Abstract
Background
Cutaneous leishmaniasis (CL) is a protozoan infectious disease. Dermoscopy is a noninvasive diagnostic tool that has been applied to several skin diseases, including infestations.
Objectives
To determine the dermoscopic patterns of CL lesions and to investigate whether a relationship exists between dermoscopic characteristics and the disease duration, localization, and type of CL lesions.
Methods
Seventy-nine patients (48 male, 31 female) from Hatay, Turkey, were enrolled in the study and a dermoscopic evaluation was performed on 139 lesions. Images of CL lesions were taken via polarized light contact dermoscopy. Chi-square and Fisher exact tests were used for statistical analyses and P values <0.05 were considered significant.
Results
Generalized erythema was seen in all CL lesions. Vascular structures (94.2%), yellow tears (75.5%), and a white starburst-like pattern (58.3%) were the other most common dermoscopic features. Hyperkeratosis (P = 0.001) and white starburst-like pattern (P < 0.001) were more prevalent in the extremities than elsewhere. Among vascular structures, linear irregular (45.8%), hairpin (43.5%), and comma-shaped (25.9%) patterns were the most common dermoscopic findings. Linear irregular (P = 0.023) and arborizing vessels (P = 0.001) were observed in the head-neck region. Dotted (P = 0.009), hairpin (P < 0.001), and glomerular-like (P = 0.016) morphological findings were more prevalent in the extremities. Statistical significances in disease duration were detected in microarborizing (P = 0.027) and arborizing (P = 0.004) vessels and were most prevalent with a disease duration of >6 months. Hairpin vessels were prevalent in the plaque and nodulo-ulcerative type of lesions. Dotted vessels were most commonly seen in the plaque type (47.4%) of lesions.
Conclusions
Generalized erythema, yellow tears, and starburst-like patterns, as well as linear irregular, hairpin, comma-shaped, and arborizing vessels, were the most commonly detected dermoscopic features of CL lesions. We suggest that the presence of these features can be helpful when diagnosing CL lesions by dermoscopy.
Keywords: dermoscopy, leishmaniasis, vascular, cutaneous
Introduction
Cutaneous leishmaniasis (CL) is a protozoan infectious disease caused by the Leishmania genus of flagellate protozoan, and the disease is widespread in most countries in the Mediterranean basin, including Turkey [1]. More than 70% of global CL cases occur in 10 countries (Afghanistan, Algeria, Brazil, Colombia, Costa Rica, Ethiopia, Islamic Republic of Iran, Peru, Sudan, and the Syrian Arab Republic) [2].
Dermoscopy is a noninvasive diagnostic tool that has been used in melanocytic lesions. Dermoscopy has also been also used in several skin diseases, such as inflammatory skin disorders, hair disorders, and infestations [3].
Although there have been a few studies about dermoscopic patterns of CL, there are conflicting results about the location, duration, type of lesions, and dermoscopic findings [4–6]. In this study, we aimed at determining the dermoscopic features of CL lesions and at investigating whether a relationship exists between the dermoscopic characteristics of CL lesions and the disease duration, localization, and type of lesion. In addition, the background color and distribution of vascular structures in the CL lesions were evaluated.
Methods
This prospective study was performed at a tertiary care hospital in the region Hatay, which is an endemic area for CL and located in the southern part of Turkey. The study was conducted in accordance with the Declaration of Helsinki. The local ethics committee approved the study (approval number 010620122-06), and informed consent was obtained from all participants. A total of 79 patients (48 male, 31 female; age range 2–85 years), who were seen in the dermatology outpatient clinic and were diagnosed with CL, were included in the study.
CL was diagnosed clinically, and the diagnosis was confirmed by a laboratory demonstration of the presence of the parasite in the smears obtained from the lesions. If the smear was negative, a histopathological examination was performed. Identification of Leishmania organisms in the histiocyte cytoplasm with Giemsa staining was also considered as Leishmania-positive. Exclusion criteria were any CL treatment (topical, intralesional, or systemic) before recruitment to the study.
Full demographic details and history of the disease, including age, gender, duration of the disease, localization, and clinical type of the lesion, were recorded in a predesigned clinical record form for each patient.
