Abstract
Background:
Alcohol-induced blackouts, a form of anterograde amnesia that restricts the encoding of short-term memories into long-term, are among the most severe alcohol-related consequences. College students are at high risk for experiencing alcohol-induced blackouts, and there is a need to determine whether alcohol interventions can effectively reduce blackouts in this population. The current study uses data from three randomized clinical trials (Murphy et al., 2012, 2010, 2018) to examine the effect of various intervention approaches on alcohol-induced blackouts.
Methods:
Four interventions were compared over three studies: 1) a computerized feedback intervention (e-Chug; Study 1), 2) a single-session brief motivational intervention (BMI; Study 1), 3) a BMI plus behavioral economic session focused on increasing substance-free activities (BMI+SFAS; Study 2 and 3), and 4) a BMI plus supplemental Relaxation Training session (BMI+Relaxation Training; Study 2 and 3). Studies 1 and 3 also included an Assessment only (AO) control condition. For each study, participants reported whether they had experienced an alcohol-induced blackout at each time point; binary logistic regressions examined differential likelihood of experiencing an alcohol-induced blackout over time.
Results:
Neither the single-session BMI or e-Chug reduced alcohol-induced blackouts over AO; however, participants in BMI+SFAS or BMI+Relaxation conditions were significantly less likely to experience an alcohol-induced blackout compared to AO at 1-month (Wald = 4.77, OR = .53, p = .03) and 6-month follow-ups (Wald = 5.72, OR = .52, p = .02). Study 2 also revealed a larger effect for the BMI+SFAS over the BMI+Relaxation condition at 6-months (Wald = 4.11 OR = .22, p = .043), although this was not replicated in Study 3. The effects for the two-session BMIs lasted 6-months, at which point maturation effect diminished differences between AO and intervention conditions.
Conclusions:
Two sessions of BMI are a substantial enough dose to result in reductions in alcohol-induced blackouts among college student heavy drinkers.
Keywords: Alcohol-induced blackouts, Brief motivational interventions, College students
Introduction
College students report high rates of episodic heavy drinking (4/5 drinks for women/men) and are at particularly high risk for experiencing alcohol-induced blackouts (White and Hingson, 2013). Estimates vary, but most studies suggest that approximately 50% of college students have experienced an alcohol-induced blackout at least once in their lives (Mundt and Zakletskaia, 2012; Schuckit et al., 2015). Although memory formation is impaired during a blackout, other functioning remains intact, and individuals can still ambulate, make decisions, and continue drinking while under significantly disinhibited regulatory capacity (Lee et al., 2009), and alcohol-induced blackouts are therefore linked to alcohol-related injury (Mundt et al., 2012; Mundt and Zakletskaia, 2012). Not surprisingly, experiencing a blackout is the most significant risk factor for most other alcohol-related consequences, including having a hangover, missing class or work, arguing with friends, and seeing a doctor because of an overdose after drinking (Hingson et al., 2016). Although long-term effects on brain functioning have not been adequately assessed, preliminary studies suggest that alcohol-induced blackouts are associated with altered frontal lobe neurochemistry, specifically in the anterior cingulate cortex (Silveri et al., 2014). These alterations are associated with worsening executive functioning deficits and are present among individuals in alcohol abusing populations, suggesting that high experience of alcohol-induced blackouts could serve as early markers of alcohol dependence (Meyerhoff and Durazzo, 2008), especially considering that they are strong predictors of future alcohol consumption (Read et al., 2013).
Given the gravity of alcohol-induced blackouts and the frequency of occurrence among adolescent and young adult populations (Schuckit et al., 2015; Wetherill and Fromme, 2016), there is a need to identify or create policy and interventions that can effectively reduce the occurrence of alcohol-induced blackouts among college students. The National Institute on Alcoholism and Alcohol Abuse’s (NIAAA) CollegeAIM matrix (2015), a document that summarizes the effectiveness and cost-utility of a wide range of potential interventions for college students, identifies brief motivational interventions (BMI) as mid-range in cost, but highly effective for reducing alcohol-related outcomes. BMIs often consist of one or two sessions (approximately 50 minutes each) delivered by a trained clinician (Carey, 2012; Neal and Carey, 2007) using a motivational interviewing style (Miller and Rollnick, 2012). These interventions are typically accompanied by alcohol education and personalized feedback (PF) that is derived from the student’s response to questionnaires. Personalized feedback can include information about the student’s drinking compared to college norms, their recent alcohol-related consequences (including blackouts if reported), and financial or health costs related to alcohol use (Miller et al., 2013). Although BMIs are considered among the most effective interventions for this age cohort, they require some financial commitment and level of expertise, and thus computerized interventions have been developed to deliver personalized feedback (e.g., e-Chug). These interventions generally have smaller effect sizes than in-person BMIs (Carey et al., 2009) but can theoretically reach more students, and thus may be an effective and economic alternative.
