Abstract
Background and aim of the work: Radius and ulna fractures are the most common long bone fractures in children and adolescents. The majority of these injuries involve the distal metaphyseal portion of the radius associated or not to physeal plate injuries. Because of the high remodelling potential of the distal radius in growing children most injuries heal without complication after closed reduction and immobilization in a long arm cast. Nonunions of closed distal radius fracture are an extremely rare occurrence especially in paediatric population. Methods: In this report, we describe a rare case of distal radius fracture nonunion in a 15-years old male rider treated conservatively with cast immobilization. Eight months later he underwent surgical closed reduction and fixation with kirschner wire and cannulated screw. Results: Follow-up at 2 years showed satisfying radiological and functional outcomes. The patient ultimately returned to ride 3 months following surgery. Conclusions: Nonunion is rarely seen in distal radius fractures in healthy children and adolescents, and there are few studies in the literature. Treatment of the nonunion must be individualized and the results are not entirely predictable. (www.actabiomedica.it)
Keywords: non-union, distal radius, physeal plate, paediatric, adolescence
Introduction
The distal part of the forearm is the most common area to sustain a fracture in the paediatric population (1-3). Among all forearm fractures, the distal radius and ulna are most commonly affected.(4,5). Several recent studies suggest that the frequency of paediatric distal radius fractures is rising, likely due to epidemiologic trends toward diminished bone density, increased body mass indices, higher-risk activities, and younger age at the time of initial sports participation (6,7). The mechanism of injury is generally a fall on the outstretched hand and it influences fracture type and degree of displacement (5).
Signs and symptoms of these kind of fractures are pain, swelling, and deformity of the distal forearm that depend on the degree of fracture displacement.
Plain radiographs are essential in order to diagnose the lesion and to assess its classification and degree of displacement. Standard anteroposterior (AP) and lateral (LL) views usually are sufficient. CT and MRI are rarely necessary and they are reserved for evaluation of suspected or misdiagnosed intra-articular fractures or associated carpal injuries and are very useful for pre-operative planning.
Fractures of the distal forearm typically occur during skeletal development. Due to the greater forces borne and imparted to the radius, as well as the increased porosity of the distal radial metaphysis, distal radial fractures are more common than distal ulnar fractures. Physeal plate injuries of this anatomic portion are also commonly seen (8).
The Salter–Harris system is the basis for classification of physeal plate fractures (9) and in the radius type II lesions are the majority (10).
Management is highly influenced by the remodelling potential of the distal radius in growing children. Generally, these injuries are successfully treated with nonoperative treatment. Surgery is recommended in patients with neurovascular compromise, severely displaced injuries and unstable fractures failing initial nonoperative care.
Loss of reduction and malunion are common occurrence after insufficient closed reduction and cast immobilization (11-16) but most injuries generally heal without complication after this treatment. Nonunion of closed distal radius fracture is an extremely rare occurrence and there are few studies among children and adolescent in the literature.
Case report
G.M. (15 years-old male biker) fell during a race with outstretched hand. After the fall he had pain and couldn’t move the right wrist which was swollen. The patient was visited at another emergency room and conventional radiographs at right wrist were done: he reported a Salter Harris type II distal radius fracture and ulnar styloid fracture with physeal plate injury. The fractures were treated with cast immobilization for 4 weeks. After removal of cast the patient started physical rehabilitation and passive and active mobilization but he kept feeling pain and he had persistent functional limitation at the wrist. Eight months after the fall he came to our attention with pain and marked reduction of strength and movement of the wrist. An important limitation of wrist’s flexion/extension and reduction of ulnar/radial deviation were observed and the patient was unable to ride. Therefore, an X-ray and CT study were performed (figures 1, 2) and nonunion of distal radius physeal plate was documented. He was operated 5 days later under plexus anaesthesia and antibiotic prophylaxis with first generation cefazolin was administered. The lesion was approached through a volar incision centred over distal radius. There was evidence of fibrous tissue interposed between radial styloid and distal radius so a cleaning of nonunion site was performed until bone fragments bleeding. Fracture was reduced with special instruments under fluoroscopy control (figure 3A and B). After bridging the gap with cancellous bone graft taken from proximal radius osteosynthesis and compression was performed with one 3 mm cannulated screw Asnis (Stryker, Mahwah, NJ, USA) and one K-wire to prevent rotations (figures 3C and 4A and B). The surgery lasted 80 minutes (tourniquet has been maintained for 60 minutes) and the patient was discharged the following day. The wrist joint was initially immobilized with plaster cast for 1 month. After the cast and k-wire has been removed, the patient started rehabilitation program with active and passive mobilizations and progressive strengthening and resistive exercises. Radiographic control performed 2 months from treatment showed bone consolidation and healing of the injury (figure 5A and B). The patient was satisfied and returned to motor race at 3 months from surgery. Nowadays, there are no limitations of strength and of range of motion of the right wrist and no pain has been reported (figure 6A and B).
