Abstract
Background: Effective collaboration among health professionals is an essential component to ensure quality of care. Many adverse events experienced by patients are attributed to misunderstanding or poor communication among members of the interprofessional team. Interprofessional simulation is a learning strategy used to improve collaboration and facilitate communication between medical and nursing students. Aim of the work: To determine the efficacy of educational program based on high-fidelity interprofessional simulation aimed at improving collaborative attitude. Method: For this purpose, a protocol for a planned single-center, non-blinded and Randomized Controlled Trial (RCT) was chosen. The present has been approved by the Ethics Committee of Area Vasta Emilia Nord (Italy) (n° 479/2018). All students attending the second and third year of nursing and all resident physicians in anesthesia, reanimation, intensive care and pain management of University of Modena and Reggio Emilia, will be recruited and randomly assigned to two groups. The Experimental Group (EG) will receive an educational intervention based on high-fidelity simulation and the Control Group (CG) will attend a traditional classroom lesson. Jefferson Scale of Attitudes toward Physician-Nurse Collaboration (JSAPNC) and Readiness for Interprofessional Learning Scale (RIPLS) will be administered before and after the educational program in both the EG and CG. Conclusion: Expected outcomes is that, at the end of the study, nursing students and resident physicians who participated in the interprofessional simulation show significantly higher levels of interprofessional collaboration compared to the CG, evaluated through the JSAPNC.
Keywords: high-fidelity interprofessional simulation, interprofessional collaboration, educational program, nursing student, resident physician
Introduction
Effective collaboration among health professionals is an essential component to guarantee safety and quality in health care (1-5). According to several authors, many errors and adverse events are frequently correlated to poor quality of communication between the members of the interprofessional team and to poor teamwork skills (6-13). In contrast, the Interprofessional Collaborative Practice (ICP) promotes the reduction of care-associated infections, hospital readmissions and patient mortality (14-17). Recent studies highlight that highly efficient teamwork among health care professionals is associated with increased patient satisfaction, with reduced costs for the healthcare system and with a lower turnover of health staff members (13, 18-21). The ICP can be defined as a decision-making process between two cooperating roles, such as physician and nurse, characterized by interdependence, trust, respect, open communication and shared responsibilities in order to promote and improve patient care (22-26). In the healthcare settings, where patient outcomes are influenced by effective communication and interprofessional collaboration, there is a need for better interdisciplinary teamwork preparation of future professionals (3, 27, 28). Despite the fact that physicians and nurses work together, their academic courses are separate and the training in effective strategies of communication and care participation is often postponed to the future professional practice (29, 30). On the contrary, Inter-Professional Education (IPE) is considered by important international organizations [Institute of Medicine (US), World Health Organization, Joint Commission (US), Agency for Healthcare Research and Quality (US)] as an essential educational requirement in the health professional curricula (31-34). IPE has been defined as occasions “where students from two or more professions in health and social care learn together during all or part of their professional training with the object of cultivating collaborative practice for providing improved quality of care” (35, 36). According to the literature, students trained to use the IPE approach more likely become members of collaborative teams where the autonomy and the role of each profession are recognized (2, 37). In addition, IPE programs prevent the development of negative attitudes and prejudices and increase the importance of teamwork both in physicians and nurses (4, 5, 37-43). Medical students scored lower on readiness for IPE than nursing students, but they presented higher need for collaboration (44).
The use of simulation or standardized patients in IPE had a positive effect on readiness for IPE (45).
Clinical simulation is an interdisciplinary teaching strategy that can be used to facilitate the ICP and to improve communication skills between medical students and nurses in a skill lab context (13, 46-48). Simulation is an activity that allows replication of clinical care in a safe environment for students, without the pressure and the complexity of a real care environment, improving the integration of theory and practice (49-53). Traineeship and competency development are essential parts of clinical teaching (54) and realistic simulation can be an effective training method, especially if it is supported by the presence of trained instructors (55, 56). The simulation environment is therefore a controlled and low-risk pedagogical context, where the students, supported by a tutor, can feel free to learn without putting patients at risk (48). The necessity to guarantee reliable and safe treatment to the assisted people means that the simulation has acquired an increasingly important role in university education (57, 58). Being actively involved in the simulation process can provide a learning integration, which combines the theoretical foundations with clinical practice, favoring critical and thoughtful thinking in the students (59-63). In the simulation laboratory, students can develop technical and communication, problem solving and decision making skills (53, 61, 64-68). The benefits of the simulation procedure were analyzed by a meta-analysis and a systematic review, which showed that, compared to traditional learning methods, simulation improves students’ knowledge, skills and behavior and, consequently, patients’ treatment and care (66, 69). The scenarios planned for the simulated health activities create the conditions favoring teamwork and integration among professions in order to improve care programs and paths (70). Although some authors report cases of efficient interprofessional simulations, many questions are still open about the feasibility, acceptability, efficacy and changes in attitudes of the students who participate in simulations (71). Moreover, in many cases the effectiveness of these educational interventions has been evaluated without the necessary psychometric assessment (72). Since the interprofessional simulation requires a significant use of economic and human resources, its adoption can be justified only if trainers implement valid and reliable outcome measures (73). An integrative recent review (2018) on the use of interprofessional learning and simulation in undergraduate nursing programs concluded that the IPE and simulation, used together, show a positive impact on the development of communication skills and collaboration of nursing students (74). The authors concluded that, although among the eight included research studies none were randomized and controlled, meticulous methodology of studies could have minimized biases, predominantly due to the use of convenience sampling. Also the systematic review of Rutherford-Hemming & Lioce (2018) suggested that more studies with rigorous designs are needed to compare outcomes of IPE (75). Finally, Labrague et colleagues conclude their review by observing that an important aspect that warrants attention is the lack of RCT studies, 96% of the studies were not RCTs, therefore, one may question whether the interprofessional simulation caused significant improvement in interprofessional competencies or such changes were caused by other factors (76).
