Abstract
Schwannoma is a soft tissue tumor that rarely presents in the foot. Patients are usually asymptomatic, but in some cases symptoms typically result from the mass effect and direct involvement of the nerve and surrounding tissue. We report on four consecutive cases. The first patient was a 57-years-old female that referred symptoms similar to the Morton’s neuroma with a mass arising from the medial plantar nerve. The second patient was treated for a schwannoma in the plantar area. The third case was a female with a schwannoma arising from the sural nerve and the fourth patient had a tumor arising from the medial plantar nerve. All patients underwent surgical excision and histological evaluation. No signs of neurological deficit or recurrence were observed at final follow-up. Purpose of the study was to define clinical features, optimal management and outcome of schwannomas of the foot, through an accurate review of the literature. (www.actabiomedica.it)
Keywords: soft tissue tumors, Schwannoma, foot, diagnosis, benign tumors, differential diagnosis, extremities, pain
Introduction
Schwannoma, also known as neurilemoma, is a benign encapsulated soft tissue tumor classified under the group of peripheral nerve sheath tumors (PNSTs) (1). Schwannoma is a well-circumscribed lesion, arising from Schwann cells of the peripheral nerve sheath (epineurium) (1). It represents about the 5% of all benign soft-tissue neoplasms, with low rate of local recurrence (less than 1%) (2). The malignant degeneration is extremely rare (3-5) but it is difficult to distinguish schwannomas from a malignant peripheral nerve sheath tumors (6). Traumas, Carney’s complex, and neurofibromatosis (NF) type 1 or 2 might play an etiological role in the development of this tumor (1, 7-9).
Schwannomas affect man and woman equally with peak age at diagnosis of 30-40 years, and are usually localized in skin or subcutaneous tissue (10). They are uncommonly found in the foot (11-13). In one single center retrospective review, only 10,3% (14 of 137) of the tumors were located in foot or ankle (13), whereas in the Rizzoli Institute experience, only 14 schwannomas out of 189 benign tumors of the foot have been treated from 1990 to 2007 (11). In another study, only 12 of 104 cases (11,5%) observed during a 32 years’ period, were located in the foot or ankle (12). The clinical presentation depends on the site and tumor volume: symptoms will typically result from the mass effect and direct involvement of the nerve and surrounding tissue. Most of the lesions are asymptomatic. The typical solitary tumors present as a slow growing painless mobile mass, which may have been present for at least one or two years (1, 4). The discovery of one schwannoma should be careful search for others. The imaging appearance of schwannoma is a not calcified tumor, clearly detectable with ultrasonography and MRI, while usually not appreciable with normal x-rays. There can be bone remodelling due to pressure and impingement from the tumor, without signs of bone invasion. Multinodular/plexiform schwannoma is an extremely rare variant (2%-5%) usually affecting skin or subcutaneous tissue of the head, neck and flexor surfaces of extremities (4, 6, 14). Most of these are small (maximal diameter less than 2 cm) originating from superficial nerves.
Aim of our study was to report four representative cases of schwannomas of the foot, describing clinical and imaging findings, type of treatment, oncologic and functional outcomes. Further objective was to critically analyze and compare our results with those reported in literature.
Material and methods
We retrospectively studied and report four consecutive patients with schwannoma of the foot observed in the same institution since 2000 to date: no history of trauma or previous pathological condition of the affected foots were observed.
Case 1
A 57-years-old female complaints right foot pain for 1 year. Symptoms were very similar to the Morton’s neuroma with pain and parestesia of the plantar region of the forefoot at the second intermetatarsal space. Radiographs showed no bone abnormalities or any tumor-like calcified masses whereas the MRI revealed an oval-shaped lesion of 1cm x 1.5 cm between 2nd and 3rd metatarsal bone (Figure 1A). A second MRI performed 1 year later (few days before surgery) did not show any significant increase of the tumor volume. Surgery was performed through a mini-invasive plantar approach. The gross appearance of the lesion was a round white-yellow mass of about 1 cm in diameter, encapsulated and well delimited to the other near tissues, strictly adherent to medial plantar nerve (Figure 1B). Histology showed a schwannoma with no evidence of malignant transformation (Figure 2). The patient was able to walk with some limitations and dysesthesia to the plantar aspect of the foot one month after surgery, whereas at two months of follow-up she comes back to her all day living activities.
