Abstract
We anticipated that bilateral Erector spinae plane (ESP) block, which was applied in 10 patients starting from lower thoracic levels (T9) might provide effective postoperative analgesia in open abdominal hysterectomies. In addition, we aimed to obtain anatomic observation of the local anaesthetic (LA) spread in the ESP block by injecting methylene blue on 4 cadavers. All the patients had excellent pain relief. There was an extensive spread to the erector spinae muscle (ESM) involving several segmental levels on cadavers. We observed the spread of dye on the ventral and dorsal rami in the paravertebral space and as an additional finding, the dye had extended to the canal vertebralis. There was a spread of dye on the dura mater. ESP block can be used with new indications and it is an effective technique for major abdominal surgery when is applied to the lower vertebral levels. Randomized controlled trials are required to explore the clinical implications of our findings.
Keywords: ultrasound, erector spinae plane block, hysterectomy, postoperative pain, cadaver study
Introduction
Thoracic epidural analgesia is still considered the gold standard for postoperative analgesia in major open abdominal surgery [1]. However, there are side effects such as hypotension and motor blockade, as well as a risk of major complications such as epidural hematoma and abscess, which have led some to question its role [2, 3]. An alternative to epidural analgesia that is often used after open abdominal surgery is ultrasound-guided Transversus Abdominis Plane (TAP) block [4–6]. Unlike epidurals, TAP and other truncal blocks can be safely used in anticoagulated patients.
TAP block is easily performed and entails the deposition of local anaesthetic (LA) between the transversus abdominis and internal oblique muscle planes. TAP block decreases postoperative pain and opioid consumption [7]. However, the greatest disadvantage of TAP block is the limited spread of LA spread and the minimal or completely lack of visceral pain relief [6]. The quadratus lumborum block is an alternative abdominal wall block. Clinical studies support its analgesic efficacy in lower-segment abdominal surgery, but imaging the area of the quadratus lumborum muscle can be very difficult in obese patients [8]. The erector spinae plane (ESP) block was first described by Forero et al. [9] in 2016 for chronic and post-operative thoracic pain.
Bilateral ESP block is applied from the lower thoracic levels when considering the existing anatomical structures. In our case series, we anticipated that this block may provide effective analgesia in hysterectomies, and we aimed to investigate its effects on postoperative pain. In addition, we aimed to obtain anatomic observations of the LA spread in the block made from the lower thoracic levels of cadavers using methylene blue. Thus, we aimed to obtain information about the distribution of the anaesthetic agent based on the staining of the muscle and nerve tissues passing through the fascial spaces.
Case reports
Written informed consent was obtained from all the patients examined in this report. All patients had undergone an open abdominal hysterectomy. There were 10 patients, and all of them were in the ASA I-II risk group. The patients’ age, height, and body mass index were 44 ± 6.8 years, 162.9 ± 5.2 cm, and 32.25 ± 6.34 kg/m2, respectively (Table 1). The routine monitoring included ECG, noninvasive blood pressure, pulse oximetry (SpO2), and body temperature. Surgery was performed under general anaesthesia, which was induced with intravenous (i.v.) propofol (2 mg/kg), fentanyl (50 μg), and rocuronium (50 mg). Anaesthesia was maintained with desflurane in an oxygen-air mixture, and a total of 5 mg of i.v. morphine was administered for additional intraoperative analgesia. Furthermore, 100 mg of tramadol was administered 15 minutes before the end of the surgery. The surgery time was 2 hours on average.
Table 1.