All CL lesions were evaluated following the diagnosis. The dermoscopic evaluation was performed by 2 clinicians (G.S., Ö.E.). Clinical and dermoscopic photographs of the lesions were performed with a polarized light contact dermoscopy (Mole Max II, Derma Instruments, Vienna, Austria; 20- to 40-fold magnification). We applied 70% alcohol or water over the lesions before taking dermoscopic images. When taking the images, we applied minimal downward pressure to visualize the vascular structures.
Dermoscopic evaluation of vascular structures was based on previous reports in the studies of Argenziano et al [7] and Zalaudek et al [8]. The background color of lesions was evaluated and performed according to the study presented by Lallas et al [3]. We also assessed the distribution of vascular structures in the CL lesions and categorized them into the following patterns: peripheral (observed predominantly at the periphery of the lesion), patchy (arranged in an asymmetrical distribution which could not be classified as clustered), central, regular (vessels distributed uniformly throughout the lesion), and cluster (aggregated in small groups) [3].
Data were analyzed using SPSS for Windows (version 13; SPSS Inc., Chicago, IL, USA). Values were given as mean ± standard deviation (SD) or frequency and percent. Disease duration was dichotomized as ≤6 months or >6 months. The dermoscopic characteristics of the CL lesions were compared with the duration of the disease, the location, and the type of lesion using the chi-square and Fisher exact tests. P values < 0.05 were considered significant.
Results
Demographic Data
One hundred thirty-nine CL lesions from 79 patients (48 male [60.76%], 31 female [39.24%]) were enrolled in the study. The mean age of the patients was 24.05 ± 18.89 (range, 2–85 years; median, 17 years) and the duration of the disease was 8.68 ± 20.63 (range, 1–240 months). The duration of the disease was ≤6 months in 54.4% of patients and >6 months in 45.6% of patients. The most frequent lesion localization was the head, followed by the upper and lower extremities. CL lesions were described as papular, nodular, nodulo-ulcerative, and plaque type. Most of the lesions were nodules (42.4%). The details of the clinical and demographic characteristics of the patients and lesions are shown in Table 1.
Table 1.
Clinical and Demographic Characteristics of the Patients and Lesions
| Characteristics | n (%) |
|---|---|
| Sex | |
| Female | 48 (60.7) |
| Male | 31 (39.2) |
| Age (yrs), mean ± SD | 24.05 ± 18.89 |
| Duration of disease, mean ± SD | |
| ≤6 months | 43 (54.4) |
| >6 months | 36 (45.6) |
| Total no. of lesions | 139 (100) |
| No. of lesions | |
| 1 | 52 (65.8) |
| 2 | 12 (15.2) |
| 3 | 4 (5.1) |
| 4 | 6 (7.6) |
| 5 | 3 (3.8) |
| 6 | 2 (2.5) |
| Type of lesion | |
| Papular | 20 (14.4) |
| Nodular | 59 (42.4) |
| Nodulo-ulcerative | 33 (23.7) |
| Plaque | 27 (19.4) |
| Location of lesions | |
| Face | |
| Forehead | 7 (5) |
| Periorbital region | 3 (2.2) |
| Malar Region | 35 (25.2) |
| Ear | 1 (0.7) |
| Nose | 9 (6.5) |
| Lip | 5 (3.6) |
| Chin | 5 (3.6) |
| Neck | 3 (2.2) |
| Upper extremities | |
| Shoulder | 3 (2.2) |
| Arm | 31 (22.3) |
| Elbow | 7 (5.0) |
| Hand | 19 (13.7) |
| Lower extremities | |
| Leg | 5 (3.6) |
| Knee | 1 (0.7) |
| Foot | 5 (3.6) |
Dermoscopic Findings
General Pattern
The descriptive results of the dermoscopic analysis are shown in Table 2. The Fitzpatrick skin types of the patients were II and III. Generalized erythema was seen in all CL lesions. The color of erythema was dusky red (33.8%), light red (43.9%), and yellowish red (22.3%) (Figure 1). Vascular structures (94.2%), yellow tears (75.5%), and white starburst-like pattern (58.3%) were the other most common dermoscopic features (Figures 2 and 3).
Table 2.
