Abstract
Background
In 2007 the International Psoriasis Council considered palmoplantar pustulosis (PPP) a condition separate from psoriasis, and several authors maintain that PPP is a reactive process to metal contact allergies independent from psoriasis.
Objectives
To evaluate the frequency of allergies and psoriasis in patients with PPP and to determine the role of allergens in PPP.
Methods
A systematic search of the English databases (PubMed and Web of Science) from January 1964 to August 2018 to identify all patients affected by PPP and allergies and/or psoriasis.
Results
In total, 16 publications describing a total of 519 patients with PPP were evaluated and 122 cases of concomitant PPP and metal allergy were found. The frequency of allergies among patients with PPP was 22.7%; between the identified allergens, 84.3% of cases correspond to metal allergies. In 65.1% of metal allergies, an improvement in PPP was seen after withdrawal of contact. The concomitant presence of psoriasis was recorded in 18% of the cases.
Conclusion
There is some evidence to support the association of PPP with metal allergies but also with psoriasis, suggesting the role of metal allergens as a trigger factor in patients with PPP.
Keywords: palmoplantar pustulosis, contact allergy, psoriasis, metals, nickel, patch test
Introduction
Palmoplantar pustulosis (PPP) is a chronic inflammatory condition characterized by the recurrent appearance of crops of sterile pustules on the palms and soles, in conjunction with erythematous keratotic lesions that tend to crack, causing bleeding and pain [1–4]. Since 1930 when Barber described the condition under the name of PPP and classified the disease as a local pustular variant of psoriasis, this entity has been in the middle of an endless debate regarding the etiology and the possible association with other diseases [1–4]. Several authors have suggested that PPP should be regarded as a separate entity and not a clinical variant of psoriasis despite the presence of certain phenotypes common in both diseases [4–8], and in 2007 the International Psoriasis Council considered PPP as a condition separate from psoriasis [9].
In the last 15 years many authors have considered PPP as a reactive process (a subtype of systemic contact dermatitis) because of the numerous reports available in the literature that link PPP to metal allergies (nickel, iron, cobalt, zinc, and copper), and such association has driven many dermatologists to ignore the possible concomitant presence of psoriasis in patients with PPP [10–12].
In the literature, there are different isolated reports of the association of PPP and allergies, but well-designed studies are missing. Motivated by these controversial issues, we performed this systematic review to assess the association between PPP and allergies.
In the current article we present a systematic literature review that identifies all cases reported of PPP patients with a concomitant contact allergy (identified by a positive patch test and/or by an aggravation of the PPP related to a contact allergy and/or patients in whom the elimination of dental alloys or devices containing metals brought to complete remission of the PPP). We also evaluated in the identified cases the concomitant presence of psoriasis, if available.
Methods
We followed the Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines during the present systematic literature review. No ethical approval was requested.
Literature Search and Selection of Studies
We performed a systematic search of English databases (PubMed and Web of Science) from January 1964 until August 2018, using the following key words and MeSH terms: “palmoplantar pustulosis,” and/or “palmoplantar,” and/or “pustulosis,” and/or “psoriasis,” and/or “palms and soles,” and/or “patch test,” and/or “contact allergy,” and/or “contact dermatitis,” and/or “metals,” and/or “psoriasis,” and/or “acropustulosis,” and/or “pustulosis palmaris et plantaris,” and/or “nickel,” and/or “zinc,” and/or “cobalt,” and/or “platinum,” and/or “tin,” and/or “iron,” and/or “mercury,” and/or “copper,” and/or “chromium,” and/or “palladium.” No exclusion criteria were applied.
Data Extraction and Quality Assessment
Three reviewers (A.B.V., C.P., and C.M.) independently screened all the identified studies and any disagreement was discussed and resolved. Because of the quality of the observational studies included (no cohort, nor case-control or cross-sectional studies) it was not possible to perform a meta-analysis.
