Abstract
The usefulness of current psychiatric classification, which is based on ICD/DSM categorical diagnoses, remains questionable. A promising alternative has been put forward as the “transdiagnostic” approach. This is expected to cut across existing categorical diagnoses and go beyond them, to improve the way we classify and treat mental disorders. This systematic review explores whether self‐defining transdiagnostic research meets such high expectations. A multi‐step Web of Science literature search was performed according to an a priori protocol, to identify all studies that used the word “transdiagnostic” in their title, up to May 5, 2018. Empirical variables which indexed core characteristics were extracted, complemented by a bibliometric and conceptual analysis. A total of 111 studies were included. Most studies were investigating interventions, followed by cognition and psychological processes, and neuroscientific topics. Their samples ranged from 15 to 91,199 (median 148) participants, with a mean age from 10 to more than 60 (median 33) years. There were several methodological inconsistencies relating to the definition of the gold standard (DSM/ICD diagnoses), of the outcome measures and of the transdiagnostic approach. The quality of the studies was generally low and only a few findings were externally replicated. The majority of studies tested transdiagnostic features cutting across different diagnoses, and only a few tested new classification systems beyond the existing diagnoses. About one fifth of the studies were not transdiagnostic at all, because they investigated symptoms and not disorders, a single disorder, or because there was no diagnostic information. The bibliometric analysis revealed that transdiagnostic research largely restricted its focus to anxiety and depressive disorders. The conceptual analysis showed that transdiagnostic research is grounded more on rediscoveries than on true innovations, and that it is affected by some conceptual biases. To date, transdiagnostic approaches have not delivered a credible paradigm shift that can impact classification and clinical care. Practical “TRANSD”iagnostic recommendations are proposed here to guide future research in this field.
Keywords: Transdiagnostic, diagnosis, classification, bibliometric analysis, conceptual analysis, anxiety, depression, psychosis, recommendations
Diagnosis, which is the medical application of the process of classification, ubiquitous in science, has been the cornerstone of modern clinical knowledge and practice1. Diagnosis in psychiatry started in Europe in the late 17th century, informed by systems that classified animal and plant species as part of other natural sciences2. Psychiatric nosology, traditionally represented by the ICD and DSM (gold standard), is based on categorical diagnoses that are intertwined with the key clinical dichotomies that characterize the realm of clinical medicine (e.g., to treat or not to treat)3, 4.
Since its inception, psychiatric nosology has always been under fire. This is documented by several lines of evidence, including two recent issues of this journal3, 5. Although current diagnostic categories have demonstrated moderate to almost perfect reliability6, their usefulness has remained questionable7.
A promising avenue has been put forward by the so‐called transdiagnostic approach. The prefix “trans” comes from Latin and it can either mean across/through (e.g., transatlantic) or beyond (e.g., transcend)8. Therefore, a transdiagnostic approach in psychiatry is expected to cut across existing categorical diagnoses and go beyond them, to produce a better classification system, compared to the existing gold standard.
Transdiagnostic approaches originated from cognitive behavioral theories and treatments for eating disorders9, 10, which were then extended to anxiety11, 12, 13 and depressive disorders14. The initial transdiagnostic rationale leveraged two core points: a) these disorders share common etiological and maintenance processes9, 10, 13, 15 as well as cognitive‐affective, interpersonal, and behavioral features9, 10, 15 (e.g., the general psychopathology latent factor – p factor16), and b) the ever‐growing number of disorder‐specific treatment manuals is a barrier to the implementation of cognitive behavioral treatments10, 13, 15.
The rationale for extending the transdiagnostic paradigm to anxiety and depressive disorders included an additional point that was not originally acknowledged10: c) disorder‐specific interventions rely on heterogeneous diagnostic categories and pay relatively limited attention to comorbidity, which is high15.
Transdiagnostic research aims at tackling these limitations to introduce a novel approach that could improve the way we classify, formulate, treat, and prevent15 mental disorders. Moving away from a single‐diagnosis approach towards a transdiagnostic conceptualization and treatment of mental disorders would thus be a significant paradigm shift15. Recently, transdiagnostic approaches have been endorsed by other paradigms that cut across different mental disorders, such as the Research Domain Criteria (RDoC) initiative17 and the clinical staging model18. At present, however, it is unclear whether transdiagnostic research meets such high expectations for delivering a radical paradigm shift that impacts classification and clinical care.
To address this issue, we present here a broad systematic review of transdiagnostic research in psychiatry. We systematically assess the transdiagnostic literature against several empirical variables which index core characteristics as well as potential pitfalls. A bibliometric and conceptual analysis complements the empirical findings, along with practical recommendations to guide future research in this field.
METHODS
The PRISMA compliant19 protocol for this study was registered on PROSPERO (CRD42018108613).
Search strategy, selection criteria and data extraction
A multi‐step literature search was performed. First, systematic searches were conducted in the Web of Science (which includes Web of Science Core Collection, BIOSIS Citation Index, KCI ‐ Korean Journal Database, MEDLINE, Russian Science Citation Index, and SciELO Citation Index), until May 5, 2018, with no restrictions on language or publication date. The keyword “transdiagnostic” was used, filtering for the category “psychiatry” through the Web of Science categories function. Second, we searched the reference lists of retrieved articles. Third, abstracts identified by this process were then screened and full‐text articles were inspected against the inclusion and exclusion criteria.
The literature search, study selection and data extraction were conducted by two authors (MS, NB) independently. During all stages, in the case of disagreement, consensus was reached through discussion with a third author (PFP).
Studies were eligible for inclusion when the following criteria were fulfilled: a) original individual articles, with no restriction on study design (including interventional and observational studies) or topic; b) a clear and primary focus on a transdiagnostic approach, demonstrated by using the word “transdiagnostic” in the title.
The exclusion criteria were: a) reviews, meta‐analyses, study protocols, abstracts and any other non‐original data; b) lacking a clear primary focus on transdiagnostic approaches, defined as above; and c) studies with less than ten participants20.
Descriptive variables
For each study, we extracted descriptive variables relating to: a) general information, b) definition of gold standard diagnostic criteria, c) outcome measures, d) definition of the transdiagnostic approach, and e) quality assessment.
General information variables included: first author and year of publication; study domain (classification, treatment, clinical prediction, neuroscience, cognition and psychological processes); study design (observational, uncontrolled interventional, controlled interventional); type of design (cross‐sectional, longitudinal, unrandomized, randomized); total sample size (total pool of participants recruited at baseline, including non‐clinical samples); and mean age (or age range).
Variables relating to the definition of the gold standard diag‐nostic criteria included: whether the study explicitly acknowledged the type of gold standard used (DSM or ICD, any version); the specific type of primary diagnoses of mental disorders and their specific ICD or DSM codes; the presence of any other clinical condition as defined by each individual study; the presence of a non‐clinical sample (e.g., healthy controls); the total number of ICD/DSM mental disorders investigated by the study; the total number of diagnostic spectra (defined according to the ICD‐10 diagnostic blocks: organic, including symptomatic mental disorders; mental and behavioral disorders due to psychoactive substance use; schizophrenia, schizotypal and delusional disorders; mood (affective) disorders; neurotic, stress‐related and somatoform disorders; behavioral syndromes associated with physiological disturbances and physical factors; disorders of adult personality and behavior; mental retardation; disorders of psychological development; behavioral and emotional disorders with onset usually occurring in childhood and adolescence; unspecified mental disorders); and the type of psychometric instrument employed to define the gold standard.
Variables relating to the outcomes included: whether the primary outcome of the study was clearly acknowledged in the manuscript; the specific type of instruments employed to define it; and the total number of primary outcomes.
Variables relating to the transdiagnostic approach included: the exact definition of the transdiagnostic construct as provided by each study; the number of transdiagnostic constructs (single or multiple)21; whether the transdiagnostic construct was descriptive (a construct which is present in multiple disorders, without regard to how or why22) or mechanistic (a construct that may reflect an underlying physiological, neurobiological or functional mechanism22); whether the construct was causally associated with the outcome (to rule out the possibility that a construct may just be epiphenomenal21); whether the transdiagnostic construct was present in all clinical conditions and spectra (universal transdiagnostic process) and in how many of them. We also extracted the type of statistical analysis used to probe the transdiagnostic construct; whether there was a formal statistical assessment of the impact of the transdiagnostic approach compared to the specific‐diagnostic approach; and the results of such a test.
Quality assessment was performed by recording if an a priori protocol had been made available, if funding was provided by industry, and if the core findings had been externally replicated in an independent sample.
Analysis
The descriptive variables were used to perform different types of analyses.
First, descriptive summary data and statistics (i.e., frequencies, means/medians, ranges) of the above variables were narratively presented in the text and in informative tables.
Second, each study was assessed against the criteria introduced by Mansell et al21 to define transdiagnostic approaches in psychiatry: a) presence of a clinical population, b) presence of at least four different mental disorders, c) presence of a non‐clinical sample, and d) demonstration of the transdiagnostic construct in all mental disorders investigated.
Third, the conceptual definition of the transdiagnostic approach was empirically deconstructed. The main aim was to explore the extent to which each transdiagnostic approach related to the existing diagnostic categorical system. As indicated in Figure 1, the simplest transdiagnostic approach – defined as “across‐diagnoses” – was to compare different ICD/DSM categorical diagnoses against each other, to test their diagnostic boundaries and cross‐cutting features. The across‐diagnoses model could include one diagnostic spectrum, multiple spectra and/or non‐clinical samples, including also healthy individuals. A more elaborated approach involved the definition of new diagnostic‐like constructs, for example based on biotypes or clinical types, and then testing the relatedness of these newly defined constructs against the gold standard. These approaches were termed “beyond‐diagnoses” , because they employed standard ICD/DSM diagnostic information but went beyond it, to test new diagnostic constructs. When studies did not fit within any of the above two categories, the specific approach was described.
Figure 1.
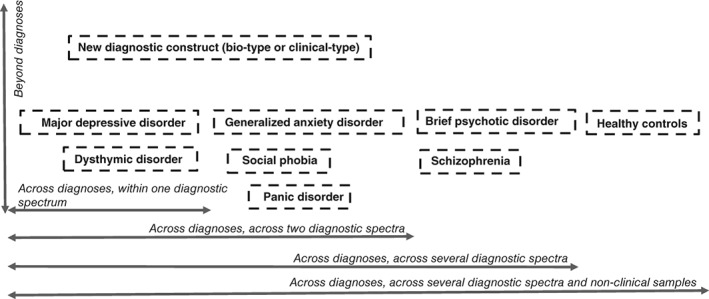
Conceptual classification of transdiagnostic approaches most widely employed in psychiatry, with some prototypical diagnostic examples
Fourth, we conducted a bibliometric analysis using the list of specific ICD/DSM mental disorders that were analyzed by each study (when available). These data were then loaded into R software and cleaned with the Bibliometrix and TM packages. The processed data were then loaded into Gephi software to generate the network map of the specific ICD/DSM mental disorders investigated by transdiagnostic research. Each node indicated a specific mental disorder, with the node's size reflecting how many different connections (frequency) with other nodes were present. The thickness of the edges reflected the number of connections between a pair of nodes/mental disorders. For graphical purposes, nodes that had frequen‐cy ≤⃒6 and number of co‐occurrent connections ≤⃒3 were filtered out.
