Abstract
Reverse shoulder arthroplasty (rTSA) is a largely used procedure with a wide variety of indications. The incidence of this surgery is increased in recent years and the literature expects similar trend for the future. Metaphyseal stem rTSA seems to be a promising solution considering major objectives the preservation of humeral bone stock and ease of revision. In our study we analyzed 19 patients treated with cementless metaphyseal stem rTSA for osteoarthritis (group A) and acute fractures (group B). In group A (7 patients) the average Constant score improved from 21,57 (16-29) to 56,85 (38-72), the average SST improved from 2,29 (1-4) to 9,43 (8-12) and the mean VAS score improved from 14,29 to 4,86. In group B (12 patients) the mean Constant-Murlay score at last follow up was 42,17; the average SST was 7 and average pain score was 8,92. Overall active range-of-motion (ROM) improved significantly. Surgical considerations, clinical (analyzing Constant score and Simple Shoulder Test) and radiological short-term outcomes are encouraging, with low rate of complications. Long term follow-up studies are necessary to confirm our findings and the potential benefits related to these implants. (www.actabiomedica.it)
Keywords: shoulder arthroplasty, reverse shoulder arthroplasty (rTSA), range-of-motion (ROM)
Introduction
The incidence of reverse shoulder arthroplasty (rTSA) is lower than hip and knee prostheses (1-3) but the number of implants is increased in last years and this trend should continue due to increasing of high demanding patients, better health care capacity and expanding indications (4-6).
In USA 42% of all shoulder arthroplasties were rTSAs in 2011 (7) with a large use in patients <60 years (8, 9).
Several designs, materials and implant characteristics are available and the indications are in particular glenohumeral osteoarthritis with rotator cuff deficiency and severe humeral head-neck fractures in elderly patients (10-15).
On the basis of these considerations and the necessity to treat often young patients that probably will need also revision surgery, short stem and metaphyseal implant recently emerged (16-22). Short-term studies reported functional and radiological results similar to the gold standard shoulder stemmed implants (16, 23).
The aim of the study is to share our experience and preliminary results with a cementless rTSA with metaphyseal stem in both glenohumeral osteoarthritis and acute fractures.
Materials and methods
Between May 2016 and June 2018 19 patients underwent rTSA by the senior author (G.S.) utilizing a cementless prosthesis with short metaphyseal stem (Verso®; Innovative Design Orthopaedics, London, UK) and also the stemmed version proposed for the treatment of acute fracture.
Seven patients suffer for glenohumeral arthropathy with deficient rotator cuff (Group A - Fig. 1) and twelve patients had acute displaced fractures of the proximal humerus (Four parts or more according to Neer classification) with rotator cuff dysfunction (Group B - Fig. 3).
Figure 1.

Preoperative x-rays
Figure 3.
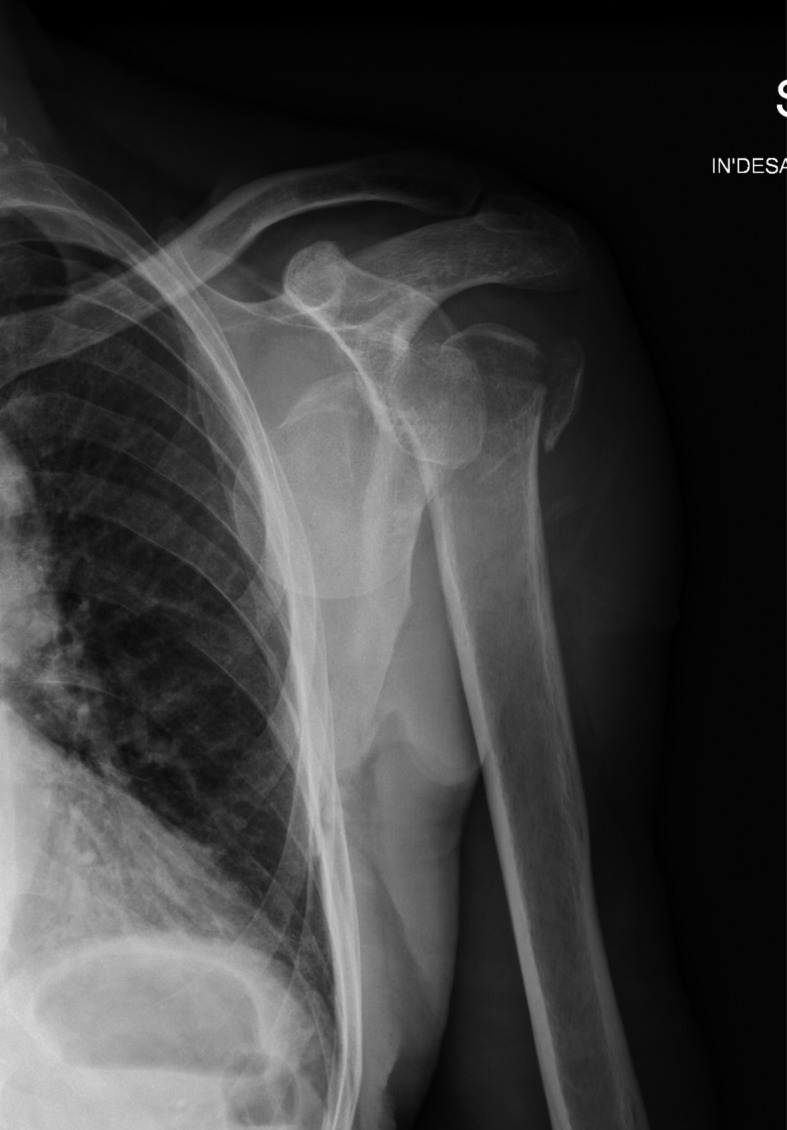
Preoperative x-rays
In group A there were 2 male and 5 females, the mean age at surgery was 77,33 years (range 65-88 years) and the average follow up was 6,43 months (range 5-9 months)
In group B there were 4 males and 8 females, the mean age at surgery was 79 years (range 68-84 years) and the average follow up was 5 months (range 3-9 months).