Results
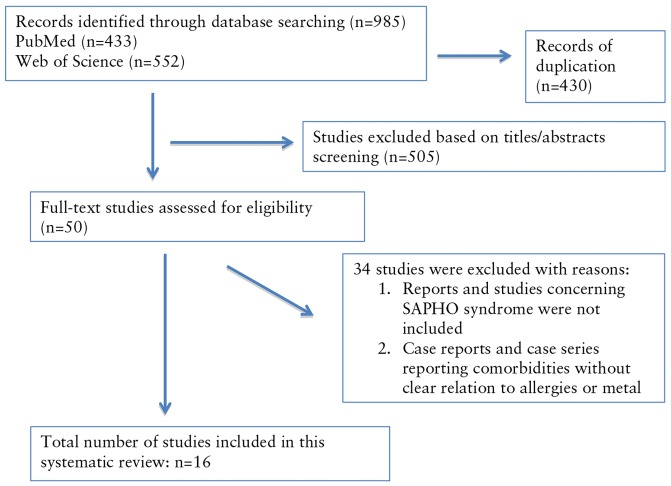
We identified 506 reports; 50 were assessed for eligibility and only 16 publications fulfilled the requirements for the present systematic review. The overview of the research strategy is illustrated in Figure 1 [1–6,8–17]. The majority of the articles retrieved are case series, case reports, and retrospective observational studies. Well-designed prospective studies in which patients affected by PPP are concomitantly tested for contact allergies are missing. Publication biases and selective reporting within studies were identified; the majority of PPP studies do not report concomitant allergies or patch test results (and were not included) and the studies analyzed in the present systematic review were prone to report a positive correlation between PPP and allergies. One hundred twenty-two cases affected by PPP and contact dermatitis or metal allergy between the years 1964 and 2018 were identified [1–6,8–17]. The patients were evaluated for the following variables: disease, sex, smoking habits, allergy type, patch test result (positivity and allergen), improvement of PPP lesions after allergen avoidance (permanent or partial improvement), exacerbation of PPP lesions after patch test, and concomitant psoriasis (psoriasis vulgaris, nail psoriasis, and/or psoriatic arthritis).
Figure 1.
Overview of the Research Strategy. SAPHO = synovitis, acne, pustulosis, hyperostosis, andosteitis. [Copyright: ©2019 Brunasso Vernetti et al.]
The patients identified were 519 in total, 105 males and 395 females, but in 19 cases sex data were not available. For those with available sex data, males comprised 21% (105/500) and females 79% (395/500) of the whole cohort (Table 1). Data regarding smoking (previous or active) were available in fewer than 50% of the records and are not included in this analysis.
Table 1.
Description of Contact Allergies and/or Metal Exposure and Psoriasis in Patients Affected by PPP
| First Author, Year | No. of PPP Patients (M/F) | No. of Patients With Eczema (Type) | No. of Patients Improved After Allergen Withdrawal (Permanent, Partial, or Absent) | Exacerbation of PPP After Patch Test | No. of Patients With Psoriasis (Skin or Nails) |
|---|---|---|---|---|---|
| Ashurst, 1964 [1] | 43 (5/38) | 1 (nickel dermatitis), 1 irritant dermatitis |
NA | NA | 1 (skin) 6 (nails) |
| Enfors, 1971 [2] | 248 (56/192) | 38 (NA) | NA | NA | 34 (14%) |
| Thomsen, 1973 [3] | 40 (8/32) | 2 (Co) 1 (Ni) 1 (neomycin) 1 (formalin) 1 (benzyl salicylate) |
NA | NA | 12 (skin and/or nails) |
| Fransson, 1985 [4] | 7 (NA) | 1 (Co chloride, balsam of Peru, fragrance mix) | NA | NA | 60% (nails) |
| Pasić, 1989 [5] | 8 (NA) | 20% (1 patient) | NA | NA | NA |
| Nakayama, 1990 [6] | 11 (2/9) | 11 (Cr, Hg, Pt, Hg, Sn, Cu, Ni, Co, Zn) | 11 permanent | NA | NA |
| Yiannias, 1998 [8] | 21 (5/16) | 9 patients, 7 with multiple positive patch tests 4 (fragrance mix) 2 (cinnamic aldehyde) 2 (balsam of Peru) 1 (Ni) |
7 partial 2 absent (1 Ni) |
NA | 2 mild psoriasis (skin) 1 family history of psoriasis |
| Nakamura, 2000 [7] | 7 (3/4) | 7 (Ni, Co, Pt, Sn, Fe, Pa) | 2 NA | 7 patients | NA |