RESULTS
Studies identified
The literature search identified 627 potential records that were screened on the basis of title and abstract reading. Of these, 239 were considered eligible for full screening. At this stage, 128 studies were further excluded, leaving a sample of 111 studies, which represented the final database for the current systematic review (Figure 2).
Figure 2.
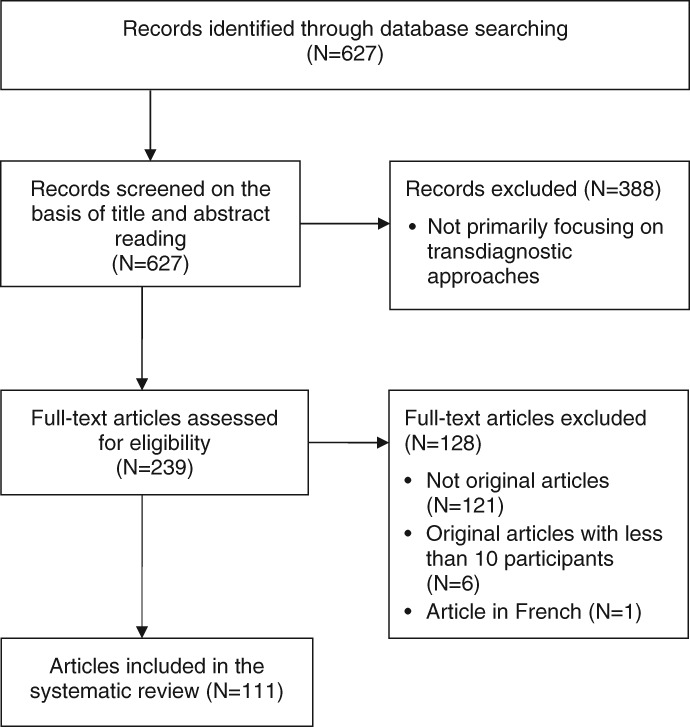
Study identification and selection (PRISMA flow chart)
Characteristics of transdiagnostic studies in psychiatry
General information
The first study, published in 2004 by Norton et al11, addressed the effects of a transdiagnostic psychological intervention for different types of anxiety disorders. Since then, there was one study published in 2006, six in 2008, four in 2009, six in 2012, six in 2013, thirteen in 2014, eleven in 2015, eighteen in 2016, thirty‐four in 2017, and eleven up to May 2018.
Most studies (45%) were investigating interventions (of which 50% were controlled, 48% uncontrolled23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, and 2% unclear47). Less than half (46%)11, 43, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68 of the interventional studies were randomized. All interventional studies focused on neurotic, stress‐related and somatoform disorders or mood (affective) disorders, while other mental disorders were rarely investigated (Table 1).
Table 1.
Studies included in the systematic review
| Study | Year | Domain | Baseline N | Mean age | Gold standard | Transdiagnostic construct | Transdiagnostic type | Mansell criteria |
|---|---|---|---|---|---|---|---|---|
| Van Dijk et al23 | 2018 | Treatment | 53 and 64 | >60 | DSM‐IV‐TR | Psychotherapeutic day treatment and activating day treatment | Across diagnoses, across spectra | No |
| Samtani et al109 | 2018 | Prediction | 183 | 23 | DSM‐IV | Repetitive negative thinking | Within the same diagnosis | No |
| Pellizzer et al69 | 2018 | Prediction | 78 | 27 | DSM‐5 | Body image flexibility | Across diagnoses, within spectrum | No |
| Nota & Coles104 | 2018 | Neuroscience | 52 | 36 | DSM‐IV‐TR | Repetitive negative thinking | Across diagnoses, across spectra | No |
| McEvoy et al82 | 2018 | Prediction | 2,088 | 20 | NA | Repetitive negative thinking | A‐diagnostic | No |
| Grisanzio et al111 | 2018 | Classification | 420 | 40 | DSM‐IV | Subtypes based on neurocognition, brain activation and functional capacity | Beyond diagnoses | No |
| Goldschmidt et al125 | 2018 | Classification | 636 | 15 | DSM‐5 | Eating disorders symptoms network | Across diagnoses, within spectrum | No |
| Dear et al24 | 2018 | Treatment | 28 | 41 | DSM‐IV | Cognitive behavioral therapy | Across physical and mental health diagnoses | No |
| Curzio et al129 | 2018 | C&P processes | 419 | 15 | DSM‐IV‐TR | Binge eating, dietary restrain, affective, interpersonal problems and perfectionism | Across diagnoses, within spectrum | No |
| Ciaramidaro et al105 | 2018 | Neuroscience | 78 | 22 | ICD‐10 | Facial recognition | Across diagnoses, across spectra and non‐clinical samples | No |
| Capobianco et al48 | 2018 | Treatment | 40 | 28 | DSM‐IV | Metacognitive and mindfulness meditation therapies | Across diagnoses, across spectra | No |
| Zwerenz et al49 | 2017 | Treatment | 82 | 40 | ICD‐10 | Psychodynamic web‐based self‐help intervention | Across diagnoses, across spectra | No |
| Zemestani et al50 | 2017 | Treatment | 43 | 23 | DSM‐IV | Cognitive behavioral therapy | Within the same diagnosis | No |
| Wigman et al70 | 2017 | C&P processes | 293 | 19 | NA | Interconnectedness of psychotic and affective experiences | A‐diagnostic | No |
| Talkovsky et al25 | 2017 | Treatment | 129 | 33 | DSM‐IV‐TR | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Talkovsky et al26 | 2017 | Treatment | 120 | 33 | DSM‐IV‐TR | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Smith et al27 | 2017 | Treatment | 49 | 33 | DSM‐IV | Anxiety symptoms questionnaire | Across diagnoses, within spectrum | No |
| Shinn et al71 | 2017 | Classification | 91 | 21 | NA | Clinical service | Across diagnoses, across spectra | No |
| Sheffield et al112 | 2017 | Neuroscience | 576 | 35 | DSM‐IV | Functional brain network integrity | Across diagnoses, across spectra and non‐clinical samples | No |
| Sharma et al51 | 2017 | Treatment | 63 | 14 | ICD‐10 | Group cognitive behavioral therapy | Across physical and mental health diagnoses | No |
| Schroder et al52 | 2017 | Treatment | 179 | 37 | DSM‐IV | Internet intervention | Across diagnoses, within spectrum | No |
| Riccardi et al53 | 2017 | Treatment | 28 | 29 | DSM‐IV | False safety behavior elimination therapy | Across diagnoses, within spectrum | No |
| Platt et al72 | 2017 | Prediction | 4,925 | 13‐18 | DSM‐IV | Timing of menarche and internalizing factors | Across diagnoses, across spectra | No |
| Pitman et al28 | 2017 | Treatment | 73 | 29 | DSM‐IV | Short‐term psychodynamic psychotherapy | Across diagnoses, across spectra | No |
| Newby et al83 | 2017 | Treatment | 2,109 | 40 | DSM‐IV | Internet‐based cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Maia et al54 | 2017 | Treatment | 67 | >18 | DSM‐IV, ICD‐10 | Cognitive behavioral therapy | Across diagnoses, across spectra | No |
| MacNamara et al113 | 2017 | Neuroscience | 199 | 26 | DSM‐IV | Affective face processing | Across diagnoses, across spectra and non‐clinical samples | No |
| Lee et al84 | 2017 | Prediction | 163 | 20 | DSM‐IV‐TR | Neuropsychological functioning | Across diagnoses, across spectra | No |
| LeBouthillier & Asmundson55 | 2017 | Treatment | 48 | 33 | DSM‐5 | Aerobic exercise and resistance training | Across diagnoses, within spectrum | No |
| Keil et al114 | 2017 | C&P processes | 108 | 12 | DSM‐5 | Emotions regulation | Across diagnoses, across spectra and non‐clinical samples | No |
| Jauhar et al115 | 2017 | Neuroscience | 60 | 24 | DSM‐IV | Dopamine synthesis capacity | Across diagnoses, across spectra and non‐clinical samples | No |
| Hankin et al85 | 2017 | C&P processes | 1,125 | 11 | NA | Temperamental and psychopathology factors | A‐diagnostic | No |
| Hamblen et al29 | 2017 | Treatment | 342 | 57 | NA | Cognitive behavioral therapy | Across symptoms | No |
| Gros et al30 | 2017 | Treatment | 16 | 47 | DSM‐5 | Cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Gong et al116 | 2017 | Neuroscience | 272 | 34 | DSM‐IV | Intra/inter‐network connectivity | Across diagnoses, across spectra and non‐clinical samples | No |
| Gibson et al86 | 2017 | C&P processes | 2,342 | 21 | NA | Exposure to traumatic life events | Across symptoms | No |
| Fusar‐Poli et al73 | 2017 | Prediction | 91,199 | 33 | CAARMS, ICD‐10 | Risk model of transition to psychosis | Across diagnoses, across spectra | No |
| Forbush et al126 | 2017 | Classification | 207 | 25 | DSM‐5 | Distress and fear‐avoidance internalizing factors | Beyond diagnoses | No |
| Feldker et al117 | 2017 | Neuroscience | 134 | 28 | DSM‐IV | Brain response to visual threat | Across diagnoses, within spectrum and non‐clinical samples | Yes |
| Espejo et al31 | 2017 | Treatment | 48 | 45 | DSM‐IV | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Ellard et al56 | 2017 | Treatment | 29 | 44 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Chen et al118 | 2017 | Neuroscience | 60 | 41 | DSM‐IV | Functional connectivity density | Across diagnoses, across spectra and non‐clinical samples | No |
| Chasson et al87 | 2017 | C&P processes | 3,094 | 15 | NA | Emotional vulnerabilities | A‐diagnostic | No |
| Berger et al57 | 2017 | Treatment | 139 | 42 | DSM‐IV | Internet‐based cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Barlow et al58 | 2017 | Treatment | 233 | 31 | DSM‐IV, DSM‐5 | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Talkovsky & Norton32 | 2016 | Treatment | 151 | 33 | DSM‐IV | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Sunderland et al119 | 2016 | C&P processes | 8,871 | 16‐85 | DSM‐IV | Two factor internalizing‐substance dependence model | Across diagnoses, across spectra and non‐clinical samples | No |
| Stanton et al106 | 2016 | C&P processes | 299 | 47 | DSM‐5 | Emotion regulation and basic personality dimensions | Across diagnoses, across spectra and non‐clinical samples | No |
| Sabharwal et al108 | 2016 | Neuroscience | 82 | 45 | DSM‐IV | Behavioral and neural measures of emotion‐related working memory | Across diagnoses, across spectra | No |
| Reininghaus et al130 | 2016 | Classification | 1,168 | 42 | RDoC | Bifactor model with general and specific psychosis dimensions | Beyond diagnoses | No |
| Philip et al74 | 2016 | Prediction/neuroscience | 46 | 39 | DSM‐IV‐TR | Thalamic connectivity in early life stress | Across diagnoses, across spectra and non‐clinical samples | No |
| Morris et al88 | 2016 | Treatment | 108 | 41 | NA | Group based psychological intervention | Across symptoms | No |
| McIntosh et al59 | 2016 | Treatment | 112 | 35 | DSM‐IV | Cognitive behavioral therapy | Within the same diagnosis | No |
| McEvoy & Erceg‐Hurn33 | 2016 | Treatment | 256 | 34 | DSM‐IV | Intolerance of uncertainty | Across diagnoses, across spectra | No |
| Kristjánsdóttir et al34 | 2015 | Treatment | 287 | 39 | DSM‐IV, ICD‐10 | Group cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Ito et al35 | 2016 | Treatment | 28 | 35 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Holliday et al89 | 2016 | C&P processes | 783 | 29 | DSM‐5 | Distress tolerance | Across diagnoses, across spectra | No |
| Hadjistavropoulos et al36 | 2016 | Treatment | 458 | 39 | DSM‐IV | Internet‐based cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Fogliati et al60 | 2016 | Treatment | 145 | 41 | DSM‐IV | Cognitive behavioral therapy | Within the same diagnosis | No |
| Dear et al61 | 2016 | Treatment | 233 | 42 | DSM‐IV | Cognitive behavioral therapy | Within the same diagnosis | No |
| Conway et al75 | 2016 | C&P processes | 815 | 15 | DSM‐IV | Internalizing and externalizing factors mediating appraisal biases | Transdiagnostic outcome | No |