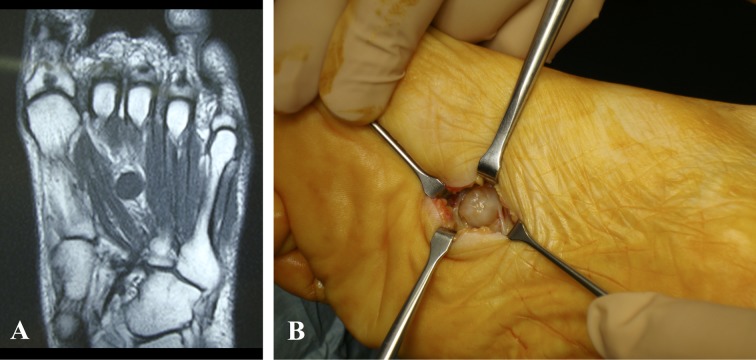
Figure 1.
Case 1. A) Axial T2-weighted image demonstrating a fusiform isogenous mass. B) Intraoperative finding of the well-circumscribed, encapsulated and solid mass along the medial plantar nerve
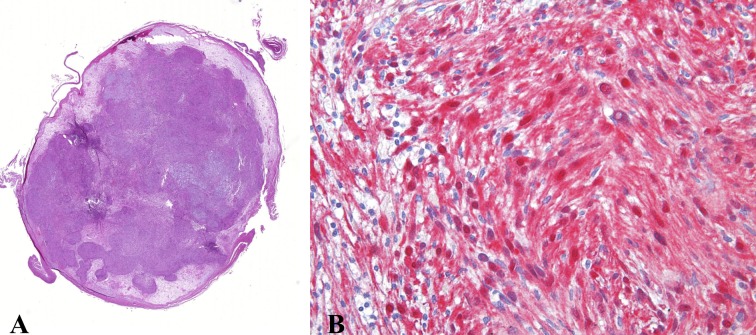
Figure 2.
Case 1. Histological feature exhibits A) low power transverse section through the mass showed a neurogenic, spindle cell proliferation with biphasic pattern of growth and prominent nuclear palisading. (hematoxylin and eosin stain, magnification 10×); B) The spindled cells arranged haphazardly within the loosely textured matrix. Classic pattern of Antoni B areas (Hematoxylin–eosin original magnification × 400)
Case 2
A 45-years-old male complaints right foot pain and swelling in the plantar aspect of the midfoot that prevent him to attend to his normal activities, including running. Plain radiographs and MRI were performed. MRI images were suggestive of a synovial angiomatosis mass due to proximity to vessels. The patient was operated on and the diagnosis of specimen was synovial angiomatosis. Six months later the patient complained the same symptoms and showed an antalgic supination of the foot. A new MRI revealed tumor-like tissue still present in the plantar region of the foot suspected for local recurrence. Histologic analysis after second operation revealed a schwannoma. Symptoms disappeared immediately after surgery and the patient was able to walk as soon as the surgical wound has healed. There was no sensory deficit on the sole of the foot. The patient come back to his activities of daily living three weeks later.
Case 3
A 58-years-old female complaints left foot pain in the last 4 years. She had stated a slow-growing swelling under the lateral malleolus. At the onset, she experienced pain with palpation of the mass (that was like a peanut), causing some difficulties during walk. MRI with and without contrast showed a mass arising from the sural nerve near the lateral malleolus. The tumor was completely removed, and definitive diagnosis was schwannoma. The recovery was fast without complication.
