Abstract
OBJECTIVES:
This prospective, randomized controlled trial explored the feasibility and efficacy of a group program of mindfulness training, a cognitive-behavioral technique, for women with irritable bowel syndrome (IBS). The technique involves training in intentionally attending to present-moment experience and non-judgmental awareness of body sensations and emotions.
METHODS:
Seventy-five female IBS patients were randomly assigned to eight weekly and one half-day intensive sessions of either mindfulness group (MG) training or a support group (SG). Participants completed the IBS severity scale (primary outcome), IBS-quality of life, brief symptom inventory-18, visceral sensitivity index, treatment credibility scale, and five-facet mindfulness questionnaire before and after treatment and at 3-month follow-up.
RESULTS:
Women in the MG showed greater reductions in IBS symptom severity immediately after training (26.4% vs. 6.2% reduction; P= 0.006) and at 3-month follow-up (38.2% vs. 11.8%; P= 0.001) relative to SG. Changes in quality of life, psychological distress, and visceral anxiety were not significantly different between groups immediately after treatment, but evidenced significantly greater improvements in the MG than in the SG at the 3-month follow-up. Mindfulness scores increased significantly more in the MG after treatment, confirming effective learning of mindfulness skills. Participants’ ratings of the credibility of their assigned interventions, measured after the first group session, were not different between groups.
CONCLUSIONS:
This randomized controlled trial demonstrated that mindfulness training has a substantial therapeutic effect on bowel symptom severity, improves health-related quality of life, and reduces distress. The beneficial effects persist for at least 3 months after group training.
INTRODUCTION
Irritable bowel syndrome (IBS) is a functional bowel disorder characterized by symptoms of abdominal discomfort associated with defecation disturbances (1). It is experienced by about 10% of American adults, and is more common in women (14% women and 8% men). The syndrome results in significant disability, quality of life impairment, and health-care burden (2–4). Conventional medical care for IBS has primarily focused on diet and lifestyle management, behavioral treatments, and pharmacological agents, particularly antispasmodics (5). Newer medications approved for IBS include serotonin type-3 receptor antagonists and chloride channel agonists (6). Although pharmacological therapies may temporarily relieve symptoms, they are often costly and may result in negative side effects. A substantial proportion of patients with IBS do not attain adequate relief through conventional medical approaches (5). This has led to efforts to find other methods to improve clinical outcomes for IBS patients.
Psychological interventions such as cognitive-behavioral therapy (CBT) and hypnosis have proven among the most successful treatments for IBS (7,8). The 2002 Technical Review on IBS by the American Gastroenterology Association (9) concluded that psychological treatment often helps to reduce both bowel symptoms and psychological symptoms and may be used in treating people with IBS in several situations: when the symptoms are moderate to severe; when they have proven refractory to medical treatment; or when evidence points to stress or psychological factors exacerbating the bowel symptoms. The Evidence-Based Position Statement on the Management of Irritable Bowel Syndrome, published by the American College of Gastroenterology Task Force on IBS in 2009 (10) and based on systematic reviews of empirical evidence for therapies of IBS, asserted that psychological therapies, including cognitive therapy, dynamic psychotherapy, and hypnotherapy, but not relaxation therapy, are more effective than usual care in relieving global symptoms of IBS. The task force assigned this conclusion a grade of “1B” meaning strong recommendation supported by moderate evidence.
Psychological treatments are a logical approach to management of the bowel symptoms of IBS because brain-gut interactions are recognized to have a prominent role in modulating gut function (9). The brain receives a continuous stream of signals from the body informing it about moment-to-moment gastrointestinal activity and events. It formulates an integrated response to this incoming information and sends messages to the gut to regulate the muscular, vascular, secretory, and immune functions of the gastrointestinal tract (11). The brain’s emotional motor system, which includes the amygdala, hypothalamus, and medial prefrontal cortex (12), makes adjustment to the brain’s gut regulation in response to emotions and stress, by means of autonomic nervous system signals to the gastrointestinal tract’s own enteric nervous system. The brain also adjusts its perceptual filtering of sensory nerve signals coming from the gastrointestinal tract according to the person’s cognitive and emotional state (11). In these ways, psychological factors can influence gut activity and contribute to or exacerbate bowel symptoms, and that deleterious influence is likely to be more readily addressed through psychological means rather than through pharmaceutical interventions. Psychological treatments may exert their beneficial effects on IBS symptoms by diminishing maladaptive cognitions, negative emotions, or stress that lead to gut disturbance through the brain-gut connection; or they may act more directly on the brain-gut connection by modifying the brain’s perception of gut sensations or its influence on the gut (e.g., by training IBS patients to adopt different habits in attention to gut sensations or to separate their emotions mentally from their gut symptoms). However, to date the particular mechanisms that underlie the demonstrated therapeutic effects of psychological treatments on IBS symptoms remain poorly understood.
Mindfulness meditation is a unique psychological approach that integrates the biopsychosocial relationships manifested in IBS, emphasizing as it does mind-body interactions, the role of self-regulation in human physiology, and the capacity for cognitive restructuring. The techniques of mindfulness, introduced 2500 years ago by Shakyamuni Buddha, are traditionally recognized as effective for calming the mind and generating both insight and compassion. The basic technique involves the intentional self-regulation of attention to present-moment experience, using the breath or other object as the focal point, combined with release of cognitive fixation on thoughts of past and future. Through mindfulness practice, one learns to evoke a non-evaluative state of present-moment awareness (13,14). Research has shown that programs such as mindfulness-based stress reduction that involve training and practice of mindfulness can reduce stress and pain symptoms in chronic functional disorders such as fibromyalgia and depression (15–19). As pain is a prominent symptom in IBS and stress exacerbates IBS symptoms (20), mindfulness-training programs would seem to be a reasonable treatment approach for this condition. To date, there have been no controlled clinical trials of the efficacy of such programs specifically for IBS.
Recent investigations have found that mindfulness meditation induces changes in the activation of neural circuits implicated in interoception (awareness of stimuli originating inside the body (21)) and emotion regulation (22,23), while improving attentional control (24–27). Hence, we theorized that mindfulness training may be uniquely suited to treat the psychological factors associated with IBS, including a heightened perception of pain from intestinal distention (28) that is correlated with selective attention to gastrointestinal sensations and anxiety about the significance of these sensations (29). As a primary technique of mindfulness involves attending to the breath and letting go of thoughts, feelings, and story lines that may enhance pain, evoke stress, and induce catastrophizing about negative events, we theorized that mindfulness may have a salutary effect on the experiences and symptoms of those with IBS.