| Conway et al107 | 2016 | Prediction | 700 | 20 | DSM‐IV | Latent model of personality disorder | Across diagnoses, across spectra and non‐clinical samples | No |
| Asnaani et al37 | 2016 | Treatment | 107 | 33 | DSM‐5 | Anxiety sensitivity, depression, rumination as moderators of cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Titov et al62 | 2015 | Treatment | 290 | 44 | DSM‐IV | Cognitive behavioral therapy | Within the same diagnosis | No |
| Thibodeau et al90 | 2015 | C&P processes | 1,255 | 22 | DSM‐IV‐TR | Intolerance of uncertainty | Across symptoms | No |
| Tang‐Smith et al91 | 2015 | C&P processes | 612 | 21 | DSM‐III | Dominance behavioral system | Across symptoms | No |
| Rodriguez‐Seijas et al127 | 2015 | C&P processes | 5,191 | NA | DSM‐IV | Internalizing and externalizing factors | Across diagnoses, across spectra | No |
| Pietrzak et al110 | 2015 | C&P processes | 267 | 54 | DSM‐IV | Loss symptoms, threat symptoms and somatic symptoms | Within the same diagnosis | No |
| Maia et al99 | 2015 | Treatment | 48 | 18‐58 | DSM‐IV, ICD‐10 | Cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Latack et al76 | 2015 | C&P processes | 34,653 | >18 | DSM‐IV | Internalizing and externalizing factors | Across diagnoses, across spectra and non‐clinical samples | No |
| Hsu et al131 | 2015 | C&P processes | 51 | 33 | DSM‐IV | Self‐reported attentional control and rumination | Across diagnoses, across spectra | No |
| Dear et al63 | 2015 | Treatment | 366 | 44 | DSM‐IV | Cognitive behavioral therapy | Within the same diagnosis | No |
| Corral‐Frías et al101 | 2015 | Neuroscience | 906 | 20 | DSM‐IV | Ventral striatal reactivity to reward | Across diagnoses, across spectra and non‐clinical samples | No |
| Bedwell et al120 | 2015 | Neuroscience | 48 | 36 | DSM‐IV | Visual evoked potentials | Across diagnoses, across spectra and non‐clinical samples | No |
| Vann et al128 | 2014 | C&P processes | 27 | 26 | DSM‐IV‐TR | Metacognitions | Across diagnoses, within spectrum | No |
| Talkovsky & Norton38 | 2014 | Treatment | 256 | 33 | DSM‐IV | Negative affectivity, anxiety sensitivity, intolerance uncertainty | Across diagnoses, within spectrum | No |
| Starr et al77 | 2014 | Prediction | 1,630 | 28 | DSM‐IV | Latent internalizing factors for psychopathology | Transdiagnostic outcome | No |
| Spielberg et al121 | 2014 | Neuroscience | 179 | 27 | DSM‐IV | Dimensions of anxiety and depression | Across diagnoses, across spectra and non‐clinical samples | No |
| Queen et al39 | 2014 | Treatment | 59 | 15 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Pietrzak et al103 | 2014 | Neuroscience | 35 | 29 | DSM‐IV‐TR | Threat and loss symptoms | Across diagnoses, across spectra and non‐clinical samples | No |
| Newby et al40 | 2014 | Treatment | 707 | 40 | DSM‐IV | Internet‐based cognitive behavioral therapy | Across diagnoses, across spectra and non‐clinical samples | No |
| McLaughlin et al78 | 2014 | Prediction | 1,065 | 12 | NA | Rumination | A‐diagnostic | No |
| McEvoy et al122 | 2014 | C&P processes | 786 | 28 | DSM‐IV | Repetitive negative thinking | Across diagnoses, across spectra and non‐clinical samples | No |
| Gros41 | 2014 | Treatment | 29 | 50 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, across spectra | No |
| Cameron et al92 | 2014 | C&P processes | 41 | 28 | NA | Emotion perception and semantic memory | A‐diagnostic | No |
| Bullis et al42 | 2014 | Treatment | 15 | 32 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Bohnke et al93 | 2014 | C&P processes | 11,939 | 38 | DSM‐IV | Negative affectivity | Across diagnoses, across spectra | No |
| Norton et al47 | 2013 | Treatment | 79 | 33 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| McEvoy et al132 | 2013 | C&P processes | 513 | 37 | DSM‐IV | Repetitive negative thinking | Across diagnoses, across spectra | No |
| McEvoy & Mahoney133 | 2013 | C&P processes | 99 | NA | DSM‐IV | Intolerance of uncertainty and negative metacognitive beliefs | Across diagnoses, within spectrum | No |
| Johnson et al94 | 2013 | C&P processes | 334 | 19 | DSM‐IV | Impulsive responses to emotion | Across diagnoses, across spectra and non‐clinical samples | No |
| Ebert et al64 | 2013 | Treatment | 400 | 45 | ICD‐10 | Internet‐based maintenance treatment | Across diagnoses, across spectra | No |
| Boswell et al43 | 2013 | Treatment | 54 | 30 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Norton & Barrera65 | 2012 | Treatment | 46 | 31 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Norton66 | 2012 | Treatment | 87 | 33 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Hoiles et al95 | 2012 | C&P processes | 224 | 31 | NA | Cognitive model for eating disorder | A‐diagnostic | No |
| Farchione et al67 | 2012 | Treatment | 37 | 29 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Conway et al79 | 2012 | C&P processes | 815 | 15 | DSM‐IV | Internalizing and externalizing factors | Across diagnoses, across spectra | No |
| Bilek & Ehrenreich‐May44 | 2012 | Treatment | 22 | 10 | DSM‐IV | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Innis et al96 | 2009 | Neuroscience | 135 | 28 | DSM‐IV | Homocysteine remethylation | Within the same diagnosis | No |
| Hagenaars et al123 | 2009 | C&P processes | 252 | 29 | DSM‐IV | Trauma and panic memories | Across diagnoses, within spectrum and non‐clinical samples | No |
| Fairburn et al68 | 2009 | Treatment | 154 | 26 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Bentall et al100 | 2009 | C&P processes | 237 | 53 | DSM‐IV, ICD‐10 | Paranoia, cognitive performance and depressive style | Across diagnoses, across spectra and non‐clinical samples | Yes |
| Norton et al46 | 2008 | Treatment | 54 | 32 | DSM‐IV | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| Norton45 | 2008 | Treatment | 52 | 33 | DSM‐IV | Group cognitive behavioral therapy | Across diagnoses, within spectrum | No |
| McFarlane et al80 | 2008 | Prediction | 58 | 30 | DSM‐IV | Predictors of relapse | Across diagnoses, within spectrum | No |
| Corcoran et al124 | 2008 | C&P processes | 148 | 38 | DSM‐IV | Theory of mind and jumping to conclusions | Across diagnoses, across spectra and non‐clinical samples | No |
| Brown et al97 | 2008 | C&P processes | 38 | 20 | NA | Measure of mundane meaning | A‐diagnostic | No |
| Bentall et al98 | 2008 | C&P processes | 148 | 38 | DSM‐IV | Negative self‐esteem and negative expectations | Across diagnoses, across spectra and non‐clinical samples | Yes |
| Wade et al81 | 2006 | C&P processes | 1,002 | 35 | DSM‐IV | Dimensional model of eating disorders | Across diagnoses, across spectra and non‐clinical samples | No |
| Norton et al11 | 2004 | treatment | 23 | >19 | DSM‐IV | Cognitive behavioral therapy | Across diagnoses, within spectrum | No |
C&P processes – cognition and psychological processes, CAARMS – Comprehensive Assessment of At Risk Mental State, RDoC – Research Domain Criteria, NA – not available
Cognition and psychological processes was the second most frequent topic (28%), followed by neuroscientific topics (13%). Classification and prediction studies were more infrequent (4% and 10% respectively) (Table 1).
The vast majority of non‐interventional studies (79%) were cross‐sectional, and only 21%69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81 longitudinal. There was a large variability in study sample size, ranging from 15 participants in the smallest study42 to 91,199 in the largest73 (median: 148 participants). The mean age of individuals (when available) ranged from 1044 to more than 6023 (median: 33 years).
Definition of gold standard diagnostic criteria
A substantial proportion (27%) of studies24, 29, 36, 40, 48, 49, 64, 69, 70, 71, 73, 78, 80, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97, 98 did not acknowledge using any psychometric interview to establish their gold standard diagnoses. Several studies (16%)29, 34, 54, 70, 71, 78, 82, 83, 85, 86, 87, 88, 92, 93, 95, 97, 99, 100 did not refer to a gold standard diagnostic manual, but speculated on comparative benefits of the transdiagnostic approach over specific diagnoses29, 71.
Some studies reported non‐existent (e.g., DSM‐IV‐TR bipolar II disorder with psychotic features84) or incorrect diagnoses (e.g., suicidality34, marijuana abuse/dependence76, 101, late onset schizophrenia‐like psychosis100, social anxiety disorder and social phobia as two distinct DSM‐IV disorders101). Other studies included health anxiety within mental disorders, confusingly defined either as not relating to a specific diagnosis90, as hypocondriasis23, or as “health‐based anxiety predominant in individuals with illness anxiety disorders and somatic symptom disorders”90.
One interventional study stated that the participants were not diagnosed at all88. The study addressed this issue by simply noting that “it would have been informative to know client diagnoses”88, raising concerns about unnecessary or excessive treatments in this sample102.
Some studies used comorbid (as opposed to primary) diagnoses to validate the transdiagnostic construct50, 52, 56, 59, 60, 61, 62, 63, 99, 103. In about one third of studies (28%)34, 36, 54, 69, 70, 72, 74, 75, 82, 85, 87, 89, 104, 105, 106, 107, the boundaries between primary and secondary diagnoses were not completely clear.
There was also some confusion between the measurement of symptoms as opposed to categorical disorders. This was mainly due to the use of continuous measurements that were not translated into ICD/DSM diagnostic categories through the use of a priori cut‐offs83. Three studies measured DSM‐related items in non‐clinical samples without applying cut‐offs to establish the intake of specific diagnostic categories86, 90, 91. The results were there interpreted in the context of the disorder‐oriented literature91, arguing that findings were related to specific categorical diagnoses86, 90. These studies concurrently acknowledged a transdiagnostic approach in their title – as for any other study included in the current review – and “the lack of diagnostic measures” in the study itself91.
