Abstract
The goals of the United Nation’s Millennium Summit for reducing maternal mortality have proven difficult to achieve. In Bolivia, where maternal mortality is twice the South American average, improving the diagnosis, treatment and ultimately prevention of preeclampsia is key for achieving targeted reductions. We held a workshop in La Paz, Bolivia to review recent revisions in the diagnosis and treatment of preeclampsia, barriers for their implementation, and means for overcoming them. While physicians are generally aware of current recommendations, substantial barriers exist for their implementation due to geographic factors increasing disease prevalence and limiting health-care access, cultural and economic factors affecting the care provided, and infrastructure deficits impeding diagnosis and treatment. Means for overcoming such barriers include changes in the culture of health care, use of standardized diagnostic protocols, the adoption of low-cost technologies for improving the diagnosis and referral of preeclamptic cases to specialized treatment centers, training programs to foster multidisciplinary team approaches, and efforts to enhance local research capacity. While challenging, the synergistic nature of current barriers for preeclampsia diagnosis and treatment also affords opportunities for making far-reaching improvements in maternal, infant and lifelong health.
Keywords: high altitude, infant mortality, maternal mortality, mobile health technologies
INTRODUCTION
Maternal mortality is an important index of the quality of life not only for mothers but all persons given women’s key role in family health. Despite the United Nations Millennium Summit’s goal for a 75% reduction by 2015, only a 44% fall was achieved (1).
Bolivian maternal mortality has consistently been more than twice the Latin American (currently 206 vs. 67 deaths, respectively, for women who die while pregnant or within 42 days of pregnancy termination per 100,000 births) (2, 3) and only decreased annually by 3.5%, half as much as recommended (4). Preeclampsia is the second leading cause of maternal death in Bolivia, next to postpartum hemorrhage (5–7) which frequently results from preeclampsia-associated coagulopathy. Infant mortality in Bolivia is also high, currently 35.3 deaths/1,000 livebirths and twice the South American, low- or middle-income country average (8). Preeclampsia is an important contributor since most deaths occur in babies born prematurely, which itself is often due to preeclampsia (9, 10). Preeclampsia also increases cardiovascular and other diseases later-in-life for both mother and child (11), and may therefore be a contributor to Bolivia’s high maternal cardiovascular mortality (12). For these reasons, improving the prevention, diagnosis and treatment of preeclampsia in Bolivia is critical.
We and leading Bolivian obstetricians or pediatricians at the three major maternity hospitals in La Paz and the neighboring city of El Alto and health-policy makers participated in a workshop in May 2018 entitled “Advances for Improving the Diagnosis, Treatments and Outcomes of Preeclampsia for Both Mother and Child”. Its purpose was to discuss recent revisions for preeclampsia diagnosis and treatment (see Table 1), the barriers for their implementation, and means for overcoming them. We summarize those discussions here with the hope that it will prove useful for improving maternal and infant health not only in Bolivia but also other low-resource settings.
Table 1:
American College of Obstetrics and Gynecology’s diagnostic guidelines (13)
| Blood pressure | ≥140 mmHg systolic or ≥90 mm Hg diastolic on 2 occasions ≥ 4 hours apart >20 wk in a previously normotensive woman, or ≥160 mmHg systolic or ≥110 mm Hg diastolic confirmed within a short interval (min). |
| And new onset of any of the following: | |
| Proteinuria | ≥300 mg protein 24-hr urine collection or this amount extrapolated from a timed collection, or Protein/creatinine ratio ≥0.3 (each measured as mg/dL), or Dipstick reading of 1+, which should be used only if other measures are not available. |
| Thrombocytopenia | Platelet count < 100,000/microliter. |
| Renal insufficiency | Serum creatinine > 1.1 mg/deciliter or a doubling of serum creatinine in the absence of other renal disease. |
| Impaired liver function | Twice normal blood concentrations of liver transaminases. |
| Pulmonary edema | Evidence of fluid accumulation in the lungs (pink sputum), difficulty breathing. |
| Cerebral or visual symptoms | Such as blurred vision, severe headache. |
BARRIERS FOR THE DIAGNOSIS OF PREECLAMPSIA IN BOLIVIA
Among such barriers are geographic challenges, late onset of prenatal care, limited health-care resources, and infrastructure deficits present in Bolivia.
