ABSTRACT
Young people often experience worse health outcomes and more dissatisfaction with healthcare compared with other age groups. This survey sought to determine the state of adolescent and young adult health training across medical specialties in the UK. An online questionnaire was distributed to higher specialty trainees in adult medical specialties. Training in adolescent/young adult health/transition was rated as minimal/non-existent by 70/73% of respondents, respectively; 52% reported that they had received no formal training and 61% had never attended a dedicated young person’s or transition clinic. The most significant barrier to delivering good adolescent and young adult healthcare was felt to be lack of training to deal with adolescent issues. This survey has identified a ‘training gap’; a lack of preparation to meet the specific care needs of the adolescent and young adult population. Improved interventions are required to help drive improvement in care for young people in the UK.
KEYWORDS: Adolescent, medical education, young adult
Introduction
The chief medical officer report, Our children deserve better: prevention pays, highlighted the importance, across all specialties, of optimising care for adolescents and young adults and improving the delivery of transition.1 The underlying evidence to support this call is that adolescents and young adults in the UK have worse long-term health outcomes compared with other age groups and compared with other developed countries.1–8
Young people aged 16–24 years consistently report poorer experience of NHS care than older adults.2,9 This population includes both young people, who find themselves acutely unwell, accessing adult services for the first time and those with long-term conditions, previously in paediatric services, requiring transition and transfer to adult services. While guidance is available to support transition,10–13 although with variable implementation,3,14,15 the specific needs of the young people presenting for the first time are largely overlooked.9
There is a need to address these issues and a body of literature has emerged that has highlighted that lack of training is one of the main barriers in the delivery of adolescent and young adult care.16–21 The 2016 National Institute for Health and Care Excellence guidance on transition from children’s to adult services13 has therefore emphasised the requirement for appropriate training for healthcare professionals involved in dealing with young people going through this process. In this survey, we aimed to look at the current state of training in adolescent and young adult health, including transition, among a sample of higher specialty trainees in the UK.
Methods
An online questionnaire based on existing formats22 was developed. The survey was accessible from December 2013 to September 2014 via a link on the NHS e-portfolio for trainees and also through email alerts sent by the Royal College of Physicians and specialist societies. There was no requirement for ethical approval or informed consent in this survey of medical trainees.
Questionnaire
The following sections were included in the survey.
About you and your region
Trainees were asked for their specialty, age, gender, stage of training (year of their higher specialty training) and region.
About your training
Trainees were asked to rate training and clinical exposure in adolescent and young adult health and in transition as either non-existent, minimal, average, good or excellent. Whether formal training had been received was recorded and rated using the same scale. Trainees were asked to estimate the number of dedicated clinics they had attended during the course of their higher specialty training.
About your practice
Trainees were asked to rate barriers they experience in working with adolescents and young adults from 1 to 5, with 1 representing the least significant and 5 the most significant barrier.23,24
About your training needs
Training needs were recorded overall as well as in specific areas. The specific areas were identified from a survey of healthcare professionals working in rheumatology.22 Trainees were asked to rate each specific training need from 1 to 5, with 1 representing the lowest level of need and 5 the highest level of need.
An option to add free text responses or explanations was provided in the survey.
Results were collated and analysed using Microsoft Excel/Numbers for Mac.
Results
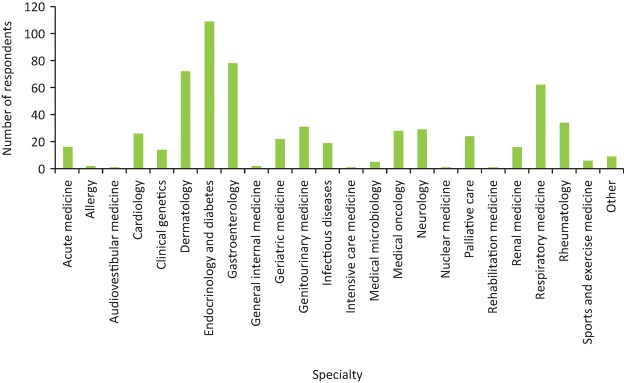
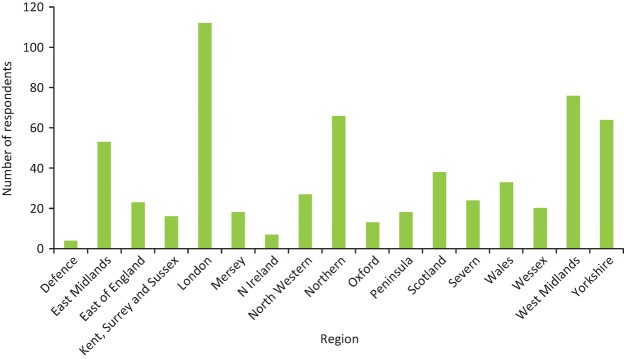
Responses were received from 613 trainees (39% male) across 23 medical specialties. This represents a response rate of approximately 10% (based on 6,500 higher specialty trainees). The highest response rates were in the specialties of dermatology, endocrinology and diabetes, gastroenterology and respiratory medicine (Fig 1). All years of higher specialty training were represented: year 1 (18%), year 2 (19%), year 3 (25%), year 4 (24%) and year 5+ (14%). All areas of the UK were represented, with the largest response number from London trainees, followed by those in the West Midlands, Northern and Yorkshire and Humberside Deaneries (Fig 2).
