Abstract
Mental health crucially depends upon affective states such as emotions, stress responses, impulses and moods. These states shape how we think, feel and behave. Often, they support adaptive functioning. At other times, however, they can become detrimental to mental health via maladaptive affect generation processes and/or maladaptive affect regulation processes. Here, we present an integrative framework for considering the role of affect generation and regulation in mental illness and well‐being. Our model views affect generation as an iterative cycle of attending to, appraising and responding to situations. It views affect regulation as an iterative series of decisions aimed at altering affect generation. Affect regulation decisions include identifying what, if anything, should be changed about affect, selecting where to intervene in the affect generation cycle, choosing how to implement this intervention, and monitoring the regulation attempt to decide whether to maintain, switch or stop it. Difficulties with these decisions, often arising from biased inputs to them, can contribute to manifestations of mental illness such as clinical symptoms, syndromes and disorders. The model has a number of implications for clinical assessment and treatment. Specifically, it offers a common set of concepts for characterizing different affective states; it highlights interactions between affect generation and affect regulation; it identifies assessment and treatment targets among the component processes of affect regulation; and it is applicable to prevention and treatment of mental illness as well as to promotion and restoration of psychological well‐being.
Keywords: Affect, affect regulation, process model, mental illness, well‐being, transdiagnostic mechanisms, psychotherapy
Someone in good mental health enjoys not only freedom from mental illness but also substantial psychological well‐being. As the World Health Organization puts it, “mental health is a state of well‐being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to his or her community”1.
These characteristics of mental health depend, among other things, upon affective states such as emotions, stress responses, impulses and moods. An instance of affect can be viewed as more or less healthy, depending on whether its intensity, duration, frequency or type facilitates or threatens mental health in a given context2, 3. For example, becoming a bit anxious before a job interview can be healthy when it improves motivation and performance. Intense anxiety, by contrast, can be unhealthy when it impairs performance and contributes to avoidance of future social challenges.
Some form of unhealthy affect can be found among the defining features of 40 to 75% of mental disorders2, 4. It is therefore important to understand how affect becomes unhealthy, and what can be done to prevent or treat unhealthy affect. These questions have long been of interest for psychology and psychiatry5. To mention only a few major lines of inquiry, the psychodynamic tradition has related affect to contests between desires and constraints6; the stress and coping tradition has elucidated cognitive antecedents and physiological consequences of affect7, 8; and the affective neuroscience tradition has revealed some of the brain mechanisms underlying affective behaviors9, 10, 11.
The diversity of literature on affect and mental health has resulted in a large number of poorly integrated accounts. For instance, accounts of affect in mental illness12 tend to be separate from accounts of affect in well‐being13. Separate accounts can also be found for similar affective phenomena in different mental illnesses14. Adding to the complexity, different accounts often operate on different levels of analysis, from neurochemical to psychosocial. The fragmented set of explanations for the role of affect in mental health makes it difficult for practitioners and researchers to conceptualize individual cases; to analyze transdiagnostic mechanisms; and to integrate advances from ongoing research.
One way to address these limitations is to construct integrative frameworks that explain different kinds of affect across mental illness as well as well‐being. When seeking to understand how unhealthy affect arises, it is important to realize that, once generated, an emotion, a stress response, an impulse or a mood need not continue to dominate behavior, because people routinely use affect regulation to change these affective states8, 15, 16, 17, 18, 19, 20, 21. Thus, unhealthy affect can result from problematic affect generation, problematic affect regulation, or some combination of the two.
Unhealthy affect may be said to be due to affect regulation failure when affect regulation is not successfully engaged to counteract maladaptive affect generation. Unhealthy affect may be said to be due to affect misregulation when affect regulation aggravates matters by changing affect in a maladaptive direction. Both affect regulation failure and affect misregulation can increase the risk of mental illness as well as hinder psychological well‐being. Conversely, adaptive affect regulation can prevent, reverse or alleviate mental illness as well as promote well‐being.
In this paper, we offer an integrative framework for thinking about the interplay between affect generation and affect regulation in mental health. We focus primarily on mental illness, but the principles we discuss are equally relevant for psychological well‐being. We also focus primarily on affect regulation but, in order to understand how affect can be regulated, we also need to consider how affect is generated.
In the first two sections of the paper, we present the process model of affect regulation, an integrative framework that views affect generation as a four‐stage process that can be altered by another four‐stage process of affect regulation15, 22, 23. In the third section of the paper, we use this framework to identify affect regulation difficulties that contribute to mental illnesses, drawing examples from a variety of symptoms, syndromes and disorders. In the final section, we consider several implications of the process model of affect regulation for clinical assessment and treatment.
AFFECT GENERATION
We use “affect” as an umbrella term to denote emotions such as anxiety or joy; stress responses such as feeling threatened or feeling challenged; impulses such as an urge to flee or to have a drink; and moods such as depression or elation. Despite their differences, what these diverse processes have in common is that they all involve valuation – a good‐for‐me vs. bad‐for‐me distinction – that can shape behavior15, 24, 25, 26, 27. For instance, anxiety, feeling threatened, an urge to flee, and depression all signal that something is unpleasant and worth avoiding. Joy, feeling challenged, an urge to drink, and elation all signal that something is pleasant and worth approaching. Valuation reflects what a situation has to offer in relation to what the individual values, needs or wants. The function of affective states is therefore to shape behavior in accordance with the relationship between situation and motivational concerns.
Given their shared function, affective states can be analyzed using common concepts. Following a cybernetic approach15, 28, 29, 30, we view affect as a series of iterative cycles comprising four stages: a) a situation that can be experienced or imagined; b) attention that shapes how the situation is perceived; c) appraisal of the situation in light of motivational concerns; and d) a response to the situation that can entail changes in subjective experience, physiology, and/or facial or whole‐body behavior (see Figure 1). For instance, an emotion of anxiety may arise when a person experiences or imagines a job interview (situation); pays attention to what could go wrong (attention); appraises the situation as threatening (appraisal); and feels anxious, starts to sweat, and wishes to flee (response).
Figure 1.
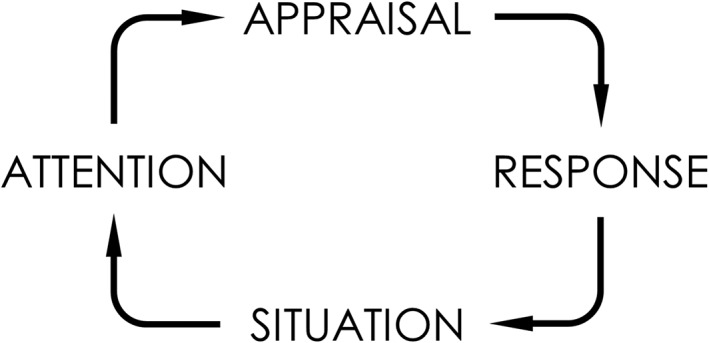
Affect generation. Different affective states such as emotions, stress responses, impulses and moods can be viewed as iterative cycles of attending to, appraising and responding to situations.
The affective responses generated on one iteration of this feedback loop may become part of the situation stage of a subsequent iteration. For instance, the person may now realize that he is being interviewed while anxious and perspiring (situation), fixate on increased chances of failure (attention), appraise the situation as even more threatening (appraisal), and experience even stronger anxiety (response). Successive iterations of the affect generation loop can produce increasingly selective attention, elaborate appraisals, and specific responses.
