Abstract
Persistent Mullerian duct syndrome (PMDS) is a rare entity of internal male pseudohermaphroditism. Transverse testicular ectopia (TTE) is the condition in which one testis moves to the other side and both testes pass the same inguinal canal. The combination of PMDS with TTE is rarer. Here, we present a case a phenotype male with left inguinal hernia and right undescended testis. On exploration of left inguinal region, uterus like tissue with its tubal structures were found. Both testes were in same side, one in left inguinal region and the other in the left scrotum.
Introduction
Persistent Mullerian duct syndrome (PMDS) is a rare entity of internal male pseudohermaphroditism. It usually presents as undescended testis. Deficiency of antimullerian hormone or its insensitivity leads to persistence of Mullerian ducts and its derivatives. Transverse testicular ectopia (TTE) is the condition in which one testis moves to the other side and both testes pass the same inguinal canal. The combination of PMDS with TTE is rarer.
Case presentation
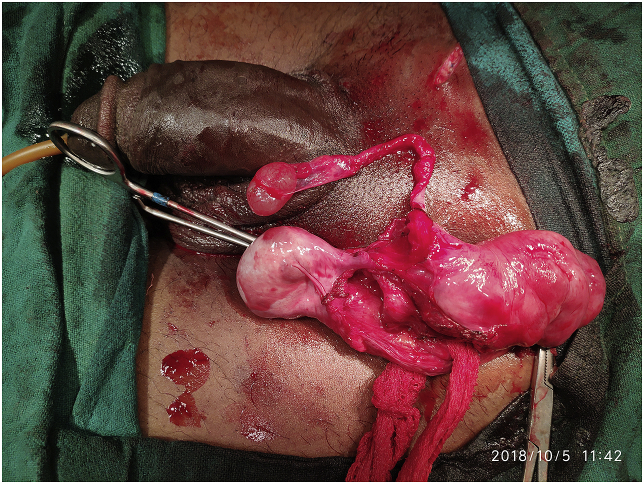
27 years male, married with a baby presented with history of swelling and pain in left inguinal region. On examination, there was reducible swelling in left inguinal region. External genitalia examination showed normal secondary sexual character development. Right testis was not palpable. USG showed normal left testis with inguinoscrotal hernia in left side, with right undescended testis in right inguinal region. Right inguinal exploration was done but we could not find the testis in right side. Left inguinal exploration showed uterus like tissue with tubal structures (Fig. 1). Testis like structure was also present in the left inguinal region which was the ectopic testis from right side. Normal left testis was present in left scrotum (Fig. 2). Removal of the inguinal testis with uterus and its tubal structures was done preserving the vas deferens of left testis. Left orchidopexy was done.
Fig. 1.
Uterus like tissue with tubal structures.
Fig. 2.

Both testis in left side - one in the inguinal canal and the other in the scrotum.
Histopathological reports showed uterus tissue with proliferative phase endometrium and unremarkable myometrium with paratubal ducts (Fig. 3). Section of testis showed atrophied testicular tissue. Semen analysis done postoperatively was normal. FSH and testosterone level were normal. Patient refused karyotyping.
Fig. 3.
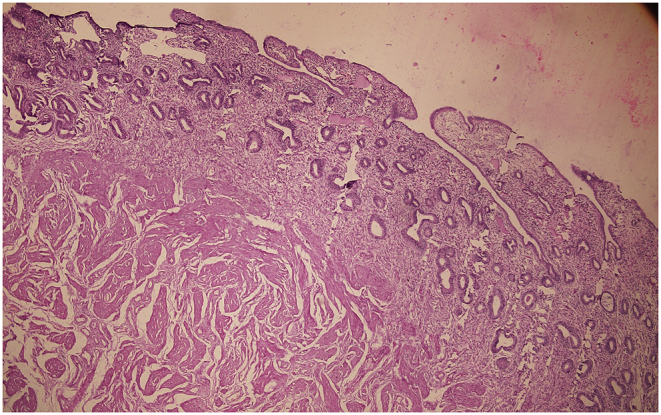
Proliferative phase of Endometrium.
Discussion
Persistent Mullerian Duct Syndrome (PMDS) was first described by Nilson in 1939. It is the persistence of derivation of Mullerian duct in male. Mullerian Inhibiting substance from Sertoli cells inhibit the development of Mullerian duct. Testosterone from leyding cells promote development of Wolffian duct structures. If Mullerian duct fails to regress, testis remains suspended to broad ligament.1 Testis may remain in inguinal canal canal hernia along with uterus named as hernia uteri inguinalis.
There are three anatomical classification of PMDSs. Type I is male type in which testis is present in the scrotum or in the inguinal canal and can be brought into scrotum by gentle traction. Type is male type with transverse testicular ectopia. Type III is female type which presents as bilateral cryptorchidism and testis is present at ovarian position with respect to uterus.2
Mullerian duct structures may anchor to pelvis and prevent further descend of testis leading to cryptorchidism.2 Incidence of PMDS is increasing because of increasing investigations for cryptorchidism and use of laparoscopy. Secondary sexual characters are usually normal.
Diagnosis is usually incidental during surgery. Infertility is the most common complication. The patient may be fertile if there is one testis in the scrotum. Fertility is rare and is possible if one testis is present in the scrotum.
Rate of malignancy is around 18%.3 Seminoma is the most common and may develop embryonal carcinoma or yolk sac tumor. Early surgical intervention, if not orchidectomy may prevent malignancy. There is also increased risk of malignancy of Mullerian remnant and removal of the Mullerian remnant decreases risk of malignancy.4 Chance to injure vas during removal of Mullerian structures is high and one should be careful while dissecting the Mullerian structures to prevent the vas injury.
Transverse Testicular Ectopia (TTE) is the condition in which one testis moves to opposite side and both testis pass the same inguinal canal. TTE is a very rare entity and till date, around 260 cases of TTE has been reported.5 Concurrence of TTE with PMDS is even more rare and around 57 cases has been reported.5
Conclusion
PMDSs is a rare entity that may present as inguinal hernia with undescended testis. Early diagnosis and treatment is necessary to prevent malignancy.
Ethics
Informed consent from the patient.
Declaration of interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.eucr.2019.100888.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Miller A., Hong M.K., Hutson J.M. The broad ligament: a review of its anatomy and development in different species and hormonal environments. Clin Anat (New York, NY) 2004;17(3):244–251. doi: 10.1002/ca.10173. [DOI] [PubMed] [Google Scholar]
- 2.Solanki S., Gowrishankar Jadhav V., Babu M.N., Ramesh S. Female form of persistent mullerian duct syndrome: rare entity. Urol Ann. 2015;7(1):104–106. doi: 10.4103/0974-7796.148640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bucci S., Liguori G., Buttazzi L., Bussani R., Trombetta C. Bilateral testicular carcinoma in patient with the persistent mullerian duct syndrome. J Urol. 2002;167(4):1790. [PubMed] [Google Scholar]
- 4.Farikullah J., Ehtisham S., Nappo S., Patel L., Hennayake S. Persistent Mullerian duct syndrome: lessons learned from managing a series of eight patients over a 10-year period and review of literature regarding malignant risk from the Mullerian remnants. BJU Int. 2012;110(11 Pt C):E1084–E1089. doi: 10.1111/j.1464-410X.2012.11184.x. [DOI] [PubMed] [Google Scholar]
- 5.Rajesh A., Farooq M. A rare case of male pseudohermaphroditism-persistent mullerian duct syndrome with transverse testicular ectopia - case report and review of literature. Int J Surg Case Rep. 2017;37:72–75. doi: 10.1016/j.ijscr.2017.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.