Dermoscopic Features in CL
| Dermoscopic Features | n (%) |
|---|---|
| General features | |
| Erythema | 139 (100) |
| Dusky red | 47 (33.8) |
| Light red | 61 (43.9) |
| Yellowish red | 31 (22.3) |
| Hyperkeratosis | 49 (35.3) |
| CE/U | 10 (7.2) |
| HK+E/U | 23 (16.5) |
| Yellow tears | 105 (75.5) |
| White starburst-like pattern | 81 (58.3) |
| White scar-like patch | 7 (5.0) |
| Milia-like cyst | 12 (8.6) |
| Yellowish hue | 1 (0.7) |
| Salmon-colored ovoid | 4 (2.9) |
| Vascular features | 131 (94.2) |
| Comma-shaped | 34 (25.9) |
| Linear irregular | 60 (45.8) |
| Dotted | 19 (14.5) |
| Hairpin | 57 (43.5) |
| Arborizing | 24 (18.3) |
| Corkscrew | 5 (3.8) |
| Glomerular-like | 28 (21.4) |
| Milky red globules/areas | 15 (11.4) |
| Microarborizing | 21 (16.0) |
| Crown | 4 (3.0) |
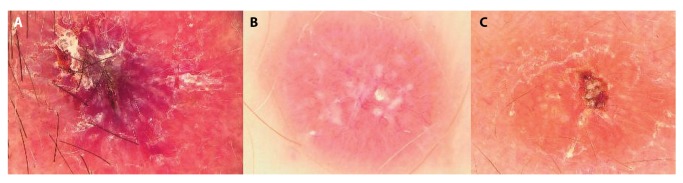
Figure 1.
Examples of background color with polarized light contact dermoscopy (PlCD). (A) Dusky red (PlCD × 20). (B) Light red (PlCD × 40). (C) Yellowish red (PlCD × 30). [Copyright: ©2019 Serarslan et al.]
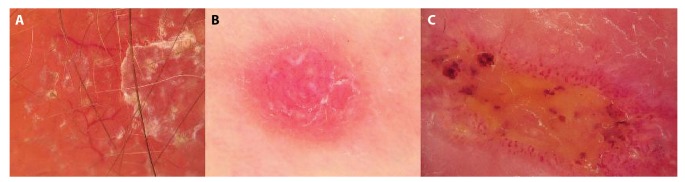
Figure 2.
(A,C) Clinical picture of CL lesion. (B) Dermoscopically lesion reveals yellow tears (PlCD × 30). (D) Yellow tears with central crust (PlCD × 30). [Copyright: ©2019 Serarslan et al.]
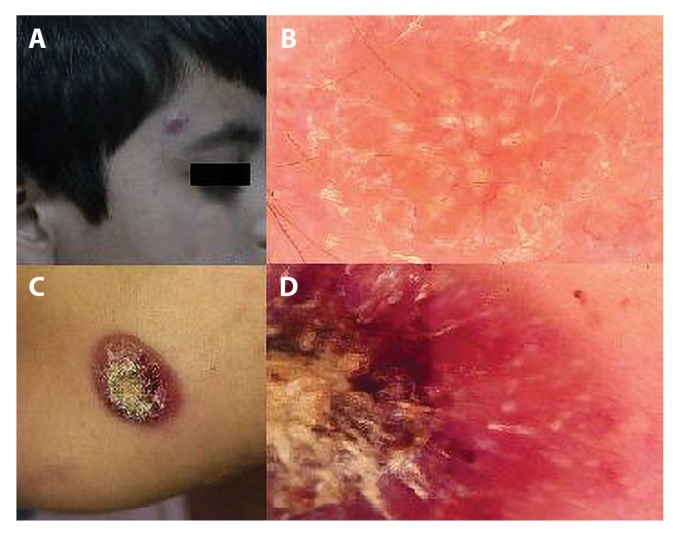
Figure 3.

(A,C) Clinical features of leishmaniasis. (B,D) Examples of starburst-like pattern (PlCD × 20 and × 30). [Copyright: ©2019 Serarslan et al.]
Hyperkeratosis and white starburst-like pattern were more prevalent in the extremities than elsewhere (P = 0.001 and P < 0.001, respectively). However, there was no statistically significant difference in color of erythema, hyperkeratosis + erosion/ulceration (HK+E/U), yellow tears, and milia with regard to localization of CL (P ≥ 0.05). Dermoscopic structures including central erosion/ulceration (CE/U), white scar-like patch, yellowish hue, and salmon-colored ovoid, corkscrew, and crown were not included in the statistical analysis because of low rate of these features.
