Abstract
Some evidence points to the positive effects of asset accumulation programs on mental health of children living in low-resource contexts. However, no evidence exists as to why and how such impact occurs. Our study aims to understand whether child poverty, child work, and household wealth serve as pathways through which the economic strengthening intervention affects the mental health AIDS-orphaned children.
The study employed a cluster-randomized experimental design with a family-based economic strengthening intervention conducted among 1,410 school-going AIDS-orphaned children ages 10 and 16 years old in 48 primary schools in South Western Uganda. To test the hypothesized relationships between the intervention, mediators (i.e. household wealth, child poverty, and child’s work) and mental health, we ran structural equation models that adjust for clustering of individuals within schools and account for potential correlation among the mediators.
We found significant unmediated effect of the intervention on children’s mental health at 24 months (B= −0.59; 95% CI: − 0.93, −0.25; p<0.001; β= −0.33). Furthermore, the results suggest that participation in the intervention reduced child poverty at 12 months, which in turn improved latent mental health outcome at 24 months (B= −0.14; 95% CI: −0.29, −0.01; p<0.06; β= −0.08). In addition, though not statistically significant at the .05 level, at 36 and 48 months, mental health of children in the treatment group improved by 0.13 and 0.16 standard deviation points correspondingly with no evidence of mediation. Our findings suggest that anti-poverty programs that aim solely to improve household income may be less advantageous to children’s mental health as compared to those that are specifically targeted towards reducing the impact of poverty on children. Further studies using more comprehensive measures of child work and age-appropriate child mental health may shed more light on understanding the link between asset accumulation interventions, child labor and children’s mental health.
Keywords: Randomized controlled trial, AIDS orphans, adolescent mental health, asset accumulation programs, economic strengthening, mediation, child poverty, Sub-Saharan Africa
INTRODUCTION
Worldwide, close to 385 million children are living in extreme poverty, with the highest rates concentrated in sub-Saharan Africa.1 Children growing up in poverty demonstrate fewer psychosocial competencies such as self-esteem and self-efficacy.2 They are also more likely to suffer from poor mental health outcomes, including internalizing disorders, such as depression and anxiety, and externalizing disorders, such as maladaptive behaviors and conduct problems.3 Furthermore, children in poverty are more likely to engage in paid and unpaid work, which interferes with schooling and poses potential dangers to their health, safety, and morale.4 There is some evidence that working children, specifically those whose work can be classified as child labor (e.g. working for strenuous hours and/or exposure to hazardous conditions), are more likely to suffer from depression and anxiety, compared to children who have never been engaged in child labor,5 suggesting a link between child poverty, child work, and poor mental health outcomes for children.
In the context of sub-Saharan Africa (SSA), the impact of HIV and AIDS may further influence this hypothesized link between poverty and child mental health. HIV heavily impacts the mental health of adolescents and their families as they endure the emotional and economic stress of the epidemic in resource limited contexts.6,7 Furthermore, due to long episodes of parental illness and/or parental death, children are at an elevated risk of poverty and school separation,8 characteristics that are commonly associated with child work classified as child labor.9 For children who have lost one or both parents to the virus, mental health concerns are exacerbated, with studies showing higher rates of depression, anxiety, and post-traumatic stress for this demographic.10,11
With poverty being a risk factor for child mental health, governments and several organizations are investing in family economic strengthening programs, and research has shown the positive effects of such interventions, including cash transfers and microfinance, for improving children’s physical12 and mental health;13 reducing child poverty and children’s material deprivations, such as clothing and food,14 and curtailing child labor.9
In this study, a conceptual model connecting poverty to child mental health is proposed based on the Asset Theory15, which posits that assets, such as savings, income generating activities, and microenterprises, not only impact economic stability for individuals and households but also have important developmental, psychological and social benefits. “Asset-building” refers to efforts that enable people with limited financial and economic resources or opportunities to acquire and accumulate long-term productive assets. Increased assets lead to expectations for more resources in the future, optimistic thinking, feelings of safety and security, and future planning.
The existing evidence predominately points to the positive effects of asset accumulation programs on children’s psychosocial outcomes16,17. This being said, however, the effect of these programs on accumulation of assets and reduction of poverty is, at best, inconclusive.18,19 Furthermore, no evidence exists as to why and how such impact occurs20. Therefore, specific mechanisms of change through which these interventions affect child mental health is yet to be understood.
To address the aforementioned gap, we use data from the Bridges to the Future study – a 5-year (2011–2016) longitudinal cluster-randomized experimental intervention funded by the National Institute of Child Health and Development (NICHD) and administered in the South Western region of Uganda (an area heavily affected by HIV, poverty and with limited health services). We examine the effects of the Bridges intervention – a family-based combination intervention, comprising economic strengthening and asset accumulation centered around micro-savings and financial management training and mentorship– on children’s mental health while exploring the intersections with household wealth, child work, and child poverty. Specifically, our study seeks to answer two primary questions:
How does participation in the Bridges to the Future intervention affect mental health among AIDS-orphaned children in our sample?
How do household wealth, child work, and child poverty mediate the effect of Bridges to the Future intervention on child mental health?
METHODS
Study design
The Bridges to the Future study was funded by the National Institute of Child Health and Human Development (NICHD) and approved by Columbia University Institutional Review Board (AAAI1950) and the Uganda National Council for Science and Technology (SS2586). The procedure for obtaining informed consent in this study was consistent with the approved IRB protocol.
The study employed a cluster-randomized experimental design to recruit 1,410 school-going AIDS-orphaned children in 48 primary schools, divided into three parallel arms: 1) a control arm receiving usual care services for school-going AIDS-affected children in the region; 2) treatment arm 1 receiving usual care plus a family-based combination intervention comprising economic strengthening and asset accumulation with savings matched on 1:1 rate—known as the Bridges; 3) treatment arm 2 receiving usual care plus a family-based combination intervention comprising economic strengthening and asset accumulation with matching ratio of 2:1— Bridges PLUS. To avoid cross-arm contamination, randomization was conducted at the school level (16 schools in each study arm). The family-based combination intervention offered to participants consisted of three components: (1) matched savings account (Child Development Accounts); (2) a workshop on family financial management and microenterprise development offered to both the children and their caregivers; and (3) the mentorship program, a nine-session curriculum aimed at helping the study participants to develop the ability to identify specific future goals and educational aspirations. The only difference between the two treatment arms was in the ratio of matched savings in Child Development Accounts (ratio of 1:1 or 2:1).