Fig 1.
Survey response rate by specialty.
Fig 2.
Survey response rate by region.
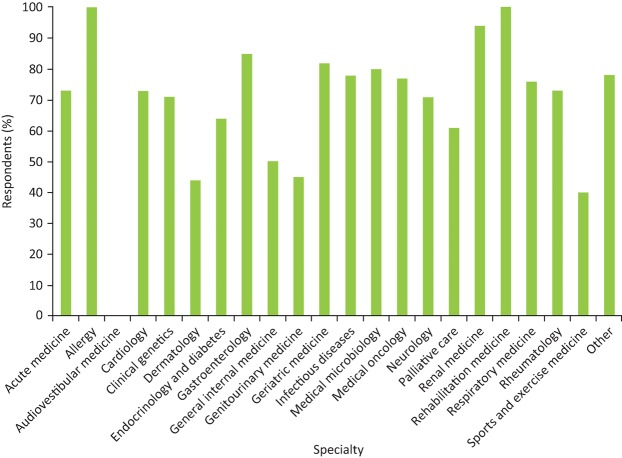
Training in adolescent and young adult health was reported to be minimal or non-existent by 70% of respondents, while training in transition was rated as minimal or non-existent by 73% (Fig 3). The perception of training experience in each individual specialty varied (Fig 4) with the percentage of trainees rating training as minimal or non-existent ranging from 0–100% (interquartile range 61.8–79.5%).
Fig 3.
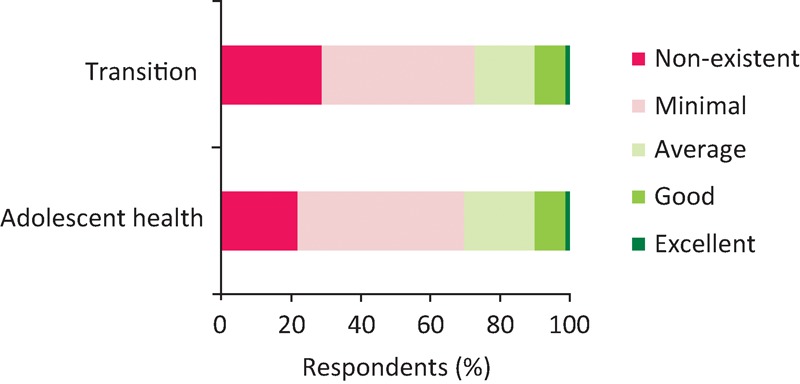
Trainee satisfaction with training in transition and adolescent and young adult health.
Fig 4.
Proportion of respondents rating adolescent and young adult health training as minimal or non-existent by specialty.
In total, 52% of respondents reported no formal training in adolescent and young adult health or transition; 11% had received training as undergraduates and 30% as postgraduates. Very few trainees (7%) had accessed e-learning on adolescent and young adult health. Of those who had received some form of formal training, 4% rated it as excellent, 33% as good, 33% as average and 30% as below average.
The majority of trainees had not attended any dedicated adolescent or young adult clinics during their training programme (61%). Only 7% reported attending more than 10 clinics. When assessing clinic attendance by year of training, 45% of final year trainees still reported no attendance at dedicated clinics, compared with 67% of first year higher specialty trainees. The number attending more than 10 clinics increased from 1% in the first year to 11% in the final year. Of those attending more than 10 clinics, 62% of them were trainees in endocrinology and diabetes.