Recent meta-analyses and mega-analyses have questioned the efficacy of BMIs due to the typically small magnitude reductions in alcohol consumption and general alcohol-related consequences across most BMI studies (Huh et al., 2015; Mun et al., 2015; Tanner-Smith and Lipsey, 2015) and have spurred efforts to supplement BMIs with additional content (Murphy et al., 2012). However, it is important to keep in mind that BMIs are a harm reduction approach geared towards non-treatment seekers and thus have flexible goals based on the individual student’s motivation. Many students are not motivated to reduce their weekly drinking or to avoid relatively minor alcohol consequences (e.g., having an argument with a friend, regretted behavior) but may be motivated to reduce more severe problems (Merrill et al., 2019). Thus, there is a need to specifically examine the influence of BMI on key drinking consequences. Consistent with this hypothesis, one previous study determined that singe session BMIs were associated with significant reductions in drinking and driving, another severe consequence that is often more of a central focus of BMIs compared to other relatively benign alcohol consequences that are included in feedback-based interventions and contribute to alcohol problem total score outcomes (Teeters et al., 2015).
Only one study has specifically examined the efficacy of BMIs in reducing the likelihood of reducing alcohol-induced blackouts. With a sample of 188 freshmen college student drinkers, Kazemi and colleagues (2013) administered two 50-minute brief motivational intervention sessions incorporating elements of alcohol education and personalized feedback, one following a baseline assessment and one after two weeks. These two sessions were followed up by 50-minute booster sessions at 3-months and 6-month post-baseline. None of the sessions focused specifically on blackout drinking. Results indicated a decrease in blackout drinking from baseline (40% reported a blackout) to the 6-month follow-up (16% reported a blackout). Although these results are promising, the study lacked a control group, which limits interpretability about whether the change was due to the direct effects of the intervention or due to maturation. The intervention duration (four sessions over six months) also represents a significant burden for students and providers that may limit the disseminability of the intervention. There are a variety of intensities, or doses, within the general category of BMI that may be associated with differential effects.
Current Study
Alcohol-induced blackouts represent a serious public health concern for young adults both because of the direct neurocognitive effects of blacking out and because drinking to the point of blackout increases risk for a variety of other drinking consequences. Based on the heavy personal and societal toll of alcohol-induced blackouts, there is a need to appropriately examine the influence of brief interventions on alcohol-induced blackouts among heavy drinking college students. Thus, the current study uses data from three randomized clinical trials (Murphy et al., 2012, 2010, 2018) conducted over the course of a decade to examine whether receiving different brief interventions (i.e., computerized personalized feedback, single session BMI, or two session BMIs) are followed by reductions in the experience of alcohol-induced blackouts. Alcohol-induced blackouts were examined in each of these trials; however, each manuscript only reported reductions in combined, general alcohol-related problems or binge drinking rather than examining alcohol-induced blackouts individually. We hypothesized that all three intervention approaches would be associated with decreases in alcohol-induced blackouts. Further, we hypothesize that clinician administered interventions will demonstrate a stronger effect than the computerized feedback intervention, and that the two-session clinician-administered BMI conditions would perform better than the single-session BMI condition. Finally, we will examine naturalistic changes in alcohol-induced blackouts across time using assessment only groups.
Materials & Methods
Parent Study Descriptions
The current study is a secondary data analysis of three randomized clinical trials. All three studies recruited non-treatment seeking undergraduate students and compensated them with either course credit or cash for participating. See Table 1 for demographic information for each sample. Intervention conditions and their inclusion in each trial is described in Table 2. Information relevant for the CONSORT checklist for the initial studies can be referenced in the published outcome studies for each trial.
Table 1.
Demographic information for Study 1, 2, and 3.
| Demographics | Study 1: Murphy et al., (2010) (n = 133) |
Study 2: Murphy et al., (2012) (n = 82) |
Study 3: Murphy et al., (2018) (n = 393) |
|---|---|---|---|
| Age in years, M (SD) | 18.57 (1.21) | 18.51 (.71) | 18.77 (1.07) |
| Race (% White) | 85 (63.9%) | 66 (80.5%) | 310 (78.9%) |
| Gender (% female) | 66 (49.6%) | 41 (50%) | 239 (60.8%) |
| Year in School | |||
| Freshman | 130 (97.7%) | 82 (100%) | 244 (62.1%) |
| Sophomore | 3 (2.3%) | - | 149 (37.9%) |
| Junior | - | - | - |
| Senior | - | - | - |
| Typical drinks per week, M (SD) | 16.19 (15.19) | 16.87 (11.55) | 17.03 (13.79) |
| Past month binge drinking, M (SD) | 5.65 (4.86) | 6.02 (4.33) | 6.19 (4.12) |
Note.
Table 2.