Surgical Technique
The surgery was performed with the patient in “beach chair” position under general anesthesia with interscalene block (blended technique).
In group A patients all the procedures were performed through the anterosuperior approach to the shoulder (Neviaser-MacKenzie approach) while in group B patients though the deltopectoral approach.
In group A patients any remnants of subscapularis or infraspinatus were detached and tagged with stay sutures.
Minimal proximal humeral bone resection was performed and the cancellous bone was used for bone graft impaction technique as purposed by Levy et al (19) and other authors (24).
In group B after individuation and isolation with stay suture of greater and lesser tuberosity parts, the humeral head was remove and used for bone graft impaction technique.
The humeral stemless component was implanted in group A patients while the humeral stemmed component was used in group B patients.
Good initial press-fit fixation was achieved in all patients.
Standard glenoid component was implanted in all patients.
Tuberosities re-attachment was performed using non-absorbable suture (Orthocord® DePuy Sinthes Raynham, Massachussetts, USA) in all cases when possible.
Postoperative rehabilitation included sling immobilization for 2 weeks followed by passive range-of-motion exercises after 2-3 weeks, active range-of-motion exercises after 4-6 weeks and incorporation of strengthening from week 12-20.
Assessment
Patient evaluation was performed by independent observers pre operatively (only in group A) and at 3,6 and 9 months.
Functional outcome was evaluated with Constant score (pain, activities of daily living, active range of motion and shoulder strength). Range of motion was measured with a goniometer. Active internal rotation was measured as the highest spine level that the patient’s thumb could reach. Patients satisfaction was assessed using the Simple Shoulder Test (SST), a functional questionnaire assessing return to work, sport and leisure activities.
Pain relief was assessed on a 0-15 Visual Analogue Scale (VAS).
Radiograph evaluation was performed analyzing AP and axillary view of the shoulder for any evidence of complication including displacement, migration, subsidence of the implant and appearance of radiolucent lines, osteolysis or sign of stress shielding (Fig. 2, 4).
Figure 2.

Tthree months follow up x-rays
Figure 4.
Six months follow up x-rays
Statistical methods
Statistical analysis was performed using Microsoft Excel (2017 version).
In group A patients improvement in Constant score or SST score were calculated for each case by comparing the latest observed postoperative value against the corresponding preoperative value and the significance of the difference was tested using the paired t test.
Results
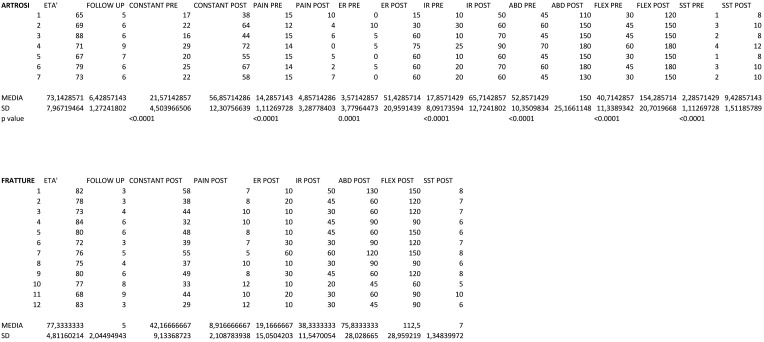
In group A patients the average Constant score improved from 21,57 (16-29) to 56,86 (38-72), the average SST improved from 2,29 (1-4) to 9,43 (8-12) and the mean VAS score improved from 14,29 to 4,86.
