Abstract
Background and aim of the Work: Groin pain after hip arthroplasty (HA) ranges from 0.4% to 18.3%. Defining the cause of groin pain after HA can be difficult. Iliopsoas impingement (IPI) has been reported to be the underlying cause of groin pain in up to 4.4% of cases. The purpose of this study is to present arthroscopic surgical outcomes in the treatment of IPI after HA. Methods: Between September 2013 and March 2018, 13 patients, 11 total hip arthroplasty (THA), 1 hip endoprosthesis and 1 total hip resurfacing affected by groin pain due to unceasing iliopsoas tendinopathy for impingement after HA were treated arthroscopically. The patients underwent to physical examination, blood analysis, hip X-rays, bone scintigraphy and CT assessment. We performed the arthroscopic OUT-IN access to hip joint in all patients. VAS scale, Harris Hip Score (HHS) and Medical Research Council (MRC) scale were performed before surgery and during follow up at 1-3-6-12 months. Results: After 10 months of mean follow-up, average HHS and MRC scale improved significantly from preoperatively to postoperatively. No complications arose in our case series. Conclusions: Hip arthroscopy after hip arthroplasty is supported in the literature for a variety of indications. Hip arthroscopy is a viable and reproducible technique in treatment of IPI, being less invasive than the classic open technique. This simple arthroscopic release provides satisfactory results and preserves HA function. Moreover an arthroscopic OUT-IN access proves good clinical outcomes, few complications and iatrogenic lesions. (www.actabiomedica.it)
Keywords: groin pain, iliopsoas impingement, hip arthroplasty, hip arthroscopy, release
Background and aim of the Work
Groin pain after total hip replacement has a prevalence rate ranging from 0.4% to 18.3% (1). The potential causes of groin pain can be classified into intrinsic and extrinsic factors, being the former infections, aseptic failure, periprosthetic osteolysis, allergic reaction and pain due to lumbar spine pathology, abdominal, vascular or oncological injuries the latter (2-4).
Iliopsoas impingement (IPI) after hip arthroplasty (HA) is a potential cause of persistent groin pain and hip joint restriction often being underdiagnosed with a 4.4% frequency according to literature (5).
This condition was first reported by Postel et al. in 1975 (6) and then by Lasquene et al. in 1991 (7). Trousdale et al. in 1995 (8) recorded 2 cases of groin pain after total hip replacement treated with revision of the acetabular component after conservative treatment failure. During surgical revision procedure they found a frayed ileopsoas tendon anteriorly, impinged on the anterior rim of the acetabular component.
The iliopsoas is an complex musculo-tendinous unit (9) that inserts into the lesser trochanter. Psoas major tendon originates above of the inguinal ligament. It exits the pelvis distally, running over the anterior acetabular wall and over the hip joint with the medial iliacus bundle that unites into the psoas major tendon. This complex musculo-tendinous unit acts as a powerful hip flexor and secondarily as a femoral rotator and stabilizer of the lumbar spine and pelvis.
IPI in HA usually happens because of tendon inflammation due to mechanical irritation with antero-inferior acetabular edge. However there are other less common causes inducing IPI. They can be divided into mechanical and not mechanical reasons (5, 10-12).
The main clinical sign of IPI is groin pain which started from the first month until a several years after HA (12, 13).
The diagnosis of IPI is composed of physical examination, x-rays (4, 8) and computed tomography (CT) images (14). Hip arthroscopy after hip arthroplasty is supported in the literature addressing several conditions (15). Hip arthroscopy can be a safe and effective method of treating IPI in hip arthroplasty and an useful diagnostic tool for further diagnostic investigation (15). The purpose of our study is to present arthroscopic surgical outcomes in the treatment of IPI after HA.
Methods
Between September 2013 and March 2018 we identified 13 patients, 11 total hip arthroplasty (THA), 1 hip endoprosthesis and 1 total hip resurfacing with a diagnosis of iliopsoas impingement. Nine patients were males and four were females, the mean age was of 65 years (range 47-82). The average time to onset of symptoms was 6 months after HA.
Seven THA were implanted in our department (Department of Orthopaedic Surgery, University Hospital of Udine, Udine, Italy). The diagnosis was based on clinical evidence and imaging.
The patients underwent physical examination, blood analysis, i.e white blood cell count, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), hip X-rays, bone scintigraphy (16) and CT assessment (14, 17). Initially, we excluded hip periprosthetic joint infection (PJI) following the diagnostic criteria for PJI that have been established (18).
