Abstract
Background and aim: The incidence of hip osteoarthritis (OA) is increasing in parallel with the aging of the population. The aim of this study is to report the efficacy of an ultrasound-guided intra-articular (IA) hip injection of a single dose of high-weight hyaluronic acid (HA) (2500 kDa) at a follow-up of 12 months. Materials and Methods: 226 patients older than 40 years of age affected by painful hip OA (Kellgren-Lawrence stage 1-2-3) were treated from January 2012 to December 2015 with viscosupplementation. Patients were clinically evaluated before injection (T0) and after 3 months (T3), 6 months (T6) and 1 year (T3) through the WOMAC scale and Harris Hip Score (HHS). Results: During the follow-up period no patients underwent to hip surgery or need adjunctive IA injection of HA. No adverse effects were registered. An improvement in WOMAC and HHS was observed in all patients after treatment. Results showed that patients with grade 2 of osteoarthritis had the higher delta of change in the scores. Discussion: Ultrasound-guided with high weight IA HA injection could be a possibility of treatment in the symptomatic osteoarthritic hip. Subjects with a moderate grade of osteoarthritis (Kellgren-Lawrence stage 2) represent the group that could report the maximum benefits from viscosupplementation. (www.actabiomedica.it)
Keywords: hip, osteoarthritis, viscosupplementation, hyaluronic acid, ultrasound
Introduction
Hip pain, which could be the consequence of different pathologies, is reported by 19.2% [95% confidence interval (CI) 17.9-20.6] of people aged 65 years and older (1-3). The incidence of hip OA is increasing in parallel with the aging of the population and is estimated at between 47.3 (95% CI 27.8-66.8) (4) and 88/100 000 patient-years (95% CI 65-101) (5). Optimal management of this disease requires a combination of non-pharmacological and pharmacological modalities, thus delaying or avoiding surgical treatments (osteotomy and/or total hip prosthesis) (6-10). HA was initially isolated in 1934 by Karl Meyer in the vitreous humor. It is a polysaccharide macromolecule, a glycosaminoglycan of high molecular weight (MW) composed of repetitions of disaccharides of glucuronic acid and N-acetylglucosamine; it is a constituent of synovial fluid in normal joints and is synthesized by chondrocytes and synoviocytes (5). HA has complex biological properties that could explain its analgesic effects (anti-inflammatory by inhibiting the formation and release of prostaglandin, immunomodulatory in situ), irrespective of its mechanical action on the joint fluid. The concentration of HA in an arthritic joint has been found to decrease to 50-33% of normal levels, and includes a reduction in molecular size with a consequent decrease in elasticity and viscosity of the synovial fluid (11). In 1997 HA received Food and Drug Administration (FDA) approval in humans and it was initially used in the treatment of knee OA. This procedure should improve the physiological environment of an osteoarthritic joint by restoring its protective viscoelasticity (12-15), reducing friction and improving mobility (16, 17). Intra-articular hip injections have been attempted for a wide variety of hip disorders, including OA, rheumatoid arthritis (18), acetabular labral tears, and femoral-acetabular impingement (19, 20). The injection of hyaluronic acid in the joint space allows to reach a high and durable concentration with low doses. Evidences suggest that this is the best conservative therapy for hip OA before surgery, and it can act on pain relief without modifying the morphological structure of the pathological hip and natural history of the disease. However, there is no general consensus on number and timing of hip injections and type of HA to be used. The aim of this study is to analyze the efficacy and safety of ultrasound-guided IA injection of a single dose of high-weight HA (2500 kDa) in patients affected by hip OA at a follow-up of 12 months.
Materials and Methods
This study was conducted in accordance with the principles of Declaration of Helsinki. All patients signed informed consent about the treatment they were subjected and the processing of their personal data.
Patients treated from January 2012 to December 2017 with an ultrasound-guided IA injection of high weight HA (figure 1) for hip osteoarthritis were scheduled for the present study.
Figure 1.

Ultrasound image with needle (white arrow) around the femoral head (black arrow)
Inclusion criteria were also age more than 40 years, mono- or bilateral hip OA with X-ray proof of at least partially preserved joint space (Kellgren-Lawrence stage 1-2-3) (21), good or full joint mobility, and hip disease persisting for at least 3 months. Exclusion criteria were: the presence of severe hip OA for which it was no longer possible to recognize radiographic joint space (Kellgren-Lawrence stage 4), of inflammatory, autoimmune and septic disease and of previous hip surgeries. All patients received a single high-weight (2500 kDa) injection of 2.5% sodium hyaluronate (60 mg/4 mL).