Elements found in each intervention condition for all studies.
| Study Conditions | Study 1 | Study 2 | Study 3 | |
|---|---|---|---|---|
|
BMI – 50-minutes Discussion of participant’s autonomy Alcohol decisional balance Alcohol PF Perceived v. actual drinking norms Discussion of student’s peak BAC Personalized list of alcohol problems Money spent on alcohol Calories consumed through drinking Goal Setting Review of Protective Strategies |
- | ✓ | ||
|
Substance-free Activity Session (SFAS) – 50-minutes Discussion of academic and career goals Academic/Career-focused Information College graduation rates Income by degree type and GPA GPA by time drinking v. in class Academic/Career-focused PF Requirements for chosen major/career Career-specific list of activities ime allocation Coping strategies List of Hobbies and Leisure Activities |
✓ | ✓ | ||
|
Relaxation Training Supplement – 30 minutes Diaphragmatic breathing exercise Progressive muscle relaxation Discussion of reaction |
✓ | ✓ | ||
|
e-Chug Brief drinking assessment Alcohol PF Quantity and frequency of drinking Comparison of drinking with actual norms Peak BAC; Tolerance Alcohol-related consequences Money spent on alcohol Calories consumed from alcohol Family risk score |
✓ | |||
|
Assessment Only Completed assessment measures at baseline and follow-ups |
✓ | ✓ | ||
Five intervention conditions were examined: 1) A single session brief motivational intervention (BMI; Study 1); 2) a computerized feedback intervention (e-Chug; Study 1); 3) a BMI plus supplemental session focused on increasing substance-free activities (BMI+SFAS; Study 2 and 3); 4) a BMI plus supplemental Relaxation Training session (BMI+Relaxation Training; Study 2 and 3); and 5) Assessment only (AO) control condition (Study 1 and 3).
BAC = Blood Alcohol Content; GPA = Grade Point Average; PF = Personalized Feedback.
Study 1 (Murphy et al., 2010).
Study 1 was a single site randomized clinical trial. Participants who reported at least one heavy drinking episode in the past month were randomized into one of three groups: A single-session BMI (n = 46), e-chug computerized personalized feedback (n = 45), or assessment only (n = 42). Participants in the two treatment groups completed the intervention (in a psychology laboratory setting) immediately following the baseline assessment and completed follow-ups at 1-, 6-, and 12-months. Groups did not differ on typical drinks per week, or heavy drinking episodes at baseline. There was no differential attrition by condition. Participants in the two treatments groups demonstrated medium effect size reductions in heavy drinking episodes and typical weekly drinking at 1-month follow-up, while the assessment only group showed no change.
Study 2 (Murphy et al., 2012).
Study 2 was a single site randomized clinical trial (NCT02837315). Participants were considered eligible if they reported at least two heavy drinking episodes in the past month. Eligible participants were assigned to either BMI + SFAS (Substance-free Activity Session, see below for details; n = 41) or BMI + Relaxation (n = 41). Participants in both groups completed the BMI with a clinician in the lab immediately following the baseline assessment and returned one-week later to complete the other intervention component (SFAS or relaxation training). Groups did not differ on any of the drinking related measures at baseline. There was no differential attrition by condition. Participants completed follow-ups at 1- and 6-months post intervention. Participants who received the BMI + SFAS demonstrated greater reductions in heavy drinking episodes and alcohol-related problems than BMI + Relaxation participants at 1- and 6-months.
Study 3 (Murphy et al., 2018).
Study 3 was a multisite, randomized clinical trial (NCT02834949). Procedures for this study were identical to those used in Murphy and colleagues (2012), other than the fact that this study included an assessment-only control group and a greater number of follow-up assessments. Participants with at least two past-month heavy drinking episodes were assigned to BMI + SFAS (n = 130), BMI + Relaxation (n = 125), or assessment only (n = 138) and completed assessments at baseline (prior to intervention), 1-month, 6-months, 12-months, and 16-months. Groups did not differ on any of the drinking related measures at baseline. There was no differential attrition by condition. Compared to the assessment only condition, participants in either the BMI + SFAS or BMI + Relaxation conditions reported significant reductions in alcohol use and problems across all follow-ups.
Measures
Alcohol-induced blackouts were assessed across all three studies using 3-items from the Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Merrill, Kahler, & Strong, 2006). Participants were asked to endorse or deny experiencing various alcohol-related problems over the past month. Three items taken from the pre-existing Blackout subscale of the YAACQ (e.g., “I’ve not been able to remember large stretches of time while drinking heavily”; “I have awakened the day after drinking and found that I could not remember a part of the evening before”; “I have had a blackout after drinking heavily (i.e., could not remember hours at a time)”) were combined and coded dichotomously (y/n).
Interventions
Assessment Only.
Elements included in each intervention condition can be found in Table 2. An assessment only condition was included in Studies 1 and 3. In this condition, participants only completed the baseline and follow-up surveys.
e-CHUG.
The e-Chug condition was an intervention condition in study 1. Participants in the e-CHUG condition participated in an interactive web-based program that presented them with personalized feedback after completing a brief drinking assessment. Participants were presented with the same six feedback components as the BMI with the addition of a family risk score based on familial history of problematic alcohol and drug use. No content, education, or feedback was provided specific to engagement in alcohol-induced blackouts. After interacting with the material for approximately 30-minutes, participants completed a brief comprehension check (Murphy et al., 2010).
Brief Motivational Intervention (BMI).
The BMI session was included in Studies 1, 2, and 3. The BMI was presented in an MI style (Miller and Rollnick, 2012) and was essentially identical across studies. Components included: a) A discussion about confidentiality and student autonomy; b) an alcohol use decisional balance exercise; c) a personalized feedback related to alcohol use; and d) summary and goal setting exercise. The personalized feedback included six elements: 1) a comparison of perceived v. actual college student drinking norms; 2) a comparison of students actual drinking v. national gender-specific norms; 3) a discussion about blood alcohol content, including personalized feedback about estimated BAC for the participant during their highest reported drinking night; 4) personalized list of alcohol-related problems endorsed by the participant (including the blackout items if endorsed); 5) money spent on alcohol and cost of DUI; 6) calories from alcohol. The goal setting activity was only initialized if participants expressed interest. The BMI condition contained the same elements across all three studies. However, in studies 2 and 3 the BMI was followed by one of two supplemental sessions.
