Abstract
Background: Fast track in total knee replacement (TKR) is a widely used protocol. Tranexamic acid proved to be effective in reducing perioperative bleeding without increasing thromboembolic risk. The aim of this study was to assess if tourniquet and suction drainage might affect perioperative blood loss and post-operative functional recovery after TKR. Methods: 151 patients, who underwent to TKR, were assessed and divided into three homogeneous groups: group A (51 patients) in which both tourniquet and suction drainage have been applied (tourniquet has been release before wound closure); group B (50 patients) in which neither tourniquet nor suction drainage have been used; group C (50 patients) in which only tourniquet has been used. Perioperative intravenous tranexamic acid and post-operative low-molecular-weight heparin have been administered. Trend of haemoglobin values, transfusion rate, pain, ability to obtain 90 degrees of flexion and length of stay were analysed. Results: The average intra-operative blood loss was statistically higher in group B in comparison to other two groups. Haemoglobin values were lower in group A in comparison to group C in the third and fifth post-operative days. Patients in group A had higher transfusion rate, higher pain and had more difficulties in reaching a 90 degrees of knee flexion than the other two groups. There was one infection in group A. No differences in length of stay. Conclusion: Suction drain seems to be associated to lower haemoglobin values, higher transfusion rate, higher pain and slower functional recovery. Short-term tourniquet does not influence post-operative bleeding and rehabilitation program. (www.actabiomedica.it)
Keywords: total knee replacement, blood loss, tourniquet, suction drainage, tranexamic acid
Background and aim of the work
Total knee arthroplasty (TKR) is one of the most common surgical operations in orthopaedics. Fast track protocol introduced in general surgery by Kehlet H. (1) is now applied in total hip and total knee replacement in several orthopaedic realities, aiming to improve the functional recovery of the patients without increasing complications, making easier the return to daily activities. Blood loss is particularly severe after TKR: a decrease of haemoglobin level from 2 to 4 g/dL is reported (2). So, with a view on fast track, blood loss management is important for avoiding cardiovascular complications related to anemia. In fact, the reported 30-day incidence of acute myocardial infarction after total hip replacement and TKR varies from 0.3% to 0.9% (3). Suction drains are routinely used in orthopaedics (4), because of the theoretical advantages of lower incidence of hematomas, wound complications, joint swelling, infections and, of improving rehabilitation, but their use is not justified by literature (5, 6). Some orthopaedic surgeons usually clamped the suction drain, but also this aspect is an age-old practice, not based on evidence (7). Intravenous and/or intra-articular tranexamic acid, acting as an inhibitor of plasminogen activation, reducing hyperfibrinolysis, has proved to be effective in reducing peri-operative bleeding in major orthopaedic surgery without increasing thromboembolic complications (8, 9). Finally the use of pneumatic tourniquet and the timing of tourniquet release are controversial too (10, 11).
Given these premises, we wondered if these aspects could affect fast track protocol in our unit. Thus, the purpose of the present study was to assess the influence of closed suction drainage and tourniquet on peri-operative bleeding and functional recovery after total knee arthroplasty.
Methods
203 consecutive patients underwent to TKR from September 2016 to November 2018 in our unit (Orthopaedics and Trauma Unit – St. Polo’s Hospital in Monfalcone, Italy). We excluded 52 patients because of coagulopathy disorders, anticoagulant and antiplatelet therapy (table 1: list of eligibility criteria). At the end we considered 151 patients that we divided in three homogenous groups based on usage of tourniquet and suction drainage: group A (51 patients – both tourniquet and suction drainage had been used), group B (50 patients – both tourniquet and suction drainage had not been used) and group C (50 patients – only tourniquet had been used). Characteristics of the groups are described in table 2. Tourniquet had been inflated for the whole surgical time at 300 mmHg and released before wound closure in groups A and C. Tourniquet had been inflated just for cementation phase in group B. Suction drainage had not been clamped and had been removed in the first post-operative day. All patients signed a proper informed consent form. Three different orthopaedic surgeons implanted the TKR using medial parapatellar approach, tibial extramedullary guide and femoral intramedullary guide after proper pre-operative planning. The type of implants used were Triathlon® (Stryker, Kalamazoo, USA) and Attune® (DePuy Synthes, Warsaw, USA). The same peri-operative fast track protocol had been applied in all three groups. Particularly, intravenous (iv) Cefazoline 2 g was administered 30 minutes before surgery. Two doses of intravenous tranexamic acid (15 mg/kg) were infused 20 minutes before surgery and after 4 hours. The antalgic therapy was periarticular infiltration with 60 mL of Ropivacaine 7.5%, Paracetamol 1 g iv every 8 hours and Oxycodone/Naloxone 10/5 mg 1 tablet every 12 hours. Thromboprophylaxis (Enoxaparine 4000 IU) started 12 hours after the operation. The knee was holded at 60-degrees of flexion for 4 hours, then the patients started continues passive motion for 30 minutes.