Case 4
A 35-years-old female was referred to our institution with a 2-year history of a slowly growing, painful mass in the medial aspect of the right ankle. The patient’s past medical history was unremarkable and there was no history of antecedent trauma. On physical examination, a poorly mobile, painful tender mass was noted (Figure 3A). Tinel sign was positive, with radiation of the pain into the plantar aspect of the foot. MRI demonstrated a fusiform lesion with iso-signal intensity on T1-weighted sequences and homogeneous high signal intensity on T2-weighted sequences (Figure 3B,C) along the course of the medial plantar nerve. Based on these features, a schwannoma was strongly suspected and the patient was scheduled for surgery. A surgical enucleation was performed under general anesthesia (Figure 3D,E), and the histological evaluation confirmed the diagnosis of schwannoma, with no signs of malignant features. The postoperative course was uneventful. After two weeks, the sutures were removed and she started progressive weight bearing. Patient referred excellent pain relief and no signs of local recurrence were observed up to final follow-up of 4 years.
Figure 3.
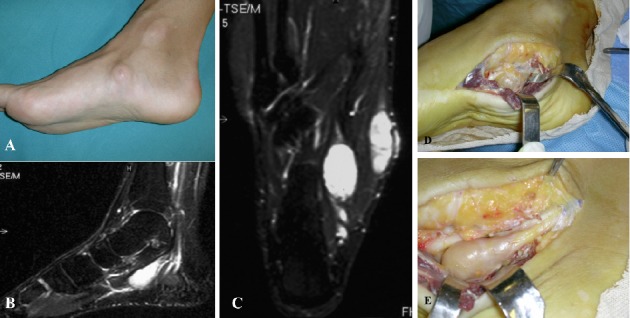
Case 4. A) Clinical photograph of the foot in lateral, non–weight-bearing view shows the presence of swelling on the medial aspect of the right foot. B) Sagittal T2-weighted MRI scan with fat suppression revealing an hyperintense homogeneous fusiform mass on medial aspect of the foot along the course of the medial plantar nerve. C) Coronal T2-weighted MRI scan with fat suppression high enhancement of the lesion. D) Intraoperative localization of the mass in the medial part of the foot. E) It is clearly shown the connection with the medial plantar nerve
Discussion
A search of the literature was done to identify patients who had been treated for their schwannoma of the foot. The English language and non-English language literature were searched in Pubmed using the «MeSH» “Neurilemmoma” and “Foot” with and without the terms «soft tissue tumors», «ankle», «benign» or «schwannoma» and in ISI Web of Knowledge database searching «schwannoma» as topic. The search was done using literature from 1996 to date (last two decades). The focus of each reference varied including: series of patients with soft tissue tumors of the foot, case reports and articles investigating specific forms of treatment of schwannoma. From the search of the literature we were able to find 51 cases of schwannomas of the foot from different articles and abstracts that were obtained and reviewed, and data were summarized in table 1 (4, 8-9, 11, 13-30).
Table 1.
Schwannoma of the foot. Systematic review of the literature from 1996 to 2017
| Author | Year | N. pts | Age | Gender | Nerve or site | NF | Variant | Treatment | Complications | Function or outcome |
| Ozdemir et al [15] | 1997 | 2 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Ikushima et al [16] | 1999 | 1 | 8 | M | Heel | - | Plexiform | Excision | - | Good |
| Bakotic et al [17] | 2001 | 8 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Odom et al [18] | 2001 | 1 | 74 | F | MP nerve | - | - | Excision | - | Good |
| Still et al [19] | 2001 | 1 | 55 | F | MP nerve | - | - | Excision | - | Good |
| Torossian et al [20] | 2001 | 1 | 30 | M | Heel | - | - | Excision | Need of flap reconstr. | Good |
| Mott et al [21] | 2003 | 1 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Mangrulkar et al [22] | 2007 | 1 | 37 | M | Foot (large mass) | - | - | Excision | - | LR (9 mos) |
| Boya et al [23] | 2008 | 1 | 20 | M | TP nerve | - | - | Excision | - | Good |
| Kwon et al [24] | 2009 | 1 | 72 | F | MP nerve | - | - | Excision | - | Good |
| Carvajal et al [13] | 2011 | 1 1 |
44 78 |
F F |
Foot Hindfoot |
- | - | Excision Excision0 |
- | Good Good |
| Jacobson et al [9] | 2011 | 1 | 65 | M | Midfoot | - | Plexiform | Excision | - | Good |
| Milnes et al [25] | 2012 | 1 | 73 | F | PT nerve | - | - | Excision | - | Good |