Hyperkeratosis was more prevalent in CL lesions with a disease duration of ≤6 months (P = 0.036). There were no statistically significant differences between the disease duration and color of erythema, HK+E/U, yellow tears, white starburst-like pattern, and milia (P ≥0.05). There was also no statistically significant difference between the disease duration and CL type (P = 0.605). The features, including CE/U, yellowish hue, salmon-colored ovoid, and white scar-like patch, were not included in the statistical analysis because of low rate of these features.
Vascular Morphology
Linear irregular (45.8%), hairpin (43.5%), and comma-shaped (25.9%) patterns were the most common dermoscopic findings among vascular structures. Vascular structures, including linear irregular, dotted, hairpin, arborizing, glomerular-like, crown, and corkscrew types, were most commonly seen in the peripheral distribution. The distributions of vascular structures are shown in Table 3. In 54.7% of lesions, there were 2 or more vascular structures, and most of the lesions were the nodular type (39.5%). Hairpin-like vessels were most frequently combined with linear and glomerular-like vessels.
Table 3.
Distribution of Vascular Structures
| Peripheral n (%) | Patchy n (%) | Central n (%) | Regular n (%) | Cluster n (%) | Total (n) | |
|---|---|---|---|---|---|---|
| Comma-shaped | 10 (29.4) | 15(44.1) | 4 (11.8) | 1 (2.9) | 4 (11.8) | 34 |
| Linear irregular | 29 (48.3) | 14 (23.3) | 4 (6.7) | 10 (16.7) | 3 (5.0) | 60 |
| Dotted | 10 (52.6) | 4 (21.0) | — | 2 (10.5) | 3 (15.8) | 19 |
| Hairpin | 24 (42.1) | 17 (29.8) | — | 7 (12.3) | 9 (15.8) | 57 |
| Arborizing | 20 (83.3) | — | — | 4 (16.7) | — | 24 |
| Corkscrew | 3 (60.0) | 1 (20.0) | 1 (20.0) | — | — | 5 |
| Glomerular | 15 (53.6) | 9 (32.1) | — | 2 (7.1) | 2 (7.1) | 28 |
| Crown | 3 (75.0) | 1 (25.0) | — | — | — | 4 |
| Microarborizing | 7 (33.3) | 2 (9.5) | — | 12 (57.7) | — | 21 |
| Milky red areas | 5 (33.3) | 5 (33.3) | 4 (26.7) | — | 1 (6.7) | 15 |
Linear irregular and arborizing vessels were observed in the head-neck localization in 60.0% and 79.2% of lesions, respectively, with a statistically significant difference (P = 0.023 and P = 0.001, respectively). Dotted (78.9%), hairpin (70.2%), and glomerular-like (71.4%) morphology were more prevalent in the extremity localizations (P = 0.009, P < 0.001, and P = 0.016, respectively). There was no statistically significant difference in comma-shaped, microarborizing, and milky red areas with regard to the localization of CL lesions (P ≥ 0.05).
A statistically significant difference was detected only in microarborizing vessels with regard to the disease duration among vascular structures, which was more prevalent with the disease duration >6 months (P = 0.027).
Hairpin vessels were more prevalent in the plaque (n = 19) and nodulo-ulcerative (n = 19) type of lesions. More than half (53.3%) of the milky red areas were seen in the nodulo-ulcerative type of lesions. The majority of the nodular type of CL lesions presented comma-shaped, linear irregular, arborizing, microarborizing, and glomerular type of vessels. Dotted vessels were most commonly seen in the plaque type (47.4%) of lesions. Dermoscopic features according to the types of CL lesions are shown in Table 4. Examples of the vascular structures are shown in Figure 4.
Table 4.