The aim of this study was to determine the feasibility of developing a clinical trial comparing the efficacy of group training in mindfulness with an IBS support group (SG) in reducing IBS symptom severity. The study utilized a design that controlled for the effects of expectancy of improvement and non-specific therapeutic factors such as social interaction and social support. Our primary hypothesis was that compared with those participating in an SG, individuals receiving mindfulness training would demonstrate significantly greater reduction in IBS symptom severity, as measured by the IBS symptom severity scale—IBS-SS (30). We also hypothesized that, after training, those participating in the mindfulness-training group would show reduced psychological distress and improvements in health-related quality of life, increasing at 3 months as compared with immediately post-intervention, and that improvement in these variables, as well as reductions in IBS symptom severity, would be associated with increases in mindfulness scores.
METHODS
Design and procedure
The study design was a randomized controlled parallel-group trial. Figure 1 illustrates the overall design and subject flow. The study was approved by the UNC School of Medicine institutional review board on 5 April 2006, as well as the UNC General Clinical Research Center. The study was registered with ClinicalTrials.gov as study number NCT00680693.
Figure 1.
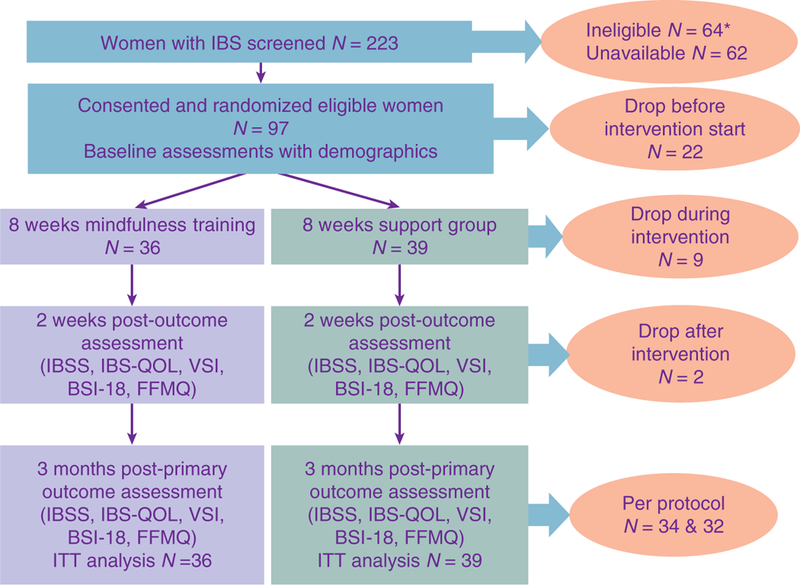
Study flow diagram for mindfulness meditation vs. support group for irritable bowel syndrome, 2006 – 2009. * Of the 64 ineligible subjects, 10 did not meet Rome II criteria for IBS, 9 had too few symptoms to participate in our study, 14 had other bowel illness or surgery in addition to IBS, 3 were pregnant or intended to become pregnant, 9 had excluded medical illness and 12 psychiatric illness, and 7 had prior experience with meditation. In addition, 62 were unavailable to participate: 32 individuals declined to participate during the screening process, largely due to distance to the study site or the time commitment and 30 were eligible and interested, but unable to schedule participation. BSI-18, brief symptom inventory-18; FFMQ, five-facet mindfulness questionnaire; IBS, irritable bowel syndrome; IBS-QOL, irritable bowel syndrome-quality of life; IBS-SS, irritable bowel syndrome severity scale; ITT, intent to treat; VSI, visceral sensitivity index.
Participants
Female patients with IBS under the care of a physician were recruited over a 3-year period from 2006 to 2009 through an existing registry of IBS patients interested in participating in research studies, as well as through physicians’ offices, local advertisements, and posted flyers. All interested participants were screened for eligibility by the project coordinator, with referral to the physician co-investigator for additional screening, if needed, to ascertain eligibility.
Inclusion/exclusion criteria
Inclusion criteria were (i) IBS diagnosis according to Rome II criteria and physician diagnosis; (ii) female; (iii) age 18–75 years; (iv) ability to understand English; (v) willingness to document bowel symptoms and medication use regularly and complete the assessments; and (vi) willingness to attend eight weekly sessions plus one additional half-day session of either mindfulness training or SG. All subjects were informed that they should continue to receive usual care from their physicians and that no specific recommendations for changes in medications for IBS would be made by the research team.
Exclusion criteria were (i) diagnosis of mental illness with psychosis; (ii) a history of inpatient admission for psychiatric disorder within the past 2 years; (iii) a history or current diagnosis of inflammatory bowel disease or gastrointestinal malignancy; (iv) active liver or pancreatic disease; (v) uncontrolled lactose intolerance; (vi) celiac disease; (vii) a history of abdominal trauma or surgery involving gastrointestinal resection; or (viii) pregnancy.
Randomization and assignment
Upon completion of written consent, baseline interview, and questionnaires, eligible study participants were randomized by a computer program to either the mindfulness group (MG) or IBS SG. Figure 1 illustrates the disposition of participants at all stages of the study. Of the 223 women assessed for eligibility, 97 were found to be eligible, and were enrolled and randomly assigned to one of the two treatment groups. Of the 64 ineligible subjects, 10 did not meet Rome II criteria for IBS, 9 had too few symptoms to participate in our study, 14 had other bowel illness or surgery in addition to IBS, 3 were pregnant or intended to become pregnant, 9 had an excluded medical illness and 12 a psychiatric illness, and 7 had prior experience with meditation. In addition, 62 were unavailable to participate: 32 individuals declined during the screening process, largely due to distance to the study site or the time commitment and 30 were eligible and interested, but unable to schedule participation. Subsequently, 75 subjects (76.5%) began treatment after randomization—36 in the MG and 39 in the SG.
Subjects attended an average of 6.7 out of the 9 intervention sessions held for each group (6.3 sessions for SG and 7.1 for MG; P = 0.09). Of the 75 individuals who started treatment, 9 subjects dropped out of the study before post-treatment data could be obtained (2 from the MG and 7 from the SG). The overall attrition rate was 12%. Study participants were remunerated for completing the assessments and for attending a minimum of six of the nine sessions.
Masking
Study staff members involved in data collection and data management were masked to treatment assignment. Due to the nature of the study interventions, subjects and therapists could not be blinded.
