ABSTRACT
Care bundles may be an effective tool to standardise care for patients admitted with an exacerbation of chronic obstructive pulmonary disease (COPD). However, it is unclear how care bundles can be implemented without the need for additional resources. We redeployed a respiratory early discharge service (REDS) to deliver a COPD discharge bundle. We audited the effect of this service redesign on length of stay (LOS) and uptake of referrals to smoking cessation and pulmonary rehabilitation services. Of 1,742 patients with COPD, 1,170 received the discharge care bundle. Mean LOS for patients who received the discharge care bundle was 6.17 days versus 7.08 days for patients who did not. Smoking cessation and pulmonary rehabilitation referrals increased during the project year. A COPD discharge care bundle can be implemented on a large scale by redeploying a REDS without an increase on hospital LOS.
KEYWORDS: Care bundle, COPD, discharge support, exacerbations
Introduction
There is emerging interest in the delivery of discharge care bundles as a strategy to deliver comprehensive and equitable care to patients requiring hospital treatment. Care bundles usually take the form of a list of evidence-based interventions that, when grouped together, represent high quality of care for a specific condition. This approach was originally developed in the field of critical care medicine in the USA. Following work in the UK, it has been shown that in-hospital mortality reduced following the introduction of care bundles in eight clinical areas.1
In an uncontrolled small study, Hopkinson and colleagues2 observed a significant reduction in readmissions following the development and implementation of a chronic obstructive pulmonary disease (COPD) discharge bundle. This initiative was led by a research team who educated staff on a single respiratory ward to deliver the care bundle. They demonstrated significant increases in the referral rates to evidence-based interventions, such as smoking cessation services and pulmonary rehabilitation. However, the scaling up and delivery of COPD discharge bundles to larger patient populations may be constrained without additional resources.
Discharge support for patients admitted with an exacerbation of COPD is variable in the UK and has been viewed as unsatisfactory by patients. A survey of 307 people completed by the British Lung Foundation3 reported that only 25% of patients felt ready to leave hospital and only 34% felt informed about their COPD and the reason for hospital admission. Discharge support for patients admitted with an exacerbation of COPD in the UK is commonly offered via early supported discharge (ESD) schemes. The aim of these schemes is to facilitate the early discharge of patients admitted for treatment for an acute exacerbation of COPD (thereby reducing lengths of hospital stay) and, additionally, to provide appropriate support at home. A national COPD audit of COPD exacerbations in England and Wales4 highlighted that only 40% of patients were discharged under the care of an early or supported discharge scheme.
A local audit of patients admitted to our own centre demonstrated that only around one third of all patients met the inclusion criteria for the service, so the majority of patients admitted with an exacerbation of COPD did not receive coordinated and specialised support from the EDS team. Patients were discharged with the support of this service if they could be discharged within 5 days of admission. The team then completed a follow-up home visit to all patients accepted onto the service within 24 hours of discharge and a further visit within 7 days.
The evaluation of a COPD care bundle was identified as a key implementation project by the Leicestershire, Northamptonshire and Rutland CLAHRC rehabilitation theme. The local COPD network also identified the discharge care bundle as an important priority and provided its support by allocating transformational funds to provide the ‘SPACE for COPD’ manual,5 an established self-management resource, for the first year of the project. The COPD care bundle project was adopted as a local Commissioning for Quality and Innovation at University Hospitals of Leicester (UHL) NHS Trust in April 2012. This was an additional key local driver for implementation. Local delivery thresholds for care bundle delivery were set at 70% of all COPD discharges by the fourth quarter of 2012–13. There was no extra funding for staff to deliver the COPD discharge bundles, so there was a requirement to identify existing staff capacity in the respiratory teams.
A process of service redesign was supported by an NHS Improvement team who worked closely with the COPD care bundle project team. They were able to carefully process map existing services and highlighted potential options to help to implement the project. This process highlighted that the respiratory early discharge service (REDS) was well placed to deliver this initiative and a process of service redesign was commenced. An increase in staff capacity to cope with the anticipated rise in post-exacerbation pulmonary rehabilitation referrals was also secured via transformational funds for 1 year.
