Abstract
Background
Pediatric patients with brain tumors who are treated with radiation therapy (RT) are at risk for neurocognitive and psychosocial late effects. Research to date has primarily examined these outcomes at a group level and in isolation. Advanced statistical techniques allow for person-centered analyses, as well as examination of relationships between domain-specific trajectories.
Methods
Patients with brain tumors (craniopharyngioma, ependymoma, low-grade astrocytoma, high-grade astrocytoma) were enrolled on a phase II clinical trial of RT. Three hundred and fifty patients completed serial neurocognitive assessments as part of their treatment monitoring, including pre-RT baseline, 6 months post-RT, and then yearly for 5 years. This secondary analysis focused on outcomes of cognition (estimated IQ, parent-reported attention problems) and psychosocial effects (parent-reported socialization and social problems) post-RT.
Results
Latent growth curve modeling indicated that estimated IQ and socialization were best served by quadratic models, while attention and social problems were best served by linear models. Growth mixture modeling indicated 3-class models were the best fit for IQ and socialization, and 2-class models for attention and social problems. Baseline IQ and socialization scores were associated, but there was no association over time. Young age at diagnosis and pre-RT treatments (surgery, chemotherapy) were associated with class membership.
Conclusions
Person-centered statistical analyses provide rich information regarding the variability in neurocognitive and psychosocial functioning following RT for pediatric brain tumor. While many patients do well over time, a subset are exhibiting significant cognitive and/or psychosocial deficits. Class membership was associated with some medical factors (eg, pre-radiation surgery/chemotherapy, age at diagnosis, shunted hydrocephalus).
Keywords: cognitive functioning, growth mixture modeling, pediatric brain tumors, psychosocial functioning, radiation therapy
Key Points.
Pediatric patients with brain tumors are at risk for cognitive and psychosocial late effects.
Person-centered analytical techniques support understanding of the variability in functioning.
While many patients do well, a subset are exhibiting weaknesses.
Importance of the Study.
This paper uses person-centered statistical techniques to describe latent trajectories of cognitive and psychosocial functioning following RT for pediatric patients with brain tumors. Results demonstrate that the majority of patients are doing well over time after treatment, but a sizable proportion demonstrate deficits, with patients receiving pre-radiation surgery/chemotherapy and those younger at diagnosis more likely to exhibit weaknesses in cognitive and psychosocial functioning. Findings from this study highlight the variability in functioning post-RT for pediatric patients with brain tumors and support the use of person-centered analytical techniques to increase understanding of functioning over time.
Radiation therapy (RT) is a mainstay of treatment for pediatric brain tumors.1 Unfortunately, the cost of this treatment, particularly for the developing brain, is the development of psychological and medical late effects.2 More specifically, RT is often associated with declines in intellectual functioning and other aspects of neurocognitive functioning over time, as well as deficits in broader psychosocial functioning.3 Significant research has focused on characterizing the trajectories of cognitive and psychosocial functioning in youth with brain tumors treated with RT, as well as other therapies (eg, chemotherapy).4–10 However, to date, research has primarily examined these two broad domains in isolation. From a cross-sectional perspective, there is a growing body of literature suggesting a relationship between cognitive and psychosocial functioning, with weaknesses in cognitive functioning frequently tied to greater deficits in psychosocial outcomes.11–14 What is unknown is how these two domains of functioning may interact over time.
Recently, advances in statistical methods have provided new approaches for examining trajectories of functioning over time. While most research to date has focused on group-based trajectories posttherapy, new statistical methodologies allow for person-centered variability to be analyzed. More specifically, such techniques sort individual patients into groups or classes that follow similar trajectories, thus allowing for a greater understanding of how individual patients may be both similar and different in their developmental course over time.15 With evidence of significant variability in functioning posttreatment for youth with brain tumors, such techniques provide the means for taking a more targeted approach to understanding late effect development. The benefit of such information may be the improved prediction of outcomes, as well as a greater understanding of variability which may aid in more targeted intervention.
The objectives of the current paper were two-fold. First, we sought to take a person-centered approach to analyzing longitudinal trajectories of cognitive and psychosocial functioning of youth with brain tumors following treatment with RT. It was hypothesized that each domain would include 3 classes of change: stability, decline, and improvement. Second, we sought to examine the trajectories of cognitive and psychosocial functioning in tandem to determine potential influences of each domain on the other. It was hypothesized that early variability in cognitive functioning would be associated with later declines in psychosocial functioning.
Methods
Patients and Procedures
Pediatric patients with brain tumors (craniopharyngioma, ependymoma, low-grade astrocytoma, high-grade astrocytoma) were enrolled on a phase II clinical trial to assess the efficacy of conformal/intensity-modulated photon therapy.16–19 The parent study was approved by the institutional review board, and consent/assent was obtained prior to treatment. As part of their enrollment, patients were scheduled for serial neuropsychological assessments at 7 timepoints both before and after treatment: pre-RT baseline, 6 months post-RT, and then annually through 5 years post-RT. A number of prior publications have described the primary intellectual, academic, adaptive, and emotional/behavioral outcomes from this trial for individual diagnoses.7–10,20–26 The current study represents a secondary analysis, with all diagnoses grouped together, and different statistical approaches taken to enhance understanding of the course of functioning.