Children between ages 10 and 16 years old were eligible to participate in the study if they met the following criteria: (1) identified as an AIDS orphan, having lost one or both parents to AIDS; (2) living within a family (broadly defined and not an institution or orphanage, as those in institutions have different familial needs); (3) enrolled in grades 5 or 6 in a public primary school in the study region.
Repeated-measures data was collected from children at 5 time points (baseline, 12 months, 24 months, 36 months, and 48 months) using a 90-minute interviewer-administered survey. Informed written consent was obtained from caregivers consenting for their children to participate in the study, and informed assent was obtained from all participating children. Children were assented separately from their caregivers to avoid the potential of coercion.
Measures
Child’s mental health is a latent variable constructed from three correlated indicators: the Beck Hopelessness Scale, Child Depression Inventory, and Tennessee Self-Concept Scale. All three indicators have been previously tested with AIDS-orphaned children in Uganda, and other sub-Saharan Africa countries21–23.
The Beck Hopelessness Scale24 is a 20-item self-report inventory measuring a child’s pessimistic outlook and negative expectations about events in her/his future. Each item on the scale is a binary variable. The score ranges from 0 to 20 (the higher the score the higher the degree of hopelessness).
The full Child Depression Inventory25 is a scale consisting of 24 items, with each item ranging from 0 to 2. The scale ranges from 0 to 48; the higher the score the higher the child’s depression level.
The full Tennessee Self-Concept Scale26: Second Edition (TSCS: 2) is an 82-item self-report inventory that includes six specific domains of self-concept (physical, moral, personal, family, social, and academic). We use a shorter version of the TSCS, previously tested in Uganda taking into account specific context and wording that reflects the language and speech used by Ugandan youth27. The shorter version of TSCS used in this study is a 17-item self-report inventory, each item measured from 1 to 5. The scale ranges from 17 to 85, with a higher score corresponding to a higher self-concept.
Mediators.
We examine three mediators—household wealth, child poverty, and child’s work—that are hypothesized to transmit the effect of family-based economic strengthening and asset accumulation intervention on child’s mental health outcomes.
Household wealth is measured by the household wealth index adapted from the Demographic Health Survey/DHS that was tested globally in more than 90 developing countries. We replicated the DHS method in constructing the household wealth index. The following three steps were taken in calculating the household wealth index: first, the indicator variables (calculating z-scores) were standardized; second, the factor coefficient scores (factor loadings) were calculated; and third the indicator values were multiplied by the loadings and summed to produce the household’s index value.
Child poverty is measured using the composite score that consists of six binary (Yes/No) variables indicating whether the child has more than two sets of clothes; a blanket; at least 2 pairs of shoes; had meat/fish at least once in the last week; had 3 meals per day in the last 7 days; and had tea with sugar at least once in the last 7 days. The questions were adapted from DHS questionnaire and Uganda Bureau of Statistics’ Household Survey. The score ranges from 0 to 6. The lower the score, the worse the child poverty.
Child’s work is measured by frequency of working (0=Never, 1=Once in a while, 2=Almost every week, 3=Few days a week, and 4=Almost every day).
Intervention.
As mentioned earlier, the only difference between the two treatment arms in this study was in the ratio of matched savings. This difference bears no conceptual significance for the analyses conducted in this paper, and, therefore, we have combined both arms into one treatment group—thus creating a binary measure of intervention (1=treatment group and 0=control group).
Statistical analyses
For baseline sample characteristics, we report proportions (for categorical variables) or means (for continuous variables), 95% confidence intervals (CIs), and adjusted Wald F-statistics (design-based F) to examine individual-level variations while accounting for potential correlation between same-school observations. We report the baseline characteristics following the CONSORT guideline (see point #15 on the checklist: http://www.consort-statement.org/checklists/view/32--consort-2010/510-baseline-data.)
To test the hypothesized relationships between the intervention, mediators and children’s mental health, we fitted three structural equation models (SEMs) using Mplus 8.128. To examine whether different mediators were important at each measurement wave, separate models were fitted for Time 3 (i.e. 24-month follow-up), Time 4 (36-month follow-up), and Time 5 (48-month follow-up). Specifically, to preserve temporal ordering, intervention group assignment predicted a) the mediators at 12 months, which in turn predicted the latent mental health outcome at 24 months (Model 1); b) the mediators at 24 months, which in turn predicted the latent mental health outcome at 36 months (Model 2), and c) the mediators at 36 months, which in turn predicted the latent mental health outcome at 48 months (Model 3). In these analyses, the direct effect (c’) is the effect of intervention in the absence of mediators (in other words, this is the effect that is not mediated). The indirect effect (a*b) quantifies the amount of mediation. Thus, the total intervention effect (c) on mental health is the sum of direct and indirect effects (c = c’ + ab). To account for possible between-individual correlation (observations clustered within schools), standard errors and test statistics adjust for clustering of individuals within schools using robust Huber-White sandwich variance estimation29. We controlled for child’s age, gender and orphanhood status (single orphan vs. double orphan). The models also account for potential correlation among the mediators by estimating correlations among their residuals.
To account for the possible exposure-mediator interactions we first fitted models with these interactions. However, none of these interactions was statistically significant. The choice of no-interaction models over the models with interactions was also strongly favored by the information theoretic criteria values (AIC and BIC). Therefore, these interactions were dropped from the model and the results presented below originate from models with main effects only.
Global model fit of each SEM was evaluated using the chi-square test of exact fit. Because the chi-square test of exact fit can be sensitive to trivial model-data fit discrepancies, especially in larger samples30, we also report the following well-studied descriptive fit statistics: the Comparative Fit Index (CFI)31, the Root Mean Square Error of Approximation (RMSEA)32, and the Standardized Root Mean Square Residual (SRMR)33. Following Hu and Bentler’s recommendations based on extensive simulations, thresholds for satisfactory model fit were determined by a) CFI ≥ .95 and SRMR ≤ .08 or b) RMSEA ≤ .06 and SRMR <.0834. For the indirect effects, we obtained the cluster-adjusted bootstrap-based confidence intervals with 5,000 requested replicate samples. Obtaining bootstrap-based confidence intervals accounts for asymmetric distributions of the indirect effects35. For each effect, we report the unstandardized linear regression coefficient B, the 95% confidence interval for B, and the standardized estimate β.