Patients complained typical symptoms (4, 13, 19-21), severe groin pain when climbing stairs and getting in and out of a car (car sign) or bed from the first months after HA, often manually assisting elevation of the lower limb.
Physical examination showed tenderness on palpation in the groin area, groin pain with active hip flexion, especially straight leg raise against resistance, and on stretching of the the hip flexors, a positive iliopsoas contracture test.
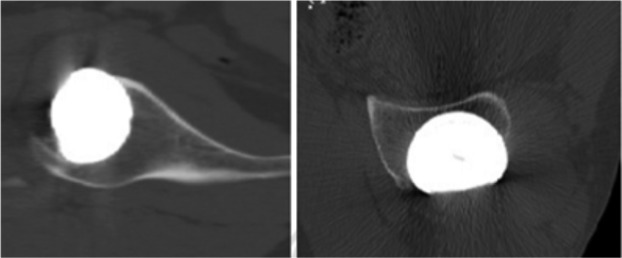
The diagnosis of IPI was confirmed by x-rays including true lateral hip view (Fig. 1) and computed tomographic (CT) scans (Fig. 2) to demonstrate anteroinferior component prominence (4, 14).
Figure 1.
Preoperative true lateral view radiographs of THA (A), Hip endoprosthesis (B), total hip resurfacing (C)
Figure 2.
CT scans tries antero-inferior component prominence
We performed arthroscopic tendon release in all screened patients after 6 months of no effective conservative treatment (10, 22) with <8 mm of acetabular component prominence (5).
Visual Analogue Scale (VAS) (23) for pain evaluation, Harris Hip Score (HHS) (24) for hip function and Medical Research Council (MRC) scale (25) for grading the patient’s muscle strength on a 0 to 5 scale were performed before surgery and during follow up at 1-3-6-12 months after surgery.
Hip arthroscopy was performed in all patients with extra-capsular (OUT-IN) access (26) and tendon release was carried out according to Wettstein technique (27) in the impingement zone on the anterior rim of the acetabular component.
In the post-operative period we recommend no weight-bearing and assisted rehabilitation program performing only passive hip mobility for 2 weeks. Active hip flexion with straight leg raise had to be avoided for 4 weeks as well.
Results
All 13 patients had a negative preoperative assessment for signs of infection or loosening.
Preoperative clinical evaluation showed the average HHS of 66.8 points (range 48.9-81.8), the average MRC scale 3.6 grade (range 3-4), the mean hip flexion of 95° (range 80°-100°), the average VAS 3.6 points (range 2-6).
Preoperative imaging assessment proved acetabular cup prominence due to poor acetabular cup anteversion in THA, to large cup of hip endoprosthesis and prominent and medialized large femoral head on the femoral neck in total hip resurfacing.
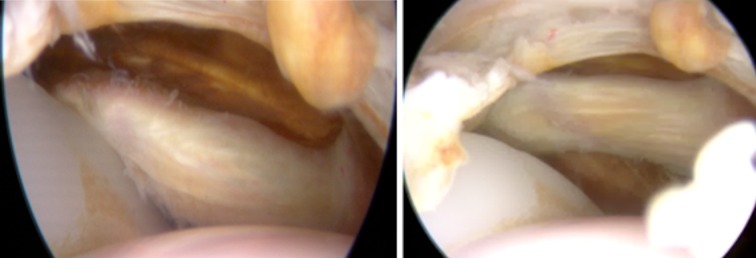
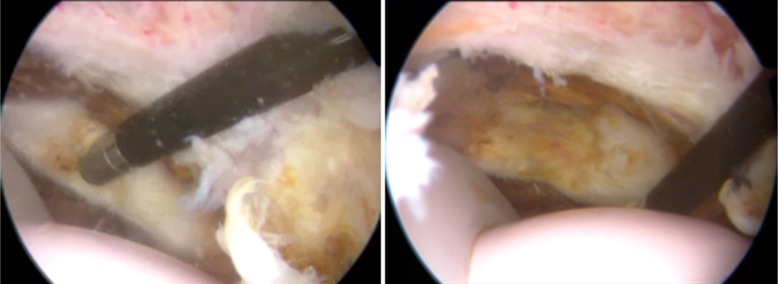
In all patients, arthroscopic examination revealed iliopsoas kneeling and mechanical irritation with antero-inferior acetabular edge (Fig. 3). The tendon release was performed using the technique described above in all patients (Fig. 4). One patient with hip endoprosthesis had large periprosthetic ossification, which was removed.
Figure 3.