We aimed to audit the impact of implementing the discharge care bundle upon uptake to individual elements of the care bundle, including smoking cessation services and pulmonary rehabilitation programmes and to determine the impact of service redesign on lengths of hospital stay. We postulated that referrals to pulmonary rehabilitation and smoking cessation services would increase following implementation of the COPD discharge care bundle. Secondly, we wanted to establish the effect of this service redesign upon length of stay (LOS) because we were concerned that redeploying the EDS in this way might lengthen hospital stay.
Methods
The aforementioned service redesign of the REDS team was proposed and delivery of the discharge bundle commenced in April 2012. According to the policy activities that constitute research at the UHL NHS Trust this work met criteria for operational improvement activities and was, thus, exempt from ethics review.
The REDS team comprised COPD nurse specialists and they were identified as the team who would be responsible for implementing the COPD discharge bundle on a day-to-day basis. The UHL COPD discharge bundle project commenced in April 2012 at which time, the REDS team moved from completing home visits to support patients discharged on the early discharge scheme to coordinating and completing the COPD care bundle in the hospital setting.
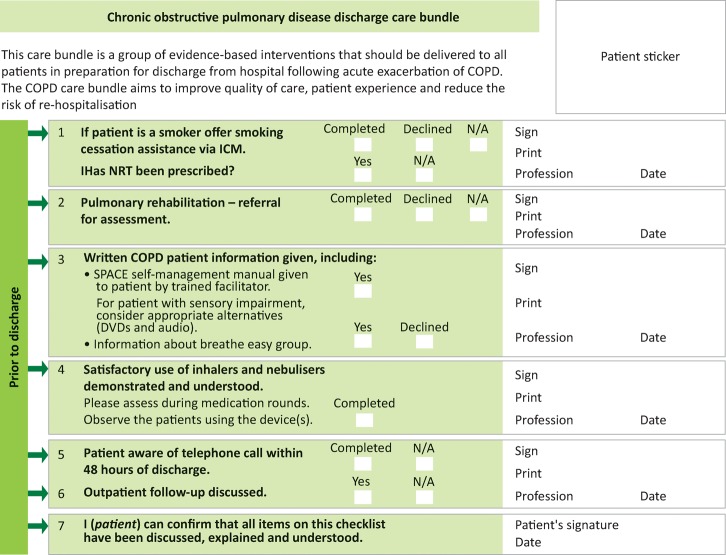
The COPD discharge care bundle (Fig 1) is based on the example documented by Hopkinson and colleagues2 and comprises the following elements:
referral to smoking cessation and pulmonary rehabilitation services
introduction of a self-management manual
assessment of inhaler technique.
Fig 1.
The COPD care bundle. Adapted from Hopkinson et al 2012.2 COPD = chronic obstructive pulmonary disease; ICM = iSoft Clinical Management (electronic referral system); NRT = nicotine replacement therapy
Patients were referred directly to the care bundle team if the primary reason for admission was suspected to be an exacerbation of COPD. The REDS team nurses liaised closely with respiratory ward teams to encourage referral to the COPD discharge care bundle; they also monitored new admissions to the clinical decisions unit to ensure maximal uptake. The REDS team worked with patients to deliver all elements of the care bundle and also completed follow-up phone calls at 2 working days and 15 days post discharge.
Project outcomes
We recorded the total number of patients discharged with a primary diagnosis of COPD (diagnosis code J41-44) from the Glenfield Hospital along with referral rates to smoking cessation and pulmonary rehabilitation services. Mean LOS for those patients receiving the care bundle was also recorded and compared to mean LOS for all COPD discharges from Glenfield Hospital for 2012–13 and 2011–12. This data was provided by UHL NHS Trust Business Analysis unit. REDS nurses collected 30-day readmission data for the patients who received the COPD care bundle.
Results
From April 2012 to March 2013, a total of 1,742 patients were discharged with a primary diagnosis of COPD. Of these, 1,170 (67.2%) patients received the COPD discharge bundle over the 12-month project duration (Table 1). Delivery rates of the COPD discharge care bundle increased throughout the duration of the year. The delivery rate for the first 3 months (Q1) was 53.8% of all COPD discharges from Glenfield Hospital. This rose to 67.0% in Q2, 70.5% in Q3 and to 73.4% in the final 3 months (Q4). Uptake to the individual elements of the care bundle also increased during the year. Smoking cessation referrals rose from 23.7% in Q1 to 48.3% in Q4. Out of 468 patients who stated that they were current smokers, 212 patients accepted a referral to smoking cessation services, so the overall uptake to smoking cessation services was 45%. Likewise, pulmonary rehabilitation referrals rose from 39.7% in Q1 to 55.9% in Q4.