All procedures were performed with an ultrasound guidance in accordance with the technique suggested by Migliore et al. (22). All subjects were clinically evaluated before injection (T0) and after 3 months (T3), 6 months (T6) and 1 years (T12) utilizing the WOMAC scale and HHS.
Results were considered for statistical analysis, which was performed with JASP (software 0.7.5). At each study time, mean, standard deviation and median endpoints were calculated. For the same endpoint, comparisons were made at different study times using Student’s t test for paired samples. Moreover, statistical comparisons were performed for the different groups of patients with different grade of osteoarthritis. Results were considered statistically significant for values of p<0.05.
Results
Overall, 226 subjects (135 female and 91 male) were included for the analysis of the data. The mean age was 64.2 years (SD 9.82, range 42-85) and the mean BMI was 25.8 (SD 3.66, range 18.25-32.95). Considering Kellgren-Lawrence classification 35 patients showed a Grade I of OA, 104 a Grade 2 and 87 a Grade III.
The results of WOMAC scale and HHS at T0, T3, T6 and T12 are summarized in table 1 and 2 and graph 1 and 2.
Table 1.
WOMAC results at T0, T3, T6 and T12
| WOMAC_T0 | WOMAC_T3 | WOMAC_T6 | WOMAC_T12 | |
| Valid | 74 | 74 | 74 | 74 |
| Missing | 0 | 0 | 0 | 0 |
| Mean | 62.20 | 52.86 | 48.05 | 50.34 |
| Std. Error of Mean | 1.973 | 1.782 | 1.780 | 2.017 |
| Median | 65.00 | 52.50 | 45.00 | 47.50 |
| Mode | 72.00 | 31.00 | 28.00 | 35.00 |
| Std. Deviation | 16.97 | 15.33 | 15.31 | 17.35 |
| Skewness | -0.2059 | 0.1181 | 0.2398 | 0.3094 |
| Std. Error of Skewness | 0.2792 | 0.2792 | 0.2792 | 0.2792 |
| Kurtosis | -1.258 | -0.8432 | -0.8696 | -1.003 |
| Std. Error of Kurtosis | 0.5517 | 0.5517 | 0.5517 | 0.5517 |
| Minimum | 33.00 | 26.00 | 23.00 | 21.00 |
| Maximum | 88.00 | 85.00 | 78.00 | 84.00 |
Table 2.
HHS results at T0, T3, T6 and T12
| HHS_T0 | HHS_T3 | HHS_T6 | HHS_T12 | |
| Valid | 74 | 74 | 74 | 74 |
| Missing | 0 | 0 | 0 | 0 |
| Mean | 57.36 | 70.16 | 75.13 | 72.50 |
| Std. Error of Mean | 1.716 | 1.646 | 1.515 | 1.710 |
| Median | 62.00 | 73.41 | 80.50 | 77.00 |
| Mode | 72.00 | 84.00 | 87.00 | 84.00 |
| Std. Deviation | 14.76 | 14.16 | 13.03 | 14.71 |
| Skewness | -0.5273 | -0.7459 | -0.9825 | -0.9874 |
| Std. Error of Skewness | 0.2792 | 0.2792 | 0.2792 | 0.2792 |
| Kurtosis | -0.9889 | -0.4125 | 0.03261 | 0.1737 |
| Std. Error of Kurtosis | 0.5517 | 0.5517 | 0.5517 | 0.5517 |
| Minimum | 24.80 | 35.20 | 41.65 | 35.20 |
| Maximum | 73.15 | 87.00 | 90.00 | 90.00 |
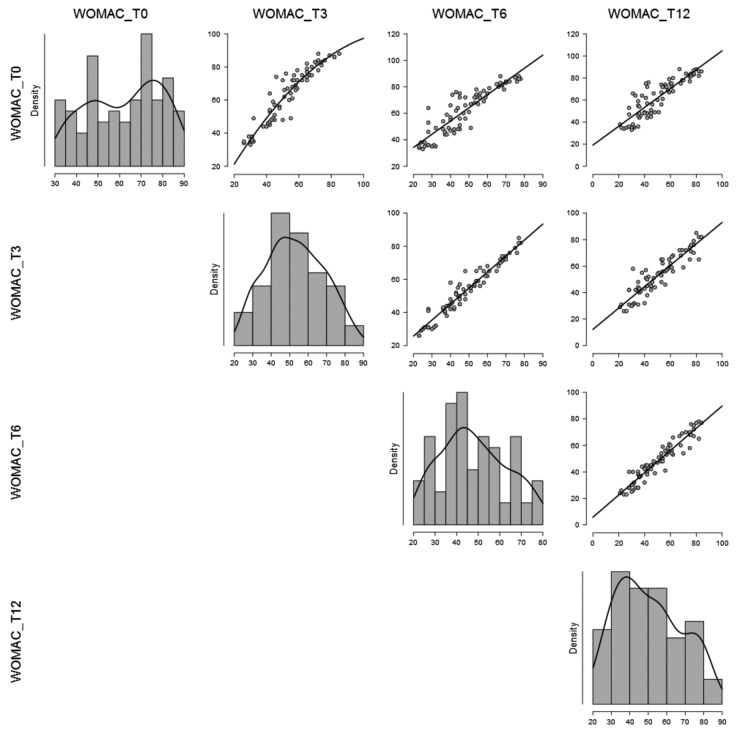
Graph 1.