Relaxation Training.
The Relaxation Training condition was a supplemental intervention condition in Studies 2 and 3. One week following the BMI, participants in this condition completed a 30-minute relaxation training session that was intended to instruct relaxation and stress reduction strategies (i.e. diaphragmatic breathing, and progressive muscle relaxation). Relaxation training was selected as an active control condition because it is a common wellness strategy and has previously been used as an alcohol treatment element (Klajner et al., 1984; Murphy et al., 2012). Due to the high levels of stress and anxiety present among college populations that is often associated with drinking severity (American College Health Association, 2015), relaxation training may be a beneficial supplement to BMI content.
Substance-free Activity Session (SFAS).
The SFAS was a supplemental intervention condition in Study 2 and 3. One week following the BMI, participants in the SFAS condition completed a 1-hour behavioral economic session that was intended to increase future orientation and substance-free activity engagement. The overarching goals of the SFAS are to increase engagement in enjoyable and meaningful alternatives to drinking, identify short-term, intermediate, and long-term goals, increase the extent to which behavior is motivated by long-term goals, explore how drinking interferes with goal achievement, and provide practical advice related to college adjustment, all while maintaining a motivational interviewing style. Feedback elements included: 1) income differences for college v. high school graduates; 2) income differences by GPA; 3) personalized information about career requirements for a previously specified occupational field; 4) personalized career-related activities relevant to successful completion of these goals; 5) personalized feedback about how the participant spends their time; 6) a discussion about personalized substance-free recreational activity options available throughout the community based on previously described interests; and 7) a goal setting activity. More detail can be found in Murphy et al., (2018). For all studies, BMI and SFAS conditions were coded for fidelity (Murphy et al., 2012, 2010).
Data Analysis
All variables containing outliers were winsorized per recommendations of Tabachnick and Fidell (2013). Chi-squared tests were conducted to evaluate differential attrition by baseline alcohol-induced blackouts for all three studies at each follow-up. Logistic regression analyses were conducted separately for each study to determine whether alcohol-induced blackouts were significantly less likely between groups at each follow-up. The dependent variable was report of an alcohol-induced blackout (no/yes). Each regression controlled for gender baseline alcohol-induced blackouts, baseline typical drinks per week, and drinks per week for the timepoint contemporaneous with the outcome timepoint of the regression (i.e., change in typical drinks per week). For all regressions that are significant, reductions in alcohol-induced blackouts for each time point compared to the baseline assessment will be reported.
Results
Study 1 (Murphy et al., 2010)
For all three studies, descriptive data of occurrence of alcohol-induced blackouts over time in each condition can be found in Table 3. Endorsement of baseline alcohol-induced blackouts was not associated with differential attrition at 1-month (χ2 = .10, p = .76), 6-month (χ2 = .09, p = .76), or 12-month (χ2 = .09, p = .77) follow-ups. There were no significant differences between an active intervention condition and the assessment only group in the likelihood of experiencing an alcohol-induced blackout at 1-month (Wald = 1.68 OR = .50, p = .20), 6-month (Wald = .70 OR = .63, p = .40), or 12-month (Wald = .23 OR = 1.30, p = .63) follow-ups. Similarly, there were no significant differences between the BMI or e-Chug and assessment only conditions at any time point.
Table 3.
Percentage of participants experiencing alcohol-induced blackouts for each study by condition at each time point.
| Study 1 | |||||
|---|---|---|---|---|---|
| Alcohol Consumption | Blackouts | ||||
| Mean (SD) | % | ||||
| Baseline | Baseline | 1-month | 6-month | 12-month | |
| Full Sample | 16.19 (15.19) | 58.6 | 46.6 | 44.5 | 46.9 |
| Assessment Only | 14.90 (10.80) | 54.8 | 38.5 | 38.5 | 44.1 |
| e-Chug | 17.48 (15.32) | 60.0 | 55.3 | 42.9 | 53.1 |
| BMI | 16.10 (18.38) | 60.9 | 46.3 | 52.8 | 43.8 |
| Study 2 | ||||
|---|---|---|---|---|
| Alcohol Consumption | Blackouts | |||
| Mean (SD) | % | |||
| Baseline | Baseline | 1-month | 6-month | |
| Full Sample | 16.87 (11.55) | 68.3 | 40.3 | 37.3 |
| BMI + Relaxation | 17.68 (11.89) | 73.2 | 53.8 | 53.3 |
| BMI + SFAS | 16.06 (11.29) | 63.4 | 26.3a | 24.3 |
| Study 3 | ||||||
|---|---|---|---|---|---|---|
| Alcohol Consumption | Blackouts | |||||
| Mean (SD) | % | |||||
| Baseline | Baseline | 1-month | 6-months | 12-months | 16-months | |
| Full Sample | 16.76 (11.98) | 61.8 | 40.3 | 36.5 | 36.1 | 38.7 |
| Assessment Only | 17.63 (12.55) | 63.8 | 55.9 | 49.6 | 44.8 | 44.7 |
| BMI + Relaxation | 14.14 (8.89) | 60.8 | 26.5c | 31.5c | 26.8c | 34.0 |
| BMI + SFAS | 18.35 (13.51) | 60.8 | 37.2b | 27.0b | 36.3b | 37.6 |
SD = Standard Deviation.