Table 1.
List of eligibility criteria
| Inclusion criteria | Exclusion criteria |
|
|
ASA status = American Society of Anesthesiologists
Table 2.
Characteristics of the groups
| Group A (n=51) | Group B (n=50) | Group C (n=50) | |
| Tourniquet applied | Yes | No | Yes |
| Suction drained applied | Yes | No | No |
| Tranexamic acid iv | Yes | Yes | Yes |
| Average age (years) | 73 (51-83) | 70 (53-81) | 75 (58-85) |
| Sex (Female/male ratio) | 1.7 | 2.2 | 1.5 |
| Average ASA status | 2.31 | 2.06 | 2.18 |
iv = intravenous
The haemoglobin values have been recorded in the pre-operative period, in the immediate post-op (T0), in the first, third and fifth post-operative days (T1, T3, T5 respectively). Intra-operative blood loss and percentage of blood transfusions have been measured in each group; blood loss in the suction drain at 24 hours has been recorded only for group A. All patients have also been clinically and functionally evaluated using the Numeric Rating Scale (NRS) at T0, T1 and T3, assessing the ability to reach a knee flexion of 90 degrees 6 hours after surgery, and recording the length of stay and possible haemorrhagic and thromboembolic complications.
Graph Pad Prism 6 and Microsoft Excel have been used for statistical analysis. All parameters have been compared in the three groups. Because the considerate variables had non-normal distribution, non parametric Mann-Whitney test (two-tailed) has been applied, considering a value as statistically significant if p <0.05.
Results
The trend of haemoglobin values and their differences in the three groups were described in graphic 1. Particularly, there was a statistically significant difference in T3 and T5 between group A and group C (T3: 9.80±1.35 g/dL versus 10.55±1.37 g/dL, p=0.049; T5: 9.66±1.36 g/dL versus 10.55±1.34 g/dL, p=0.024).
Graphic 1.
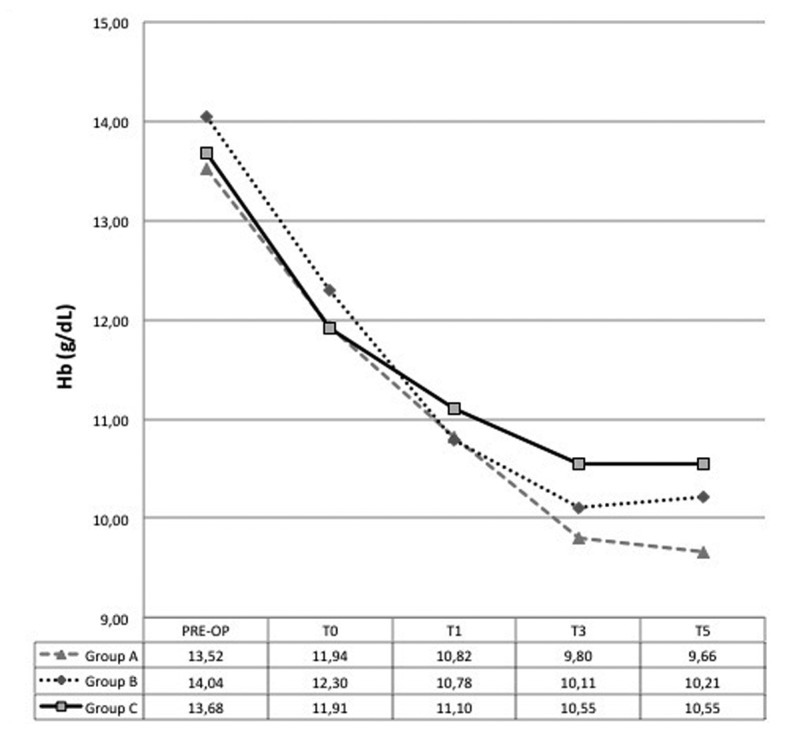
Trend of haemoglobin values in the three groups: pre-operative, T0 (immediate post-op), T1 (the first post-op day), T3 (the third post-op day), T5 (the fifth post-op day)
The average intra-operative blood loss was statistically higher without tourniquet inflation (group B) in comparison to group A and C (group B 607.14±171.13 mL versus group A 199.00±106.19 mL versus group C 168.42±101.67 mL, p <0.0001). The average blood loss in the suction drain in group A was 553±284 mL. As regards the blood transfusions, group A (in which suction drain had been inserted) had higher transfusion rate (group A 20.00% versus group B 2.86% versus group C 5.00%). The results are summarised in table 3.