An interventional study which did not use cut‐offs to define post‐traumatic stress disorder concluded that treating distress was better than treating the categorical disorder29. Another interventional study which measured symptoms but not disorders tautologically concluded that the potential advantage of transdiagnostic interventions was a reduced need for disorder‐based assessments88. Some studies did apply cut‐offs but eventually did not use them for their main analyses48, 94.
Frequently, studies did not specify the exact ICD/DSM types of mental disorders that were investigated, but only referred to the general domains of psychotic disorders34, 106, substance induced disorders28, 34, 108, anxiety disorders23, 28, 54, 88, 93, 104, mood disorders23, 28, 48, 49, 54, 64, 88, 93, or mood and anxiety disorders54, 93. The specific ICD/DSM diagnostic codes were hardly ever reported.
The number of primary mental disorders investigated by each study was highly variable and overall relatively low, ranging from no evidence of mental disorders at all (13% of studies)24, 29, 70, 78, 82, 85, 86, 87, 88, 90, 91, 92, 95, 97 and one mental disorder (8% of studies)50, 59, 60, 61, 62, 63, 96, 109, 110, up to 353 mental disorders73 (median: four mental disorders per study). Similarly, the number of ICD‐defined diagnostic spectra was heterogeneous, ranging from zero (12% of studies)29, 70, 78, 82, 85, 86, 87, 88, 90, 91, 92, 95, 97 to ten73 (median: one spectrum) per study. The largest transdiagnostic study published to date leveraged an electronic case register to include 353 mental disorders clustered across ten spectra, representing all ICD‐10 mental disorders except organic mental disorders73. About one third of the studies (35%)29, 40, 70, 74, 76, 78, 81, 82, 85, 86, 87, 90, 91, 92, 94, 95, 96, 97, 98, 100, 101, 103, 105, 106, 107, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 122, 123, 124 included at least one non‐clinical sample.
Outcome measures
Only a minority (35%)23, 24, 25, 32, 34, 35, 36, 40, 48, 49, 51, 52, 53, 56, 57, 58, 59, 60, 61, 62, 64, 66, 67, 68, 73, 74, 83, 84, 88, 100, 103, 111, 112, 115, 125, 126, 127, 128 of studies explicitly acknowledged their primary outcome measure, which may be suggestive of suboptimal study quality. There was also a high variability in the number of primary outcome measures, ranging from one48 to thirteen81 (median: two measures) per study.
Definition of the transdiagnostic approach
The exact definition of the transdiagnostic construct per study is provided in Table 1. Only a minority of constructs (36%) involved multiple processes28, 37, 38, 48, 55, 59, 70, 72, 75, 76, 77, 79, 80, 85, 87, 91, 92, 96, 98, 100, 103, 106, 110, 111, 113, 114, 116, 119, 120, 121, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132. Most studies (81%) were descriptive in nature. Mechanistic constructs were more infrequent (19%)28, 32, 38, 48, 50, 51, 52, 53, 58, 70, 83, 103, 112, 113, 114, 115, 116, 117, 118, 131, 133, and causal transdiagnostic constructs were hardly ever reported (7%)24, 48, 50, 51, 52, 53, 58, 115 and only during the most recent years (2017‐2018).
The transdiagnostic construct was demonstrated across all clinical conditions investigated only in a minority (34%) of studies24, 27, 30, 32, 38, 42, 43, 45, 47, 50, 52, 53, 57, 58, 60, 61, 62, 63, 65, 71, 80, 83, 89, 96, 98, 109, 110, 111, 112, 113, 115, 117, 118, 123, 128, 129, 130, 133. It was demonstrated in a median of three conditions and one spectrum. Several studies did not clarify at all whether the construct was present in the conditions investigated. Overall, no clear universal transdiagnostic construct that could be valid across all mental disorders and diagnostic spectra was identified.
The statistical methods used to test the impact of the transdiagnostic construct encompassed analysis of variance/covariance, correlations, regressions and general linear models, mixed effect models, moderation and mediation analysis, principal component analysis, structural equation modelling, network analysis, and machine learning.
Less than half (44%) of the studies27, 33, 38, 58, 60, 61, 65, 72, 73, 74, 75, 77, 79, 80, 81, 83, 84, 89, 93, 98, 100, 101, 103, 105, 107, 108, 109, 111, 112, 113, 114, 115, 116, 117, 118, 119, 120, 121, 123, 124, 125, 126, 127, 128, 129, 130, 131, 132, 133 performed a statistical comparative assessment of the transdiagnostic approach versus a specific‐diagnostic approach. This problem was particularly relevant for interventional studies, half of which lacked a comparative specific‐diagnostic group. Overall, only 16% of them27, 33, 38, 58, 60, 61, 65, 83 performed a statistical comparative assessment. Some of these studies acknowledged that reliable conclusions regarding the diagnostic specificity of the findings could not be drawn34, 64. However, other interventional studies lacking both a control group and statistical comparative assessment eventually (over)stated that the transdiagnostic cognitive behavioral treatment was effective in improving outcomes40 or that it was more effective than the specific‐diagnostic approach29. When comparative analyses were available, they generally indicated similar effects of the transdiagnostic vs. the specific‐diagnostic intervention58, 60, 61, 83.
The qualitative appraisal of the transdiagnostic vs. specific‐diagnostic effects – when available – revealed further inconsistencies. For example, some predictive modelling studies indicated that the transdiagnostic approach was only able to explain an additional 1% of the variance109. Other studies acknowledged that the observed transdiagnostic effects were small in magnitude, but at the same time suggested developing transdiagnostic clinical interventions131.
In general, neuroscientific studies provided better descriptions of these effects. For example, one of them concluded that the transdiagnostic biotypes identified specific, coherent associations between symptoms, behavior, brain function, and real‐world function that cut across DSM‐IV defined diagnoses111. Other neuroscientific studies demonstrated shared neurobiological mechanisms across current categories of mental disorders108, 112, 113, 115, 117 or both specific and transdiagnostic effects across mental disorders74, 116, 129.
Quality assessment
A substantial proportion of studies (40%)23, 28, 29, 30, 37, 40, 47, 67, 69, 70, 71, 73, 75, 78, 80, 82, 83, 84, 85, 86, 87, 88, 93, 96, 97, 98, 100, 104, 105, 106, 107, 108, 109, 113, 114, 115, 116, 117, 118, 120, 124, 126, 128, 130 did not acknowledge an a priori protocol. There were very few studies reporting industry involvement (4%)52, 57, 103, 110, 111. Transdiagnostic findings were hardly ever externally replicated, with the exception of four studies (4%)73, 85, 93, 111. Other methodological weaknesses involved the use of clinical prediction methods (i.e., stepwise selection methods) that produce biased models82, 109, in particular in small databases80, 120, 131. The use of small samples80 also led to underpowered analyses across diagnostic subgroups133.
Some studies interpreted overfitted and not externally replicated models to favor transdiagnostic over disorder‐specific approaches76. Other studies conducted a large number of comparative analyses without controlling for multiple comparisons106. One study stated that participants were randomized, but eventually allocated them to a single treatment arm38. Another study re‐analyzed data from three previously published interventional studies that adopted different designs, without clarifying how the final database was amalgamated47.
Literature analysis
Mansell's transdiagnostic criteria
Only three studies (3%)98, 100, 117 met Mansell's transdiagnostic criteria. The most frequently unmet requirement was the demonstration of the transdiagnostic construct across all conditions investigated by the study.
Type of transdiagnostic approach
The majority of studies (82 out of 111, 74%) (Table 1) endorsed an across‐diagnoses approach. Of them, 33 (40%) were conducted within the same diagnostic spectrum (three of which also included a non‐clinical sample) and 49 (60%) were across different diagnostic spectra (22 of which also included a non‐clinical sample) (Table 1). Only three studies (3%)111, 126, 130 endorsed a beyond‐diagnoses approach. They were also the most methodologically sophisticated.
For most of these across/beyond‐diagnoses studies, the transdiagnostic approach was intertwined in the baseline recruitment of participants with different diagnoses. However, two studies (2%) defined their transdiagnostic approach through the inclusion of different diagnostic outcomes, as opposed to different patient groups at baseline (these studies were termed “transdiagnostic outcomes”)75, 77. Two other studies (2%)24, 51 defined their transdiagnostic approach as the overlap between physical (gastrointestinal, headache) and mental health (anxiety and depression) symptoms (these studies were termed “across physical and mental health diagnoses”).
Despite their self‐proclaimed transdiagnostic status, the remaining 22 studies (20%) were actually not transdiagnostic at all.
Eight studies (7%)70, 78, 82, 85, 87, 92, 95, 97 did not consider any ICD/DSM diagnostic information as gold standard nor defined any new diagnostic construct. These were usually population‐based studies which adopted a continuum rather than a categorical measurement of psychopathology, the results of which were completely unrelatable to any existing ICD/DSM category. Therefore, these studies were termed as being “a‐diagnostic” rather than transdiagnostic.
Five studies (5%)29, 86, 88, 90, 91 confounded symptoms and disorders. These studies explored only DSM or ICD‐related symptoms without any clear reference to diagnostic categories of mental disorders, and were therefore defined as “across symptoms” .
Nine studies (8%)50, 59, 60, 61, 62, 63, 96, 109, 110 were defined as “within the same diagnosis” . Six of them investigated comorbid disorders in addition to a single primary disorder: comorbid depression, generalized anxiety disorder and social anxiety disorder in addition to panic disorder60; comorbid depression, generalized anxiety disorder and panic disorder in addition to social anxiety disorder61; comorbid generalized anxiety disorder, panic disorder and social anxiety disorder in addition to major depressive disorder62; comorbid major depressive disorder, social anxiety disorder and panic disorder in addition to generalized anxiety disorder63; comorbid panic disorder, social anxiety disorder and generalized anxiety disorder in addition to major depression50; and multiple mental disorders in addition to binge eating disorder59. Another study investigated comorbid depressive and anxiety symptoms (but not disorders) in patients with post‐traumatic stress disorder110.
Two further studies used the investigated different subtypes (restricting type and binge eating type) of the same disorder (DSM‐IV anorexia nervosa)96 or different clinical states of the same disorder (never depressed, past depression, current depression)109.
Bibliometric analysis
Figure 3 illustrates the network of specific mental disorders that have been investigated by transdiagnostic research to date. A predominant focus on anxiety and depressive disorders is evident.
Figure 3.