To minimize differences in subject expectancy, subjects were not informed about the test hypotheses regarding the predicted superior effects of mindfulness training on IBS. The experimental interventions were described to subjects only as two psychological interventions—a set of meditation procedures and a SG—both of which have been reported in previous studies to benefit patients with IBS. To verify that patients assigned to the SG had the same expectation of benefit as those in the MG, all patients completed a treatment credibility scale (31) after the first treatment session.
Intervention conditions
Subjects continued with their usual medical care throughout the study. Following completion of assessment and random assignment, subjects met for a series of sessions in small groups for their assigned intervention. The MG was taught by an experienced mindfulness instructor and the SG was led by a licensed clinical social worker or one of two of his well-trained master’s students. All group leaders followed an explicit protocol; their compliance with the protocol was monitored through videotaping. No protocol deviations were observed.
The intervention for both study arms consisted of eight weekly 2-h sessions plus one half-day retreat. Subjects were asked to keep a daily diary during the intervention, in which they recorded minutes of practice time and any IBS symptoms. Subjects could choose to record diary information either electronically on-line (submitted daily) or on paper (submitted weekly at the meetings or mailed). (Seven of the 75 individuals starting the intervention chose to complete paper diaries.)
Mindfulness intervention.
The mindfulness-based stress and pain management program, used as an intervention for the MG, was taught by trained mindfulness instructors and based on the mindfulness-based stress reduction program developed by Jon Kabat-Zinn and Saki Santorelli at the University of Massachusetts. This program has been adapted for a wide range of health conditions (32). The course used in this study was typical in length and content, with instruction and homework assignments related to the body scan (i.e., focusing attention on different parts of the body sequentially to detect sensations such as muscle tension), sitting and walking meditation, and mindful yoga. The basic course was adapted to an IBS population by emphasizing the relevance of mindfulness in coping with IBS-related symptoms and perceptions. For example, participants were instructed to notice any sensations in the abdominal area and distinguish those sensations from thoughts about the sensations. In doing so, the mindfulness-training intervention promoted sensory vs. emotional processing of interoceptive signals and counteracted catastrophizing, which is a maladaptive cognitive coping style characterized by ruminative thoughts about the significance of symptoms; catastrophizing has been shown to exacerbate irritable bowel symptoms (33,34). Details of the mindfulness as well as SG protocol have been previously reported by our group (35). Homework assigned each week throughout the course included daily mindfulness practices and readings from provided texts: “Full Catastrophe Living” for the MG (32) and “IBS for Dummies” for both the MG and SG (36).
SG intervention.
We selected a social-support group intervention led by master’s level social workers to control for expectations of benefit and amount of group contact. A previous study successfully used an SG as a control condition for CBT (37). In that study, while the SG produced an expectation of benefit comparable with the CBT group, there was less change in IBS symptoms than in the CBT group.
As in the mindfulness intervention, the SG included one half-day session during the second half of the 8-week intervention. The half-day session involved the preparation and sharing of an “IBS-friendly” meal by the group participants. Weekly sessions, facilitated by social-work group leaders, focused on specific pre-designated topics and involved open group discussions about subjects’ experiences with, or reaction to, the topic. Please see our previous report for complete details of the SG protocol (35). Weekly homework assignments included readings from the provided text, “IBS for Dummies” ( 36 ).
Measures
Administration of outcome and process measures took place upon entry into the study, at the completion of the 8-week program, and again 3 months after program completion. Collection of these data required approximately 1 h. All measures have been described in detail in a previous report (35) and are presented here only briefly.
Outcome measures.
The IBS-SS, a well-validated clinical indicator of illness severity in IBS, served as the primary outcome variable (30) with the 3-month post-intervention assessment selected a priori as the primary time point to assess efficacy. The IBS-SS has been frequently used in clinical studies. Responders rated retrospectively, for the past 10 days, abdominal pain severity and frequency (separate ratings), bloating severity, dissatisfaction with bowel habits and life interference from bowel symptoms. These five ratings were totaled to obtain an overall IBS severity score with a maximum score of 500. According to the scale developers, a 50-point or greater change on this scale is considered clinically significant ( 30 ).
Secondary outcome variables included (i) the IBS-quality of life (IBS-QOL), a 34-item disease-specific quality-of-life scale measuring changes in physical and psychosocial functioning as a result of IBS that is responsive to change over 12 weeks (38) and has been shown to have high internal consistency and high reproducibility (39); (ii) the visceral sensitivity index, a validated 15-item scale measuring anticipatory anxiety with respect to the likely occurrence of symptoms, (40) which is a strong predictor of symptom severity (40); and (iii) the brief symptom inventory-18, a validated 18-item short version of the symptom checklist-90-R (41) with separate subscale scores for anxiety, depression, and somatization, plus a global symptom severity index. (One question, on suicidality, was omitted from the version of the questionnaire used in this study. Full depression and global severity scores were estimated through pro-rating based on the mean for all other items on the same scale.)
Process measures.
The construct of mindfulness was measured by the five-facet mindfulness questionnaire, a 39-item Likert-type scale that assesses five identified facets of mindfulness: non-reactivity to inner experience; a non-judgmental attitude; acting with awareness; describing emotional experience; and observing. Individual facets correlate positively with openness to experience, emotional intelligence, and self-compassion, and negatively with alexethymia, dissociation, and psychological distress (42).
The Borkovec and Nau (43) attitude-towards-treatment questionnaire, in the version adapted for IBS (44), is a five-item scale (each question offering a response range from 0 to 9) used to assess patients’ expectations of treatment benefit and perceptions of the value of the treatment, once treatment has been explained. Subjects completed this scale after the first group session. It is standard procedure to apply the Borkovec and Nau instrument after the beginning of an intervention to allow participants a brief exposure to the study upon which to base their assessments.
Data analysis
Data were examined to ensure that they were normally distributed and met assumptions for parametric statistical tests. All outcome variables were approximately normally distributed. Bivariate correlations, t-tests, χ2 tests, and repeated-measures analyses of variance (ANOVA) as implemented in SPSS 17.0 (SPSS, Inc., Chicago, IL), were used to test hypotheses and compare group differences at baseline and over time. All group comparisons of changes in outcome variables over time were conducted according to intent-to-treat (ITT) methodology, with data from all dropouts included in analyses by carrying forward the last available observation for each subject. No adjustments were made for multiple comparisons. The diaries were analyzed for adverse events and differences in abdominal pain between the treatment groups (MG vs. SG) during the treatment period.