Table 3.
Results in the different groups. NA = not applicable
| Group A (n = 51) | Group B (n = 50) | Group C (n = 50) | ||
| Blood loss: | ||||
| • intra-operative (mL) | 199.00±106.19 | 607.14±171.13* | 168.42±101.67 | p<0.0001 |
| • suction drain (mL) | 553±284 | NA | NA | |
| Transfusion rate | 20.00%* | 2.86% | 5.00% | p<0.0001 |
| Ability to 90 degrees | 62.5%* | 92.5% | 87.5% | p<0.05 |
| Lengh of stay (days) | 8.53 (4-18) | 7.56 (4-12) | 7.53 (4-11) | p>0.05 |
| Complications | 1 infection | 0 | 0 |
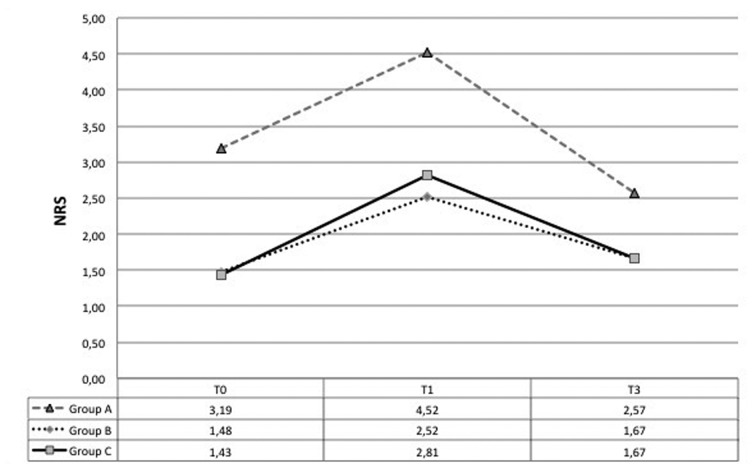
Pain measured as NRS was higher in group A in comparison to the other two groups. The NRS values are described in graphic 2. Patients in group B and C were better in obtaining a 90 degrees of knee flexion at 6 hours after surgery (group B 92.5% versus group C 87.5% versus group A 62.5%, p<0.05). There were no statistically significant differences in terms of length of stay (group A 8.53 days versus group B 7.56 days versus group C 7.53 days). We had one early periprosthetic infection in group A; neither hematomas nor cardiovascular nor thromboembolic complications had been recorded in the other two groups.
Graphic 2.
Trend of pain measured with NRS: T0 (immediate post-op), T1 (the first post-op day), T3 (the third post-op day)
Conclusions
Fast track protocol in TKR is widely used in all over the world. Several orthopaedics surgeons still use suction drain and/or tourniquet, although their use is not supported by scientific data, but it is related to our beliefs and routine behaviours (4, 6, 12). Thus in the present study we wondered if these practice could influence blood loss and functional recovery after TKR.