We suggest that the same four iterative stages are involved in different kinds of affective states, although the stages can differ in their automaticity, specificity, duration, and other features. One way to organize different affective states within this framework is to place them on a continuum based on how many affect generation stages are generally part of the conscious experience of the given affective state.
At one end of this continuum are emotions, where all four stages are generally part of the experience. Emotions such as anxiety or joy tend to involve strong feelings directed at a situation that commands attention and is at least in part consciously appraised27, 31.
At the other end of the continuum are moods such as depression or elation, that tend to be experienced as diffuse feelings and action tendencies (i.e., only the response stage). We argue that the remaining affect generation stages play a role in moods outside of conscious awareness. Thus, moods tend to relate to situations that have been selectively perceived and appraised largely outside of awareness32, 33.
Between emotions and moods in the continuum are stress responses and impulses. Stress responses, such as feeling threatened or feeling challenged8, 34, resemble emotions in that the attention, appraisal and response stages are usually part of the experience. However, instead of a single identifiable situation, these experiences revolve around broader circumstances, such as a divorce or a new job, that span several specific situations.
Impulses, such as an urge to flee or to have a drink, can be viewed as affective states experienced as a constellation of the response and the situation stages. Impulses can feel almost like reflexes – strong action tendencies (i.e., response stage) elicited by some threat or opportunity (i.e., situation stage)17. We argue that the intermediate stages of selectively perceiving and appraising the situation are often operative in impulses, albeit outside awareness.
The four‐stage model of affect generation is a flexible way to appreciate both commonalities and differences among different kinds of affective states. Importantly for current purposes, the model also suggests that unhealthy affect can be traced back to maladaptive unfolding of one or more of the four affect generation stages. Sometimes, unhealthy affect arises simply due to a maladaptive situation, such as being a victim of violence. When unhealthy affect arises from otherwise adaptive situations, however, it may be because of maladaptive unfolding of attention, appraisal or response stages of affect generation. For instance, the mental health consequences of maladaptive attention are illustrated by the role of attention biases in mood and anxiety disorders35, 36. The consequences of maladaptive appraisal are illustrated by the role of interpretation biases in people with depressive symptoms37. The consequences of maladaptive affective responses are illustrated by the role of low physiological reactivity in externalizing syndromes such as sociopathy38.
Maladaptive affect generation is therefore an important part of a comprehensive account of unhealthy affect. However, in this paper, our primary focus is affect regulation. This is because maladaptive affect generation manifests in unhealthy affect mostly when affect regulation fails to neutralize – or even further aggravates – the maladaptive affect.
AFFECT REGULATION
Affect regulation involves intentional (but not necessarily conscious) attempts to change the intensity, duration, frequency or type of current or anticipated affect39. We focus in this paper on self‐generated or intrinsic affect regulation, which can be distinguished from other‐generated or extrinsic affect regulation40, 41. The latter – which involves one person's attempt to regulate the affective states of another person – is also important for mental health, but falls beyond the scope of this paper.
Mirroring the four kinds of affective states distinguished earlier, we may distinguish four kinds of affect regulation: a) emotion regulation15, 16, 42; b) regulation of stress, i.e. coping8, 43; c) regulation of impulses, i.e. self‐regulation17, 44; and d) mood regulation18, 45. Even though the type of affect targeted by regulation can be important to distinguish, our analysis of common mechanisms of affect generation suggests that there are also common mechanisms of affect regulation.
The process model of affect regulation highlights these shared mechanisms by addressing two fundamental questions: a) how can affect be regulated (strategies), and b) what processes underlie affect regulation (stages).
Affect regulation strategies
To understand how affect can be regulated, it is useful to return to the four stages of the affect generation loop outlined in Figure 1. Given the stages of situation, attention, appraisal and response, we can distinguish four families of affect regulation strategies, based on which affect generation stage they primarily influence (see Figure 2).
Figure 2.
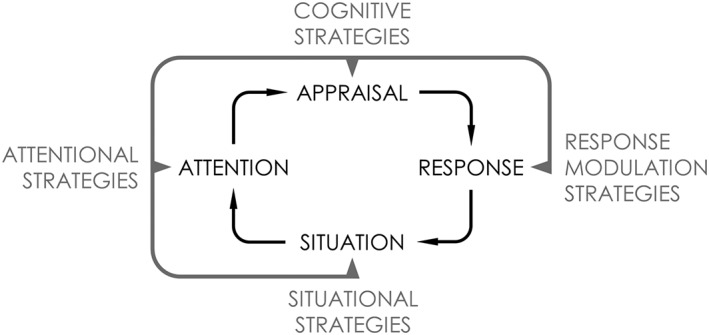
Affect regulation strategies. Four families of affect regulation strategies can be distinguished based on which stage of affect generation they primarily seek to alter.
Situational strategies seek to alter affect generation at the situation stage, by selecting which situations are encountered (situation selection) or modifying what is going on in them (situation modification)44. For instance, people wishing to lift their depressed mood may call a friend (situation selection) or guide an already ongoing conversation to uplifting topics (situation modification).
Attentional strategies seek to alter affect generation at the attention stage, by changing what aspects of the situation are attended to46. For instance, the person experiencing depressed mood may distract himself from negative thoughts by diverting his attention to a game such as Tetris.
Cognitive strategies seek to alter affect generation at the appraisal stage, by modifying how the situation is viewed in light of goals, values, and other motivational concerns47. For instance, depressed mood could be fought off by considering how things are not as bad as they initially seemed.
Finally, response modulation strategies seek to alter affect at the response stage, by counteracting the affect‐related experiential, behavioral or physiological changes. For instance, the person experiencing depressed mood may prepare a cup of coffee to energize his body.
In addition to mood regulation, the same strategy families have been found to be relevant for regulating emotions42, stress22 as well as impulses44, 48.
Each of the four broad ways of changing affect can be effective, but each has different costs and benefits49, 50. For instance, strategies that intervene early in the affect generation cycle can provide powerful relief from the affective state51, but this may come at the cost of limited learning52, 53. As researchers have identified different costs and benefits of regulation strategies, it has become clear that adaptive affect regulation requires matching strategies to the characteristics of the affect being regulated, the individual, and the current context54, 55, 56. For instance, in a context where a frustrating situation can be improved, it is sensible to try to change the situation rather than to use cognitive strategies to change how the situation is appraised. By contrast, in a context where nothing much could be done to improve the situation, it is sensible to use cognitive rather than situational strategies57, 58, 59.
Affect regulation stages
If deciding how to best regulate affect appears such a complex task, how is it accomplished? The process model of affect regulation addresses this question by envisioning a series of four stages: identification, selection, implementation and monitoring (see Figure 3). Each stage can be thought of as a decision that the person makes, consciously or otherwise60, 61. Returning to the example of the person experiencing depressed mood, what decisions does he need to make to regulate his mood?
Figure 3.
