ABSTRACT
Medicine is increasingly complex, involving a highly connected system of people, resources, processes, and institutions. Attempts to improve care involve disruptions to this system, with the potential for wide-ranging consequences, both positive and negative. Despite this, many improvement methodologies are poorly equipped to manage either complexity or risk – instead focusing on discrete interventions whose effects are narrowly monitored. Engineers have long understood that complex problems require a systems view, and that attempts to make things better can themselves introduce new risk into a system. Given this, an engineering systems approach may be of significant value to those trying to improve healthcare. Two fundamental questions emerge from such an approach: what can we do better, and what could possibly go wrong? This paper describes the evolution of a systems approach to healthcare, and explores a recently co-developed framework outlining a systems approach based upon a synergy between healthcare and engineering.
KEYWORDS: Systems approach, systems engineering, quality improvement, healthcare improvement, healthcare systems
Introduction
Healthcare is the product of a complex adaptive system of people, equipment, processes, and institutions working together. Problems can arise with either deficiencies in individual system elements, or in their relationship with each other, and improving the overall function of such a system can be challenging.1 This insight – a systems view of healthcare – reframes our understanding as to how care is delivered and can be improved.
A striking example of this is the case of Dr Hadiza Bawa-Garba,2,3 a paediatrician convicted of gross negligence and manslaughter in 2015, temporarily suspended from practising medicine by a medical practitioners tribunal, and later struck off by the General Medical Council (GMC). The case has raised many questions both about how we allocate blame when systems fail and how we improve them in the future to avoid catastrophe. The British Medical Journal (BMJ) responded: ‘It is tragic that a child has died. But no one is served when one doctor is blamed for the failings of an overstretched and understaffed system.’4
The Bawa-Garba case highlights the complexity of direct healthcare, where the actions of an individual doctor can be contextualised within a team, a ward, and a hospital all facing deficiencies. However, it also throws into relief the wider system in play – of regulatory bodies, the legal framework within which medicine is practised, the media, and prevailing cultural attitudes toward the NHS.
‘Systems that work do not just happen, they need to be planned, designed and built.’ This is the view of the Royal Academy of Engineering,5 experts in the design of complex systems. Engineers have long understood that well designed systems can prompt individuals toward desired behaviours, and act to restrain them from undesirable ones. This understanding is reflected in much of the medical literature around improvement from fields such as quality improvement, implementation science, and operational research. However, a consolidated systems approach to healthcare improvement has been elusive.
Critics of a systems approach to healthcare might argue that it is simply a mechanism to absolve individuals where they have made mistakes or acted inappropriately, or that it is an excuse to paint improvement as too difficult to attempt. We argue instead that a systems approach should seek to answer fundamental questions about the people involved in a given situation, the wider system in which they operate, the opportunities for risk, and what can be designed to mitigate these. There will be occasions where individuals are culpable, where machines fail, or where processes are weak; the system should be designed to reduce the possible harm which results. More optimistically perhaps, robust systems offer the opportunity for increased quality and efficiency without a commensurate increase in material resources – an increasing priority for an NHS under pressure.
Background to the need for a systems approach
The idea of a systems approach is not new. The first half of the 20th century saw a growing interest in systems and their inherent complexities in several disciplines including engineering and biology.6 Within healthcare, however, the turn of the new millennium may be seen as a watershed in the recognition of a systems approach to improvement.
The World Health Report 2000 had a primary focus on health systems.7 This report on global health systems began to address questions around the elements of a good health system and the monitoring of system performance. In the following few years, high profile reports were published both in the USA and the UK that were to significantly challenge the status quo and justify the need for a better approach to improving the quality of the healthcare delivery systems in these countries.
In the USA, the publication of two key reports by the Institute of Medicine (IOM) – To err is human8 and Crossing the Quality Chasm9 – demonstrated a disparity in the state of patient safety and the concerning discrepancy between the care that was possible and that which many patients were receiving. The revelation of these challenges within the American healthcare system were enough to raise quality of healthcare to centre stage.