Seniority of trainee did not impact on experience of training, with the highest percentage (71%) rating training as minimal or non-existent in their final year. Number of clinics attended did have an effect on perception of training (as shown in Table 1), with trainees attending more clinics rating training more highly.
Table 1.
Clinic attendance, year of training and impact on experience of training
| Number of clinics | ||||||||
|---|---|---|---|---|---|---|---|---|
| Year of training | 0 | 1–2 | 3–5 | 6–10 | 11–20 | >20 | No answer | Minimal/non-existent, % |
| 1 | 67 | 9 | 9 | 7 | 0 | 1 | 7 | 67 |
| 2 | 57 | 15 | 14 | 4 | 0 | 1 | 9 | 66 |
| 3 | 54 | 15 | 9 | 5 | 2 | 8 | 7 | 69 |
| 4 | 59 | 14 | 10 | 8 | 3 | 6 | 0 | 64 |
| 5+ | 45 | 15 | 11 | 15 | 5 | 6 | 3 | 71 |
| Minimal/non-existent, % | 81 | 79 | 46 | 51 | 27 | 24 | – | – |
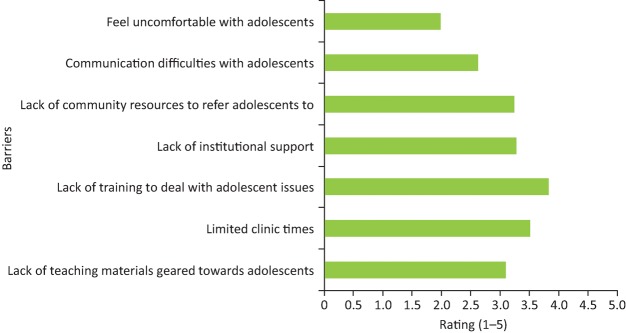
The main barriers cited by trainees were lack of training to deal with adolescents and limited clinic time (Fig 5).
Fig 5.
Barriers to working effectively with adolescents and young adults.
A large proportion of respondents (74%) reported that they had unmet training needs in adolescent and young adult health and transition. Training needs in specific areas of adolescent and young adult health training (Table 2) were highest in disease-specific issues relating to adolescence, followed by legislative issues and interpersonal skills.
Table 2.
Training needs in specific areas of adolescent and young adult health, rated from 1 (low) to 5 (high)
| Training need | Mean (SD) |
| Disease-specific issues relating to adolescents | 3.14 (1.2) |
| Legislative issues | 2.86 (1.3) |
| Interpersonal skills | 2.84 (1.2) |
| Resources available | 2.81 (1.3) |
| Psychosocial issues | 2.80 (1.3) |
| Adolescent mental health | 2.77 (1.3) |
| Transition and transfer issues | 2.76 (1.3) |
| Educational issues | 2.75 (1.2) |
| Interagency services | 2.72 (1.3) |
| Growth and puberty | 2.72 (1.2) |
| Sexual health | 2.70 (1.2) |
| Substance use | 2.61 (1.1) |
| Vocational issues | 2.54 (1.2) |
| Independent living | 2.49 (1.2) |
| Benefit entitlement | 2.47 (1.4) |
Free text responses demonstrate overall dissatisfaction with training in adolescent and young adult health, with a strong desire to experience more training in the area. A minority of trainees expressed that they did not feel any such training should be part of their curriculum or did not understand why it should have any added importance compared with current practice. A collection of those responses are displayed in Box 1.
Box 1.
How do trainees feel about training in adolescent and young adult health?
| We need more training in this area especially as adolescents have skin problems with possible long time psychological effects. Dermatology trainee |
| A massively important area that is overlooked in the curriculum. Having not had much formal training in paeds and no real experience of working with young adults, I would really appreciate further experience in interacting with this group and advice as to how to facilitate good care during this period. Genitourinary medicine trainee |
| Isolated pocket of inspiration from motivated consultant. Endocrinology and diabetes trainee |
| More training and exposure is urgently needed; from my experience the transition is very poorly managed and adolescents and young adults suffer as a consequence. Dermatology trainee |
| Very minimal exposure to adolescent and young adult health in my training. Endocrinology and diabetes trainee |
| All transitional care exposure is minimal and there is little in the way of specific training. Endocrinology and diabetes trainee |
| Clinics do exist but to date there is little trainee involvement. Infectious diseases trainee |
Discussion
This is the first survey to examine training experience in adolescent and young adult health for higher specialty trainees in adult medical specialties in the UK. It has demonstrated that the vast majority of trainees do not feel that they get adequate training in adolescent and young adult health, and feel under-prepared to deal with young people who either transition from children’s services or present for the first time to adult services. The results have demonstrated that increased clinical exposure, in the form of clinic attendance, is associated with increased training satisfaction in this area.