Significant difference between BMI+SFAS and BMI+Relaxation;
Significant difference between BMI+SFAS and Assessment only;
Significant difference between BMI+Relaxation and Assessment only.
Study 2 (Murphy et al., 2012)
Endorsement of baseline alcohol-induced blackouts was not associated with differential attrition by condition at 1-month (χ2 = 3.00, p = .39) or 6-month (χ2 = 1.93, p = .59) follow-ups. There was a nonsignificant trend-level effect of intervention on likelihood of experiencing an alcohol-induced blackout at 1-month follow-up (Wald = 3.49, OR = .29, p = .06) and a significant effect at the 6-month follow-ups (Wald = 4.11 OR = .22, p = .043), suggesting that those in the BMI+SFAS condition were less likely to report experiencing an alcohol-induced blackout than those in BMI + Relaxation condition. In the BMI+SFAS condition, 26 participants reported an alcohol-induced blackout at baseline compared with 10 and 9 at 1- and 6-month follow-ups (61.5% and 65.3% reduction, respectively). In the BMI+Relaxation condition, 30 participants reported an alcohol-induced blackout at baseline compared with 21 and 16 at 1- and 6-month follow-ups (30.0% and 46.6% reduction, respectively).
Study 3 (Murphy et al., 2018)
Endorsement of baseline alcohol-induced blackouts was not associated with differential attrition at 1-month (χ2 = 1.18, p = .28), 6-month (χ2 = .58, p = .45), 12-month (χ2 = .07, p = .80), or 16-month (χ2 = .18, p = .67) follow-ups. At the 1-month (Wald = 4.77, OR = .53, p = .03) and 6-month follow-ups (Wald = 5.72, OR = .52, p = .02), those in either BMI condition (BMI+SFAS or BMI+Relaxation) were significantly less likely to report an alcohol-induced blackout compared to the assessment only control. When examining effects separated by BMI conditions, the BMI+SFAS condition remained the same; the BMI+Relaxation condition, however, was only significant at 1-month follow-up. There was no treatment effect at 12-month (Wald = 1.24, OR = 1.72, p = .27) or 16-months follow-ups (Wald = .001, OR = 1.01, p = .97). There were no significant differences between the SFAS and the Relaxation groups at any time point. For any participant in a BMI condition, 155 participants reported an alcohol induced blackout at baseline, compared with 76 at 1-month (50.1% reduction), 64 at 6-months (58.7% reduction), 71 at 12-months (54.1% reduction), and 74 at 16-months (52.2% reduction). In the assessment only condition, 88 participants reported an alcohol induced blackout compared with 71 at 1-month (19.3% reduction), 61 at 6-months (30.7% reduction), 52 at 12-months (40.1% reduction), and 46 at 16-months (47.7% reduction).
Discussion
Although the efficacy of BMIs in reducing general alcohol problems is well established, only one study has examined the effect of BMIs on the likelihood of experiencing alcohol-induced blackouts over time (Kazemi et al., 2013). The present study replicates and extends this area of research using data from three randomized clinical trials. The findings from study 1 indicated that there were no significant differences between the assessment only, single-session BMI, or e-Chug conditions in reducing the likelihood of experiencing an alcohol induced blackout. Study 2 compared two supplemental sessions to BMIs to examine whether increasing the dose could increase the efficacy of the BMI intervention for reducing alcohol-induced blackouts. Study 2 revealed that participants in the BMI + SFAS condition were significantly less likely to report an alcohol-induced blackout at both time points compared to those in the BMI + Relaxation group. Study 3 compared these two groups with an assessment only condition in a larger, multi-site sample of heavy drinking college students and found that participants receiving any two-session BMI were significantly less likely to experience an alcohol-induced blackout at 1-month and 6-month follow-up compared to the assessment-only control.
In the previous study examining the influence of BMI sessions on reducing alcohol-induced blackouts among heavy drinking college students (Kazemi et al., 2013), all participants engaged in four, one-hour sessions over the course of 6-months, and the results suggest that participants reduced alcohol-induced blackouts, albeit, without a comparison group. Our results extend this finding by comparing the effect of the BMI with a control group over a longer follow-up period. Our results suggest that two sessions may be adequate to observe significant short-term reductions in the likelihood of alcohol-induced blackouts. The sample generally demonstrated maturation effects, as all conditions experienced reductions over time. Given the dose effect found in the current study, we suspect that the Kazemi et al. (2013) findings are also the result of increased BMI dose, although the effect cannot be parsed apart from maturation effects.
