Abstract
Background and aim of the work: Ring avulsion are relatively common hand lesions and are associated with significant disability, especially in hand-workers. The treatment choice is still debatable. We sought to conduct a detailed systematic review in attempt to collate evidence on functional, cosmetic and patient-reported outcomes (PROs) following ray amputation for the management of traumatic hand injury and ring avulsion injury. Methods: Using the PubMed database we made a systematic search for articles regarding single ray amputation after traumatic hand lesion. Nine articles met our including criteria and were analysed. Results: Most of the included studies suggest that for those worse cases ray amputation still represent a good option. Indeed ray resection can eliminate the gap, remove a cumbersome or painful digit and guarantes better cosmesis but reduces grip and pinch strength (from 15% to 30%) and decreased palm width. Conclusions: Different surgical techniques are available, almost all of them results in a loss of strength but ensure good both functional and cosmetic results. (www.actabiomedica.it)
Keywords: ray resection, ring finger injury, outcomes, grip strength, pinch strength, review
Introduction
A certain kind of finger injuries is ring avulsion injury: they usually involve only one finger (1) and happen when a ring is caught on an immobile object, from crush traumas or less common means such as thermal injury (2).
Severity of injury increases as the ring maintains traction on the skin and strips the underling tissues from the underlying skeleton. Moreover dislocation or traumatic amputation at the distal interphalangeal joint (DIPJ) and proximal phalanx fracture may also complicate the injury. Furthermore, avulsion injury also have the potential of damaging the flexor tendon sheaths and neurovascular structures (2).
These specific lesions have been classified by Urbaniak et al. in three classes (Table 1):
Table 1.
Urbaniak’s et al. classification of ring finger injuries
| I | Circulation adequate |
| II | Circulation inadequate with venous and/or arterial injury |
| III | Complete degloving or amputation |
1) circulation adequate, 2) circulation inadequate with venous and/or artery injury, 3) complete degloving or amputation (2-5). Kay et al. modified the classification as follow: 1) circulation adequate, with or without skeletal injury, 2) circulation inadequate (arterial only or venous only), no skeletal injury, 3) circulation inadequate (arterial and venous), fracture or joint injury present, 4) complete amputation or degloving (Table 2) (2-4).
Table 2.
Kay’s et al. modified classification of ring finger injuries
| Ia | Circulation adequate without skeletal injury |
| Ib | Circulation adequate with skeletal injury |
| II | Circulation inadequate (venous only or arterial injury) + no skeletal injury |
| III | Circulation inadequate (venous and arterial injury) + fracture or joint injury |
| IV | Complete degloving or amputation |
Adani et al. described a further subclassification of IV class: those with amputation proximal to the insertion of flexor digitorum superficialis fared worse than those amputated distal to its insertion (4).
The treatment of finger injuries, and in particular ring injuries, has always presented complex management problems: before the advent of microsurgery debate centred on whether distal flap coverage or grafting was preferable to amputation. In the era of microvascular repair the choices have become more complicated; alternatives include replantation and free tissue transfer in addition to local flap, pedicle flap, or graft coverage (3).
The indications for ray resection are ischemic necrosis involving the metacarpal, severe dysfunction of the proximal interphalangeal joint (PIPJ) and amputations at the level of the proximal phalanx (6, 7). Amputations performed distal to the PIPJ have good outcomes without ray resection (6, 8-10). However a stiff, obstructive finger, regardless of length, may cause decreased function and dexterity of the remainder of the hand and sometime may be painful, repeatedly traumatized and useless (6, 11). The primary contraindication to this procedure is any psychological barrier to amputation (6).
The surgical techniques include: ray resection without bony transposition, small finger-to-ring finger ray transposition, second finger-to-long finger transposition, ray transposition by intercarpal osteotomy (12). Other techniques have been described by Iselin and Peze (15) who practice an osteotomy of the carpus, or Le Viet who described a V-shaped osteotomy of the carpus proximal to the fourth metacarpal through the hamate (16).
The advantages of ray resection are gap elimination, removal of a cumbersome or painful digit, and better cosmesis (6, 13, 17). The gap caused by missing digit, especially central fingers, could jeopardize the function of the whole hand, weaken the grip strength, or result in difficulty in the control of small objects or performing skilful movements because of malalignment of the fingers close to the injured one (11, 15, 17).