In the 2016-2017 Academic Year (A.Y.), a sample composed of three student groups of the University of Modena and Reggio Emilia 108, nursing students, 18 students of obstetrics and 20 residents in the School of Specialization in Pediatrics, participated in an interprofessional training program aimed at developing collaborative attitudes (77). The training intervention consisted of a preparatory meeting, a high-fidelity simulation “Reanimation of a new-born infant in a neonatal island” and a debriefing. The effects of the simulation was measured through the Jefferson Scale of Attitudes towards Physician-Nurse Collaboration (JSAPNC) (78), which showed a significant increase in the attitude of interprofessional collaboration only among nursing students but not in the other two groups of participants. The results of this study, which reports one of the first Italian experiences of simulated interprofessional didactics, suggest the value of simulation in improving interprofessional cooperative attitude, even though the low number of obstetric students and resident physicians may have influenced the lack of significant results (77).
In line with the literature, which promotes the research of strong experimental evidence of the effect of IPE combined with simulation activities (79), the aim of the present study is to evaluate the attitude of collaboration between nursing students and resident physicians in anesthesia, reanimation, intensive care and pain management, through an interprofessional simulation. The assumption is that, at the end of the study, nursing students and resident physicians in specialist training who participated in the interprofessional laboratory based on a high-fidelity simulation, show significantly higher levels of collaborative attitudes than the group of nursing students and resident physicians who participated in the standard education.
Method
Study design
This study protocol describes the design of a single-center, non-blinded, parallel-group RCT (1:1 ratio). A randomized, controlled, monocentric study will be carried out, involving two parallel groups of students, the Experimental Group (EG) and the Control Group (CG): in both groups, the interprofessional collaboration will be measured before (T0) and after (T1) their education session based on high-fidelity simulation for EG and traditional classroom lesson for CG. The study will be conducted at the Advanced Training and Medical Simulation Center of the Faculty of Medicine and Surgery of the University of Modena and Reggio Emilia and will last 12 months, starting from 1 October 2018.
The study protocol is consistent with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) and conforms with the Consolidated Standards of Reporting Trials (CONSORT) statement for reporting RCTs (80, 81).
Study population
The students attending the 2nd and 3rd year of the nursing course and the resident physicians of the school of specialization in anesthesia, reanimation, intensive care and pain management, of the University of Modena and Reggio Emilia, during the 2018-2019 A.Y., will be considered eligible and invited to participate in the study. All members will be informed of objectives and methods of the study. Their participation will be voluntary. All participants will be asked to sign an informed consent.
Inclusion criteria
- Enrollment in the second or third year of the nursing course for nursing students in the 2018-2019 A.Y.,
- Enrollment in one of 5 years of the specialization school in anesthesia, reanimation, intensive care and pain management in the 2018-2019 A.Y.
Exclusion criteria
- Irregularity in the payment of university fees for both nursing students and residents,
- Refusal of written informed consent.
After having agreed to participate in the study, nursing students and residents will be allocated to one of the two groups (EG and CG) through a randomization list generated by software (Figure 1). The study will be conducted in the 2018-2019 A.Y. (from 1-10-2018 to 30-9-2019).
Figure 1.