Arthroscopic view shows iliopsoas kneeling and mechanical irritation with antero-inferior acetabular edge
Figure 4.
Arthroscopic psoas release in the impingement zone on the anterior rim of the acetabular component
During post-operative recovery patients had no complications and the hospital stay was 1 day. Patients underwent 1-3-6-12 months follow-up.
All patients had immediately improvement in pain and function, no complications arose during follow-up period and evaluation of their satisfaction degree revealed to be high. For these reasons many patients did not completely respect the follow-up monitoring.
After 10 months of mean follow-up (3-12), average HHS, MRC scale, hip flexion and VAS improved significantly from preoperatively to postoperatively to 85 points (range 80-95), 4.7 grade (range 3-5), 105°(range 90°-120°) 1 point (range 0-3), respectively.
Conclusions
Pain in the groin area is due to several injuries and often different pathologies overlap becoming, sometimes, a real diagnostic challenge (21, 28). Iliopsoas-related groin pain generally occur with pain on resisted hip flexion and/or pain on stretching the hip flexors (21). Iliopsoas impingement may be a cause for persistent groin pain after hip arthroplasty (HA). Other possible and more frequent causes for HA failure should of course be excluded. Among all, PJI must be early excluded. Laboratory tests (white blood cell count, ESR, CRP), radiographs and bone scintigraphy can help to rule out this diagnosis (16, 29, 30). IPI after HA is more frequent than previously assumed. This condition is very disabling; severe groin pain appears in the first months after hip replacement during hip flexion against resistance and stretching of the iliopsoas tendon (4, 20, 21).
Iliopsoas tendon sheath corticosteroid and anesthetic agent injections represents a valuable diagnostic test with an immediate therapeutic effect. Conservative treatment should always be attempted for at least 6 months (31, 32).
Physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs), and local corticosteroid or botulinum toxin A injections are nonoperative options to relieve pain at the beginning or in the long term in patients who can not undergo surgery (10, 22).
Outcomes reported a pain average improvement of 50% after one year (31, 32). The indication for surgical treatment was recommended after unsuccessful conservative treatment, with the typical clinical signs and symptoms, a positive local anesthesia test and radiological signs for an anterior prominent acetabular component (5). Acetabular revision is associated with high complication and revision rates, but when cup prominence is ≥8mm acetabular revision is recommended with a high success rate of groin pain resolution and excellent clinical outcomes (5, 31). On the other hand, patients with <8 mm of acetabular prominence can benefit from the iliopsoas tenotomy (5). Iliopsoas tenotomy can be performed either by open technique or arthroscopic release. Open tenotomy allows evaluation of component positioning, stability of the acetabular component and other abnormal processes that might contribute to the patient ’s groin pain. The success rate ranges between 75% and 91.5% (2). However open tenotomy is more invasive, requiring a longer hospital stay and recovery period. It has a higher risk of implant infection or bearing surface damage than the arthroscopic release (10), whereas arthroscopic treatment of IPI after hip replacement has about 94% of success rate (2). In our case series, all patients affected by IPI had <8 mm of acetabular anteroinferior prominence on true lateral hip radiographs. Another topic debated is the size of the head in addition to the acetabular protrusion as a cause of groin pain after THA.
Varadarajan et al. (33) assessed the contact between the femoral head and the iliopsoas complex with heads of various sizes. This contact was visually observed following dissection and THA implantation, as well as the “ileopsoas tenting” caused by the traditional heads. The use of small diameter femoral heads relieves hip pain but increases the risk of dislocation. Therefore, in order to use larger diameter heads, it is necessary to use heads with the most anatomical peripheral profile in its lower half.
In our case series, all patients experienced immediately improvement in pain and function, no complications arose and everyone was highly satisfied.
Analyzing the prosthesis with IPI, we had 7 Collum Femoris Preserving (CFP) (34) THA implanted in our surgical department despite we followed surgical technique for CFP implantation to avoid this complication. The acetabular cup of this implant has a middle-caudal groove to limits the possibility of the impingement with psoas tendon and femoral nerve. In addition we had been careful not to overflow the collar component more than 1-2 mm to avoid collar impingement with the psoas tendon (34).
Pain incidence by total hip endoprosthesis implantation is around 1-17.6% depending on the type of prosthesis. Few reports describe IPI as a cause of pain following implantation of an endoprosthesis in total hip arthroplasty (35). We treated successfully one patient for IPI following hip endoprosthesis with large cup component.