All these gains were statistically significant (P<0.001)
Overall active range-of-motion (ROM) improved significantly (Tab. 1).
Table 1.
In group B patients the mean Constant-Murlay score at last follow up was 42,17, the average SST was 7 and average VAS score was 8,92.
Average active range of motion at last follow up is described in table 1.
There were no cases of intraoperative fractures or dislocations in follow-up period.
No findings of subsidence, radiolucent lines around the components and notching at the radiological follow up. No signs of mobilization or position changing over the time of the humeral stem were recognized.
One patient in B group presented axillary nerve palsy after surgery, but it recovery spontaneously within six months.
At the time of the study no patient had undergo to revision surgery.
Discussion
The decision to perform a study analysing both stemmed and unstemmed version of this prosthesis come from the concept that with Verso the surgeon doesn’t have to obtain the cortical press fit with the stem as usually performed with the majority of the available implants (19, 25).
The stemmed version used for the treatment of acute fracture has the same proximal shape of the stemless implant for achieve the primary stability while the distal part works like a “rudder” in particular in complex fracture patterns. The press fit is with metaphyseal cancellous bone in both groups.
We decided to perform the anterosuperior approach in group A patients while the deltopectoral approach in group B patients. The reason is that we usually use the deltopectoral approach for all the other implants and indications and we believe is easier to enlarge distally in case of peri-implant or intraoperative fractures. Nevertheless we observe that the exposition and preparation of the anatomical structures, in particular the glenoid, is better with the anterosuperior approach, that allows to perform also the open acromion-clavicular decompression and the best suture of the posterior cuff to the humeral bone.
In all cases the glenoid preparation is performed carefully, in particular the round movements of the handy reamer should be as gentle as possible because the pressure exerted on the glenoid bone is very high.
In both groups the humeral preparation is conducted saving much cancellous bone possible. The three tapered thin fins give a theoretical immediate methaphyseal press fit fixation as reported in literature (19, 25). The sensation of stability is not always so secure after the insertion of the last humeral punch, in particular in case of fractures when surgical humeral neck is involved.
In this stage a key role is played by the “bone graft impaction technique” (19, 24) that consists in morselize the cancellous bone of the humeral head and put the small pieces inside the metaphysis between first and last humeral punch insertion and before the humeral shell positioning. Thus in combination with the titanium and hydroxyapatite coating of the definitive humeral component give always a sensation of stability to the surgeon in all cases of our series, and allowed us to avoid the use of cement that could complicate any further revision surgery.
In our opinion the highest difficulty is to move from the concept of achieve cortical press fit to methaphyseal cancellous bone press fit and trust in this philosophy.
Analyzing clinical results all patients had good pain relief and statistical significative improvement of Constant-Murlay and SST scores according to the recent literature (26-28). Considering the ROM the outcomes are encouraging, in particular regarding internal and external rotation. Several studies in literature analysing Grammont-type reverse arthroplasties reported poor values of rotation, our results could be positive influenced by the very low medial profile of polyethylene liner combined with the glenoid sphere offset and 30° of humeral shell retroversion as suggested by the technique (19).
In our opinion also the suture of the tuberosities as much as possible in the original anatomic position, is mandatory for obtaining the best ROM after rTSA surgery for both fracture and osteoarthritis patterns (29).
Radiological outcomes are excellent, without any complication (30), probably related to the short-term follow up (9 months maximum). Not in all cases, in particular in group A (shorter stem), the humeral stem was perfectly aligned with the diaphysis, in 2 cases there were small degrees of varus angulation but without any clinical implication.
In one series conducted with the same implant (Verso prosthesis) glenoid notching was observed in 21,4% of patients (19) lower than those reported in other studies on rTSA in literature (31-36). At the follow up time we didn’t observe any case of glenoid notching probably related to the little cohort of patients and follow up duration.
Regarding the case of transitory axillary nerve palsy we hypothesized a strong relationship with high energy trauma. Neurological signs could be underestimated at the admission and the findings at the follow up not related to the surgical procedure. At six months follow up we observe spontaneous recovery of the nerve palsy, with good values of clinical scores and satisfaction.
Conclusions
Analysing the increase number of implants and the widening of the indications, in particular in younger patients, a cementless short stem reverse arthroplasty could be a precious solution in line with the principles of “tissue sparing surgery”. Our preliminary experience has reported positive sensations and encouraging results. More randomized controlled studies about short stem rTSA are necessary and currently under clinical investigation. In our opinion advantages as easier revision with stemmed implant and periprosthetic fracture involving the metaphysis rather than diaphysis are useful and considerable.