Patients’ demographic data
| Patient | Age (year) | Height (cm) | Weight (kg) | BMI (kg/m2) |
|---|---|---|---|---|
| 1 | 46 | 165 | 85 | 31.25 |
| 2 | 42 | 156 | 64 | 26.33 |
| 3 | 53 | 159 | 77 | 30.50 |
| 4 | 33 | 170 | 108 | 37.37 |
| 5 | 32 | 164 | 52 | 19.40 |
| 6 | 43 | 160 | 96 | 37.50 |
| 7 | 47 | 158 | 68 | 27.30 |
| 8 | 49 | 172 | 118 | 40 |
| 9 | 50 | 160 | 89 | 34.76 |
| 10 | 45 | 165 | 100 | 36.76 |
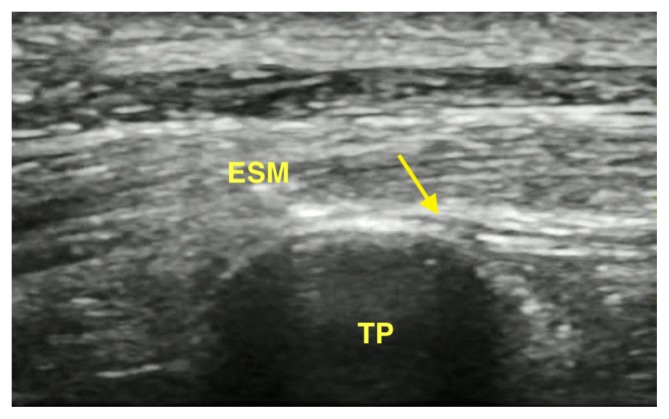
An ultrasound-guided ESP block was performed bilaterally in the lateral position on 10 patients before extubation. The ESP block was performed using a high-frequency linear ultrasound transducer. The transducer was placed in a longitudinal orientation 3 cm lateral to the T9 spinous process. A hyperechoic shadow of the transverse process and erector spinae was defined. An in-plane approach was used with a 21-gauge 100-mm atraumatic needle for peripheral nerve blocks (Stimuplex® A Insulated Needle, B.Braun, Melsungen, Germany). The needle was inserted in the cephalad-to-caudad direction through the ESM to gently contact the T9 transverse process. When the appropriate needle tip location was confirmed, 15 ml of 0.25% bupivacaine was injected as LA on each side. Sonographic confirmation of the LA spread was observed as an anechoic shadow in the paravertebral spaces from T7 to T12.
At the recovery unit, the patients’ numeric rating scale (NRS 0–10) was evaluated at rest and when coughing postoperatively at 0, 6, 12, 24 hours. At the 15th minute after extubation, a pinprick test showed that cutaneous sensory loss was among the T7-L1 dermtomes. Rescue analgesia was planned in the form of 75 mg of intramuscular diclofenac sodium (NRS > 4/10). The patients were routinely given 1 g of paracetamol i.v. every 8 hours. Rescue analgesia consisted of diclofenac 75 mg i.m., but none of patients required rescue analgesia (NRS scores at rest and with movement were between 0–4 / not NRS > 4/10) (Table 2–3). There were no complications. The patients were discharged in 48 hours.
Table 2.
Numeric rating scale (NRS) of patients at rest
| Patient | NRS0 | NRS6 | NRS12 | NRS24 |
|---|---|---|---|---|
| 1 | 1 | 1 | 2 | 2 |
| 2 | 0 | 2 | 2 | 3 |
| 3 | 1 | 2 | 1 | 1 |
| 4 | 1 | 4 | 2 | 2 |
| 5 | 0 | 2 | 2 | 2 |
| 6 | 1 | 3 | 3 | 3 |
| 7 | 1 | 1 | 2 | 3 |
| 8 | 0 | 2 | 2 | 2 |
| 9 | 0 | 4 | 2 | 2 |
| 10 | 1 | 1 | 1 | 1 |
Table 3.
Numeric rating scale (NRS) of patients with movement
| Patient | NRS0 | NRS6 | NRS12 | NRS24 |
|---|---|---|---|---|
| 1 | 2 | 4 | 3 | 3 |
| 2 | 1 | 3 | 3 | 3 |
| 3 | 2 | 2 | 2 | 2 |
| 4 | 3 | 4 | 3 | 3 |
| 5 | 2 | 3 | 3 | 2 |
| 6 | 1 | 3 | 2 | 3 |
| 7 | 2 | 3 | 3 | 3 |
| 8 | 2 | 2 | 2 | 2 |
| 9 | 3 | 4 | 3 | 3 |
| 10 | 1 | 2 | 3 | 3 |
The cadavereric investigation
We also wanted to confirm our clinical findings with a cadaver study. In the anatomy laboratory, we performed ESP blocks bilaterally on 4 cadavers at the T9 transversus process level with the same technique using ultrasound guidance (a total of 8 injections were performed on 4 non-fresh cadavers; Fig. 1). 20 ml of methylene blue was injected into each side. Table 4 shows the full extent of dye spread in the planes deep into the ESMs, ventral ramus, dorsal ramus, ganglion spinale, and dura mater (n: number of stained cadavers’ sides, %: percentage of the number of stained cadavers’ sides at the vertebral levels at Table 4).