The rate of groin pain following hip resurfacing is about 18%, a greater rate than conventional THA (12, 36). In hip resurfacing the possible causes of pain are hypersensitivity to metal-on-metal bearing surfaces or greater impingement of the psoas tendon across the larger femoral heads used (37). Our patient experienced moderate groin pain that was relieved after arthroscopic release. The cup is not prominent anteriorly, but the large femoral head is prominent and medialized on the femoral neck. Cobb et al. (38) suggested that IPI may be caused by the oversized apron of the metal head that extends well beyond the limit of the normal femoral head. This zone is used as a fulcrum by the tendon of iliopsoas in full extension. Then in total hip resurfacing if the centre of the acetabulum is moved forward, or the size of the head is increased, IPI is almost assured.
Hip arthroscopy is a viable and reproducible technique in treatment of IPI, being less invasive than the classic open technique. Also it is a valuable diagnostic tool to address the diagnosis, if metallosis or infection were detected (15).
The arthroscopic iliopsoas tendon release was performed in the impingement zone on the anterior rim of the acetabular component to avoid loss of hip flexion strength that can be caused by its tenotomy at trochanteric insertion (2, 27, 39, 40).
Moreover, two recent case series showed good outcomes in terms of pain and recovery of muscle strength with endoscopic tenotomy at the lesser trochanter (10, 41).
This simple arthroscopic release provides satisfactory results and preserves HA function with a low rate of complications.
Our experience in arthroscopic treatment of IPI after hip arthroplasty agrees with the literature that present small cases series (between 7 and 35 cases) showing excellent results and no complications (2, 10, 13, 42).
Guicherd W et al. (41) presents the only prospective multicenter case series (64 cases performed in 8 centers) that shows two early complications after arthroscopic iliopsoas relesase: one case of anterior dislocation in transcapsular tenotomy and one case of compressive hematoma affecting the peroneal nerve.
Our arthroscopic extracapsular access (OUT-IN) to the hip, as previously published (26), allows some important advantages. The introduction of the instruments takes place after the capsulotomy under arthroscopic vision, away from the prosthesis avoiding damage. Hip distraction during the arthroscopic accesses is not necessary as well as the use of X-ray, which prevents patient and surgeons exposure to ionizing radiations, reduces surgical timing and risk of hip joint infection.
References
- 1.Forster-Horvath C, Egloff C, Valderrabano V, Nowakowski A. M. The painful primary hip replacement - review of the literature. Swiss Med. Wkly. 2014;144(w13974) doi: 10.4414/smw.2014.13974. [DOI] [PubMed] [Google Scholar]
- 2.Jerosch J, Neuhäuser C, Sokkar S. M. Arthroscopic treatment of iliopsoas impingement (IPI) after total hip replacement. Arch. Orthop. Trauma Surg. 2013;133:1447–1454. doi: 10.1007/s00402-013-1806-6. [DOI] [PubMed] [Google Scholar]
- 3.Duffy P, Masri B. A, Garbuz D, Duncan C. P. Evaluation of patients with pain following total hip replacement. Instr. Course Lect. 2006;55:223–232. [PubMed] [Google Scholar]
- 4.Lachiewicz P. F, Kauk J. R. Anterior iliopsoas impingement and tendinitis after total hip arthroplasty. J. Am. Acad. Orthop. Surg. 2009;17:337–344. doi: 10.5435/00124635-200906000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Chalmers B. P, Sculco P. K, Sierra R. J, Trousdale R. T, Berry D. J. Iliopsoas Impingement After Primary Total Hip Arthroplasty: Operative and Nonoperative Treatment Outcomes. J. Bone Joint Surg. Am. 2017;99:557–564. doi: 10.2106/JBJS.16.00244. [DOI] [PubMed] [Google Scholar]
- 6.Postel M. [Painful prosthesis. I. Possible causes] Rev. Chir. Orthop. Reparatrice Appar. Mot. 1975;61(2):57–61. [PubMed] [Google Scholar]