Dermoscopic Features According to the Types of CL Lesions
| Papule (n) | Plaque (n) | Nodule (n) | NU (n) | Total (n) | |
|---|---|---|---|---|---|
| General features | |||||
| Erythema | 20 | 27 | 59 | 33 | 139 |
| Hyperkeratosis | 3 | 19 | 23 | 4 | 49 |
| CE/U | 1 | — | 2 | 7 | 10 |
| HK+E/U | — | 1 | 2 | 20 | 23 |
| Yellow tears | 13 | 23 | 44 | 25 | 105 |
| White starburst-like | 2 | 23 | 27 | 29 | 81 |
| White scar-like | — | 2 | 4 | 1 | 7 |
| Milia-like cyst | 1 | 4 | 3 | 4 | 12 |
| Yellowish hue | — | — | 1 | — | 1 |
| Salmon-colored ovoid | — | 1 | 3 | — | 4 |
| Vascular features | |||||
| Comma-shaped | 4 | 7 | 16 | 7 | 34 |
| Linear irregular | 7 | 12 | 30 | 11 | 60 |
| Dotted | — | 9 | 3 | 7 | 19 |
| Hairpin | 2 | 19 | 17 | 19 | 57 |
| Arborizing | 2 | 2 | 15 | 5 | 24 |
| Corkscrew | — | 2 | 1 | 2 | 5 |
| Glomerular-like | 5 | 7 | 9 | 7 | 28 |
| Milky red globules/areas | 1 | 2 | 4 | 8 | 15 |
| Microarborizing | 4 | 2 | 12 | 3 | 21 |
| Crown | — | 2 | 2 | — | 4 |
NU = nodulo-ulcerative.
Figure 4.
Vascular structures of CL lesions (PlCD × 40). (A) Arborizing vessels with peripheral distribution. (B) Regularly distributed hairpin vessels. (C) Microarborizing vessels. [Copyright: ©2019 Serarslan et al.]
Discussion
We detected that generalized erythema (100%), vascular structures (94.2%), yellow tears (75.5%), and white starburst-like pattern (58.3%) were the most common dermoscopic features in CL lesions. Similar to our study, Llambrich et al [9], Ayhan et al [4], and Yücel et al [5] also reported that generalized erythema was present in all lesions. However, in their study, Taheri et al [6] reported that generalized erythema was present in 81.9% of lesions and was more common in advanced and ulcerated lesions. We also detailed the color of erythema as dusky red (33.8%), light red (43.9%), and yellowish red (22.3%). We detected no significant differences in our analyses of the color of erythema and disease duration and localization. However, we detected that 45.5% of dusky red lesions were of the nodulo-ulcerative type, 63% of light red lesions were the plaque type, and 50% of yellowish red lesions were the papular type.
Yellow tear-like structures were the third most common dermoscopic finding in our study. These structures were observed both in the head-neck region (52.4%) and extremities (47.6%). Although in several studies these structures have been reported only on the face and neck [4,5], in another study [6] extremities were reported to be the more prevalent localization. Similar to other studies, in our study yellow tear-like structures were more common in lesions with a duration of ≤6 months (58.1%) [5, 9]. These structures were seen mostly in the nodular type (41.9%) of lesions followed by the nodulo-ulcerative (23.8%), plaque (21.9%), and papule (12.4%) type. Taheri et al [6] reported that these structures were more prevalent in ulcerated plaques. Yücel et al [5] reported that yellow tear-like structures were observed more commonly in nodules.
We detected that the white starburst-like pattern was more prevalent in the extremities localization and nodulo-ulcerative type of lesions. In 61.7% of lesions, the disease duration was ≤6 months. Yücel et al [5] reported that the white starburst-like pattern was observed more commonly in nodulo-ulcerative lesions and lesions with durations of 0–6 and 7–12 months. Also, Llambrich et al [9] detected that the white starburst-like pattern was more prevalent in the extremities. However, in another study, in contrast to our findings, these authors reported that this pattern was more prevalent in lesions older than 6 months and was related to nodular lesions [6].
Vascular structures, including linear irregular (45.8%), hairpin (43.5%), and comma-shaped (25.9%) morphology, were the most common dermoscopic findings among vascular structures in our study. Although previous studies reported conflicting results on these common vascular structures, most of them, including in our study, showed that linear irregular and hairpin vessels were the most common (Table 5). We also evaluated the distribution of vascular structures in the lesions. As shown in Table 3, most of the vascular structures were present in peripheral distribution.
Table 5.