Doubts regarding the usefulness of the suction drain had been reported in the late 1980’s, when Reilly TJ et al. (13) reported more than twice blood transfusions given to the patients whose knees were drained with a greater decrease in haemoglobin level than the non-drained group. Hematoma is always a complication feared by orthopaedic surgeons. In fact it can be colonized by bacteria and it can swell the joint and increase the pain, creating discomfort to the patient and delaying his/her rehabilitation. Although correlation between suction drainage and periprosthetic infections is not supported (5-7), this is described in different animal study (14, 15) and also in some clinical studies in general surgery (16, 17), because suction drain might be an entryway for bacteria. Sorensen AI et al. (18) reported positive drain tip cultures and an increased risk of infection only when the drain removal occurred after 6 days. In our study we had one early infection in the group in which suction drain had been used.
Even if Lee QJ et al. reported better clinical results inserting the drainage (19), in the literature the absence of drainage is not associated to increased amount of hematomas and periprosthetic infections (2, 12), but to a higher need for transfusions (2, 30). In the present study use of suction drainage was associated to a greater decrease in haemoglobin level and to a higher transfusion rate (20% versus <5%). In the literature blood transfusions after TKR are reported up to 50% of TKR in the different case series (2). Transfused patients can develop immunological, infectious, cardiovascular complications and death (20), so guidelines and protocols for describing the proper use of blood products are applied in every hospital (21, 22). The bleeding control in the perioperative time is fundamental for reducing blood transfusions and their potential risks and for avoiding complications related to anemia. Especially in a fast track protocol, different strategies are applied. Proper surgical technique, particularly addressed to soft tissue sparing, use of electrocautery, compressive dressing, post-operative knee flexion, cryotherapy (23), tranexamic acid, clamping of the suction drain when applied (24, 25), are treatment that can improve the bleeding (22, 26). Intravenous and/or topical tranexamic acid is commonly used in orthopaedic surgery and its effectiveness is widely demonstrated without increasing thromboembolic complications (8, 9, 27). In fact tranexamic acid acts against fibrinolysis that in surgical patients is pretty high and it is associated to high mortality rate (28). Clamping the suction drainage for few hours after surgery might help in reducing blood loss and requirement for blood transfusion (24), creating a tamponade effect, but the usefulness of this practice and the duration of drain clamping are debated in the literature (25).
Blood transfusions are associated to longer length of stay in hospital, delayed rehabilitation programs and increased costs (29, 30). Bierbaum BE et al. reported up to a 20% increase in hospital costs and a 20 to 25% increase in the length hospitalization in transfused patients (26). Different studies showed that better blood management is associated to cost reduction. Mehra T et al. observed that reduction in the blood transfusions by 27% allowed saving more than 2 million USD in a year (31).
Routine use of tourniquet in TKR is another point of discussion. It allows a better view for the surgeon creating a bloodless surgical field and it seems to reduce intra-operative bleeding, but these aspects are not supported by scientific studies (32). Also its role in cementing technique could be just theoretical (33). In the present study there were no differences in haemoglobin levels drop down and in transfusion rate using or not the tourniquet. Even if tourniquet is described as one of the most important risks for thromboembolism (32) and associated to several complications (34-36), in the present study tourniquet was not associated to higher complication rate, particularly neurovascular deficit, skin necrosis, thromboembolic events and difficulties in quadriceps recruitment. In fact tourniquet can be safely applied following some simple recommendations to avoid ischemia-reperfusion injury, and limiting its long duration use (36, 37). Dennis DA et al. (38) reported reduced quadriceps strength during the first 3 months after TKR and lower intra-operative blood loss when tourniquet had been used. Even if reduction of quadriceps electromyographic signal has been described at the first post-operative period, it is not shown the initial quadriceps damage leads to long-term muscular atrophy and weakness (39). In fact the presence of lot of confounding factors should be considered. Different inflation timing and period, different inflation pressure and pre-operative muscular conditions might prevent proper comparisons. In the present study tourniquet has not been associated to late functional recovery, to prolonged length of stay and to higher pain level, but a correlation with the use of drainage has been observed. In fact patients with drainage had worse pain (this difference remained statistically significant not only in the immediate post-operative time, but also in the first and third post-operative days) and less ability to flex the knee. Only clinical quadriceps recruitment and not a leg-raise test had been evaluated.