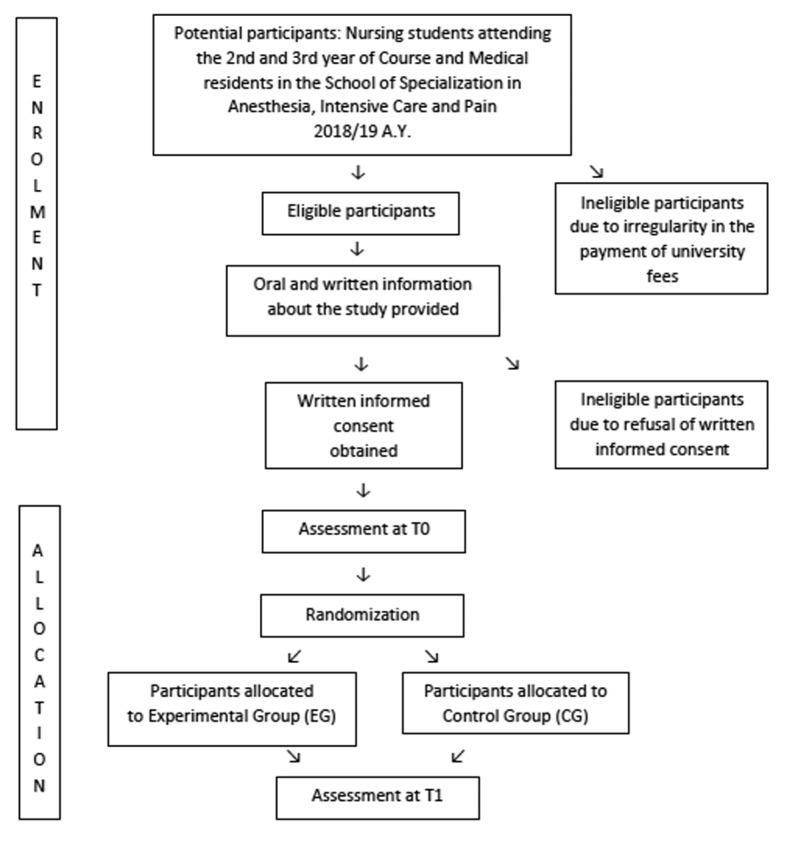
Diagram of the protocol (planned)
Randomization and allocation concealment
The randomization list, stratified by gender and study course attended, will be generated by software (R v3.5.1), in order to randomly assign the participants to the intervention group and the control group, in a ratio of 1:1. Randomization will be performed by an external statistician, not involved in training or data collection. Student recruitment will be completed before randomization. The allocation will be sealed on an envelope and held by a study assistant who is blinded to the subsequent allotment.
Intervention
The EG will participate in an experimental intervention based on high-fidelity simulation at the Advanced Training and Medical Simulation Center, realized by Faculty facilitators who are experts in this methodology. The members of the EG will be 6 nursing students and 2 residents. Before the simulation, the topic of interprofessional collaboration will be introduced and, afterwards, this group will be divided into two further subgroups, the first consisting of second year nursing students and residents attending the first three years of specialization, the second one consisting of third year nursing students and residents attending the last two years of specialization. All EG participants will receive an interprofessional training session in the laboratory using high-fidelity simulation, which provides two different scenarios, one after the other, in which the two sub groups will be involved. The first scenario, addressed to the first sub group will simulate the conditions of a patient admitted to a surgery unit who, after a surgical operation, presents a modification in his mental state, showing symptoms of acute cognitive deterioration. General clinical conditions, vital parameters and laboratory tests will suggest the evolution of a septic state. Nursing students should be able to recognize changes in mental status of the patient and in his vital signs and alert the medical doctor and, on his indication, take a blood sample. In the same simulation, the residents must be able to formulate a first diagnostic suspicion. After having formulated the diagnosis, the residents will prescribe a therapy and transfer the patient to the Intensive Care Unit (ICU). Following this first scenario, a Faculty facilitator will implement a debriefing session in both subgroups in order to deal with the issues highlighted by this first simulation. The second subgroup, after having observed the first simulation described above through a video link, will participates in the debriefing session and, afterwards, accept the patient in ICU and provide him with intensive monitoring and supportive therapies for vital functions, after having considered the necessity of mechanical ventilator support. Nursing students and residents will take into consideration the aforementioned procedures and treatments in accordance with their professional competency. The handover between the two subgroups will have to take place in a standardized way, including a “patient” evaluation through the Confusion Assessment Method in ICU (CAM-ICU) and a passage of information through the Situation, Background, Assessment and Recommendation (SBAR) instrument.
At the end of the second simulation, a new debriefing session will be conducted by the same Faculty facilitator of the first session with all the participants in the two scenarios of simulation.
Control
The CG will receive a standard training intervention, consisting in a traditional classroom using lectures and powerpoint presentation lesson on the topic of interprofessional collaboration.
Questionnaires
To measure the attitude in interprofessional collaboration, the following scales will be administered to the participants of both groups before and after the training:
1. Jefferson Scale of Attitudes toward Physician-Nurse Collaboration (JSAPNC) (78, 82), a self-report questionnaire already validated in a sample of Italian medical doctors and nurses with a Cronbach alpha of 0.70 (83). The most recent version of JSAPNC consists of 15 items with answers concerning participants’ degree of agreement/disagreement on a 4-point Likert scale (from 1 = strongly disagree to 4 = strongly agree). The score ranges from a minimum of 15 to a maximum of 60 points; the higher the score, the greater the attitude of collaboration. Items in each of the four factors are as follow:
a) Shared education and collaboration (1, 3, 6, 9, 12, 14, 15);
b) Caring versus curing (2, 4, 7);
c) Nurse’s autonomy (5, 11, 13);
d) Physician’s authority (8, 10).
2. Readiness for Interprofessional Learning Scale (RIPLS) (84), validated and adapted to the Italian educational context by Sollami and Colleagues, with a Cronbach alpha of 0.92 (85). This questionnaire has been widely used in literature to measure the readiness and attitudes of students in health professions towards the IPE. This scale consists of 10 items with a Likert 5-point scale (from 1 = strongly disagree to 5 = strongly agree).
3. A short anonymous questionnaire to investigate few socio-demographic variables (age, gender, high school diploma, year of university course).