- 7.Lequesne M, Dang N, Montagne P, Lemoine A, Witvoet J. [Conflict between psoas and total hip prosthesis] Rev. Rhum. Mal. Osteoartic. 1991;58:559–564. [PubMed] [Google Scholar]
- 8.Trousdale R. T, Cabanela M. E, Berry D. J. Anterior iliopsoas impingement after total hip arthroplasty. J. Arthroplasty. 1995;10:546–549. doi: 10.1016/s0883-5403(05)80160-3. [DOI] [PubMed] [Google Scholar]
- 9.Iliopsoas: Pathology, Diagnosis, and Treatment. - PubMed - NCBI. doi: 10.1016/j.csm.2016.02.009. Available at: https://www.ncbi.nlm.nih.gov/pubmed/27343394. (Accessed: 8th December 2018) [DOI] [PubMed] [Google Scholar]
- 10.Gédouin J.-E., Huten D. Technique and results of endoscopic tenotomy in iliopsoas muscle tendinopathy secondary to total hip replacement: a series of 10 cases. Orthop. Traumatol. Surg. Res. OTSR. 2012;98:S19–25. doi: 10.1016/j.otsr.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Heaton K, Dorr L. D. Surgical release of iliopsoas tendon for groin pain after total hip arthroplasty. J. Arthroplasty. 2002;17:779–781. doi: 10.1054/arth.2002.33570. [DOI] [PubMed] [Google Scholar]
- 12.O’Sullivan M, et al. Iliopsoas tendonitis a complication after total hip arthroplasty. J. Arthroplasty. 2007;22:166–170. doi: 10.1016/j.arth.2006.05.034. [DOI] [PubMed] [Google Scholar]
- 13.Van Riet A, De Schepper J, Delport H. P. Arthroscopic psoas release for iliopsoas impingement after total hip replacement. Acta Orthop. Belg. 2011;77:41–46. [PubMed] [Google Scholar]
- 14.Cyteval C, et al. Iliopsoas impingement on the acetabular component: radiologic and computed tomography findings of a rare hip prosthesis complication in eight cases. J. Comput. Assist. Tomogr. 2003;27:183–188. doi: 10.1097/00004728-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Heaven S, et al. Hip arthroscopy in the setting of hip arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA. 2016;24:287–294. doi: 10.1007/s00167-014-3379-5. [DOI] [PubMed] [Google Scholar]
- 16.Trevail C, Ravindranath-Reddy P, Sulkin T, Bartlett G. An evaluation of the role of nuclear medicine imaging in the diagnosis of periprosthetic infections of the hip. Clin. Radiol. 2016;71:211–219. doi: 10.1016/j.crad.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 17.Cyteval C, Bourdon A. Imaging orthopedic implant infections. Diagn. Interv. Imaging. 2012;93:547–557. doi: 10.1016/j.diii.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Di Benedetto P, et al. Algoritmo decisionale nelle infezioni periprotesiche. LO SCALPELLO-OTODI Educ. 2017;31:247–252. [Google Scholar]
- 19.Jasani V, Richards P, Wynn-Jones C. Pain related to the psoas muscle after total hip replacement. J. Bone Joint Surg. Br. 2002;84:991–993. doi: 10.1302/0301-620x.84b7.13194. [DOI] [PubMed] [Google Scholar]
- 20.Henderson R. A, Lachiewicz P. F. Groin pain after replacement of the hip: aetiology, evaluation and treatment. J. Bone Joint Surg. Br. 2012;94:145–151. doi: 10.1302/0301-620X.94B2.27736. [DOI] [PubMed] [Google Scholar]
- 21.Bisciotti G. N, et al. Groin Pain Syndrome Italian Consensus Conference on terminology, clinical evaluation and imaging assessment in groin pain in athlete. BMJ Open Sport Exerc. Med. 2016;2:e000142. doi: 10.1136/bmjsem-2016-000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fish D. E, Chang W. S. Treatment of iliopsoas tendinitis after a left total hip arthroplasty with botulinum toxin type A. Pain Physician. 2007;10:565–571. [PubMed] [Google Scholar]
- 23.Haefeli M, Elfering A. Pain assessment. Eur. Spine J. 2006;15:S17–S24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris W. H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Joint Surg. Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 25.Compston A. Aids to the investigation of peripheral nerve injuries. Medical Research Council: Nerve Injuries Research Committee. His Majesty’s Stationery Office: 1942; pp. 48 (iii) and 74 figures and 7 diagrams; with aids to the examination of the peripheral nervous system. By Michael O’Brien for the Guarantors of Brain. Saunders Elsevier: 2010; pp. [8] 64 and 94 Figures. Brain J. Neurol. 2010;133:2838–2844. doi: 10.1093/brain/awq270. [DOI] [PubMed] [Google Scholar]