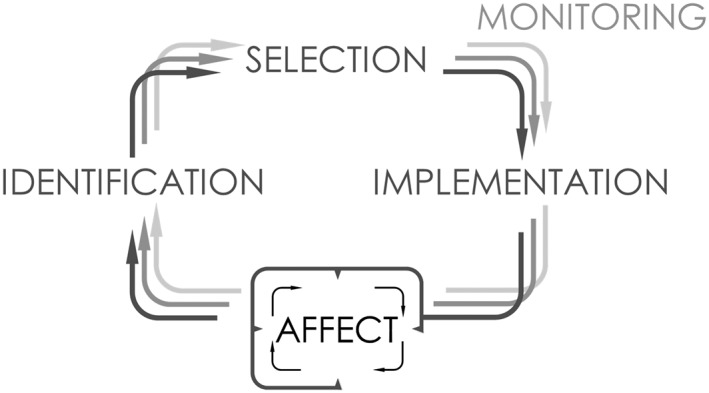
Affect regulation stages. Affect regulation consist of key decisions that people make, consciously or otherwise, during four stages. At the identification stage, people decide what, if anything, should change about affect. At the selection stage, they decide which affect regulation strategy to use in service of that goal. At the implementation stage, they decide which actions to take as part of the chosen strategy to alter the affect generation process. The monitoring stage consists of iterative updates to the identification, selection and implementation decisions that amounts to a separate decision about whether ongoing efforts should be maintained, switched or stopped.
First, at the identification stage, he needs to decide that his current mood should be improved. This decision then activates the selection stage, where he needs to decide which affect regulation strategy to use (i.e., where to intervene in the affect generation cycle). For instance, he may select an attentional strategy to keep his mind off ruminative thoughts. Strategy selection triggers the implementation stage, where the person needs to decide which specific actions to take. For instance, he may play a game of Tetris.
As the chosen actions intervene in affect generation, all three decisions may need to be updated – whether the affect continues to require regulation, whether an attentional strategy continues to be the best strategy, and whether playing Tetris continues to be the best course of action. The continued iteration of the three decisions can be thought of as a separate monitoring stage of affect regulation, where the person needs to decide whether to maintain, switch or stop the ongoing affect regulation attempt.
To better understand the identification, selection, implementation and monitoring stages, it is helpful to consider what information is processed to reach the decisions required at each stage. The process model of affect regulation suggests that each stage makes use of two main inputs, and we now turn to describing the role that these inputs play in each of the four stages.
The identification decision of what, if anything, should change about affect (i.e., what is the regulation goal) relies on: a) a representation of the current affective state together with alternative states, and b) the evaluation of the costs and benefits of these states in the given context.
The first input to the identification decision thus requires representing ongoing affective states together with other states that the person could experience in the given situation. The importance of this input is illustrated by the finding that people who are good at detecting and labelling their affective states tend to also be good at affect regulation62, 63.
The second input to the identification decision consists of the evaluation of the current and alternative affective states based on their costs and benefits. Most of the time, people evaluate affective states in light of the hedonic motive to increase pleasant feelings and decrease unpleasant feelings. However, people can also make counter‐hedonic (i.e., instrumental) evaluations, for instance when they wish to be angrier than they currently are because they believe that this will help them negotiate64.
When the identification stage is working well, the person detects the current affective state together with alternatives, evaluates them appropriately, and decides (consciously or otherwise) what, if anything, should change about the current affective state.
A decision to change affect triggers the selection stage, at which point the person decides where to intervene in affect generation (i.e., which regulation strategy to use). The selection decision relies on: a) a representation of available regulation strategies, and b) the evaluation of the costs and benefits of these strategies in the given context.
The availability of strategies can vary between situations as well as individuals. For instance, cognitive strategies are more likely to be considered in situations that have multiple interpretations65. Different individuals may consider different strategies based on their skills and abilities. For instance, attentional strategies work better for people with relatively high working memory capacity66, suggesting that they are more likely to consider these strategies as a viable regulation option.
The second input to the selection decision is the evaluation of costs and benefits of available strategies67. One major benefit of each available strategy is its expected efficacy to change affect. For instance, when attempting to downregulate intense emotions, people tend to prefer distraction (an attentional strategy) over reappraisal (a cognitive strategy), because the former is believed to be more effective67. Some of the major costs include the time and effort needed to use the strategy68. Other costs and benefits, more specific to different strategies, individuals and contexts, also help to shape the eventual choice of strategy.
When the selection stage is working well, the person represents available strategies, evaluates them appropriately, and decides which regulation strategy to use.
The selection decision triggers the implementation stage, where the person decides how to enact the selected strategy in the given context. This stage is needed because the broad strategies of intervening at one of the four stages of affect generation can be enacted in different ways69, sometimes referred to as regulation tactics. For instance, having made an identification decision to lift depressed mood, and a selection decision to rely on attentional strategies, the person may decide to play Tetris as a way to get his mind off his negative thoughts. Such an implementation decision relies on: a) a representation of different actions afforded by the situation, and b) the evaluation of the costs and benefits of these actions in the given context.
The implementation stage is where the regulation process reaches its target, as specific mental or physical actions impact the affect generation process (see Figure 3). For instance, playing Tetris diverts cognitive resources away from the attention stage involved in generating depressed mood.
When the implementation stage is working well, the person represents actions afforded by the specific context, evaluates them appropriately, and decides how to enact the regulation attempt.
The identification, implementation and selection decisions form an iterative cycle. As the strategy selected to serve the identified regulation goal is implemented, each of these decisions may need to be updated to mirror changes in the regulated affect as well as in the broader context. Iterative updates to the affect regulation decisions can be viewed as a separate monitoring stage, involving a decision to either maintain, switch or stop the regulation attempt. Inputs to this decision include: a) changes in affect, which can be spontaneous as well as caused by ongoing regulation, and b) changes in context.
As long as the regulation attempt continues to produce desired changes to affect, and the context also does not change substantially, the person can maintain regulation by relying on the latest identification, selection and implementation decisions (e.g., play Tetris to fend off rumination in order to lift depressed mood). However, if affect resists change, or changes in undesired ways, the chosen implementation, strategy or regulation goal can be switched, or the regulation attempt can be stopped altogether. Switching or stopping may also be mandated by a change in context, such as when a friend calls in the middle of the Tetris game.
To be adaptive, affect regulation should respond with optimal flexibility to changes in affect as well as in context43, 55. Not enough flexibility can lead to overuse of certain affect regulation behaviors, whereas too much flexibility can lead to lack of persistence.
When the monitoring stage is working well, the person appropriately represents ongoing changes in affect as well as in context, and decides to maintain, switch or stop regulation accordingly.
MALADAPTIVE AFFECT REGULATION AND MENTAL ILLNESS
The process model of affect regulation outlined in the previous sections can be helpful for considering how maladaptive affect regulation can contribute to mental illness. The identification, selection, implementation and monitoring decisions can be considered maladaptive when they are misaligned with the targeted affective state, the current motives of the person, and/or contextual demands54, 55, 56. In this section, we consider how each of these decisions can become maladaptive. We use selective examples of manifestations of mental illness such as different symptoms, syndromes and disorders. Note that, even when we discuss a particular mechanism in relation to a particular manifestation, we do not intend to imply that a given manifestation could not be related to other mechanisms nor that a given mechanism could not be involved in other manifestations of mental illness.
Identification difficulties
Unhealthy affect may arise from the identification stage of affect regulation when the decision of what, if anything, should change about an affective state is maladaptive. This can happen when a person encounters difficulty with at least one of the inputs to the identification decision, i.e., by misrepresenting affective states and/or misevaluating their costs and benefits.
The first kind of difficulty is characteristic of individuals high on trait alexithymia, who struggle to attend to and accurately identify their affective experiences70. Compared to healthy controls, these individuals have been found to engage in maladaptive affect regulation patterns71 which may arise from the low granularity with which they represent affect. Alexithymia is also common among individuals with mental illnesses such as autism spectrum disorder72 or eating disorders73, suggesting that the unhealthy affect characterizing these mental illnesses may also arise in part from misrepresented affective states.