| Azevedo et al [26] | 2013 | 5 | n/a | n/a | n/a | - | - | Excision | n/a | LR- |
| Hallahan et al [27] | 2014 | 1 | 54 | F | PT nerve | - | - | Excision | Axonal tibial neuropathy | LR- |
| Kallini et al [28] | 2014 | 1 | 25 | M | Heel | - | - | Excision | n/a | n/a |
| Kellner et al [29] | 2014 | 1 1 1 |
n/a n/a n/a |
n/a n/a n/a |
PT nerve PT nerve Sural nerve | - | - | Excision Excision Excision |
n/a n/a n/a |
n/a n/a n/a |
| Li et al [8] | 2014 | 1 | 19 | F | CPD nerve | - | Plexiform | Excision | - | Good |
| Mohammed et al [4] | 2014 | 1 1 |
38 11 |
F M |
Heel subcutaneous Midfoot | - | Plexiform Plexiform |
Excision Excision |
- | Good Good |
| Ruggieri et al [11] | 2014 | 14 | n/a | n/a | Hindfoot (6) Midfoot (8) | n/a | n/a | n/a | n/a | n/a |
| Nishio et al [14] | 2015 | 1 | 32 | F | PT nerve | - | Plexiform | Excision | - | Good |
| Min et al [30] | 2015 | 1 | 38 | M | MP nerve | Type III* | - | Excision | - | Good |
NF: Neurofibromatosis; LR: local recurrence; CPD: Common Plantar Digital nerve; PT: Posterior Tibial; MP: Medial Plantar; n/a: not available; ° Recurrent lesion * Schwannomatosis has been considered as Type III NF
Clinical observation. Schwannomas are soft tissue tumors that cause a variability of symptoms related to their location. Pain and/or numbness are the primary complaints in most of the cases, and the precise distribution of these symptoms allowed accurate localization of the tumor to a particular peripheral nerve, especially when they are superficial. Clinical examination is very important: the presence of lumps painful at the compression along the course of peripheral nerve it’s a common finding. The clinical diagnosis is usually straightforward, but may be delayed for many years in a slow-growing schwannoma of the foot (13). In a study on 137 patients surgically treated for a PNST in a 16-years’ experience, comparing 14 cases with PNST of the foot with those of other site, they found a significant female predilection and a smaller tumor volume (13). In our literature analysis, we found a 55% of cases affecting females, without a significant difference.
Radiographic features. Standard X-rays are often negative in soft tissue tumors. Ultrasonography and MRI examinations are valuable diagnostic tools that allow direct evaluation of mostly superficial-lying tumors. MRI is extremely useful in defining the extent of deep-seated schwannomas and for identification of the nerve of origin (6, 22). The lesion typically appears as ovalar shaped mass with iso-signal intensity relative to skeletal muscle on T1-weighted images and high signal intensity on T2-weighted images (6). However, the tumor stands out very well from surrounding tissues. In some cases, degenerative changes can be present, including cyst formation, calcification, hemorrage and fibrosis (6, 31). The main differential diagnosis includes synovial cyst, neurofibroma, low-flow venous malformations, lymphangioma or high grade sarcomas such as fibrosarcoma, leiomyosarcoma or synovial sarcoma (11, 14). MRI with gadolinium is useful to discriminate a schwannoma and a synovial cyst when a nerve connected to the lesion is not clearly showed (6). Plexiform neurofibromas are essentially pathognomonic of neurofibromatosis type 1 (NF1) and can be present at birth or develop within the first year of life (32). Differential diagnosis is important considering the risk of malignant transformation of the neurofibroma (4). Previous studies have found specific MRI features that can be used for differentiating between schwannomas and neurofibromas, even if the definite diagnosis should be confirmed by histological examination, especially in the plexiform variant (8). High grade sarcomas of the extremities could present with indolent growing or symptoms, mimicking benign soft tissue lesions (27, 33). In our experience, biopsy should be done with ultrasonography guidance through the surgical approach of definitive surgery, avoiding excisional biopsies as more as possible (34).
