ABSTRACT
Digital maturity assessments (DMAs) are a self-assessment mechanism for organisations. They can be effectively utilised to generate local digital roadmaps. In their simplest form, these allow organisations to understand their state of readiness to integrate digital technologies. This is achieved by assessing the capability and compatibility of their information systems to communicate or interface both within and across organisations. Through utilising and responding to the findings of DMAs, it is thought that the NHS will be better able to provide a patient-centred service to meet local needs within a national framework. It is this exchange and integration of information across health and social care systems that will drive innovation and transformation in the NHS.
KEYWORDS: Digital maturity, interoperability, learning healthcare system
Are we ready to use technology in the NHS?
Healthcare is acknowledged as being highly complex work, supporting an environment and a broad range of healthcare professionals to undertake a series of complex tasks and processes. Digital maturity assessments (DMAs) are a self-assessment mechanism for organisations. They can be effectively utilised to generate local digital roadmaps. In their simplest form, these allow organisations to understand their state of readiness to integrate digital technologies. This is achieved by assessing the capability and compatibility of their information systems to communicate or interface both within and across organisations.1 It is a novel concept that is evolving to be a critical discussion point.2–5 Through utilising and responding to the findings of DMAs, it is thought that the NHS will be better able to provide a patient-centred service to meet local needs within a national framework. It is this exchange and integration of information across health and social care systems that will drive innovation and transformation in the NHS.2,6–8
Moving towards a digital NHS
Well established in the digital health technology debate, electronic medical records are believed to be cornerstone to the advancement in digital maturity of a healthcare system or institution. The government's Personalised health and care 2020 plan outlines how data and technology should improve patient outcomes.4 It states that all medical records should be paperless by 2020 by means of electronic medical records. This is through creating the means to manage and transfer digital patient information across clinical and geographical boundaries, across an entire network of care providers.9,10 This sits at the centre of NHS England's digital strategy.1
Successful integration of electronic medical records exists predominantly within the primary care setting and mostly in mental health trusts. This success has not spread evenly across organisations operating within the NHS.11 Secondary acute care trusts are lagging behind, and this has led to recent recommendations to extend the implementation timeline to 2023.2,12 It is thought that a current shortfall in nationally approved templates and guidance has hindered wide-scale implementation.6 Looking forward, the government intends for assessments of digital maturity to be published annually and the overall map of the NHS's digital maturity to be assessed by the Care Quality Commission from 2018. This underpins the need for a system-wide approach to integrate new technologies to open up lines of communication across healthcare.
What is digital maturity?
DMAs are the second part of a four-stage comprehensive transformation programme that NHS England commenced in October 2015. DMAs ask an organisation's managers and front-line service users to understand the current capability of their digital landscape, through a series of questions. This is intended to identify the ‘anticipated, typical, logical and desired evolution path’ to readiness for an organisation.13 The implementation of these digital technologies is to enable transfers of patient care between different agencies at admission, referral or discharge. This includes the management of medicines, and the establishment and monitoring of clinical standards.14
DMAs can offer a pragmatic method to establish a ‘road map’ or inform a pathway. This enables organisations to understand and engage their staff, patients and technical providers, and to meaningfully challenge existing workflows with digital technology. As catalysts for change, DMAs may pose many challenges and question current practices of clinicians, hospital administrators, IT engineers and their organisations; however, opportunities exist (summarised in Table 1) for critical service transformation in a pressured NHS.
Table 1.
Building the case for digital maturity assessments
| Key questions | Opportunities |
|---|---|
| A unique opportunity to depart from traditional service arrangements | How are informatics systems designed and who do they serve? |
| An instrument-driving innovation to organise change | How can localised systems be interoperable with national solutions? |
| An opportunity to standardise a complex analytical process across care organisations | How to offset the need for patient privacy and information security against the need for clinicians to deliver care? |
| Defines what good information systems are and directs assessors to the type of data that is required, ie quantitative, qualitative and evidence of processes | How are staff supported and trained to use new information technologies? |
| This creates a foundation for defining the ‘digital architecture’ of information systems within an organisation | How to encourage innovation while ensuring operational ‘business as usual’? |
The framework is intended to provide a structured analytical approach with scope to accommodate for the needs of a local setting. The DMA process is staged into three components:
readiness
capability
infrastructure.
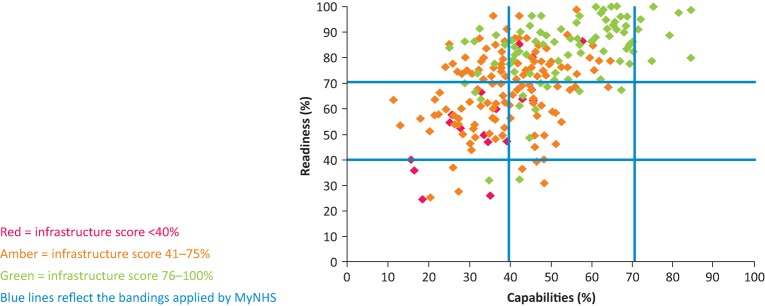
The analysis of concurrent data for each component provides a numerical and descriptive status of digital maturity. Fig 1 charts where all participating English NHS trusts were in January 2016.