Density of WOMAC global scores
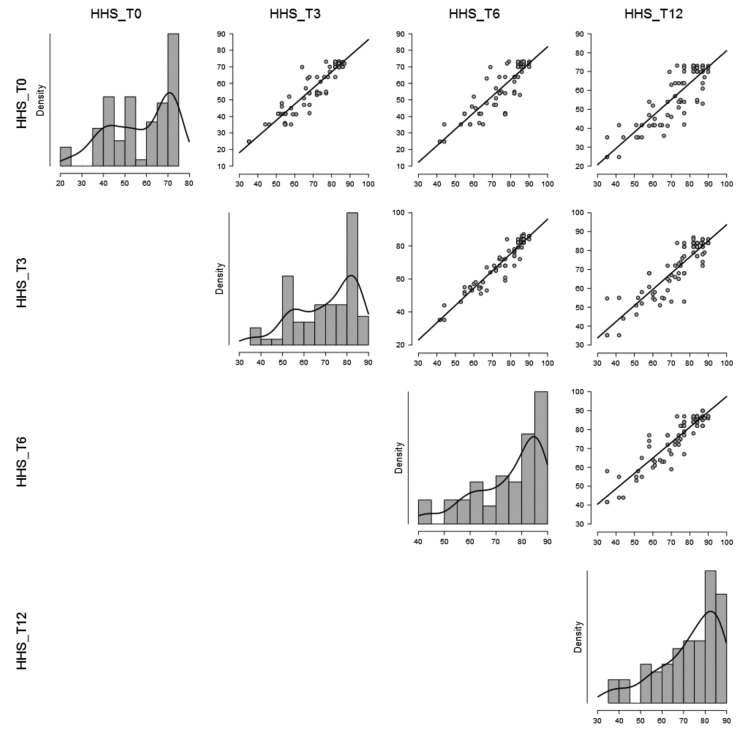
Graph 2.
Density of HHS global scores
Statistical analysis showed significant improvements for WOMAC scale and HHS between results before (T0) and after HA injection (T3, T6 and T12) (p<0.001).
No patients had adverse effects, underwent to other surgical procedures and/or need adjunctive IA injection of HA.
For each group of Kellgren-Lawrence classification a separate analysis was performed and the scores were separately calculated (graph 3 and 4). Considering the delta of change between T0 and T3 for WOMAC and Harris Hip Score, the higher was documented in patients with grade 2 of osteoarthritis.
Graph 3.
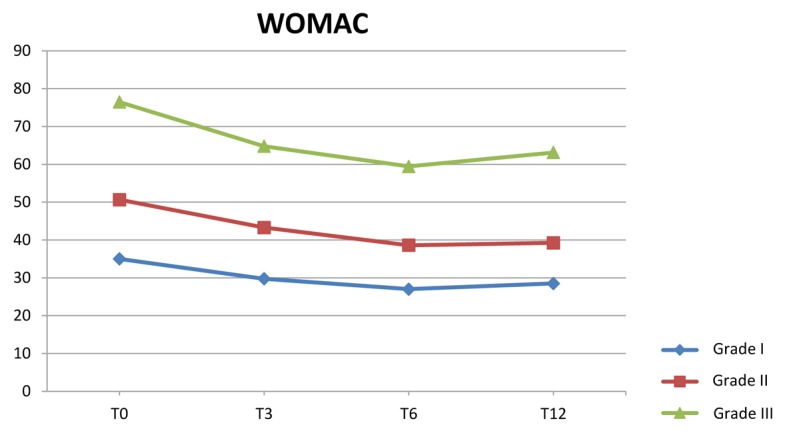
WOMAC scale results at T0, T3, T6 and T12 in different stages of OA
Graph 4.