Treatment indications and complications. Asymptomatic patients with small tumors should be only monitored clinically. The reason to operate a patient with benign neurogenic tumors should be based on the balance between the risk and benefit of the surgery. Surgical excision is necessary for large tumors arising from major peripheral nerves in the extremities and in case of compressive symptoms (35). In the foot, also a small schwannoma affecting the plantar aspect of the foot become symptomatic during walking and jumping (as reported in our case 1 and 2) (14). Surgery consists of excision or intracapsular enucleation of the lesion after incision of the epineurium, which allows sparing of the parent nerve owing to its eccentric location, preserving the neurological function (14). It is important to expose adequately the affected nerve with sufficient proximal and distal margin. The exposure will allow for exact visualization of the tumor and for intraoperative nerve stimulation and monitoring. Obviously, the use of intraoperative magnifying glass and a gentle manipulation of the nerve, help to preserve the continuity and the function of the nerve. The patient should be informed about a possible transitory partial loosening of sensory or motor function of the nerve, as happened in our case 1.
Outcome. Adequate surgical excision of schwannomas in the foot and ankle is associated with minimal postoperative morbidity. Local recurrence is rare even if it is not an uncommon finding associated with plexiform variants (13, 36). It has been attribuited to incomplete resection, a focal lack of thick encapsulation, and irregular, finger-like tumor growth (9, 13). However recurrent schwannomas can be successfully treated with revisional surgery although the small sample size reported in literature (13, 22). Patients with identified plexiform schwannomas should be educated about the risk of recurrence. Malignant transformation of schwannomas is extremely rare and has only be reported in less than 15 cases in literature, usually associated with NF-2, Carney complex I and schwannomatosis (4-5).
Conclusions
Schwannoma rarely affect the foot. We have described four cases with different localizations: between the 2nd and 3rd metatarsal, between the muscle quadrauts of the sole and flexor brevis of the toes and under the lateral malleolus. MRI is a clinically useful modality in the evaluation and detection of deep-seated schwannoma, even if not always pathognomonic. A complete workup and examination will lead to the ideal diagnosis and treatment. Biopsy with histological examination should be performed in doubtful cases. Surgical excision with careful dissection from the nerve, seems to be an acceptable treatment for this peculiar condition affecting the foot.
References
- 1.Ferner RE, O’Doherty MJ. Neurofibroma and schwannoma. Curr Opin Neurol. 2002;15:679–84. doi: 10.1097/01.wco.0000044763.39452.aa. [DOI] [PubMed] [Google Scholar]
- 2.Pilavaki M, Chourmouzi D, Kiziridou A, Skordalaki A, Zarampoukas T, Drevelengas A. Imaging of peripheral nerve sheath tumors with pathologic correlation: pictorial review. Eur J Radiol. 2004;52:229–239. doi: 10.1016/j.ejrad.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Rockwell GM, Thoma A. Schwannoma of the hand and wrist. Plast Reconstr Surg . 2003;111(3):1227–32. doi: 10.1097/01.PRS.0000046039.28526.1A. [DOI] [PubMed] [Google Scholar]