| Dantzig, 2003 [10] | 4 (NA) | 4 (Hg) | 4 permanent | NA | 1 psoriasis |
| Yanagi, 2005 [11] | 1 (F) | 1 (Zn) | 1 permanent | NA | NA |
| Wen, 2008 [12] | 1 (F) | 1 (Cu) | 1 permanent | Yes | NA |
| Song, 2011 [13] | 1 (M) | 1 (Co) | 1 permanent | No | NA |
| Ito, 2014 [14] | 1 (F) | 1 (Ni) | 1 permanent | Yes | NA |
| Liu, 2016 [15] | 2 (1/1) | 1 (No + Co) 1 (Ni) |
2 permanent | No | No/NA |
| Kouno, 2017 [16] | 85 (23/62) | 29 (10 Hg, 8 Ni, 8 Go, 7 Pa, 6 Sn, 5 Co, 5 Zn) 4(3 Cr, 2 Ir, 2 Mo) |
3 permanent | NA | NA |
| Misiak-Galazka, 2018 [17] | 39 (1/38) | 12 (5 Ni, 1 Cr, 2 Co, rest other allergens) | 7/9 NA | NA | 27% + 5% family history |
NA = not available; Co = cobalt; Cr = chromium; Cu = copper; Fe = iron; Go = gold; Hg = mercury; Ir = iridium; Mo = molybdenum; Ni = nickel; Pa = palladium; Pt = platinum; Sn = tin; Zn = zinc.
Positive patch tests were recorded in 121 of 519 (23.3%) patients. Metal allergens (chromium, mercury, platinum, tin, copper, nickel, cobalt, zinc, iron, gold, iridium, molybdenum, and palladium) were reported in 67 cases (55%), and another 4 cases presented high blood mercury levels that improved PPP after diet changes and/or chelation [10]. One patient presented with concomitant PPP and irritant dermatitis. In 19 cases contact allergies were due to different allergens (neomycin, formalin, benzyl salicylate, colophony, Eucerin, turpentine, p-phenylenediamine, fragrance mix, cinnamic aldehyde, and balsam of Peru), and in 35 cases (28.9%) allergic reactions were reported without the specific allergen [1–6,8–17]. In summary, in 67 of the 86 cases the allergens were metals corresponding to 78% (67/86), while in 22% (19/86) other allergens (not metals) were described.
In 10 publications regarding 48 patients affected concomitantly by PPP and allergies, data about improvement after allergen withdrawal were available [6,8,9–17]. In 31 of these 48 patients, permanent/definitive improvement of PPP was seen after allergen withdrawal (in 28 of 31 cases metals were identified as the causative allergen and the source was mainly from dental amalgams: chromium, mercury, platinum, tin, copper, nickel, cobalt, and zinc) [9–17]. Partial PPP improvement was observed in 7 cases (not related to metal allergies), while in 8 cases no improvement was observed after allergen avoidance [8–16] and in 2 cases an improvement was described but it was not clear whether it was permanent or partial [17]. In 9 cases an exacerbation of PPP lesions after patch testing was reported; all were patients with metal contact allergies (platinum, tin, copper, nickel, cobalt, iron, and palladium) [9,12,14].
Data regarding concomitant psoriasis and PPP were available in 7 publications concerning 428 patients affected by PPP; in 77 of such cases the presence of concomitant psoriasis (mild to moderate plaque psoriasis and/or nail psoriasis and/or psoriatic arthritis) was reported and in 4 cases family history of psoriasis was recorded [1–3,8,10,17]. The frequency of psoriasis in the available data regarding patients affected by PPP and allergies was 18%, but in 115 cases the concomitant presence of psoriasis in patients with PPP was not recorded.
