Abstract
Abdominal aortic aneurysm (AAA) in association with external iliac artery (EIA) occlusion is a rare entity which may limit endovascular aortic aneurysm repair (EVAR) feasibility. We describe the case of an 84-year-old man affected by a 64mm infrarenal inflammatory abdominal aortic aneurysm with complete bilateral occlusion of EIA and patency of both common and internal iliac arteries. The common femoral arteries (CFA) were patent, and the patient was asymptomatic for lower limb claudication. The treatment was performed by EVAR using a bifurcated stent-graft after the recanalization of the left EIA, achieving technical success. (www.actabiomedica.it)
Keywords: aortic aneurysm, abdominal [MeSH], endovascular procedures [MeSH], iliac occlusion
Introduction
Concurrent external iliac artery (EIA) occlusion and abdominal aortic aneurysm (AAA) is rare and limits usage of endovascular aortic aneurysm repair (EVAR) (1). Traditionally open abdominal surgery is the first approach in these patients. Compared with open surgery, EVAR has been found to have lower rates of early mortality and morbidity (2). However, endovascular treatment strategy differs with severity of iliofemoral occlusive disease.
We present a case report illustrating an infrarenal AAA with bilateral EIA occlusion treated through EVAR using a bifurcated stent-graft after recanalization of the left EIA.
Case Report
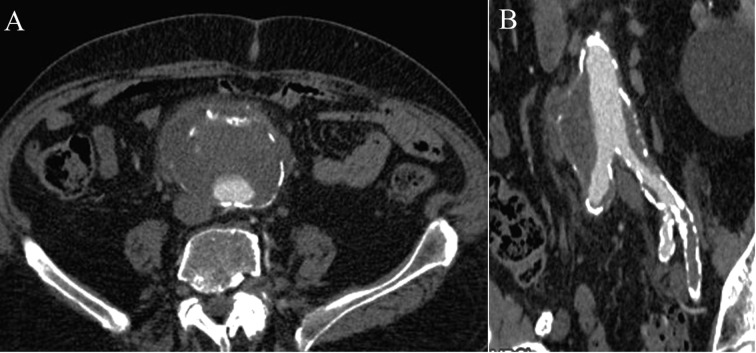
An 84-year-old man, affected by chronic obstructive pulmonary disease, hypertension and an infrarenal AAA (diagnosed two years earlier), was admitted for fever of unknown origin. A computed tomography angiography (CTA) showed that the diameter of AAA has enlarged since its initial detection and was now approaching 64 mm with signs of perianeurismal inflammation (figure 1a). Moreover, this CTA revealed the patency of both common (CIA) and internal iliac arteries (IIA), and a complete bilateral occlusion of the EIA (figure 1b). The common femoral arteries (CFA) were patent, and the patient was asymptomatic for lower limb claudication.
Figure 1.
Preoperative computed tomography angiography (CTA). A: Infrarenal inflammatory aneurysm. B: Multiplanar reconstruction showing the patency of both common iliac and hypogastric artery and the occlusion of external iliac artery
The need for urgent intervention for his 64mm AAA was discussed with the patient. Informed consent was obtained.
Considering the high risk of complications of major open abdominal surgery due to his multiple comorbidities (ASA score 4), we agreed to attempt EVAR after recanalization of the chronic occlusion of the left EIA. We planned to perform EVAR using a bifurcated stent graft in order to preserve the patency of both IIA.
The procedure was performed in the operating room with the patient under general anesthesia. Both CFA and the left axillary artery were surgically exposed.
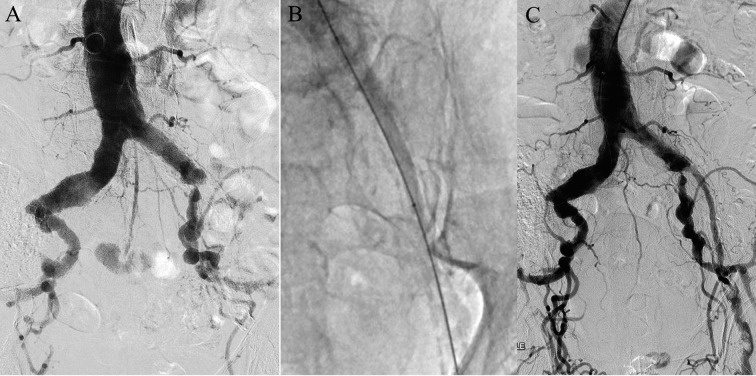
Then, the left axillary artery was then punctured for insertion of a 12Fr sheath introducer, 90cm in length (Flexor KCFW, Cook medical Inc.) and abdominal aortography was obtained (figure 2a).