Measures
Intellectual functioning
Cognitive functioning was assessed at each timepoint, though abbreviated indices were often used rather than the full battery to reduce participant burden and practice effects. The measure administered was age dependent and included the Bayley Scales of Infant Development27 and the age-appropriate version of the Wechsler Preschool and Primary Scale of Intelligence (WPPSI),28 Child,29 and Adult.30 Estimated IQ was the primary variable of interest and was available at each timepoint. Calculated using a formula developed by Sattler,31 the estimated IQ score is highly correlated (r = 0.93) with full-scale IQ. It is expressed as a standard score (M = 100, SD = 50).
Psychosocial functioning
Psychosocial functioning was assessed at each timepoint by 2 well-validated and commonly used parent-completed measures. The Vineland Adaptive Behavior Scales32 is a parent-reported semi-structured interview appropriate for individuals birth through adulthood. As such, it spanned our entire age range. The socialization subscale was of primary interest and is expressed as a standard score (M = 100, SD = 15). The Child Behavior Checklist (CBCL)33 is a parent-reported questionnaire for children 4–18 years of age. Two subscales were of primary interest: social problems and attention problems, with each expressed as a T-score (M = 50, SD = 10) and higher scores indicative of more problems.
Statistical Approaches
Analyses were completed using Mplus.34 For the first objective, latent growth curve modeling15 was used to identify the optimal rate of change for each of our 4 outcome variables: intercept only, linear, quadratic, cubic, etc. Model fit was evaluated using Comparative Fit Index (CFI), scaled Χ2 statistic, Tucker Lewis Index (TLI), and the root mean square error of approximation (RMSEA) statistic,15 with the same evaluation procedure used for all 4 outcome variables. Models with a Χ2 to degrees of freedom ratio ≤2,35 CFI/TLI > 0.95,36,37 and RMSEA < 0.0538 were considered to be a good fit. Missing data were handled using full-information maximum likelihood (FIML).39
Growth mixture modeling15,40 was then used to determine the number of latent classes that best fit the data. The number of classes was determined by best fit using Bayesian information criteria,41 the Lo-Mendell-Rubin test,42 and the Bootstrap Likelihood Ratio Test (BLRT)43 (in conjunction with FIML estimations, because BLRT is not available with imputations).
For the second objective, parallel process models44,45 were used to assess how cognitive and psychosocial functioning variables change over time. For ease of interpretation, estimated IQ and socialization were paired, as were attention and social problems.
As an exploratory step, following growth mixture modeling, analyses were completed in SPSS (v22) to assess predictors of most likely class membership. Known risk factors for neurocognitive/psychosocial difficulties were examined: age at diagnosis, diagnosis, pre-RT chemotherapy, number of prior resections, and shunted hydrocephalus. Continuous variables were assessed with ANOVA, while categorical variables were assessed with χ-square.
Results
Participants
Of 361 patients enrolled on the parent treatment protocol, 350 (96.9%) completed at least one assessment and were included in analyses (M = 5.12 assessments, SD = 1.88, median = 6, range 1–7; 95.4% ≥2 assessments) (Supplementary Fig. 1). On average, participants were 7.88 years old at the start of RT (SD = 5.26, 1–24.33 y) and 6.89 years old at diagnosis (SD = 5.31, 0–24.17 y). Diagnoses were varied, with 147 (42%) diagnosed with ependymoma and 94 (26.9%) with a low-grade astrocytoma. About half (49.4%) were female and the majority (80.9%) were Caucasian. Table 1 has additional demographic and treatment information.
Table 1.
Demographic and treatment information (n = 350)
| N (%) | M ± SD, range | |
| Sex | ||
| Male | 177 (50.6) | |
| Female | 173 (49.4) | |
| Race | ||
| White | 283 (80.9) | |
| Black | 53 (15.1) | |
| Other | 14 (4.0) | |
| Diagnosis | ||
| Ependymoma | 147 (42.0) | |
| Low-grade astrocytoma | 94 (26.9) | |
| Craniopharyngioma | 74 (21.1) | |
| High-grade astrocytoma | 33 (9.4) | |
| Other | 2 (0.6) | |
| Age at diagnosis | 6.89 ± 5.31, 0.00–24.17 | |
| Age at radiation therapy | 7.88 ± 5.26, 1.00–24.33 | |
| Prior treatments | ||
| Surgery | 326 (93.1) | |
| Number of surgeries | 1.37 ± 0.89, 0–5 | |
| Chemotherapy | 95 (24.0) | |
| Shunt | 127 (36.3) |
Latent Growth Curve Modeling
Intercept only, linear, quadratic, and cubic models were estimated to examine the shape and growth of psychosocial and cognitive functioning from pre-RT baseline to 5 years post-RT (Table 2).