Figure 1.
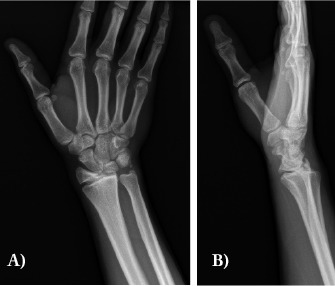
Preoperative X-rays (8 month after fall); AP (A) and LL views (B)
Figure 2.
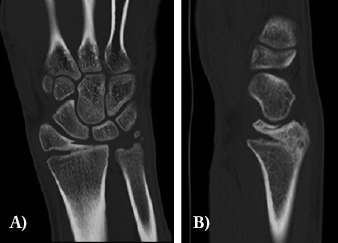
Preoperative CT study with physeal plate nonunion of distal radius; AP (A) and LL views (B)
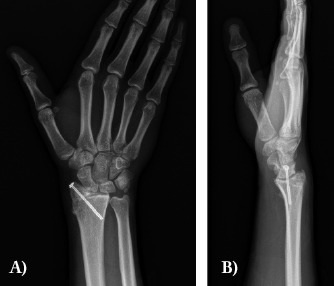
Figure 3.

Intraoperative fluoroscopic controls: reduction of fracture (A); transitory stabilization with K-wire (B); definitive fixation with k-wire and compression screw (C)
Figure 4.

Post-operative X-rays; AP (A) and LL views (B)
Figure 5.
X-rays 2 months after surgery and removal of K-wire; AP (A) and LL views (B)
Figure 6.
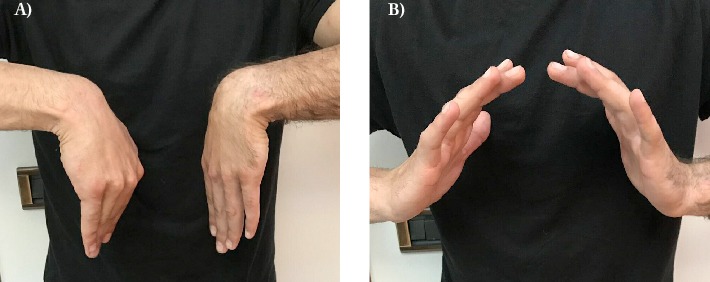
Clinical images 2 months after fixation with good recovery in function
Discussion
Distal radius fractures are the most common orthopaedic injuries that occur in the paediatric and adolescent population. Most of these lesions involves the distal metaphyseal portion of the radius but physeal plates traumas are also commonly seen, with the majority being Salter Harris type I or II fractures (17). The annual incidence of distal radius fractures has increased as a result of earlier participation in sporting activities, increased body mass index, and decreased bone mineral density (1). Distal radius fractures are more frequently sustained after a fall onto an outstretched arm that results in axial compression on the extremity or from direct trauma to the extremity. AP and LL x-ray views of the wrist usually are sufficient to diagnose a distal radius fracture. The management is based on several factors, including patient age, fracture pattern, and the amount of growth remaining. Nonsurgical management is the most common treatment option for patients who have distal radius fractures because marked potential for remodelling exists. If substantial angulation or displacement is present, closed reduction manoeuvres with or without percutaneous pinning should be performed (18).