At the end of interprofessional simulation, the Educational Practices Questionnaire (EPQ) will be administered only to the participants in the EG in order to evaluate perceptions of educational best practices’ presence and importance in simulation (86). The Italian version of this scale presented a Cronbach alpha of 0.95 (56). It consists of 16 items to which the participants respond through a Likert 5-point scale (from 1 = strongly disagree to 5 = strongly agree). The questionnaire is divided into the following sub-scales: “Active learning” (10 items) measuring opportunities for active learning and participation in simulation; “Collaboration” (2 items) measuring opportunities for working together during simulation; “Learning diversity” (2 items) measuring opportunities for learning material in simulation and “High Expectation” (2 items) measuring objectives and expectations presented during simulation (86). Higher scores represent greater recognition of best educational practice in simulation.
Data collection procedure
To guarantee anonymity in completing the questionnaires and to allow a comparative analysis of the data, the students will be invited to put on the questionnaires a code known only to themselves. All participants will be asked to anonymously complete the investigative questionnaires, before and after the simulation. Anonymity regarding the pre- and post-test will be guaranteed by assigning a code. The operator who inserts the data of the questionnaires in the file for analysis will not be aware of the groups to which the nursing student and resident physician belongs.
Expected outcomes
The expected primary outcome is that, at the end of the study, nursing students and residents who participated in the interprofessional simulation show significantly higher levels of interprofessional collaboration compared to the CG, evaluated through the JSAPNC.
The secondary outcomes are represented by an improved readiness for interprofessional education, evaluated by RIPLS, in the EG compared to the CG and, only for EG, the effectiveness of simulation training, evaluated by EPQ.
Sample size and statistical study power
In accordance with the data collected in a pilot study focused on pre-post intervention, without a control group, performed in the same training context (Nursing students and resident physicians of the University of Modena and Reggio Emilia in the 2016-2017 A.Y.), with an identical primary outcome (77), we expected to detect a difference of 2 points in the mean JSAPNC scale scores between the EG and CG. Assuming a minimum difference between the EG and CG of 2 points in the mean JSAPNC scale scores, on the average total value of the JSAPNC scale, and a variance of 35, with an alpha error of 0.05 and a power of at least 0.80, the minimum sample to be enrolled in the present study is 153 students per group.
Data collection, management and analysis
The analysis of JSAPNC and RIPLS score variation will be conducted within the EG and CG at T0 and T1; from this comparison, it is expected that the difference between EG and CG at T0 is not present or is not statistically significant, while at T1 it is statistically significant. Descriptive statistics such as frequency, mean and standard deviations will be used to summarize the socio-demographic characteristics of the participants and the JSAPNC, RIPLS and EPQ scores. Statistical comparisons between T0 and T1 of both JSAPNC and RIPLS mean scores will be applied using the Student’s t-test or the ANOVA, when appropriate. The comparison of categorical variables between groups will be performed through the chi-square test or Fisher test, when appropriate. Results will be calculated by software R v3.5.1 (7). A p<0.05 value is defined statistically significant. All randomised participants will be included in the intention to treat analysis.
Ethical considerations
This study has been approved by the Ethics Committee of Area Vasta Emilia Nord (Italy) (n° 479/2018) and will be conducted in agreement with the Helsinki declaration. Informed consent will be obtained before the students’ and residents’ participation in the study. All eligible participants will be informed of the purpose and characteristics of the study and of the proposed teaching interventions and will receive a clear informative written document, explaining the design, aims and procedure of the study. The investigator will present the study to the students and answer any questions. Each student will be given the opportunity to discuss the study with other people and will have at least one day to reflect before giving informed consent. The students and residents who sign the consent will be informed that participation in the study is voluntary and that they can withdraw their consent to participate at any time they wish and this will not affect training. The data collected will be reserved and used in compliance with the current legislation on the protection of sensitive data and privacy regulations. The investigator is the data processor, pursuant to EU Regulation 2016/679. The investigator will guarantee, at every stage of the study, monitoring, verification, review by the Ethics Committee and regulatory authorities, providing direct access to both the data and the original documents.
Strengths and limitations of this study
- This study addresses an important gap regarding utilizing of robust methods of research and reliable assessment methods.
- Randomised controlled trial design minimizes risk of selection bias.
- The power of the study was calculated in order to reach a potential statistical significance.
- Single-center study design may limit the generalizability of the study.
- Owing to the type of intervention, blinding of the nursing students and residents physicians is not possible.