Our results are also consistent with previous research demonstrating the influence of BMIs on alcohol consumption and alcohol-related problems more generally (Murphy et al., 2012; Murphy and Dennhardt, 2016; Tanner-Smith and Lipsey, 2015). The results lasted approximately 6-months, which is a shorter time frame than for reductions in effect sizes for reductions in general problems after a BMI (Tanner-Smith and Lipsey, 2015). These results accounted for changes in drinking over time, suggesting that the reductions in alcohol-induced blackouts occurred over and above any decrease in drinking accounted for by the intervention. Instead of reducing consumption levels, the effect of the two-session BMI interventions might be through shifting patterns in drinking that result in lower overall BAC values, resulting in fewer blackouts (e.g., drinking the same amount over an extended period of time, avoiding shots or hard alcohol). Thus, although previous work has demonstrated that single-session BMIs reduce alcohol consumption and problems, our results suggest more intensive approaches may be needed to reduce blackouts. It is important to note, however, that the single-session BMI in Study 1 was associated with changes in alcohol consumption but not in general alcohol problems (secondary data analysis). Other research suggests that another risky behavior, driving after drinking, is reduced following single-session brief interventions (Teeters et al., 2015), and has more recently been shown to reduce following a text message intervention (Teeters et al., 2018). Perhaps driving after drinking is conceptualized as a riskier behavior within the student’s mental framework before the BMI begins, which leads to a greater likelihood of decreases in this behavior post-intervention. Reductions in driving after drinking may also be achieved without changing drinking behavior, whereas reductions in alcohol-induced blackouts require some change in drinking.
Considering the high prevalence rate of alcohol-induced blackouts (62% in our sample), the profound implications associated with this phenomenon, and the cost efficiency of BMIs, these results are promising and suggest that brief contact (no more than 2 hours) can drastically decrease the occurrence of alcohol-induced blackouts among heavy drinking college students until at least 6-months, at which point maturation effect reduces the difference between the BMI and control conditions. Even so, the BMI interventions accelerate the natural downward-sloping trajectory of maturation, which may lead to enhanced gains in alcohol-free areas (e.g., school) and reductions in other alcohol-related problems, highlighting the need for more intervention to increase the duration of the effects. Previous research suggests that individuals who experience blackouts may show greater overall response to BMIs (Miller et al., 2018a, 2018b), which suggest that there may be utility in specifically identifying students for BMIs on the basis of a recent blackout experience.
Strengths, Limitations, and Future Directions
The current study has several notable strengths. We used three samples of heavy drinking college students, representative of the college population that often engages in high levels of alcohol consumption that result in alcohol-induced blackouts. We also examined several different interventions (computer-delivered, BMI, BMI+SFAS, BMI+Relaxation training) over the course of multiple studies that enhances our confidence in the current findings. The final study included a large sample and examined outcomes out to 16 months.
Despite these strengths, several limitations should be noted. First, we used an aggregate and retrospective measure of blackout drinking from the YAACQ. Although the YAACQ produces reliable and valid indices of alcohol problems (Read et al., 2006), blackout drinking represents periods of short-term memory loss, which may or may not be accurately recalled by heavy drinking college students. Second, our samples were restricted to heavy drinking college students, which may not generalize to other populations. Despite this, we suggest that this high-risk sample is necessary to study the phenomenology of this high-risk phenomena. Third, our study did not differentiate between blackout (en bloc) and brownout (fragmentary) drinking, which are conceptually different and demonstrate differences within the literature (Miller et al., 2018c). We used the higher threshold en bloc definition of blackouts which likely missed many fragmentary (brownout) episodes and resulted in an underestimation of the number of individuals who are blacking out. Future studies should explore the effects of BMIs on fragmentary blackouts, which are considered less serious but occur more frequently and still result in higher levels of problems. Finally, different aspects of study design (i.e., small sample size and lack of control group) for studies 1 and 2 leave some room for error in findings and suggest that future research should examine these separate interventions with larger sample sizes and adequate controls. A study examining one session interventions for alcohol-induced blackouts among college students with more power may find differential results, although the results from the current study suggest the effects are still negligible. The third study did address some of these issues.
Despite these limitations, these results have clear clinical implications and extend BMI and alcohol-induced blackout literatures. The results suggest that two-session BMIs are associated with substantial reductions in the report of alcohol-induced blackouts. BMIs are typically one session long. Although they consistently result in decreases in problematic alcohol use, a greater dose may be necessary to address alcohol-induced blackouts. Based on the outcome of Study 3, an increased time spent with a counselor focused on alcohol use generally may impact patterns of consumption just enough to reduce blackout rates overall. Further, the BMI+SFAS condition outperformed the BMI+Relxation Training condition in study 2, and lasted longer in study 3, although the study 2 differences were not replicated. The content of the BMI+SFAS, focused on increasing substance-free reward and enhancing consideration of the future, may work additively with increased counselor dose to account for the duration of the effect. The studies also had notable differences in sample characteristics, including different gender and college class differences. Given the lack of specific alcohol-induced blackouts content in these interventions, the dose may also be effectively increased through a single session focused specifically on reducing alcohol-induced blackouts, rather than general sessions with feedback elements relevant to different aspects of drinking. Considering that alcohol-induced blackouts are highly predictive of all other consequences (Hingson et al., 2016), an intervention focused on decreasing alcohol-induced blackouts may reduce all other consequences as well and result in significant reductions in the public health burden overtime. The relation between alcohol-induced blackouts and other consequences has not been established as causal, however, and alcohol-induced blackouts may serve as a marker of heavy drinking rather than a cause of alcohol-related problems.