An identical survey, examining training in adolescent and young adult health across paediatric trainees and adult trainees in endocrinology and diabetes in the UK, revealed the problem is not isolated to those training in adult medicine, with both paediatric and adult trainees expressing a desire for more training to increase confidence and experience in dealing with young people.25 This emphasises that the issue spans paediatric and adult services,26 leaving adolescents and young adults not only in a healthcare gap but also a training gap. Studies in healthcare professionals providing care for young people undergoing transition in rheumatology and gastroenterology have also identified an unmet training need.17,22 And this is not isolated to the UK; a previous survey of paediatric societies throughout Europe has shown heterogeneity in the services and training offered.27
These survey results may be explained by the ongoing challenge of accessing adequate training alongside service provision, an issue highlighted by previous surveys of core medical trainees28 and higher specialty trainees.29 In addition, there are competing training needs; trainees are expected to acquire evidence through workplace-based assessments for numerous competencies and therefore the competencies that do reflect adolescent and young adult health, present in most curricula to a greater or lesser extent, may be neglected. Trainees may also only have access to supervisors who have similarly had minimal levels of training in this area.
The survey provides some suggestions as to how training could be improved, as increased clinical exposure through clinic attendance was associated positively with training experience, particularly in those trainees attending more than 10 clinics. However, access to dedicated clinics was clearly limited. Dedicated adolescent and young adult services will not be available in all specialties in all trusts; the finding that trainees in endocrinology and diabetes were more likely to attend 10 or more clinics focusing on the care of young people reflects the move nationally within diabetes towards this model of care to support transition.30 Even when dedicated services do exist, the challenge of providing continuity to facilitate the patient-doctor relationship may mean that trainees who may only be in that post transiently are discouraged from attending. Meeting the challenge of increasing experiential learning is paramount. Trainees need to recognise that each individual patient who is a young person either presenting to acute care or other outpatient settings provides an opportunity for training through detailed case-based discussions with supervisors with an understanding of the key issues. Rotations need to be planned so that all trainees get exposure to dedicated services, if possible.
Trainees rated their greatest training need (greater than 3) in disease-specific issues, demonstrating physicians are leaning towards focusing on the condition rather than the wider context of working with young people. This is in keeping with a survey of West Midland paediatric trainees who rated the overall importance, their knowledge, skill and confidence much higher for asthma than for substance use, and sexual and mental health.31 The other areas identified by trainees as having the highest training need were legislative issues, including safeguarding and interpersonal skills; this includes communication, which is critical to working effectively with young people.32 These areas lend themselves to more innovative training opportunities, including the use of video consulting to assist in feedback, as is done in general practice training, with a particular focus on lone consulting, confidentiality, psychosocial screening and challenging consultations.
Many issues relating to young people’s health are generic across specialties and, therefore, core competencies could be introduced into the higher specialty training curricula. This could be similar to those in the core medical training curriculum, to support the competencies reflecting more specialty-specific adolescent and young adult issues. This provides opportunity for efficiencies with core training being provided regionally. Palliative care have produced a useful document33 providing guidance for trainers and trainees on the competencies required for general physicians to support training in an area that all physicians come into contact with, but few have had dedicated training in. The Royal College of Paediatrics and Child Health has also developed a framework of competences in young people’s health for paediatric trainees,34 which could be accessed by trainees in adult specialties, as well as trainers, to help guide development of the necessary competencies. Signposting of available training resources is also key; for example, an e-learning programme in adolescent health has been available since 2008 (revised in 2015),35 yet only 7% of trainees had accessed this resource. Work has begun to link this to the training curricula.