References
- 1.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;13(1):i85–i90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baker DP, Gustafson S, Beaubien J, Salas E, Barach P. Medical teamwork and patient safety: The evidence-based relation. AHRQ Publication No. 05–0053. Rockville: Agency for Healthcare Research and Quality. 2005 [Google Scholar]
- 3.Buckley S, Hensman M, Thomas S, Dudley R, Nevin G, Coleman J. Developing interprofessional simulation in the undergraduate setting: experience with five different professional groups. J Interprof Care. 2012;26:362–9. doi: 10.3109/13561820.2012.685993. [DOI] [PubMed] [Google Scholar]
- 4.Joyal KM, Katz C, Harder N, Dean H. Interprofessional education using simulation of an overnight inpatient ward shift. J Interprof Care. 2015;29:268–70. doi: 10.3109/13561820.2014.944259. [DOI] [PubMed] [Google Scholar]
- 5.Turrentine FE, Rose KM, Hanks JB, Lorntz B, Owen JA, Brashers VL, et al. Interprofessional training enhances collaboration between nursing and medical students: A pilot study. Nurse Educ Today. 2016;40:33–8. doi: 10.1016/j.nedt.2016.01.024. [DOI] [PubMed] [Google Scholar]
- 6.Kohn LT, Corrigan JM, Donaldson MS. Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Washington (DC): National Academies Press; 2000. [PubMed] [Google Scholar]
- 7.Ternov S, Akselsson R. System weaknesses as contributing causes of accidents in health care. Int J Qual Health Care. 2005;17:5–13. doi: 10.1093/intqhc/mzi006. [DOI] [PubMed] [Google Scholar]
- 8.Mann S, Marcus R, Sachs B. Lessons from the cockpit: how team training can reduce errors on L&D. Contemporary OB/GYN. 2006;51:34–45. [Google Scholar]
- 9.Davenport DL, Henderson WG, Mosca CL, Khuri SF, Mentzer RM Jr. Risk-adjusted morbidity in teaching hospitals correlates with reported levels of communication and collaboration on surgical teams but not with scale measures of teamwork climate, safety climate, or working conditions. J Am Coll Surg. 2007;205:778–84. doi: 10.1016/j.jamcollsurg.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 10.Reader TW, Flin R, Cuthbertson BH. Communication skills and error in the intensive care unit. Curr Opin Crit Care. 2007;13:732–6. doi: 10.1097/MCC.0b013e3282f1bb0e. [DOI] [PubMed] [Google Scholar]
- 11.Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat AH, Dellinger EP, et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist-based surgical safety intervention. BMJ Qual Saf. 2011;20:102–7. doi: 10.1136/bmjqs.2009.040022. [DOI] [PubMed] [Google Scholar]
- 12.Poley MJ, van der Starre C, van den Bos A, van Dijk M, Tibboel D. Patient safety culture in a Dutch pediatric surgical intensive care unit: an evaluation using the Safety Attitudes Questionnaire. Pediatr Crit Care Med. 2011;12:e310–6. doi: 10.1097/PCC.0b013e318220afca. [DOI] [PubMed] [Google Scholar]
- 13.Zhang C, Miller C, Volkman K, Meza J, Jones K. Evaluation of the team performance observation tool with targeted behavioral markers in simulation-based interprofessional education. J Interprof Care. 2015;29:202–8. doi: 10.3109/13561820.2014.982789. [DOI] [PubMed] [Google Scholar]
- 14.Baggs JG, Ryan SA, Phelps CE, Richeson JF, Johnson JE. The association between interdisciplinary collaboration and patient outcomes in a medical intensive care unit. Heart Lung. 1992;21:18–24. [PubMed] [Google Scholar]
- 15.Baggs JG, Schmitt MH, Mushlin AI, Mitchell PH, Eldredge DH, Oakes D, et al. Association between nurse-physician collaboration and patient outcomes in three intensive care units. Crit Care Med. 1999;27:1991–8. doi: 10.1097/00003246-199909000-00045. [DOI] [PubMed] [Google Scholar]
- 16.Wheelan SA, Burchill CN, Tilin F. The link between teamwork and patients’ outcomes in intensive care units. Am J Crit Care. 2003;12:527–34. [PubMed] [Google Scholar]
- 17.Boev C, Xia Y. Nurse-physician collaboration and hospital-acquired infections in critical care. Crit Care Nurse. 2015;35:66–72. doi: 10.4037/ccn2015809. [DOI] [PubMed] [Google Scholar]
- 18.San Martin-Rodriguez L, D’Amour D, Leduc N. Outcomes of interprofessional collaboration for hospitalized cancer patients. Cancer Nurs. 2008;31:e18–27. doi: 10.1097/01.NCC.0000305701.99411.ac. [DOI] [PubMed] [Google Scholar]
- 19.O’Leary KJ, Sehgal NL, Terrell G, Williams MV. Interdisciplinary teamwork in hospitals: a review and practical recommendations for improvement. J Hosp Med. 2012;7:48–54. doi: 10.1002/jhm.970. [DOI] [PubMed] [Google Scholar]
- 20.Havyer RD, Wingo MT, Comfere NI, Nelson DR, Halvorsen AJ, McDonald FS, et al. Teamwork assessment in internal medicine: a systematic review of validity evidence and outcomes. J Gen Intern Med. 2014;29:894–910. doi: 10.1007/s11606-013-2686-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galletta M, Portoghese I, Carta MG, D’Aloja E, Campagna M. The Effect of Nurse-Physician Collaboration on Job Satisfaction, Team Commitment, and Turnover Intention in Nurses. Res Nurs Health. 2016;39:375–85. doi: 10.1002/nur.21733. [DOI] [PubMed] [Google Scholar]