Transposition of the neighboring metacarpal for a central digit amputation has been suggested to prevent gapping, scissoring, malrotation or discrepancies of digit length. It also improves function of hand as an entity (7, 11, 13).
Ray amputation of the index finger, even though disabling, is better than amputation at proximal interphalangeal (PIP) or metacarpophalangeal (MCP) level, as middle finger adapt to the role of index finger.
The main disadvantages of the procedure include decreased grip and pinch strength (from 15% to 30%), decreased palm width, and an abnormal finger count (6).
The complications that may occur are infection, cold intolerance, pain, neuroma, tenderness of the scar, tendon adhesion and joint stiffness. In those cases where bony transposition is performed non-union, pseudarthrosis or malunion may occur (2, 7, 14, 17, 18).
The aim of this study is to review the literature regarding amputation of one ray as treatment for traumatic injuries of the hand, especially ring avulsion injuries. First ray was excluded because it has different indication of treatment and it should always be tried to save the thumb. We have focused on functional and cosmetic results and patients’ satisfaction to determine whether ray amputation is a good treatment choice and which are the indications.
Materials and Methods
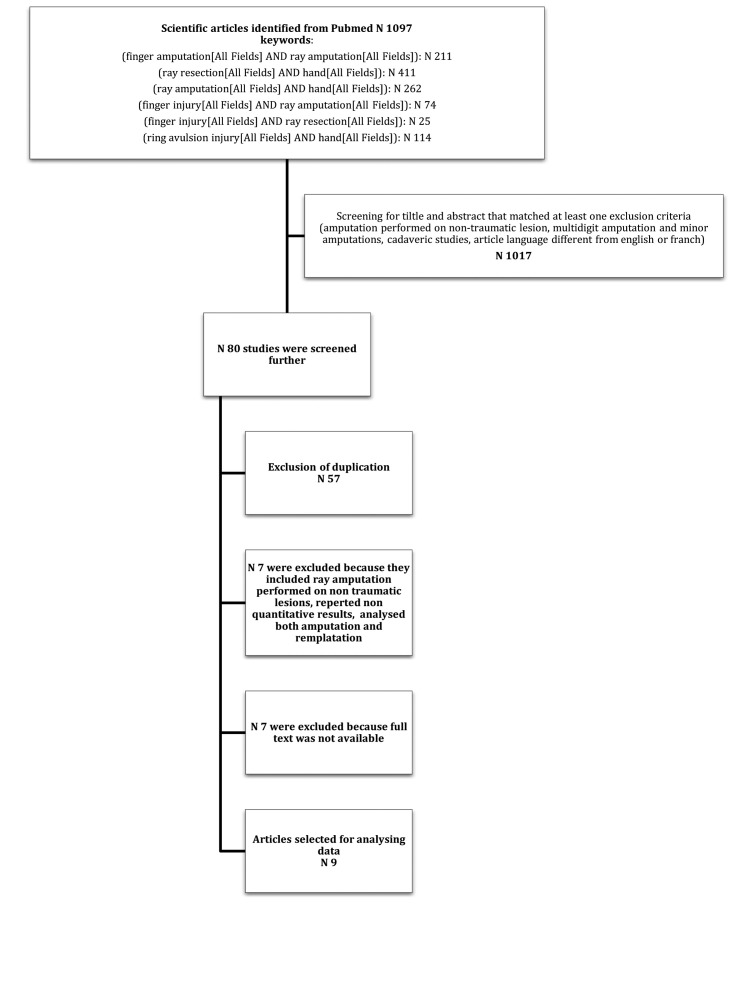
PubMed was systematically searched from January 1970 through August 2018 to identify relevant studies. The search items were listed as the flowchart 1 shows.
Flowchart 1.
First the resulting articles were screened based on the title and abstracts. Inclusion criteria were: (1) studies regarding adult patients, (2) traumatic injuries of one ray treated by ray amputation with or without metacarpal transposition (first ray injuries were excluded), (3) evaluation of functional results and patients’ satisfaction, (4) French and English articles. Studies were excluded if (1) the amputation was performed on non-traumatic lesion, (2) multidigit amputation or first ray amputation, (3) if they analysed minor amputations such as distal or proximal phalanx amputation only, (4) cadaveric studies. The selected articles were then fully read and nine were included in this review, their results were collected and analysed (Table 3).