Figure 2.
Recanalization of left external iliac artery. A: Diagnostic angiography. B: Predilation of the left external iliac artery with 4x120mm;7x40mm balloon C: Completion angiography
Anterograde recanalization of the left EIA through the left axillary access was attempted by using a 0.035 inch angled glidewire (Terumo Medical) supported by a 4Fr Vertebral Glidecath catheter (Terumo Medical). This guidewire crossed easily the occlusion of the left CFA. Multiple predilatations of the EIA were performed with balloon catheters Powerflex 4x120 mm-7x40 mm (Cordis) (figure 2b) getting the recovery of the left femoral pulse (figure 2c).
The same procedure was attempted without success for the recanalization of the contralateral EIA.
A 9Fr sheath introducer was placed into the left CFA from the groin.
Numerous dilations of the left external iliac artery using 16Fr then 18Fr dilators (Cook Medical Inc) (figure 3) were performed with success. The main body of a Zenith Alpha (Cook Medical, Inc) abdominal endovascular bifurcated stent-graft (ZIMB-26-84) was introduced through the left CFA and deployed below the renal arteries. Then we implanted the ipsilateral limb extender (ZISL-16-42) just proximal to the left IIA origin ensuring continued patency.
Figure 3.
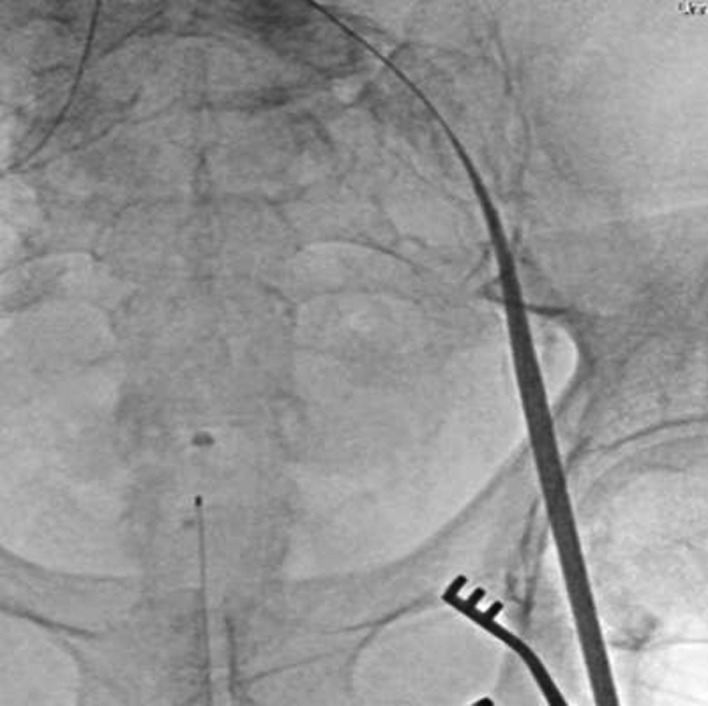
Dilation the left external iliac artery using 16Fr sheath introducer dilators (Cook Medical Inc)
Through the left axillary access, the contralateral gate of the bifurcated aortic stent-graft was engaged and a stiff guidewire was placed in the right IIA. Two Viabahn stent grafts 13x100 mm-13x50 mm (W.L. Gore, Flagstaff, AZ, USA) were advanced and released as a bridging stent-graft from the right gate of the aortic main body to the origin of right IIA to both achieve distal sealing and maintain the patency of the right IIA.
The main body and the contralateral limb (two Viabahn stent-grafts) were dilated with a Coda balloon catheter (Cook Medical Inch). The kissing balloon was performed inside the stent-graft limbs with an 18 mm non compliant balloon Esophageal XXL (Boston SC) into the left limb and an 12 mm balloon Powerflex (Cordis) into the Viabahn (right limb).
The completion angiography was satisfactory. It showed the patency of the endograft and both hypogastric iliac arteries (figure 4) and revealed a low-flow type II endoleak from lumbar arteries.
Figure 4.

Completion angiography shows patency of the endograft and both hypogastric iliac arteries
Endarterectomy of the left CFA was required before arterial reconstruction. The patient had no intraoperative or postoperative complications.
A CTA performed 7 days after the operation, demonstrated the patency of the both CIIA, IIA and left EIA (figure 5a) and a type II EL (figure 5b). The patient was discharged on 8th postoperative day.