Fig 1.
Digital maturity assessment across English healthcare regions in January 2016. Data from NHS England.
Interoperability
Transfers of care require developed digital systems to have interoperability. This is the ability for two or more units, departments and organisations to use and share information.7,14 This benefits care providers by revealing variation across services, institutions, organisations and regions of the health and social care system.15 This electronic exchange has the capability to identify where variability in care standards and quality are present.2,14,16
Digital architecture
The digital architecture defines how information systems are individually and collectively designed to interact. This determines how healthcare staff and patients engage with services. NHS England is intent on creating an open environment capable of supporting emerging new models of care, with common technical requirements called building blocks. Building blocks are essential for care providers and developers of innovative application tools to ensure patient information is managed efficiently while not compromising patient privacy, but still providing sufficient clinical data.7
Digital strategy and literacy
Digital maturity is dependent on strategies that necessitate an organisation functions collaboratively and with an ethos compatible with the wider NHS transformational healthcare agenda. Flott et al15 outline significant problems with global DMA frameworks as they currently exist. Frameworks are currently unable to evaluate care pathways over time and offer no evidence of how digital maturity can ease a patient's entire care pathway. Flott et al flag issues for how DMAs inform the digital architecture of health organisations and the implications for understanding how interoperability and system analytics manage patient quality and safety.15
This is not just about implementing more and better technologies, readiness involves digital congruence, aligning strategy to patient outcomes. This digital evolution in the NHS is forging the beginning of ‘learning health systems’ capable of reducing error and promoting patient safety and quality.13,16–18
A pathway to digital maturity
The NHS has committed to generating its first digital maturity index, which will be annually updated.13 This index has informed pre-requisites to readiness for each of the 73 local digital roadmaps that are now championed by appointed chief clinical information officers across 211 clinical commissioning groups.
There are notable innovations already shaping NHS digital performance, infrastructure, readiness and capability. This extends beyond electronic health records and key areas of enterprise are:
analytics performance benchmarks
test beds for combined innovations
telehealth
healthcare apps
integrated care
privacy and security.
Analytics performance benchmarks
The rapid emergence of digital health technologies holding electronic data is generating large complex and diverse datasets, commonly referred to as ‘big data’.16,19,20 This information is unmanageable for common data management tools and methods. This proliferation of ‘big data’ is producing a new knowledge-set of science to understand patterns and trends in healthcare and is proving to be increasingly effective in supporting decisions – from patient medical management to directing institution operations or national healthcare strategy.2,20
Test beds for combined innovations – implementation models
Test beds enable a collective understanding of how technologies influence each other and how their outcomes on patients are supported to provide innovation within the ‘real world’. Test bed centres are now established across seven sites in England; these sites comprise clinical environments committed to developing appropriate conditions and platforms for supporting new technologies and or practices.8,21
Telehealth (telecare and telemedicine)
Telehealth is a rapidly developing specialty of care that applies a combination of concurrently developing telecommunication technologies to deliver healthcare at a distance. The multiple terms highlight the variety of formats that have recently emerged, responding to a diverse range of clinical settings – ie inpatient, outpatient and social care, where telehealth is being implemented.6,22,23
Healthcare application program interfaces
Application program interfaces permit open access to NHS data for web and mobile technologies. These standards are being applied to invite innovation to harness opportunity, internal as well as external to the NHS, to attain digitals tools (apps) that may benefit the healthcare services.
Integrated care models
The Integrated Digital Care Fund in 201424 was designed to invest in greater movement of digital information, to improve access to all providers across health and social care. The primary objective being to deliver information capable of being available at the point of need to improve outcomes and provide informed responsive care.
Privacy and security
As digitisation rapidly progresses so will the necessity for innovative technology that facilitates accessibility to patient health information from a range of medical and social care sources while also ensuring information governance. This requires new systems to evolve with adequate measures embedded to safeguard security and privacy to patients. In the near term this calls for optimisation of existing software across the NHS as well as calling upon new models for empowering patients to manage their own data with opt-out consent.25,26
Conclusions
Improving digital maturity across the NHS is critical. Digital versatility and innovation demands a high level of digital maturity and an interoperable means of transferring data within and across health and social care organisations.7,27
Education regarding analytics will be necessary to support senior decision makers in healthcare services to ensure they are fully equipped to understand the types of data being collected and what constitutes digital readiness. Emerging literature suggests healthcare organisations would benefit from implementing a peer validation process for how DMAs are implemented within and across organisations as well as addressing how care pathways can be accurately captured. Digital maturity is acknowledged as an enabler of service transformation and the digital maturity agenda may be a key transformative component in delivering modern day care.28
Conflicts of interest
The author has no conflicts of interest to declare.