Geographic challenges.
Two-thirds of Bolivians live at high altitude (7), conventionally defined as above 2500 m or 8250 ft, and one-third live in rural regions with limited transportation services. High altitude acts independently of other risk factors to slow fetal growth and reduce birth weight (14, 15). It also increases the incidence of hypertensive disorders of pregnancy, with perhaps as many as 20% of primiparous women being affected (5, 15–17) and, in turn, accounts for half the birth-weight reduction (16, 18). High altitude also exaggerates the rise in intrauterine mortality seen in pregnancies with hypertensive disorders (16).
Late onset or lack of prenatal care.
Traditional childbearing beliefs, geographic, and economic factors delay the onset of prenatal care and often result in home birth without the assistance of trained medical personnel (7, 19–22). Late onset of care limits the ability to detect women at high risk due to preeclampsia in a prior pregnancy or preexisting conditions (e.g., chronic hypertension, diabetes), as well as the physician’s ability to counsel their patients about diagnostic symptoms. As elaborated in Table 2, additional factors are the difficulty of travel to prenatal clinics or hospitals, all of which are in urban areas. Many rural Bolivians speak only indigenous languages (Aymara or Quechua), which impedes their ability to communicate with principally Spanish-speaking health-care personnel. Long wait times at urban clinics due, in turn, to limited health-care personnel and up to 1200 patients being seen/day (23) further discourage attendance.
Table 2.
The “Ruta Critica” or Perilous Pathway.
| Sra. Quispe woke up late at night, feeling unwell and decided to go to the clinic in the neighboring village. Since there were no public transportation services available and neither she norher husband could afford a taxi, she waited until morning. When she arrived, a room full of pregnant women and babies were waiting to be seen. She signed in with the receptionist, who scolded her for coming because it was not a regularly-scheduled visit. After several hours, a nurse measured her blood pressure as 140/90 mmHg. Since it was elevated, the nurse called the family medicine physician. He was busy seeing other patients so Sra. Quispe waited another hour. He confirmed her elevated blood pressure but could not test for proteinuria because the clinic wasnot authorized to do so or have the requisite dipsticks. The woman said she had blurred visionand pain on her right side, but neither the nurse nor the physician understood what she was saying asshe spoke only Aymara. They referred her to a level-two hospital for further evaluation. Two dayslater, after arranging for child care and a several hour bumpy bus ride, she arrived at the hospital. Herblood pressure was measured as 150/110 mm Hg so she was referred to a level-three hospital. She returned home and several days elapsed while she and her husband arranged for child care and transport. After another bumpy bus ride, she reached the level-three hospital, waited several hours tobe seen and then was admitted. A 24-hr urine was ordered that confirmed significant proteinuria, soshe was diagnosed with preeclampsia. She was asked by the physician via a translator if she had usedany traditional remedies, and then was scolded when she said that she had used herbs. No treatments were administered or other diagnostic tests performed. Four days after her due date (which was approximate since she had not had a mid-pregnancy ultrasound and the date of her lastmenstrual period was uncertain), she gave birth to a 1900 gm baby boy. He developed severe respiratory distress but could not be admitted to the neonatal intensive care unit because all bedswere occupied. He was given blow-by oxygen supplementation but died four days later. |
Limited health-care resources.
Health care in Bolivia is structured by the source of payment. Public (government-subsidized) programs provide free or low-cost prenatal, infant and child care (up to age five) as part of the “Seguro Integral de Salud” (comprehensive health-care system). Insured organizations, the largest being the Caja Nacional de Salud (national health-care fund), serve 20% of the population. Private-clinic services are compensated by personal insurance or self-pay.
Public and insured systems operate at three levels. The first, consisting of neighborhood clinics staffed by generalists and nursing personnel, provides all prenatal care through week 28. Outpatient clinics at second- or third-level hospitals provide prenatal care after week 28. All deliveries are performed at second- or third-level hospitals, with the former generally performing uncomplicated ones and the latter those with, but also without, pregnancy complications.