Similar challenges were being described in the UK over the same period.10–12 A report into the systematic failures that led to the deaths of nearly 30 children at the Bristol Royal Infirmary (BRI) in 2001 concluded that the poor performance and errors identified at the BRI were the results of systems which were poorly performing.13 More importantly, the report suggested that these problems were reflective of the state of the wider NHS at the time. In response to these findings the Department of Health (DoH) made far-reaching changes to the health system with a focus on standards, performance monitoring, patient-centeredness, patient and public involvement. The response also provided opportunity for design and systems engineers to contribute to the challenges through a commitment to ‘working with the Design Council to identify opportunities for design solutions to patient safety’.14 The Design Council also establishes the RED team to bring design thinking to healthcare improvement and transformation.15,16
This led to the first review of design and systems practice within the NHS. The review concluded that ‘the NHS is seriously out of step with modern thinking and practice with regard to design’.17 Since then, several reports, initiatives and models have been produced but of particular relevance is Building a Better Delivery System, the report which launched the ‘New Engineering/Health Care Partnership’.18 More than a dozen major reports had echoed the essence of this new partnership by 2010 with many describing the heightened interest in solving problems in healthcare delivery using industrial and systems engineering tools.19 More recently, the President’s Council of Advisors on Science and Technology (PCAST) recommended that a systems engineering approach be propagated at all levels of the health care system in the USA.20
Several other high profile reports have consistently alluded to the need for a systems approach, although often lacking guidance on how to realise this at any level of the NHS or in the USA.17,21–32 Even within the academic literature, it is difficult to find a definition or presentation of a systems approach that lends itself to pragmatic improvement efforts.
Realising a systems approach in practice
In 2016, in response to the calls to adopt a systems approach to designing and delivering high-quality services in the UK, the Royal Academy of Engineering (RAEng), in collaboration with the Royal College of Physicians (RCP) and the Academy of Medical Sciences (AMS), established a cross-disciplinary Working Group to work with the health and care professions to explore how engineers can add to current understanding and practice of systems engineering in quality improvement and healthcare design.’
To an engineer, the world is full of systems. From the simple water heater to the fully integrated international airport, all systems share one key feature: their elements together produce results not obtainable by the same elements alone. A systems approach involves integrating the necessary disciplines into a team who then use a structured process to deliver a system, working from needs to requirements and from design to delivery.33–35 A systems approach has also been described as
…a framework for seeing interrelationships rather than things, for seeing patterns rather than static snapshots – it is a set of general principles spanning fields as diverse as physical and social sciences, engineering, and management.36
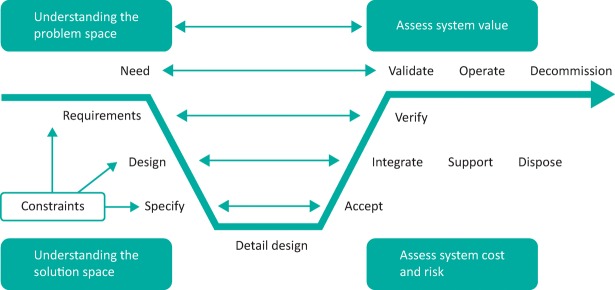
This can be depicted as a ‘V-model’ (Fig 1), which illustrates the logical relationships between different activities. However, to those unfamiliar with the language of systems engineering, the nuances and value of the V-model may be difficult to appreciate.
Fig 1.
The INCOSE (2009) V-model.
Early discussions within the RAEng Working Group reflected on the importance of people, systems, design and risk perspectives on a system, and on the realisation that particular focus on these complementary views could deliver many of the benefits of a systems approach (Table 1).
Table 1.
The elements of a systems approach
| Perspective | Description |
|---|---|
| People | The understanding of interaction among humans and other elements of a system in order to optimise human wellbeing and overall system performance |
| Systems | The means to address complex and uncertain problems, involving highly interconnected technical and social entities that produce emergent behaviour |
| Design | The identification of the right problem to solve, creation of solution options and refinement of the best of these to deliver an appropriate solution to the problem |
| Risk | The management of what can go wrong (and right), based on the identification, assessment and management of hazards and opportunities present within the system |
These perspectives provided the framework for a series of workshops with engineers and health and care professionals to explore the relevance of each perspective to health and care improvement and to express them as a series of open questions. These were subsequently merged with a number of project management questions to form a simple spiral (Fig 2), an ordered list of questions pertinent to systems improvement. The spiral illustrates that the questions are revisted at each stage of design and delivery in an iterative manner.
Fig 2.