- 22.Disch J, Beilman G, Ingbar D. Medical directors as partners in creating healthy work environments. AACN Clin Issues. 2001;12:366–77. doi: 10.1097/00044067-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 23.D’Amour D, Oandasan I. Interprofessionality as the field of interprofessional practice and interprofessional education: an emerging concept. J Interprof Care. 2005;19(1):8–20. doi: 10.1080/13561820500081604. [DOI] [PubMed] [Google Scholar]
- 24.Bleakley A, Boyden J, Hobbs A, Walsh L, Allard J. Improving teamwork climate in operating theatres: the shift from multiprofessionalism to interprofessionalism. J Interprof Care. 2006;20:461–70. doi: 10.1080/13561820600921915. [DOI] [PubMed] [Google Scholar]
- 25.Weiss SJ, Davis HP. Validity and reliability of the Collaborative Practice Scales. Nurs Res. 1985;34:299–305. [PubMed] [Google Scholar]
- 26.Taylor JS. Collaborative practice within the intensive care unit: a deconstruction. Intensive Crit Care Nurs. 1996;12:64–70. doi: 10.1016/s0964-3397(96)80962-1. [DOI] [PubMed] [Google Scholar]
- 27.Wagner J, Liston B, Miller J. Developing interprofessional communication skills. Teaching and Learning in Nursing. 2011;6:97–101. [Google Scholar]
- 28.Caricati L, Mancini T, Sollami A, Guidi C, Prandi C, Bianconcini M, et al. Nurse-Physician Collaboration Scale: A contribution to the Italian validation. TPM - Testing, Psychometrics, Methodology in Applied Psychology. 2013;20:263–76. [Google Scholar]
- 29.Lavin MA, Ruebling I, Banks R, Block L, Counte M, Furman G, et al. Interdisciplinary health professional education: a historical review. Adv Health Sci Educ Theory Pract. 2001;6:25–47. doi: 10.1023/a:1009875017951. [DOI] [PubMed] [Google Scholar]
- 30.Leggat SG. Effective healthcare teams require effective team members: defining teamwork competencies. BMC Health Serv Res. 2007;7:17. doi: 10.1186/1472-6963-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greiner AC, Knebel E. Institute of Medicine (US) Committee on the Health Professions Education Summit. Health Professions Education: A Bridge to Quality. Washington (DC): National Academies Press (US); 2003; 2003. https://www.ncbi.nlm.nih.gov/books/NBK221528/ (accessed 12 July 2018). [PubMed] [Google Scholar]
- 32. World Health Organization. Framework for action on interprofessional education and collaborative practice. 2010. http://www.who.int/hrh/resources/framework_action/en/ (accessed 12 July 2018). [Google Scholar]
- 33. The Joint Commission. Improving patient and worker safety: opportunities for synergy, collaboration and innovation. 2012. https://www.jointcommission.org/improving_patient_worker_safety/ (accessed 12 July 2018). [Google Scholar]
- 34. Agency for Healthcare Research and Quality. Patient Safety Primer. Teamwork Training. 2017. https://psnet.ahrq/gov/primers/primer/8/teamwork-training. (accessed 12 July 2018). [Google Scholar]
- 35.Reese CE, Jeffries PR, Engum SA. Learning together: Using simulations to develop nursing and medical student collaboration. Nurs Educ Perspect. 2010;31:33–7. [PubMed] [Google Scholar]
- 36.Barr H, Low H. Principles of Interprofessional Education. 2011. https://www.caipe.org/download/barr-low-2011-principles-interprofessional-education. (accessed 12 July 2018). [Google Scholar]
- 37.Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: effects on professional practice and healthcare outcomes (update) Cochrane Database Syst Rev. 2013;28:CD002213. doi: 10.1002/14651858.CD002213.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Casanova J, Day K, Dorpat D, Hendricks B, Theis L, Wiesman S. Nurse-physician work relations and role expectations. J Nurs Adm. 2007;37(2):68–70. doi: 10.1097/00005110-200702000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Coster S, Norman I, Murrells T, Kitchen S, Meerabeau E, Sooboodoo E, et al. Interprofessional attitudes amongst undergraduate students in the health professions: a longitudinal questionnaire survey. Int J Nurs Stud. 2008;45:1667–81. doi: 10.1016/j.ijnurstu.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 40.Ateah CA, Snow W, Wener P, MacDonald L, Metge C, Davis P, et al. Stereotyping as a barrier to collaboration: Does interprofessional education make a difference? Nurse Educ Today. 2011;31:208–13. doi: 10.1016/j.nedt.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 41.Hood K, Cant R, Baulch J, Gilbee A, Leech M, Anderson A, et al. Prior experience of interprofessional learning enhances undergraduate nursing and healthcare students’ professional identity and attitudes to teamwork. Nurse Educ Pract. 2014;14:117–22. doi: 10.1016/j.nepr.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 42.Kowitlawakul Y, Ignacio J, Lahiri M, Khoo SM, Zhou W, Soon D. Exploring new healthcare professionals’ roles through interprofessional education. J Interprof Care. 2014;28:267–9. doi: 10.3109/13561820.2013.872089. [DOI] [PubMed] [Google Scholar]