In adults pseudoarthrosis consequent to distal radius fractures is a rare occurrence but reports in the literature are present. Bacorn and Kurtzke (20) found an incidence of nonunion of 0.2%. Watson-Jones (21) reported only one nonunion out of 3199 distal radius fractures.
This type of nonunion can be observed after internal fixation, external fixation, or non-operative treatment (22) and it has been reported that comorbidities medical conditions such as diabetes, peripheral vascular disease, alcoholism, smoking and obesity may increase its risk (23-25)
An ulnar styloid fracture often occur in association with a distal radial fracture but a meta-analysis by Yuan et al. suggest that it doesn’t affect the outcomes (26). In the same way Zenke et al. showed that the presence of an ulnar styloid fracture does not affect the outcome of a fracture of the distal radius which is stabilized with a volar locking plate (27).
In children, nonunion has been universally related to a pathologic condition of the bone or vascularity (10). Congenital pseudoarthrosis, neurofibromatosis, osteomyelitis and bone loss should be always suspected in a patient with a nonunion after a benign fracture (19). In paediatric fractures, nonunions have been usually reported in diaphyseal regions (28). Pseudoarthrosis following a closed radial or ulnar fracture is extremely rare and to the best of our knowledge only few reports are cited in literature in paediatric age group (29-35).
Kwa et al. in the first ever case reported had described a distal radius nonunion following a closed fracture in an otherwise healthy child (30). This was managed by bone grafting and casting. The factors attributed to nonunion in this report were inadequate immobilization and severe initial displacement. In two other case reports, nonunion in children had been attributed to open surgery (35), soft-tissue or vascular problems (36).
Sivashanmugam et al., focusing on pseudoarthrosis treatment, stressed the great osteogenic potential of the periosteum in children and adolescents. Their case report highlights the possibility of stimulating bony union by distracting the minimally disturbed soft tissue and thick osteogenic periosteal envelope to treat paediatric atrophic nonunion in selected patients (37). In general, in these type of patients excision of the fibrous tissue followed by compression and stabilization are sufficient in order to obtain consolidation.
Debridement of the necrotic bone and either traditional bone grafting, osteoclasis lengthening, vascularised bone grafting, or creation of a single-bone forearm are surgical options and the choice depends on the individual patient (17)
Conclusions
Because of favourable local biological factors, nonunion is rarely seen in distal radius fractures in children and adolescents.
As consequence of the great osteogenic potential of the periosteum in children and adolescents, its treatment usually requires isolated excision of the fibrous tissue and internal fixation.
References
- 1.Bailey DA, Wedge JH, McCulloch RG, Martin AD, Bernhardson SC. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989 Sep;71(8):1225–31. [PubMed] [Google Scholar]
- 2.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001 Sep;26(5):908–15. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 3.Jones IE, Cannan R, Goulding A. Distal forearm fractures in New Zealand children: Annual rates in a geographically defined area. N Z Med J. 2000 Oct;113(1120):443–5. [PubMed] [Google Scholar]