Table 1.
Uptake of the COPD discharge care bundle, referral to smoking cessation and pulmonary rehabilitation services by project quarter
| Quarter | Received care bundle (n) | Referred to smoking cessation (n) | Referred to pulmonary rehabilitation (n) |
|---|---|---|---|
| 1 (Apr–Jun) | 228 | 20 | 88 |
| 2 (Jul–Sep) | 270 | 47 | 157 |
| 3 (Oct–Dec) | 330 | 75 | 190 |
| 4 (Jan–Mar) | 342 | 70 | 192 |
| Total | 1,170 | 212 | 627 |
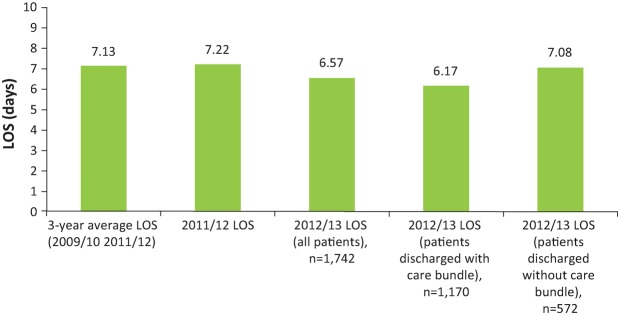
Average LOS for all COPD patients did not increase despite the withdrawal of the established respiratory early discharge service. Mean LOS for patients who received the discharge care bundle was 6.17 days compared with 7.22 days in 2011–12. The mean LOS for patients who did not receive the care bundle was 7.08 days (Fig 2). A total of 300 patients that received the care bundle were readmitted at 30 days (all causes). This is an all-cause readmission rate of 25.6%.
Fig 2.
Mean length of stay for patients discharged from Glenfield Hospital following admission for an acute exacerbation of COPD. COPD = chronic obstructive pulmonary disease; LOS = length of stay
Discussion
This audit has shown that a discharge COPD care bundle can be delivered on a large scale by redesigning an early discharge scheme to deliver a care bundle for a broader group of COPD patients without an increase in additional nursing staff resources. We were concerned that shifting away from an early discharge scheme would lead to an increased mean LOS. Reassuringly, these data indicate that LOS did not increase following the service redesign. Indeed, patients who received the care bundle had a reduced LOS in 2012–13 compared with the mean LOS for the 3 years previous to the implementation of the care bundle project. It is important to note that this reduction in LOS is in line with data from the COPD audit.4 We suggest that in light of national trends to shorter LOS, early discharge schemes may not be the most appropriate use of nurse specialist resources. Additionally, the COPD audit4 also recommends that COPD care bundles may be useful tools to improve the coordination of care at discharge. The COPD discharge bundle offers standardisation of the care offered to all patients admitted with an exacerbation of COPD, ensuring that key components of treatment are not forgotten. We suggest that a dedicated team is needed to ensure efficient and appropriate delivery of the bundle. Practitioners currently working in early discharge schemes may be best placed to coordinate its delivery.
Uptake of the COPD care bundle was not universal but increased throughout the project duration. This was expected as ward staff became increasingly familiar with the referral process. The REDS nurses worked throughout the length of the project to communicate the aims of the discharge care bundle with the multidisciplinary team. It should also be noted that the REDS team were only able to provide cover from Monday to Friday, so some patients who were admitted and discharged over the weekend may not have been referred. Additionally, there were discrepancies between the expected and actual code allocated for primary reason for admission. It is possible that the primary reason for admission for patients with significant comorbidities and disease complexity was not identified as being COPD but later coded as such after discharge. This could account for non-referral of these patients to the COPD discharge care bundle.
Those patients who did receive the care bundle received support from a dedicated team of COPD nurses and this may have led to improved communication with the multidisciplinary team and contributed to an overall reduced LOS. The completion of the care bundle was recorded in the medical notes, making it clear to the medical team that the patient had received the appropriate support and could be discharged when appropriate. Notably, the medical teams were aware that the REDS team would be providing telephone support at both 2 working days and 15 days post discharge. This may have provided reassurance about the level of follow-up care after discharge. It should also be noted there was no change to other community respiratory COPD pathways during this time.