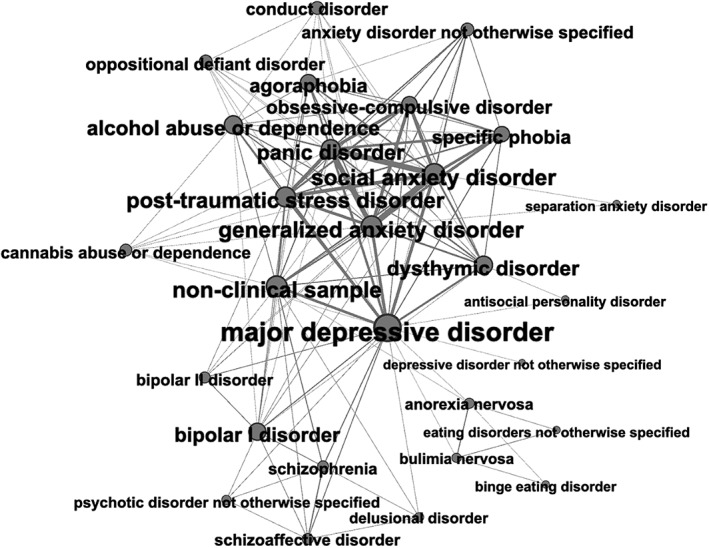
Network map of specific mental disorders analyzed by transdiagnostic research in psychiatry to date. Each node indicates a specific mental disorder, with the node's size reflecting how many different connections with other nodes were present. The thickness of the edges reflects the number of connections between a pair of nodes/mental disorders.
DISCUSSION
To the best of our knowledge, this is the most comprehensive review systematically appraising transdiagnostic research in psychiatry. The empirical analysis revealed that the transdiagnostic literature is heterogeneous and intrinsically incoherent. The bibliometric analysis showed that, to date, transdiagnostic research has focused on a limited number of mental disorders. The conceptual analysis leveraged these findings to demonstrate that, at present, transdiagnostic research does not represent a credible paradigm shift that can impact the classification of or clinical care for mental disorders.
This systematic review provides several lines of evidence showing that transdiagnostic approaches in psychiatry are heterogeneous. For example, only three studies out of 111 qualified as being truly transdiagnostic, according to established criteria21. This empirical test demonstrates that the transdiagnostic designation is applied in a loose and unstandardized way, encompassing a number of different and often conflicting conceptualizations.
Paradoxically, some of these approaches were intrinsically incoherent and incompatible with a transdiagnostic framework, because they investigated symptoms and not disorders (across‐symptoms), a single disorder (within‐disorder) or, to the extreme, reported no diagnostic information at all (a‐diagnostic).
Furthermore, transdiagnostic studies were often characterized by methodological weaknesses. For example, the exact ICD/DSM types of mental disorders were frequently poorly defined, raising the question of how the researchers could legitimately challenge the boundaries of mental disorders, if these were not even accurately determined. In addition, the boundaries between primary and comorbid disorders in transdiagnostic literature have often been blurred. Arguably, transdiagnostic approaches have been more heterogeneous, incoherent and paid less attention to the problem of comorbidities than the DSM/ICD diagnoses that were criticized for the very same problems.
The other key methodological caveat was that transdiagnostic studies often tested several outcomes, enhancing the likelihood of type I error from data fishing expeditions. This problem was amplified by the use of arbitrary cut‐offs to measure symptom severity134, a general lack of external replication studies, and by overenthusiastic interpretations of the results. In line with these arguments, there were only a few methodologically sound studies which have been able to identify robust mechanistic transdiagnostic constructs that were causally related with the outcome of interest.
Consistent with the above limitations, most transdiagnostic studies (excluding those not properly transdiagnostic, as noted above) limited their analyses to the search for shared features across a certain set of mental disorders (across‐diagnoses). However, the bibliometric analysis revealed that these studies remained almost entirely confined within the restricted original area of interest of transdiagnostic research: anxiety and depressive disorders.
No universal transdiagnostic process has been identified, and the extent to which transdiagnostic approaches could pragmatically benefit other mental disorders and diagnostic spectra is undetermined. In fact, only a few transdiagnostic studies have eventually tested new classification systems, beyond the existing gold standard (beyond‐diagnoses).
To date, the contribution of transdiagnostic literature to the development and validation of an alternative classification system, which has genuine clinical value – and which is not a “fudge”135 – has been negligible. Notably, transdiagnostic approaches have not replaced classification systems in any other branches of clinical medicine. On the contrary, continuous (transdiagnostic) and categorical (specific‐diagnostic) dimensions frequently co‐exist in organic medicine (e.g., vascular surgery)136, as well as in psychiatry (e.g., the new DSM‐5 dimensional approach to personality disorders137). In reality, transdiagnostic studies have also produced evidence to support the existence of diagnostic categories130, 138.
It is thus apparent that future extensive research in this field is greatly needed, in particular beyond‐diagnoses studies that include several diagnostic spectra. However, a key prerequisite would be to overcome the empirical weaknesses of current transdiagnostic research. To facilitate this outcome, we propose in Table 2 some pragmatic “TRANSD”iagnostic guidelines. We hope these guidelines will improve the consistency and quality of the next generation of transdiagnostic research.
Table 2.
“TRANSD”iagnostic research recommendations in psychiatry
| Transparent definition of the gold standard (ICD, DSM, other), including specific diagnostic types, official codes, primary vs. secondary diagnoses, diagnostic assessment interviews. |
| Report the primary outcome of the study, the study design and the definition of the transdiagnostic construct in the abstract and main text. |
| Appraise the conceptual framework/approach of the transdiagnostic approach: across‐diagnoses, beyond‐diagnoses, other (explain). |
| Numerate the diagnostic categories, spectra and non‐clinical samples in which the transdiagnostic construct is being tested and then validated. |
| Show the degree of improvement of the transdiagnostic approach against the specific diagnostic approach through specific comparative analyses. |
| Demonstrate the generalizability of the transdiagnostic construct through external validation studies. |
Transdiagnostic research is also affected by some significant conceptual weaknesses. First, it is less innovative than it often proclaims. The fundamental argument for transdiagnostic approaches is that diagnostic categories (mostly anxiety, depressive and eating disorders) are not discrete entities, because there are shared features cutting across them. However, twenty‐four years ago, when the DSM‐IV was released, an official disclaimer was added to its forefront: “there is no assumption that each category of mental disorder is a completely discrete entity with absolute boundaries dividing it from other mental disorders”139.
It has to be considered that current polythetic (i.e., based on a list of symptoms and signs believed to be characteristic140) diagnostic categories originate in prototypical descriptions containing a core structure (gestalt) of the disorder and its polysymptomatic manifestations. Accordingly, the boundaries of mental disorders, as illustrated in Figure 1, are dotted, not solid. Unfortunately, psychiatric knowledge has overlooked these issues and, over the ensuing two decades, the abstract (rather than physical) nature of DSM‐IV categories141 has been reified to the point that they are often seen as real ontological entities, discrete and demarcated from each other by distinct boundaries.
During this process, the symptoms shared by two or several mental disorders tended to be omitted from the diagnostic lists, in order to strengthen the clinical distinctiveness of the categories140. Therefore, transdiagnostic research represents more of a rediscovery of what has been forgotten from prototypical descriptions as well as the consequence of the diagnostic reification. In fact, it would make no sense to challenge the diagnostic boundaries without assuming that these do exist on some ontological level.
Second, transdiagnostic approaches are largely based on an epistemological error, which triggers an illusion of continuity142. The devaluation143 and simplification of psychopathological phenomena – introduced by recent versions of the DSM and ICD – to brief, ordinary, non‐technical lay language descriptions, has converted complex symptoms and psychic phenomena into phenomenological primitives or homogeneous elementals140. For example, there is only one kind of depressive state, one kind of anxiety, one kind of delusion, and it is assumed that all of these states share the same phenomenological structure when they are observed in different mental disorders140. Consequently, mental disorders, solely constituted by aggregates of such elementals, lose their characteristic salience, and their clinical boundaries become blurred140.
An illustrative example is provided by the use of self‐report psychometric scales that – not surprisingly – are frequently adopted in transdiagnostic research in order to reduce psychopathology to elementals. Some studies measured the severity of “a specific symptom of depression”78 in children through self‐reported lay statements such as “I am sad once in a while” , “I am sad many times” and “I am sad all the time”78. The trivialization of the contextual significance of these statements144 (there are potentially infinite reasons why one could feel sad), is associated with the deprivation of any phenomenological framework (e.g., subjective appraisal of sadness, level of insight, presence of existential despair, perception of time)145, 146. Such a simplification process transforms these statements into self‐contained atomic symptoms147, which become highly blurred and aspecific, in contrast with the claim of the authors that they are specific symptoms. This point is empirically confirmed by the fact that transdiagnostic literature frequently confounded the measurement of psychometric items in non‐clinical samples with clinical symptoms and/or established mental disorders.
Third, the highest interest and biggest clinical contribution of transdiagnostic research has been in the development of emotion‐focused cognitive behavioral therapy (CBT) protocols (e.g., the Unified Protocol58) for anxiety disorders. A recent meta‐analysis indicated that these transdiagnostic treatments lack clinical superiority compared to diagnostic‐specific treatments148.
Although these results and the Unified Protocol are presented as a breakthrough, they are again more like a rediscovery. In fact, psychotherapy was broadly transdiagnostic, driven by a psychoanalytical focus on core emotional issues (termed neurotic conflicts) until 1980, when the DSM‐III initiated a gradual splitting of psychopathology into psychiatric categories149. This led to an outpouring of CBT diagnosis‐specific protocols, which have allowed CBT to balkanize and dominate the psychotherapeutic landscape for over two decades149. In this context, some authors have interpreted the Unified Protocol as the end of the CBT‐centric dominion and as the resurgence of psychodynamic psychotherapies149.
This review has some limitations. Because of the intrinsic heterogeneity in the design, methodology and topic covered, we were unable to perform quantitative analyses. However, our main aim was to provide an extensive, detailed snapshot of transdiagnostic research and not to produce summary estimates. Furthermore, there are most probably other studies that have implicitly employed transdiagnostic approaches which have not been included in this review. However, to deconstruct the core characteristics of transdiagnostic research, we selectively focused on those studies that have explicitly acknowledged transdiagnostic approaches as their core distinctive features in their titles.
In conclusion, transdiagnostic research in psychiatry has, to date, been overenthusiastic and undercritical, heterogeneous, intrinsically incoherent and predominantly focused on a limited subset of mental disorders. It is grounded more in rediscoveries than true innovations, and it is demonstrably affected by conceptual biases. Medicine has always worked by a gradual evolutionary evidence‐based process and, before rejecting time‐tested and progressively refined concepts that are rooted in clinical tradition5, 102, a reliable and valid alternative is needed150.
To date, transdiagnostic approaches have not delivered the substantial empirical clinical “meat”135 required for them to represent a credible paradigm shift5. The risk of an acritical endorsement of transdiagnostic approaches would be to throw the baby out with the bathwater151 and be lost in a controversial102 mare magnum of diagnostic uncertainty that may be deleterious for patients and clinicians5.
Transdiagnostic research has promised (too) much to psychiatry. It is hoped that this review will guide the next generation of transdiagnostic research to complement, refine and improve – less likely to replace5, 136 – the way we currently classify and treat mental disorders.
ACKNOWLEDGEMENTS
This study was supported by a King's College London Confidence in Concept Award from the UK Medical Research Council (MC_PC_16048) to P. Fusar‐Poli. M. Solmi and N. Brondino contributed equally to this work.