- 4.Mohammed SA, Pressman MM, Schmidt B, Babu N. Case presentations and review of plexiform schwannoma in the foot. J Foot Ankle Surg. 2014 Mar-Apr;53(2):179–85. doi: 10.1053/j.jfas.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 5.Carroll SL. Molecular mechanisms promoting the pathogenesis of Schwann cell neoplasms. Acta Neuropathol. 2012;123:321–348. doi: 10.1007/s00401-011-0928-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stramare R, Beltrame V, Gazzola M, Gerardi M, Scattolin G, Coran A, Faccinetto A, Rastrelli M, Rossi CR. Imaging of soft tissue tumors. J Magn Reson Imaging. 2012;37:791–804. doi: 10.1002/jmri.23791. [DOI] [PubMed] [Google Scholar]
- 7.Sasaki M, Aoki M, Yoshimine T. Mobile schwannoma of the cauda equina incarcerated following caudal migration after trauma—case report. Neurol Med Chir. 2011;51:710–712. doi: 10.2176/nmc.51.710. [DOI] [PubMed] [Google Scholar]
- 8.Li XN, Cui JL, Christopasak SP, Kumar A, Peng ZG. Multiple plexiform schwannomas in the plantar aspect of the foot: case report and literature review. BMC Musculoskelet Disord. 2014 Oct 11;15:342. doi: 10.1186/1471-2474-15-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobson JM, Felder JM 3rd, Pedroso F, Steinberg JS. Plexiform schwannoma of the foot: a review of the literature and case report. J Foot Ankle Surg. 2011 Jan-Feb;50(1):68–73. doi: 10.1053/j.jfas.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Iwashita T, Enjoji M. Plexiform neurilemmoma: a clinicopathological and immunohistochemical analysis of 23 tumours from 20 patients. Virchows Arch A Pathol Anat Histopathol. 1987;411(4):305–9. doi: 10.1007/BF00713373. [DOI] [PubMed] [Google Scholar]
- 11.Ruggieri P, Angelini A, Jorge FD, Maraldi M, Giannini S. Review of foot tumors seen in a university tumor institute. J Foot Ankle Surg. 2014 May-Jun;53(3):282–5. doi: 10.1053/j.jfas.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 12.Kehoe NJ, Reid RP, Semple JC. Solitary benign peripheral-nerve tumours: review of 32 years experience. J Bone Joint Surg Br. 1995;77:497–500. [PubMed] [Google Scholar]
- 13.Carvajal JA, Cuartas E, Qadir R, Levi AD. Peripheral nerve sheath tumors of the foot and ankle. Foot Ankle Int. 2011;32:163–167. doi: 10.3113/FAI.2011.0163. [DOI] [PubMed] [Google Scholar]
- 14.Nishio J, Mori S, Nabeshima K, Naito M. Successful enucleation of large multinodular/plexiform schwannoma of the foot and ankle. Springerplus. 2015;17(4):260. doi: 10.1186/s40064-015-1087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ozdemir HM, Yildiz Y, Yilmaz C, Saglik Y. Tumors of the foot and ankle: analysis of 196 cases. J Foot Ankle Surg. 1997 Nov-Dec;36(6):403–8. doi: 10.1016/s1067-2516(97)80089-0. [DOI] [PubMed] [Google Scholar]
- 16.Ikushima K, Ueda T, Kudawara I, Nakanishi K, Yoshikawa H. Plexiform schwannoma of the foot. Eur Radiol. 1999;9:1653–1655. doi: 10.1007/s003300050904. [DOI] [PubMed] [Google Scholar]
- 17.Bakotic BW, Borkowski P. Primary soft-tissue neoplasms of the foot: the clinicopathologic features of 401 cases. J Foot Ankle Surg. 2001 Jan-Feb;40(1):28–35. doi: 10.1016/s1067-2516(01)80038-7. [DOI] [PubMed] [Google Scholar]
- 18.Odom RD, Overbeek TD, Murdoch DP, Hosch JC. Neurilemoma of the medial plantar nerve: a case report and literature review. J Foot Ankle Surg. 2001 Mar-Apr;40(2):105–9. doi: 10.1016/s1067-2516(01)80052-1. [DOI] [PubMed] [Google Scholar]
- 19.Still GP. Neurilemoma of the medial plantar nerve: a case report. J Foot Ankle Surg. 2001 Jul-Aug;40(4):236–9. doi: 10.1016/s1067-2516(01)80024-7. [DOI] [PubMed] [Google Scholar]
- 20.Torossian JM, Augey F, Salle M, Beziat JL. Giant foot schwannoma. Br J Plast Surg. 2001 Jan;54(1):74–6. doi: 10.1054/bjps.1999.3478. [DOI] [PubMed] [Google Scholar]