- 26.Di Benedetto P, et al. Extracapsular vs standard approach in hip arthroscopy. Acta Bio-Medica Atenei Parm. 2016;87(1):41–45. [PubMed] [Google Scholar]
- 27.Wettstein M, Jung J, Dienst M. Arthroscopic psoas tenotomy. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2006;22(907):e1–4. doi: 10.1016/j.arthro.2005.12.064. [DOI] [PubMed] [Google Scholar]
- 28.Pogliacomi F, Costantino C, Pedrini MF, Pourjafar S, De Filippo M, Ceccarelli F. Anterior groin pain in athlete as consequence of bone diseases: aetiopathogenensis, diagnosis and principles of treatment. Medicina dello Sport. 2014;67(1):1–27. [Google Scholar]
- 29.Della Valle C, et al. American Academy of Orthopaedic Surgeons clinical practice guideline on: the diagnosis of periprosthetic joint infections of the hip and knee. J. Bone Joint Surg. Am. 2011;93:1355–1357. doi: 10.2106/JBJS.9314ebo. [DOI] [PubMed] [Google Scholar]
- 30.de Vries E. F. J, Roca M, Jamar F, Israel O, Signore A. Guidelines for the labelling of leucocytes with 99mTc-HMPAO. Eur. J. Nucl. Med. Mol. Imaging. 2010;37:842–848. doi: 10.1007/s00259-010-1394-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dora C, Houweling M, Koch P, Sierra R. J. Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J. Bone Joint Surg. Br. 2007;89:1031–1035. doi: 10.1302/0301-620X.89B8.19208. [DOI] [PubMed] [Google Scholar]
- 32.Adler R. S, Buly R, Ambrose R, Sculco T. Diagnostic and therapeutic use of sonography-guided iliopsoas peritendinous injections. AJR Am. J. Roentgenol. 2005;185:940–943. doi: 10.2214/AJR.04.1207. [DOI] [PubMed] [Google Scholar]
- 33.Varadarajan K. M, et al. Next-generation soft-tissue-friendly large-diameter femoral head. Semin. Arthroplasty. 2013;24:211–217. [Google Scholar]
- 34.Pipino F, Calderale P. M. A biequatorial acetabular cup for hip prosthesis. Acta Orthop. Belg. 1980;46:5–13. [PubMed] [Google Scholar]
- 35.Kälicke T, Wick M, Frangen T. M, Muhr G, Seybold D. [Iliopsoas tendinitis--rare cause of pain following implantation of a total hip endoprosthesis] Unfallchirurg. 2005;108(1078):1080–1082. doi: 10.1007/s00113-005-0981-5. [DOI] [PubMed] [Google Scholar]
- 36.Bin Nasser A, Beaulé P. E., O, Neill M, Kim P. R, Fazekas A. Incidence of groin pain after metal-on-metal hip resurfacing. Clin. Orthop. 2010;468:392–399. doi: 10.1007/s11999-009-1133-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bartelt R. B, Yuan B. J, Trousdale R. T, Sierra R. J. The prevalence of groin pain after metal-on-metal total hip arthroplasty and total hip resurfacing. Clin. Orthop. 2010;468:2346–2356. doi: 10.1007/s11999-010-1356-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cobb J. P, et al. Why large-head metal-on-metal hip replacements are painful: the anatomical basis of psoas impingement on the femoral head-neck junction. J. Bone Joint Surg. Br. 2011;93:881–885. doi: 10.1302/0301-620X.93B7.26054. [DOI] [PubMed] [Google Scholar]
- 39.Alpert J. M, Kozanek M, Li G, Kelly B. T, Asnis P. D. Cross-sectional analysis of the iliopsoas tendon and its relationship to the acetabular labrum: an anatomic study. Am. J. Sports Med. 2009;37:1594–1598. doi: 10.1177/0363546509332817. [DOI] [PubMed] [Google Scholar]
- 40.Blomberg J. R, Zellner B. S, Keene J. S. Cross-sectional analysis of iliopsoas muscle-tendon units at the sites of arthroscopic tenotomies: an anatomic study. Am. J. Sports Med. 2011;39(58S-63S) doi: 10.1177/0363546511412162. [DOI] [PubMed] [Google Scholar]
- 41.Guicherd W, et al. Endoscopic or arthroscopic iliopsoas tenotomy for iliopsoas impingement following total hip replacement. A prospective multicenter 64-case series. Orthop. Traumatol. Surg. Res. OTSR. 2017;103:S207–S214. doi: 10.1016/j.otsr.2017.09.007. [DOI] [PubMed] [Google Scholar]
- 42.Filanti M, et al. The role of arthroscopy in the treatment of groin pain after total hip arthroplasty: our experience. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2016;26(1):28–33. doi: 10.5301/hipint.5000405. [DOI] [PubMed] [Google Scholar]