Table 2.
Model fit statistics for latent growth curve models of 4 primary variables of interest (shaded area indicates selected model)
| Model | BIC | Χ 2 | Χ 2 / df | CFI | TLI | RMSEA |
| Socialization | ||||||
| Intercept only | 11 775.88 | 133.87 | 5.15 | 0.797 | 0.836 | 0.112 |
| Linear | 11 710.18 | 53.17 | 2.31 | 0.943 | 0.948 | 0.063 |
| Quadratic | 11 708.12 | 29.32 | 1.54 | 0.981 | 0.978 | 0.041 |
| Cubic | 11 729.14 | 22.99 | 1.64 | 0.983 | 0.975 | 0.044 |
| Social Problems | ||||||
| Intercept only | 8398.88 | 78.37 | 3.01 | 0.864 | 0.890 | 0.082 |
| Linear | 8365.42 | 40.08 | 1.74 | 0.956 | 0.960 | 0.050 |
| Quadratic | 8368.61 | 25.04 | 1.32 | 0.984 | 0.983 | 0.032 |
| Estimated IQ | ||||||
| Intercept only | 11 549.71 | 234.39 | 12.33 | 0.829 | 0.865 | 0.180 |
| Linear | 11 458.83 | 138.48 | 8.65 | 0.903 | 0.909 | 0.148 |
| Quadratic | 11 392.50 | 45.36 | 3.78 | 0.973 | 0.967 | 0.089 |
| Attention Problems | ||||||
| Intercept only | 8552.29 | 71.68 | 2.76 | 0.882 | 0.904 | 0.076 |
| Linear | 8517.17 | 38.99 | 1.69 | 0.959 | 0.962 | 0.048 |
| Quadratic | 8514.20 | 22.41 | 1.18 | 0.991 | 0.990 | 0.024 |
| Cubic | 8535.06 | 17.00 | 1.21 | 0.992 | 0.988 | 0.027 |
BIC: Bayesian information criteria; CFI: Comparative Fit Index; df: degrees of freedom; RMSEA: root mean square error of approximation; TLI: Tucker Lewis Index.
Note. Cubic models would not converge for socialization, social problems, and estimated IQ.
Psychosocial functioning
For socialization, the quadratic model provided the best fit (Χ2 = 551.47, P < 0.001; CFI = 0.981; TLI = 0.978; RMSEA = 0.041). Participants started with average-range skills at baseline (intercept = 97.14, P < 0.001), which increased slightly but not significantly (slope = 1.20, P = 0.11), but the rate of change decelerated significantly (quadratic = −0.372, P = 0.008).
The quadratic model also provided the best fit for social problems (Table 2). However, the quadratic variance was not significantly different from zero, thus the linear model was selected in favor of parsimony (Χ2 = 40.08, P = 0.01; CFI = 0.956; TLI = 0.96; RMSEA = 0.05). Overall, participants started with average levels of social problems (intercept = 55.20, P < 0.001) that increased over time, though non-significantly (slope = 0.138, P = 0.21).
Cognitive functioning
Examination of the IQ plots indicated an odd pattern surrounding the 2-year post-RT timepoint, such that all modeling attempts resulted in non-interpretable models due to out of range values. Further examination of the data suggested that, based on child age, this was a timepoint when a number of the youngest patients switched from the Bayley to the WPPSI (eg, 42 Bayleys administered at 1 y vs 7 at 2 y), resulting in a significant change in how IQ was assessed. To increase model fit, the decision was made to remove this timepoint from analyses. Ultimately, the quadratic model was the best fit (Χ2 = 45.36, P < 0.001; CFI = 0.973; TLI = 0.967; RMSEA = 0.089). Specifically, IQ was in the average range at baseline (intercept = 94.68, P < 0.001), increased over time (slope = 2.73, P < 0.001), but decelerated over time (quadratic = −0.70, P < 0.001).
For attention problems, the linear model provided the best fit (Χ2 = 38.99, P = 0.02; CFI = 0.959; TLI = 0.962; RMSEA = 0.048). Participants demonstrated average-range parent-reported attention issues at baseline (intercept = 54.57, P < 0.001) that increased significantly over time (slope = 0.32, P = 0.004).
Growth Mixture Modeling
Given known variability in cognitive and psychosocial functioning over time, analyses were completed to allow participants to align with individual classes, rather than adjusting to the overall mean. For all models, 1- to 5-class models were attempted. Model fit information for each of the 4 outcome measures is presented in Table 3.
Table 3.