Discussion
After extensive review we found 519 PPP patients evaluated for contact allergies; 23.5% were affected by both PPP and contact allergies. In 28.7% of the cases, the allergen was not reported and metal allergies were identified in 55% of the patients. Considering that in only 86 cases of PPP and contact allergies the allergen was described, 67 of such cases (78%) had metal allergies while in only 19 (22%) contact allergy was associated with other nonmetallic allergens. Of interest, 4 other cases of high blood levels of mercury and PPP improved after diet and/or chelation, suggesting a close relation between metal exposure and PPP [10]. Considering only the 28 out of 48 cases (58.3%) of metal allergies or high blood mercury levels (excluding 3 cases of nonmetal allergies, see Table 1), an improvement in PPP was seen after withdrawal of contact and/or diet change or chelation, suggesting that patients affected by PPP and metal allergies may benefit from allergen contact withdrawal [1–6,8–17]. Other supporting evidence for the role of metal allergy in PPP regards the exacerbation of PPP lesions after patch test (effect only described with metals and not with other allergens) [9,12,14]. Our data support and confirm the frequency of allergic sensitization in patients with PPP (121/519: 23.3%) previously reported in a study conducted with 248 patients with PPP (allergic sensitization frequency of 15.3%) [1].
On the other hand, in the same cohort of patients it was possible to establish the concomitant presence of psoriasis in 18% of the patients with PPP. It is notable that in the 121 patients found to have concomitant PPP and allergies, the presence of psoriasis elsewhere in the body was evaluated and reported in only 45% of cases [1–4,8,10,15,17]. This psoriasis frequency in PPP is lower than the known prevalence of psoriasis in patients with PPP (approximately 33.5%), but this finding probably represents a collection bias of the studies selected for the present systematic review that can be attributed to the fact that many authors consider PPP a form of contact allergy and ignore the concomitant presence of psoriasis. The concomitant presence of psoriasis in patients with PPP is 10 to 25 times higher than in the general population in different cohorts [18–21].
There were several limitations concerning the quality of the data found in the literature. The majority of the articles included were case reports and case series; cohort or case-control studies are missing. In addition, significant heterogeneity among reports was found. Considering that PPP is still considered a rare disease, in order to understand the role of allergies and/or metal exposure in such cases it would be helpful in the future to report the association of PPP with a number of factors, such as sex, age, smoking habits, patch test results, presence of dental amalgams containing metals, type of metal, outcome of PPP after allergen avoidance, presence of other concomitant comorbidities, presence of psoriasis elsewhere in the body, and presence of psoriatic arthritis.
After the extensive review we conducted, we can conclude that there is enough evidence to support some sort of association between PPP and metal allergies in a subgroup of patients; data regarding the improvement of PPP after allergen avoidance confirms such a link. Unfortunately, the frequency of contact allergy among PPP patients that we were able to calculate needs to be considered with caution because of the presence of publication biases. In fact, several authors reported metal allergies as the cause of PPP or classified PPP as a reactive process or a form of allergy, ignoring the possible coexistence of psoriasis and forgetting the possibility that koebnerization (isomorphic response) that may occur in allergic contact dermatitis might explain the association of PPP with contact eczema [22]. Exacerbation of PPP after metal patch test has been reported in 7 patients, with improvement in 2 cases after dental amalgam removal, confirming the trigger role of contact allergens [11]. Moreover, the onset of pustular patch reactions has been described for more than 30 years [23]. Such reactions have been particularly observed with metal compounds (nickel, chromium, mercury, arsenic) and halogens (iodine, fluoride) [23]. The new onset of pustules seems to directly correlate with concentration and vehicle of contact [21–25].
If we decide to ignore the available data that connect PPP to psoriasis and we consider the condition a reactive process to a contact allergy, the avoidance of the allergen will be our primary matter of contention, although nickel is very hard to avoid completely. Several proven facts have brought some colleagues to consider PPP a condition separate from psoriasis: the female predominance in PPP, the strong association of PPP with smoking (much stronger than psoriasis vulgaris), the close relation to metal allergies, some genetic findings as the absence of association between PPP and PSOR1 locus and a higher expression of several genes involved in neural pathways (GPRIN and ADAM23) in PPP compared with psoriasis vulgaris, and the differences in the response to therapy between the 2 conditions [26].
There is a strong association between smoking and PPP, suggesting that smoking has a role in the pathogenesis of this disease. The reported prevalence of current or previous smoking among patients with PPP ranges from 42% to 100%. The mechanism through which smoking could contribute to PPP has not been established. Proposed mechanisms have included effects of nicotine on sweat gland function or keratinocyte function (eg, nicotine-induced increase in keratinocyte cornification). In addition, differences in nicotine acetylcholine receptor staining patterns in PPP skin observed in a study of biopsy specimens taken from patients with PPP, healthy smokers, and healthy nonsmokers prompted consideration that an abnormal response to nicotine could contribute to inflammation [27].