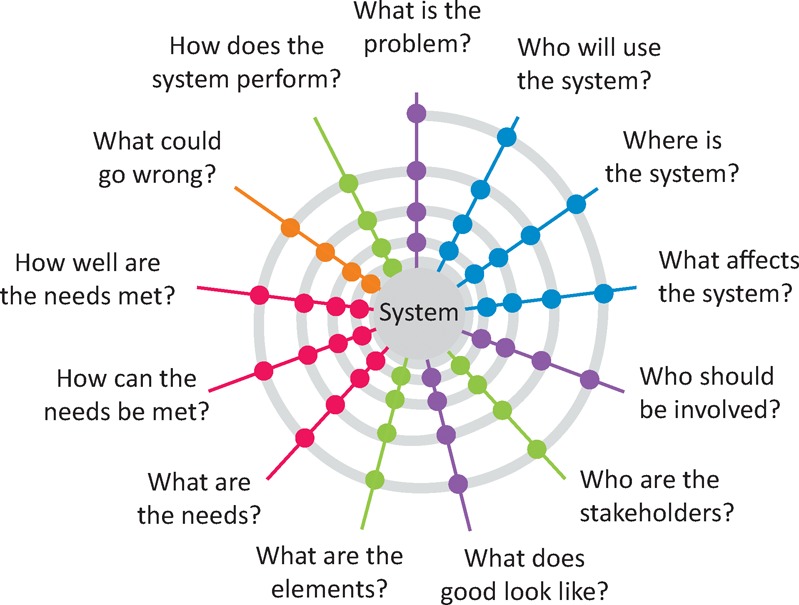
A spiral model of the questions that define an iterative approach to health and care improvement.
This representation, of an idealised view of a systems approach, does little to guide how it might be used in practice. The health and care professionals consulted were more used to a linear improvement process, typified as one that transforms current performance into something measurably better (Fig 3). This approach is common to all improvement processes with a focus on the critical stages required for success (Table 2).
Fig 3.
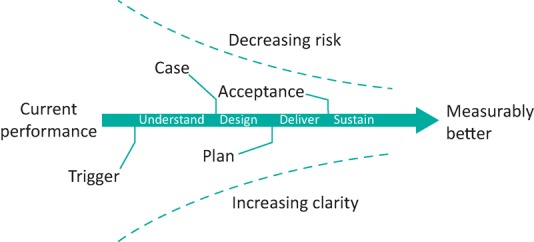
A linear improvement process transforming current performance into a measurably better state.
Table 2.
The critical stages of an improvement approach
| Stage | Description |
|---|---|
| Understand | Leads to a description of the current system (now), a common understanding of the problem, a consensus view of what the future system might look like (better) and a clearly articulated case for changing the system |
| Design | Leads to a clear description of the future system, based on the iterative design of the system architecture with its elements and interfaces, the evaluation through successive prototyping of its likely behaviour, and a plan for its delivery |
| Deliver | Leads to the successful deployment of the new system with the levels of measurement necessary to evidence its success, and acceptance that it achieves appropriate value for its stakeholders |
| Sustain | Leads to the continued operational success of the new system along with consideration of further improvement potential or wider deployment |
The linear (improvement) and spiral (systems) models may be combined to generate a helical model of health and care improvement (Fig 4). This resonated with health and care improvement specialists, going some way toward translating the description of a systems approach into a practical implementation guide. To help further, case studies from published work were used to illustrate the potential of a systems approach in practice, reviews of improvement approaches eg the Model for Improvement, Lean etc, and key literature were undertaken. Further background to the core concepts were provided. The final report, Engineering Better Care: a systems approach to health and care design and continuous improvement,37 provides an accessible description of a systems approach, and how it can build on current approaches to improvement in healthcare, nearly 20 years after the first call to adopt such an approach.17
Fig 4.

A systems-spiral improvement process. An ordered and iterative set of activities drawn from people, systems, design and risk perspectives and linked to the spiral questions, applied at each stage of the improvement process.
A healthcare–engineering synergy
The practice of healthcare can be conceived as two objectives: to provide care, and to avoid causing harm. Similarly, engineering can be considered as the practice of solving problems, while managing the risk inherent in those solutions. A shared understanding between engineering and healthcare might then be – what can we do better, and what could possibly go wrong?