Table 3.
Studies included in the review
| Study and year of publication | Country | Kind of study | N° of cases | Male/Female | Age | Dominant hand | Follow up (months) |
| Sadek 2015 (11) | Egypt | Prospective comparative study | 12 Primary amputation 13 Delayed amputation | 10/2 9/4 |
35±9 (19-48) 29±16 (7-56) |
4 5 |
28±10 (16-48) |
| Pedrazzini 2009 (13) | Italy | Case report | 1 | 0/1 | 56 | 1 | 18 |
| Segret 2008 (8) | France | Retrospective study | 11 | 8/3 | 35 (16-69) | 5 | 9 (3-19) |
| Nuzumlali 2003 (9) | Turkey | Retrospective study | 14 | 8/6 | 33 (16-58) | 9 | 37 (24-63) |
| Peimer 1999 (10) | USA | Retrospective comparative study | primary amputation secondary amputation |
18/7 | 28 (16-64) | 14 | 41 (16-154) |
| Levy 1999 (12) | USA | Case report | 1 | 1/0 | 13 | 1 | 300 |
| Van Overstraeten 1995 (22) | France | Retrospective study | 9 primary amputation 34 secondary amputation | 36/7 | 30 (4-55) | 14 | 40 |
| Peze Iselin 1988 (15) | France | Retrospective study | 12 | / | / | / | 6 |
| Steinchen 1986 (14) | USA | Retrospective study | 13 | 10/3 | 38 (16-54) | 4 | 43 (3-93) |
| Mean/total | 145 | 100/33 | 37.1 | 101 | 58 |
Results
Our search through PubMed selected 9 studies, two of them are case report and the others are retrospective studies or retrospective comparative studies. Altogether we could analyse the functional and cosmetic results of 145 cases of ray amputation, eighteen of them were border digit the others were central ray (Table 4). Three studies separated patients who underwent primary amputation from those who had secondary ray resection and collected their outcomes separately (Table 3). Most of the patients involved were males, the mean age was 37,1. The injured hand was the dominant in 57 cases. The minimum follow-up was 3 months and the longest was 25 years.
Table 4.
Description of surgical technique and ray resected for each study
| Study | Ray resected | Surgical technique | Revision surgery |
| Sadek (11) | IV | IV ray resection, transposition of V MC, fixed with K wire and reconstruction of deep transverse inermetacarpal ligament | / |
| Pedrazzini (13) | IV | IV ray resection, transposition of V MC, fixed with K wire and reconstruction of deep transverse inermetacarpal ligament | / |
| Segret (8) | IV | IV ray resection, transposition of V MC, fixed with K wire and reconstruction of deep transverse inermetacarpal ligament | 20% (2 cases) intermetacarpal space too wide |
| Nuzumlali (9) | IV | Not described | / |
| Peimer (10) | III or IV (7 cases) II or V (18 cases) |
Only in case of central amputation a ray transfer of border digit was done by ostetotomy | / |
| Levy (12) | III | Secondary ray resection without ray transposition, reconstruction of intermetacarpal ligament | / |
| Van Overstraeten (22) | (19 cases) (24 cases) |
III Metacarpal resection (6 cases), with transposition II-III (13 cases), IV metacarpal resection (16 cases), translocation IV-V according to Leviet (7 cases), classic translocation (1 cases) | / |
| Peze Iselin (15) | III | Ray resection, osteotomy of the hamate, reconstruction of intermetacarpal ligament | / |
| Steinchen (14) | III (4 cases) IV (9 cases) |
Ray resection without bony transposition, reconstruction of deep transverse metacarpal ligament e dorsal dermadesis | 4 (for complication) |
The most frequent surgical technique performed by the selected studies was ray resection with metacarpal transposition. Six patients needed additional surgery because of complications.
Every study measured grip strength after metacarpal resection, four reported also pinch strength and seven recorded MCPJ range of motion at the transposed ray (Table 5). Only Sadek compared supination and pronation strength of the operated arm and the healthy one. Residual pain was investigated only by Sadek and Van Overstraeten. The complications that occurred are shown in Table 7, its aerage rate is low (6%): infection, neuromas, palmar tenderness and intolerance to cold are the most frequent. Even though most of the patients said to be satisfied of the surgery eight of them had psychological problems in accepting a four-finger-hand. The mean time before returning to work is 3,6 months.