RESULTS
Pre-treatment group comparisons
There were no significant differences between groups in demographic characteristics (Table 1), although there was a tendency for MG subjects to have a higher level of education and income than SG subjects. The average overall IBS severity score before treatment was in the upper end of moderate range on the IBS-SS (30) and was nearly identical for the two groups.
Table 1.
Comparison of subject characteristics of the study of mindfulness meditation training compared with an attentional control for women with irritable bowel syndrome 2006–2009a
| Mindfulness group | Support group | |
|---|---|---|
| (a) Demographic characteristics | ||
| Age | 44.72 (12.55) | 40.89 (14.68) |
| Race | ||
| White | 29 (81%) | 25 (64%) |
| African-American | 5 (14%) | 8 (21%) |
| Other or not disclosed | 2 (6%) | 6 (15%) |
| Education | ||
| High-school graduate | 0 (0%) | 3 (8%) |
| Some college or technical school | 9 (25%) | 14 (36%) |
| Completed 4 years of college | 7 (19%) | 9 (23%) |
| Some graduate/ professional school | 6 (17%) | 4 (10%) |
| Completed graduate/ professional school | 13 (36%) | 8 (21%) |
| Not disclosed | 1 (3%) | 1 (3%) |
| Family income | ||
| < $20,000 | 3 (8%) | 4 (10%) |
| $21,000–40,000 | 6 (17%) | 15 (38%) |
| $41,000–$60,000 | 9 (25%) | 6 (15%) |
| $61,000–$80,000 | 5 (14%) | 7 (18%) |
| > $80,000 | 10 (28%) | 5 (13%) |
| Not disclosed | 3 (8%) | 2 (5%) |
| Relationship status | ||
| Single—never married | 8 (22%) | 16 (41%) |
| Living with a partner— not married | 2 (6%) | 3 (8%) |
| Married | 18 (50%) | 10 (26%) |
| Divorced or separated | 5 (14%) | 8 (21%) |
| Widowed | 2 (6%) | 1 (3%) |
| Not disclosed | 1 (3%) | 1 (3%) |
| (b)Clinical characteristics at enrollment | ||
| Overall IBS severity (IBS-SS) | 284.06 (84.34) | 287.54 (109.90) |
| IBS-QOL score | 64.80 (19.80) | 67.42 (20.50) |
| Psychological distress (BSI-18) | 57.06 (8.35) | 56.24 (9.67) |
| Mindfulness score (FFMQ) | 127.87 (22.33) | 129.70 (23.31) |
BSI-18, brief symptom inventory-18; FFMQ, five-facet mindfulness questionnaire; IBS, irritable bowel syndrome; IBS-QOL, irritable bowel syndrome-quality of life.
Values are given as mean (s.d.) or n (%).
No differences between groups were statistically significant.
Treatment credibility
Participants’ rating of the credibility of their assigned treatment was not different between the two groups (mean total scale sums±s.d. out of a maximum possible score of 45 was 35.03±6.31 for MG vs. 32.69±10.04 for SG; P = 0.26). Subjects in both groups rated their intervention as similarly logical for IBS treatment (6.91±2.15 on a 0–9 scale for MG vs. 6.28±2.67 for SG; P = 0.29) and reported similar confidence in their intervention’s likely success in reducing bowel symptoms (5.94±1.68 on a 0–9 scale for MG vs. 5.56±2.35 for SG; P = 0.449).
Outcomes
Effects on IBS severity—primary end point variable.
There was a significant main effect of time in the repeated-measures ANOVA. Intent-to-treat analyses of changes in overall IBS severity scores between baseline and post-treatment assessment (F(1,71) = 20.81, P<0.0001) and between baseline and 3-month follow-up (F(1,72) =21.449, P<0.0001). A significant intervention×time interaction for IBS severity was also found in both comparisons, indicating that participants in the MG experienced substantially greater improvements in IBS severity compared with baseline than did those in the SG (see Figure 2), both at post-treatment evaluation (F(1, 72) =7.88, P = 0.006) and at 3-month follow-up (F(1, 71) = 11.29, P = 0.001). Main effect for group was not significant in either ANOVA. Compared with baseline scores, overall IBS severity was reduced by 26.4% in the MG vs. 6.2% in the SG post-treatment and 38.2% vs. 11.8% at 3-month follow-up. The percentage of subjects who had at least 50-point reduction on the IBS-SS, which is considered clinical significant improvement on this test according to the scale developers (30), showed a non-significant trend toward difference between MG and SG on Mann-Whitney U-test both post-treatment (68.8% vs. 45.2%, P = 0.06) and at 3-month follow-up (75.0% vs. 53.1%; P = 0.08).
Figure 2.
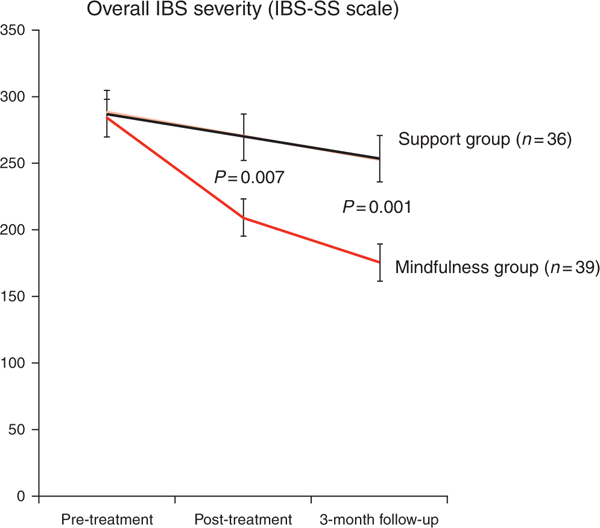
Comparison of changes in overall severity of IBS symptoms (IBS-SS score) in the two intervention groups from pre-treatment baseline to post-treatment and at 3-month follow-up assessments: The figure is based on ITT analysis, and P value shows significance of the timexgroup effect in the repeated-measures ANOVAs. ANOVAs, analyses of variances; IBS, irritable bowel syndrome; IBS-SS, irritable bowel syndrome severity scale; ITT, intent to treat.
Effects on individual IBS-SS symptoms.
Individual components of the IBS-SS scale were tested with repeated-measures ANOVA, followed by paired t-tests. The results are reported in Table 2. Abdominal pain severity was significantly more improved in the MG than the SG both immediately after treatment and at follow-up. Improvement in abdominal pain frequency and life interference due to bowel symptoms was not significantly different immediately following the treatment course, but the MG was more improved than the SG on both of those variables at 3-month follow-up, the study’s primary end point. Among all the ANOVA tests for changes in individual IBS-SS symptoms, main effect for group was only significant in the baseline vs. 3-month follow-up comparisons for dissatisfaction with bowel functioning (F(1,72) = 4.55, P = 0.036) and life interference from bowel symptoms (F(1,72) = 5.29, P = 0.024).