In England the New Care Models programme38 and similar work, are showing promise in a redesigning and delivering health and care systems to meet population and system needs. These have had varying approaches to design and improvement, with varying outcomes.
The value of the systems approach put forward in Engineering Better Care is that it provides a simple framework for those trying to improve care to reflect on their efforts with a new perspective. Seeking to answer the questions posed prompts reflection on both the methodologies used, and the desired outcomes. This does not need to supplant existing methods, but instead might suggest where alternative techniques could add value. The ongoing challenge is to bring this framework to bear on real problems, in partnership with those already striving to make things better.
Further work is now underway to develop a practical toolkit that transforms the systems approach into practice (Fig 5). The focus here is on the definition of a range of simple but effective interventions to identify a real need, define a problem and a business case for change, develop viable solutions and deliver the preferred solution into practice.
Fig 5.
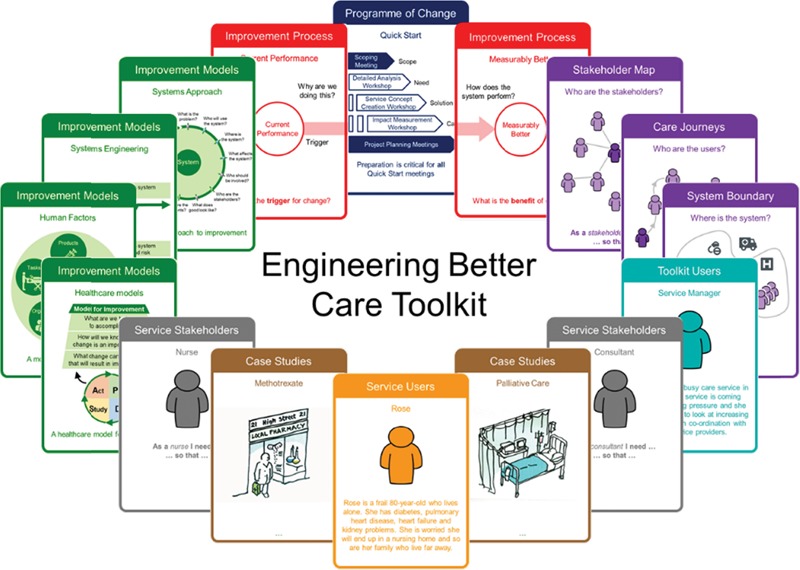
An Engineering Better Care toolkit, facilitating a systems approach to health and care improvement.
References
- 1.Braithwaite J. Changing how we think about healthcare improvement. BMJ 2018:k2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dyer C. Bawa-Garba case has left profession shaken and stirred. BMJ 2018:k456. [DOI] [PubMed] [Google Scholar]
- 3.Dyer C. Paediatrician convicted of manslaughter must be erased from register, rules High Court. BMJ 2018:k417. [DOI] [PubMed] [Google Scholar]
- 4.Ladher N, Godlee F. Criminalising doctors. BMJ 2018:k479. [DOI] [PubMed] [Google Scholar]
- 5.Elliott C, Deasley P. Creating Systems That Work: Principles of Engineering Systems for the 21st Century. R Acad Eng 2007;293074. [Google Scholar]
- 6.Jackson MC. Systems approaches to management. Springer US, 2000. [Google Scholar]
- 7.World Health Organization. World Health Report: 2000: Health Systems: Improving performance. Geneva: World Health Organisation, 2000. [Google Scholar]
- 8.Kohn LT, Corrigan J, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academy Press, 2000. [PubMed] [Google Scholar]
- 9.Institute of Medicine (IOM) Crossing the quality chasm. crossing the quality chasm: a new health system for the 21st century. National Academies Press, 2001. [PubMed] [Google Scholar]
- 10.Department of Health The NHS plan: a plan for investment, a plan for reform. Crown Copyright, 2000. [Google Scholar]
- 11.Department of Health An organisation with a memory: report of an expert group on learning from adverse events in the NHS. DH, 2000. [Google Scholar]
- 12.Department of Health Building a safer NHS for patients: implementing an organisation with a memory. DH, 2001. [Google Scholar]
- 13.Kennedy I. Learning from Bristol: The report of the public inquiry into children’s heart surgery at the Bristol Royal Infirmary 1984–1995. 2001. [DOI] [PubMed] [Google Scholar]
- 14.Department of Health Learning from Bristol: The Department of Health’s response to the report of the public inquiry into the death of children’s heart surgery at Bristol Royal Infirmary 1984–1995. DH, 2002. [Google Scholar]
- 15.Cottam H, Leadbeater C. RED Paper 01, Health: Co-creating services. The Design Council, 2004. [Google Scholar]