These findings also highlight that alcohol-induced blackout drinking may be more difficult to reduce than other outcomes. Interestingly, recent research demonstrates that reporting an alcohol-induced blackout at baseline results in better treatment response (Miller et al., 2018a, 2018b). Theoretically, these individuals are drinking at a high level and thus have a higher potential for reduction. However, these studies did not report on those who continue to experience alcohol-induced blackouts at follow-ups, nor the effect on future blackout drinking. A subset of these individuals that are resistant to change, and thus continue to drink to blackout, could account for a significant proportion of null effects among this population. An important research priority should include the identification of predictors of stable blackout drinking over time. Some research suggests that those who experience a blackout may be more susceptible to future blackouts, partly because of inhibitory processing difficulties. These individuals may be the ones resistant to change. Identifying and targeting variables like this could potentially increase the overall efficacy of BMIs, particularly in light of our findings.
Supplementary Material
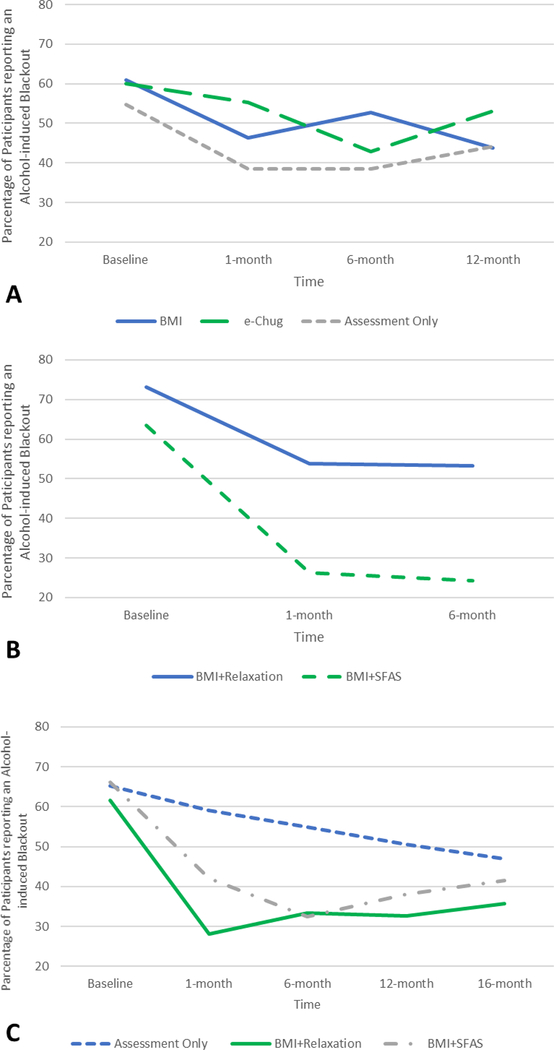
Figure 1.
Percentage of participants reporting alcohol-induced blackouts at each time point in A) Study 1 (Murphy et al., 2010); B) Study 2 (Murphy et al., 2012); and C) Study 3 (Murphy et al., 2019). In Study 1, there were no significant differences between any condition. In Study 2, the BMI+SFAS condition resulted in significantly less likelihood of an alcohol-induced blackout at 1-month, but not 6-month, compared to the BMI+Relaxation condition. In Study 3, both BMI conditions were associated with a decreased likelihood of experiencing an alcohol-induced blackout out to 12-months compared to the assessment only condition. BMI = brief motivational intervention.
Acknowledgments
This work was supported by research grants from the Alcohol Research Foundation (ABMRF; JGM), and the National Institutes of Health (R21 AA016304, JGM; R01 AA020829, JGM). The funding source had no role other than financial support. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Alcohol Abuse and Alcoholism or the National Institutes of Health.