As with any survey, there are identifiable limitations. We only captured responses from approximately 10% of higher specialty trainees, which may reflect the methods used in dissemination, and it is possible that not all trainees were exposed to the survey link. Despite this, the total number of respondents, at greater than 600, is a substantial number and is likely to reflect those with more interest in the area, so conclusions are likely to be accurate. This survey did not explore the specifics of access to training; it is anticipated that work will follow in each specialty to establish ways of plugging this training gap. However, the free text responses do shed some light on the available training and this certainly suggests that it is often limited.
Based on this survey, there is a need to enhance training in adolescent and young adult health. Work is ongoing nationally, including within the Royal College of Physicians, to raise awareness among physicians that young people are their responsibility. The recognition that young people have differing needs, which extend well into the third decade of life, strengthens the case for adult physicians being actively involved in any training initiative. Any initiative needs to be supported by the training hierarchy and by training the trainers. A focus on training in adolescent and young adult health provides opportunities for collaborative working between the Royal College of Physicians and the Royal College of Paediatrics and Child Health. Such an initiative would genuinely begin to close the ‘training gap’. With the Shape of Training review underway,36 the possibility of post-certificate of completion of training fellowship training or credentialing specifically in adolescent and young adult health may be possible although the details on this remain sketchy and funding opportunities are severely limited.
Conclusions
The importance of improving care for young people and, therefore, the training of future consultant physicians cannot be underestimated. In young people with long-term conditions, there is a risk that inadequate healthcare provision may precipitate disengagement, bringing with it increased morbidity with increased use of emergency and urgent care. Young people may not see their GP at all and the presentation of young people at an outpatient clinic or as an acute admission provides a unique opportunity to help promote good health in terms of their presenting condition, but also in terms of health promotion, specifically considering sexual health, smoking, alcohol and substance use, diet and exercise, and mental health, as well as addressing wider social, educational and vocational issues. While it is clear that trainees have a lot of competing demands on their time, the need to improve services for young people is recognised and this issue must be highlighted and addressed as a matter of urgency.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author contributions
All authors contributed to the study design, data collection and interpretation, and drafting and finalising of the manuscript.
References
- 1.Viner R. Life stage: adolescence. In: Davies SC. Annual report of the chief medical officer 2012. Our children deserve better: prevention pays. London: Department of Health, 2013. [Google Scholar]
- 2.Children and Young People’s Health Outcomes Forum Report of the Children and Young People’s Health Outcomes Forum. London: Department of Health, 2012. [Google Scholar]
- 3.Gleeson H, McCartney S, Lidstone V. ‘Everybody’s business’: Transition and the role of adult physicians. Clin Med 2012;12:561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Viner R. Transition from paediatric to adult care. Bridging the gaps or passing the buck? Arch Dis Child 1999;81:271–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maslow G, Haydon A, Ford C, et al. Young adult outcomes of children growing up with chronic illness: an analysis of the national longitudinal study of adolescent and young adult health. Arch Pediatr Adolesc Med 2011;165:256–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sawyer S, Drew S, Yeo MS, Britto MT. Adolescents with a chronic condition: challenges living, challenges treating. Lancet 2007;369:1481–9. [DOI] [PubMed] [Google Scholar]
- 7.Bleyer WA. Tejeda H, Murphy SB, et al. National cancer clinical trials: children have equal access; adolescents do not. Adolesc Health 1997;21:366–73. [DOI] [PubMed] [Google Scholar]
- 8.Bleyer WA. Cancer in older adolescents and young adults: epidemiology, diagnosis, treatment, survival and importance of clinical trials. Med Pediatr Oncol 2002;38:1–10. [DOI] [PubMed] [Google Scholar]
- 9.Hargreaves DS, Viner RM. Children’s and young people’s experience of the National Health Service in England: a review of national surveys 2001–2011. Arch Dis Child 2012;97:661–6. [DOI] [PubMed] [Google Scholar]