We were able to demonstrate a large increase in referrals to smoking cessation services during the COPD discharge bundle project. Smoking cessation referral uptake rates of 48% by the end of the project were lower than those of 54% reported by Hopkinson and colleagues.2 However, it should be noted that the total number of current smokers was 25.5% in the cohort studied by Hopkinson et al2 compared with 40% in our cohort and this could account for difference in uptake to smoking cessation services.
A limitation of this audit is that readmission data for patients who did not receive the care bundle were not collected. We reported a 30-day readmission rate for patients that did receive the care bundle of 25.6% and this is similar to the 30-day readmission rate of 24% recorded in the latest national COPD audit.6 It is not known if COPD discharge care bundles are able to decrease readmission rates for patients with COPD. A recent 3-year randomised controlled trial was not able to demonstrate a decrease in readmissions.7 There is some early evidence from Hopkinson and colleagues2 that suggests there may be a trend for a reduction in readmissions but this is yet to be shown on a large scale.
Seymour et al8 have shown that early post-exacerbation pulmonary rehabilitation did reduce readmissions in this patient population. It may be reasonable to hypothesise that inclusion of pulmonary rehabilitation referral as an essential component in a care bundle may lead to an increased uptake in pulmonary rehabilitation and therefore help to prevent readmissions. We were able to document an increase in referrals to our post-exacerbation pulmonary rehabilitation programme following large scale delivery of the discharge bundle, but adherence and attendance rates have yet to be audited. Further longitudinal studies are needed to establish this case.
Conclusions
A COPD discharge care bundle can be implemented on a large scale by redeploying a respiratory early discharge service. This ensures standardised and equitable access to evidence-based interventions for patients discharged following an exacerbation of COPD without adversely impacting on LOS.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author contributions
LS and SJS had full access to all data from the study and take responsibility for the integrity of the data and the accuracy of the data analysis. LS drafted the article and SS, MS and SJS revised the article critically for important intellectual content and gave final approval of the version to be published.
Acknowledgements
SJS, SS and MS were supported by the CLAHRC East Midlands and/or NIHR Leicester Biomedical Research Centre (Respiratory). The views expressed are those of the author(s) and not necessarily those of the NHS and NIHR or the Department of Health.
The authors tweet using the following monikers:
• Louise Sewell = @LouiseSewell_OT
• Sally Schreder = @SallyBoyce1
• Michael Steiner = @Mickst46
• Sally J Singh = @SallySingh_
References
- 1.Robb E, Jarman B, Suntharalingam G, et al. Using care bundles to reduce in-hospital mortality: quantitative survey. BMJ 2010;340:861–6. [DOI] [PubMed] [Google Scholar]
- 2.Hopkinson NS, Englebretsen C, Cooley N, et al. Designing and implementing a COPD discharge care bundle. Thorax 2012; 67:90–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.British Lung Foundation , British Thoracic Society Ready for home? Improving hospital discharge care for people living with COPD. London: British Lung Foundation, 2010. [Google Scholar]
- 4.Stone RA, Holzhauer Barrie J, Lowe D, et al. COPD: Who cares matters. National Chronic Obstructive Pulmonary Disease (COPD) Audit Programme: Clinical audit of COPD exacerbations admitted to acute units in England and Wales 2014. National clinical audit report. London: RCP, 2015. [Google Scholar]
- 5.Mitchell KE, Johnson-Warrington V, Apps LD, et al. A self-management programme for COPD: a randomised controlled trial. Eur Respir J 2014;44:1538–47. [DOI] [PubMed] [Google Scholar]
- 6.Stone RA, Holzhauer Barrie J, Lowe D, et al. COPD: Who cares when it matters Most? National Chronic Obstructive Pulmonary Disease (COPD) Programme: outcomes from the clinical audit of COPD exacerbations admitted to acute units in England 2014. National supplementary report. London: RCP, 2017. [Google Scholar]
- 7.Jennings JH, Thavarajah K, Mendez MP, et al. Predischarge bundle for patients with acute exacerbations of COPD to reduce readmissions and ED visits: a randomised trial. Chest 2015;147:1227–34. [DOI] [PubMed] [Google Scholar]
- 8.Seymour JM, Moore L, Jolley CJ, et al. Outpatient pulmonary rehabilitation following acute exacerbation of COPD. Thorax 2010;65:423–8. [DOI] [PubMed] [Google Scholar]