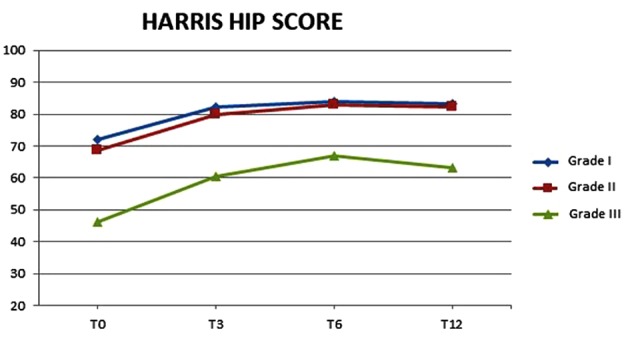
HHS results at T0, T3, T6 and T12 in different stages of OA
Discussion
OA can affect all the synovial joints, but knee and hip are the most frequent localizations. Although its incidence is higher in elderly, this pathology is also observed in young adults, especially in the case of intense sporting and working activities and following articular pelvic fractures (22). It is estimated that 25-30% of the population over 45 years of age is affected by a form of OA. Hyaluronic acid plays an important role in lubrication, shock absorption and visco-elastic behaviour of synovial fluid, whose rheological properties confer the characteristic of reducing mechanical stress on the joint (23).
At the beginning of the 90s, the Hungarian doctor Endre Alexander Balazs hypothesized that infiltrations with exogenous hyaluronic acid in patients suffering from OA could restore the visco-elasticity of the synovial fluid (11).
The concept of viscosupplementation was subsequently developed because of the scientific evidence that the rheological properties of the synovial fluid were altered in OA and that these changes were related to the qualitative modification and quantitative decrease of hyaluronic acid (14). It has been demonstrated that infiltrations with hyaluronic acid are effective in this pathology, thus determining the control of pain and improving joint function (20). In addition, exogenous derivatives seem to have biological activities such as the induction of endogenous high molecular weight hyaluronic acid synthesis, interaction with pain receptors and inhibition of pro-inflammatory mediators (11). Lùrati et al. (25) studied the effects of HA viscosupplementation on peripheral T cells in knee and hip OA and they showed that HA injection results in a decrease in proinflammatory T cells concentrations. In particular, HA can reduce synovial inflammation and restore the rheological properties of synovial fluid.
The significant results obtained in the infiltrative treatment of other degenerative joint diseases, such as knee OA (24), have led the scientific community to identify new reliable therapeutic patterns also for symptomatic osteoarthritis of the hip. Even if hip viscosupplementation is certainly characterized by a greater technical difficulty than the knee one, given the deep anatomical position of the joint and the presence of the femoral vascular-nervous bundle that require the preferential use of an ultrasound guide, results for hip viscosupplementation are usually encouraging. Dallari et al. (26) compared Platelet Rich Plasma (PRP) injections to HA or their association (PRP1HA) at 6 and 12 months follow-up. All intra-articular injections lead to a significant clinical and functional improvement, with no significant differences between the three methods of treatment. Battaglia et al. (27) combined HA and PRP injections following a specific protocol for moderate to severe hip OA (4 injections), and they performed VAS and radiological evaluation after 1, 3, 6 and 12 months. The results showed that in 93.7% of cases there was a significant reduction of subjective pain (VAS scores) but consumption of NSAIDs was greater in patients who received the combined therapy. Migliore et al. (22) compared HA injections to mepivacaine at 6 months follow-up (2 injections): patients in the HA group exhibited a significantly reduced Lequesne’s algofunctional index and VAS at 3 and 6 months after treatment when compared with the local anesthetic group. Conrozier et al. (28) assessed the clinical response of patients presenting with symptomatic hip osteoarthritis to the first intra-articular HA injection at 3 months of follow-up (up to four injections according to symptoms). Clinical response was defined as a 50% reduction from baseline in the Lequesne index one month after treatment. The response rate was 50% after the first injection and about half of the patients experienced significant pain relief during the 3 months following a single injection, and some of the patients who did not respond to the first injection received significant benefit from a second one.
