Abstract
Introduction
Adherence to a gluten-free (GF) diet is the mainstay of therapy for celiac disease (CD). Until now, those wishing to avoid gluten in restaurants had to rely on menu labels, word of mouth, intuition, and restaurant workers’ advice, with a relative dearth of supporting data. We used crowd-sourced data from users of a portable gluten detection device to estimate rates of, and identify risk factors for, gluten contamination of supposed GF restaurant foods.
Methods
We analyzed data from a portable gluten detection device (Nima), collected across the United States during an 18-month period by users who opted to share results of their point-of-care tests. Data was sorted by region, time of day, median household income in the restaurant’s vicinity, restaurant genre, and food item. We used chi-squared test for bivariate analysis and multiple logistic regression for multivariate analysis to identify predictors of gluten detection in restaurant food.
Results
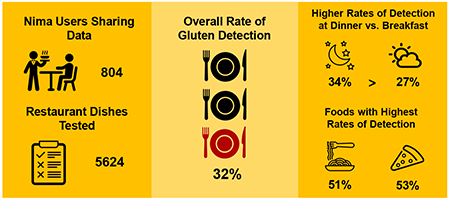
There were 5624 tests, performed by 804 users, in the examined period. Gluten was detected in 32% of GF labeled foods. Rates of gluten detection differed by meal, with 27.2% at breakfast and 34.0% at dinner (p=0.0008). GF labeled pizza and pasta were most likely to test positive for gluten, with gluten detected in 53.2% of pizza and 50.8% of pasta samples. On multivariate analysis, GF labeled food was less likely to test positive for gluten in the West than in the Northeast United States (OR 0.80; 95% CI 0.67-0.95).
Conclusions
This study of crowd-sourced data suggests that a substantial fraction of GF labeled restaurant foods contain detectable gluten. Although the highly sensitive Nima device may detect gluten at levels < 20 parts per million (ppm), leading to gluten exposure of unknown clinical significance, our findings raise potential concern. Additionally, our findings of higher rates of gluten detection in pizza and pasta provide practical data when providing dining strategies for patients with CD.
Graphical Abstract
INTRODUCTION
Celiac disease (CD) is an autoimmune disorder triggered by the consumption of gluten, a protein found in cereal grains wheat, rye, and barley. CD currently affects approximately 1% of the population (1, 2), and its prevalence is increasing (3). The disease primarily affects the small intestine, and common symptoms include iron deficiency, bloating, constipation, chronic fatigue, and abdominal pain (4).
Adherence to a gluten-free (GF) diet is the mainstay of therapy for CD. Despite its effectiveness, as many as 80% of CD patients report difficulty maintaining this lifestyle (5). Indeed, inadvertent gluten ingestion has been cited as the leading cause of nonresponsive CD (6, 7), and a recent study measuring traces of gluten in urine and stool suggested that many CD patients accidentally consume enough gluten to trigger symptoms and cause intestinal damage (8).
In order to protect CD patients from unintentionally ingesting gluten, the FDA issued a rule in August 2013 that packaged foods labeled GF must contain less than 20 ppm of gluten. No similar rule applies to restaurant foods claiming to be GF and, consequently, potential gluten exposure when dining out is a source of anxiety for many CD patients. In one study, 83% of patients with CD or non-celiac gluten sensitivity found the GF diet to be a problem in restaurants and 63% avoided restaurants altogether (9). Multiple surveys of CD patients found dining out to be the most common lifestyle situation presenting difficulty when following a GF diet, more so than traveling, socializing, and personal relationships (5, 10).
In the present study, we aimed to quantify rates of gluten contamination of restaurant foods and identify risk factors associated with the presence of gluten. The recent advent of a portable gluten detection device allowed us to use crowd-sourced data to estimate the prevalence of gluten contamination in restaurants throughout the United States.