Conclusions
We believe that such findings cannot be ignored, making PPP a particular condition with a specific epidemiological presentation and with a precise genetic background but closely related to psoriasis, also in cases in which the role contact allergic reactions, mainly metal exposure, represents a key factor. Of interest, the European Rare and Severe Psoriasis Expert Network (ERASPEN) in 2017 agreed that there is insufficient evidence-based proof to support the classification of pustular psoriasis in 3 groups: PPP, generalized pustular psoriasis, and acrodermatitis continua of Hallopeau. The association of PPP and psoriasis vulgaris remains in debate [28].
Footnotes
Funding: None.
Competing interests: The authors have no conflicts of interest to disclose.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Ashurst PJ. Relapsing pustular eruptions of the hands and feet. Br J Dermatol. 1964;76:169–180. doi: 10.1111/j.1365-2133.1964.tb14502.x. [DOI] [PubMed] [Google Scholar]
- 2.Enfors W, Molin L. Pustulosis palmaris et plantaris: a follow-up study of a ten-year material. Acta Derm Venereol. 1971;51(4):289–294. [PubMed] [Google Scholar]
- 3.Thomsen K, Osterbye P. Pustulosis palmaris et plantaris. Br J Dermatol. 1973;89(3):293–296. doi: 10.1111/j.1365-2133.1973.tb02977.x. [DOI] [PubMed] [Google Scholar]
- 4.Fransson J, Storgårds K, Hammar H. Palmoplantar lesions in psoriatic patients and their relation to inverse psoriasis, tinea infection and contact allergy. Acta Derm Venereol. 1985;65(3):218–223. [PubMed] [Google Scholar]
- 5.Pasić A, Lipozencić J, Kansky A, Ben-Ghazeil M. Contact allergy in psoriatic patients with palmar and plantar lesions. Acta Derm Venereol Suppl (Stockh) 1989;146:66–68. [PubMed] [Google Scholar]
- 6.Nakayama H, Nogi N, Kasahara N, Matsuo S. Allergen control: an indispensable treatment for allergic contact dermatitis. Dermatol Clin. 1990;8(1):197–204. [PubMed] [Google Scholar]
- 7.Nakamura K, Imakado S, Takizawa M, et al. Exacerbation of pustulosis palmaris et plantaris after topical application of metals accompanied by elevated levels of leukotriene B4 in pustules. J Am Acad Dermatol. 2000;42(6):1021–1025. [PubMed] [Google Scholar]
- 8.Yiannias JA, Winkelmann RK, Connolly SM. Contact sensitivities in palmar plantar pustulosis (acropustulosis) Contact Dermatitis. 1998;39(3):108–111. doi: 10.1111/j.1600-0536.1998.tb05857.x. [DOI] [PubMed] [Google Scholar]
- 9.Griffiths CE, Christophers E, Barker JN, et al. A classification of psoriasis vulgaris according to phenotype. Br J Dermatol. 2007;156(2):258–262. doi: 10.1111/j.1365-2133.2006.07675.x. [DOI] [PubMed] [Google Scholar]
- 10.Dantzig P. The role of mercury in pustulosis palmaris et plantaris. J Occup Environ Med. 2003;45(5):468–469. doi: 10.1097/01.jom.0000069241.06498.5d. [DOI] [PubMed] [Google Scholar]
- 11.Yanagi T, Shimizu T, Abe R, Shimizu H. Zinc dental fillings and palmoplantar pustulosis. Lancet. 2005;366(9490):1050. doi: 10.1016/S0140-6736(05)67384-9. [DOI] [PubMed] [Google Scholar]
- 12.Wen L, Xu T, Yin J. Boils? Or coils? Lancet. 2008;372(9637):506. doi: 10.1016/S0140-6736(08)61201-5. [DOI] [PubMed] [Google Scholar]
- 13.Song H, Yin W, Ma Q. Allergic palmoplantar pustulosis caused by cobalt in cast dental crowns: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(6):e8–e10. doi: 10.1016/j.tripleo.2010.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Ito T, Mori T, Fujiyama T, Tokura Y. Dramatic exacerbation of palmoplantar pustulosis following strongly positive nickel patch testing. Int J Dermatol. 2014;53(5):e327–e329. doi: 10.1111/ijd.12242. [DOI] [PubMed] [Google Scholar]