Table 5.
Funcional results and pain evalutation (visual analogic scale=VAS). For Sadek and Peimer are reported separate data for primary amputation and secondary amputation
| Study | Grip strength compared with healthy side (%) | Pinch strength compared with healthy side (%) | Preoperative MCP joint active ROM at the transposed ray (%) | Postoperative MCP joint active ROM at the transposed ray (%) | Pronation strength compared with healthy side (%) | Supination strength compared with healthy side (%) | Pre - and postoperative hand width (cm) | VAS |
| Sadek (11) | 84±8 | 94±5 | 87±24 | 83±13 | 87±4 | 76±11 | 8.5±0.8 7.1±1.1 |
0.65±1.3 |
| 75±7 | 91±5 | 80±11 | 79±13 | 77+-10 | 71±11 | 8.2±1.1 7.5±0.9 |
0.9±1.2 | |
| Pedrazzini (13) | 74.3 | / | / | 100 | / | / | / | / |
| Segret (8) | 70 | 77 | / | 70.58 | / | / | / | / |
| Nuzumlali (9) | 78.9 | 87.5 | / | / | / | / | 9.5±5 8.8±5 |
/ |
| Peimer (10) | 82.4 63.7 |
94.5 81 |
/ | 100 | / | / | / | / |
| Levy (12) | 85.7 | / | / | / | / | / | 9.0 8.25 |
/ |
| Van Overstraeten (22) | 65.5 (III ray)* 76.8 (IV ray)* |
/ | / | / | / | / | / | * |
| Peze Iselin (15) | 66.7 | / | / | 100 | / | / | / | / |
| Steinchen (14) | 67 (non-dominant involved) 74 (dominant hand involved) |
/ | / | 100 | / | / | / | / |
* see Table 6
Table 7.
Complications, cosmetic evalutation and time before return to work
| Study and year of publication | Complications | Cosmetic evaluation | Time before return to work (months) |
| Sadek 2015 | None | 10 excellent, 1 good, 1 satisfectory 9 excellent, 1 good, 1 poor | / |
| Pedrazzini 2009 | None | Satisfied | 3 |
| Segret 2008 | 1 phantom hand, 8 psychological problems | All satisfied | 3 |
| Nuzumlali 2003 | None | All satisfied | 2.3 |
| Peimer 1999 | Not mentioned | All satisfied | 2.2 4 |
| Levy 1999 | None | Satisfied | 1.5 |
| Van Overstraeten 1995 | 2 local infections, 1 pseudoarthrosis | Excellent 65%, good 15%, fair 15%, poor 4% | 2.5 |
| Peze Iselin 1988 | 1 postoperative distrophy | All satisfied | / |
| Steinchen 1986 | 2 digital neuromas 1 lumbrical/interosseous adhesions, 1 scar contracture, 4 palmar tenderness, 4 intolerance to cold | All satisfied | 6.7 |
Table 6.
Detalied results of Van Overstraeten study according to specifical surgical technique
| Van Overstraeten 1995 | Impaired mobility (19 patients) | Rotational deficit (18 patients) | Intermetacarpal laxity (18 patients) | Residual pain n° Patients | Pain score % (Min-Max) | Grip strength % |
| Resection III ray | 0° 4 cases 80% F°<15°(MP) 2 cases 20% |
1/5 | 2/5 | 1/5 | 4.0 | 62.9 |
| Resection III ray with transposition | 0° 1 case 33% E°<15° (MP) 2 cases 67% |
1/3 | 0/3 | 2/3 | 10.0 (5-15) | 70 |
| Resection IV ray | 0° 4 cases 80% F°<15° (IPP) 1 case 20% |
1/6 | 1/4 | 2/4 | 6.0 (5-7) | 67.7 |
| Resection IV ray with Leviet technique | 0° 5 cases 83% F°<15° (MP) 1 case 17% |
0/6 | 1/6 | 4/6 | 15.7 (1-45) | 82.8 |
Discussion
According to Urbaniak classification, class I ring injuries recover very well with soft tissue treatment alone (2). Class II injuries can be successfully revascularized in almost all instances, with sensibility, strength, motion, and appearance approaching normal in the majority of patients (3). Except in those cases that present also laceration of the sublimis and profundus tendons and proximal phalanx fractures which demonstrate poor motion and cold intolerance (2,5). In contrast class III ring finger injuries present the greatest challenge both to revascularize and to achieve function and they may best be managed by primary amputation (2,3). Also Sood stated that any patients who have lost a portion of a central ray at or proximal to the midportion of the proximal phalangeal level should be considered for ray amputation and adjacent ray transposition (18).