REFERENCES
- 1. van den Tweel JG, Taylor CR. A brief history of pathology: preface to a forthcoming series that highlights milestones in the evolution of pathology as a discipline. Virchows Arch 2010;457:3‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kendler KS. An historical framework for psychiatric nosology. Psychol Med 2009;39:1935‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kendler KS. Classification of psychopathology: conceptual and historical background. World Psychiatry 2018;17:241‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lawrie SM, O'Donovan MC, Saks E et al. Improving classification of psychoses. Lancet Psychiatry 2016;3:367‐74. [DOI] [PubMed] [Google Scholar]
- 5. Maj M. Why the clinical utility of diagnostic categories in psychiatry is intrinsically limited and how we can use new approaches to complement them. World Psychiatry 2018;17:121‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reed GM, Sharan P, Rebello TJ et al. The ICD‐11 developmental field study of reliability of diagnoses of high‐burden mental disorders: results among adult patients in mental health settings of 13 countries. World Psychiatry 2018;17:174‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. First MB, Rebello TJ, Keeley JW et al. Do mental health professionals use diagnostic classifications the way we think they do? A global survey. World Psychiatry 2018;17:187‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Treccani Institute . http://www.treccani.it/vocabolario/trans/.
- 9. Fairburn CG, Harrison PJ. Eating disorders. Lancet 2003;361:407‐16. [DOI] [PubMed] [Google Scholar]
- 10. Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther 2003;41:509‐28. [DOI] [PubMed] [Google Scholar]
- 11. Norton PJ, Hayes SA, Hope DA. Effects of a transdiagnostic group treatment for anxiety on secondary depression. Depress Anxiety 2004;20:198‐202. [DOI] [PubMed] [Google Scholar]
- 12. Norton PJ, Philipp LM. Transdiagnostic approaches to the treatment of anxiety disorders: a quantitative review. Psychotherapy 2008;45:214‐26. [DOI] [PubMed] [Google Scholar]
- 13. Norton PJ, Hope DA. Preliminary evaluation of a broad‐spectrum cognitive‐behavioral group therapy for anxiety. J Behav Ther Exp Psychiatry 2005;36:79‐97. [DOI] [PubMed] [Google Scholar]
- 14. Clark DA. Cognitive behavioral therapy for anxiety and depression: possibilities and limitations of a transdiagnostic perspective. Cogn Behav Ther 2009;38(Suppl. 1):29‐34. [PubMed] [Google Scholar]
- 15. Newby JM, McKinnon A, Kuyken W et al. Systematic review and meta‐analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev 2015;40:91‐110. [DOI] [PubMed] [Google Scholar]
- 16. Caspi A, Houts RM, Belsky DW et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci 2014;2:119‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cuthbert BN. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry 2014;13:28‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Scott J, Leboyer M, Hickie I et al. Clinical staging in psychiatry: a cross‐cutting model of diagnosis with heuristic and practical value. Br J Psychiatry 2013;202:243‐5. [DOI] [PubMed] [Google Scholar]
- 19. Moher D, Liberati A, Tetzlaff J et al. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA Statement. J Clin Epidemiol 2009;62:1006‐12. [DOI] [PubMed] [Google Scholar]
- 20. Cipriani A, Zhou X, Del Giovane C et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta‐analysis. Lancet 2016;388:881‐90. [DOI] [PubMed] [Google Scholar]
- 21. Mansell M, Harvey A, Watkins E et al. Conceptual foundations of the transdiagnostic approach to CBT. J Cogn Psychother 2009;23:6‐19. [Google Scholar]
- 22. Sauer‐Zavala S, Gutner CA, Farchione TJ et al. Current definitions of “transdiagnostic” in treatment development: a search for consensus. Behav Ther 2017;48:128‐38. [DOI] [PubMed] [Google Scholar]
- 23. van Dijk SDM, Bouman R, Lam J et al. Outcome of day treatment for older adults with affective disorders: an observational pre‐post design of two transdiagnostic approaches. Int J Geriatr Psychiatry 2018;33:510‐6. [DOI] [PubMed] [Google Scholar]
- 24. Dear BF, Fogliati VJ, Fogliati R et al. Transdiagnostic internet‐delivered cognitive‐behaviour therapy (CBT) for adults with functional gastrointestinal disorders (FGID): a feasibility open trial. J Psychosom Res 2018;108:61‐9. [DOI] [PubMed] [Google Scholar]
- 25. Talkovsky AM, Paulus DJ, Kuang F et al. Quality of life outcomes following transdiagnostic group cognitive‐behavioral therapy for anxiety. Int J Cogn Ther 2017;10:93‐114. [Google Scholar]
- 26. Talkovsky AM, Green KL, Osegueda A et al. Secondary depression in transdiagnostic group cognitive behavioral therapy among individuals diagnosed with anxiety disorders. J Anxiety Disord 2017;46:56‐64. [DOI] [PubMed] [Google Scholar]
- 27. Smith AH, Paulus DJ, Norton PJ. Transdiagnostic assessment of anxiety symptoms using the Anxiety Disorder Diagnostic Questionnaire ‐ weekly version. Anxiety Stress Coping 2017;30:96‐106. [DOI] [PubMed] [Google Scholar]
- 28. Pitman SR, Hilsenroth MJ, Weinberger J et al. Psychotherapy technique related to changes in anxiety symptoms with a transdiagnostic sample. J Nerv Ment Dis 2017;205:427‐35. [DOI] [PubMed] [Google Scholar]
- 29. Hamblen JL, Norris FH, Symon KA et al. Cognitive behavioral therapy for postdisaster distress: a promising transdiagnostic approach to treating disaster survivors. Psychol Trauma Theory Res Pract Policy 2017;9:130‐6. [DOI] [PubMed] [Google Scholar]
- 30. Gros DF, Szafranski DD, Shead SD. A real world dissemination and implementation of transdiagnostic behavior therapy (TBT) for veterans with affective disorders. J Anxiety Disord 2017;46:72‐7. [DOI] [PubMed] [Google Scholar]
- 31. Espejo EP, Gorlick A, Castriotta N. Changes in threat‐related cognitions and experiential avoidance in group‐based transdiagnostic CBT for anxiety disorders. J Anxiety Disord 2017;46:65‐71. [DOI] [PubMed] [Google Scholar]
- 32. Talkovsky AM, Norton PJ. Intolerance of uncertainty and transdiagnostic group cognitive behavioral therapy for anxiety. J Anxiety Disord 2016;41:108‐14. [DOI] [PubMed] [Google Scholar]
- 33. McEvoy PM, Erceg‐Hurn DM. The search for universal transdiagnostic and trans‐therapy change processes: evidence for intolerance of uncertainty. J Anxiety Disord 2016;41:96‐107. [DOI] [PubMed] [Google Scholar]
- 34. Kristjansdottir H, Salkovskis PM, Sigurdsson BH et al. Transdiagnostic cognitive behavioural treatment and the impact of co‐morbidity: an open trial in a cohort of primary care patients. Nord J Psychiatry 2016;70:215‐23. [DOI] [PubMed] [Google Scholar]
- 35. Ito M, Horikoshi M, Kato N et al. Transdiagnostic and transcultural: pilot study of unified protocol for depressive and anxiety disorders in Japan. Behav Ther 2016;47:416‐30. [DOI] [PubMed] [Google Scholar]
- 36. Hadjistavropoulos HD, Nugent MM, Alberts NM et al. Transdiagnostic Internet‐delivered cognitive behaviour therapy in Canada: an open trial comparing results of a specialized online clinic and nonspecialized community clinics. J Anxiety Disord 2016;42:19‐29. [DOI] [PubMed] [Google Scholar]
- 37. Asnaani A, Kaczkurkin AN, Tannahill H et al. Moderators of change in social anxiety during CBT in a transdiagnostic, naturalistic treatment‐seeking sample. J Exper Psychopathol 2016;7:655‐70. [Google Scholar]
- 38. Talkovsky AM, Norton PJ. Mediators of transdiagnostic group cognitive behavior therapy. J Anxiety Disord 2014;28:919‐24. [DOI] [PubMed] [Google Scholar]
- 39. Queen AH, Barlow DH, Ehrenreich‐May J. The trajectories of adolescent anxiety and depressive symptoms over the course of a transdiagnostic treatment. J Anxiety Disord 2014;28:511‐21. [DOI] [PubMed] [Google Scholar]
- 40. Newby JM, Mewton L, Williams AD et al. Effectiveness of transdiagnostic internet cognitive behavioural treatment for mixed anxiety and depression in primary care. J Affect Disord 2014;165:45‐52. [DOI] [PubMed] [Google Scholar]
- 41. Gros DF. Development and initial evaluation of Transdiagnostic Behavior Therapy (TBT) for veterans with affective disorders. Psychiatry Res 2014;220:275‐82. [DOI] [PubMed] [Google Scholar]
- 42. Bullis JR, Fortune MR, Farchione TJ et al. A preliminary investigation of the long‐term outcome of the Unified Protocol for transdiagnostic treatment of emotional disorders. Compr Psychiatry 2014;55:1920‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Boswell JF, Farchione TJ, Sauer‐Zavala S et al. Anxiety sensitivity and interoceptive exposure: a transdiagnostic construct and change strategy. Behav Ther 2013;44:417‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bilek EL, Ehrenreich‐May J. An open trial investigation of a transdiagnostic group treatment for children with anxiety and depressive symptoms. Behav Ther 2012;43:887‐97. [DOI] [PubMed] [Google Scholar]
- 45. Norton PJ. An open trial of a transdiagnostic cognitive‐behavioral group therapy for anxiety disorder. Behav Ther 2008;39:242‐50. [DOI] [PubMed] [Google Scholar]
- 46. Norton PJ, Hayes SA, Springer JR. Transdiagnostic cognitive‐behavioral group therapy for anxiety: outcome and process. Int J Cogn Ther 2008;1:266‐79. [Google Scholar]
- 47. Norton PJ, Barrera TL, Mathew AR et al. Effect of transdiagnostic CBT for anxiety disorders on comorbid diagnoses. Depress Anxiety 2013;30:168‐73. [DOI] [PubMed] [Google Scholar]
- 48. Capobianco L, Reeves D, Morrison AP et al. Group metacognitive therapy vs. mindfulness meditation therapy in a transdiagnostic patient sample: a randomised feasibility trial. Psychiatry Res 2018;259:554‐61. [DOI] [PubMed] [Google Scholar]
- 49. Zwerenz R, Becker J, Johansson R et al. Transdiagnostic, psychodynamic web‐based self‐help intervention following inpatient psychotherapy: results of a feasibility study and randomized controlled trial. JMIR Mental Health 2017;4:e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zemestani M, Imani M, Ottaviani C. A preliminary investigation on the effectiveness of unified and transdiagnostic cognitive behavior therapy for patients with comorbid depression and anxiety. Int J Cogn Ther 2017;10:175‐85. [Google Scholar]
- 51. Sharma P, Mehta M, Sagar R. Efficacy of transdiagnostic cognitive‐behavioral group therapy for anxiety disorders and headache in adolescents. J Anxiety Disord 2017;46:78‐84. [DOI] [PubMed] [Google Scholar]
- 52. Schroder J, Jelinek L, Moritz S. A randomized controlled trial of a transdiagnostic Internet intervention for individuals with panic and phobias – One size fits all. J Behav Ther Exper Psychiatry 2017;54:17‐24. [DOI] [PubMed] [Google Scholar]
- 53. Riccardi CJ, Korte KJ, Schmidt NB. False Safety Behavior Elimination Therapy: a randomized study of a brief individual transdiagnostic treatment for anxiety disorders. J Anxiety Disord 2017;46:35‐45. [DOI] [PubMed] [Google Scholar]
- 54. Maia A, Sanford J, Boettcher H et al. Improvement in quality of life and sexual functioning in a comorbid sample after the unified protocol transdiagnostic group treatment. J Psychiatr Res 2017;93:30‐6. [DOI] [PubMed] [Google Scholar]