Daniel Johnston tweets using the moniker @Dansjohnston
References
- 1.NHS England The forward view into action: paper-free at the point of care completing the digital maturity self-assessment. London: NHS, 2015. [Google Scholar]
- 2.Wachter R. Making IT work: harnessing the power of health information technology to improve care in England. Report of the National Advisory Group on Health Information Technology in England. London: National Advisory Group on Health Information Technology in England, 2016. [Google Scholar]
- 3.NHS England Safer hospitals safer wards: achieving an integrated digital care record. Leeds: NHS England, 2014. [Google Scholar]
- 4.NHS England Personalised health and care 2020: using data and technology to transform outcomes for patients and citizens. A framework for action. Leeds: NHS England, 2014. [Google Scholar]
- 5.NHS England Five year forward view. Leeds: NHS England, 2014. [Google Scholar]
- 6.Honeyman M, Dunn P, McKenna H. A digital NHS? An introduction to the digital agenda and plans for implementation. London: The Kings Fund, 2016. [Google Scholar]
- 7.NHS England, HSCIC, South, Central and West Commissioning Support Unit Interoperability Handbook. Leeds: NHS England, 2015. [Google Scholar]
- 8.Wilson P, Boaden R, Harvey G. Plans to accelerate innovation in health systems are less than IDEAL. BMJ Qual Saf 2016;25:572–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boonstra A, Versluis A, Vos JF. Implementing electronic health records in hospitals: a systematic literature review. BMC Health Serv Res 2014;14:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarke A, Adamson J, Sheard L, et al. Implementing electronic patient record systems (EPRs) into England's acute, mental health and community care trusts: a mixed methods study. BMC Med Inform Decis Mak 2015;15:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sood HS, McNeil K. How is health information technology changing the way we deliver NHS hospital care? Future Healthcare Journal 2017;4:117–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clarke A, Watt I, Sheard L, Wright J, Adamson J. Implementing electronic records in NHS secondary care organizations in England: policy and progress since 1998. Br Med Bull 2017;121:95–106. [DOI] [PubMed] [Google Scholar]
- 13.De Carvalho JV, Rocha A, Vasconcelos J. Towards an encompassing maturity model for the management of hospital information systems. J Med Syst 2015;39:99. [DOI] [PubMed] [Google Scholar]
- 14.Gottschalk P. Maturity levels for interoperability in digital government. Government Information Quarterly 2009;26:75–81. [Google Scholar]
- 15.Flott K, Callahan R, Darzi A, Mayer E. A patient-centered framework for evaluating digital maturity of health services: a systematic review. J Med Internet Res 2016;18:e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kaggal VC, Elayavilli RK, Mehrabi S, et al. Toward a learning health-care system – knowledge delivery at the point of care empowered by big data and NLP. Biomed Inform Insights 2016;8(Suppl 1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ovretveit J, Nelson E, James B. Building a learning health system using clinical registers: a non-technical introduction. J Health Organ Manag 2016;30:1105–18. [DOI] [PubMed] [Google Scholar]
- 18.Kane G, Palmer D, Phillips A, Kiron D, Buckley N. Aligning the organization for its digital future. Boston: MITSloan Management Review, 2016. [Google Scholar]
- 19.Krumholz H. Big data and new knowledge in medicine: the thinking, training, and tools needed for a learning health system. Health Aff 2014;33:1163–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raghupathi W, Raghupathi2 V. Big data analytics in healthcare: promise and potential. Health Inf Sci Syst 2014;2:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.NHS England Real world testing of ‘combinatorial innovation’: a global invitation to innovators. Leeds: NHS England, 2015. [Google Scholar]
- 22.Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015;(9):CD002098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mackintosh N, Terblanche M, Maharaj R, et al. Telemedicine with clinical decision support for critical care: a systematic review. Syst Rev 2016;5:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.NHS England Integrated Digital Care Technology Fund. www.england.nhs.uk/digitaltechnology/info-revolution/idct-fund/ [Accessed 25 August 2017].
- 25.National Data Guardian for Health and Care Review of data security, consent and opt-outs. Leeds: Office of the National Data Guardian, 2016. [DOI] [PubMed] [Google Scholar]
- 26.Department of Health, Data Sharing and Cyber Security Team Your data: better security, better choice, better care. Government response to the National Data Guardian for Health and Care's review of data security, consent and opt-outs and care quality commission's review ‘safe data, safe care’. London: Department of Health, 2017. [Google Scholar]
- 27.NHS England Open API Architecture Policy. Leeds: NHS England, 2014. [Google Scholar]
- 28.Tan J. Healthcare information technology innovation and sustainability: frontiers and adoption. Hershey PA: Medical Information Science Reference, 2015. [Google Scholar]