According to Kay classification, Kay et al. found that skeletal injury is correlated with successful salvage leading to significant difference in total active motion. They also found significant difference in occurrence of complications requiring further surgery (36% in class II, 83% in class III). In class II there were no primary amputation whereas 16,7% of class III had primary amputations (3).
Many surgical techniques are available to treat class III finger injuries, and in the selected studies there is no agreement on which one is the more suitable.
Advocates of the ray resection without bony transposition feel that even though this technique results decreased grip strength, scissoring of adjacent fingers, inability to cup small objects, and difficulty with skilled activities, it is easier to perform, has shorter recovery time and avoids potential complications (nonunion, extensor tendon adherence and loss of motion) (12, 13). They also feel that closure of the gap results in improved cosmetic appearance (13).
Some Authors advocated isolated fourth ray amputation with no fifth ray translation owing to both good functional results in the form of 68% grip power compared with the healthy side and excellent cosmetic results (12, 14, 20).
Ray resection without bony transposition is ideal for fourth ray resection, since its metacarpal is narrower than the others and gap closure using the small finger is easily accomplished because of the relatively mobile fifth carpometacarpal joint (14).
Conversely, some other authors preferred combined fourth ray amputation and fifth ray translation, achieving better functional results in the form of 94% pinch strength and 84% grip strength in comparison with the healthy side. In addition, the ROM of the MCP joint was 83° (11).
Peimer found that patients with single ray amputation and with translation of the adjacent digit showed 28% grip, 3% key pinch and 26% oppositional pinch strength loss compared to the healthy hand. Furthermore, gross hand function as measured by the Minnesota Rate of Manipulation test (Educational test Bureau, 720 Washington Avenue S. E., Minneapolis, Minnesota) and fine finger dexterity as measured by the Timed Grooved Pegboard test showed 12% and 24% loss, respectively (10).
Segret et al. (8) analysed a series of 10 patients with ring avulsion injury treated by ray resection of the metacarpal with conservation of the proximal end in emergency. They found that grip strength was 30% of grip strength of the unaffected side (range 3-70%) and the time to return to work was three months. The 80% of their patients underwent only one surgery procedure. They concluded that this treatment is a valid choice in complete amputation with proximal disarticulation or P2 or IPPJ fracture but each case has to be discussed with the patient because there may be psychological consequence (8). Also Levy suggested that the treatment has to be discussed with the patient (12).
In a study that compare functional results in patients with ring avulsion injury at the level of PIPJ treated with ray resection or amputation, Nuzumlali et al. suggest that for those patients with lesions that cannot be replanted or undergo failed replantation the choice of treatment should be determined by the patients. They advise against ray resection in patients who have occupations that require string key and chuck pinch (9).
Some authors proposed transposing the neighboring metacarpal for central digit amputation to prevent gaping, scissoring or discrepancies of digit length (17, 18), others advocated disarticulating the carpometacarpal joint to prevent the osteotomised end of the metacarpal protruding dorsally (21).
Steichen and Idler performed a central ray resection without bony transposition on 13 patients with reconstruction of the deep transverse metacarpal ligament and dorsal dermadesis which prevented rotation after gap closure. Considering ring injuries in this series the average time to return to work was 2.8 months. All patients but one were satisfied with cosmetic appearance and function of the treated hand. None of the patients had rotational malalignament produced by this technique or angular deformity. Average grip strength was 67% of that of the dominant hand and 74% of that of the nondominant hand (14). The authors also suggest that ray transposition may not be an ideal procedure in elderly people, and patients with multiple injuries of the hand where prolonged immobilization while waiting for healing of the transferred ray might result in loss of joint motion or tendon adherence (14).
The important points of the technique of central ray resection without transposition are the tight and secure reconstruction of the transverse metacarpal ligament and the dorsal dermadesis that derotates any malrotation produced by the gap closure after ray resection. Most criticism on ray resection without bony transposition has been on a cosmetic basis. In Steichen series all patients have been satisfied with the cosmetic appearance (14).