- 10.Department of Health You’re welcome – quality criteria for young people friendly health services. London: Department of Health, 2011. [Google Scholar]
- 11.Royal College of Paediatrics and Child Health Not Just a phase: a guide to the participation of children and young people in health services. London: RCPCH, 2010. [Google Scholar]
- 12.Royal College of Physicians of Edinburgh Transition Steering Group Think transition: developing the essential link between paediatric and adult care. Edinburgh: RCPE, 2008. [Google Scholar]
- 13.National Institute for Health and Care Excellence Transition from children’s to adults’ services for young people using health or social care services. NICE guideline No 43 London: NICE, 2016. [Google Scholar]
- 14.Lyons SK, Becker DJ, Helgeson VS. Transfer from pediatric to adult health care; effects on diabetes outcome. Pediatr Diabetes 2014;15:10–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andreoni KA, Forbes R, Andreoni RM, et al. Age-related kidney transplant outcomes: health disparities amplified in adolescence. JAMA Intern Med 2013;173:1524–32. [DOI] [PubMed] [Google Scholar]
- 16.Fernandes SM, O’Sullivan-Oliveira J, Landzberg MJ. Transition and transfer of adolescents and young adults with pediatric onset chronic disease: the patient and parent perspective. J Pediatr Rehabil Med 2014;7:43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sebastian S, Jenkins H, McCartney S, et al. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: differing perceptions from a survey of adult and paediatric gastroenterologists. J Crohns Colitis 2012;6:830–44. [DOI] [PubMed] [Google Scholar]
- 18.Scal P, Ireland M. Addressing transition to adult health care for adolescents with special health care needs. Pediatrics 2005;115:1607–12. [DOI] [PubMed] [Google Scholar]
- 19.Tylee A, Dagmar M, Graham T, et al. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet 2007;369:1565–73. [DOI] [PubMed] [Google Scholar]
- 20.Crowley R, Wolfe I, Lock K, Mckee M. Improving the transition between paediatric and adult healthcare: a systematic review. Arch Dis Child 2011;96:548–53. [DOI] [PubMed] [Google Scholar]
- 21.Ohn U, Offner G, Breuch K, Oldhafer M. Concept to improve adherence in adolescents following renal transplantation: vision or reality? Urologe A 2009;48:1468–72. [DOI] [PubMed] [Google Scholar]
- 22.McDonagh JE, Southwood TR, Shaw KL, British Paediatric Rheumatology Group Unmet education and training needs of rheumatology health professionals in adolescent and young adult health and transitional care. Rheumatology 2004;43:737–43. [DOI] [PubMed] [Google Scholar]
- 23.Viner R. Barriers and good practice in transition from pediatric to adult care. J R Soc Med 2001;94:2–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fox A. Physicians as barriers to successful transitional care. Int J Adolesc Med Health 2002;14:3–7. [DOI] [PubMed] [Google Scholar]
- 25.Wright R J, Chapman S, Cheer K, et al. Training needs in adolescent and young adult health and transition in UK paediatric and adult higher specialist trainees in endocrinology and diabetes. Br J Diabetes Vasc Dis 2015;15:159–65. [Google Scholar]
- 26.McDonagh JE, Minnaar G, Kelly K, O’Connor D, Shaw KL. Unmet education and training needs in adolescent and young adult health of health professionals in a UK children’s hospital. Acta Paediatr 2006;95:715–9. [DOI] [PubMed] [Google Scholar]
- 27.Ercan O, Alikasifoglu M, Erginoz E, et al. Demography of adolescent and young adult health care delivery and training in Europe. Eur J Pediatr 2009;168:417–26. [DOI] [PubMed] [Google Scholar]
- 28.Tasker F, Newbery N, Burr B, Goddard AF. Survey of core medical trainees in the United Kingdom 2013 – inconsistencies in training experience and competing with service demands. Clin Med 2014;14:149–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.General Medical Council National Training Surveys 2010 Key findings. London: GMC, 2010. [Google Scholar]
- 30.NHS England Medical Directorate Diabetes transition and young adult service specification and guidance document. Leeds: NHS England, 2016. [Google Scholar]
- 31.Dieppe C R, Kumar M, Crome I. Adolescent exploratory behavior – what do trainees know? J Adolesc Health 2008;43:520–2. [DOI] [PubMed] [Google Scholar]
- 32.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 33.Hicks P. Training in palliative and end-of-life care. Guidance for trainees (and their trainers) in non-palliative medicine training posts. London: JRCPTB, 2014. [Google Scholar]
- 34.Royal College of Paediatrics and Child Health A framework of competences for the special interest module in young people’s health. London: RCPCH, 2010. [Google Scholar]
- 35.e-Learning for Healthcare Adolescent Health Programme. www.e-lfh.org.uk/projects/adolescent-health/ [Accessed 1 February 2017].
- 36.Greenaway D. Securing the future of excellent patient care. London: Shape of Training, 2013. [Google Scholar]