Health-care resources have improved in recent years, but persistent problems remain. Bolivia spends only half as much (6.3%) of its gross domestic product on health compared to the 14% Latin American average (24). There is only one hospital bed for every 1000 inhabitants nationally, and a total of 31 intensive care beds at the three largest women’s and infant’s hospitals (two of which are level-three facilities) serving the 2.8 million inhabitants of La Paz/El Alto (23, 24). Most physicians are generalists given that there are very few specialty programs and no board certification for recognizing specialists or ensuring standardization of care. Blood pressures are often measured by auxiliary nursing personnel who are not always fully trained in techniques for accurate measurement. There are no automated blood-pressure instruments at level-one clinics and very few at level-two or even level-three hospitals in La Paz/El Alto. Proteinuria is measured routinely only in timed or 24-hr collections at level-two or -three hospitals, and other diagnostic tests (i.e., platelet counts, serum creatinine, liver transaminases) are infrequently performed.
Infrastructure deficits
limit coordination of care even among clinics or hospitals within the same system. To illustrate this, workshop participants described the case history below.
In short, infrastructure deficits and a failure to appreciate the importance of teamwork resulted in delays in diagnosis and lack of treatment, which in this case would have been the administration of corticosteroids to hasten fetal lung development. Such deficits also impede surveillance of outcomes. For example, while Bolivia has a national birth and death database, there are few means for verifying the cause of death and ~40% of births occur at home where no birth data are recorded (7). Mandatory reporting of maternal or infant deaths is not required and, even if attempted, hampered by shortages of personnel or other health-care resources. As a result, there is little information available concerning the outcomes of preeclamptic pregnancies, and few means or incentives for sharing whatever treatment or outcome measures exist.
In summary, while many Bolivian physicians are aware of current recommendations for the diagnosis and treatment of preeclampsia (5–7), there are substantial barriers for their implementation due to geographic factors acting to increase prevalence and limit access to health care, cultural and economic factors affecting the timing and care provided, and infrastructure deficits impeding diagnosis and treatment. As a result, patients often arrive at level-three facilities with eclamptic seizures, subscapular hematoma or other life-threatening conditions (25).
MEANS TO OVERCOME THE BARRIERS IMPEDING PREECLAMPSIA DIAGNOSIS AND TREATMENT
While the above barriers are challenging, their synergistic nature also affords opportunities for far-reaching improvements in maternal, infant and lifelong health. Four means were identified: changes in the health-care culture, infrastructure improvements, new technologies, and enhancing local research capacity.
Changes in the health-care culture.
Evident during the workshop was a genuine desire and renewed commitment to resolve common problems in the public and insured health-care systems. Further, since physicians at public- or insured-hospitals often also have private practices, there is an opportunity to implement improvements across the full health-care spectrum. The health-care work force is becoming more inclusive with, for example, the percent of women entering Bolivia’s largest public medical school rising from 51 to 59% over the past 10 years (R. Amaru, personal communication). Women and persons from indigenous groups (e.g., Aymara, Quechua) are also more frequently occupying leadership positions in medical and other professions (26).
Infrastructure improvements.
Since 1989 Bolivia has had governmental programs to care for mothers and infants not otherwise being served. These were expanded in 2009 with the “Bono Juana Azurduy” (Juana Azurduy bonus, see Figure 1), which offers food subsidies to improve maternal nutrition; $7 US/prenatal visit, $17 US/hospital delivery, and $18 US/visit for up to 12 infant or child visits to encourage the use of medical facilities; and other incentives to encourage breast-feeding (21). However, while accessed by over 1.8 million women and children from 2009– 2017, this comprises only 30% and 20% of eligible women and babies, respectively (22). Hence expansion of governmental programs has not proven sufficient for improving health-care infrastructure.
Figure 1.
Sign in a rural, altiplano village encouraging women to enroll in the “Juana Azurduy” program, named for a heroine during Bolivia’s Chaco War, to assure that she has a safe delivery (along with the logos of various political parties or mayoral candidates).
Three ways to further improve health-care infrastructure were identified.