Finally the timing of tourniquet release during TKR is also controversial. Tourniquet can be release either before or after wound closure. According to different Authors, both might bring to some advantages and influence perioperative bleeding in different ways. Early release should allow better identification of vascular injuries, reducing post-operative complications and improving patellar tracking assessment (10, 40), instead late release preceded by compressive dressing should reduce surgical time and limit the bleeding creating a tamponade effect (41). Actually, review and meta-analysis did not confirm these aspects (5, 42). Rama KR et al. (11) described higher total blood loss in early tourniquet release even if there was a higher early re-operation rate in late tourniquet release (0.3% versus 3.1%). In our study we did not analysed this aspect, because tourniquet had always been released before wound closure.
The present study has some limits. It is not a prospective randomized control study. The groups are made of small number of patients. Patients in each group had been operated for the most part by the same surgeon; so surgical technique and expertise of the single surgeon might have influenced bleeding. Blood loss in each group has been measured and not calculated (for example with Gross’s method, 43). In literature measured total blood loss is often underestimated compared to calculated blood loss (44).
In a fast track protocol for TKR not to use the suction drainage should become common practice, even if the decision should be personalized on patient’s risks factors. Avoiding the drainage in association of other elements of blood management, like tranexamic acid, might help in reducing the blood transfusion rate, improving patient’s functional recovery, reducing not only the costs related to length of stay and patient’s management, but also the social costs. As regards the decision to use or not to use the tourniquet, even if intra-operative blood loss might be reduced, there is no agreement about reduction of total blood loss. Thus the literature does not prove against its use, as long as surgical time is short, rehabilitation program starts early and patient’s thromboembolic risks factors are identified.
References
- 1.Kehlet H, Aasvang EK. Regional or general anesthesia for fast-track hip and knee replacement - what is the evidence? F1000Res. 2015;4:F1000. doi: 10.12688/f1000research.7100.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adalberth G, Byström S, Kolstad K, Mallmin H, Milbrink J. Postoperative drainage of knee arthroplasty is not necessary: a randomized study of 90 patients. Acta Orthop Scand. 1998;69:475–8. doi: 10.3109/17453679808997781. [DOI] [PubMed] [Google Scholar]
- 3.Petersen PB, Kehlet H, Jørgensen CC. Lundbeck Foundation Center for Fast-track Hip and Knee Replacement Collaborative Group. Myocardial infarction following fast-track total hip and knee arthroplasty-incidence, time course, and risk factors: a prospective cohort study of 24,862 procedures. Acta Orthop. 2018;17:1–7. doi: 10.1080/17453674.2018.1517487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chandratreya A, Giannikas K, Livesley P. To drain or not drain: literature versus practice. J R Coll Surg Edinb. 1998;43:404–6. [PubMed] [Google Scholar]
- 5.Zhang Q, Liu L, Sun W, et al. Are closed suction drains necessary for primary total knee arthroplasty?: A systematic review and meta-analysis. Medicine (Baltimore) 2018;97:e11290. doi: 10.1097/MD.0000000000011290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tejwani NC, Immerman I. Myths and legends in orthopaedic practice: are we all guilty? Clin Orthop Relat Res. 2008;466:2861–72. doi: 10.1007/s11999-008-0458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park JH, Shon HC, Kim JW, Park SJ, Ko TS, Park JH. Effectiveness of closed suction drainage tip culture in hip arthroplasty. Acta Orthop Traumatol Turc. 2016;50:16–21. doi: 10.3944/AOTT.2016.15.0022. [DOI] [PubMed] [Google Scholar]
- 8.Hunt BJ. The current place of tranexamic acid in the management of bleeding. Anaesthesia. 2015;70S:50–3. doi: 10.1111/anae.12910. [DOI] [PubMed] [Google Scholar]