Table 2.
Changes in individual components of the IBS-SS from baseline to post-treatment and from baseline to 3-month follow-up among women with irritable bowel syndrome participating in mindfulness meditation training compared with those participating in a support group 2006–2009a
| Mindfulness group | Support group | Significance of change (P values) |
|||
|---|---|---|---|---|---|
| Mean (s.d.) | Mean (s.d.) | Within-group |
Time × group interaction | ||
| MG | SG | ||||
| Abdominal pain severity | |||||
| Baseline | 54.54 (22.82) | 53.35 (28.12) | |||
| Post-treatment | 35.00 (28.24) | 50.49 (28.85) | < 0.001 | 0.505 | 0.013 |
| 3-Month follow-up | 31.11 (25.69) | 45.49 (28.33) | < 0.001 | 0.065 | 0.015 |
| Abdominal pain frequency | |||||
| Baseline | 5.06 (2.57) | 4.88 (3.07) | |||
| Post-treatment | 4.37 (3.08) | 4.91 (3.25) | 0.108 | 0.941 | 0.188 |
| 3-Month follow-up | 3.14 (2.49) | 4.63 (3.14) | < 0.001 | 0.857 | 0.007 |
| Bloating severity | |||||
| Baseline | 55.03 (29.98) | 52.91 (29.80) | |||
| Post-treatment | 42.57 (28.86) | 49.22 (29.39) | 0.012 | 0.303 | 0.135 |
| 3-Month follow-up | 37.46 (29.18) | 47.55 (30.26) | 0.002 | 0.209 | 0.067 |
| Dissatisfaction with bowel habit | |||||
| Baseline | 68.17 (25.78) | 72.59 (26.13) | |||
| Post-treatment | 49.94 (27.48) | 65.15 (30.24) | 0.001 | 0.096 | 0.106 |
| 3-Month follow-up | 45.69 (30.18) | 62.56 (25.65) | 0.001 | 0.033 | 0.105 |
| Life interference | |||||
| Baseline | 55.74 (26.04) | 59.85 (31.02) | |||
| Post-treatment | 38.40 (26.53) | 55.72 (28.16) | 0.004 | 0.333 | 0.061 |
| 3-Month follow-up | 30.29 (27.93) | 50.85 (28.16) | < 0.001 | 0.057 | 0.037 |
ANOVA, analyses of variance.
Tested with repeated measures ANOVA, followed by post hoc within-group paired t-tests.
Post hoc tests comparing baseline to each post-treatment time point showed significant reductions for the MG subjects in all five IBS-SS components both immediately after treatment and at follow-up, with the single exception that frequency of abdominal pain (number of days with pain out of the past 10 days) was not significantly reduced at the immediate post-treatment assessment time point. In contrast, the SG subjects did not show a significant reduction on any IBS-SS component at either post-treatment assessment point.
Effects of IBS-QOL.
There was a significant main effect for time in IBS-QOL both between baseline and post-treatment assessment (F(1,71) = 14.98, P< 0.0001) and baseline and 3-month follow-up (F(1,71) = 17.94, P< 0.0001) on repeated-measures ANOVAs. The intervention×time interaction in IBS-QOL score changes trended toward significance immediately after treatment (F(1,70) = 3.28, P = 0.08), and reached significance at 3-month follow-up (F(1,71) = 5.12, P = 0.027), indicating that MG participants had experienced significantly greater improvement in IBS-QOL at the latter time point compared with SG participants. Main effect for group was not significant in either ANOVA. On post hoc within-group tests, only the MG group was found to have significantly increased IBS-QOL scores post-treatment and at follow-up compared with initial baseline values.
Effects on psychological symptoms.
Table 3 shows the results of intent-to-treat analyses of changes in psychological symptoms in the two groups. As expected, the MG group improved more at the 3 months, compared with the immediate post-treatment time point. On the brief symptom inventory-18, the degree of improvement from baseline to 3-month follow-up was significantly different between the two groups for anxiety and general symptom severity scores, and in both of those cases, the MG subjects improved more than the SG subjects. Main effect for group was not significant in any of the ANOVA tests of effects on psychological symptoms. In post hoc paired t-tests, the SG was not found to be significantly improved in any brief symptom inventory-18 subscale at either post-treatment time point, whereas the MG showed significant improvement on all the scales at 3-month follow-up, as well as on anxiety and general severity at the immediate post-treatment assessment point.
Table 3.
Changes in IBS-related psychological factors from baseline to post-treatment and from baseline to 3-month follow-up among women with IBS participating in mindfulness meditation training compared with those participating in a support group, 2006–2009a
| Mindfulness group | Support group | Significance of change from baseline (P values) |
|||
|---|---|---|---|---|---|
| Mean (s.d.) | Mean (s.d.) | Within group |
Time × group interaction | ||
| MG | SG | ||||
| IBS-QOL | |||||
| Baseline | 64.80 (19.80) | 67.22 (20.73) | |||
| Post-treatment | 74.99 (15.14) | 70.92 (17.40) | 0.001 | 0.135 | 0.075 |
| 3-Month follow-up | 76.73 (17.42) | 71.05 (18.25) | < 0.001 | 0.129 | 0.027 |
| BSI-18 anxiety | |||||
| Baseline | 55.00 (9.84) | 54.84 (10.60) | |||
| Post-treatment | 51.14 (8.82) | 53.20 (10.15) | 0.008 | 0.138 | 0.20 |
| 3-Month follow-up | 51.06 (9.92) | 54.65 (9.89) | < 0.001 | 0.879 | 0.02 |
| BSI-18 depression | |||||
| Baseline | 55.11 (10.55) | 54.78 (11.30) | |||
| Post-treatment | 53.62 (9.75) | 54.00 (12.66) | 0.266 | 0.591 | 0.725 |
| 3-Month follow-up | 52.49 (10.24) | 54.60 (12.42) | 0.040 | 0.899 | 0.205 |
| BSI-18 somatization | |||||
| Baseline | 57.37 (8.94) | 56.71 (8.86) | |||
| Post-treatment | 55.00 (7.86) | 56.42 (9.49) | 0.061 | 0.791 | 0.205 |
| 3-Month follow-up | 54.63 (8.33) | 55.03 (8.92) | 0.031 | 0.145 | 0.526 |
| BSI-18 general severity | |||||
| Baseline | 57.06 (8.35) | 56.24 (7.93) | |||
| Post-treatment | 53.66 (7.93) | 54.92 (11.08) | 0.002 | 0.605 | 0.154 |
| 3-Month follow-up | 53.51 (8.58) | 55.66 (10.40) | 0.001 | 0.564 | 0.049 |
| VSI | |||||
| Baseline | 52.28 (15.19) | 50.90 (16.03) | |||
| Post-treatment | 58.06 (12.78) | 52.06 (14.83) | 0.005 | 0.564 | 0.101 |
| 3-Month follow-up | 61.88 (14.20) | 52.49 (16.71) | < 0.001 | 0.568 | 0.023 |
ANOVA, analyses of variance; BSI, brief symptom index; IBS-QOL, irritable bowel syndrome-quality of life; MG, mindfulness group; SG, support group; VSI, visceral sensitivity index.