Model fit statistics for growth mixture models for the 4 primary variables of interest (shaded area indicates final number of classes)
| Classes | Entropy | AIC | BIC | VLMR LRT† | LMR† | BLRT† |
| Socialization | ||||||
| 1 | 12 285.611 | 12 323.541 | ||||
| 2 | 0.816 | 11 810.107 | 11 863.209 | 0.0001 | 0.0001 | <0.001 |
| 3 | 0.820 | 11 664.516 | 11 732.791 | <0.001 | <0.001 | <0.001 |
| 4 | 0.793 | 11 639.463 | 11 722.909 | 0.1074 | 0.1157 | <0.001 |
| Social Problems | ||||||
| 1 | 8884.418 | 8917.812 | ||||
| 2 | 0.902 | 8345.512 | 8390.037 | 0.0004 | 0.0006 | <0.001 |
| 3 | 0.845 | 8247.155 | 8302.811 | 0.1437 | 0.1572 | <0.001 |
| 4 | 0.849 | 8171.355 | 8238.143 | 0.1292 | 0.1391 | <0.001 |
| Estimated IQ | ||||||
| 1 | 12 863.345 | 12 898.015 | ||||
| 2 | 0.835 | 12 123.338 | 12 173.417 | 0.0008 | 0.001 | <0.001 |
| 3 | 0.872 | 11 770.473 | 11 835.960 | 0.0013 | 0.0017 | <0.001 |
| 4 | 0.851 | 11 607.923 | 11 688.820 | 0.0511 | 0.0558 | <0.001 |
| 5 | 0.831 | 11 528.662 | 11 624.967 | 0.0451 | 0.0496 | <0.001 |
| Attention Problems | ||||||
| 1 | 9057.908 | 9091.332 | ||||
| 2 | 0.890 | 8540.876 | 8585.441 | 0.0457 | 0.0523 | <0.001 |
| 3 | 0.901 | 8380.756 | 8436.462 | 0.1088 | 0.117 | <0.001 |
| 4 | 0.866 | 8307.395 | 8374.242 | 0.0991 | 0.1084 | <0.001 |
| 5 | 0.884 | 8237.988 | 8315.977 | 0.1043 | 0.1148 | <0.001 |
AIC: Akaike information criteria; BIC: Bayesian information criteria; VLMR LRT: Vuong-Lo-Mendell-Rubin Likelihood Ratio Test; LMR: Lo-Mendell-Rubin adjusted LRT test; BLRT: Bootstrap Likelihood Ratio Test.
†P-value indicating significance of test comparing n classes versus n − 1 classes.
Psychosocial functioning
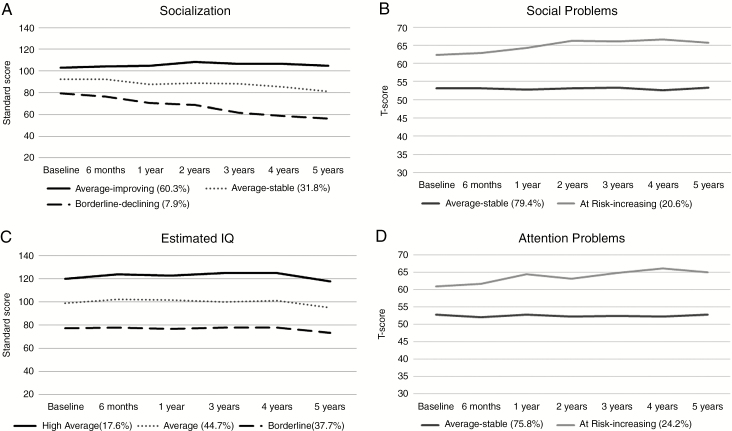
For socialization, a 3-class model provided the best fit to the data (Fig. 1A): average-improving, average-stable, and borderline-declining. Specifically, the average-improving group consisted of 60.3% of the sample, with average-range scores at baseline (intercept = 102.78, P < 0.001) that significantly increased over time (slope = 3.12, P = 0.001), but decelerated (quadratic = −0.55, P < 0.001). The average-stable group (31.8%) demonstrated scores at the lower end of average at baseline (intercept = 91.56, P < 0.001), but both the change (slope = −0.77, P = 0.62) and rate of change (quadratic = −0.22, P = 0.47) were non-significant. Finally, the borderline-declining group (7.9%) demonstrated baseline scores in the borderline range (intercept = 79.05, P < 0.001) that decreased significantly over time (slope = −7.25, P = 0.01), but with no change in acceleration (quadratic = 0.55, P = 0.36).
Fig. 1.
Visual depiction of growth mixture models for each outcome: (A) socialization; (B) social problems; (C) estimated IQ; and (D) attention problems. For socialization and estimated IQ, higher scores are indicative of better functioning. For social and attention problems, higher scores are indicative of more problems.