On the opposite, other results are not so well interpretable. Richette et al. (29) performed a single injection of HA or placebo. VAS and WOMAC were evaluated after 3 months and compared to baseline. The results showed that there was no significant difference in terms of efficacy after one injection of HA compared with placebo in patients with hip osteoarthritis. Furthermore, an ideal hyaluronic acid derivative, by molecular weight, density and duration of action, has not yet been identified.
Some Authors compared the efficacy of lower and higher molecular weight viscosupplementation in the treatment of hip OA.
Tikiz et al. (30) performed three hip injections (one injection per week), and evaluated VAS scale, WOMAC and Lequesne index after 1, 3 and 6 months. Both types of visco-supplementation produced a significant clinical improvement during the 6-month follow-up period, with no significant difference between higher and lower molecular weight hyaluronic acid. Atchia et al. (31) reported no significant improvement in pain and function after a single high molecular weight HA injection in low grade hip OA when compared to standard care with no injections or to saline or non animal stabilized HA. This suggests that high molecular weight hyaluronic acids may not have a role to play in low grade hip osteoarthritis.
The results of this study suggest that the use of a preparation with high molecular weight hyaluronic acid allows to obtain satisfactory improvements in pain and joint function with a single infiltration (32).
No patients had adverse effects, underwent to other surgical procedures and/or needs adjunctive IA injection of HA, thus demonstrating the validity and durability of the treatment over follow-up time.
However, several other therapeutic schemes are described which suggest the use of low or medium molecular weight hyaluronic acid, with a higher frequency of infiltrative sessions. The results, in relation to different situations, are contrasting and not entirely appreciable (33).
As reported by the literature, in patients assessed with grade 1 Kellgren-Lawrence OA, the overall improvement twelve months after the infiltration is lower than that measured for grades 2 and 3 (34,35).
This study has several limitations which includes the low number of participants, the absence of a control group, the absence of a blinded methodology, the low duration of follow-up. However, this report proved the efficacy of ultrasound guided high weight IA HA injection for hip osteoarthritic treatment.
Conclusions
Authors can affirm that a single ultrasound-guided viscosupplementation with high weight IA HA injection could be a possibility in the symptomatic treatment of hip osteoarthritis. Subjects with a moderate grade of osteoarthritis seem to represent the group that could report the maximum benefits from the procedure.
References
- 1.Pogliacomi F, Costantino C, Pedrini MF, Pourjafar S, De Filippo M, Ceccarelli F. Anterior groin pain in athlete as consequence of bone diseases: aetiopathogenensis, diagnosis and principles of treatment. Medicina dello Sport. 2014;67(1):1–27. [Google Scholar]
- 2.Pogliacomi F, Costantino C, Pedrini MF, Pourjafar S, De Filippo M, Ceccarelli F. Anterior groin pain in athletes as a consequence of intra-articular diseases: aetiopathogenensis, diagnosis and principles of treatment. Medicina dello Sport. 2014;67(3):341–68. [Google Scholar]
- 3.Pogliacomi F, Calderazzi F, Paterlini M, Pompili M, Ceccarelli F. Anterior iliac spines fractures in the adolescent athlete: surgical or conservative treatment? Medicina dello Sport. 2013;66(2):231–40. [Google Scholar]
- 4.Tait RC, Chibnall JT. Physician judgments of chronic pain patients. Soc Sci Med. 1997;45:1199–205. doi: 10.1016/s0277-9536(97)00033-6. [DOI] [PubMed] [Google Scholar]