RESULTS
At baseline, the average age of participants enrolled in the study was 12.7 years. About 19.6% of participants were double orphans (i.e. children who have lost both biological parents). Females composed 56% of the sample. At baseline, the average depression score among the study participants was 9.8 out of 48, the average score on the Beck Hopelessness Scale was 5.4 out of 20, and the average score on Tennessee Self-Concept Scale was 66.8.
In the original Child Depression Inventory consisting of 27 items, the cutoff point of 12 was established to distinguish children at risk of depression from non-depressed children25. In the original 20-item short form of the Tennessee Self-Concept Scale26, scores below 30 are interpreted as person having very low self-concept, 31–40 = low, 41–59 = average, 60–69 = high, and score above 70 is interpreted as person having very high self-concept. Finally, in the original Beck Hopelessness Scale24, the score ranging from 0 to 3 corresponds to the minimal hopelessness, 4–8 = mild hopelessness, 9–14 moderate hopelessness, and 15–20 corresponds to severe hopelessness. This being said, however, we refrain from using these cutoff points due to likely cross-cultural differences in somatization and expression of mental health issues36. It has been documented that the cutoff points and the diagnostic criteria prescribed in the DSM (Diagnostic and Statistical Manual of Mental Disorders) often inadequately capture cross-cultural variation in mental health experiences37. Therefore, all three measures used in our study were culturally adapted to the specific population of interest, i.e. vulnerable AIDS-orphaned children and adolescents in Southern Uganda. The measures were tested in previous studies13,27 and they demonstrated strong psychometric properties and performed significantly better than other mental health measures used. In this study, we treat children’s mental health as a continuum where even subclinical deficits in mental health may lower quality of life and may be a public health concern.
The mediation model
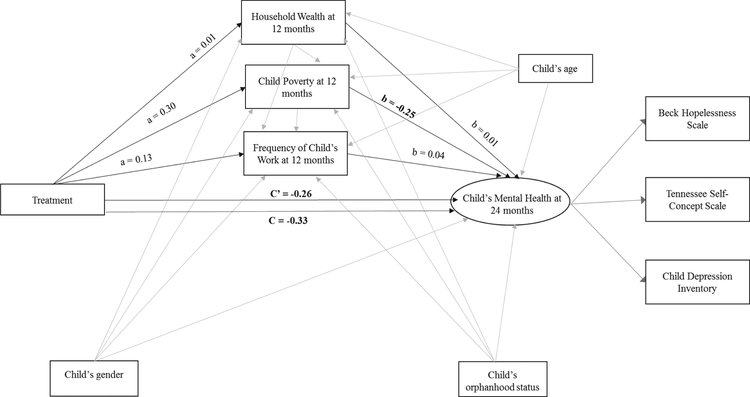
The results for Model 1 (Table 2, Figure 1) examining the effects of intervention participation on mental health at 24 months demonstrated excellent global fit of the model to the data (χ2(14) = 24.3, p = .04; CFI = .99; RMSEA = .02, and SRMR = .02). There was a significant (at 0.1% level) total effect of the intervention on the latent mental health variable at 24-months. Participants in treatment group reported better mental health outcomes at 24 months than control participants (B= −0.59; 95% CI: - 0.93, −0.25; p<0.001; β= −0.33). In other words, at 24 months, mental health of children in the treatment group improved by 0.33 standard deviation points. The direct (i.e. unmediated) effect of the intervention on mental health was also statistically significant at the 1% level (B= −0.47; 95% CI: - 0.8, −0.12; p<0.01; β= −0.26). The indirect effect of the intervention on mental health through household wealth was not significant (B = 0; 95% CI: −0.01, 0.02; p<1; β=0); nor was the effect of the intervention on mental health through frequency of child’s work (B = 0.01; 95% CI: 0, 0.04; p<0.3; β= 0.01) with the 95% confidence intervals tightly grouped near zero, suggesting that these potential mediators’ indirect effects were close to zero. However, the indirect effect of the intervention on mental health through child poverty was marginally significant at 6% level (B= −0.14; 95% CI: −0.29, −0.01; p<0.06; β= −0.08), indicating that intervention participation reduced child poverty at 12 months which, in turn, was associated with better mental health outcomes for children at 24 months. The variation in the latent mental health outcome at 24 months explained by the intervention and mediators together is 10% (R2=0.1, 95% CI: 0.06, 0.14).