For social problems, a 2-class model provided the best fit to the data (Fig. 1B). Specifically, the majority of participants fell within an average-stable class. However, about 20% of participants demonstrated social problems in the at-risk range at baseline (intercept = 63.40, P < 0.001) that increased over time, albeit not significantly (slope = 0.73, P = 0.09).
Cognitive functioning
A 3-class model provided the best fit for IQ (Fig. 1C): high average, average, and borderline. For the high average group (17.6%), baseline IQ scores were in the high average range (intercept = 120.18, P < 0.001) and increased over time (slope = 5.15, P = 0.001), though the rate of change decelerated over time (quadratic = −1.08, P < 0.01). The average group (44.7%) demonstrated solidly average IQs at baseline (intercept = 99.93, P < 0.001), which increased over time (slope = 2.61, P = 0.006) but decelerated over time (quadratic = −0.69, P < 0.001). Finally, the borderline group (37.7%) demonstrated borderline-range IQs at baseline (intercept = 76.94, P < 0.001), which increased slightly (slope = 1.83, P = 0.07) but decelerated (quadratic = −0.48, P = 0.009).
A 2-class model provided the best fit for parent-reported attention problems (Fig. 1D): average-stable and at-risk increasing. The average-stable group (75.8%) demonstrated baseline scores within normal limits (intercept = 52.44, P < 0.001), with no change over time (slope = 0.00). In contrast, the at-risk increasing group (24.2%) demonstrated baseline scores in the at-risk range (intercept = 62.02, P < 0.001) that increased significantly over time (slope = 0.83, P = 0.02).
Parallel Process Models
To assess potential relationships between social and cognitive functioning, parallel process models were conducted with socialization and IQ and social problems and attention problems. Outcome variables were paired due to similarities in measurement (standard scores, T-scores), as well as similar latent growth curves (quadratic, linear).
Results of the first model—socialization and IQ—indicated that the intercepts were strongly positively associated (estimate = 133.59, SE = 19.29, P < 0.001), suggesting that higher IQ scores at baseline were associated with stronger social functioning. However, there was no association between slopes (estimate = 11.54, SE = 8.56, P = 0.18) or quadratic terms (estimate = 0.22, SE = 0.26, P = 0.39). The second model—social problems and attention problems—resulted in out of range values and non-convergence of models. This non-convergence may be in part a reflection of the non-significant linear change in the overall social problems model.
Exploratory Analyses: Medical and Demographic Predictors of Latent Classes
Exploratory analyses were completed to assess predictors of latent classes. For simplicity, each measure was assessed separately and analyses were completed with individuals placed in their most likely class. Diagnostic category (low-grade astrocytoma, ependymoma, craniopharyngioma) was unrelated to class membership. There was a trend for an association with attention problems, with patients with ependymoma marginally less likely to be in the at-risk increasing class compared with the other diagnoses (Χ2 = 5.55, P = 0.06). Age at diagnosis was a significant predictor of class membership for IQ, with younger patients more likely to be in the borderline group (F(2,345) = 10.58, P < 0.001). It was unrelated to class membership for the other measures.
Patients who received a higher mean number of surgeries prior to RT were more likely to be in the borderline class for IQ, F(2,345) = 6.12, P = 0.002, while those with fewer surgeries were more likely to be in the average-improving class for socialization, F(2,325) = 7.02, P = 0.001. There were no differences based on attention or social problems. Patients who received pre-RT chemotherapy were more likely to be in the borderline class for IQ (Χ2 = 8.14, P < 0.02), while those in the average-improving class for socialization were less likely to have received pre-RT chemotherapy (Χ2 = 6.82, P < 0.04). There were no differences for attention or social problems. Shunted hydrocephalus was unrelated to class membership for attention or social Problems. Patients without a shunt were more likely to be in the average or high average class for IQ (Χ2 = 25.64, P < 0.001) and the average-improving class for socialization (Χ2 = 20.63, P < 0.001).
Discussion
The current paper reflects a secondary analysis and extension of longitudinal trajectories of social and cognitive functioning in a large sample of pediatric patients with brain tumors treated with RT. Findings provide additional information regarding the variability of functioning post-RT for pediatric patients and indicate a subsample—about 8% to 37%—that exhibit significant difficulties. Fortunately, the majority of patients treated on this trial appear to be doing well from neurocognitive and psychosocial perspectives, with many participants demonstrating stable to improved functioning over time.
That the best growth model for 2 outcomes was quadratic in nature is interesting and worth discussion. Specifically, this suggests that there is a change in the acceleration or deceleration of slopes over the course of the study. This may indicate a need to expand serial assessments of neurocognitive and psychosocial functioning beyond the 5 years often used in studies like this. That is, while patients appear to be largely stable over the course of the 5 years, the quadratic finding may indicate that there is additional change in functioning happening at later timepoints that may continue after 5 years post-RT. Such findings point to the need for continual serial neurocognitive assessments for pediatric patients with brain tumors treated with RT.