The second difficulty associated with the identification stage involves misevaluation of the costs and benefits of either the current affective state or alternative states that could be experienced. For example, people with panic disorder tend to overestimate the costs of current anxiety74. They may interpret a normal anxiety‐related increase in heart rate as a sign of imminent heart failure, or anxiety‐related thoughts as a sign of imminent loss of their grip on reality. Such overestimation of costs of affect can produce a maladaptive identification decision to launch an unnecessary regulation attempt. In addition to costs, people can also misestimate the benefits of affective states. For instance, individuals with bipolar disorder often choose not to downregulate maladaptive positive affect, even though they are able to do so when instructed75. One reason may be that individuals with bipolar disorder overvalue the hedonic benefits of positive affective states at the expense of the costs of these states as well as the benefits of alternative states76.
Selection difficulties
Unhealthy affect may arise from the selection stage of affect regulation when the decision about which regulation strategy to use in order to accomplish the regulation goal is maladaptive. This can happen when a person encounters difficulty with at least one of the inputs to this decision, i.e., by misrepresenting available strategy options and/or misevaluating the costs and benefits of these strategies.
One reason for misrepresenting available strategies may be that the person has limited skills or experiences with different strategies. For instance, people with alcohol use disorder may struggle to consider strategies other than consuming alcohol, which they are most familiar with77. A similar limitation may characterize individuals suffering from binge eating disorder, who often engage in unhealthy eating patterns for affect regulatory purposes78.
Another way the selection stage may contribute to unhealthy affect is via difficulties with evaluating the costs and benefits of different strategies. Many mental illnesses are associated with misevaluation of maladaptive regulation strategies. For example, engagement in non‐suicidal self‐injury relies in part on the evaluation of this costly behavior as an effective affect regulation strategy79, 80. People with generalized anxiety disorder meanwhile view worry, another strategy with negative consequences, as productive (e.g., “Worrying helps me to be prepared and avoid adversities”) or as an indicator of good character (e.g., “Worrying means that I care”)83.
Difficulties with the cost‐benefit analysis of strategy options may also arise from more general decision biases. For instance, a broad range of mental illnesses are associated with amplified temporal discounting, whereby immediate outcomes are overvalued relative to long‐term outcomes even more than in healthy populations81. Amplified discounting can bias affect regulation strategy selection towards underestimating long‐term costs and benefits relative to short‐term ones. For instance, people with social anxiety disorder tend to choose behavioral avoidance to reduce anxiety despite it severely restricting social or professional outlooks for the future82.
Implementation difficulties
Unhealthy affect may arise from the implementation stage of affect regulation when the decision about how to enact the selected strategy in a given situation is maladaptive. This can happen when a person encounters difficulty with at least one of the inputs to this decision, i.e., by misrepresenting available affordances for action and/or misevaluating their costs and benefits.
The first difficulty may arise when a person fails to consider action affordances beyond obvious ones suggested by habit and the environment. For instance, someone looking for ways to implement a situational strategy for increasing excitement may fail to consider options beyond watching the TV that happens to be in the room. Detecting less obvious action affordances often requires cognitive control84, a set of processes that tends to be impaired across a range of mental illnesses85. Cognitive control impairments are particularly relevant in attention‐deficit/hyperactivity disorder (ADHD)86, which is also characterized by maladaptive affect regulation87. Our analysis suggests that maladaptive affect regulation in ADHD may stem, among other pathways, from difficulties to detect less obvious regulation tactics.
Another difficulty encountered at the implementation stage is the misevaluation of costs and benefits of different action affordances. This suggests that mental illnesses that impair predictions about action outcomes, such as major depressive disorder88, 89, may contribute to maladaptive affect regulation by making it harder to appropriately evaluate action affordances even if they are detected. For instance, a person may come up with more ways than watching TV to implement an attentional strategy to feel more excited, but then fail to consider some of their outcomes, leading to a maladaptive choice. According to the present framework, one mechanism through which affect regulation becomes maladaptive in people with depressive symptoms90 may therefore involve misevaluation of the action affordances that have been detected during the affect regulation process.
Monitoring difficulties
Unhealthy affect may arise from the monitoring stage of affect regulation, when the decision to maintain, switch or stop regulation is maladaptive. This can happen when the person encounters difficulties with at least one of the inputs to this decision, i.e., by misrepresenting changes to the regulated affect and/or to the relevant context. As the consequences of these difficulties are quite similar, we will not distinguish between them. Instead, we consider two directions of misrepresentations – under‐representing changes in affect or context that contributes to insufficient regulation flexibility, and over‐representing changes in affect or context that contributes to too high regulation flexibility55.
Insufficient flexibility can lead to unnecessary maintenance of regulation efforts that have already succeeded or are unlikely to succeed. Such inertia in regulation has been observed for numerous mental illnesses. For example, people with generalized anxiety disorder continue to worry despite it elevating anxiety and being cognitively costly91, 92. Similarly, people with major depressive disorder continue to ruminate despite it increasing rather than decreasing depressed mood93.
At the other extreme, the monitoring decision can become overly flexible when changes in affect or context are over‐represented. This difficulty can manifest in premature switches between strategies and their implementation before they have had a chance to become effective, or premature stopping of regulation altogether55. For instance, borderline personality disorder is characterized both by frequent shifts in affective states94 as well as high levels of impulsivity95. This suggests that one reason for the affective lability in individuals suffering from borderline personality disorder may be insufficient persistence in applying affect regulation, i.e. overly high affect regulation flexibility.
IMPLICATIONS FOR ASSESSMENT AND TREATMENT
Assessment and treatment of unhealthy affect is central to a number of psychotherapeutic approaches, including cognitive‐behavioral therapy96, dialectical‐behavioral therapy97, acceptance and mindfulness‐based interventions98, 99, 100, 101, emotion‐focused therapy102, affect regulation training103, and emotion regulation therapy104. The present framework complements these approaches by offering four broad insights that have implications for clinical assessment as well as treatment.
First, the framework suggests that problems with different affective states, such as emotions, stress responses, impulses and moods, can be analyzed in common terms. Second, unhealthy affect usually arises from some combination of maladaptive affect generation and maladaptive affect regulation. Third, maladaptive affect regulation can arise from identification, selection, implementation and monitoring decisions. Finally, affective processes are equally relevant for mental illness and psychological well‐being. In this final section, we briefly discuss the assessment and treatment implications of each of these insights.
Common concepts for different affective states
Emotions, stress responses, impulses and moods have often been studied as separate phenomena, leading to separate assessment instruments and treatment approaches. Without denying instances where such distinctions are useful, the process model of affect regulation suggests that is also reasonable to focus on the similarities rather than differences between affective states.
The framework highlights the iterative stages of situation, attention, appraisal and response, and the ways to regulate them, as a set of concepts that are sufficiently broad to capture different affective states. For instance, take a problematic affect such as generalized anxiety, that is experienced as a diffuse feeling with variable awareness of the situation, attention and appraisal stages of affect generation. Working with a client reporting this affective pattern, a clinician may seek to reveal the contents of these antecedent stages105. What are the situational triggers for these states? Are there selective perceptual processes involved? How is the selectively perceived situation appraised? Even though the client may initially lack awareness of these stages, he may provide reliable information through interviewing techniques such as behavioral chain analysis97. Relevant information may also be obtained through daily assessment techniques that can recover aspects of situations and cognitions that tend to be less available at later recall106.