Table 2:
Structural Equation Model (SEM) Results
| MODEL 1: 24-MONTH FOLLOW UP (N=l,337) | MODEL 2: 36-MONTH FOLLOW UP (N=l,304) | MODEL 3: 48-MONTH FOLLOW UP (N=l,295) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non- stand. Coeff. | [95% Conf. Interval] | Standr. Coeff. | Non-stand. Coeff. | [95% Conf. Interval] | Standr. Coeff. | Nonstand. Coeff. | [95% Conf. Interval] | Standr. Coeff | ||||
| MENTAL HEALTH BY | ||||||||||||
| Beck Hopelessness Scale | 1.00 | — | — | 0.63 | 1.00 | — | — | 0.67 | 1.00 | — | — | 0.71 |
| Tennessee Self-Concept | −4.01 | −4.68 | −3.54 | −0.76 | −3.39 | −3.87 | −2.98 | −0.73 | −3.29 | −3.68 | −2.89 | −0.74 |
| Depression | 1.57 | 1.31 | 1.88 | 0.66 | 1.85 | 1.62 | 2.10 | 0.72 | 1.23 | 1.10 | 1.37 | 0.72 |
| MENTAL HEALTH ON | ||||||||||||
| Household wealth | 0.01 | −0.11 | 0.12 | 0.01 | −0.13 | −0.28 | 0.02 | −0.06 | −0.21 | −0.36 | −0.06 | −0.10 |
| Child poverty | −0.33 | −0.43 | −0.24 | −0.25 | −0.31 | −0.40 | −0.23 | −0.21 | −0.34 | −0.44 | −0.24 | −0.22 |
| Frequency of child’s work | 0.06 | −0.04 | 0.16 | 0.04 | 0.05 | −0.04 | 0.14 | 0.03 | 0.18 | 0.07 | 0.30 | 0.12 |
| Child’s gender | −0.07 | −0.39 | 0.22 | −0.04 | 0.94 | 0.63 | 1.27 | 0.47 | 0.64 | 0.33 | 0.91 | 0.30 |
| Child’s age | 0.09 | −0.01 | 0.18 | 0.05 | 0.21 | 0.11 | 0.32 | 0.11 | 0.20 | 0.09 | 0.30 | 0.10 |
| Child’s orphanhood status | −0.15 | −0.44 | 0.12 | −0.08 | −0.30 | −0.59 | −0.03 | −0.15 | −0.08 | −0.40 | 0.22 | −0.04 |
| WEALTH ON | ||||||||||||
| Treatment | 0.01 | −0.16 | 0.19 | 0.01 | −0.03 | −0.21 | 0.11 | −0.03 | −0.02 | −0.16 | 0.10 | −0.02 |
| Child’s gender | −0.24 | −0.38 | −0.11 | −0.24 | −0.28 | −0.41 | −0.17 | −0.28 | −0.26 | −0.40 | −0.14 | −0.26 |
| Child’s age | 0.03 | −0.03 | 0.08 | 0.03 | 0.00 | −0.07 | 0.06 | 0.00 | −0.07 | −0.13 | −0.01 | −0.07 |
| Child’s orphanhood status | −0.08 | −0.21 | 0.07 | −0.08 | 0.00 | −0.13 | 0.14 | 0.00 | 0.05 | −0.08 | 0.20 | 0.05 |
| CHILD POVERTY ON | ||||||||||||
| Treatment | 0.43 | −0.01 | 0.84 | 0.30 | 0.38 | 0.04 | 0.73 | 0.28 | 0.24 | −0.02 | 0.50 | 0.19 |
| Child’s gender | 0.10 | −0.03 | 0.24 | 0.07 | 0.38 | 0.27 | 0.48 | 0.27 | 0.43 | 0.28 | 0.58 | 0.33 |
| Child’s age | −0.07 | −0.15 | 0.01 | −0.05 | −0.04 | −0.10 | 0.03 | −0.03 | −0.01 | −0.07 | 0.06 | 0.00 |
| Child’s orphanhood status | 0.13 | −0.04 | 0.31 | 0.09 | 0.04 | −0.14 | 0.22 | 0.03 | −0.02 | −0.22 | 0.17 | −0.02 |
| FREQUENCY ON | ||||||||||||
| Treatment | 0.15 | −0.02 | 0.30 | 0.13 | 0.12 | −0.04 | 0.26 | 0.10 | 0.13 | −0.01 | 0.27 | 0.09 |
| Child’s gender | −0.54 | −0.71 | −0.39 | −0.45 | −0.54 | −0.68 | −0.40 | −0.46 | −0.49 | −0.64 | −0.34 | −0.36 |
| Child’s age | 0.07 | 0.01 | 0.12 | 0.06 | 0.08 | 0.01 | 0.14 | 0.07 | 0.16 | 0.10 | 0.21 | 0.12 |
| Child’s orphanhood status | −0.02 | −0.17 | 0.13 | −0.01 | −0.09 | −0.29 | 0.10 | −0.07 | −0.06 | −0.25 | 0.12 | −0.05 |
| WEALTH WITH | ||||||||||||
| Child poverty | 0.30 | 0.23 | 0.38 | 0.22 | 0.21 | 0.12 | 0.30 | 0.16 | 0.13 | 0.05 | 0.22 | 0.10 |
| Frequency of child’s work | −0.02 | −0.09 | 0.05 | −0.01 | −0.02 | −0.09 | 0.05 | −0.02 | −0.12 | −0.20 | −0.05 | −0.09 |
| CHILD POVERTY WITH FREQUENCY OF CHILD’S WORK | 0.00 | −0.08 | 0.09 | 0.00 | 0.07 | −0.02 | 0.16 | 0.05 | 0.01 | −0.10 | 0.12 | 0.00 |
| INTERCEPTS | ||||||||||||
| Beck Hopelessness Scale | 4.16 | 2.73 | 5.68 | 1.45 | 1.20 | −0.27 | 2.55 | 0.40 | 1.38 | −0.15 | 2.98 | 0.47 |
| Tennessee Self-Concept | 69.30 | 63.46 | 75.14 | 7.22 | 79.39 | 74.73 | 84.04 | 8.42 | 77.94 | 72.95 | 82.55 | 8.35 |
| Depression | 9.72 | 7.35 | 12.14 | 2.25 | 3.63 | 1.01 | 6.22 | 0.70 | 14.58 | 12.58 | 16.52 | 4.04 |
| Household wealth | 0.11 | −0.70 | 0.89 | 0.11 | 0.50 | −0.40 | 1.40 | 0.50 | 1.26 | 0.47 | 2.09 | 1.26 |
| Child poverty | 3.99 | 2.84 | 5.12 | 2.83 | 3.48 | 2.58 | 4.42 | 2.53 | 3.46 | 2.54 | 4.33 | 2.62 |
| Frequency of child’s work | 0.44 | −0.48 | 1.33 | 0.36 | 0.30 | −0.59 | 1.22 | 0.26 | −0.69 | −1.41 | 0.02 | −0.51 |
| RESIDUAL VARIANCES | ||||||||||||
| Beck Hopelessness Scale | 4.93 | 4.16 | 5.80 | 0.60 | 5.03 | 4.23 | 5.83 | 0.55 | 4.38 | 3.70 | 5.10 | 0.50 |
| Tennessee Self-Concept | 39.19 | 32.81 | 45.68 | 0.43 | 42.09 | 36.70 | 47.33 | 0.47 | 39.53 | 33.47 | 45.93 | 0.45 |
| Depression | 10.57 | 9.18 | 12.00 | 0.56 | 12.80 | 10.88 | 14.91 | 0.48 | 6.31 | 5.40 | 7.32 | 0.48 |
| Household wealth | 0.98 | 0.86 | 1.13 | 0.98 | 0.98 | 0.87 | 1.10 | 0.98 | 0.98 | 0.90 | 1.06 | 0.98 |
| Child poverty | 1.93 | 1.77 | 2.14 | 0.97 | 1.81 | 1.66 | 2.02 | 0.96 | 1.69 | 1.57 | 1.84 | 0.97 |
| Frequency of child’s work | 1.36 | 1.18 | 1.56 | 0.94 | 1.26 | 1.06 | 1.48 | 0.93 | 1.68 | 1.45 | 1.92 | 0.93 |
| Mental health latent | 2.98 | 2.26 | 3.85 | 0.90 | 3.63 | 2.96 | 4.41 | 0.89 | 3.95 | 3.26 | 4.80 | 0.89 |
| INDIRECT EFFECTS | ||||||||||||
| Household wealth | 0 | −0.01 | 0.02 | 0 | 0 | −0.02 | 0.04 | 0 | 0.01 | −0.02 | 0.05 | 0 |
| Child poverty | −0.14 | −0.29 | −0.01 | −0.08 | −0.12 | −0.25 | −0.01 | −0.06 | −0.08 | −0.19 | 0.00 | −0.04 |
| Frequency of child’s wosrk | 0.01 | 0.00 | 0.04 | 0.01 | 0.01 | 0.00 | 0.03 | 0.00 | 0.02 | 0.00 | 0.07 | 0.01 |
| Total indirect | −0.13 | −0.28 | 0.01 | −0.07 | −0.11 | −0.25 | 0.00 | −0.05 | −0.06 | −0.17 | 0.05 | −0.03 |
| TOTAL EFFECT | −0.59 | −0.93 | −0.25 | −0.33 | −0.27 | −0.60 | 0.04 | −0.13 | −0.33 | −0.64 | 0.00 | −0.16 |
| DIRECT EFFECT | −0.47 | −0.80 | −0.12 | −0.26 | −0.16 | −0.51 | 0.14 | −0.08 | −0.27 | −0.60 | 0.02 | −0.13 |
Figure 1: Mediation model at 24 months follow-up.