Known risk factors for neurocognitive and psychosocial deficits were somewhat unrelated to class membership. The most notable associations were younger age at diagnosis being associated with a greater likelihood of being in the borderline IQ class, and pre-RT treatments (surgeries, chemotherapy) and shunted hydrocephalus associated with class membership for IQ and socialization. Diagnosis was not related to class membership. Such findings may indicate that there are other factors, both psychosocial (eg, socioeconomic status, family functioning, access to intervention) and medical (eg, hearing loss, seizures, endocrine dysfunction), that need to be explored to assist with the prediction of functioning post-RT in childhood.
Unfortunately, hypotheses regarding the potential for interactive change in social and cognitive functioning were not supported. More specifically, while baseline functioning for 2 measures (IQ and socialization) were associated, consistent with cross-sectional research,11–14 there was no relationship between the 2 over time. Further, analyses with the other 2 measures could not be completed. There are several possible reasons for the lack of demonstrated association between social and cognitive functioning in this study. First, the primary factor that appeared to be driving performance in this study was baseline functioning. Indeed, a significant proportion of patients had received prior treatment, whether that be chemotherapy or multiple surgeries. Both of these factors were associated with class membership for some outcomes. As such, there is a strong likelihood that significant neurocognitive and/or psychosocial change occurred prior to the start of RT. Second, the measures used in this study represent a limitation. More specifically, it is now well established that the most vulnerable indices post-RT are working memory, processing speed, attention, and executive functions, and not IQ. Indeed, there is some suggestion that estimated IQ scores may not accurately reflect neurocognitive weaknesses in patients with brain tumors who have undergone radiation.46 Further, prior studies that have found associations between cognitive and social functioning have assessed one of these indices.11,12,47 This study was launched prior to this establishment, and thus, these indices were not routinely assessed in all patients (eg, only available for those school-aged and older). As such, it is possible that the neurocognitive sequelae assessed in this paper via estimated IQ do not fully capture the range of weaknesses potentially present in this sample. Relatedly, social functioning is notoriously difficult to assess, and while the Vineland and the CBCL are widely used and well-validated measures that have been used in many prior studies,48–50 parent-reported measures are viewed as particularly weak.51 The CBCL in particular has limitations in measurement such that there is limited variability in available scores (eg, the lowest/best possible score is 50, thereby truncating examination of variability in stronger functioning). As such, future studies may wish to include self- or teacher-report indicators of social functioning, and/or consider the use of objective measures of social skills. Ultimately, future studies would benefit from re-approaching the question of a longitudinal interaction between cognitive and psychosocial functioning in patients with pediatric brain tumors, but with improvements in assessment strategies.
In summary, findings from this secondary analysis provide support for the use of person-centered analytical approaches in pediatric patients with brain tumors. These approaches provide interesting and valuable information about the variability in functioning posttreatment and may yield additional necessary evidence regarding risk and protective factors for reduced and stable functioning, respectively. Future studies would benefit from the use of improved measures for assessing neurocognitive and psychosocial outcomes, and may consider the benefit of limiting analyses to single diagnoses so as to assess medical outcomes specific to individual diagnoses.
Funding
This work was supported in part by Cancer Center Support Grant No. CA21765 from the National Cancer Institute, a Mentored Research Scholar Grant in Applied and Clinical Research (MRSG-16-054-01-PCSM, PI: Willard) from the American Cancer Society and ALSAC.
Conflict of interest statement.
No conflicts.
Authorship statement.
Collected data: HMC, TEM; analyzed data: VWW, KSB; interpreted the data: all authors. All authors wrote the manuscript.