Figure 5.
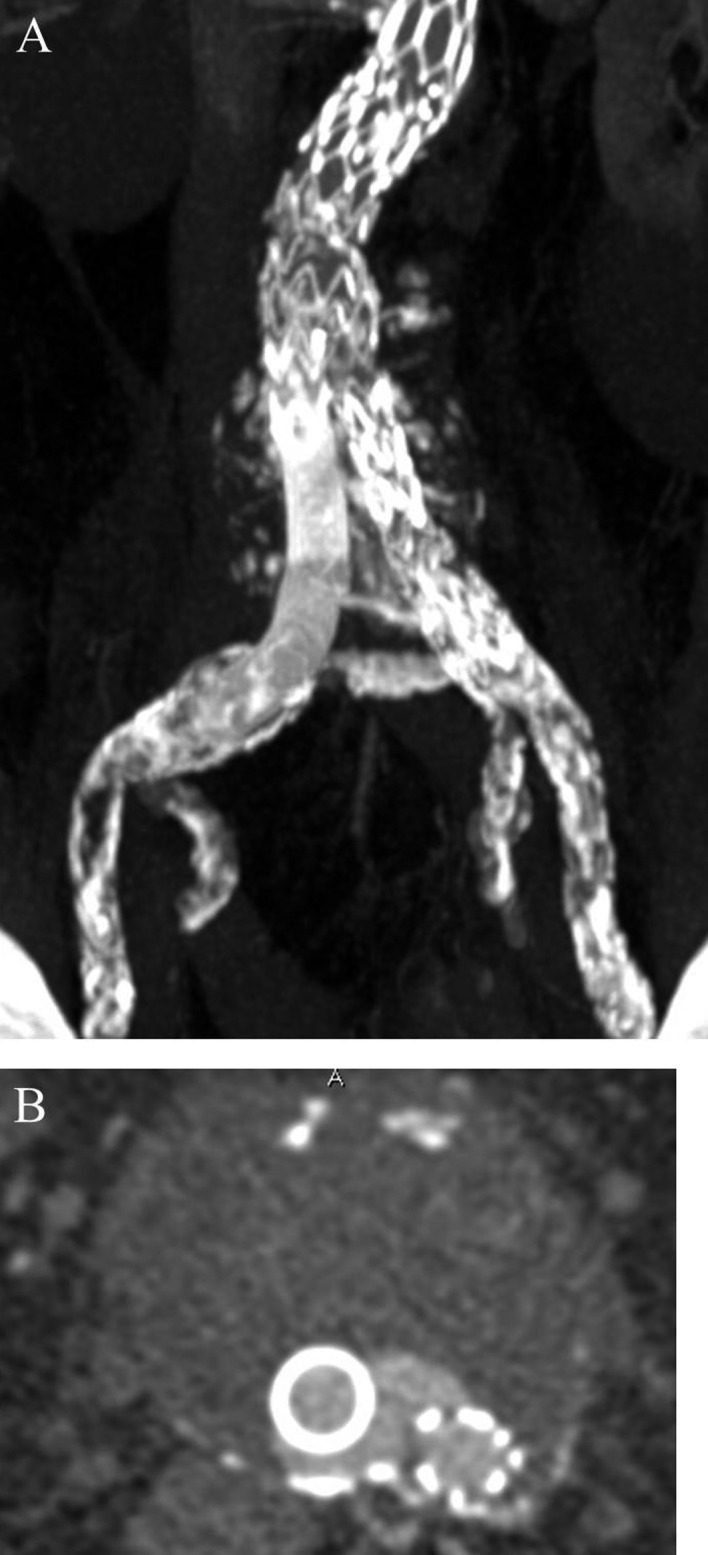
Computed tomography angiography performed 7 days after the operation. A: Maximum intensity projection reconstruction showing stent-grafts and extensive calcification of iliac axes. B: Axial image showing type II endoleak from lumbar arteries.
Discussion
Open surgical repair is the traditional therapy in patients with concurrent iliac occlusion and AAA. However, open surgical repair is associated with higher rates of perioperative morbidity and mortality compared with EVAR (2).
Given the current state of endovascular technology, challenging aortoiliac anatomy represents one of the more frequent limiting factors in EVAR applicability (3). Iliofemoral occlusive disease is a possible contraindication for EVAR, and the treatment strategy differs depending on severity of the lesion (4). Small size, severe calcified stenoses, and severe angulation of the iliac anatomy represent some of the most frequently cited reasons for non-navigability of the stent-graft delivery systems.