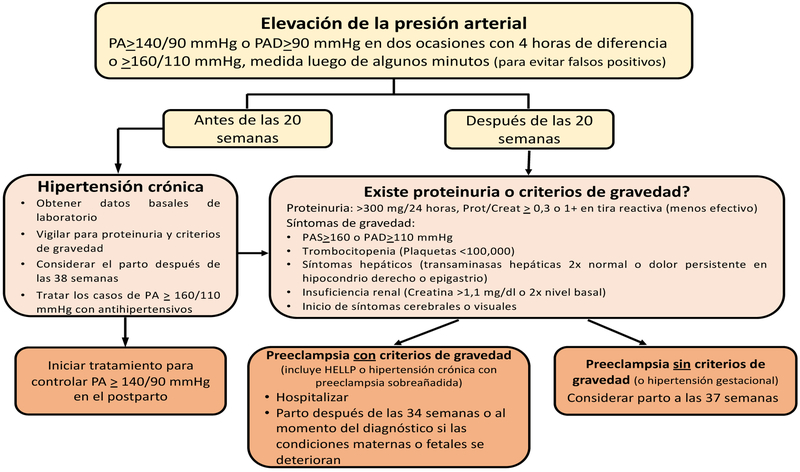
Standardized protocols. Workshop participants felt that simplified protocols such as that shown in Figure 2 would aid physicians and other health-care workers in adhering to the World Health Organization and American College of Obstetrics and Gynecology’s diagnostic and treatment guidelines (13, 27). Such adherence requires that proteinuria and other diagnostic symptoms be recorded at each prenatal visit at level one, two and three facilities. Benefits include the ability to identify women at increased risk due, for example, to chronic hypertension; treat other causes of proteinuria such as a urinary tract infection (and avoid its long-term sequelae); distinguish preeclampsia from other hypertensive disorders; identify women with the most severe, early-onset disease in time to treat; and, thus, be able to allocate scarce health-care resources to those at greatest mortality risk. Standardized diagnostic protocols would also facilitate data sharing between centers and conducting research on the factors contributing to the various pregnancy complications observed.
- New technologies have recently been developed that could improve preeclampsia diagnosis.
- The use of automated or semi-automated blood-pressure measuring devices designed for pregnancy application can improve accuracy, save time, reduce training requirements, hence help overcome personnel shortages and facilitate data-sharing between clinics or hospitals. Several hundred devices are on the market but not all have not been validated for use during pregnancy or are well suited to low-resource settings due to their expense or calibration requirements. Fortunately, efforts have been made to develop accurate, low-cost instruments that have been validated for use in pregnancy and preeclampsia in particular (28, 29).
- New urinary tests for proteinuria have become available that can help overcome the limitations of “spot” samples and the logistical challenges for making timed or 24-hr collections unless women are hospitalized. Since creatinine excretion is constant throughout the day, measuring both urinary protein and creatinine in a single sample allows extrapolating “spot” collections to 24-hr values. Fortunately, dipsticks have been developed and are being tested in low-resource settings that enable measuring both protein and creatinine in a single sample (30). Other urine-based tests are also being developed with potential for not only diagnosing preeclampsia but also assessing severity and the need for medically-indicated delivery (31).
- Smart phones or other mobile-technology devices are widely available in low- or middle-income countries, which creates opportunities for their use as effective surveillance tools, aids for clinical decision-making, and means for improving patient education. Even in remote settings, smart phones and tablets can be effective for increasing patient-provider communication in setting up appointments, educating patients about diagnostic symptoms, and reporting such symptoms to providers. They can also aid providers within a given health-care sector by relaying diagnostic symptoms for deciding when referral to a specialist is required (32), and thus help overcome the successive referrals and consequent time delays described in Table 2. The use of smart phones and tablets can also alleviate personnel shortages by improving the effectiveness of ancillary health-care workers in making clinical decisions or direct care with the aid of pre-programmed algorithms. Finally, smart phones or mobile devices could be uploaded with an electronic version of the Centro Latinoameriano de Perinatología (CLAP) form (33), and the data captured centrally so as to facilitate communication among the various levels of care and regular assessment of morbidity/mortality across systems for developing more targeted quality-improvement initiatives.