References
- American College Health Association (2015) American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015. Hanover, MD: American College Health Association; 2015. [Google Scholar]
- Carey KB (2012) Brief Motivational Interventions In: College Student Alcohol Abuse: A Guide to Assessment, Intervention, and Prevention (Correia CJ, Murphy JG, Barnett NP eds), pp 218–245. Hoboken, New Jersey, John Wiley & Sons, Ltd. [Google Scholar]
- Carey KB, Scott-Sheldon LAJ, Elliott JC, Bolles JR, Carey MP (2009) Computer-delivered interventions to reduce college student drinking: A meta-analysis. Addiction 104:1807–1819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, Simons-Morton B, White AM (2016) Alcohol-Induced Blackouts as Predictors of Other Drinking Related Harms Among Emerging Young Adults. Alcohol Clin Exp Res 40:776–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh D, Mun E-Y, Larimer ME, White HR, Ray AE, Rhew IC, Kim S-Y, Jiao Y, Atkins DC (2015) Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcohol Clin Exp Res 39:919–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi DM, Levine MJ, Dmochowski J, Nies MA, Sun L (2013) Effects of motivational interviewing intervention on blackouts among college freshmen. J Nurs Scholarsh 45:221–229. [DOI] [PubMed] [Google Scholar]
- Klajner F, Hartman LM, Sobell MB (1984) Treatment of substance abuse by relaxation training: A review of its rationale, efficacy and mechanisms. Addict Behav 9:41–55. [DOI] [PubMed] [Google Scholar]
- Lee H, Roh S, Kim DJ (2009) Alcohol-induced blackout. Int J Environ Res Public Health 6:2783–2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Carey KB, Miller MB, Dibello AM (2019) How do college students subjectively evaluate “blackouts”? Addict Behav 89:65–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyerhoff DJ, Durazzo TC (2008) Proton magnetic resonance spectroscopy in alcohol use disorders: A potential new endophenotype? Alcohol Clin Exp Res 32:1146–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, DiBello AM, Carey KB, Pedersen ER (2018a) Blackouts as a Moderator of Young Adult Veteran Response to Personalized Normative Feedback for Heavy Drinking. Alcohol Clin Exp Res 42:1145–1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, DiBello AM, Meier E, Leavens ELS, Merrill JE, Carey KB, Leffingwell TR (2018b) Alcohol-Induced Amnesia and Personalized Drinking Feedback: Blackouts Predict Intervention Response. Behav Ther 50:25–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Leffingwell TR, Claborn K, Meier E, Walters S, Neighbors C (2013) Personalized feedback interventions for college alcohol use: An update of Walters & Neighbors (2005). Psychol Addict Behav 27:909–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MB, Merrill JE, DiBello AM, Carey KB (2018c) Distinctions in Alcohol-Induced Memory Impairment: AMixed Methods Study of En Bloc Versus Fragmentary Blackouts. Alcohol Clin Exp Res 42:2000–2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Rollnick S (2012) Motivational Interviewing: Helping People Change. New York, NY, Guilford Press. [Google Scholar]
- Mun E-Y, de la Torre J, Atkins DC, White HR, Ray AE, Kim S-Y, Jiao Y, Clarke N, Huo Y, Larimer ME, Huh D (2015) Project INTEGRATE: An integrative study of brief alcohol interventions for college students. Psychol Addict Behav 29:34–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt MP, Zakletskaia LI (2012) Prevention for college students who suffer alcohol-induced blackouts could deter high-cost emergency department visits. Health Aff 31:863–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt MP, Zakletskaia LI, Brown DD, Fleming MF (2012) Alcohol-induced memory blackouts as an indicator of injury risk among college drinkers. Inj Prev 18:44–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA (2016) The behavioral economics of young adult substance abuse. Prev Med (Baltim) 92:24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari BE, Barnett NP, Colby SM, Martens MP (2012) A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. J Consult Clin Psychol 80:876–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Martens MP, McDevitt-Murphy ME (2010) Computerized versus motivational interviewing alcohol interventions: impact on discrepancy, motivation, and drinking. Psychol Addict Behav 24:628–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neal DJ, Carey KB (2007) Association Between Alcohol Intoxication and Alcohol-Related Problems: An Event-level Analysis. Psychol Addict Behav 6:790–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, Colder CR (2006) Development and preliminary validation of the young adult alcohol consequences questionnaire. J Stud Alcohol 67:169–177. [DOI] [PubMed] [Google Scholar]
- Read JP, Wardell JD, Bachrach RL (2013) Drinking consequence types in the first college semester differentially predict drinking the following year. Addict Behav 38:1464–1471. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Heron J, Hickman M, Macleod J, Munafò MR, Kendler KS, Dick DM, Davey-Smith G (2015) Latent Trajectory Classes for Alcohol-Related Blackouts from Age 15 to 19 in ALSPAC. Alcohol Clin Exp Res 39:108–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silveri MM, Cohen-Gilbert J, Crowley DJ, Rosso IM, Jensen JE, Sneider JT (2014) Altered Anterior Cingulate Neurochemistry in Emerging Adult Binge Drinkers with a History of Alcohol-Induced Blackouts. Alcohol Clin Exp Res 38:969–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS (2013) Using multivariate statistics, 6th ed Boston, MA, Pearson. [Google Scholar]
- Tanner-Smith EE, Lipsey MW (2015) Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. J Subst Abuse Treat 51:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, Borsari B, Martens MP, Murphy JG (2015) Brief Motivational Interventions Are Associated With Reductions in Alcohol-Impaired Driving Among College Drinkers. J Stud Alcohol Drugs 76:700–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, Soltis KE, Murphy JG (2018) A mobile phone-based brief intervention with personalized feedback and text messaging is associated with reductions in driving after drinking among college drinkers. J Stud Alcohol Drugs 710–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The National Institute on Alcoholism and Alcohol Abuse’s (NIAAA) CollegeAIM matrix (2015). Available at: https://www.collegedrinkingprevention.gov/CollegeAIM/Resources/NIAAA_College_Matrix_Booklet.pdf
- Wetherill RR, Fromme K (2016) Alcohol-Induced Blackouts : A Review of Recent Clinical Research with Practical Implications and Recommendations for Future Studies 40:922–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, Hingson RW (2013) The burden of alcohol use: Excessive alcohol consumption and related consequences among college students. Alcohol Res Curr Rev 35:201–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.