- 5.Wilson MG, Michet CJ Jr, Ilstrup DM, Melton LJ 3rd. Idiopathic symptomatic osteoarthritis of the hip and knee: a population-based incidence study. Mayo Clin Proc. 1990;65(9):1214–21. doi: 10.1016/s0025-6196(12)62745-1. [DOI] [PubMed] [Google Scholar]
- 6.Pogliacomi F, Stark A, Wallensten R. Periacetabular osteotomy: good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthopaedica. 2005;76(1):67–74. doi: 10.1080/00016470510030346. [DOI] [PubMed] [Google Scholar]
- 7.Pogliacomi F, De Filippo M, Costantino C, Wallensten R, Soncini G. 2006: the value of pelvic and femoral osteotomies in hip surgery: up to date. Acta Biomed. 2007;78(1):60–70. [PubMed] [Google Scholar]
- 8.Pogliacomi F, Stark A, Vaienti E, Wallensten R. Periacetabular osteotomy of the hip: the ilio-inguinal approach. Acta Biomed. 2003;74(1):38–46. [PubMed] [Google Scholar]
- 9.Pogliacomi F, Paraskevopoulos A, Costantino C, Marenghi P, Ceccarelli F. Influence of surgical experience in the learning curve of a new approach in hip replacement: ant-erior mini-invasive vs standard lateral. Hip International. 2012;22(5):555–61. doi: 10.5301/HIP.2012.9710. [DOI] [PubMed] [Google Scholar]
- 10.Pogliacomi F, De Filippo M, Paraskevopoulos A, Alesci M, Marenghi P, Ceccarelli F. Mini-incision direct lateral approach versus anterior mini-invasive approach in total hip replacement: results 1 year after surgery. Acta Biom. 2012;83(2):114–21. [PubMed] [Google Scholar]
- 11.Balazs EA, Denlinger JL. Viscosupplementation: a new concept in the treatment of osteoarthritis. J Rheumatol. 1993;39:3–9. [PubMed] [Google Scholar]
- 12.Laurent TC, Laurent UB, Fraser JR. The structure and function of hyaluronan: An overview. Immunol Cell Biol. 1996;74(2):A1–7. doi: 10.1038/icb.1996.32. [DOI] [PubMed] [Google Scholar]
- 13.Fraser JR, Laurent TC, Laurent UB. Hyaluronan: its nature, distribution, functions and turnover. J Intern Med. 1997;242(1):27–33. doi: 10.1046/j.1365-2796.1997.00170.x. [DOI] [PubMed] [Google Scholar]
- 14.Henrotin Y, Raman R, Richette P, Bard H, Jerosch J, Conrozier T, et al. Consensus statement on viscosupplementation with hyaluronic acid for the management of osteoarthritis. Semin Arthritis Rheum. 2015;45:140–9. doi: 10.1016/j.semarthrit.2015.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Hui AY, McCarty WJ, Masuda K, Firestein GS, Sah RL. A systems biology approach to synovial joint lubrication in health, injury, and disease. Wiley Interdiscip Rev Syst Biol Med. 2012;4:15–37. doi: 10.1002/wsbm.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhee DK1, Marcelino J, Baker M, et al. The secreted glycoprotein lubricin protects cartilage surfaces and inhibits synovial cell overgrowth. J Clin Invest. 2005;115:622–31. doi: 10.1172/JCI200522263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ludwig TE, McAllister JR, Lun V, Wiley JP, Schmidt TA. Diminished cartilage-lubricating ability of human osteoarthritic synovial fluid deficient in proteoglycan 4: restoration through proteoglycan 4 supplementation. Arthritis Rheum. 2012;64:3963–71. doi: 10.1002/art.34674. [DOI] [PubMed] [Google Scholar]
- 18.Saito S, Momohara S, Taniguchi A, Yamanaka H. The intra-articular efficacy of hyaluronate injections in the treatment of rheumatoid arthritis. Mod Rheumatol. 2009;19(5):493–501. doi: 10.1007/s10165-009-0207-8. [DOI] [PubMed] [Google Scholar]
- 19.Khan W, Khan M, Alradwan H, Williams R, Simunovic N, Ayeni OR. Utility of Intra-articular Hip Injections for Femoroacetabular Impingement. Orthop J Sports Med. 2015 Sep 1;3(9):1–8. doi: 10.1177/2325967115601030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abate M, Scuccimarra T, Vanni D, Pantalone A, Salini V. Femoroacetabular impingement: is hyaluronic acid effective? Knee Surg Sports Traumatol Arthrosc. 2014 Apr;22(4):889–92. doi: 10.1007/s00167-013-2581-1. [DOI] [PubMed] [Google Scholar]