Training programs. Workshop participants were supportive of having regular, formalized training programs to update physicians and other health-care providers across the public-private spectrum. Such programs could demonstrate the benefits of and provide training for the use of standardized diagnostic protocols. One mechanism for doing so is a national system using continuing medical education and requiring attendance at a certain number of courses annually. Such programs could include work being done internationally to improve the diagnosis and treatment of pregnancy complications, and thereby benefit practitioners in low- to middle-income countries where the overwhelming majority of such complications occur (34). Training requirements should be reinforced by strengthening self-assessment programs within the medical community. This could be overseen by medical societies such as the Colegio Médico or the Sociedad Boliviana de Ginecología y Obstetricia. Such self-assessment should include a focus on medical failures such as deaths and “near misses” and be done at both the hospital and higher levels to look for commonalities in causation. Key for the success of such training programs is to foster a multidisciplinary, team approach. Therefore, training programs should include not only physicians, nurses and other direct-care providers but also hospital administrators, specialty society representatives, experts from social service agencies, and patient advocates operating at all levels of care within the public, insured, and private sectors. Such a multidisciplinary, team approach would help to provide feedback between referral and referring centers that could, in turn, strengthen the relationship between networks, help integrate resources, and prevent fragmentation of care.
Enhancing Local Research Capacity and Engagement would enable Bolivian health-care personnel to identify their own solutions for reducing maternal and infant mortality or morbidity. The May workshop was funded by a grant to CGJ and LGM as part of a broader NIH initiative to help build sustainable research capacity in low- to middle- income countries. This grant is also involving Bolivian and USA medical and public health students in a medical record study for documenting the diagnostic criteria and treatments in use before vs. after the workshop using Research Electronic Data Capture (RedCap) and the Global Pregnancy Collaboration (CoLab)’s online system COLLECT (35); such databases will be used for assessing the workshop’s efficacy but could also be used for future studies. Other efforts are being made to enhance local research capacity and engagement in low-resource settings that involve faculty exchanges and postgraduate programs for stimulating South American research and scientific output (36). For Bolivia, a pressing need is to distinguish the incidence of preeclampsia from other hypertensive complications, and their relationships to neonatal outcomes and disease prevalence later in life for both mother and child. Major benefits could accrue by using drugs already approved for prevention or delay in the onset of preeclampsia, such as low-dose aspirin or calcium supplementation (27), and thereby have major effects for improving health outcomes. Finally, such efforts could help pay for themselves by reducing the number of preterm deliveries, their attendant high costs, and hence enable such funds to be used for new therapeutic or preventive initiatives.
Figure 2.
Flow chart for diagnosing preeclampsia, translated into Spanish from that used for diagnosing preeclampsia at University of Colorado Hospital according to ACOG recommendations (13) (A. Euser, personal communication).
In conclusion, maternal mortality in Bolivia is the highest in Latin America and preeclampsia is one of its major causes; therefore, improving the diagnosis, treatment and prevention of preeclampsia is critical. Current barriers impeding its diagnosis and treatment can be overcome with the use of low-cost technologies, standardized diagnostic protocols, training programs to foster multidisciplinary team approaches, and efforts to enhance local research capacity which, in turn, could significantly reduce maternal as well as infant mortality.
HIGHLIGHTS.
Bolivia has consistently had the highest maternal mortality in Latin America.
Preeclampsia is the 2nd leading cause of maternal death in Bolivia and an important contributor to the leading cause, postpartum hemorrhage, underscoring the need for improving preeclampsia’s diagnosis and treatment for achieving a meaningful reduction in maternal mortality.
While current guidelines for preeclampsia diagnosis and treatment are generally known in Bolivia, there are substantial barriers for their implementation due to geographic factors, cultural and economic considerations affecting the timing and care provided, and infrastructure deficits impeding diagnosis and treatment.
Such barriers can be overcome with the use of low-cost technologies for monitoring diagnostic symptoms, implementing standardized diagnostic protocols, undertaking training programs to foster multidisciplinary team approaches and effective self-assessment, and enhancing local research capacity.
