischemia with a high level of accuracy (6-8). Furthermore, deferring PCI in the presence of FFR<0.75 can significantly diminish long-term adverse events of revascularization procedures (9). Besides helpful role of cardiovascular diagnostic procedures, the cost-effectiveness of these procedures should be considered judiciously (10-12). In this context, the cost-effectiveness of FFR is currently under survey and there are a small number of studies on this subject. In several studies, high effectiveness of FFR for diagnosis of borderline coronary lesions has been revealed (13-16); however in some other studies, the cost of coronary pressure wire for assessment of moderate coronary lesions has been reported noticeably high (17, 18). The present study aimed to assess cost-effectiveness of FFR in detection of these moderate coronary lesions.
Materials and methods
This cross-sectional study was conducted on140 consecutive patients who were candidate for coronary angiography and had moderate coronary lesions (coronary stenosis between 50 to 70 percent in angiography). The patients were randomly assigned into two groups that undergoing CABG or PCI without considering FFR value (control group) and undergoing these procedures when FFR estimated less than 0.75 (case group). Baseline information including demographics and medical history of patients were recorded. Cost-effectiveness of the two procedures (defined as reduction in necessitating CABG or PCI and also reduction of materials and agents which are needed for revascularization) was assessed and compared between the two study groups. Results were showed as mean ± standard deviation (SD) for quantitative variables and were summarized by frequency (percentage) for clear-cut variables. Continuous variables were compared using T-Test and Mann-Whitney test. On the other hand, categorical (clear-cut) variables were compared using chi-square test. For the statistical analysis, the statistical software SPSS version 20.0 for windows (SPSS Inc., Chicago, IL) was used. P values less than 0.05 were considered statistically significant.
Results
Totally, 140 patients were included in our study. The mean age was 58.71 ± 9.88 years ranged 33 to 83 years and 64.3% were male. The most common cardiovascular risk factors were hypertension (57.9%) followed by hyperlipidemia (42.9%), diabetes mellitus (36.4%), and cigarette smoking (29.3%). Family history of coronary disease was revealed in 22.9% and 15.7% were obese. Regarding clinical symptoms, 66.4% had chest pain, 10.7% had dyspnea, and 22.9% had both symptoms. Mean LVEF was 51.19 ± 9.46 in echocardiography. In coronary angiography, 36.4% had single-vessel disease, 38.6% had two-vessel disease, and 25% had three-vessel disease. Also, the number of coronary vessels needing angioplasty was one vessel in 45%, two vessels in 37.1%, and three vessels in 12.9%.
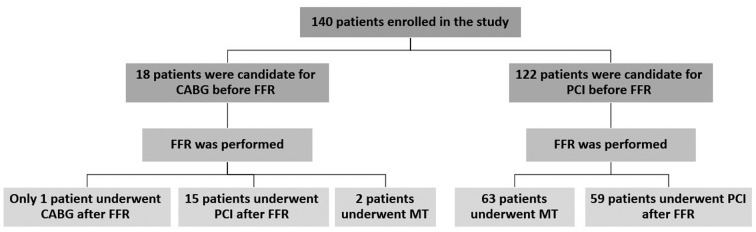
Of 18 patients who candidate for CABG before FFR, only one patient underwent CABG after determining FFR (P-value<0.05), while 15 patients were scheduled for PCI and 2 patients for medical treatment. Of 122 patients who candidate for PCI, 59 were programmed to underwent PCI after FFR determination (P-value<0.05), while the strategy in 63 patients (47 with one-vessel disease, 15 with two vessel diseases, and 1 with three vessel diseases) was modified to medical treatment (Figure 1). In those with remained PCI strategy, PCI on two vessels was modified to one vessel in 27 cases, PCI on three vessels was modified to two vessels in 4 cases, and PCI on three vessels was modified to one vessel in 8 cases(P-value<0.05). In total, considering strategy modifying from PCI to medical treatment, 101 stents were saving (P-value<0.05). Also, in change of strategy from CABG to PCI, spending has decreased as much as 77.3% (P-value<0.05). Furthermore, the change of treatment approach from PCI on more coronary vessels to PCI on less coronary lesions led to saving 52.2% of cost spending(P-value<0.05).
Figure 1.