Supplementary Material
References
- 1. Merchant TE, Hodgson D, Laack NN, Wolden S, Indelicato DJ, Kalapurakal JA; COG Radiation Oncology Discipline Committee Children’s Oncology Group’s 2013 blueprint for research: radiation oncology. Pediatr Blood Cancer. 2013;60(6):1037–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Merchant TE, Pollack IF, Loeffler JS. Brain tumors across the age spectrum: biology, therapy, and late effects. Semin Radiat Oncol. 2010;20(1):58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mulhern RK, Merchant TE, Gajjar A, Reddick WE, Kun LE. Late neurocognitive sequelae in survivors of brain tumours in childhood. Lancet Oncol. 2004;5(7):399–408. [DOI] [PubMed] [Google Scholar]
- 4. Spiegler BJ, Bouffet E, Greenberg ML, Rutka JT, Mabbott DJ. Change in neurocognitive functioning after treatment with cranial radiation in childhood. J Clin Oncol. 2004;22(4):706–713. [DOI] [PubMed] [Google Scholar]
- 5. Merchant TE, Kiehna EN, Li C, et al. Modeling radiation dosimetry to predict cognitive outcomes in pediatric patients with CNS embryonal tumors including medulloblastoma. Int J Radiat Oncol Biol Phys. 2006;65(1):210–221. [DOI] [PubMed] [Google Scholar]
- 6. Brinkman TM, Palmer SL, Chen S, et al. Parent-reported social outcomes after treatment for pediatric embryonal tumors: a prospective longitudinal study. J Clin Oncol. 2012;30(33):4134–4140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Merchant TE, Conklin HM, Wu S, Lustig RH, Xiong X. Late effects of conformal radiation therapy for pediatric patients with low-grade glioma: prospective evaluation of cognitive, endocrine, and hearing deficits. J Clin Oncol. 2009;27(22):3691–3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Merchant TE, Kiehna EN, Kun LE, et al. Phase II trial of conformal radiation therapy for pediatric patients with craniopharyngioma and correlation of surgical factors and radiation dosimetry with change in cognitive function. J Neurosurg. 2006;104(Suppl 2):94–102. [DOI] [PubMed] [Google Scholar]
- 9. Willard VW, Conklin HM, Boop FA, Wu S, Merchant TE. Emotional and behavioral functioning after conformal radiation therapy for pediatric ependymoma. Int J Radiat Oncol Biol Phys. 2014;88(4):814–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Willard VW, Conklin HM, Wu S, Merchant TE. Prospective longitudinal evaluation of emotional and behavioral functioning in pediatric patients with low-grade glioma treated with conformal radiation therapy. J Neurooncol. 2015;122(1):161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Moyer KH, Willard VW, Gross AM, et al. The impact of attention on social functioning in survivors of pediatric acute lymphoblastic leukemia and brain tumors. Pediatr Blood Cancer. 2012;59(7):1290–1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Willard VW, Allen TM, Hardy KK, Bonner MJ. Social functioning in survivors of pediatric brain tumors: the contribution of neurocognitive and social-cognitive skills. Child Health Care. 2017;46(2):181–195. [Google Scholar]
- 13. Wolfe KR, Walsh KS, Reynolds NC, et al. Executive functions and social skills in survivors of pediatric brain tumor. Child Neuropsychol. 2013;19(4):370–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Conklin HM, Reddick WE, Ashford J, et al. Long-term efficacy of methylphenidate in enhancing attention regulation, social skills, and academic abilities of childhood cancer survivors. J Clin Oncol. 2010;28(29):4465–4472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Berlin KS, Parra GR, Williams NA. An introduction to latent variable mixture modeling (part 2): longitudinal latent class growth analysis and growth mixture models. J Pediatr Psychol. 2014;39(2):188–203. [DOI] [PubMed] [Google Scholar]
- 16. Merchant TE, Kun LE, Wu S, Xiong X, Sanford RA, Boop FA. Phase II trial of conformal radiation therapy for pediatric low-grade glioma. J Clin Oncol. 2009;27(22):3598–3604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Merchant TE, Li C, Xiong X, Kun LE, Boop FA, Sanford RA. Conformal radiotherapy after surgery for paediatric ependymoma: a prospective study. Lancet Oncol. 2009;10(3):258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Merchant TE, Zhu Y, Thompson SJ, Sontag MR, Heideman RL, Kun LE. Preliminary results from a phase II trail of conformal radiation therapy for pediatric patients with localised low-grade astrocytoma and ependymoma. Int J Radiat Oncol Biol Phys. 2002;52(2):325–332. [DOI] [PubMed] [Google Scholar]