- 43.Sollami A, Caricati L, Sarli L. Nurse-physician collaboration: a meta-analytical investigation of survey scores. J Interprof Care. 2015;29:223–9. doi: 10.3109/13561820.2014.955912. [DOI] [PubMed] [Google Scholar]
- 44.Keshtkaran Z, Sharif F, Rambod M. Students’ readiness for and perception of inter-professional learning: a cross-sectional study. Nurse Educ Today. 2014;34:991–8. doi: 10.1016/j.nedt.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 45.Solomon P. Student perspectives on patient educators as facilitators of interprofessional education. Med Teach. 2011;33:851–3. doi: 10.3109/0142159X.2010.530703. [DOI] [PubMed] [Google Scholar]
- 46.Ivanitskaya L, Clark D, Montgomery G, Primeau R. Interdisciplinary Learning: Process and Outcomes. Innovative Higher Education. 2002;27:95–111. [Google Scholar]
- 47.Bradley P. The history of simulation in medical education and possible future directions. Med Educ. 2006;40:254–62. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 48.Jeffries PR. A framework for designing, implementing, and evaluating simulations used as teaching strategies in nursing. Nurs Educ Perspect. 2005;26:96–103. [PubMed] [Google Scholar]
- 49.Morgan R. Using clinical skills laboratories to promote theory-practice integration during first practice placement: an Irish perspective. J Clin Nurs. 2006;15:155–61. doi: 10.1111/j.1365-2702.2006.01237.x. [DOI] [PubMed] [Google Scholar]
- 50.Ward-Smith P. The effect of simulation learning as a quality initiative. Urol Nurs. 2008;28:471–3. [PubMed] [Google Scholar]
- 51.Arthur C, Levett-Jones T, Kable A. Quality indicators for the design and implementation of simulation experiences: a Delphi study. Nurse Educ Today. 2013;33:1357–61. doi: 10.1016/j.nedt.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 52.Ewertsson M, Allvin R, Holmström IK, Blomberg K. Walking the bridge: Nursing students’ learning in clinical skill laboratories. Nurse Educ Pract. 2015;15:277–83. doi: 10.1016/j.nepr.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 53.Haraldseid C, Friberg F, Aase K. Nursing students’ perceptions of factors influencing their learning environment in a clinical skills laboratory: A qualitative study. Nurse Educ Today. 2015;35:e1–6. doi: 10.1016/j.nedt.2015.03.015. [DOI] [PubMed] [Google Scholar]
- 54.Magnani D, Di Lorenzo R, Bari A, Pozzi S, Del Giovane C, Ferri P. The undergraduate nursing student evaluation of clinical learning environment: an Italian survey. Prof Inferm. 2014;67:55–61. doi: 10.7429/pi.2014.671055. [DOI] [PubMed] [Google Scholar]
- 55.Cremonini V, Ferri P, Artioli G, Sarli L, Piccioni E, Rubbi I. Nursing students’ experiences of and satisfaction with the clinical learning environment: the role of educational models in the simulation laboratory and in clinical practice. Acta Biomed. 2015;86(S3):194–204. [PubMed] [Google Scholar]
- 56.Rubbi I, Ferri P, Andreina G, Cremonini V. Learning in clinical simulation: observational study on satisfaction perceived by students of nursing. Prof Inferm. 2016;69:84–94. doi: 10.7429/pi.2016.692084. [DOI] [PubMed] [Google Scholar]
- 57.McCaughey CS, Traynor MK. The role of simulation in nurse education. Nurse Educ Today. 2010;30:827–32. doi: 10.1016/j.nedt.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 58.Salminen L, Stolt M, Saarikoski M, Suikkala A, Vaartio H, Leino-Kilpi H. Future challenges for nursing education--a European perspective. Nurse Educ Today. 2010;30:233–8. doi: 10.1016/j.nedt.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 59.Meyer T, Xu Y. Academic and clinical dissonance in nursing education: are we guilty of failure to rescue? Nurse Educ. 2005;30:76–9. doi: 10.1097/00006223-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Norman L, Buerhaus PI, Donelan K, McCloskey B, Dittus R. Nursing students assess nursing education. J Prof Nurs. 2005;21:150–8. doi: 10.1016/j.profnurs.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 61.Benner P, Sutphen M, Leonard V, Day L. Educating Nurses: A Call for Radical Transformation. San Francisco: Jossy-Bass. 2010 [Google Scholar]
- 62.Bland AJ, Topping A, Wood B. A concept analysis of simulation as a learning strategy in the education of undergraduate nursing students. Nurse Educ Today. 2011;31:664–70. doi: 10.1016/j.nedt.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 63.Flood LS, Robinia K. Bridging the gap: strategies to integrate classroom and clinical learning. Nurse Educ Pract. 2014;14:329–32. doi: 10.1016/j.nepr.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 64.Lasater K. High-fidelity simulation and the development of clinical judgment: students’ experiences. J Nurs Educ. 2007;46:269–76. doi: 10.3928/01484834-20070601-06. [DOI] [PubMed] [Google Scholar]
- 65.Mikkelsen J, Reime MH, Harris AK. Nursing students’ learning of managing cross-infections--scenario-based simulation training versus study groups. Nurse Educ Today. 2008;28:664–71. doi: 10.1016/j.nedt.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 66.Cant RP, Cooper SJ. Use of simulation-based learning in undergraduate nurse education: An umbrella systematic review. Nurse Educ Today. 2017;49:63–71. doi: 10.1016/j.nedt.2016.11.015. [DOI] [PubMed] [Google Scholar]