Marked bold are statistically significant coefficients.
The model in the figure includes the following: a = effect of the intervention on mediators; b = effect of the mediators on children’s mental health; c’ = direct (unmediated) effect of the intervention on children’s mental health; c = total effect of the intervention on children’s mental health.
The model account for potential correlation among the mediators by estimating correlations among their residuals. The models also control for child’s age, gender, and orphanhood status (single orphan vs. double orphan). Given the complexity of the model, coefficients are shown only for a, b, c, and c’ paths. All other coefficients produced by the model are available in Table 2.
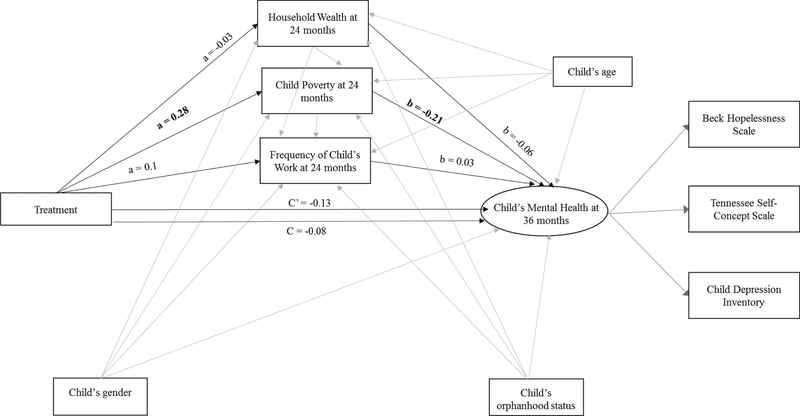
The results for Model 2 (Table 2, Figure 2) examining the effects of intervention participation on mental health at 36 months demonstrated very good global fit of the model to the data (χ2(14) = 38.12, p < .001; CFI = .98; RMSEA = .04, and SRMR = .02). At 36 months, mental health of children in the treatment group improved by 0.13 standard deviation points, but the total effect of the intervention on mental health was not statistically significant at the 5% level (B = −0.27; 95% CI: −0.6, 0.04; p<0.1; β= −0.13). The direct (i.e. unmediated) effect of the intervention on mental health was also not statistically significant at the 5% level (B = −0.16; 95% CI: −0.51, 0.14; p<0.3; β= −0.08). While the indirect effect of the intervention on mental health was not significant at the 5% level either through household wealth (B = 0.004; 95% CI: −0.02, 0.04; p<0.7; β=0.002) or through the frequency of child’s work (B = −0.01; 95% CI: 0, 0.03; p<0.5; β=0.003), the indirect effect of the intervention on mental health was again significant (at the 5% level) through child poverty (B= −0.12; 95% CI: −0.25, −0.01; p<0.05; β= −0.06). At 36 months, the variation in the latent mental health outcome at 36 months explained by the intervention and mediators together is 11% (R2=0.11, 95% CI: 0.07, 0.14).
Figure 2: Mediation model at 36 months follow-up.
Marked bold are statistically significant coefficients.
The model in the figure includes the following: a = effect of the intervention on mediators; b = effect of the mediators on children’s mental health; c’ = direct (unmediated) effect of the intervention on children’s mental health; c = total effect of the intervention on children’s mental health.
The model account for potential correlation among the mediators by estimating correlations among their residuals. The models also control for child’s age, gender, and orphanhood status (single orphan vs. double orphan). Given the complexity of the model, coefficients are shown only for a, b, c, and c’ paths. All other coefficients produced by the model are available in Table 2.