Fig. 1.
Pre-injection longitudinal parasagittal view of the tip of the T9 transverse process (TP) and erector spinae muscle (ESM), linear pattern of dye spread (arrow)
Table 4.
Spread of dye to muscles and nerves on 4 non-fresh cadavers
| vertebra level | latissumus dorsi | spinalis | longissimus | iliocostalis | levator costarum | rhomboid major | dorsal rami | ventral rami | ganglion spinale | dura mater | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n* | %* | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| T1 | ||||||||||||||||||||
| T2 | ||||||||||||||||||||
| T3 | 2 | 25 | 2 | 25 | 1 | 12,5 | ||||||||||||||
| T4 | 2 | 25 | 4 | 50 | 1 | 12,5 | 1 | 12,5 | ||||||||||||
| T5 | 3 | 37,5 | 5 | 62,5 | 1 | 12,5 | 1 | 12,5 | 3 | 37,5 | 1 | 12,5 | ||||||||
| T6 | 4 | 50 | 7 | 87,5 | 2 | 25 | 3 | 37,5 | 3 | 37,5 | 2 | 25 | ||||||||
| T7 | 2 | 25 | 5 | 62,5 | 8 | 100 | 4 | 50 | 6 | 75 | 5 | 62,5 | ||||||||
| T8 | 4 | 50 | 5 | 62,5 | 8 | 100 | 4 | 50 | 7 | 87,5 | 7 | 87,5 | 2 | 25 | 3 | 37,5 | 2 | 25 | ||
| T9 | 7 | 87,5 | 8 | 100 | 8 | 100 | 5 | 62,5 | 8 | 100 | 8 | 100 | 6 | 75 | 5 | 62,5 | 5 | 62,5 | ||
| T10 | 7 | 87,5 | 8 | 100 | 8 | 100 | 4 | 50 | 6 | 75 | 6 | 75 | 5 | 62,5 | 1 | 12,5 | ||||
| T11 | 4 | 50 | 3 | 37,5 | 7 | 87,5 | 3 | 37,5 | 2 | 25 | 5 | 62,5 | 3 | 37,5 | ||||||
| T12 | 3 | 37,5 | 3 | 37,5 | 6 | 75 | 3 | 37,5 | 3 | 37,5 | ||||||||||
| L1 | 2 | 25 | 2 | 25 | 4 | 50 | 2 | 25 | ||||||||||||
| L2 | 2 | 25 | 3 | 37,5 | 1 | 12,5 | ||||||||||||||
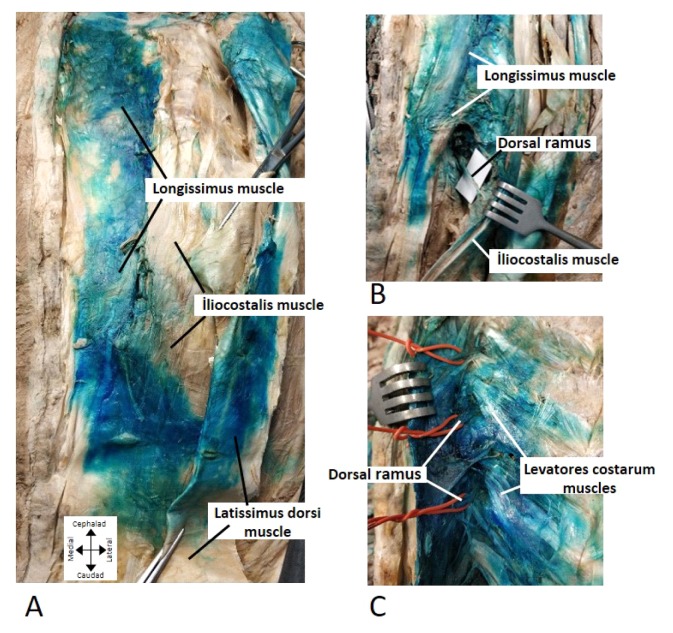
The cephalocaudad spread of the dye was usually over many segments. For example, in the region of the T3-L1 vertebrae, the dye spread to the spinalis muscles in 25 to 100% of the 8 injections, and in the region of T3-L2, the dye spread to the longissimus in 25 to 100% of the total injections. At the T4-L2 levels, the dye was in the iliocostalis muscles in 12.5 to 62.5% of the injections. At