Tested with repeated measures ANOVA, followed by post hoc within-group paired t-tests.
At 3-month follow-up, but not immediately after treatment, participants in the MG evidenced significantly greater improvements in visceral anxiety compared with the SG (see Table 3). Within-group analyses showed that visceral sensitivity index scores were significantly reduced from baseline at both subsequent time points for the MG subjects, while no significant changes in visceral sensitivity index scores were seen in the SG subjects.
Effects on mindfulness.
There was a significant main effect for time in mindfulness scores both between baseline and post-treatment assessment (F(1,71) = 14.98, P< 0.0001) and between baseline and 3-month follow-up (F(1,71) = 17.94, P< 0.0001) on repeated-measures ANOVAs. The MG showed a significantly greater increase in mindfulness scores than the SG group (i.e., significant time-group interaction on repeated-measures ANOVA) at both time points: (F(1, 71) = 4.67, P = 0.03) and (F(1,69) = 4.27, P = 0.04). Main effect for group was not significant on either ANOVA. Only the MG group showed a significant increase in mindfulness after treatment on post hoc paired t -tests.
DISCUSSION
This study has demonstrated for the first time, using a well-controlled design, that 8 weeks of mindfulness training can reduce IBS symptom severity substantially and produce benefits that persist for at least 3 months after the intervention. The observed therapeutic impact of mindfulness training on IBS severity was clinically significant, as the mean reduction in severity was well above the 50 points recommended as a guideline for clinically significant change on this scale (30). On average, MG participants dropped 75 points after treatment in their IBS-SS scores, and that drop grew to 108 points by 3 months after treatment. In contrast, the SG’s drop in IBS severity was only 14 and 30 points, respectively, for the same two time points—far below clinical significance—indicating that the treatment outcomes observed for MG participants likely were the result of learning specific mindfulness techniques and not merely due to non-specific therapeutic factors such as social support and instructor attention. As we expected, the quality-of-life and psychological symptom benefits of mindfulness training above the control group developed gradually, manifesting at the trial’s primary end point, the 3-month follow-up. This, combined with the trend toward continuing improvement in bowel symptoms over time after treatment, suggests that mindfulness training may have long-lasting beneficial effects. Additional follow-up and analyses will be conducted to confirm a continued lasting effect of the mindfulness training up to 1 year after termination of intervention.
This study had a number of notable strengths. Randomization succeeded in producing groups that were well matched at base-line both in IBS severity and quality of life, and comparable in all demographics. We used a credibility scale to establish that the two interventions were perceived as equally credible treatments for IBS symptoms. Hence, differences in expectancy for the two interventions are not likely to have played a role in the different outcomes for the groups. The conduct of the two interventions was also highly similar in all non-specific aspects: both interventions were carried out in a small-group format with the same number and length of sessions and with a similar number of participants per group, and both included an IBS educational book as a part of the intervention package. In addition, we employed a validated process measure to confirm that the MG intervention led to significantly greater increases in dispositional mindfulness, which was the putative therapeutic mechanism, while the SG intervention did not produce a change in mindfulness. We also tested the therapeutic effects of mindfulness training 3 months after the end of the intervention to confirm that learning mindfulness likely has lasting, training-specific benefits. However, 3 months is a relatively short follow-up; future studies should test whether treatment benefits are maintained for longer periods such as 1 year or more.
A limitation of this study was that only female IBS patients were included, so the generalizability of the benefits of mindfulness training to male IBS patients is unknown. However, exclusion of men was a strategy adopted to minimize heterogeneity in this small-scale trial, and the generalizability is still broad since IBS is twice as common in women as in men. Future trials with larger samples should include male patients.
Although the two intervention groups in this study were not significantly different in any of the measured demographic characteristics, there was a trend for more highly educated and affluent individuals to be in the MG than the SG (see Table 1). To verify that differences in socioeconomic group composition did not bias our primary analyses, we re-ran the repeated measurement ANOVAs for our primary end point variable, IBS severity, with these two demographic variables as covariates. The results were comparable with those obtained without controlling for the influence of these variables, and education and income, therefore, do not seem to bias the findings presented here in Results.
This study adds to the growing body of literature on the efficacy of mindfulness training for other chronic illnesses. There is now evidence to support the therapeutic effect of training in mindfulness on a range of stress-related conditions, including type-2 diabetes (30,45), rheumatoid arthritis (46,47), attention-deficit hyperactivity disorder (48), and chronic low back pain (49,50).
At present, a number of other psychological interventions have been found to be helpful in ameliorating the severity of IBS. CBT, clinical hypnosis, and brief dynamic therapy have all been shown to be effective in multiple studies (7,8). Like these psychological interventions, mindfulness training leads to substantial improvements in bowel symptoms, as well as quality-of-life and psychological symptoms. Yet, mindfulness is conceptually and procedurally distinct from these other psychological treatments. For example, CBT uses Socratic dialog to restructure catastrophic appraisals of gut sensations, whereas mindfulness training does not attempt to restructure thought content, but instead promotes a non-reactive stance toward gut-related thoughts and feelings. Similarly, while clinical hypnosis employs suggestions and imagery to induce relaxation and alter the perception of visceral sensations, mindfulness training does not attempt to change sensations in the gut as much as foster awareness and acceptance of such sensations. Given these procedural differences, mindfulness training for IBS may act through a number of therapeutic mechanisms, including increasing nonreactivity to gut-focused anxieties and catastrophic thoughts about the ability to manage pain; enhancing awareness of IBS symptoms as innocuous interoceptive signals rather than threats to wellbeing; decreasing psychophysiological stress responses; and facilitating attentional disengagement from gut sensations and obsessive thoughts about visceral function.