METHODS
Gluten Sensor
We obtained uploaded data from users of Nima, a commercially available gluten detection device. Nima consists of a 3-inch-tall sensor and single-use capsules that contain test strips loaded with proprietary anti-gluten antibodies. To test food for the presence of gluten, users place a pea-sized sample into the capsule. Screwing on the lid grinds the sample, which is then mixed with an extraction buffer. The resulting solution passes onto the test strip, which is then read by an optical sensor. The output of the sensor is a binary result, either gluten detected (displayed as a wheat symbol) or gluten not detected (displayed as a smiley face). The Nima sensor currently sells for $209 on Amazon; each test capsule costs $5. Recently published validation data suggest that Nima has high sensitivity for detecting gluten at levels of 20ppm or more. The device’s specificity is high for purely gluten free ingredients, but when testing foods that are intentionally “spiked” with gluten at levels <20ppm, the specificity is considerably lower; for a food “spiked” to a level in the 10ppm range (still considered gluten-free by regulatory standards), the device’s specificity is closer to 50% (11, 12). Users of Nima have the option of pairing the device with their smartphones, enabling them to share test results with Nima and other users.
Study design
We examined all shared tests performed in the United States between August 2016 and January 2018. Each test included a date, time, restaurant name, address, food item tested, presence or absence of a gluten-free label, and test result. Using these parameters, we calculated rates of gluten detection by region, meal, median household income in the restaurant’s vicinity, restaurant genre, and specific foods.
For geographic analysis, we used the four regions used by the Census Bureau: Northeast (Connecticut, Maine, Massachusetts, New Hampshire, New Jersey New York, Pennsylvania, Rhode Island, Vermont), Midwest (Illinois, Indiana, Iowa, Kansas, Michigan, Minnesota, Missouri, Nebraska, North Dakota, Ohio, South Dakota, Wisconsin), South (Alabama, Arkansas, Delaware, District of Columbia, Florida, Georgia, Kentucky, Louisiana, Maryland, Mississippi, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, West Virginia, Virginia), and West (Alaska, Arizona, California, Colorado, Idaho, Hawaii, Montana, Nevada, New Mexico, Oregon, Utah, Washington). For analysis by meal, we defined breakfast time as 5am to 10:59am, lunchtime as 11am to 2:59pm, and dinner time as 3pm to 11:59pm. Median household income in a restaurant’s vicinity was extrapolated from zip codes and the 2016 American Community Survey. Zip codes were ranked by median household income and then divided into quartiles.
Building on previous methods used in the neighborhood food environment literature, we categorized restaurants into quick service, fast casual, and casual dining (13). We did this by cross-referencing the restaurants in our dataset with a list of nearly 400 restaurant chains sorted by restaurant type. We made this list by combining several annual lists of top chains from Technomics (a consulting firm for the restaurant industry) and Dun & Bradstreet (a company that tracks commercial data), with results from Google searches of “CITY NAME and Top Fast Food Restaurants.” Although we were able to sort several restaurants into additional categories using this methodology (fine dining, sweets, and coffee establishments), these categories were not included in the analysis due to a low number of tests performed in these settings.
The names of specific foods were free-texted by users. Given this heterogeneity, we classified foods manually, first reviewing the data to identify common dishes, and then assigning each test to a food category. We excluded tests that included more than one food item, and we restricted our analysis to food types with > 100 tests.
Statistical Analyses
All statistical analyses were performed in SAS University Edition (SAS Institute Inc, Cary, NC). For bivariate analyses, categorical variables were compared using chi-squared test. For multivariate analyses, we used multiple logistic regression, adjusting for region, median household income, and meal time, calculating odds ratios (ORs) and 95% confidence intervals (CIs). A two-tailed p value of <0.05 was considered statistically significant. This study was deemed “not human subjects research” by the Columbia University Medical Center’s Institutional Review Board, as data were deidentified before being provided to the investigators.
RESULTS
General Characteristics of Gluten Tests
During the study period, there were 5624 tests performed by 804 users. 84% of tested foods carried a GF label (Table 1). 59% of tests were performed during dinner hours; 27% were during lunch hours; and only about 11% were during breakfast hours. Tests were reported from 50 states. The greatest number of tests were performed in the West, accounting for about 46% of the data, followed by the South, accounting for another 25%. Regarding the distribution of data by median household income, the majority of tests were done at restaurants in the wealthiest quartile of zip codes, and 81% were done in the wealthier half of zip codes.
Table 1.