Dermoscopic Features of CL in the 5 Performed Studies
| Dermoscopic Features | Llambrich et al [9] (n = 26) % | Taheri et al [6] (n = 144) % | Yücel et al [5] (n = 145) % | Ayhan et al [4] (n = 127) % | Current Study (n = 139) % |
|---|---|---|---|---|---|
| General features | |||||
| Generalized erythema | 100 | 81.9 | 100 | 100 | 100 |
| Yellow tears | 53 | 41.7 | 40 | 42.5 | 75.5 |
| White starburst-like pattern | 38 | 60.4 | 19 | 8.6 | 58.3 |
| Hyperkeratosis | 50 | 33.3 | — | 15 | 35.3 |
| HK+E/U | 38 | — | 35 | — | 16.5 |
| Milia-like cyst | — | 4.9 | — | 15.7 | 8.6 |
| Salmon-colored ovoid | — | — | 13 | 15.7 | 2.9 |
| CE/U | 46 | 59 | — | 44.1 | 7.2 |
| Yellowish hue | — | 43.8 | — | — | 0.7 |
| Perilesional hypopigmented halo | — | — | 3 | — | — |
| Scar (white scar-like patch) | — | — | — | 17.3 | 5.0 |
| Pustules | — | — | — | 7.1 | — |
| Crust | — | — | — | 70.1 | — |
| Vascular features | 100 | 87 | 90.6 | 94.2 | |
| Glomerular-like vessels | 7 | 22.9 | 17 | 3.1 | 21.4 |
| Hairpin vessels | 19 | 37.5 | 17 | 39.4 | 43.5 |
| Linear irregular vessels | 57 | 30.6 | 54 | 26 | 45.8 |
| Arborizing telangiectasia | 11 | 10.4 | 37 | 38.6 | 18.3 |
| Crown-like vessels | — | — | — | 1.6 | 3.0 |
| Dotted vessels | 53 | 61.1 | 16 | 24.4 | 14.5 |
| Comma-shaped vessels | 73 | 29.9 | 4 | 19.7 | 25.9 |
| Polymorphous/atypical vessels | 26 | — | 3 | 40.2 | 15.2 |
| Corkscrew vessels | 7 | 4.2 | — | 3.1 | 3.8 |
| Strawberry pattern | — | — | — | 1.6 | — |
| Milky red globules/areas | — | — | — | — | 11.4 |
| Microarborizing | — | — | — | — | 16.0 |
—Not reported or evaluated.
The linear irregular type of vascular morphology was more prevalent in the head-neck region. The linear irregular vascular morphology was seen mostly in the nodular (50.0%) and plaque (20.0%) type of lesions. The distribution of linear irregular vascular structure in the CL lesions represented peripheral (48.3%), followed by patchy (23.3%) and regular (16.7%). Duration of the disease was ≤6 months in 34 (56.7%) lesions and >6 months in 26 (43.3%) lesions, and there was no statistical significance. Similar to our study, the face has been reported to be the most common localization of linear irregular vessels [4]. However, in another study, linear irregular vessels were reported to be more common in advanced lesions and not related to the lesion site [6].
Comma-shaped vessels were seen mostly in the nodular type (47.1%) of lesions and were not related to the lesion site (head-neck, 52.9%; extremity, 47.1%) or duration of the disease. In our study, the distribution of comma-shaped vessels was mostly in the patchy pattern (44.1%). The prevalence of hairpin vessels has been reported to be between 17% and 43.5% in CL lesions. We found that hairpin vessels were more prevalent in the extremities and that these structures were more common in advanced lesions, but were not related to the lesion site. Hairpin vessels were seen mostly in the plaque and nodulo-ulcerative type of lesions. Other studies, including Ayhan et al [4], Llambrich et al [9], and Yücel et al [5], also reported that extremities were the most common site and were observed in nodulo-ulcerative lesions. In contrast, Taheri et al [6] reported that hairpin vessels were not related to the type of skin lesions.
We differentiated arborizing structures as arborizing or microarborizing based on the study of Zalaudek et al. Microarborizing vessels represented a variation of arborizing vessels and were defined as linear straight/linear serpentine vessels with a small caliber [8]. The arborizing type of vascular morphology was most prevalent in the head-neck region. However, no statistical difference was detected for microarborizing vessels when comparing lesion sites. Both structures were more frequent in the nodular type of lesions, and also both of these structures were common when the disease duration was >6 months.