- 15.Liu F, Zhang M, Lou Y, et al. The spontaneous regression of palmoplantar pustulosis following removal of dental amalgams: a report of two cases. Australas J Dermatol. 2016;57(3):e93–e96. doi: 10.1111/ajd.12366. [DOI] [PubMed] [Google Scholar]
- 16.Kouno M, Nishiyama A, Minabe M, et al. Retrospective analysis of the clinical response of palmoplantar pustulosis after dental infection control and dental metal removal. J Dermatol. 2017;44(6):695–698. doi: 10.1111/1346-8138.13751. [DOI] [PubMed] [Google Scholar]
- 17.Misiak-Galazka M, Wolska H, Galazka A, Kwiek B, Rudnicka L. General characteristics and comorbidities in patients with palmoplantar pustulosis. Acta Dermatovenerol Croat. 2018;26(2):109–118. [PubMed] [Google Scholar]
- 18.Brunasso AM, Puntoni M, Aberer W, et al. Clinical and epidemiological comparison of patients affected by palmoplantar plaque psoriasis and palmoplantar pustulosis: a case series study. Br J Dermatol. 2013;168(6):1243–1251. doi: 10.1111/bjd.12223. [DOI] [PubMed] [Google Scholar]
- 19.Brunasso AM, Massone C. Can we really separate palmoplantar pustulosis from psoriasis? J Eur Acad Dermatol Venereol. 2010;24(5):619–621. doi: 10.1111/j.1468-3083.2010.03648.x. [DOI] [PubMed] [Google Scholar]
- 20.Misiak-Galazka M, Wolska H, Rudnicka L. What do we know about palmoplantar pustulosis? J Eur Acad Dermatol Venereol. 2017;31(1):38–44. doi: 10.1111/jdv.13846. [DOI] [PubMed] [Google Scholar]
- 21.Kubota K, Kamijima Y, Sato T, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015;5(1):e006450. doi: 10.1136/bmjopen-2014-006450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Quaranta M, Eyerich S, Knapp B, et al. Allergic contact dermatitis in psoriasis patients: typical, delayed, and non-interacting. PLoS One. 2014;9(7):e101814. doi: 10.1371/journal.pone.0101814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wahlberg JE, Maibach HI. Sterile cutaneous pustules: a manifestation of primary irritancy? Identification of contact pustulogens. J Invest Dermatol. 1981;76(5):381–383. doi: 10.1111/1523-1747.ep12520895. [DOI] [PubMed] [Google Scholar]
- 24.Nielsen NH, Menné T. Allergic contact dermatitis caused by zinc pyrithione associated with pustular psoriasis. Am J Contact Dermat. 1997;8(3):170–171. [PubMed] [Google Scholar]
- 25.Bangsgaard N, Engkilde K, Thyssen JP, et al. Inverse relationship between contact allergy and psoriasis: results from a patient and a population-based study. Br J Dermatol. 2009;161(5):1119–1123. doi: 10.1111/j.1365-2133.2009.09314.x. [DOI] [PubMed] [Google Scholar]
- 26.Bissonnette R, Suárez-Fariñas M, Li X, et al. Based on molecular profiling of gene expression, palmoplantar pustulosis and palmoplantar pustular psoriasis are highly related diseases that appear to be distinct from psoriasis vulgaris. PLoS One. 2016;11(5):e0158190. doi: 10.1371/journal.pone.0155215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brunasso AMG, Massone C. Palmoplantar pustulosis: epidemiology, clinical features, and diagnosis. [Accessed November 12, 2018]. Available at: http://www.uptodate.com.
- 28.Navarini AA, Burden AD, Capon F, et al. ERASPEN Network. European consensus statement on phenotypes of pustular psoriasis. J Eur Acad Dermatol Venereol. 2017;31(11):1792–1799. doi: 10.1111/jdv.14386. [DOI] [PubMed] [Google Scholar]