General characteristics of Nima tests
| Gluten-free label | |
| - Yes | 4732 (84.1%) |
| - No | 892 (15.9%) |
| Time of day/meal | |
| - Breakfast (5am - 10:59am) | 635 (11.3%) |
| - Lunch (11am - 2:59pm) | 1494 (26.6%) |
| - Dinner (3pm - 11:59pm) | 3327 (59.2%) |
| - Other (12am - 4:59am) | 168 (3.0%) |
| Region | |
| - Northeast | 980 (17.4%) |
| - South | 1378 (24.5%) |
| - Midwest | 690 (12.3%) |
| - West | 2576 (45.8%) |
| Median household income, zip code quartile | |
| - First (lowest) | 423 (7.7%) |
| - Second | 622 (11.3%) |
| - Third | 1027 (18.6%) |
| - Fourth (highest) | 3449 (62.5%) |
Overall Rate of Gluten Detection
32.2% of all foods in our study tested positive for gluten. The rate of gluten detection was essentially the same when we restricted this calculation to those 4732 foods that were specifically labeled GF (32.0%).
Bivariate Analysis of Factors Associated with Gluten Detection in GF Labeled Foods
After determining the overall rate of gluten detection, we searched for factors associated with detection of gluten in GF labeled foods. Through bivariate analysis, we found that rates of gluten detection did not differ significantly by region or median household income in the area around the restaurant. However, rates of gluten detection differed significantly by meal time, with 27% of GF labeled foods at breakfast testing positive for gluten, 30% at lunch, and 34% at dinner (p = 0.0008) (Table 2). Moreover, among restaurant types, fast casual had significantly lower rates of gluten detection (22%) when comparing this setting to all other foods tested (p = 0.0063). GF labeled pizza and pasta had the highest rates of gluten detection compared to all other tested foods, 53% (p < 0.0001) and 51% (p < 0.0001), respectively.
Table 2.
Factors associated with detection of gluten in GF labeled foods*
| Gluten present in GF labeled food | p-value | |
|---|---|---|
| Region | ||
| - Northeast | 294/853 (34.5%) | |
| - South | 382/1188 (32.2%) | 0.0668 |
| - Midwest | 205/595 (34.5%) | |
| - West | 633/2096 (30.2%) | |
| Median household income quartile | ||
| - First (lowest) | 95/343 (27.2%) | |
| - Second | 157/503 (31.2%) | 0.2801 |
| - Third | 297/914 (32.5%) | |
| - Fourth (highest) | 942/2877 (32.7%) | |
| Time of day/meal | ||
| - Breakfast | 138/508 (27.2%) | 0.0008 |
| - Lunch | 358/1213 (29.5%) | |
| - Dinner | 977/2873 (34.0%) | |
| Restaurant type | ||
| - Casual | 158/552 (28.6%) | 0.0708 |
| - Fast casual | 37/166 (22.3%) | 0.0063 |
| - Quick service | 67/201 (33.3%) | 0.6767 |
| Food item | ||
| - French fries | 53/175 (30.3%) | 0.6213 |
| - Pizza | 199/374 (53.2%) | <0.0001 |
| - Salad | 78/261 (29.9%) | 0.4522 |
| - Dessert | 59/195 (30.3%) | 0.5951 |
| - Burger | 50/165 (30.3%) | 0.6353 |
| - Soup | 35/125 (28.0%) | 0.3318 |
| - Taco | 32/110 (29.1%) | 0.5088 |
| - Pasta | 62/122 (50.8%) | <0.0001 |
| - Vegetables | 22/94 (23.4%) | 0.0713 |
| - Fish | 29/98 (29.6%) | 0.6063 |
p values derived from chi-square tests. In the case of restaurant type and food items, 2×2 chi-square tests were performed, comparing each restaurant/food item to all other tested foods not in that classification.
Multivariate Analysis of Factors Associated with Gluten Detection in GF Labeled Foods
Multivariate analysis adjusting for region, median household income, and time of day revealed a decreased likelihood of gluten detection in the West as compared with the Northeast (OR 0.80, 95% CI 0.67-0.95, p = 0.01). There was also an increased likelihood of gluten detection at dinner as compared with breakfast (OR 1.46, 95% CI 1.18-1.81, p = 0.0008) (Figure 1).