Patients treatment plan before and after performance of FFR; table under the diagram, shows 1-year follow up results of each groups. CABG: coronary artery bypass graft; FFR: fractional fellow reserve; MT: medical therapy; PCI: percutaneous coronary intervention
In 1-year follow up, in the “PCI before FFR” arm, of 63 patients who finally underwent medical treatment after FFR, only one patient had non-STEMI who was admitted and PCI was performed for the patient; also, one mortality due to non-cardiovascular causes was recorded; of 59 patients who finally underwent PCI after FFR, only one re-admission due to unstable angina was recorded and managed conservatively. In the “CABG before FFR“, of 15 patients who finally underwent PCI after FFR, only one patient re-admitted due to unstable angina and managed conservatively; those patients who finally underwent medical treatment or CABG, revealed no adverse event after 1-year follow up. All of these results were showed in the table under the diagram (Figure 1).
Discussion
The cost of interventions and related materials in the field of cardiology and cardiac surgery is one of the essential issues of health care systems and all efforts are focused to lessen these costs as much as possible. The main goal of the present study was to assess cost-effectiveness of FFR in determining reasonable treatment approach in patients with moderate coronary lesions (coronary stenosis between 50 to 70 percent). In fact, decision on selecting the best treatment method in these patients had been ever challenging; thus inappropriate selection of treatment method may result in adverse consequences and also unnecessary expenditure. Thus, the current study aimed to determine the role of FFR on reduction of treatment costs and cost-effectiveness. Based on our results, assessment of FFR before therapeutic procedures can effectively reduce costs. On the other hand, in most patients scheduled for CABG, the type of protocol was changed from CABG to PCI or medical treatment leading considerably decrease of medical costs. Also, notable number of patients programmed to undergo PCI on coronary lesions were considered to undergo PCI on less lesions or even to receive medical treatment. In total, it seems that those patients with moderate coronary lesions can finally managed by medical treatment after considering FFR.
Almost all previous reports confirm high cost-effectiveness of FFR in CAD patients (19). In one study, the FFR strategy saved 1795 dollars per patient compared with the nuclear stress imaging study strategy and 3830 dollars compared with the stenting of all intermediate lesions strategy, while quality-adjusted life expectancy was similar among the 3 strategies (20). In another study of patients with multi-vessel CAD and borderline lesions, FFR measurement identified those who can be treated conservatively with a good long-term outcome and prevented unnecessary PCI (21). In another investigation; Two-thirds of those for whom PCI had appeared to be warranted, were treated conservatively; and only one quarter of the original “surgical” group underwent CABG (22). It was shown that the decision for bypass surgery was supported by FFR; in FFR above 0.75, a conservative approach was acceptable (13).
As a conclusion, in patients with an intermediate coronary lesion, measuring FFR to guide the decision to determine treatment strategy may lead to significant cost savings. Our study is a single center study with relatively small sample size and limited resources; and is considered as a pilot study for future large multicenter studies. The result of our pilot study revealed that FFR-guided interventions (including PCI or CABG) of moderate coronary lesions could be more cost-effective in comparison of conventional decision for PCI or CABG.
References
- 1.de Bruyne B, Bartunek J, Sys SU, et al. Simultaneous coronary pressure and flow velocity measurements in humans. Feasibility, reproducibility, and hemodynamic dependence of coronary flow velocity reserve, hyperemic flow versus pressure slope index, and fractional flow reserve. Circulation. 1996;94:1842–9. doi: 10.1161/01.cir.94.8.1842. [DOI] [PubMed] [Google Scholar]
- 2.De Bruyne B, Pijls NH, Barbato E, et al. Intracoronary and intravenous adenosine 5’-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation. 2003;107:1877–83. doi: 10.1161/01.CIR.0000061950.24940.88. [DOI] [PubMed] [Google Scholar]
- 3.Legalery P, Seronde MF, Meneveau N, et al. Measuring pressure-derived fractional flow reserve through four French diagnostic catheters. Am J Cardiol. 2003;91:1075–8. doi: 10.1016/s0002-9149(03)00151-6. [DOI] [PubMed] [Google Scholar]