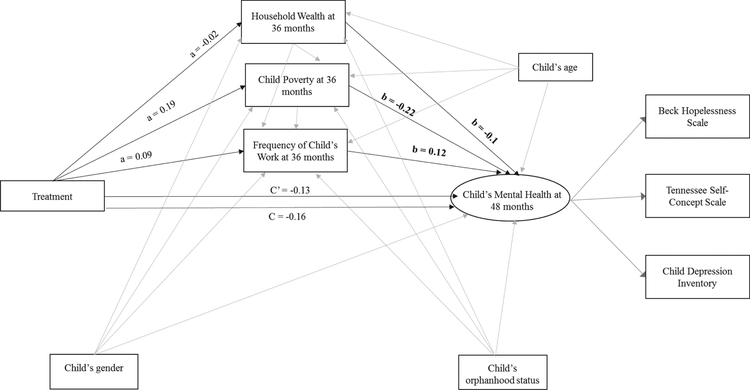
The results for Model 3 (Table 2, Figure 3) examining the effects of intervention participation on mental health at 48 months demonstrated very good global fit of the model to the data (χ2(14) = 54.57, p < .001; CFI = .96; RMSEA = 0.05, and SRMR = .02). At 48 months, mental health of children in treatment group improved by 0.16 standard deviation points, but the total effect of the intervention on the latent mental health was not statistically significant at the 5% level (B = −0.33; 95% CI: −0.64, 0.002; p<0.05; β= −0.16). As indicated earlier, given the asymmetric distribution of the indirect effects, we are cautious in interpreting the statistical significant of indirect effects solely based on the p-values. In particular, despite the p-value below 0.05, the bootstrapped 95% CI [−0.6, 0.04] falls on zero, and, therefore, we refrain from asserting the statistical significance of the effect. The direct (i.e. unmediated) effect of the intervention on the latent mental health variable was also not statistically significant at the 5% level (B = −−0.27; 95% CI: −.06, 0.02; p<0.08; β= −0.13). Similar to earlier results, the indirect effect of the intervention on mental health was not significant at the 5% level either through household wealth (B = 0.005; 95% CI: −0.02, 0.05; p<0.7; β=0.002) or through the frequency of child’s work (B = 0.02; 95% CI: 0, 0.07; p<0.2; β=0.01), the indirect effect of the intervention on mental health was marginally significant (at the 5% level) through child poverty (B= −0.08; 95% CI: −0.2, −0.002; p<0.08; β= −0.04). At 48 months, the variation in the latent mental health outcome accounted for by the intervention and mediators together is 11% (R2=0.11, 95% CI: 0.07, 0.15).
Figure 3: Mediation model at 48 months follow-up.
Marked bold are statistically significant coefficients.
The model in the figure includes the following: a = effect of the intervention on mediators; b = effect of the mediators on children’s mental health; c’ = direct (unmediated) effect of the intervention on children’s mental health; c = total effect of the intervention on children’s mental health.
The model account for potential correlation among the mediators by estimating correlations among their residuals. The models also control for child’s age, gender, and orphanhood status (single orphan vs. double orphan). Given the complexity of the model, coefficients are shown only for a, b, c, and c’ paths. All other coefficients produced by the model are available in Table 2.
DISCUSSION
This study is among the first to explore the mechanisms of change by which asset accumulation programs (such as Bridges to the Future) influence children’s mental health. We investigated these mechanisms by answering two questions. The first question investigated the effect of the intervention on children’s mental health. Consistent with findings from previous studies13,17,21, our results demonstrate a significant positive effect of intervention on children’s mental health at 24 months.
On one hand, these findings align with other findings in the region that have found mental health gains to diminish after cash assistance is no longer provided.38 While tracer studies have demonstrated the positive long-term effects of cash transfers on a range of physical and cognitive outcomes for children39,40, to date, there is a dearth of evidence to show sustained mental health effects as a result of economic interventions, either cash or savings-led. On the other hand, however, it is possible that the specific mental health indicators used in the construction of latent mental health variable, especially the CDI index, work best with relatively young children compared to older adolescents (above age 17, the age at which the majority of the participants were by Waves 4 and 5 follow-ups). More research is needed throughout SSA to understand adolescent development within varied cultural contexts. Improving the evidence base would allow implementers to design programs that offer tailored interventions at each stage of adolescence.
The study’s second question investigated whether household wealth, child work and child poverty mediated the intervention on children’s mental health. To summarize, we found no evidence for mediating effect of the household poverty or the child’s work in transmitting the effect of family-based economic empowerment intervention on children’s mental health. The strongest evidence for mediation of the intervention effect by childhood poverty is seen at 24 months where statistical significance at p<.05 was observed. Though not statistically significant, the same overall pattern of results is seen at 36 and 48 months. Furthermore, our findings indicate that the variation in the latent mental health outcome accounted for by the intervention and mediators together ranged between 10% and 11%, which falls between the small and medium mediation effect41. Our findings suggest that child poverty may transmit some of the effect of intervention on mental health outcomes at 24 months. In line with numerous previous studies demonstrating the negative effect of poverty on children’s mental health.42,43, we found some evidence that the effect of the asset accumulation program on children’s mental health, at least in the short-run, may occur through reductions in poverty among these children. We found no evidence that the effect of the asset accumulation program on children’s mental health occurs through reduction of household poverty. This finding is in line with argument that children experience poverty differently from adults; and, therefore, using household poverty in reference to child well-being may not render an accurate picture of child poverty44,45. Our findings would then suggest that anti-poverty programs that aim solely to improve household income may be less advantageous to children’s mental health as compared to those that are specifically targeted towards reducing the impact of poverty on children. Additionally, our findings also suggest that changes to the frequency of children’s work were not influential in improving mental health. However, it is important to note that the module assessing children’s work was limited. Therefore it was unable to elicit sufficient information to gauge whether children were involved in child labor, specifically work that is mentally, physically, socially, or morally harmful to children and that interferes with schooling. More research is needed to understand the link between asset accumulation interventions, child labor and children’s mental health.
Limitations
One of the key limitations of this study is the possibility that the measures assessing mental health were not sufficiently exhaustive to capture the full-range of feelings and experiences of adolescent participants within the Ugandan context. The study utilized culturally adapted and tested versions of the Beck Hopelessness scale, the Child Depression Inventory, and the Tennessee Self-Concept scale. However, it is possible that these measures function differently with younger children (the age at which the measures were administered at baseline), compared to older adolescents—the age at which the measures were administered in subsequent waves, especially the last two waves—in years 4 and 5 post intervention initiation. There may, also, be more comprehensive measurements which future studies can utilize to achieve optimal child mental health assessment. In addition, mental health may have been affected by unidentified factors such as life events, which were unaccounted for in this study. Furthermore, the study did not account for secondary outcomes related to functional impairment: for example, subjective well-being, satisfaction, quality of life, and activities of daily life. Capturing these outcomes in future studies will allow assessing functional impairment that can persist even after remission of the symptoms of depression.
Despite the limitations highlighted above, the findings of this study provide valuable insight into how family combination interventions based on economic strengthening coupled with financial management training and mentorship can benefit children’s mental health in resource-limited settings and how child poverty can potentially mediate the effect of these interventions on children’s mental health. However, further study on these mechanisms and others are necessary to inform the development of future intervention strategies and policy.