- 21.Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Stockholm Suppl. 1968;277:70–72. [PubMed] [Google Scholar]
- 22.Migliore A, Massafra U, Bizzi E, et al. Comparative, double blind, controlled study of intra-articular hyaluronic acid (Hyalubrix) injections versus local anesthetic in osteoarthritis of the hip. Arthritis Res Ther. 2009;11(6):R183. doi: 10.1186/ar2875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fam H, Bryant JT, Kontopoulou M. Rheological properties of synovial fluids. Biorheology. 2007;44:59–74. [PubMed] [Google Scholar]
- 24.Bannuru RR, Natov NS, Dasi UR, Schmid CH, McAlindon TE. Therapeutic trajectory following intra-articular hyaluronic acid injection in knee osteoarthritis. Meta-analysis. Osteoarthritis Cartilage. 2011;19:611–9. doi: 10.1016/j.joca.2010.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lurati A, Laria A, Mazzocchi D, Re KA, Marrazza M, Scarpellini M. Effects of hyaluronic acid (HA) viscosupplementation on peripheral Th cells in knee and hip osteoarthritis. Osteoarthritis Cartilage. 2015;23(1):88–93. doi: 10.1016/j.joca.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 26.Dallari D, Stagni C, Rani N, Sabbioni G, Pelotti P, Torricelli P. Ultrasound-Guided Injection of Platelet-Rich Plasma and Hyaluronic Acid, Separately and in Combination, for Hip Osteoarthritis: A Randomized Controlled Study. Am J Sports Med. 2016 Mar;44(3):664–71. doi: 10.1177/0363546515620383. [DOI] [PubMed] [Google Scholar]
- 27.Battaglia M, Guaraldi F, Vannini F, Rossi G, Timoncini A, Buda R, Giannini S. Efficacy of ultrasound-guided intra-articular injections of platelet-rich plasma versus hyaluronic acid for hip osteoarthritis. Orthopedics. 2013;36(12):e1501–8. doi: 10.3928/01477447-20131120-13. [DOI] [PubMed] [Google Scholar]
- 28.Conrozier T, Bertin P, Bailleul F. Clinical response to intra-articular injections of hylan G-F 20 in symptomatic hip osteoarthritis: the OMERACT-OARSI criteria applied to the results of a pilot study. Joint Bone Spine. 2006;73(6):705–9. doi: 10.1016/j.jbspin.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 29.Richette P, Ravaud P, Conrozier T, Euller-Ziegler L, Mazières B, Maugars Y. Effect of hyaluronic acid in symptomatic hip osteoarthritis: a multicenter, randomized, placebo-controlled trial. Arthritis Rheum. 2009;60(3):824–30. doi: 10.1002/art.24301. [DOI] [PubMed] [Google Scholar]
- 30.Tikiz C, Unlü Z, Sener A, Efe M, Tüzün C. Comparison of the efficacy of lower and higher molecular weight viscosupplementation in the treatment of hip osteoarthritis. Clin Rheumatol. 2005;24(3):244–50. doi: 10.1007/s10067-004-1013-5. [DOI] [PubMed] [Google Scholar]
- 31.Atchia I, Kane D, Reed MR, Isaacs JD, Birrell F. Efficacy of a single ultrasound-guided injection for the treatment of hip osteoarthritis. Ann Rheum Dis. 2011;70(1):110–6. doi: 10.1136/ard.2009.127183. [DOI] [PubMed] [Google Scholar]
- 32.Van den Bekerom MP, Lamme B, Sermon A, Mulier M. What is the evidence for viscosupplementation in the treatment of patients with hip osteoarthritis? Systematic review of the literature. Arch Orthop Trauma Surg. 2008;128:815–23. doi: 10.1007/s00402-007-0447-z. [DOI] [PubMed] [Google Scholar]
- 33.Arrich J, Piribauer F, Mad P, Schmid D, Klaushofer K, Müllner M. Intra-articular hyaluronic acid for the treatment of osteoarthritis: a systematic review and meta-analysis. CMAJ. 2005;172:1039–43. doi: 10.1503/cmaj.1041203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rivera F. Single intra-articular injection of high molecular weight hyaluronic acid for hip osteoarthritis. J Orthop Traumatol. 2016 Mar;17(1):21–6. doi: 10.1007/s10195-015-0381-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Legré-Boyer V. Viscosupplementation: techniques, indications, results. Orthop Traumatol Surg Res. 2015 Feb;101:S101–8. doi: 10.1016/j.otsr.2014.07.027. [DOI] [PubMed] [Google Scholar]