- 16.Burns C, Cottam H, Vanstone C, Winhall J. RED Paper 02, Transformation design. The Design Council, 2006. [Google Scholar]
- 17.Buckle P, Clarkson PJ, Coleman R. et al. Design for patient safety: a system-wide design-led approach to tackling patient safety in the NHS. DH, 2003. [Google Scholar]
- 18.Reid PP, Compton WD, Grossman JH, Fanjiang G. Building a better delivery system: a new engineering/health care partnership. Washington DC: National Academies Press (US), 2005. [PubMed] [Google Scholar]
- 19.Valdez RS, Ramly E, Brennan P. Industrial and systems engineering and health care: critical areas of research – final report. Rockville, MD: Agency for Healthcare Research and Quality, 2010. [Google Scholar]
- 20.Cassel CK, Saunders RS. Engineering a better health care system: A report from the president’s council of advisors on science and technology. JAMA 2014;312:787–8. [DOI] [PubMed] [Google Scholar]
- 21.Department of Health High quality care for all. DH, 2008. [Google Scholar]
- 22.Department of Health Equity and Excellence: Liberating the NHS. DH, 2010. [Google Scholar]
- 23.Department of Health Innovation health and wealth: accelerating adoption and diffusion in the NHS. DH, 2011. [Google Scholar]
- 24.Boyle S. United Kingdom (England): Health system review. Health Syst Transit 2011;13:1–483. [PubMed] [Google Scholar]
- 25.National Advisory Group on the Safety of Patients in England A promise to learn – a commitment to act. Improving the safety of patients in England. 2013. [Google Scholar]
- 26.Future Hospitals Commission Future hospitals: Caring for medical patients. RCP, 2013. [Google Scholar]
- 27.Francis R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry Executive Summary. London: The Stationery Office, 2013. [Google Scholar]
- 28.Keogh B. Review into the quality of care and treatment provided by 14 hospital trusts in England: Overview report. NHS England, 2013. [Google Scholar]
- 29.NHS England Five Year Foward View. NHS England, 2014. [Google Scholar]
- 30.Pronovost PJ, Ravitz AD, Stoll RA, Kennedy SB. Transforming patient safety a sector-wide systems approach: Report of the WISH Patient Safety Forum 2015. WISH, 2015. [Google Scholar]
- 31.Kaplan G, Bo-Linn G, Carayon P. et al. Bringing a systems approach to Health. Washington, DC: Institute of Medicine and National Academy of Engineering, 2013. [Google Scholar]
- 32.Grossmann C, Goolsby WA, Olsen L, Mcginnis JM, Academy N. Engineering a learning healthcare system. Washington, DC: The National Academies Press, 2011. [Google Scholar]
- 33.Cowper D, Elphick J, Kemp D, Evans R. 8.2.1 To V or not to V – that MUST be the question: knowing when to apply the right approach. INCOSE Int Symp 2014;24:793–814. [Google Scholar]
- 34.NASA NASA Systems Engineering Handbook. Vol 6105; 2007. [Google Scholar]
- 35.Greene MT, Gonzalez R, Papalambros PY, McGowan A-M. Design thinking vs systems thinking for engineering design: what’s the difference? ICED 2017 Conference Proceedings 2017;2:467–6. [Google Scholar]
- 36.INCOSEUK What is systems engineering? Creating successful systems. Z Guides, Issue 3.0 March; 2009. Available at http://incoseonline.org.uk/Documents/zGuides/Z1_What_is_SE.pdf [Accessed 13 September 2018]. [Google Scholar]
- 37.Clarkson PJ, Bogle D, Dean J. et al. Engineering better care: a systems approach to health and care design and continuous improvement. London: Royal Academy of Engineering, 2017. [Google Scholar]
- 38.England NHS. NEW care models: Vanguards – developing a blueprint for the future of NHS and care services. NHS England, 2016. [Google Scholar]