- 9.Yates J, Perelman I, Khair S, et al. Exclusion criteria and adverse events in perioperative trials of tranexamic acid: a systematic review and meta-analysis. Transfusion. 2018 Dec 5 doi: 10.1111/trf.15030. [DOI] [PubMed] [Google Scholar]
- 10.Kvederas G, Porvaneckas N, Andrijauskas A, et al. A randomized double-blind clinical trial of tourniquet application strategies for total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2013;21:2790–9. doi: 10.1007/s00167-012-2221-1. [DOI] [PubMed] [Google Scholar]
- 11.Rama KR, Apsingi S, Poovali S, et al. Timing of tourniquet release in knee arthroplasty: A meta-analysis of randomized, controlled trials. J Bone Joint Surg. 2007;89:699–705. doi: 10.2106/JBJS.F.00497. [DOI] [PubMed] [Google Scholar]
- 12.Parker MJ, Roberts CP, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2004;86-A:1146–52. doi: 10.2106/00004623-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Reilly TJ, Gradisar IA Jr, Pakan W, Reilly M. The use of postoperative suction drainage in total knee arthroplasty. Clin Orthop Relat Res. 1986;208:238–42. [PubMed] [Google Scholar]
- 14.Raves JJ, Slifkin M, Diamond DL. A bacteriologic study comparing closed suction and simple conduit drainage. Am J Surg. 1984;148:618–20. doi: 10.1016/0002-9610(84)90336-2. [DOI] [PubMed] [Google Scholar]
- 15.Bristow PC, Halfacree ZJ, Baines SJ. A retrospective study of the use of active suction wound drains in dogs and cats. J Small Anim Pract. 2015;56:325–30. doi: 10.1111/jsap.12339. [DOI] [PubMed] [Google Scholar]
- 16.Seneviratne S, Hoffman G, Varadhan H, Kitcher J, Cope D. Does microbial colonisation of a neck drain predispose to surgical site infection: clean vs clean-contaminated procedures. Eur Arch Otorhinolaryngol. 2018;275:1249–55. doi: 10.1007/s00405-018-4921-8. [DOI] [PubMed] [Google Scholar]
- 17.Cruse PJ, Foord R. The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin North Am. 1980;60:27–40. doi: 10.1016/s0039-6109(16)42031-1. [DOI] [PubMed] [Google Scholar]
- 18.Sorensen AI, Sorensen TS. Bacterial growth on suction drain tips: prospective study of 489 clean orthopedic operations. Acta Orthop Scand. 1991;62:451–54. doi: 10.3109/17453679108996642. [DOI] [PubMed] [Google Scholar]
- 19.Lee QJ, Mak WP, Hau WS, Yeung ST, Wong YC, Wai YL. Short duration and low suction pressure drain versus no drain following total knee replacement. J Orthop Surg (Hong Kong) 2015;23:278–81. doi: 10.1177/230949901502300302. [DOI] [PubMed] [Google Scholar]
- 20.Beal EW, Bagante F, Paredes A, et al. Perioperative use of blood products is associated with risk of morbidity and mortality after surgery. Am J Surg. 2018 Nov 27 doi: 10.1016/j.amjsurg.2018.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Althoff FC, Neb H, Herrmann E, et al. Multimodal Patient Blood Management Program Based on a Three-pillar Strategy: A Systematic Review and Meta-analysis. Ann Surg. 2018 Nov 9 doi: 10.1097/SLA.0000000000003095. [DOI] [PubMed] [Google Scholar]
- 22.Spahn DR. Patient Blood Management: the new standard. Transfusion. 2017;57:1325–27. doi: 10.1111/trf.14095. [DOI] [PubMed] [Google Scholar]
- 23.Ni SH, Jiang WT, Guo L, et al. Cryotherapy on postoperative rehabilitation of joint arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23:3354–61. doi: 10.1007/s00167-014-3135-x. [DOI] [PubMed] [Google Scholar]
- 24.Zan P, Yao JJ, Fan L, et al. Efficacy of a four-hour drainage clamping technique in the reduction of blood loss following total hip arthroplasty: a prospective cohort study. Med Sci Monit. 2017;23:2708–14. doi: 10.12659/MSM.904864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao JG, Wang L, Liu J. The use of clamped drainage to reduce blood loss in total hip arthroplasty. J Orthop Surg Res. 2015;10:130. doi: 10.1186/s13018-015-0259-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bierbaum BE, Callaghan JJ, Galante JO, Rubash HE, Tooms RE, Welch RB. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am. 1999;81:2–10. doi: 10.2106/00004623-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Pappa E, Vergados N, Spiridakis E, Chountas G, Apostolopoulou A, Sourmelis S. A Retrospective Comparative Study of Different Methods of Blood Management in Total Knee Replacement. J Knee Surg. 2018 Nov 13 doi: 10.1055/s-0038-1675217. [DOI] [PubMed] [Google Scholar]