- 21.Mott R, Dellon AL. Multiple Schwannomas of the foot: Case report and strategy for treatment. J Amer Podiatric Med Assn. 2003;93:51–57. doi: 10.7547/87507315-93-1-51. [DOI] [PubMed] [Google Scholar]
- 22.Mangrulkar VH, Brunetti VA, Gould ES, Howell N. Unusually large pedal schwannoma. J Foot Ankle Surg. 2007 Sep-Oct;46(5):398–402. doi: 10.1053/j.jfas.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Boya H, Ozcan O, Oztekin HH. Tarsal tunnel syndrome associated with a neurilemoma in posterior tibial nerve: a case report. Foot (Edinb) 2008 Sep;18(3):174–7. doi: 10.1016/j.foot.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 24.Kwon JH, Yoon JR, Kim TS, Kim HJ. Peripheral nerve sheath tumor of the medial plantar nerve without tarsal tunnel syndrome: a case report. J Foot Ankle Surg. 2009 Jul-Aug;48(4):477–82. doi: 10.1053/j.jfas.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 25.Milnes HL, Pavier JC. Schwannoma of the tibial nerve sheath as a cause of tarsal tunnel syndrome—a case study. Foot (Edinb) 2012;22:243–246. doi: 10.1016/j.foot.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 26.Azevedo CP, Casanova JM, Guerra MG, Santos AL, Portela MI, Tavares PF. Tumors of the foot and ankle: a single-institution experience. J Foot Ankle Surg. 2013 Mar-Apr;52(2):147–52. doi: 10.1053/j.jfas.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Hallahan K, Vinokur J, Demski S, Faulkner-Jones B, Giurini J. Tarsal tunnel syndrome secondary to schwannoma of the posterior tibial nerve. J Foot Ankle Surg. 2014 Jan-Feb;53(1):79–82. doi: 10.1053/j.jfas.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 28.Kallini JR, Khachemoune A. Schwannoma of the left foot: a brief overview with focus on associated clinical syndromes. J Am Podiatr Med Assoc. 2014 Sep-Oct;104(5):535–8. doi: 10.7547/0003-0538-104.5.535. [DOI] [PubMed] [Google Scholar]
- 29.Kellner CP, Sussman E, Bar-David T, Winfree CJ. Schwannomas of the foot and ankle: a technical report. J Foot Ankle Surg. 2014 Jul-Aug;53(4):505–10. doi: 10.1053/j.jfas.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 30.Min HJ, Kim KC, Jun SH, Lee YG. Schwannomatosis on a single foot: a case report. Foot Ankle Spec. 2015 Jun;8(3):226–9. doi: 10.1177/1938640014565047. [DOI] [PubMed] [Google Scholar]
- 31.Gruber H, Glodney B, Bendix N, Tzankov A, Peer S. High-resolution ultrasound of peripheral neurogenic tumors. Eur Radiol. 2007;17:2880–8. doi: 10.1007/s00330-007-0645-7. [DOI] [PubMed] [Google Scholar]
- 32.Korf BR. Plexiform neurofibromas. Am J Med Genet. 1999;89:31–37. doi: 10.1002/(sici)1096-8628(19990326)89:1<31::aid-ajmg7>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 33.Angelini A, Barastegui D, Gambarotti M, Ruggieri P. Leiomyosarcoma of the hand. Handchir Mikrochir Plast Chir. 2015 Apr;47(2):139–41. doi: 10.1055/s-0034-1395605. [DOI] [PubMed] [Google Scholar]
- 34.Mavrogenis AF, Angelini A, Errani C, Rimondi E. How should musculoskeletal biopsies be performed? Orthopedics. 2014 Sep;37(9):585–8. doi: 10.3928/01477447-20140825-03. [DOI] [PubMed] [Google Scholar]
- 35.Carter J, Ben-Ghashir N, Chandrasekar C.R. Giant Schwannoma of the medial plantar nerve The Foot 26. 2016:4–6. doi: 10.1016/j.foot.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 36.Kim DH, Ryu S, Tiel RL, Kline DG. Surgical management and results of 135 tibial nerve lesions at the Louisiana State University Health Sciences Center. Neurosurgery. 2003;53:1114–1124. doi: 10.1227/01.neu.0000089059.01853.47. [DOI] [PubMed] [Google Scholar]