Focusing on similarities between different affective states can also be useful for selecting and tailoring treatments for specific clients. For example, borrowing an insight from systematic desensitization107, a therapist may develop a hierarchy of affective states based on how difficult they are for a client to regulate. For instance, a client may resist unhealthy food with ease, downregulate his anger with moderate success, but almost never overcome a bout of depressed mood. The therapist could incorporate this hierarchy into a program of guided affect regulation practice that introduces different regulation techniques using assignments from the lower end of the hierarchy and gradually moving upwards. For instance, a client could first foster healthier eating habits through situation modification by putting healthy snacks in easily accessible locations. He may then use this experience as a helpful metaphor for finding ways to use situation modification to improve his depressed mood.
Interplay of affect generation and regulation
The process model of affect regulation suggests that the same manifestation of unhealthy affect may arise from different mixtures of maladaptive affect generation and maladaptive affect regulation2.
On the one hand, this suggests that affect generation and affect regulation form an integrated dynamic system that can be analyzed as a single functional unit. For instance, for many clinical purposes, such as initial screening for affective disturbances, it is largely unimportant whether a problematic affective pattern reflects overly strong affect generation or overly weak affect regulation. On the other hand, the process model also exemplifies the value of separating the contributions of affect generation and regulation to unhealthy affect. Teasing these contributions apart can be challenging, as the client may have limited awareness of the functioning of different affective processes. The interviewing techniques discussed above may be adapted to this task. In addition, the research community has started to devise promising combinations of self‐report, behavioral and statistical approaches for separating affect generation from affect regulation39.
Differentiating affect generation from affect regulation can also be important for designing targeted treatments. In many cases, people suffer from a combination of maladaptive affect generation and maladaptive affect regulation, and thus benefit from simultaneous – or sensibly sequenced – treatments targeting both. For instance, in the case of major depressive disorder, pharmacological interventions can be used to treat maladaptive affect generation, while psychotherapy can be used to improve affect regulation108. Omitting one or the other component from the treatment regime would reduce its overall efficacy. There can also be cases where the unhealthy affective pattern can be traced back to a single primary source among affect generation and affect regulation processes. In these instances, adequate targeting of treatment becomes even more important. For instance, consider a client who is already relatively proficient in affect regulation but suffers primarily from maladaptive affect generation. If offered only further affect regulation training, with no help with maladaptive generation, he might experience reduced self‐efficacy that could lead to deterioration of the therapeutic relationship and treatment compliance.
Decomposing affect regulation
The third implication of the process model of affect regulation is that the stages of identification, selection, implementation and monitoring, and their respective inputs, can be used as more specific targets for assessment as well as treatment.
For instance, an assessment approach could be designed to determine difficulties with identifying regulation goals, selecting regulation strategies, implementing them through contextually suitable actions, and monitoring the outcomes to make necessary modifications. Parts of these phenomena can be assessed using existing self‐report instruments, such as the Toronto Alexithymia Scale109, the Emotion Regulation Questionnaire110, the Cognitive Emotion Regulation Questionnaire111, the Difficulties in Emotion Regulation Scale112, the Coping Flexibility Scale113, and many others. However, as these measures assess overlapping but incomplete aspects of the four affect regulation stages, we encourage future efforts to design comprehensive measures of the process model of affect regulation. These efforts may extend beyond self‐reports to behavioral and psychophysiological assessments such as measuring affective responses to standardized stimuli using physiological correlates under specific instructions114.
Clarifying whether a particular affect regulation problem arises from difficulties during the identification, selection, implementation or monitoring stage can be an important step toward making informed decisions about personalized treatment options. For instance, people who exhibit difficulties during the identification stage due to misrepresentation of current affective states might benefit from mindfulness‐based therapy modules and technological aids. People who exhibit difficulties during the selection stage might benefit from learning new adaptive strategies, from increasing strategy specific self‐efficacy, as well as from modification of dysfunctional beliefs contributing to misevaluation of strategies. People who struggle with the implementation stage might benefit from external aids such as mobile applications with suggestions on how to execute different strategies. People who struggle with the monitoring stage might benefit from mindfulness interventions to increase awareness about changes in the affective state and context as well as training to switch between strategies according to changing circumstances. In most cases, individual clients may exhibit difficulties with more than one, but not necessarily all, decisions involved in affect regulation.
From mental illness to well‐being
Although this paper has focused primarily on mental illness, the process model of affect regulation is equally relevant when considering the role of affect in psychological well‐being115. The goals of psychiatry and clinical psychology extend from preventing and reversing maladaptive affect generation and regulation patterns to promoting and restoring their adaptive counterparts. To live up to this ideal, assessment as well as treatment approaches should be designed without forgetting about healthy affect. For instance, assessment approaches should target affective states that are known to improve well‐being. These include hedonically positive experiences such as satisfaction, happiness or love, as well as affective states that can be hedonically negative but still add eudaimonic value by providing meaning, elevating experiences, or fostering personal growth116.
Psychological well‐being is equally relevant for designing interventions. We have seen how the process model of affect regulation can be used to organize regulation techniques aimed at reducing hedonically negative (e.g., depressed mood) and instrumentally harmful affective states (e.g., maladaptive positive affect in bipolar disorder). However, the process model is an equally useful framework for organizing techniques that promote hedonically positive or instrumentally helpful affective states. For instance, situational strategies such as going for hike can be used to generate pleasant mood117. Attentional strategies such as focusing on things that a person is grateful for can be used to promote happiness and a sense of meaning118. Cognitive strategies such as contrasting a mental image of a job well done with the current situation where more work is needed can be used to promote feeling challenged and thereby more motivated119. Response modulation strategies such as exercising can be used to generate feelings of being relaxed and fulfilled120. Promoting each of these behaviors can further benefit from analyzing their antecedents within the identification, selection, implementation and monitoring stages.
CONCLUSIONS
We have proposed a process model of affect regulation as a common framework for understanding how affect is generated, how it can be regulated, and how both processes jointly contribute to mental health. This framework conceives of affect generation as a four‐stage feedback loop, and affect regulation as a coordinated four‐stage decision process. Adaptive functioning of each of these stages promotes mental health and well‐being, whereas maladaptive functioning of these stages can increase the risk of mental illness.
We believe that the process model of affect regulation offers a useful framework for clinical research as well as practice. The model is in line with broader efforts to reveal the transdiagnostic dimensions underlying mental illnesses14, 121. It relates complex affective patterns to simple psychological mechanisms such as feedback loops29 and decision processes122, 123, which are amenable for computational and neural research.
The model calls for more research, in particular to realize the assessment and treatment avenues it opens up. On the one hand, it is important to provide further evidence that different symptoms, syndromes and disorders are indeed linked to difficulties in different affect generation and affect regulation stages. On the other hand, it is also important to clarify how existing treatments impact these stages as well as to devise novel treatments.
We hope that, by facilitating and scaffolding these important advances, the process model of affect regulation can contribute to the advancement of evidence‐based personalized psychiatry and psychotherapy.
ACKNOWLEDGEMENT
This work was supported by the Estonian Research Council grants IUT2‐13, PUTJD‐79, and MOBTP‐17.