- 28.Gando S, Mayumi T, Ukai T. Activated protein C plays no major roles in the inhibition of coagulation or increased fibrinolysis in acute coagulopathy of trauma-shock: a systematic review. Thromb J. 2018;16:13. doi: 10.1186/s12959-018-0167-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bower WF, Jin L, Underwood MJ, Lam YH, Lai PB. Peri-operative blood transfusion increases length of hospital stay and number of postoperative complications in non-cardiac surgical patients. Hong Kong Med J. 2010;16:116–20. [PubMed] [Google Scholar]
- 30.Banerjee S, Kapadia BH, Issa K, et al. Postoperative blood loss prevention in total knee arthroplasty. J Knee Surg. 2013;26:395–400. doi: 10.1055/s-0033-1357491. [DOI] [PubMed] [Google Scholar]
- 31.Mehra T, Seifert B, Bravo-Reiter S, et al. Implementation of a patient blood management monitoring and feedback program significantly reduces transfusions and costs. Transfusion. 2015;55:2807–15. doi: 10.1111/trf.13260. [DOI] [PubMed] [Google Scholar]
- 32.Tai TW, Lin CJ, Jou IM, Chang CW, Lai KA, Yang CY. Tourniquet use in total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2010;19:1121–30. doi: 10.1007/s00167-010-1342-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vertullo CJ, Nagarajan M. Is cement penetration in TKR reduced by not using a tourniquet during cementation? A single blinded, randomized trial. J Orthop Surg (Hong Kong) 2017:25. doi: 10.1177/2309499016684323. [DOI] [PubMed] [Google Scholar]
- 34.Palmer SH, Graham G. Tourniquet-induced rhabdomyolysis after total knee replacement. Ann R Coll Surg Engl. 1994;76:416–7. [PMC free article] [PubMed] [Google Scholar]
- 35.Murphy CG, Winter DC, Bouchier-Hayes DJ. Tourniquet injuries: pathogenesis and modalities for attenuation. Acta Orthop Belg. 2005;71:635–45. [PubMed] [Google Scholar]
- 36.Sharma JP, Salhotra R. Tourniquets in orthopedic surgery. Indian J Orthop. 2012;46:377–83. doi: 10.4103/0019-5413.98824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vaishya R, Agarwal AK, Vijay V, Tiwari MK. Short term outcomes of long duration versus short duration tourniquet in primary total knee arthroplasty: A randomized controlled trial. J Clin Orthop Trauma. 2018;9:46–50. doi: 10.1016/j.jcot.2017.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dennis DA, Kittelson AJ, Yang CC, Miner TM, Kim RH, Stevens-Lapsley JE. Does Tourniquet Use in TKA Affect Recovery of Lower Extremity Strength and Function? A Randomized Trial. Clin Orthop Relat Res. 2016;474:69–77. doi: 10.1007/s11999-015-4393-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu D, Graham D, Gillies K, Gillies RM. Effects of tourniquet use on quadriceps function and pain in total knee arthroplasty. Knee Surg Relat Res. 2014;26:207–13. doi: 10.5792/ksrr.2014.26.4.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marson BM, Tokish JT. The effect of a tourniquet on intraoperative patellofemoral tracking during total knee arthroplasty. J Arthroplasty. 1999;14:197–9. doi: 10.1016/s0883-5403(99)90125-0. [DOI] [PubMed] [Google Scholar]
- 41.Zhang P, Liang Y, He J, Fang Y, Chen P, Wang J. Timing of tourniquet release in total knee arthroplasty: A meta-analysis. Medicine (Baltimore) 2017;96:e6786. doi: 10.1097/MD.0000000000006786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang W, Liu A, Hu D, Tan Y, Al-Aidaros M, Pan Z. Effects of the timing of tourniquet release in cemented total knee arthroplasty: a systematic review and meta-analysis of randomized controlled trials. J Orthopaedic Surg Res. 2014;9:125. doi: 10.1186/s13018-014-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58:277–80. doi: 10.1097/00000542-198303000-00016. [DOI] [PubMed] [Google Scholar]
- 44.Gibon E, Courpied JP, Hamadouche M. Total joint replacement and blood loss: what is the best equation? Int Orthop. 2013;37:735–9. doi: 10.1007/s00264-013-1801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]