- 55. LeBouthillier DM, Asmundson GJG. The efficacy of aerobic exercise and resistance training as transdiagnostic interventions for anxiety‐related disorders and constructs: a randomized controlled trial. J Anxiety Disord 2017;52:43‐52. [DOI] [PubMed] [Google Scholar]
- 56. Ellard KK, Bernstein EE, Hearing C et al. Transdiagnostic treatment of bipolar disorder and comorbid anxiety using the Unified Protocol for Emotional Disorders: a pilot feasibility and acceptability trial. J Affect Disord 2017;219:209‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Berger T, Urech A, Krieger T et al. Effects of a transdiagnostic unguided Internet intervention (‘velibra') for anxiety disorders in primary care: results of a randomized controlled trial. Psychol Med 2017;47:67‐80. [DOI] [PubMed] [Google Scholar]
- 58. Barlow DH, Farchione TJ, Bullis JR et al. The unified protocol for transdiagnostic treatment of emotional disorders compared with diagnosis‐specific protocols for anxiety disorders: a randomized clinical trial. JAMA Psychiatry 2017;74:875‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. McIntosh VVW, Jordan J, Carter JD et al. Psychotherapy for transdiagnostic binge eating: a randomized controlled trial of cognitive‐behavioural therapy, appetite‐focused cognitive‐behavioural therapy, and schema therapy. Psychiatry Res 2016;240:412‐20. [DOI] [PubMed] [Google Scholar]
- 60. Fogliati VJ, Dear BF, Staples LG et al. Disorder‐specific versus transdiagnostic and clinician‐guided versus self‐guided internet‐delivered treatment for panic disorder and comorbid disorders: a randomized controlled trial. J Anxiety Disord 2016;39:88‐102. [DOI] [PubMed] [Google Scholar]
- 61. Dear BF, Staples LG, Terides MD et al. Transdiagnostic versus disorder‐specific and clinician‐guided versus self‐guided internet‐delivered treatment for social anxiety disorder and comorbid disorders: a randomized controlled trial. J Anxiety Disord 2016;42:30‐44. [DOI] [PubMed] [Google Scholar]
- 62. Titov N, Dear BF, Staples LG et al. Disorder‐specific versus transdiagnostic and clinician‐guided versus self‐guided treatment for major depressive disorder and comorbid anxiety disorders: a randomized controlled trial. J Anxiety Disord 2015;35:88‐102. [DOI] [PubMed] [Google Scholar]
- 63. Dear BF, Staples LG, Terides MD et al. Transdiagnostic versus disorder‐specific and clinician‐guided versus self‐guided internet‐delivered treatment for generalized anxiety disorder and comorbid disorders: a randomized controlled trial. J Anxiety Disord 2015;36:63‐77. [DOI] [PubMed] [Google Scholar]
- 64. Ebert D, Tarnowski T, Gollwitzer M et al. A transdiagnostic internet‐based maintenance treatment enhances the stability of outcome after inpatient cognitive behavioral therapy: a randomized controlled trial. Psychother Psychosom 2013;82:246‐56. [DOI] [PubMed] [Google Scholar]
- 65. Norton PJ, Barrera TL. Transdiagnostic versus diagnosis‐specific CBT for anxiety disorders: a preliminary randomized controlled noninferiority trial. Depress Anxiety 2012;29:874‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Norton PJ. A randomized clinical trial of transdiagnostic cognitive‐behavioral treatments for anxiety disorder by comparison to relaxation training. Behav Ther 2012;43:506‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Farchione TJ, Fairholme CP, Ellard KK et al. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav Ther 2012;43:666‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Fairburn CG, Cooper Z, Doll HA et al. Transdiagnostic cognitive‐behavioral therapy for patients with eating disorders: a two‐site trial with 60‐week follow‐up. Am J Psychiatry 2009;166:311‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Pellizzer ML, Waller G, Wade TD. Body image flexibility: a predictor and moderator of outcome in transdiagnostic outpatient eating disorder treatment. Int J Eat Disord 2018;51:368‐72. [DOI] [PubMed] [Google Scholar]
- 70. Wigman JTW, de Vos S, Wichers M et al. A transdiagnostic network approach to psychosis. Schizophr Bull 2017;43:122‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Shinn AK, Bolton KW, Karmacharya R et al. McLean OnTrack: a transdiagnostic program for early intervention in first‐episode psychosis. Early Interv Psychiatry 2017;11:83‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Platt JM, Colich NL, McLaughlin KA et al. Transdiagnostic psychiatric disorder risk associated with early age of menarche: a latent modeling approach. Compr Psychiatry 2017;79:70‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Fusar‐Poli P, Rutigliano G, Stahl D et al. Development and validation of a clinically based risk calculator for the transdiagnostic prediction of psychosis. JAMA Psychiatry 2017;74:493‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Philip NS, Tyrka AR, Albright SE et al. Early life stress predicts thalamic hyperconnectivity: a transdiagnostic study of global connectivity. J Psychiatr Res 2016;79:93‐100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Conway CC, Starr LR, Espejo EP et al. Stress responsivity and the structure of common mental disorders: transdiagnostic internalizing and externalizing dimensions are associated with contrasting stress appraisal biases. J Abnorm Psychol 2016;125:1079‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Latack JA, Rodriguez‐Seijas C, Stohl M et al. Transdiagnostic psychopathology mediates the relationship between childhood sexual abuse and HIV/AIDS and other sexually transmitted infections in adulthood. Compr Psychiatry 2015;62:71‐9. [DOI] [PubMed] [Google Scholar]
- 77. Starr LR, Conway CC, Hammen CL et al. Transdiagnostic and disorder‐specific models of intergenerational transmission of internalizing pathology. Psychol Med 2014;44:161‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. McLaughlin KA, Aldao A, Wisco BE et al. Rumination as a transdiagnostic factor underlying transitions between internalizing symptoms and aggressive behavior in early adolescents. J Abnorm Psychol 2014;123:13‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Conway CC, Hammen C, Brennan PA. Expanding stress generation theory: test of a transdiagnostic model. J Abnorm Psychol 2012;121:754‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. McFarlane T, Olmsted MP, Trottier K. Timing and prediction of relapse in a transdiagnostic eating disorder sample. Int J Eat Disord 2008;41:587‐93. [DOI] [PubMed] [Google Scholar]
- 81. Wade TD, Bergin JL, Martin NG et al. A transdiagnostic approach to understanding eating disorders. J Nerv Ment Dis 2006;194:510‐17. [DOI] [PubMed] [Google Scholar]
- 82. McEvoy PM, Hyett MP, Ehring T et al. Transdiagnostic assessment of repetitive negative thinking and responses to positive affect: structure and predictive utility for depression, anxiety, and mania symptoms. J Affect Disord 2018;232:375‐84. [DOI] [PubMed] [Google Scholar]
- 83. Newby JM, Mewton L, Andrews G. Transdiagnostic versus disorder‐specific internet‐delivered cognitive behaviour therapy for anxiety and depression in primary care. J Anxiety Disord 2017;46:25‐34. [DOI] [PubMed] [Google Scholar]
- 84. Lee RSC, Hermens DF, Scott J et al. A transdiagnostic study of education, employment, and training outcomes in young people with mental illness. Psychol Med 2017;47:2061‐70. [DOI] [PubMed] [Google Scholar]
- 85. Hankin BL, Davis EP, Snyder H et al. Temperament factors and dimensional, latent bifactor models of child psychopathology: transdiagnostic and specific associations in two youth samples. Psychiatr Res 2017;252:139‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gibson LE, Cooper S, Reeves LE et al. The association between traumatic life events and psychological symptoms from a conservative, transdiagnostic perspective. Psychiatry Res 2017;252:70‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Chasson GS, Bello MS, Luxon AM et al. Transdiagnostic emotional vulnerabilities linking obsessive‐compulsive and depressive symptoms in a community‐based sample of adolescents. Depress Anxiety 2017;34:761‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Morris L, Mansell W, Emsley R et al. Prospective cohort feasibility study of a transdiagnostic group intervention for common mental health problems: The Take Control Course. Psychol Psychother Theory Res Pract 2016;89:163‐80. [DOI] [PubMed] [Google Scholar]
- 89. Holliday SB, Pedersen ER, Leventhal AM. Depression, posttraumatic stress, and alcohol misuse in young adult veterans: the transdiagnostic role of distress tolerance. Drug Alcohol Depend 2016;161:348‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Thibodeau MA, Carleton RN, McEvoy PM et al. Developing scales measuring disorder‐specific intolerance of uncertainty (DSIU): a new perspective on transdiagnostic. J Anxiety Disord 2015;31:49‐57. [DOI] [PubMed] [Google Scholar]
- 91. Tang‐Smith E, Johnson SL, Chen S. The dominance behavioural system: a multidimensional transdiagnostic approach. Psychol Psychother Theory Res Pract 2015;88:394‐411. [DOI] [PubMed] [Google Scholar]
- 92. Cameron C, Kaplan RA, Rossell SL. An investigation of a novel transdiagnostic model of delusions in a group with positive schizotypal symptoms. Cogn Neuropsychiatry 2014;19:285‐304. [DOI] [PubMed] [Google Scholar]
- 93. Bohnke JR, Lutz W, Delgadillo J. Negative affectivity as a transdiagnostic factor in patients with common mental disorders. J Affect Disord 2014;166:270‐8. [DOI] [PubMed] [Google Scholar]
- 94. Johnson SL, Carver CS, Joormann J. Impulsive responses to emotion as a transdiagnostic vulnerability to internalizing and externalizing symptoms. J Affect Disord 2013;150:872‐8. [DOI] [PubMed] [Google Scholar]
- 95. Hoiles KJ, Egan SJ, Kane RT. The validity of the transdiagnostic cognitive behavioural model of eating disorders in predicting dietary restraint. Eating Behav 2012;13:123‐6. [DOI] [PubMed] [Google Scholar]
- 96. Innis SM, Birmingham CL, Harbottle EJ. Are plasma homocysteine and methionine elevated when binging and purging behavior complicates anorexia nervosa? Evidence against the transdiagnostic theory of eating disorders. Eat Weight Disord 2009;14:e184‐9. [DOI] [PubMed] [Google Scholar]
- 97. Brown GP, Roach A, Irving L et al. Personal meaning: a neglected transdiagnostic construct. Int J Cogn Ther 2008;1:223‐36. [Google Scholar]
- 98. Bentall RP, Rouse G, Kinderman P et al. Paranoid delusions in schizophrenia spectrum disorders and depression – the transdiagnostic role of expectations of negative events and negative self‐esteem. J Nerv Ment Dis 2008;196:375‐83. [DOI] [PubMed] [Google Scholar]
- 99. Maia A, Nardi AE, Cardoso A. The utilization of unified protocols in behavioral cognitive therapy in transdiagnostic group subjects: a clinical trial. J Affect Dis 2015;172:179‐83. [DOI] [PubMed] [Google Scholar]
- 100. Bentall RP, Rowse G, Shryane N et al. The cognitive and affective structure of paranoid delusions: a transdiagnostic investigation of patients with schizophrenia spectrum disorders and depression. Arch Gen Psychiatry 2009;66:236‐47. [DOI] [PubMed] [Google Scholar]