Figure 1.
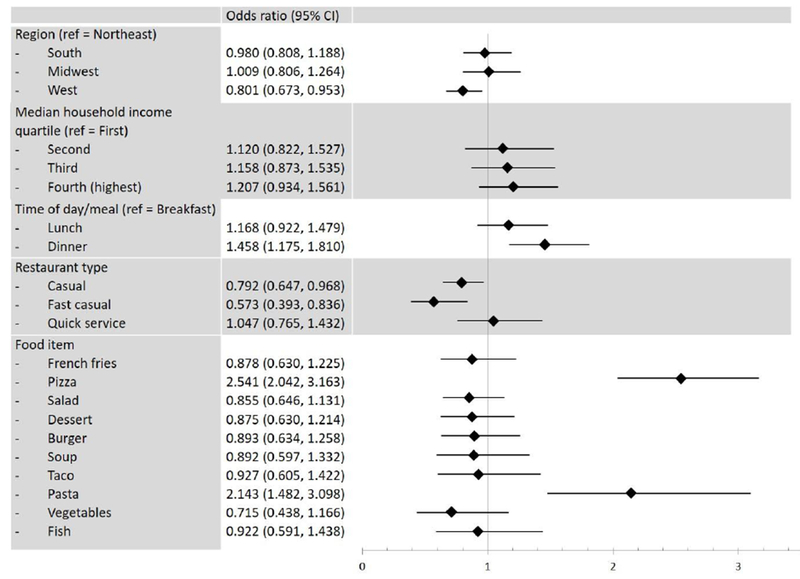
Multivariate analysis of factors associated with detection of gluten in GF labeled foods
Odds ratios for region, median household income, and time of day/meal were mutually adjusted. Analyses for the Restaurant Type and Food Items were run for each type/item versus all the other types/items combined and adjusted for region, median household income, and time of day/meal. Analysis of food items was limited to food items with > 100 tests.
Regarding restaurant types, GF labeled foods at casual (OR 0.79, 95% CI 0.65 to 0.97, p = 0.02) and fast casual (OR 0.57, 95% CI 0.39 to 0.84, p = 0.004) restaurants were less likely to test positive for gluten when comparing these settings to all other foods tested. Consistent with the bivariate analysis, pizza (OR 2.54, 95% CI 2.04 to 3.16, p < 0.0001) and pasta (OR 2.14, 95% CI 1.48 to 3.10, p < 0.0001) were more likely than other GF labeled foods to have gluten detected (Figure 1).
DISCUSSION
In this study of crowd-sourced data, approximately one-third of restaurant foods labeled GF tested positive for gluten. Rates of gluten detection were highest during dinner hours and lowest during breakfast hours. The West was the region within the United States with the lowest rate of gluten detection. Likewise, casual and fast casual restaurants stood out for lower rates of gluten detection. Pizza and pasta were the most likely to contain gluten, with more than 50% of samples testing positive.
Adherence to a GF diet is currently the only effective treatment for CD. Ingestion of as little as 50 mg of gluten per day can cause measurable damage to the small intestinal mucosa of CD patients (14). As a result of the vigilance required to maintain a truly GF diet, the burden of treatment of CD is high. Patients with CD rated their burden of treatment higher than patients with hypertension did, and similarly to patients with diabetes and end-stage renal disease (15). Multiple studies cite exposure to gluten while dining out as a leading source of anxiety for CD patients (5, 9, 10). Our study results lend some credence to widespread anecdotal reports offered by patients of symptoms suggestive of gluten exposure after eating in restaurants, though recent work has shown that symptoms are poorly predictive of mucosal injury (16).