REFERENCES
- 1. World Health Organization . Strengthening mental health promotion. Geneva: World Health Organization, 2001. [Google Scholar]
- 2. Gross JJ, Jazaieri H. Emotion, emotion regulation, and psychopathology: an affective science perspective. Clin Psychol Sci 2014;2:387‐401. [Google Scholar]
- 3. Gross JJ, Muñoz RF. Emotion regulation and mental health. Clin Psychol Sci Pract 1995;2:151‐164. [Google Scholar]
- 4. Jazaieri H, Urry HL, Gross JJ. Affective disturbance and psychopathology: an emotion regulation perspective. J Exp Psychopathol 2013;4:584‐99. [Google Scholar]
- 5. Kring AM, Sloan DM. (eds). Emotion regulation and psychopathology: a transdiagnostic approach to etiology and treatment. New York: Guilford, 2010. [Google Scholar]
- 6. Freud S. Inhibitions, symptoms and anxiety. In: Strachey J, Freud A. (eds). The standard edition of the complete psychological works of Sigmund Freud. London: Hogarth Press, 1926:77‐175. [Google Scholar]
- 7. Godoy LD, Rossignoli MT, Delfino‐Pereira P et al. A comprehensive overview on stress neurobiology: basic concepts and clinical implications. Front Behav Neurosci 2018;12:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer, 1984. [Google Scholar]
- 9. Etkin A, Büchel C, Gross JJ. The neural bases of emotion regulation. Nat Rev Neurosci 2015;16:693‐700. [DOI] [PubMed] [Google Scholar]
- 10. Harrison NA, Critchley HD. Affective neuroscience and psychiatry. Br J Psychiatry 2007;191:192‐4. [DOI] [PubMed] [Google Scholar]
- 11. Panksepp J. Affective neuroscience: the foundations of human and animal emotions. New York: Oxford University Press, 1998. [Google Scholar]
- 12. Kring AM. Emotion disturbances as transdiagnostic processes in psychopathology In: Lewis M, Haviland‐Jones JM, Feldman Barrett L. (eds). Handbook of emotions, Vol. 3, 3rd ed New York: Guilford, 2008:691‐705. [Google Scholar]
- 13. Donaldson SI, Dollwet M, Rao MA. Happiness, excellence, and optimal human functioning revisited: examining the peer‐reviewed literature linked to positive psychology. J Posit Psychol 2015;10:185‐95. [Google Scholar]
- 14. Krueger RF, Kotov R, Watson D et al. Progress in achieving quantitative classification of psychopathology. World Psychiatry 2018,17:282‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gross JJ. Emotion regulation: current status and future prospects. Psychol Inq 2015;26:1‐26. [Google Scholar]
- 16. Koole SL. The psychology of emotion regulation: an integrative review. Cogn Emot 2009;23:4‐41. [Google Scholar]
- 17. Kotabe HP, Hofmann W. On integrating the components of self‐control. Perspect Psychol Sci 2015;10:618‐38. [DOI] [PubMed] [Google Scholar]
- 18. Larsen RJ. Toward a science of mood regulation. Psychol Inq 2000;11:129‐41. [Google Scholar]
- 19. Parkinson B, Totterdell P. Classifying affect‐regulation strategies. Cogn Emot 1999;13:277‐303. [Google Scholar]
- 20. Webb TL, Schweiger Gallo I, Miles E et al. Effective regulation of affect: an action control perspective on emotion regulation. Eur Rev Soc Psychol 2012;23:143‐86. [Google Scholar]
- 21. Westen D. Toward an integrative model of affect regulation: applications to social‐psychological research. J Pers 1994;62:641‐67. [Google Scholar]
- 22. O'Leary D, Suri G, Gross JJ. Reducing behavioural risk factors for cancer: an affect regulation perspective. Psychol Health 2018;33:17‐39. [DOI] [PubMed] [Google Scholar]
- 23. Sheppes G, Suri G, Gross JJ. Emotion regulation and psychopathology. Annu Rev Clin Psychol 2015;11:379‐405. [DOI] [PubMed] [Google Scholar]
- 24. Carruthers P. Valence and value. Philos Phenomenol Res 2018;97:658‐80. [Google Scholar]
- 25. Lang PJ. Emotion and motivation: toward consensus definitions and a common research purpose. Emot Rev 2010;2:229‐33. [Google Scholar]
- 26. Russell J. Core affect and the psychological construction of emotion. Psychol Rev 2003;110:145‐72. [DOI] [PubMed] [Google Scholar]
- 27. Scherer KR. What are emotions? And how can they be measured? Soc Sci Inf 2005;44:695‐729. [Google Scholar]
- 28. Carver CS. Control processes, priority management, and affective dynamics. Emot Rev 2015;7:301‐7. [Google Scholar]
- 29. Pezzulo G, Cisek P. Navigating the affordance landscape: feedback control as a process model of behavior and cognition. Trends Cogn Sci 2016;20:414‐24. [DOI] [PubMed] [Google Scholar]
- 30. Uusberg A, Suri G, Dweck CS et al. Motivation: a valuation systems perspective. Nebr Symp Motiv (in press). [Google Scholar]
- 31. Frijda NH. Emotion experience and its varieties. Emot Rev 2009;1:264‐71. [Google Scholar]
- 32. Siemer M. Mood experience: implications of a dispositional theory of moods. Emot Rev 2009;1:256‐63. [Google Scholar]
- 33. Trimmer PC, Paul ES, Mendl MT et al. On the evolution and optimality of mood states. Behav Sci 2013;3:501‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kemeny ME. The psychobiology of stress. Curr Dir Psychol Sci 2003;12:124‐9. [Google Scholar]
- 35. Cisler JM, Koster EHW. Mechanisms of attentional biases towards threat in anxiety disorders: an integrative review. Clin Psychol Rev 2010;30:203‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Leppänen JM. Emotional information processing in mood disorders: a review of behavioral and neuroimaging findings. Curr Opin Psychiatry 2006;19:34‐9. [DOI] [PubMed] [Google Scholar]
- 37. Everaert J, Podina IR, Koster EHW. A comprehensive meta‐analysis of interpretation biases in depression. Clin Psychol Rev 2017;58:33‐48. [DOI] [PubMed] [Google Scholar]
- 38. Lorber MF. Psychophysiology of aggression, psychopathy, and conduct problems: a meta‐analysis. Psychol Bull 2004;130:531‐52. [DOI] [PubMed] [Google Scholar]
- 39. Gross JJ, Sheppes G, Urry HL. Emotion generation and emotion regulation: a distinction we should make (carefully). Cogn Emot 2011;25:765‐81. [DOI] [PubMed] [Google Scholar]
- 40. Reeck C, Ames DR, Ochsner KN. The social regulation of emotion: an integrative, cross‐disciplinary model. Trends Cogn Sci 2016;20:47‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zaki J, Williams WC. Interpersonal emotion regulation. Emotion 2013;13:803‐10. [DOI] [PubMed] [Google Scholar]
- 42. Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol 1998;2:271‐99. [Google Scholar]
- 43. Bonanno GA, Burton CL. Regulatory flexibility: an individual differences perspective on coping and emotion regulation. Perspect Psychol Sci 2013;8:591‐612. [DOI] [PubMed] [Google Scholar]
- 44. Duckworth AL, Gendler TS, Gross JJ. Situational strategies for self‐control. Perspect Psychol Sci 2016;11:35‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Davidson RJ, Lewis DA, Alloy LB et al. Neural and behavioral substrates of mood and mood regulation. Biol Psychiatry 2002;52:478‐502. [DOI] [PubMed] [Google Scholar]