- 101. Corral‐Frias NS, Nikolova YS, Michalski LJ et al. Stress‐related anhedonia is associated with ventral striatum reactivity to reward and transdiagnostic psychiatric symptomatology. Psychol Med 2015;45:2605‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Lawrie SM, Hall J, McIntosh AM et al. The ‘continuum of psychosis': scientifically unproven and clinically impractical. Br J Psychiatry 2010;197:423‐5. [DOI] [PubMed] [Google Scholar]
- 103. Pietrzak RH, Naganawa M, Huang YY et al. Association of in vivo k‐opioid receptor availability and the transdiagnostic dimensional expression of trauma‐related psychopathology. JAMA Psychiatry 2014;71:1262‐70. [DOI] [PubMed] [Google Scholar]
- 104. Nota JA, Coles ME. Shorter sleep duration and longer sleep onset latency are related to difficulty disengaging attention from negative emotional images in individuals with elevated transdiagnostic repetitive negative thinking. J Behav Ther Exper Psychiatry 2018;58:114‐22. [DOI] [PubMed] [Google Scholar]
- 105. Ciaramidaro A, Bolte S, Schlitt S et al. Transdiagnostic deviant facial recognition for implicit negative emotion in autism and schizophrenia. Eur Neuropsychopharmacol 2018;28:264‐75. [DOI] [PubMed] [Google Scholar]
- 106. Stanton K, Rozek DC, Stasik‐O'Brien SM et al. A transdiagnostic approach to examining the incremental predictive power of emotion regulation and basic personality dimensions. J Abnorm Psychol 2016;125:960‐75. [DOI] [PubMed] [Google Scholar]
- 107. Conway CC, Hammen C, Brennan PA. Optimizing prediction of psychosocial and clinical outcomes with a transdiagnostic model of personality disorder. J Pers Disord 2016;30:545‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Sabharwal A, Szekely A, Kotov R et al. Transdiagnostic neural markers of emotion‐cognition interaction in psychotic disorders. J Abnorm Psychol 2016;125:907‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Samtani S, McEvoy PM, Mahoney AEJ et al. Examining a transdiagnostic measure of repetitive thinking in depressed, formerly depressed and never‐depressed individuals. J Affect Disord 2018;229:515‐22. [DOI] [PubMed] [Google Scholar]
- 110. Pietrzak RH, Rosenheck RA, Cramer JA et al. Elucidating the transdiagnostic dimensional structure of trauma‐related psychopathology: findings from VA cooperative study 504 ‐ risperidone treatment for military service related chronic post traumatic stress disorder. J Affect Disord 2015;172:331‐6. [DOI] [PubMed] [Google Scholar]
- 111. Grisanzio KA, Goldstein‐Piekarski AN, Wang MY et al. Transdiagnostic symptom clusters and associations with brain, behavior, and daily function in mood, anxiety, and trauma disorders. JAMA Psychiatry 2018;75:201‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Sheffield JM, Kandala S, Tamminga CA et al. Transdiagnostic associations between functional brain network integrity and cognition. JAMA Psychiatry 2017;74:605‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. MacNamara A, Klumpp H, Kennedy AE et al. Transdiagnostic neural correlates of affective face processing in anxiety and depression. Depress Anxiety 2017;34:621‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Keil V, Asbrand J, Tuschen‐Caffier B et al. Children with social anxiety and other anxiety disorders show similar deficits in habitual emotional regulation: evidence for a transdiagnostic phenomenon. Eur Child Adolesc Psychiatry 2017;26:749‐57. [DOI] [PubMed] [Google Scholar]
- 115. Jauhar S, Nour MM, Veronese M et al. A test of the transdiagnostic dopamine hypothesis of psychosis using positron emission tomographic imaging in bipolar affective disorder and schizophrenia. JAMA Psychiatry 2017;74:1206‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Gong QY, Hu XY, Pettersson‐Yeo W et al. Network‐level dysconnectivity in drug‐naive first‐episode psychosis: dissociating transdiagnostic and diagnosis‐specific alterations. Neuropsychopharmacology 2017;42:933‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Feldker K, Heitmann CY, Neumeister P et al. Transdiagnostic brain responses to disorder‐related threat across four psychiatric disorders. Psychol Med 2017;47:730‐43. [DOI] [PubMed] [Google Scholar]
- 118. Chen X, Liu C, He H et al. Transdiagnostic differences in the resting‐state functional connectivity of the prefrontal cortex in depression and schizophrenia. J Affect Disord 2017;217:118‐24. [DOI] [PubMed] [Google Scholar]
- 119. Sunderland M, Carragher N, Chapman C et al. The shared and specific relationships between exposure to potentially traumatic events and transdiagnostic dimensions of psychopathology. J Anxiety Disord 2016;38:102‐9. [DOI] [PubMed] [Google Scholar]
- 120. Bedwell JS, Butler PD, Chan CC et al. Transdiagnostic psychiatric symptoms related to visual evoked potential abnormalities. Psychiatry Res 2015;230:262‐70. [DOI] [PubMed] [Google Scholar]
- 121. Spielberg JM, Miller GA, Warren SL et al. Transdiagnostic dimensions of anxiety and depression moderate motivation‐related brain networks during goal maintenance. Depress Anxiety 2014;31:805‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. McEvoy PM, Thibodeau MA, Asmundson GJG. Trait repetitive negative thinking: a brief transdiagnostic assessment. J Exper Psychopathol 2014;5:382‐98. [Google Scholar]
- 123. Hagenaars MA, van Minnen A, Hoogduin CAL et al. A transdiagnostic comparison of trauma and panic memories in PTSD, panic disorder, and healthy controls. J Behav Ther Exper Psychiatry 2009;40:412‐22. [DOI] [PubMed] [Google Scholar]
- 124. Corcoran R, Rowse G, Moore R et al. A transdiagnostic investigation of ‘theory of mind' and ‘jumping to conclusions' in patients with persecutory delusions. Psychol Med 2008;38:1577‐83. [DOI] [PubMed] [Google Scholar]
- 125. Goldschmidt AB, Crosby RD, Cao L et al. Network analysis of pediatric eating disorder symptoms in a treatment‐seeking, transdiagnostic sample. J Abnorm Psychol 2018;127:251‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Forbush KT, Hagan KE, Kite BA et al. Understanding eating disorders within internalizing psychopathology: a novel transdiagnostic, hierarchical‐dimensional model. Compr Psychiatry 2017;79:40‐52. [DOI] [PubMed] [Google Scholar]
- 127. Rodriguez‐Seijas C, Stohl M, Hasin DS et al. Transdiagnostic factors and mediation of the relationship between perceived racial discrimination and mental disorders. JAMA Psychiatry 2015;72:706‐13. [DOI] [PubMed] [Google Scholar]
- 128. Vann A, Strodl E, Anderson E. The transdiagnostic nature of metacognitions in women with eating disorders. Eat Disord 2014;22:306‐20. [DOI] [PubMed] [Google Scholar]
- 129. Curzio O, Maestro S, Rossi G et al. Transdiagnostic vs. disorder‐focused perspective in children and adolescents with eating disorders: findings from a large multisite exploratory study. Eur Psychiatry 2018;49:81‐93. [DOI] [PubMed] [Google Scholar]
- 130. Reininghaus U, Bohnke JR, Hosang G et al. Evaluation of the validity and utility of a transdiagnostic psychosis dimension encompassing schizophrenia and bipolar disorder. Br J Psychiatry 2016;209:107‐13. [DOI] [PubMed] [Google Scholar]
- 131. Hsu KJ, Beard C, Rifkin L et al. Transdiagnostic mechanisms in depression and anxiety: the role of rumination and attentional control. J Affect Disord 2015;188:22‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. McEvoy PM, Watson H, Watkins ER et al. The relationship between worry, rumination, and comorbidity: evidence for repetitive negative thinking as a transdiagnostic construct. J Affect Disord 2013;151:313‐20. [DOI] [PubMed] [Google Scholar]
- 133. McEvoy PM, Mahoney AEJ. Intolerance of uncertainty and negative metacognitive beliefs as transdiagnostic mediators of repetitive negative thinking in a clinical sample with anxiety disorders. J Anxiety Disord 2013;27:216‐24. [DOI] [PubMed] [Google Scholar]
- 134. Zimmerman M, Morgan T, Stanton K. The severity of psychiatric disorders. World Psychiatry 2018;17:258‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Tyrer P. Dimensions fit the data, but can clinicians fit the dimensions? World Psychiatry 2018;17:295‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Fulford K, Handa A. Categorical and/or continuous? Learning from vascular surgery. World Psychiatry 2018;13:304‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Strickland CM, Hopwood CJ, Bornovalova MA et al. Categorical and dimensional conceptions of personality pathology in DSM‐5: toward a model‐based synthesis. J Pers Disord (in press). [DOI] [PubMed] [Google Scholar]
- 138. Jauhar S, Krishnadas R, Nour MM et al. Is there a symptomatic distinction between the affective psychoses and schizophrenia? A machine learning approach. Schizophr Res 2018;202:241‐7. [DOI] [PubMed] [Google Scholar]
- 139. American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Washington: American Psychiatric Association, 1994. [Google Scholar]
- 140. Parnas J. Differential diagnosis and current polythetic classification. World Psychiatry 2015;14:284‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Jablensky A. The dialectic of quantity and quality in psychopathology. World Psychiatry 2018;17:300‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Parnas J, Henriksen MG. Epistemological error and the illusion of phenomenological continuity. World Psychiatry 2016;15:126‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Zachar P. Quantitative classification as (re‐)descriptive psychopathology. World Psychiatry 2018;17:294‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Fusar‐Poli P, Raballo A, Parnas J. What is an attenuated psychotic symptom? On the importance of the context. Schizophr Bull 2017;43:687‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Parnas J. The RDoC program: psychiatry without psyche? World Psychiatry 2014;13:46‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Ghaemi SN. Feeling and time: the phenomenology of mood disorders, depressive realism, and existential psychotherapy. Schizophr Bull 2007;33:122‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Parnas J. Delusions, epistemology and phenophobia. World Psychiatry 2015;14:174‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Pearl SB, Norton PJ. Transdiagnostic versus diagnosis specific cognitive behavioural therapies for anxiety: a meta‐analysis. J Anxiety Disord 2017;46:11‐24. [DOI] [PubMed] [Google Scholar]
- 149. Roy‐Byrne P. Transdiagnostic cognitive behavioral therapy and the return of the repressed. JAMA Psychiatry 2017;74:867‐8. [DOI] [PubMed] [Google Scholar]
- 150. Reed GM. HiTOP must meet the use requirements of the ICD before it can aspire to replace it. World Psychiatry 2018;17:297‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Wittchen H, Beesdo‐Baum K. “Throwing out the baby with the bathwater”? Conceptual and methodological limitations of the HiTOP approach. World Psychiatry 2018;17:298‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]