- 19. Vern-Gross TZ, Schreiber JE, Broniscer A, Wu S, Xiong X, Merchant TE. Prospective evaluation of local control and late effects of conformal radiation therapy in children, adolescents, and young adults with high-grade glioma. Neuro Oncol. 2014;16(12):1652–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Conklin HM, Li C, Xiong X, Ogg RJ, Merchant TE. Predicting change in academic abilities after conformal radiation therapy for localized ependymoma. J Clin Oncol. 2008;26:3695–3970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Netson KL, Conklin HM, Wu S, Xiong X, Merchant TE. A 5-year investigation of children’s adaptive functioning following conformal radiation therapy for localized ependymoma. Int J Radiat Oncol Biol Phys. 2012;84(1):217–223.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Netson KL, Conklin HM, Wu S, Xiong X, Merchant TE. Longitudinal investigation of adaptive functioning following conformal irradiation for pediatric craniopharyngioma and low-grade glioma. Int J Radiat Oncol Biol Phys. 2013;85(5):1301–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Di Pinto M, Conklin HM, Li C, Merchant TE. Learning and memory following conformal radiation therapy for pediatric craniopharyngioma and low-grade glioma. Int J Radiat Oncol Biol Phys. 2012;84(3):e363–e369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Di Pinto M, Conklin HM, Li C, Xiong X, Merchant TE. Investigating verbal and visual auditory learning after conformal radiation therapy for childhood ependymoma. Int J Radiat Oncol Biol Phys. 2010;77(4):1002–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Dolson EP, Conklin HM, Li C, Xiong X, Merchant TE. Predicting behavioral problems in craniopharyngioma survivors after conformal radiation therapy. Pediatr Blood Cancer. 2009;52(7):860–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Merchant TE, Kun LE, Hua CH, et al. Disease control after reduced volume conformal and intensity modulated radiation therapy for childhood craniopharyngioma. Int J Radiat Oncol Biol Phys. 2013;85(4):e187–e192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bayley N. Bayley Scales of Infant Development. 2nd ed. San Antonio, TX: The Psychological Corporation; 1993. [Google Scholar]
- 28. Wechsler D. Wechsler Preschool and Primary Scale of Intelligence, Revised. San Antonio, TX: The Psychological Corporation; 1989. [Google Scholar]
- 29. Wechsler D. Wechsler Intelligence Scale for Children. 3rd ed. San Antonio, TX: The Psychological Corporation; 1991. [Google Scholar]
- 30. Wechsler D. Wechsler Adult Intelligence Scale. 3rd ed. San Antonio, TX: The Psychological Corporation; 1997. [Google Scholar]
- 31. Sattler JM. Assessment of Children. 3rd ed. San Diego, CA: Jerome M. Sattler, Publisher Inc.; 1992. [Google Scholar]
- 32. Sparrow SS, Balla D, Cicchetti D.. Vineland Adpative Behavior Scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- 33. Achenbach TM. Manual for the CBCL. Burlington, VT: University of Vermont; 1991. [Google Scholar]
- 34. Muthén L, Muthén B.. Mplus User’s Guide. 7th ed. Los Angeles, CA: Muthén & Muthén; 1998–2015. [Google Scholar]
- 35. Ullman JB. Structural equation modeling. In: Tabachnick BG, Fidell LS, eds. Understanding Multivariate Statistics. 4th ed. Needham Heights, MA: Allyn & Bacon; 2001:653–771. [Google Scholar]
- 36. Bollen KA. Structural Equations with Latent Variables. Oxford, England: John Wiley & Sons; 1989. [Google Scholar]
- 37. Hoyle RH, Panter AT. Writing about structural equation modeling. In: Hoyle RH, ed. Structural Equation Modeling: Concepts, Issues, and Applications. Thousand Oaks, CA: Sage; 1995:158–176. [Google Scholar]
- 38. MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance stucture modeling. Psychol Methods. 1996;1:130–149. [Google Scholar]
- 39. Little TD, Jorgensen TD, Lang KM, Moore EW. On the joys of missing data. J Pediatr Psychol. 2014;39(2):151–162. [DOI] [PubMed] [Google Scholar]
- 40. Berlin KS, Williams NA, Parra GR. An introduction to latent variable mixture modeling (part 1): overview and cross-sectional latent class and latent profile analyses. J Pediatr Psychol. 2014;39(2):174–187. [DOI] [PubMed] [Google Scholar]
- 41. Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–464. [Google Scholar]
- 42. Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- 43. McLachlan G, Peel D.. Finite Mixture Models. New York: Wiley; 2000. [Google Scholar]
- 44. Duncan T, Duncan S, Strycker L.. An Introduction to Latent Variable Growth Curve Modeling. New York, NY: Routledge; 2006. [Google Scholar]
- 45. Muthén LK, Muthén BO.. Mplus User’s Guide. 8th ed. Los Angeles, CA: Muthén & Muthén; 1998–2017. [Google Scholar]
- 46. Burgess L, Pulsifer MB, Grieco JA, et al. Estimated IQ systematically underestimates neurocognitive sequelae in irradiated pediatric brain tumor survivors. Int J Radiat Oncol Biol Phys. 2018;101(3):541–549. [DOI] [PubMed] [Google Scholar]
- 47. Patel SK, Lai-Yates JJ, Anderson JW, Katz ER. Attention dysfunction and parent reporting in children with brain tumors. Pediatr Blood Cancer. 2007;49(7):970–974. [DOI] [PubMed] [Google Scholar]
- 48. Bonner MJ, Hardy KK, Willard VW, Anthony KK, Hood M, Gururangan S. Social functioning and facial expression recognition in survivors of pediatric brain tumors. J Pediatr Psychol. 2008;33:1153–1162. [DOI] [PubMed] [Google Scholar]
- 49. Willard VW, Qaddoumi I, Chen S, et al. Developmental and adaptive functioning in children with retinoblastoma: a longitudinal investigation. J Clin Oncol. 2014;32(25):2788–2793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Schulte F, Barrera M. Social competence in pediatric brain tumor survivors: evaluating the psychometric properties of assessment tools. Support Care Cancer. 2014;22(2):561–569. [DOI] [PubMed] [Google Scholar]
- 51. Noll RB, Bukowski WB. Commentary: social competence in children with chronic illness: the devil is in the details. J Pediatr Psychol. 2012;37(9):959–966; discussion 867. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.