- 4.De Bruyne B, Baudhuin T, Melin JA, et al. Coronary flow reserve calculated from pressure measurements in humans. Validation with positron emission tomography. Circulation. 1994;89:1013–22. doi: 10.1161/01.cir.89.3.1013. [DOI] [PubMed] [Google Scholar]
- 5.McGeoch RJ, Oldroyd KG. Pharmacological options for inducing maximal hyperaemia during studies of coronary physiology. Catheter Cardiovasc Interv. 2008;71:198–204. doi: 10.1002/ccd.21307. [DOI] [PubMed] [Google Scholar]
- 6.De Bruyne B, Sarma J. Fractional flow reserve: a review: invasive imaging. Heart. 2008;94:949–59. doi: 10.1136/hrt.2007.122838. [DOI] [PubMed] [Google Scholar]
- 7.Pijls NH, De Bruyne B, Peels K, et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334:1703–8. doi: 10.1056/NEJM199606273342604. [DOI] [PubMed] [Google Scholar]
- 8.Pijls NH, Van Gelder B, Van der Voort P, et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92:3183–93. doi: 10.1161/01.cir.92.11.3183. [DOI] [PubMed] [Google Scholar]
- 9.Wijns W, De Bruyne B, Vanhoenacker PK. What does the clinical cardiologist need from noninvasive cardiac imaging: is it time to adjust practices to meet evolving demands? J Nucl Cardiol. 2007;14:366–70. doi: 10.1016/j.nuclcard.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 10.Bech GJ, De Bruyne B, Pijls NH, et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation. 2001;103:2928–34. doi: 10.1161/01.cir.103.24.2928. [DOI] [PubMed] [Google Scholar]
- 11.Fard-Esfahani A, Assadi M, Saghari M, et al. The role of myocardial perfusion imaging in the evaluation of patients undergoing percutaneous transluminal coronary angioplasty. Hellenic J Cardiol. 2009;50:396–401. [PubMed] [Google Scholar]
- 12.Pijls NH, van Schaardenburgh P, Manoharan G, et al. Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol. 2007;49:2105–11. doi: 10.1016/j.jacc.2007.01.087. [DOI] [PubMed] [Google Scholar]
- 13.Bech GJ, Droste H, Pijls NH, et al. Value of fractional flow reserve in making decisions about bypass surgery for equivocal left main coronary artery disease. Heart. 2001;86:547–52. doi: 10.1136/heart.86.5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Legutko J, Dudek D, Rzeszutko L, et al. Fractional flow reserve assessment to determine the indications for myocardial revascularisation in patients with borderline stenosis of the left main coronary artery. Kardiol Pol. 2005;63:499–506. discussion 07-8. [PubMed] [Google Scholar]
- 15.Lindstaedt M, Spiecker M, Perings C. How good are experienced interventional cardiologists at predicting the functional significance of intermediate or equivocal left main coronary artery stenoses? Int J Cardiol. 2007;120:254–61. doi: 10.1016/j.ijcard.2006.11.220. [DOI] [PubMed] [Google Scholar]
- 16.Lindstaedt M, Yazar A, Germing A, et al. Clinical outcome in patients with intermediate or equivocal left main coronary artery disease after deferral of surgical revascularization on the basis of fractional flow reserve measurements. Am Heart J. 2006;152:156.e1–9. doi: 10.1016/j.ahj.2006.03.026. [DOI] [PubMed] [Google Scholar]
- 17.Hamilos M, Muller O, Cuisset T, et al. Long-term clinical outcome after fractional flow reserve-guided treatment in patients with angiographically equivocal left main coronary artery stenosis. Circulation. 2009;120:1505–12. doi: 10.1161/CIRCULATIONAHA.109.850073. [DOI] [PubMed] [Google Scholar]
- 18.Suemaru S, Iwasaki K, Yamamoto K, et al. Coronary pressure measurement to determine treatment strategy for equivocal left main coronary artery lesions. Heart Vessels. 2005;20:271–7. doi: 10.1007/s00380-005-0849-1. [DOI] [PubMed] [Google Scholar]
- 19.Petraco R, Sen S, Nijjer S, et al. Fractional flow reserve-guided revascularization: practical implications of a diagnostic gray zone and measurement variability on clinical decisions. JACC Cardiovasc Interv. 2013;6:222–5. doi: 10.1016/j.jcin.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 20.Fearon WF, Yeung AC, Lee DP, et al. Cost-effectiveness of measuring fractional flow reserve to guide coronary interventions. Am Heart J. 2003;145:882–7. doi: 10.1016/S0002-8703(03)00072-3. [DOI] [PubMed] [Google Scholar]
- 21.Reczuch K, Jankowska E, Telichowski A, et al. Measurement of fractional flow reserve in patients with multi-vessel coronary artery disease and borderline lesions prevents unnecessary revascularisation procedures. Kardiol Pol. 2004;60:311–19. discussion 20-1. [PubMed] [Google Scholar]
- 22.Trivedi S, Aroney CN, Walters DL, et al. Measurement of myocardial fractional flow reserve is a cost-effective way to identify coronary artery lesions of indeterminate severity that warrant revascularisation. Heart Lung Circ. 2005;14:239–41. doi: 10.1016/j.hlc.2005.06.001. [DOI] [PubMed] [Google Scholar]