Our study adds a new and distinctive psychological intervention option to the clinical armamentarium for addressing chronic IBS. Moreover, the intervention tested in our study has the potential advantage of being more cost effective than other psychological treatments for IBS, because mindfulness training may be conducted in moderately large groups, whereas the other types of psychological intervention for IBS are more commonly conducted in individual therapy format. Mindfulness-based stress reduction and similar programs, staffed by well-trained, experienced instructors, can be found at many medical centers throughout the US; physicians referring their patients to these programs can continue to prescribe standard-of-care therapies. Mindfulness training is safe and fully compatible with conventional care approaches and provides patients with greater autonomy in the control of their symptoms.
The results of this study raise a number of questions that should be addressed in further research. The similarities between the therapeutic effects of mindfulness training observed in our trial and in tests of other psychological treatments suggest that common mechanisms are likely responsible for the beneficial changes. Future research could test for common mediators of change in direct, head-to-head trials of different psychological interventions for this disorder, measuring the differential effects of various evidence-supported interventions on changes in cognitive-emotional factors, attentional mechanisms, and interoceptive processing of gut-related sensations.
Study Highlights.
WHAT IS CURRENT KNOWLEDGE
 Irritable bowel syndrome (IBS) is a common functional bowel disorder causing significant discomfort and impaired quality of life.
Irritable bowel syndrome (IBS) is a common functional bowel disorder causing significant discomfort and impaired quality of life.
 A substantial proportion of persons with IBS do not attain adequate relief through conventional medical approaches.
A substantial proportion of persons with IBS do not attain adequate relief through conventional medical approaches.
 Psychological interventions have been successful in improving clinical outcomes for IBS patients.
Psychological interventions have been successful in improving clinical outcomes for IBS patients.
WHAT IS NEW HERE
 This study has demonstrated, for the first time, using a well-controlled design, that 8 weeks of mindfulness training can substantially reduce IBS symptom severity.
This study has demonstrated, for the first time, using a well-controlled design, that 8 weeks of mindfulness training can substantially reduce IBS symptom severity.
 The therapeutic impact of mindfulness training on IBS severity was clinically significant and lasts at least 3 months.
The therapeutic impact of mindfulness training on IBS severity was clinically significant and lasts at least 3 months.
 Mindfulness training also resulted in quality-of-life and psychological symptom benefits by the primary end point, the 3-month follow-up.
Mindfulness training also resulted in quality-of-life and psychological symptom benefits by the primary end point, the 3-month follow-up.
ACKNOWLEDGMENTS
We gratefully acknowledge funding support for this trial from the National Institutes of Health, National Center for Complementary and Alternative Medicine Grant # R21 AT003619, as well as the National Institutes of Health, National Institute of Diabetes, Digestive and Kidney Disease Grant #s R24 DK067674 and R01 DK031369. We thank Gloria Suarez, Christine Meyer, Nicholas Scott, and Paula Umstead for their research assistance, Emily Fitch and Noah Martinson for facilitating the Support Group, and Julie Kosey for her initial work in developing and refining the interventions.
Financial support: This study was supported by Grant # R21 AT003619 from the National Institutes of Health, National Center for Complementary, and Alternative Medicine Grant.
Footnotes
CONFLICT OF INTEREST
Potential competing interests: Susan Gaylord was PI, and William Whitehead co-PI, on the funded proposal, with Douglas Mann and Olafur Palsson as co-investigators on the proposal. Rebecca Coble was project coordinator.
REFERENCES
- 1.Thompson WG, Longstreth GF, Drossman DA et al. Functional bowel disorders and functional abdominal pain. Gut 1999;45 (Suppl 2): II43–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sandler RS, Everhart JE, Donowitz M et al. The burden of selected digestive diseases in the United States. Gastroenterology 2002;122:1500–11. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Li Z, Andruzzi E et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci 1993; 38: 1569–80. [DOI] [PubMed] [Google Scholar]
- 4.Drossman DA. What does the future hold for irritable bowel syndrome and the functional gastrointestinal disorders? J Clin Gastroenterol 2005;39:S251–6. [DOI] [PubMed] [Google Scholar]
- 5.Whitehead WE, Levy RL, Von Korff M et al. The usual medical care for irritable bowel syndrome. Aliment Pharmacol Ther 2004; 20: 1305–15. [DOI] [PubMed] [Google Scholar]
- 6.Gaman A, Bucur MC, Kuo B. Therapeutic advances in functional gastrointestinal disease: irritable bowel syndrome. Ther Adv Gastroenterol 2009; 2: 169–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lackner JM, Mesmer C, Morley S et al. Psychological treatments for irritable bowel syndrome: a systematic review and meta-analysis. J Consult Clin Psychol 2004;72:1100–13. [DOI] [PubMed] [Google Scholar]
- 8.Kearney DJ, Brown-Chang J. Complementary and alternative medicine for IBS in adults: mind-body interventions. Nat Clin Pract Gastroenterol Hepatol 2008; 5: 624–36. [DOI] [PubMed] [Google Scholar]
- 9.Drossman DA, Camilleri M, Mayer EA et al. AGA technical review on irritable bowel syndrome. Gastroenterology 2002; 123: 2108–31. [DOI] [PubMed] [Google Scholar]
- 10.Brandt LJ, Chey WD, Foxx-Orenstein AE et al. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol 2009;104 (Suppl 1): S1–S35. [DOI] [PubMed] [Google Scholar]
- 11.Mayer EA, Tillisch K. The brain-gut axis in abdominal pain syndromes. AnnuRevMed 2011;62:381–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nieuwenheuys R The greater limbic system, the emotional motor system and the brain In: Hostege G, Bandler R, Saper CB (eds). The Emotional Motor System. Elsevier: Amsterdam, 1996, p 627. [Google Scholar]
- 13.Garland EL. The meaning of mindfulness: a second-order cybernetics of stress, metacognition, and coping. Complement Health Pract Rev 2007; 12: 15–30. [Google Scholar]