Beyond suggesting an overall high rate of gluten contamination at restaurants, we identified several specific associations with higher or lower rates of gluten detection. For example, lower rates of gluten contamination were found in the West. Though data are sparse regarding regional differences in interest and knowledge about GF diets, higher rates of produce consumption and overall healthy lifestyle have been reported in the West (17), suggesting that people living in the western United States may be more health-conscious and thus more knowledgeable about diets perceived to be healthy. We previously found that the ratio of non-celiac gluten sensitivity to celiac disease appears to be highest in the Western United States (18). Given the rapid rise in gluten avoidance in recent years, outpacing the rise in celiac disease diagnosis (19), regional differences in the rise of non-celiac gluten sensitivity might yield greater awareness among both diners and restaurant staff. Food workers may take better precautions to guard against cross-contamination, and diners may make safer selections, such as avoiding salad dressings that are at risk of contamination.
Our finding of higher rates of gluten detection during dinner hours may reflect cumulative contamination of GF ingredients and/or equipment over the course of the day. It is not entirely clear why pizza and pasta were more likely to test positive for gluten than other GF labeled foods. GF pizza may become contaminated by aerosolized wheat flour during various stages of production. Sharing of ovens with gluten-containing pizza is a common concern, though a recent study suggests that it is not an inevitable setting for contamination (20). Although gluten is generally poorly soluble in water, it is possible that GF pasta may become contaminated by being cooked in the same water as conventional pasta. Alternatively, it is possible that the sauce on GF pizza or pasta is responsible for the detected gluten content. While these are both basic precautions, knowledge deficits among food preparers are likely considerable; indeed, a 2010 survey found that 23% of chefs had not heard of CD, and a significant minority incorrectly believed that peanut butter and wine contain gluten (9).
Lower rates of gluten detection at casual and fast casual restaurants was an unexpected finding. The survey of chefs referenced above found a direct relationship between average check price and chefs’ awareness of CD (9). One might therefore have expected more expensive restaurants to have lower rates of gluten contamination. Conversely, less expensive/chain restaurants may have more standardized training of their personnel in regards to gluten contamination. Admittedly, our analysis of restaurant genre was limited by the fact that the only one-fifth of all tests came from chain restaurants that were categorizable. Despite this limitation, it is fair to conclude that less expensive restaurants and chain restaurants, do not fair worse than their more expensive and independent counterparts in regards to gluten contamination.
As alluded to above, the vigilance required to maintain a strictly GF diet can be the source of significant anxiety. In fact, anxiety is more common in CD patients who have achieved mucosal healing on follow-up biopsy, a reflection of strict adherence. (21). Similarly, CD patients classified as “hyper-vigilant” in their efforts to avoid gluten have been found to report lower quality of life than their less vigilant counterparts. (22). So as to not cause undue alarm it is therefore important to note the limitations of these results.
First, our study did not involve systematic testing of all GF restaurant foods; it was a crowd-sourced study and the foods tested could have been conceivably chosen specifically because of doubts regarding their GF status. Furthermore, Nima users may be more inclined to share “gluten-found” than “gluten-free” results. Perhaps more importantly, our study relied on data from a portable gluten detection device that variably reports “gluten found” at levels less than 20 ppm. While a recent study from the makers of Nima reported a 7.8% false positive rate, they defined false positive as gluten being detected when the food actually contained less than 2 ppm gluten, though 20 ppm is the widely recognized threshold for packaged GF foods (11). Similarly, a third-party evaluation of Nima found the device frequently detects gluten at levels of 5 and 10 ppm (12). This high level of sensitivity may protect CD patients from potentially harmful gluten that may be present in greater quantity given the non-homogenized sampling inherent in point-of-care restaurant testing, but this same feature may also overestimate the prevalence of contamination of foods with > 20 ppm of gluten. The accuracy of our reported rates of gluten contamination is critically dependent on the underlying distribution of gluten concentrations (i.e. the percentage of positive tests containing 10, 30, or 300 ppm), data that are unknown in restaurant foods. However, even if we were to assume that only half of the reported positive tests contained > 20 ppm, cutting our estimated rate of contamination from 32% to 16%, that would still be triple the rate quantified for packaged GF-labeled foods (23). Additionally, the differences we found between regions, time of day, and specific foods are unlikely to be differentially affected by overestimation resulting from a hypersensitive sensor.