Conclusions
CL presents a variety of dermoscopic patterns that might cause difficulties during dermoscopic diagnosis. When we compared the most frequent first 5 findings for general dermoscopic and vascular features, we found that generalized erythema, yellow tears, and white starburst-like patterns, as well as and linear irregular, hairpin, comma-shaped, and arborizing vessels, were associated with CL lesions in our study, as well as in most previous studies. Therefore, we suggest that the presence of these parameters will help during the diagnosis of CL lesions by dermoscopy. We also think that dermoscopy can be used more reliably in the diagnosis of CL by comparing the dermoscopic features of the diseases with similar clinical appearances, such as other granulomatous diseases [10] and cutaneous B-cell lymphoma [11–13].
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Uz OK, Balcıoğlu IC, Taylan Özkan A, Ozensoy S, Ozbel Y. Leishmaniasis in Turkey. Acta Trop. 2002;84(1):43–48. doi: 10.1016/s0001-706x(02)00134-1. [DOI] [PubMed] [Google Scholar]
- 2.WHO. Leishmaniasis in high-burden countries: an epidemiological update based on data reported in 2014. Wkly Epidemiol Rec. 2016;91(22):287–296. [PubMed] [Google Scholar]
- 3.Lallas A, Kyrgidis A, Tzellos TG, et al. Accuracy of dermoscopic criteria for the diagnosis of psoriasis, dermatitis, lichen planus and pityriasis rosea. Br J Dermatol. 2012;166(6):1198–1205. doi: 10.1111/j.1365-2133.2012.10868.x. [DOI] [PubMed] [Google Scholar]
- 4.Ayhan E, Ucmak D, Baykara SN, Akkurt ZM, Arica M. Clinical and dermoscopic evaluation of cutaneous leishmaniasis. Int J Dermatol. 2015;54(2):193–201. doi: 10.1111/ijd.12686. [DOI] [PubMed] [Google Scholar]
- 5.Yücel A, Günasti S, Denli Y, Uzun S. Cutaneous leishmaniasis: new dermoscopic findings. Int J Dermatol. 2013;52(7):831–837. doi: 10.1111/j.1365-4632.2012.05815.x. [DOI] [PubMed] [Google Scholar]
- 6.Taheri AR, Pishgooei N, Maleki M, et al. Dermoscopic features of cutaneous leishmaniasis. Int J Dermatol. 2013;52(11):1361–1366. doi: 10.1111/ijd.12114. [DOI] [PubMed] [Google Scholar]
- 7.Argenziano G, Zalaudek I, Corona R, et al. Vascular structures in skin tumors. Arch Dermatol. 2004;140(12):1485–1489. doi: 10.1001/archderm.140.12.1485. [DOI] [PubMed] [Google Scholar]
- 8.Zalaudek I, Kreusch J, Giacomel J, Ferrara G, Catriacala C, Argenziano G. How to diagnose nonpigmented skin tumors: a review of vascular structures seen with dermoscopy, part I: melanocytic skin tumors. J Am Acad Dermatol. 2010;63(3):361–374. doi: 10.1016/j.jaad.2009.11.698. [DOI] [PubMed] [Google Scholar]
- 9.Llambrich A, Zaballos P, Terrasa F, Torne I, Puig S, Malvehy L. Dermoscopy of cutaneous leishmaniasis. Br J Dermatol. 2009;160(4):756–761. doi: 10.1111/j.1365-2133.2008.08986.x. [DOI] [PubMed] [Google Scholar]
- 10.Errichetti E, Stinco G. Dermoscopy of granulomatous disorders. Dermatol Clin. 2018;36(4):369–375. doi: 10.1016/j.det.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Piccolo V, Russo T, Agozzino M, et al. Dermoscopy of cutaneous lymphoproliferative disorders: where are we now? Dermatology. 2018;234(3–4):131–136. doi: 10.1159/000490412. [DOI] [PubMed] [Google Scholar]
- 12.Piccolo V, Mascolo M, Russo T, Staibano S, Argenziano G. Dermoscopy of primary cutaneous B-cell lymphoma (PCBCL) J Am Acad Dermatol. 2016;75(4):e137–e139. doi: 10.1016/j.jaad.2016.02.1217. [DOI] [PubMed] [Google Scholar]
- 13.Mascolo M, Piccolo V, Argenziano G, et al. Dermoscopy pattern, histopathology and immunophenotype of primary cutaneous B-cell lymphoma presenting as a solitary skin nodule. Dermatology. 2016;232(2):203–207. doi: 10.1159/000442251. [DOI] [PubMed] [Google Scholar]