- 14.Lutz A, Slagter HA, Dunne JD et al. Attention regulation and monitoring in meditation. Trends Cogn Sci 2008; 12: 163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kabat-Zinn J An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psychiatry 1982; 4: 33–47. [DOI] [PubMed] [Google Scholar]
- 16.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med 1985;8:163–90. [DOI] [PubMed] [Google Scholar]
- 17.Kabat-Zinn J, Lipworth L, Burney R et al. Four-year follow-up of a meditation-based program for the self-regulation of chronic pain: treatment outcomes and compliance. Clin J Pain 1986; 2: 159–73. [Google Scholar]
- 18.Kaplan KH, Goldenberg DL, Galvin-Nadeau M. The impact of a meditation-based stress reduction program on fibromyalgia. Gen Hosp Psychiatry 1993;15:284–9. [DOI] [PubMed] [Google Scholar]
- 19.Goldenberg DL, Kaplan KH, Nadeau MG et al. A controlled study of a stress-reduction, cognitive-behavioral treatment program in fibromyalgia. J Musculoskeletal Pain 1994; 2: 53–66. [Google Scholar]
- 20.Palsson OS, Drossman DA. Psychiatric and psychological dysfunction in irritable bowel syndrome and the role of psychological treatments. Gastroenterol Clin North Am 2005;34:281–303. [DOI] [PubMed] [Google Scholar]
- 21.Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol 2003;13:500–5. [DOI] [PubMed] [Google Scholar]
- 22.Holzel BK, Ott U, Hempel H et al. Differential engagement of anterior cingulate and adjacent medial frontal cortex in adept meditators and non-meditators. Neurosci Lett 2007;421:16–21. [DOI] [PubMed] [Google Scholar]
- 23.Lazar SW, Kerr CE, Wasserman RH et al. Meditation experience is associated with increased cortical thickness. Neuroreport 2005;16:1893–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Slagter HA, Lutz A, Greischar LL et al. Mental training affects distribution oflimited brain resources. PLoS Biol 2007;5:e138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jha A, Krompinger J, Baime M. Mindfulness training modifies subsystems of attention. Cogn, Affect Behav Neurosci 2007;7:109–19. [DOI] [PubMed] [Google Scholar]
- 26.Brefczynski-Lewis JA, Lutz A, Schaefer HS et al. Neural correlates of attentional expertise in long-term meditation practitioners. Proc Natl Acad Sci USA 2007;104:11483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tang YY, Ma Y, Wang J et al. Short-term meditation training improves attention and self-regulation. Proc Natl Acad Sci USA 2007; 104: 17152–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whitehead WE, Palsson OS. Is rectal pain sensitivity a biological marker for irritable bowel syndrome: psychological influences on pain perception. Gastroenterology 1998; 115: 1263–71. [DOI] [PubMed] [Google Scholar]
- 29.Whitehead WE, Crowell MD, Robinson JC et al. Effects of stressful life events on bowel symptoms: subjects with irritable bowel syndrome compared with subjects without bowel dysfunction. Gut 1992; 33: 825–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther 1997;11:395–402. [DOI] [PubMed] [Google Scholar]
- 31.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiat 1972; 3: 257–60. [Google Scholar]
- 32.Kabat-Zinn J Full Catastrophe Living. Delacorte Press: NY, 1990. [Google Scholar]
- 33.Lackner JM, Jaccard J, Krasner SS et al. How does cognitive behavior therapy for irritable bowel syndrome work? A mediational analysis of a randomized clinical trial. Gastroenterology 2007;133:433–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lackner JM, Quigley BM, Blanchard EB. Depression and abdominal pain in IBS patients: the mediating role of catastrophizing. Psychosom Med 2004; 66: 435–41. [DOI] [PubMed] [Google Scholar]
- 35.Gaylord SA, Whitehead WE, Coble RS et al. Mindfulness for irritable bowel syndrome: protocol development for a controlled clinical trial. BMC Complement Altern Med 2009; 9: 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dean C, Wheeler LC. IBS for Dummies. Wiley: Hoboken, NJ, 2005. [Google Scholar]
- 37.Payne A, Blanchard EB. A controlled comparison of cognitive therapy and self-help support groups in the treatment of irritable bowel syndrome. J Consult Clin Psychol 1995; 63: 779–86. [DOI] [PubMed] [Google Scholar]
- 38.Drossman DA, Patrick DL, Whitehead WE et al. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol 2000;95:999–1007. [DOI] [PubMed] [Google Scholar]
- 39.Patrick DL, Drossman DA, Frederick IO et al. Quality of life in persons with irritable bowel syndrome: development and validation of a new measure. Dig Dis Sci 1998; 43: 400–11. [DOI] [PubMed] [Google Scholar]
- 40.Labus JS, Bolus R, Chang L et al. The visceral sensitivity index: development and validation of a gastrointestinal symptom-specific anxiety scale. Aliment Pharmacol Ther 2004;20:89–97. [DOI] [PubMed] [Google Scholar]
- 41.Derogatis LR. BSI-18: Administration, Scoring, and Procedures Manual. National Computer Systems: Minneapolis, MN, 2000. [Google Scholar]
- 42.Baer RA, Smith GT, Hopkins J et al. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006;13:27–45. [DOI] [PubMed] [Google Scholar]
- 43.Borkovec TD, Nau SD. Credibility of analogue therapy rationales. J Behav Ther Exp Psychiatry 1972;3:257–60. [Google Scholar]
- 44.Drossman DA, Toner BB, Whitehead WE et al. Cognitive-behavioral therapy vs. education and desipramine vs. placebo for moderate to severe functional bowel disorders. Gastroenterology 2003;125:19–31. [DOI] [PubMed] [Google Scholar]
- 45.van Son J, Nyklicek I, Pop VJ et al. Testing the effectiveness of a mindfulness-based intervention to reduce emotional distress in outpatients with diabetes (DiaMind): design of a randomized controlled trial. BMC Public Health 2011; 11:131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pradhan EK, Baumgarten M, Langenberg P et al. Effect of mindfulness-based stress reduction in rheumatoid arthritis patients. Arthritis Rheum 2007; 57: 1134–42. [DOI] [PubMed] [Google Scholar]
- 47.Zautra AJ, Davis MC, Reich JW et al. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. J Consult Clin Psychol 2008; 76: 408–21. [DOI] [PubMed] [Google Scholar]
- 48.Zylowska L, Ackerman DL, Yang MH et al. Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. J Atten Disord 2008;11:737–46. [DOI] [PubMed] [Google Scholar]
- 49.Morone NE, Greco CM, Weiner DK. Mindfulness meditation for the treatment of chronic low back pain in older adults: a randomized controlled pilot study. Pain 2008;134:310–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Esmer G, Blum J, Rulf J et al. Mindfulness-based stress reduction for failed back surgery syndrome: a randomized controlled trial. J Am Osteopath Assoc 2010;110:646–52. [PubMed] [Google Scholar]