The long finger metacarpal is the largest and its removal creates a larger gap that is not as easily closed by the index finger, with its stiff carpometacarpal joint. The result is that slight angulation will occur in the index finger through its metacarpophalangeal joint and the new second web space may be somewhat wider (14).
In III ray resection, Van Overstraeten and Foucher (22) suggested translocation of the index on the third metacarpal in manual workers, whereas III ray amputation without metacarpal transposition which give better sizing and less complications, because they have better strength results. These Authors believed also that in IV ray amputation seems better to propose a translocation according to Leviet technique in any case. They also found that, as for the fourth ray resection and transposition of the fifth ray, the patients achieved superior results to the isolated fourth ray amputation (22).
Sadek et al. compared early versus delayed fourth ray amputation with fifth metacarpal translation and found better functional results in early amputations rather than delayed amputation: in the first group the found grip strength and pinch strength to be respectively 84% and 94% compared with healthy side, whereas the second group showed respectively 75% and 91% compared with the other side. They also believe that the main underlying factor favouring sudden intervention is the early rehabilitation allowing better active ROM, grip and pinch strength, and supination/pronation strength (11).
Also Peimer et al. feel that primary amputation is preferable in shortening the total disability and improving ultimate function: average 9 total weeks out of work for primary ray resection versus average 16 weeks out of work for patients who had secondary amputation (10).
Long-term benefits of primary middle ray amputation include removal of a middle finger that is likely to function poorly and that will compromise power gripping activities of the hand, avoidance of the problems of dissociation of the ulnar and radial parts of the hand, including isolation of the thumb-index unit from the ulnar part of the hand, which results in difficulty in chuck-pinch gripping. A primary amputation will prevent problems of a gap hand and will result in a three fingered hand in which the retained fingers are optimally aligned to provide the best possible function and appearance and allow early uncompromised use of the hand (19).
The complications incidence is low in all analysed studies, the most frequent are palmar tenderness, cold intolerance, neuromas and infection. Only one case of pseudoarthosis is reported. Although almost all patients declared to be satisfied of the surgery and of the cosmetic appearance of their hand the psychological aspect is not negligible in the choice of treatment (8,9). The average time before return to work is 3,6 months.
This study was limited by the heterogeneity of available literature. Some studies analysed only amputations of border digits some others only central fingers. Several studies focused on a specific surgical technique and this hindered comparing outcomes of different studies. Also not all the studies analysed the same outcomes and most of them were collected retrospectively. Therefore it was impossible for us to perform a meta-analysis.
Conclusions
Finger injuries are complex lesions of the hand and can require different treatments. Classifying the lesion may help to decide which is the best approach. For those worse cases ray amputation still represent a good option. There are different surgical techniques; each of them has advantages and disadvantages. Almost all of them results in a certain loss of strength but ensure good both functional and cosmetic results. Although performing a primary ray resection may lead to better functional results and faster recovery with early return to work.
References
- 1.Carroll RE. Ring injuries in the hand. Clin Orthop Relat Res. 1974;104:175–82. doi: 10.1097/00003086-197410000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Crosby N, Hood J, Baker G, Lubahn J. Ring injuries of the finger: long term follow up. HAND. 2014;9:274–281. doi: 10.1007/s11552-014-9651-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kay S, Werntz J, Wolff TW. Ring avulsion injuries: classification and prognosis. J Hand Surg Am. 1989;14:204–13. doi: 10.1016/0363-5023(89)90008-7. [DOI] [PubMed] [Google Scholar]