- 67.Szpak JL, Kameg KM. Simulation decreases nursing student anxiety prior to communication with mentally ill patients. Clinical Simulation in Nursing. 2013;9:e13–e19. [Google Scholar]
- 68.Khalaila R. Simulation in nursing education: an evaluation of students’ outcomes at their first clinical practice combined with simulations. Nurse Educ Today. 2014;34:252–8. doi: 10.1016/j.nedt.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 69.Shin S, Park JH, Kim JH. Effectiveness of patient simulation in nursing education: meta-analysis. Nurse Educ Today. 2015;35:176–82. doi: 10.1016/j.nedt.2014.09.009. [DOI] [PubMed] [Google Scholar]
- 70.Bray B, Schwartz CR, Weeks DL, Kardong-Edgren S. Human patient simulation technology: perceptions from a multidisciplinary sample of health care educators. Clinical Simulation in Nursing. 2009;5:e145–e150. [Google Scholar]
- 71.Liaw SY, Siau C, Zhou WT, Lau TC. Interprofessional simulation-based education program: a promising approach for changing stereotypes and improving attitudes toward nurse-physician collaboration. Appl Nurs Res. 2014;27:258–60. doi: 10.1016/j.apnr.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 72.Zhang C, Thompson S, Miller C. A Review of Simulation-Based Interprofessional Education. Clinical simulation in nursing. 2011;7:e117–e126. [Google Scholar]
- 73.Weller JM, Nestel D, Marshall SD, Brooks PM, Conn JJ. Simulation in clinical teaching and learning. Med J Aust. 2012;196:594. doi: 10.5694/mja10.11474. [DOI] [PubMed] [Google Scholar]
- 74.Granheim BM, Shawb JM, Mansah M. The use of interprofessional learning and simulation in undergraduate nursing programs to address interprofessional communication and collaboration: An integrative review of the literature. Nurse Educ Today. 2018;62:118–27. doi: 10.1016/j.nedt.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 75.Rutherford-Hemming T, Lioce L. State of Interprofessional Education in Nursing. A Systematic Review. Nurse Educator. 2018;43:9–13. doi: 10.1097/NNE.0000000000000405. [DOI] [PubMed] [Google Scholar]
- 76.Labrague LJ, McEnroe-Petitte DM, Fronda DC, Obeidat AA. Interprofessional simulation in undergraduate nursing program: An integrative review. Nurse Educ Today. 2018;67:46–55. doi: 10.1016/j.nedt.2018.05.001. [DOI] [PubMed] [Google Scholar]
- 77.Ferri P, Rubbi I, Magnani D, Ricchi A, Iughetti L, Molinazzi T, et al. Bologna, Italy: 22-23 September 2017. Effects of an inter-professional training intervention, with high-fidelity simulation, on the attitude to the collaboration of nursing and obstetrics students and doctors in training in pediatrics: quasi-experimental study. Poster presented at the Permanent Conference of the graduate classes of the Health Professions. [Google Scholar]
- 78.Hojat M, Fields SK, Veloski JJ, Griffiths M, Cohen MJ, Plumb JD. Psychometric properties of an attitude scale measuring physician-nurse collaboration. Eval Health Prof. 1999;22:208–20. doi: 10.1177/01632789922034275. [DOI] [PubMed] [Google Scholar]
- 79.Brandt B, Lutfiyya ML, King JA, Chioreso C. A scoping review of interprofessional collaborative practice and education using the lens of the Triple Aim. J Interprof Care. 2014;28:393–9. doi: 10.3109/13561820.2014.906391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586. doi: 10.1136/bmj.e7586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:e869. doi: 10.1136/bmj.c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hojat M, Ward J, Spandorfer J, Arenson C, Van Winkle LJ, Williams B. The Jefferson Scale of Attitudes Toward Interprofessional Collaboration (Jeff SATIC): development and multi-institution psychometric data. J Interprof Care. 2015;29:238–44. doi: 10.3109/13561820.2014.962129. [DOI] [PubMed] [Google Scholar]
- 83.Hojat M, Gonnella JS, Nasca TJ, Fields SK, Cicchetti A, Lo Scalzo A, et al. Comparisons of American, Israeli, Italian and Mexican physicians and nurses on the total and factor scores of the Jefferson scale of attitudes toward physician-nurse collaborative relationships. Int J Nurs Stud. 2003;40:427–35. doi: 10.1016/s0020-7489(02)00108-6. [DOI] [PubMed] [Google Scholar]
- 84.Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS) Med Educ. 1999;33:95–100. doi: 10.1046/j.1365-2923.1999.00298.x. [DOI] [PubMed] [Google Scholar]
- 85.Sollami A, Caricati L, Mancini T. Attitudes towards Interprofessional Education among Medical and Nursing Students: the Role of Professional Identification. Curr Psycho. 2017:1–8. [Google Scholar]
- 86.Franklin AE, Burns P, Lee CS. Psychometric testing on the NLN Student Satisfaction and Self-Confidence in Learning, Simulation Design Scale, and Educational Practices Questionnaire using a sample of pre-licensure novice nurses. Nurse Educ Today. 2014;34:1298–304. doi: 10.1016/j.nedt.2014.06.011. https://www.rdocumentation.org/packages/base/versions/3.5.1. (accessed 12 January 2018) [DOI] [PubMed] [Google Scholar]