Multiple innovative techniques are described in the literature to modify the iliac anatomy to facilitate the advancement of the EVAR delivery system. These include simple dilation of the iliofemoral segment using over-the-wire dilators, balloon angioplasty, stenting or surgical conduit (5-7).
Although good results are reported using an aorto-uni-iliac configuration, bifurcated stent-grafts seem to have better hemodynamic results from direct flow (8) and to increase primary and secondary patency rates compared to AUI device and femoro-femoral crossover bypass. A prosthetic femoro-femoral bypass graft is also associated with possible postoperative complications (infection of the prosthesis in the groin area, steal phenomenon caused by the bypass) (8, 9). Furthermore, the presence of the anastomosis at the CFA limits possible secondary interventions, especially with percutaneous access.
Our case shows that the use of a bifurcated EVAR to treat patients with concomitant infrarenal AAA and bilateral chronic total occlusion of the EIA is feasible, effective and essential in patient asymptomatic for lower limb claudication and with patency of both IIA. On the other hand, our case showed the lack of available material necessary to achieve EVAR with bifurcated stent-graft. In this specific case Viabahn stent-graft has congruous diameter (13 mm), sheath length (120 cm) and delivery system diameter (12F) to be deployed from axillary access and to achieve a good sealing in the contralateral gate of Zenith Alpha main body (11 mm).
The thorough knowledge of endovascular techniques and devices is an essential condition to a successful treatment. With the left CFA access after recanalization of the left EIA and the axillary access, we are able to insert and deploy an aortic abdominal bifurcated stent-graft to treat infrarenal AAA with bilateral complete occlusion EIA.
Conflict of interest:
None to declare
References
- 1.Vallabhanemi R, Sorial EE, Jordan WD, et al. Iliac artery recanalization of chronic occlusions to fsacilitate endovascular aneurysm repair. J Vasc Surg. 2012;56:1549–54. doi: 10.1016/j.jvs.2012.05.089. [DOI] [PubMed] [Google Scholar]
- 2.Prinssen M, Verhoeven EL, Buth J, et al. A randomized trial comparing conventional and endovascular repair of abdominal aortic aneurysms. N Engl J Med. 2004;351:1607–18. doi: 10.1056/NEJMoa042002. [DOI] [PubMed] [Google Scholar]
- 3.Arko FR, Filis KA, Seidel SA, et al. How many patients with infrarenal aneurysms are candidates for endovascular repair? The Northern California experience. J Endovasc Ther. 2004;11:33–40. doi: 10.1177/152660280401100104. [DOI] [PubMed] [Google Scholar]
- 4.Scurr J, How T, Vallabhanemi SR, et al. EVAR in iliac occlusion. J Endovasc Ther. 2007;14:59–61. doi: 10.1583/06-1925.1. [DOI] [PubMed] [Google Scholar]
- 5.Yano OJ, Faries PL, Morrisey N, Teodorescu V, Hollier LH, Marin ML. Ancillary techniques to facilitate endovascular repair of aortic aneurysms. J Vasc Surg. 2001;34:69–75. doi: 10.1067/mva.2001.116005. Pub Med:11436077. [DOI] [PubMed] [Google Scholar]
- 6.Henretta JP, Karch LA, Hodgson KJ, et al. Special iliac artery considerations during aneurysm endografting. Am J surg. 1999;178:212–8. doi: 10.1016/s0002-9610(99)00156-7. [DOI] [PubMed] [Google Scholar]
- 7.Wu T, Carson JG, Skelly CL. Use of internal endoconduits as an adjunct to endovascular aneurysm repair in the setting of challenging aortoiliac anatomy. Ann Vasc Surg. 2010;24(114):e7–11. doi: 10.1016/j.avsg.2009.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yilmaz LP, Abraham CZ, Reilly LM, et al. Is cross-femoral bypass grafting a disadvantage of aortomonoiliac endovascular aortic an eurysm repair? J vasc surg. 2003;38:753–7. doi: 10.1016/s0741-5214(03)00721-3. [DOI] [PubMed] [Google Scholar]
- 9.Jean Baptiste E, Batt M, Azzaoui R, et al. comparison of the mid-term result following the use of bifurcated and aorto-uni-iliac devices in the treatment of AAA. EUR J Vasc Endovasc Surg. 2009;38:298–304. doi: 10.1016/j.ejvs.2009.06.004. [DOI] [PubMed] [Google Scholar]