- 46. Ochsner KN, Gross JJ. The cognitive control of emotion. Trends Cogn Sci 2005;9:242‐9. [DOI] [PubMed] [Google Scholar]
- 47. Uusberg A, Taxer JL, Yih J et al. Reappraising reappraisal. Emot Rev (in press). [Google Scholar]
- 48. O'Leary D, Uusberg A, Gross JJ. Identity and self‐control: linking identity‐value and process models of self‐control. Psychol Inq 2017;28:132‐8. [Google Scholar]
- 49. Morawetz C, Bode S, Derntl B et al. The effect of strategies, goals and stimulus material on the neural mechanisms of emotion regulation: a meta‐analysis of fMRI studies. Neurosci Biobehav Rev 2017;72:111‐28. [DOI] [PubMed] [Google Scholar]
- 50. Webb TL, Miles E, Sheeran P. Dealing with feeling: a meta‐analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychol Bull 2012;138:775‐808. [DOI] [PubMed] [Google Scholar]
- 51. Sheppes G, Gross JJ. Is timing everything? Temporal considerations in emotion regulation. Personal Soc Psychol Rev 2011;15:319‐31. [DOI] [PubMed] [Google Scholar]
- 52. Paul S, Kathmann N, Riesel A. The costs of distraction: the effect of distraction during repeated picture processing on the LPP. Biol Psychol 2016;117:225‐34. [DOI] [PubMed] [Google Scholar]
- 53. Uusberg H, Uusberg A, Talpsep T et al. Mechanisms of mindfulness: the dynamics of affective adaptation during open monitoring. Biol Psychol 2016;118:94‐106. [DOI] [PubMed] [Google Scholar]
- 54. Aldao A. The future of emotion regulation research: capturing context. Perspect Psychol Sci 2013;8:155‐72. [DOI] [PubMed] [Google Scholar]
- 55. Aldao A, Sheppes G, Gross JJ. Emotion regulation flexibility. Cogn Ther Res 2015;39:263‐78. [Google Scholar]
- 56. Doré BP, Silvers JA, Ochsner KN. Toward a personalized science of emotion regulation. Soc Personal Psychol Compass 2016;10:171‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ford BQ, Feinberg M, Lam P et al. Using reappraisal to regulate negative emotion after the 2016. U.S. Presidential election: does emotion regulation trump political action? J Pers Soc Psychol (in press). [DOI] [PubMed]
- 58. Haines SJ, Gleeson J, Kuppens P et al. The wisdom to know the difference: strategy‐situation fit in emotion regulation in daily life is associated with well‐being. Psychol Sci 2016;27:1651‐9. [DOI] [PubMed] [Google Scholar]
- 59. Troy AS, Shallcross AJ, Mauss IB. A person‐by‐situation approach to emotion regulation: cognitive reappraisal can either help or hurt, depending on the context. Psychol Sci 2013;24:2505‐14. [DOI] [PubMed] [Google Scholar]
- 60. Braunstein LM, Gross JJ, Ochsner KN. Explicit and implicit emotion regulation: a multi‐level framework. Soc Cogn Affect Neurosci 2017;12:1545‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Gyurak A, Gross JJ, Etkin A. Explicit and implicit emotion regulation: a dual‐process framework. Cogn Emot 2011;25:400‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Füstös J, Gramann K, Herbert BM et al. On the embodiment of emotion regulation: interoceptive awareness facilitates reappraisal. Soc Cogn Affect Neurosci 2013;8:911‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Barrett LF, Gross J, Christensen TC et al. Knowing what you're feeling and knowing what to do about it: mapping the relation between emotion differentiation and emotion regulation. Cogn Emot 2001;15:713‐24. [Google Scholar]
- 64. Tamir M. Why do people regulate their emotions? A taxonomy of motives in emotion regulation. Personal Soc Psychol Rev 2015;20:199‐222. [DOI] [PubMed] [Google Scholar]
- 65. Suri G, Sheppes G, Young G et al. Emotion regulation choice: the role of environmental affordances. Cogn Emot 2018;32:963‐71. [DOI] [PubMed] [Google Scholar]
- 66. Kobayashi R, Miyatani M, Nakao T. High working memory capacity facilitates distraction as an emotion regulation strategy. Curr Psychol (in press). [Google Scholar]
- 67. Sheppes G, Scheibe S, Suri G et al. Emotion regulation choice: a conceptual framework and supporting evidence. J Exp Psychol Gen 2014;143:163‐81. [DOI] [PubMed] [Google Scholar]
- 68. Sheppes G, Meiran N. Divergent cognitive costs for online forms of reappraisal and distraction. Emotion 2008;8:870‐4. [DOI] [PubMed] [Google Scholar]
- 69. Naragon‐Gainey K, McMahon TP, Chacko TP. The structure of common emotion regulation strategies: a meta‐analytic examination. Psychol Bull 2017;143:384‐427. [DOI] [PubMed] [Google Scholar]
- 70. van der Velde J, van Tol M‐J, Goerlich‐Dobre KS et al. Dissociable morphometric profiles of the affective and cognitive dimensions of alexithymia. Cortex 2014;54:190‐9. [DOI] [PubMed] [Google Scholar]
- 71. Swart M, Kortekaas R, Aleman A. Dealing with feelings: characterization of trait alexithymia on emotion regulation strategies and cognitive‐emotional processing. PLoS One 2009;4:e5751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Berthoz S, Hill EL. The validity of using self‐reports to assess emotion regulation abilities in adults with autism spectrum disorder. Eur Psychiatry 2005;20:291‐8. [DOI] [PubMed] [Google Scholar]
- 73. Nowakowski ME, McFarlane T, Cassin S. Alexithymia and eating disorders: a critical review of the literature. J Eat Disord 2013;1:1‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Clark DM. A cognitive approach to panic. Behav Res Ther 1986;24:461‐70. [DOI] [PubMed] [Google Scholar]
- 75. Gruber J. Can feeling too good be bad? Positive emotion persistence (PEP) in bipolar disorder. Curr Dir Psychol Sci 2011;20:217‐21. [Google Scholar]
- 76. Meyer B, Johnson SL, Winters R. Responsiveness to threat and incentive in bipolar disorder: relations of the BIS/BAS scales with symptoms. J Psychopathol Behav Assess 2001;23:133‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Britton PC. The relation of coping strategies to alcohol consumption and alcohol‐related consequences in a college sample. Addict Res Theory 2004;12:103‐14. [Google Scholar]
- 78. Leehr EJ, Krohmer K, Schag K et al. Emotion regulation model in binge eating disorder and obesity – a systematic review. Neurosci Biobehav Rev 2015;49:125‐34. [DOI] [PubMed] [Google Scholar]
- 79. McKenzie KC, Gross JJ. Nonsuicidal self‐injury: an emotion regulation perspective. Psychopathology 2014;47:207‐19. [DOI] [PubMed] [Google Scholar]
- 80. Nock MK. Why do people hurt themselves? New insights into the nature and functions of self‐injury. Curr Dir Psychol Sci 2009;18:78‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Robbins TW, Gillan CM, Smith DG et al. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci 2012;16:81‐91. [DOI] [PubMed] [Google Scholar]