It is also important to consider the clinical significance of our findings. In CD, intestinal damage is related to the quantity of ingested gluten, not its concentration within food. Therefore, eating a single food portion with > 20 ppm gluten will not necessarily cause symptoms or villus atrophy. Rather, the 20-ppm threshold is valuable because it keeps intake of gluten below potentially toxic quantities (which vary between individuals, but are commonly injurious at levels of 50 mg per day) (14).
Despite the above caveats, this study provides much needed data for CD patients and the healthcare providers who treat and advise them. The crowdsourced nature of these data provides an unprecedented view of restaurant testing of food throughout the United States. As such, this is the largest study to date on gluten contamination of restaurant foods. It capitalizes on a newly available technology and reveals that a significant percentage of GF labeled restaurant foods contain detectable levels of gluten. Our findings of increased gluten detection in pizza, pasta, and evening hours lend themselves to practical advice for CD patients and also hint at possible mechanisms of contamination. Future studies should focus on quantifying the degree of gluten contamination in specific foods and the development of interventions on reducing gluten contamination in restaurants.
STUDY HIGHLIGHTS.
What is current knowledge?
Adherence to a gluten-free (GF) diet is the mainstay of therapy for celiac disease (CD).
Exposure to gluten while dining out is a major barrier to quality of life for CD patients.
What is new here?
We used crowd-sourced data from users of a portable gluten detection device to estimate rates of and identify risk factors for gluten contamination of supposed GF restaurant foods.
Approximately one-third of restaurant foods labeled GF contained detectable levels of gluten.
Rates of gluten detection were highest during dinner hours.
Pizza and pasta were the foods most likely to contain gluten, with more than 50% of samples testing positive.
Acknowledgments
Financial Support: The Nima device was developed with funding from the National Institutes of Health (Small Business Innovation Award DK105770). The database used for sorting restaurants by genre was produced with support from a grant from the NIA-NIH, 1R01AG049970-01A1: Communities Designed to Support Cardiovascular Health for Older Adults (PI Gina Lovasi).
Footnotes
Guarantor of the article: Benjamin Lebwohl, MD, MS.
Disclosures: BL serves as a consultant for Takeda and serves on the Advisory Board of Innovate Biopharmaceuticals. BL and PG are both unpaid members of Nima’s Scientific Advisory Board.
REFERENCES
- 1.Rubio-Tapia A, Ludvigsson JF, Brantner TL, Murray JA, and Everhart JE. The prevalence of celiac disease in the United States. Am J Gastroenterol. 2012;107(10):1538–44. [DOI] [PubMed] [Google Scholar]
- 2.Choung RS, Larson SA, Khaleghi S, Rubio-Tapia A, Ovsyannikova IG, King KS, et al. Prevalence and Morbidity of Undiagnosed Celiac Disease From a Community-Based Study. Gastroenterology. 2017;152(4):830–9 e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubio-Tapia A, Kyle RA, Kaplan EL, Johnson DR, Page W, Erdtmann F, et al. Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology. 2009;137(1):88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lebwohl B, Sanders DS, and Green PHR. Coeliac disease. Lancet. 2018;391(10115):70–81. [DOI] [PubMed] [Google Scholar]
- 5.Barratt SM, Leeds JS, and Sanders DS. Quality of life in Coeliac Disease is determined by perceived degree of difficulty adhering to a gluten-free diet, not the level of dietary adherence ultimately achieved. J Gastrointestin Liver Dis. 2011;20(3):241–5. [PubMed] [Google Scholar]
- 6.Abdulkarim AS, Burgart LJ, See J, and Murray JA. Etiology of nonresponsive celiac disease: results of a systematic approach. Am J Gastroenterol. 2002;97(8):2016–21. [DOI] [PubMed] [Google Scholar]