ACKNOWLEDGEMENTS
Workshop direct costs were provided by NIH grant R21 TW010797 funded through the NIH Global Noncommunicable Diseases and Injury Across the Lifespan: Exploratory Research Initiative. In addition to the authors, the workshop participants were Ángel Alcázar, Yuri Pérez, Daniel Cárdenas, Víctor Paniagua, Ronald Vargas, Marisol Yucra (Hospital de la Mujer); German Arcienaga, Patricia Asturizaga, Abraham Badner, José Luis Barriga, Richard Gómez, Carlos Loayza, Rosario Ruiz (Hospital Materno Infantil); Lidia Durán, Manfredo Vargas, Lina Velasco (Hospital Boliviano Holandés); Giomar Higueras (Programa de Coordinación en Salud Integral); Gonzalo Aramayo (Sociedad de Obstetricia – Filial La Paz); Luis Buscarons (Inter-American Development Bank). We thank all workshop participants, Ricardo Amaru and Anna Euser for the information about the barriers described here and their potential resolution.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DECLARATION OF INTERESTS
We declare no competing interests.
REFERENCES CITED
- 1.Alkema L, Chou D, Hogan D, Zhang S, Moller AB, Gemmill A, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. Lancet. 2016;387(10017):462–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kassebaum NJ, Bertozzi-Villa A, Coggeshall MS, Shackelford KA, Steiner C, Heuton KR, et al. Global, regional, and national levels and causes of maternal mortality during 1990– 2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9947):980–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roser M Maternal Mortality: Our World in Data; 2019. [Available from:https://ourworldindata.org/maternal-mortality.
- 4.WHO, UNICEF, UNFPA, Group WB, Division UNP. Trends in Maternal Mortality: 1990 to 2015. Geneva, Switzerland: World Health Organization; 2015. [Google Scholar]
- 5.de la Gálvez Murillo A. Atención obstétrica y complicaciones del embarazo y parto en Bolivia. Cuadernos Hospital de Clínicas. 2009;54(100–107). [Google Scholar]
- 6.Roost M, Altamirano VC, Liljestrand J, Essen B. Priorities in emergency obstetric care in Bolivia--maternal mortality and near-miss morbidity in metropolitan La Paz. BJOG : an international journal of obstetrics and gynaecology. 2009;116(9):1210–7. [DOI] [PubMed] [Google Scholar]
- 7.Campero Nava A, Parada Barba C, Mamani Huallpa G, Rios Vacaflor M, Flores Velasco O, Enriquez Nava M. Estudio Nacional de Mortalidad Materna 2011 Bolivia: resumen ejecutivo. In: Md Salud, editor. La Paz, BO: Ministerio de Salud; 2016. p. 1–98. [Google Scholar]
- 8.IndexMundi. [Available from: https://www.indexmundi.com/bolivia/infant_mortality_rate.html.
- 9.UNICEF. [Available from: https://data.unicef.org/topic/child-survival/under-five-mortality/.
- 10.Vogel JP, Lee AC, Souza JP. Maternal morbidity and preterm birth in 22 low- and middle-income countries: a secondary analysis of the WHO Global Survey dataset. BMC Pregnancy Childbirth. 2014;14:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roberts JM, Hubel CA. Pregnancy: a screening test for later life cardiovascular disease. Womens Health Issues. 2010;20(5):304–7. [DOI] [PubMed] [Google Scholar]
- 12.Bank W Trends in Maternal Mortality: 1990–2015. Estimates Developed by WHO, UNICEF, UNFPA and the World Bank; 2018. [Available from: https://datos.bancomundial.org/indicator/SH.MMR.DTHS?end=2015&locations=ZJ-BO&start=2015&view=bar. [Google Scholar]
- 13.ACOG. Hypertension in pregnancy. Obstet Gynecol. 2013;122(5):1122–31. [DOI] [PubMed] [Google Scholar]
- 14.Moore LG. Measuring high-altitude adaptation. Journal of applied physiology.2017;123:1371–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jensen GM, Moore LG. The effect of high altitude and other risk factors on birthweight: independent or interactive effects? Am J Public Health. 1997;87(6):1003–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keyes LE, Armaza JF, Niermeyer S, Vargas E, Young DA, Moore LG. Intrauterine growth restriction, preeclampsia, and intrauterine mortality at high altitude in Bolivia. Pediatr Res. 2003;54(1):20–5. [DOI] [PubMed] [Google Scholar]
- 17.Giachini FR, Galaviz-Hernandez C, Damiano AE, Viana M, Cadavid A, Asturizaga P, et al. Vascular Dysfunction in Mother and Offspring During Preeclampsia: Contributions from Latin-American Countries. Curr Hypertens Rep. 2017;19(10):83. [DOI] [PubMed] [Google Scholar]
- 18.Bujold E, Roberge S, Lacasse Y, Bureau M, Audibert F, Marcoux S, et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116(2 Pt 1):402–14. [DOI] [PubMed] [Google Scholar]
- 19.Heath A Embarazo y parto entre los indígenas Aymaras en Bolivia. Tropenmedizin. 15(98): Curare Sonderband 1997. p. 243–56. [Google Scholar]
- 20.ENDSA INdE-. Encuesta Nacional de Demografía y Salud - ENDSA 2008. Calverton, MD: MEASURE DHS, Macro International; 2009. p. 1–453. [Google Scholar]
- 21.Md Salud. Bono Juana Azurduy: una oportunidad para la vida 2018. [Available from: www.bja.gob.bo/.