Table 1:
Baseline characteristics of sample
| VARIABLES | Control Group (n=496) | Treatment Arm 1 (n=402) | Treatment Arm 2 (n=512) | Total (n=l,410) |
|---|---|---|---|---|
| Child’s gender | ||||
| Male | 45 [40.4,49.6] | 43.3 [36.9,49.9] | 43.8 [39.8,47.8] | 44 [41.2,46.9] |
| Female | 55 [50.4,59.6] | 56.7 [50.1,63.1] | 56.3 [52.2,60.2] | 56 [53.1,58.8] |
| Child’s age (Range: 9–17) | 12.7 [12.6, 12.9] | 12.6 [12.4, 12.7] | 12.7 [12.6, 12.8] | 12.7 [12.6, 12.7] |
| Child’s orphanhood status | ||||
| Double orphan | 22.8 [19.9,26.0] | 15.9 [12.2,20.5] | 19.3 [15.2,24.3] | 19.6 [17.2,22.1] |
| Single orphan | 77.22 [74.04,80.11] | 84.08 [79.46,87.82] | 80.66 [75.68,84.83] | 80.43 [77.87,82.75] |
| MEDIATORS | ||||
| Child’s poverty (Range: 0–6) | 3.2 [2.96; 3.5] | 3.4 [3.1; 3.7] | 3.3 [3.1; 3.46] | 3.3 [3.2; 3.4] |
| Household wealth (Range: −3.5 – 2.5)(a) | 0.06 [−0.1; 0.2] | −0.07 [−0.3; 0.1] | −0.001 [−0.1; 0.1] | −3.03E-11 [−0.1; 0.1] |
| Child labor: frequency of working | ||||
| Never | 77.2 [72.9,81.0] | 76.6 [70.4,81.9] | 69.7 [65.4,73.7] | 74.3 [71.3,77.1] |
| Once in a while | 6.1 [3.5,10.4] | 5.7 [3.9,8.3] | 8.8 [6.6,11.6] | 7 [5.4,8.9] |
| Almost every week | 2 [1.2,3.5] | 2.5 [1.1,5.8] | 1.6 [0.8,3.0] | 2 [1.3,3.0] |
| Few days a week | 11.1 [8.9,13.8] | 9.2 [7.0,12.1] | 13.3 [9.9,17.5] | 11.4 [9.6,13.3] |
| Almost every day | 3.6 [2.3,5.7] | 6 [3.8,9.2] | 6.6 [4.9,9.0] | 5.4 [4.3,6.8] |
| OUTCOMES | ||||
| Depression (Range: 0–48) | 9.7 [9.1; 10.4] | 9.7 [9.1; 10.3] | 9.99 [9.3; 10.7] | 9.8 [9.4; 10.2] |
| Tennessee Self-Concept Scale (17–85) | 67 [66; 68] | 67.5 [66; 68.7] | 65.7 [64.5; 66.8] | 66.8 [66; 67.5] |
| Beck Hopelessness Scale (0–20) | 5.4 [5,5.7] | 5 [4.9,5.4] | 5.5 [5.1,5.9] | 5.4 [5.2,5.6] |
Boldface type indicates statistically significant results
p≤ 0.05,
p ≤ 0.01
p ≤ 0.001
We report adjusted Wald F-statistics (Design-based F) to examine individual-level variations while accounting for potential correlation between same-school observations
Household index is calculated by replicating the DHS method of using principal components analysis to assign the indicator weights. The following three steps were taken in calculating the index: first, the indicator variables (calculating z-scores) were standardized; second, the factor coefficient scores (factor loadings) were calculated; and third, the indicator values were multiplied by the loadings and summed to produce the household’s index value.
Acknowledgments
The study was funded by the National Institute of Child Health and Human Development (NICHD) and approved by Columbia University Institutional Review Board (AAAI1950) and the Uganda National Council for Science and Technology (SS2586). The study protocol is registered at Clinicaltrial.gov (ID# NCT01447615): https://clinicaltrials.gov/ct2/show/NCT01447615.The procedure for obtaining informed consent in this study was consistent with the approved IRB protocol.
REFERENCES
- 1.United Nations Children’s Fund & World Bank Group. Ending extreme poverty: A focus on children. New York: UNICEF;2016. [Google Scholar]
- 2.Dercon S, Krishnan P. Poverty and the psychosocial competencies of children: evidence from the young lives sample in four developing countries. Children Youth and Environments. 2009;19(2):138–163. [Google Scholar]
- 3.Reiss F Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Social science & medicine. 2013;90:24–31. [DOI] [PubMed] [Google Scholar]
- 4.International Labor Organization / International Program on the Elimination of Child Labor. Making progress against child labour: Global estimates and trends 2000–2012. Geneva: International Labour Organization;2013. [Google Scholar]
- 5.Sturrock S, Hodes M. Child labour in low-and middle-income countries and its consequences for mental health: a systematic literature review of epidemiologic studies. European child & adolescent psychiatry. 2016;25(12):1273–1286. [DOI] [PubMed] [Google Scholar]
- 6.Cluver L, Boyes M, Orkin M, Sherr L. Poverty, AIDS and child health: Identifying highest-risk children in South Africa. SAMJ: South African Medical Journal. 2013;103(12):910–915. [DOI] [PubMed] [Google Scholar]
- 7.Thurman TR, Kidman R, Nice J, Ikamari L. Family functioning and child behavioral problems in households affected by HIV and AIDS in Kenya. AIDS and Behavior. 2015;19(8):1408–1414. [DOI] [PubMed] [Google Scholar]
- 8.Case A, Paxson C, Ableidinger J. Orphans in Africa: Parental death, poverty, and school enrollment. Demography. 2004;41(3):483–508. [DOI] [PubMed] [Google Scholar]
- 9.De Hoop J, Rosati FC. Cash transfers and child labor. The World Bank Research Observer. 2014;29(2):202–234. [Google Scholar]
- 10.Atwine B, Cantor-Graae E, Bajunirwe F. Psychological distress among AIDS orphans in rural Uganda. Social science & medicine. 2005;61(3):555–564. [DOI] [PubMed] [Google Scholar]
- 11.Cluver LD, Orkin M, Gardner F, Boyes ME. Persisting mental health problems among AIDS-orphaned children in South Africa. Journal of Child Psychology and Psychiatry. 2012;53(4):363–370. [DOI] [PubMed] [Google Scholar]
- 12.Owusu-Addo E, Cross R. The impact of conditional cash transfers on child health in low-and middle-income countries: a systematic review. International journal of public health. 2014;59(4):609–618. [DOI] [PubMed] [Google Scholar]
- 13.Han C-K, Ssewamala FM, Wang JS-H. Family economic empowerment and mental health among AIDS-affected children living in AIDS-impacted communities: evidence from a randomised evaluation in southwestern Uganda. J Epidemiol Community Health. 2013;67(3):225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang JS FM; Neilands T; Bermudez LG; Garfinkel I; Waldfogel J; Brooks-Gunn J; You J. Effects of financial incentives on saving outcomes and material well-being: Evidence from a randomized controlled trial in Uganda. Journal of Policy Analysis & Managment. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sherraden M, Gilbert N. Assets and the poor: new American welfare policy. Routledge; 2016. [Google Scholar]