- 82. Hofmann SG. Cognitive factors that maintain social anxiety disorder: a comprehensive model and its treatment implications. Cogn Behav Ther 2007;36:193‐209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Borkovec TD, Hazlett‐Stevens H, Diaz ML. The role of positive beliefs about worry in generalized anxiety disorder and its treatment. Clin Psychol Psychother 1999;6:126‐38. [Google Scholar]
- 84. Cohen JD. Cognitive control: core constructs and current considerations In: Egner T. (ed). The Wiley handbook of cognitive control. Chichester: Wiley, 2017:1‐28. [Google Scholar]
- 85. McTeague LM, Goodkind MS, Etkin A. Transdiagnostic impairment of cognitive control in mental illness. J Psychiatr Res 2016;83:37‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Barkley RA. Behavioral inhibition, sustained attention, and executive functions: constructing a unifying theory of ADHD. Psychol Bull 1997;121:65‐94. [DOI] [PubMed] [Google Scholar]
- 87. Martel MM. A new perspective on attention‐deficit/hyperactivity disorder: emotion dysregulation and trait models. J Child Psychol Psychiatry 2009;50:1042‐51. [DOI] [PubMed] [Google Scholar]
- 88. Chen C, Takahashi T, Nakagawa S et al. Reinforcement learning in depression: a review of computational research. Neurosci Biobehav Rev 2015;55:247‐67. [DOI] [PubMed] [Google Scholar]
- 89. Dunlop BW, Nemeroff CB. The role of dopamine in the pathophysiology of depression. Arch Gen Psychiatry 2007;64:327‐37. [DOI] [PubMed] [Google Scholar]
- 90. Aldao A, Nolen‐Hoeksema S, Schweizer S. Emotion‐regulation strategies across psychopathology: a meta‐analytic review. Clin Psychol Rev 2010;30:217‐37. [DOI] [PubMed] [Google Scholar]
- 91. Mennin DS, Heimberg RG, Turk CL et al. Applying an emotion regulation framework to integrative approaches to generalized anxiety disorder. Clin Psychol Sci Pract 2002;9:85‐90. [Google Scholar]
- 92. Wells A. The metacognitive model of GAD: assessment of meta‐worry and relationship with DSM‐IV generalized anxiety disorder. Cogn Ther Res 2005;29:107‐21. [Google Scholar]
- 93. Nolen‐Hoeksema S. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. J Abnorm Psychol 2000;109:504‐11. [PubMed] [Google Scholar]
- 94. Rosenthal MZ, Gratz KL, Kosson DS et al. Borderline personality disorder and emotional responding: a review of the research literature. Clin Psychol Rev 2008;28:75‐91. [DOI] [PubMed] [Google Scholar]
- 95. Links PS, Heslegrave R, van Reekum R. Impulsivity: core aspect of borderline personality disorder. J Personal Disord 1999;13:1‐9. [DOI] [PubMed] [Google Scholar]
- 96. Beck AT. Cognitive therapy and the emotional disorders. Oxford: International Universities Press, 1976. [Google Scholar]
- 97. Linehan MM. Cognitive‐behavioral treatment of borderline personality disorder. New York: Guilford, 1993. [Google Scholar]
- 98. Farb NA, Anderson AK, Irving JA et al. Mindfulness interventions and emotion regulation In: Gross JJ. (ed). Handbook of emotion regulation, 2nd ed New York: Guilford, 2014:548‐67. [Google Scholar]
- 99. Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy. The process and practice of mindful change, 2nd ed New York: Guilford, 2012. [Google Scholar]
- 100. Kabat‐Zinn J. Full catastrophe living: how to cope with stress, pain and illness using mindfulness meditation. Hachette: Piatkus, 2013. [Google Scholar]
- 101. Segal ZV, Williams M, Teasdale J. Mindfulness‐based cognitive therapy for depression, 2nd ed New York: Guilford, 2013. [Google Scholar]
- 102. Greenberg LS. Emotion‐focused therapy: coaching clients to work through their feelings. Washington: American Psychological Association, 2015. [Google Scholar]
- 103. Berking M, Whitley B. Affect regulation training. New York: Springer, 2014. [Google Scholar]
- 104. Mennin DS, Fresco DM. Emotion regulation therapy In: Gross JJ. (ed). Handbook of emotion regulation, 2nd ed New York: Guilford, 2014:469‐90. [Google Scholar]
- 105. Wells A. Meta‐cognition and worry: a cognitive model of generalized anxiety disorder. Behav Cogn Psychother 1995;23:301‐20. [Google Scholar]
- 106. Stone AA, Neale JM. New measure of daily coping: development and preliminary results. J Pers Soc Psychol 1984;46:892‐906. [Google Scholar]
- 107. Wolpe J. Psychotherapy by reciprocal inhibition. Cond Reflex Pavlov J Res Ther 1968;3:234‐40. [DOI] [PubMed] [Google Scholar]
- 108. DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci 2008;9:788‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Bagby RM, Parker JDA, Taylor GJ. The twenty‐item Toronto Alexithymia scale – I. Item selection and cross‐validation of the factor structure. J Psychosom Res 1994;38:23‐32. [DOI] [PubMed] [Google Scholar]
- 110. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well‐being. J Pers Soc Psychol 2003;85:348‐62. [DOI] [PubMed] [Google Scholar]
- 111. Garnefski N, Kraaij V. Cognitive emotion regulation questionnaire – development of a short 18‐item version (CERQ‐short). Personal Individ Differ 2006;41:1045‐53. [Google Scholar]
- 112. Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess 2004;26:41‐54. [Google Scholar]
- 113. Kato T. Development of the Coping Flexibility Scale: evidence for the coping flexibility hypothesis. J Couns Psychol 2012;59:262‐73. [DOI] [PubMed] [Google Scholar]
- 114. Hajcak G, MacNamara A, Olvet DM. Event‐related potentials, emotion, and emotion regulation: an integrative review. Dev Neuropsychol 2010;35:129‐55. [DOI] [PubMed] [Google Scholar]
- 115. Quoidbach J, Mikolajczak M, Gross JJ. Positive interventions: an emotion regulation perspective. Psychol Bull 2015;141:655‐93. [DOI] [PubMed] [Google Scholar]
- 116. Henderson LW, Knight T. Integrating the hedonic and eudaimonic perspectives to more comprehensively understand wellbeing and pathways to wellbeing. Int J Wellbeing 2012;2:196‐221. [Google Scholar]
- 117. Bratman GN, Hamilton JP, Daily GC. The impacts of nature experience on human cognitive function and mental health. Ann NY Acad Sci 2012;1249:118‐36. [DOI] [PubMed] [Google Scholar]
- 118. Wood AM, Froh JJ, Geraghty AWA. Gratitude and well‐being: a review and theoretical integration. Clin Psychol Rev 2010;30:890‐905. [DOI] [PubMed] [Google Scholar]
- 119. Oettingen G. Future thought and behaviour change. Eur Rev Soc Psychol 2012;23:1‐63. [Google Scholar]
- 120. Penedo FJ, Dahn JR. Exercise and well‐being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry 2005;18:189‐93. [DOI] [PubMed] [Google Scholar]
- 121. Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry 2014;13:28‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Gold JI, Shadlen MN. The neural basis of decision making. Annu Rev Neurosci 2007;30:535‐74. [DOI] [PubMed] [Google Scholar]
- 123. Ratcliff R, Smith PL, Brown SD et al. Diffusion decision model: current issues and history. Trends Cogn Sci 2016;20:260‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]