- 7.Hollon JR, Cureton PA, Martin ML, Puppa EL, and Fasano A. Trace gluten contamination may play a role in mucosal and clinical recovery in a subgroup of diet-adherent non-responsive celiac disease patients. BMC Gastroenterol. 2013;13:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Syage JA, Kelly CP, Dickason MA, Ramirez AC, Leon F, Dominguez R, et al. Determination of gluten consumption in celiac disease patients on a gluten-free diet. Am J Clin Nutr. 2018;107(2):201–7. [DOI] [PubMed] [Google Scholar]
- 9.Simpson S, Lebwohl B, Lewis SK, Tennyson CA, Sanders DS, and Green PH. Awareness of gluten-related disorders: A survey of the general public, chefs and patients. E Spen Eur E J Clin Nutr. 2011;6:e227–e31. [Google Scholar]
- 10.Lee A, and Newman JM. Celiac diet: its impact on quality of life. J Am Diet Assoc. 2003;103(11):1533–5. [DOI] [PubMed] [Google Scholar]
- 11.Zhang J, Portela SB, Horrell JB, Leung A, Weitmann DR, Artiuch JB, et al. An integrated, accurate, rapid, and economical handheld consumer gluten detector. Food Chem. 2019;275:446–56. [DOI] [PubMed] [Google Scholar]
- 12.Taylor SL, Nordlee JA, Jayasena S, and Baumert JL. Evaluation of a Handheld Gluten Detection Device. J Food Prot. 2018;81(10):1723–8. [DOI] [PubMed] [Google Scholar]
- 13.Rundle A, Neckerman KM, Freeman L, Lovasi GS, Purciel M, Quinn J, et al. Neighborhood food environment and walkability predict obesity in New York City. Environ Health Perspect. 2009;117(3):442–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Catassi C, Fabiani E, Iacono G, D’Agate C, Francavilla R, Biagi F, et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am J Clin Nutr. 2007;85(1):160–6. [DOI] [PubMed] [Google Scholar]
- 15.Shah S, Akbari M, Vanga R, Kelly CP, Hansen J, Theethira T, et al. Patient perception of treatment burden is high in celiac disease compared with other common conditions. Am J Gastroenterol. 2014;109(9):1304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahadev S, Murray JA, Wu TT, Chandan VS, Torbenson MS, Kelly CP, et al. Factors associated with villus atrophy in symptomatic coeliac disease patients on a gluten-free diet. Aliment Pharmacol Ther. 2017;45(8):1084–93. [DOI] [PubMed] [Google Scholar]
- 17.Troost JP, Rafferty AP, Luo Z, and Reeves MJ. Temporal and regional trends in the prevalence of healthy lifestyle characteristics: United States, 1994–2007. Am J Public Health. 2012;102(7):1392–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zylberberg HM, Yates S, Borsoi C, Green PHR, and Lebwohl B. Regional and National Variations in Reasons for Gluten Avoidance. J Clin Gastroenterol. 2018;52(8):696–702. [DOI] [PubMed] [Google Scholar]
- 19.Kim HS, Patel KG, Orosz E, Kothari N, Demyen MF, Pyrsopoulos N, et al. Time Trends in the Prevalence of Celiac Disease and Gluten-Free Diet in the US Population: Results From the National Health and Nutrition Examination Surveys 2009–2014. JAMA Intern Med. 2016;176(11):1716–7. [DOI] [PubMed] [Google Scholar]
- 20.Vincentini O, Izzo M, Maialetti F, Gonnelli E, Neuhold S, and Silano M. Risk of Cross-Contact for Gluten-Free Pizzas in Shared-Production Restaurants in Relation to Oven Cooking Procedures. J Food Prot. 2016;79(9):1642–6. [DOI] [PubMed] [Google Scholar]
- 21.Ludvigsson JF, Lebwohl B, Chen Q, Broms G, Wolf RL, Green PHR, et al. Anxiety after coeliac disease diagnosis predicts mucosal healing: a population-based study. Aliment Pharmacol Ther. 2018;48(10):1091–8. [DOI] [PubMed] [Google Scholar]
- 22.Wolf RL, Lebwohl B, Lee AR, Zybert P, Reilly NR, Cadenhead J, et al. Hypervigilance to a Gluten-Free Diet and Decreased Quality of Life in Teenagers and Adults with Celiac Disease. Dig Dis Sci. 2018;63(6):1438–48. [DOI] [PubMed] [Google Scholar]
- 23.Thompson T, and Simpson S. A comparison of gluten levels in labeled gluten-free and certified gluten-free foods sold in the United States. Eur J Clin Nutr. 2015;69(2):143–6. [DOI] [PubMed] [Google Scholar]