- 4.Landin LA. Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950-1979. Acta Orthop Scand Suppl. 1983;202:1–109. [PubMed] [Google Scholar]
- 5.Worlock P, Stower M. Fracture patterns in Nottingham children. J Pediatr Orthop. 1986 Nov-Dec;6(6):656–60. doi: 10.1097/01241398-198611000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Khosla S, Melton LJ 3rd, Dekutoski MB, Achenbach SJ, Oberg AL, Riggs BL. Incidence of childhood distal forearm fractures over 30 years: a population-based study. JAMA. 2003 Sep;290(11):1479–85. doi: 10.1001/jama.290.11.1479. [DOI] [PubMed] [Google Scholar]
- 7.Skaggs DL, Loro ML, Pitukcheewanont P, Tolo V, Gilsanz V. Increased body weight and decreased radial cross-sectional dimensions in girls with forearm fractures. J Bone Miner Res. 2001 Jul;16(7):1337–42. doi: 10.1359/jbmr.2001.16.7.1337. [DOI] [PubMed] [Google Scholar]
- 8.Peterson CA, Peterson HA. Analysis of the incidence of injuries to the epiphyseal growth plate. J Trauma. 1972 Apr;12(4):275–81. doi: 10.1097/00005373-197204000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Joint Surg Am. 1963 Apr;45(3):587–622. [Google Scholar]
- 10.Cannata G, De Maio F, Mancini F, Ippolito E. Physeal fractures of the distal radius and ulna: long-term prognosis. J Orthop Trauma. 2003 Mar;17(3):172–179. doi: 10.1097/00005131-200303000-00002. discussion 179-80. [DOI] [PubMed] [Google Scholar]
- 11.Alemdaroglu KB, Iltar S, Cimen O, Uysal M, Alagöz E, Atlihan D. Risk factors in redisplacement of distal radialfractures in children. J Bone Joint Surg Am. 2008 Jun;90(6):1224–30. doi: 10.2106/JBJS.G.00624. [DOI] [PubMed] [Google Scholar]
- 12.Bae DS. Pediatric distal radius and forearm fractures. J Hand Surg Am. 2008 Dec;33(10):1911–23. doi: 10.1016/j.jhsa.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Devalia KL, Asaad SS, Kakkar R. Risk of redisplacement after first successful reduction in paediatric distal radius fractures: sensitivity assessment of casting indices. J Pediatr Orthop B. 2011 Nov;20(6):376–81. doi: 10.1097/BPB.0b013e328349212d. [DOI] [PubMed] [Google Scholar]
- 14.Hang JR, Hutchinson AF, Hau RC. Risk factors associated with loss of position after closed reduction of distal radial fractures in children. J Pediatr Orthop. 2011 Jul-Aug;31(5):501–6. doi: 10.1097/BPO.0b013e31821fffc3. [DOI] [PubMed] [Google Scholar]
- 15.McQuinn AG, Jaarsma RL. Risk factors for redisplacement of pediatric distal forearm and distal radius fractures. J Pediatr Orthop. 2012 Oct-Nov;32(7):687–92. doi: 10.1097/BPO.0b013e31824b7525. [DOI] [PubMed] [Google Scholar]
- 16.Proctor MT, Moore DJ, Paterson JM. Redisplacement after manipulation of distal radial fractures in children. J Bone Joint Surg Br. 1993 May;75(3):453–4. doi: 10.1302/0301-620X.75B3.8496221. [DOI] [PubMed] [Google Scholar]
- 17.Schoenecker JG, Bae DS. Fractures of the Distal Radius and Ulna. Rockwood & Wilkins’ fractures in children. In: Flynn JM, Skaggs DL, Waters PM, editors. 8th Edition. Wolters Kluwer; 2015. pp. 349–411. [Google Scholar]
- 18.Dua K, Abzug JM, Sesko Bauer A, Cornwall R, Wyrick TO. Pediatric Distal Radius Fractures. Instr Course Lect. 2017 Feb;66:447–60. [PubMed] [Google Scholar]
- 19.Burgess RC, Watson HK. Hypertrophic ulnar styloid nonunions. Clin Orthop Relat Res. 1988 Mar;228:215–7. [PubMed] [Google Scholar]
- 20.Barcorn RW, Kurztke JF. Colles’ fracture. A study of two thousand cases from the New York State Workmen’s Compensation Board. J Bone Joint Surg Am. 1953 Jul;35-A(3):643–58. [PubMed] [Google Scholar]
- 21.Watson-Jones R. Edinburgh: Churchill Livingstone; 1942. Fractures and other bone and joint injuries. [Google Scholar]