the T3–T6 levels, the dye spread to the rhomboid major muscles in 12.5 to 37.5% of the injections. At the T5-T11 levels, the dye also spread to the levator costarum muscles in 12.5 to 100% of the injections (Table 4 and Fig. 2A, Fig. 2B, Fig. 2C). The dye spread in the region of T7-L1 in the vertebrae in 25 to 87.5% of the injections, and there was dye at or around the latissimus dorsi muscles.
Fig. 2.
Cadaveric image. A: Latissumus dorsi muscle dissected and deviated Spread of dye on the longissimus muscle, iliocostalis muscle and spinalis muscle. B: Spread of dye on the dorsal ramus of spinal nerve between the longissimus muscle and iliocostalis muscle. C: Spread of dye on the dorsal ramus of the spinal nerve and levatores costarum muscles
Dissection showed that methylene blue spread through the costo-transverse foramen and stained the dorsal rami at different levels. At T5–T12 level, the dye spread to the dorsal rami in 12.5 to 100% of the total injections (Table 4, Fig. 2B, Fig. 2C).
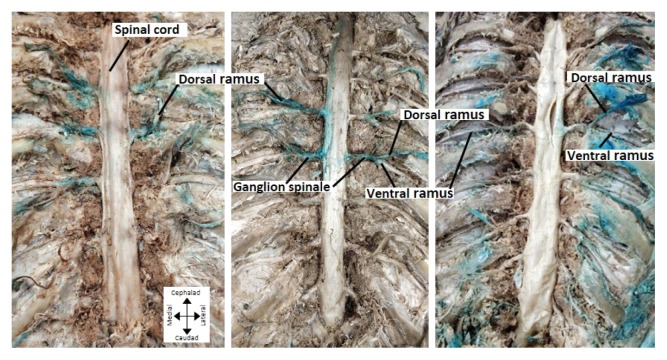
The dye also spread to the ventral rami in 25 to 75% of the injections at level T8–T11. At the T8–T10 levels, the dye spread through the costo-transverse foramen and onto the ganglion spinale in 12.5 to 62.5% of the injections (Table 4, Fig. 2B, Fig. 2C, Fig. 3A, Fig. 3B, Fig. 3C).
Fig. 3.
Cadaveric image A-B: Spread of dye on the dorsal ramus of spinal nerve and some of the ventral ramus of spinal nerve. C: Spread of dye on ganglion spinales with ventral and dorsal rami and extended to the dura mater
Furthermore, the methylene blue spread inside of the foramen intervertabralis and extended to the canal vertebralis at the T9 level. The methylene blue stained the dural spinal cord spanning the medulla spinal along the radix posterior at the same level (epidural space). Moreover, the subdural space was also a little stained (Table 4, Fig. 3C, Fig. 4).
Fig. 4.