- 4.McDonald AH, Cleland HJ, Leung M, Slattery PG. Ring avulsion injuries. Aust N Z J Surg. 1999 Jul;69(7):514–6. doi: 10.1046/j.1440-1622.1999.01614.x. [DOI] [PubMed] [Google Scholar]
- 5.Nissenbaum M. Class IIA, ring avulsion injuries: an absolute indication for microvascular repair. J Hand Surg Am. 1984;9:810–5. doi: 10.1016/s0363-5023(84)80053-2. [DOI] [PubMed] [Google Scholar]
- 6.Blazar PE, Garon MT. Ray Resections of the Fingers: Indications, Techniques, and Outcomes. J Am Acad Orthop Surg. 2015 Aug;23(8):476–84. doi: 10.5435/JAAOS-D-14-00056. [DOI] [PubMed] [Google Scholar]
- 7.Bhat AK, Acharya AM, Narayanakurup JK, Kumar B, Nagpal PS, Kamath A. Functional and cosmetic outcome of single-digit ray amputation in hand. Musculoskelet Surg. 2017 Dec;101(3):275–281. doi: 10.1007/s12306-017-0484-x. [DOI] [PubMed] [Google Scholar]
- 8.Segret J, Barbary S, Pétry D, Dautel G. Primary ray resection as an alternative to microsurgical replantation in the management of ring finger avulsion. Chir Main. 2008 Oct;27(5):202–7. doi: 10.1016/j.main.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Nuzumlali E, Orhun E, Oztürk K, Cepel S, Polatkan S. Results of ray resection and amputation for ring avulsion injuries at the proximal interphalangeal joint. J Hand Surg Br. 2003 Dec;28(6):578–81. doi: 10.1016/s0266-7681(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 10.Peimer CA, Wheeler DR, Barrett A, Goldschmidt PG. Hand function following single ray amputation. J Hand Surg Am. 1999 Nov;24(6):1245–8. doi: 10.1053/jhsu.1999.1245. [DOI] [PubMed] [Google Scholar]
- 11.Sadek AF, Fouly EH, Hassan MY. Early versus delayed fourth ray amputation with fifth ray trasposition for management of mutilating ring fingerinjuries. J Hand Surg Am. 2015 Jul;40(7):1389–96. doi: 10.1016/j.jhsa.2015.04.010. [DOI] [PubMed] [Google Scholar]
- 12.Levy HJ. Ring finger ray amputation: a 25-year follow up. Am J Orthop (Belle Mead NJ) 1999 Jun;28(6):359–60. [PubMed] [Google Scholar]
- 13.Pedrazzini A, Calderazzi F, Bertoni N, Ceccarelli F. Cosmetic amputation of the fourth ray as possible outcome of the traumatic amputation of the ring finger injury: a case report. Acta Biomed. 2008 Dec;79(3):227–32. [PubMed] [Google Scholar]
- 14.Steichen JB, Idler RS. Results of central ray resection without bony transposition. J Hand Surg Am. 1986 Jul;11(4):466–74. doi: 10.1016/s0363-5023(86)80179-4. [DOI] [PubMed] [Google Scholar]
- 15.F. Peze, W. Iselin. Ray centralization without bone fixation for amputation of the middle finger. J Hand Surg Br. 1988 Feb;13(1):97–9. doi: 10.1016/0266-7681_88_90064-2. [DOI] [PubMed] [Google Scholar]
- 16.Le Viet D. Translocation of the fifth finger by intracarpal osteotomy. Ann Plast Surg. 1986 Sep;17(3):228–38. doi: 10.1097/00000637-198609000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Posner MA. Ray transposition for central digital loss. J Hand Surg Am. 1979;4(3):242–257. doi: 10.1016/s0363-5023(79)80159-8. [DOI] [PubMed] [Google Scholar]
- 18.Colen L, Bunkis J, Gordon L, Walton R. Functional assessment of ray transfer for central digital loss. J Hand Surg Am. 1985;10(2):232–237. doi: 10.1016/s0363-5023(85)80111-8. [DOI] [PubMed] [Google Scholar]
- 19.Sood MK, Elliot D. Amputation of the middle ray in the primary treatment of severe injuries of the central hand. Plast Reconstr Surg. 2000 Jul;106(1):115–8. doi: 10.1097/00006534-200007000-00022. [DOI] [PubMed] [Google Scholar]
- 20.Melikyan EY, Beg MS, Woodbridge S, Burke FD. The functional results of ray amputation. Hand Surg. 2003 Jul;8(1):47–51. doi: 10.1142/s0218810403001388. [DOI] [PubMed] [Google Scholar]
- 21.Masmejean E, Alnot JY, Couturier C, Cadot B. Resection of the fourth ray for annular lesions: amputations of the fourth ray of the hand. Rev Chir Orthop Reparatrice Appar Mot. 1997;83(4):324–9. [PubMed] [Google Scholar]
- 22.Van Overstraeten L, Foucher G. A comparative study of metacarpal resection and translocation after amputation of the middle finger. [Article in French] Ann Chir Main Memb Super. 1995;14(2):74–83. [PubMed] [Google Scholar]