- 16.Huang J, Sherraden M, Kim Y, Clancy M. Effects of Child Development Accounts on early social-emotional development: An experimental test. JAMA pediatrics. 2014;168(3):265–271. [DOI] [PubMed] [Google Scholar]
- 17.Ssewamala FM, Karimli L, Torsten N, et al. Applying a family-level economic strengthening intervention to improve education and health-related outcomes of school-going AIDS-orphaned children: lessons from a randomized experiment in Southern Uganda. Prevention Science. 2016;17(1):134–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldman G Saving from poverty: A critical review of Individual Development Accounts. Critical Social Policy. 2018;38(2). [Google Scholar]
- 19.Richards KV, Thyer BA. Does Individual Development Account participation help the poor? A review. Research on Social Work Practice. 2011;21(3):348–362. [Google Scholar]
- 20.Karimli L, Ssewamala FM. Do savings mediate changes in adolescents’ future orientation and health-related outcomes? Findings from randomized experiment in Uganda. Journal of Adolescent Health. 2015;57(4):425–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ssewamala FM, Neilands TB, Waldfogel J, Ismayilova L. The impact of a comprehensive microfinance intervention on depression levels of AIDS-orphaned children in Uganda. Journal of Adolescent Health. 2012;50(4):346–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Traube D, Dukay V, Kaaya S, Reyes H, Mellins C. Cross-cultural adaptation of the Child Depression Inventory for use in Tanzania with children affected by HIV. Vulnerable children and youth studies. 2010;5(2):174–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wallis A, Dukay V. Learning how to measure the well-being of OVC in a maturing HIV/AIDS crisis. Journal of Health Care for the Poor and Underserved. 2009;20(4):170–184. [DOI] [PubMed] [Google Scholar]
- 24.Dozois DJ, Covin R. The Beck Depression Inventory-II (BDI-II), Beck Hopelessness Scale (BHS), and Beck Scale for Suicide Ideation (BSS). Comprehensive handbook of psychological assessment, Vol 2: Personality assessment. 2004. [Google Scholar]
- 25.Kovacs M The Children’s Depression Inventory (CDI): Technical Manual Update. . Toronto, ON: Multi-Health Systems;2003. [Google Scholar]
- 26.Fitts WH, Warren WL. Tennessee self-concept scale: TSCS-2. Western psychological services; Los Angeles; 1996. [Google Scholar]
- 27.Ssewamala FM, Han C-K, Neilands TB. Asset ownership and health and mental health functioning among AIDS-orphaned adolescents: Findings from a randomized clinical trial in rural Uganda. Social science & medicine. 2009;69(2):191–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Muthén LK, Muthén BO. Mplus User’s Guide: Eigth Edition. Los Angeles, CA: Muthén and Muthén; 1998-2017. [Google Scholar]
- 29.White H A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica: Journal of the Econometric Society. 1980;48:817–838. [Google Scholar]
- 30.Bollen KA, Long JS. Introduction In: Bollen KA, Long JS, eds. Testing Structural Equation Models. Newbury Park, CA: Sage Publications; 1993:1–9. [Google Scholar]
- 31.Bentler PM, Bonnett DG. Significance Tests and Goodness of Fit in the Analysis of Covariance Structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- 32.Browne MW, Cudek R. Alternative ways of assessing model fit In: Bollen KA, Long JS, eds. Testing Structural Equation Models. Newbury Park, CA: Sage Publications; 1993:136–162. [Google Scholar]
- 33.Kline RB. Principles and Practices of Structural Equation Modeling. 3rd ed New York, NY: Guilford Press; 2010. [Google Scholar]
- 34.Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 35.MacKinnon DP, Lockwood CM, Williams J. Confidence Limits for the Indirect Effect: Distribution of the Product and Resampling Methods. Multivariate Behavioral Research. 2004;39(1):99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ali G-C, Ryan G, De Silva MJ. Validated screening tools for common mental disorders in low and middle income countries: a systematic review. PloS one. 2016;11(6):e0156939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Haroz E, Ritchey M, Bass J, et al. How is depression experienced around the world? A systematic review of qualitative literature. Social Science & Medicine. 2017;183:151–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baird S, De Hoop J, Özler B. Income shocks and adolescent mental health. Journal of Human Resources. 2013;48(2):370–403. [Google Scholar]
- 39.Fernald LC, Gertler PJ, Neufeld LM. Role of cash in conditional cash transfer programmes for child health, growth, and development: an analysis of Mexico’s Oportunidades. The Lancet. 2008;371(9615):828–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paxson C, Schady N. Does money matter? The effects of cash transfers on child development in rural Ecuador. Economic development and cultural change. 2010;59(1):187–229. [DOI] [PubMed] [Google Scholar]
- 41.Cohen J Statistical power analysis for the behavioural sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 42.Evans GW, Cassells RC. Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clinical Psychological Science. 2014;2(3):287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Das-Munshi J, Lund C, Mathews C, Clark C, Rothon C, Stansfeld S. Mental health inequalities in adolescents growing up in post-apartheid South Africa: cross-sectional survey, SHaW Study. PloS one. 2016;11(5):e0154478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Delamonica EE, Minujin A. Incidence, depth and severity of children in poverty. Social Indicators Research. 2007;82(2):361–374. [Google Scholar]
- 45.United Nations Children’s Fund. Poverty reduction begins with children. New York: UNICEF;2000. [Google Scholar]