- 22.Ring D. Nonunion of the distal radius. Hand Clin. 2005 Aug;21(3):443–7. doi: 10.1016/j.hcl.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Smith VA, Wright TW. Nonunion of the distal radius. J Hand Surg Br. 1999 Oct;24(5):601–3. doi: 10.1054/jhsb.1999.0267. [DOI] [PubMed] [Google Scholar]
- 24.Ring D, Jupiter JB. Nonunion of the distal radius. Tech Hand Up Extrem Surg. 2002;6:6–9. doi: 10.1097/00130911-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Shinohara T, Hirata H. Distal radius nonunion after volar locking plate fixation of a distal radius fracture: a case report. Nagoya J Med Sci. 2017 Nov;79(4):551–7. doi: 10.18999/nagjms.79.4.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yuan C, Zhang H, Liu H, Gu J. Does concomitant ulnar styloid fracture and distal radius fracture portend poorer outcomes? A meta-analysis of comparative studies. Injury (Int J Care Injured) 2017 Nov;48(11):2575–81. doi: 10.1016/j.injury.2017.08.061. [DOI] [PubMed] [Google Scholar]
- 27.Zenke Y, Sakai A, Oshige T, Moritani S, Nakamura T. The effect of an associated ulnar styloid fracture on the outcome after fixation of a fracture of the distal radius. J Bone Joint Surg Br. 2009 Jan;91(1):102–7. doi: 10.1302/0301-620X.91B1.21026. [DOI] [PubMed] [Google Scholar]
- 28.Shrader MW, Stans AA, Shaughnessy WJ, Haidukewych GJ. Nonunion of fractures in paediatric patients: 15-year experience at a level I trauma center. Orthopedics. 2009 Jun;32(6):410. doi: 10.3928/01477447-20090511-11. [DOI] [PubMed] [Google Scholar]
- 29.Song KS, Lee SW, Bae KC, Yeon CJ, Naik P. Primary nonunion of the distal radius fractures in healthy children. J Pediatr Orthop B. 2016 Mar;25(2):165–69. doi: 10.1097/BPB.0000000000000257. [DOI] [PubMed] [Google Scholar]
- 30.Kwa S, Tonkin MA. Nonunion of a distal radial fracture in a healthy child. J Hand Surg Br. 1997 Apr;22(2):175–77. doi: 10.1016/s0266-7681(97)80056-3. [DOI] [PubMed] [Google Scholar]
- 31.Song KS, Kim HK. Nonunion as a complication of an open reduction of a distal radial fracture in a healthy child: A case report. J Orthop Trauma. 2003 Mar;17(3):231–33. doi: 10.1097/00005131-200303000-00015. [DOI] [PubMed] [Google Scholar]
- 32.Arslan H, Subaşý M, Kesemenli C, Ersuz H. Occurrence and treatment of nonunion in long bone fractures in children. Arch Orthop Trauma Surg. 2002 Dec;122(9-10):494–98. doi: 10.1007/s00402-002-0439-y. [DOI] [PubMed] [Google Scholar]
- 33.Lewallen RP, Peterson HA. Nonunion of long bone fractures in children: a review of 30 cases. J Pediatr Orthop. 1985 Mar-Apr;5(2):135–42. [PubMed] [Google Scholar]
- 34.Shahryar Kamrani R, Farhoud AR, Nabian MH, Farhadi L. Treatment of nonunion of forearm bones using radial forearm bone flap. Trauma Mon. 2015 Nov;20(4):e22622. doi: 10.5812/traumamon.22622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernandez DL, Ring D, Jupiter JB. Surgical management of delayed union and nonunion of distal radius fractures. J Hand Surg Am. 2001 Mar;26(2):201–9. doi: 10.1053/jhsu.2001.22917. [DOI] [PubMed] [Google Scholar]
- 36.Waters P, Bae DS. Fractures of distal radius and ulna. Rockwood and Wilkins Fractures in Children. In: Beaty JH, Kasser JR, editors. Philadelphia: Lippincott Williams and Wilkins; 2009. p. 335. [Google Scholar]
- 37.Sivashanmugam R, Vijay S, Balakumar B. Nonunion in a distal radius metaphyseal fracture in a child: Role of intact periosteal sleeve in management. Indian J Orthop. 2015 Jan-Feb;49(1):109–13. doi: 10.4103/0019-5413.143919. [DOI] [PMC free article] [PubMed] [Google Scholar]