- 22.Md Mundo. Bolivia 2016. [Available from: https://www.medicosdelmundo.org/que-hacemos/america/bolivia.
- 23.Yupanqui Márquez RM. Anuario Estadistico Hospitalario. In: Paz UdSVSL, editor. La Paz, BO: 2016. p. 1–35. [Google Scholar]
- 24.Tudela Canaviri M Los hospitales de la salud pública: pobres pero eficientes. Fundación para el Periodismo; 2017. [Google Scholar]
- 25.Morbilidad Obstétrica Grave Más Frecuente en Bolivia: Guia de bolsillo para su diagnóstico y tratamiento. La Paz, BO: Ministerio de Salud y Deportes; 2013. p. 116. [Google Scholar]
- 26.Monitor CS. Cholita Power in Bolivia 2018. [Available from: https://www.csmonitor.com/Photo-Galleries/In-Pictures/CHOLITA-POWER-IN-BOLIVIA.
- 27.WHO Recommendations for Prevention and Treatment of Pre-Eclampsia and Eclampsia. WHO Guidelines Approved by the Guidelines Review Committee; Geneva 2011. [Google Scholar]
- 28.Nathan HL, de Greeff A, Hezelgrave NL, Chappell LC, Shennan AH. An accurate semiautomated oscillometric blood pressure device for use in pregnancy (including pre-eclampsia) in a low-income and middle-income country population: the Microlife 3AS1–2. Blood Press Monit. 2015;20(1):52–5. [DOI] [PubMed] [Google Scholar]
- 29.Nathan HL, Boene H, Munguambe K, Sevene E, Akeju D, Adetoro OO, et al. The CRADLE vital signs alert: qualitative evaluation of a novel device designed for use in pregnancy by healthcare workers in low-resource settings. Reprod Health. 2018;15(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zwisler G, Lee A, Gerth-Guyette E, Leader BT. 7 A new, low-cost protein-to-creatinine strip dipstick to improve proteinuria screening for preeclampsia: Preeclampsia in low and middle income countri. Pregnancy Hypertension. 2016;6(3):181. [Google Scholar]
- 31.Millen KR, Buhimschi CS, Zhao G, Rood KM, Tabbah S, Buhimschi IA. Serum and Urine Thioflavin-T-Enhanced Fluorescence in Severe Preeclampsia. Hypertension. 2018;71(6):1185–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White A, Thomas DS, Ezeanochie N, Bull S. Health Worker mHealth Utilization: A Systematic Review. Comput Inform Nurs. 2016;34(5):206–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Organization PAH. SIP consolidates in Bolivian hospitals 2018. [Available from: https://www.paho.org/clap/index.php?option=com_content&view=article&id=390:el-sip-se-consolida-en-los-centros-hospitalarios-de-bolivia&Itemid=354&lang=en.
- 34.Nathan HL, Seed PT, Hezelgrave NL, De Greeff A, Lawley E, Anthony J, et al. Early warning system hypertension thresholds to predict adverse outcomes in pre-eclampsia: A prospective cohort study. Pregnancy Hypertens. 2018;12:183–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Myatt L, Roberts JM, Redman CWG, Global Pregnancy C. Availability of COLLECT, a database for pregnancy and placental research studies worldwide. Placenta. 2017;57:223–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Noorden R The impact gap: South America by the numbers. Nature. 2014;510(7504):202–3. [DOI] [PubMed] [Google Scholar]