Spread of the dye on the dura mater at T9 levels
Discussion
ESP block was first described by Forero et al [9] in 2016 for chronic and post-operative thoracic pain. According to more recent reports, the ESP block can also be used to provide analgesia for laparoscopic abdominal surgery by injection at a lower thoracic level of T7–T9 [8, 10]. There are numerous possible theories regarding the mechanism of the ESP block. According to Forero et al [9], it is possible that the sufficient resolution of thoracic pain might be due to both the dorsal and ventral rami of the spinal nerves emerging in close proximity to the costotransverse foramen. Furthermore, the LA spread might be eased by the thoracolumbar fascia. The distribution of the LA spread is unclear when injected deep into the ESM. We performed post-injection ultrasound, which revealed an anechoic shadow in T7 to T12, and the pinprick test showed that cutaneous sensory loss was among the T7-L1 dermatomes. There may be differences in pain sensitivity between patients. In our cases, patients described mild to moderate pain during 6 hours post-operation, particularly in the pubic region. They also complained about the Foley catheter. However, the patients were under pain control and seemed comfortable. Furthermore, the NRS may not be always correlate with objective pain [11].
In our cadaver investigation, we performed the ESP block bilaterally on 4 non-fresh cadavers with 20 mL of methylene blue at the T9 level. We preferred to use 20 mL of dye because our cadavers were not fresh, and in the case of living patients, the spread of LA may be affected by intrathoracic pressure changes; postmortem changes in the integrity, permeability, and tension of tissues; the positioning of the patient; and gravitational effects [12]. There was extensive spread to the ESM involving several segmental levels (Table 4).
In contrast to Ivanusic et al. [12], we observed the spread of dye into the paravertebral spaces. The ventral and dorsal rami in the paravertebral space were dyed. This result correlated with our clinical findings. Our first anticipation was the dyeing of the ganglion spinales, but as an additional finding, we observed that the dye had spread inside of the foramen intervertebralis and extended to the canal vertebralis. The dye had also spread to the duramater (Table 4, Fig. 2B, Fig. 2C, Fig. 3A, Fig. 3B, Fig. 3C). This finding raises new questions to answer for future work.
In our cases, we might have chosen epidural analgesia, but the side effects include hypotension, persistent neurological deficit, motor blockade, kinking or knotting while inserting the catheter and entrapment by ligaments, accidental placement of the epidural catheter into the pleural space, and a risk of major complications, such as epidural hematoma and abscess [2, 3, 13]. These factors may limit the use of epidural analgesia in all patients. Furthermore, some studies have reported incidences between 1:800 and 1:85 000 for an epidural abscess, as well as a rate of 1.3 to 18:10 000 for a cardiac arrest [13]. Compared to epidural analgesia, ESP block can be considered easier to perform and safer because the needle remains in the bone structure. Similar to the findings of Adhikary et al. [14] we observed the spread of dye to the neural foramina and epidural space. As Adhikary et al. [14] noted, the occurrence of epidural spread raises the possibility of symptomatic hypotension, but the incidence is unlikely to exceed that observed with thoracic paravertebral blockade.
Compared to epidural analgesia, the greatest disadvantage of the TAP block is the limited LA spread and minimal or complete lack of visceral pain relief [15]. ESP block is a peri-paravertebral block that affects both visceral and somatic pain fibers [10]. The use of the ESP block for postoperative analgesia is increasing incrementally [10, 16]. In our cadaver study, we showed that dye spread to the ventral/dorsal rami and ganglion spinales. This may show that the technique provides effective analgesia at the visceral and somatic pain fibers. We also confirmed our findings in live cases of open abdominal hysterectomy surgery. This was also done to document the extent of associated sensory block and analgesia. However, there is a need for prospective randomized controlled trials and comparison trials with other regional anesthesia techniques.
The quadratus lumborum block is an alternative abdominal wall block. Clinical studies support its analgesic efficacy in lower-segment abdominal surgery, but imaging the area of the quadratus lumborum muscle can be very difficult in obese patients [8]. The ESP block is a safe technique because the neuraxis is protected by the bone structure. However, the safety profile of the ESP block cannot be confirmed with case reports, and further investigations regarding its efficacy and safety are required.
Conclusion
Bilateral postoperative ultrasound-guided ESP block can result in a good sensory blockade and visceral analgesia after an open abdominal hysterectomy. We have demonstrated extensive craniocaudal and medial-to-lateral spread to the ESM involving several segmental levels. The dye spread to the ventral and dorsal rami in the paravertebral space, which correlated with our clinical findings. Furthermore, the methylene blue spread inside of the foramen intervertabralis and extended to the canal vertebralis at the T9 level. The methylene blue stained the dural spinal cord spanning the medulla spinal along the radix posterior at the same level (epidural space). Moreover, the subdural space was also a little stained. Randomized controlled trials are required to explore the clinical implications of our findings.
Footnotes
Conflict of interest
Nothing to declare
References
- 1.Guay JL, Nishimori M, Kopp SL. Epidural local anaesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting and pain after abdominal surgery. Cochrane Database Syst Rev. 2016;7:CD001893. doi: 10.1002/14651858.CD001893.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chilvers CR, Nguyen MH, Robertson IK. Changing from epidural to multimodal analgesia for colorectal laparotomy: an audit. Anaesth Intensive Care. 2007;35:230–238. doi: 10.1177/0310057X0703500213. [DOI] [PubMed] [Google Scholar]
- 3.Rawal N. Epidural technique for postoperative pain: gold standard no more? Reg Anesth Pain Med. 2012;37:310–317. doi: 10.1097/AAP.0b013e31825735c6. [DOI] [PubMed] [Google Scholar]
- 4.Abrahams MS, Horn JL, Noles LM, Aziz MF. Evidence-based medicine: ultrasound guidance for truncal blocks. Reg Anesth Pain Med. 2010;35:36–42. doi: 10.1097/AAP.0b013e3181d32841. [DOI] [PubMed] [Google Scholar]
- 5.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–1026. doi: 10.1111/j.1365-2044.2001.2279-40.x. [DOI] [PubMed] [Google Scholar]
- 6.Hebbard PD. Transversalis fascia plane block, a novel ultrasound-guided abdominal wall nerve block. Can J Anaesth. 2009;56:618–620. doi: 10.1007/s12630-009-9110-1. [DOI] [PubMed] [Google Scholar]
- 7.McDonnell JG, O’Donnell B, Curley G, Heffernan A, Power C, Laffey JG. The analgesic efficacy of transversus abdominus plane block after abdominal surgery; a prospective randomized controlled trial. Anesth Analg. 2007;104:193–197. doi: 10.1213/01.ane.0000250223.49963.0f. [DOI] [PubMed] [Google Scholar]
- 8.Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med. 2017;42:372–376. doi: 10.1097/AAP.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 9.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–627. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 10.Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–460. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
- 11.Younger J, McCue R, Mackey S. Pain outcomes: a brief review of instruments and techniques. Curr Pain Headache Rep. 2009;13:39–43. doi: 10.1007/s11916-009-0009-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ivanusic J, Konishi Y, Barrington MJ. A Cadaveric Study Investigating the Mechanism of Action of Erector Spinae Blockade. Reg Anesth Pain Med. 2018;43:567–571. doi: 10.1097/AAP.0000000000000789. [DOI] [PubMed] [Google Scholar]
- 13.von Hösslin T, Imboden P, Lüthi A, Rozanski MJ, Schnider TW, Filipovic M. Adverse events of postoperative thoracic epidural analgesia: A retrospective analysis of 7273 cases in a tertiary care teaching hospital. Eur J Anaesthesiol. 2016;33:708–714. doi: 10.1097/EJA.0000000000000446. [DOI] [PubMed] [Google Scholar]
- 14.Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector Spinae Plane Block Versus Retrolaminar Block: A Magnetic Resonance Imaging and Anatomical Study. Reg Anesth Pain Med. 2018;43:756–762. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 15.Hebbard PD. Transversalis fascia plane block, a novel ultrasound-guided abdominal wall nerve block. Can J Anaesth. 2009;56:618–620. doi: 10.1007/s12630-009-9110-1. [DOI] [PubMed] [Google Scholar]
- 16.Aksu C, Gürkan Y. Ultrasound guided erector spinae block for postoperative analgesia in pediatric nephrectomy surgeries. J Clin Anesth. 2017;45:35–36. doi: 10.1016/j.jclinane.2017.12.021. [DOI] [PubMed] [Google Scholar]