References
- 1.Pabinger C, Geissler A. Utilization rates of hip arthroplasty in OECD countries. Osteoarthritis Cartilage. 2014;22(6):734–41. doi: 10.1016/j.joca.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 2.Pabinger C, Lothaller H, Geissler A. Utilization rates of knee-arthroplasty in OECD countries. Osteoarthritis Cartilage. 2015;23(10):1664–73. doi: 10.1016/j.joca.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 3.Schairer WW, Nwachukwu BU, Lyman S, Creig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24(1):91–7. doi: 10.1016/j.jse.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 4.Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE. Understanding of regional variation in the use of surgery. Lancet. 2013;382(9898):1121–9. doi: 10.1016/S0140-6736(13)61215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Villacis D, Sivasundaram L, Pannell WC, Heckmann N, Omid R, Hatch GF 3rd. Complication rate and implant survival for reverse shoulder arthroplasty versus total shoulder arthroplasty: results during the initial 2 years. J Shoulder Elbow Surg. 2016;25(6):927–35. doi: 10.1016/j.jse.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 6.Beltrame A, Di Benedetto P, Salviato D, Niccoli G, Gisonni R, Cainero V, Causero A. The SMR reverse shoulder arthroplasty in rotator cuff arthropathy management. Acta Biomed. 2017;88(4S):81–89. doi: 10.23750/abm.v88i4-S.6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014;15:4. doi: 10.1186/1471-2474-15-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jain NB, Yamaguchi K. The contribution of reverse shoulder arthroplasty to utilization of primary shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23:1905–12. doi: 10.1016/j.jse.2014.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wagner ER, Chang MJ, Welp KM, Solberg MJ, Hunt TJ, Woodmass JM, Higgins LD, Warner JJP. The impact of the reverse prosthesis on revision shoulder arthroplasty: analysis of a high-volume shoulder practice. J Shoulder Elbow Surg. 2018;S1058(2746(18)30597-4) doi: 10.1016/j.jse.2018.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Mata-Fink A, Meinke M, Jones C, Kim B, Bell JE. Reverse shoulder arthroplasty for treatment of proximal humeral fractures in older adults: a systematic review. J Shoulder Elbow Surg. 2013;22(12):1737–48. doi: 10.1016/j.jse.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 11.Szerlip BW, Morris BJ, Edwards TB. Reverse Shoulder Arthroplasty for Trauma: When, Where, and How. Instr Course Lect. 2016;65:171–9. [PubMed] [Google Scholar]
- 12.Lübbeke A, Rees JL, Barea C, Combescure C, Carr AJ, Silman AJ. International variation in shoulder arthroplasty. Acta Orthop. 2017;88(6):592–599. doi: 10.1080/17453674.2017.1368884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holton J, Yousri T, Arealis G, Levy O. The Role of Reverse Shoulder Arthroplasty in Management of Proximal Humerus Fractures with Fracture Sequelae: A Systematic Review of the Literature. Orthop Rev (Pavia) 2017;9(1):6977. doi: 10.4081/or.2017.6977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merolla G, Walch G, Ascione F, Paladini P, Fabbri E, Padolino A, Porcellini G. Grammont humeral design versus onlay curved-stem reverse shoulder arthroplasty: comparison of clinical and radiographic outcomes with minimum 2-year follow-up. J Shoulder Elbow Surg. 2018;27(4):701–710. doi: 10.1016/j.jse.2017.10.016. [DOI] [PubMed] [Google Scholar]
- 15.Tashjian RZ, Chalmers PN. Future Frontiers in Shoulder Arthroplasty and the Management of Shoulder Osteoarthritis. Clin Sports Med. 2018;37(4):609–630. doi: 10.1016/j.csm.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Razfar N, Reeves JM, Langohr DG, Willing R, Athwal GS, Johnson JA. Comparison of proximal humeral bone stresses between stemless, short stem, and standard stem length: a finite element analysis. J Shoulder Elbow Surg. 2016;25(7):1076–83. doi: 10.1016/j.jse.2015.11.011. [DOI] [PubMed] [Google Scholar]
- 17.Churchill RS, Athwal GS. Stemless shoulder arthroplasty – current results and designs. Curr Rev Musculoskelet Med. 2016;9(1):10–6. doi: 10.1007/s12178-016-9320-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawi N, Tauber M, Messina MJ, Habermeyer P, Martetschläger F. Anatomic stemless shoulder arthroplasty and related outcomes: a systematic review. BMC Musculoskelet Disord. 2016;17(1):376. doi: 10.1186/s12891-016-1235-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levy O, Narvani A, Hous N, Abraham R, Relwani J, Pradhan R, Bruguera J, Sforza G, Atoun E. Reverse shoulder arthroplasty with a cementless short metaphyseal humeral implant without a stem: clinical and radiologic outcomes in prospective 2- to 7-year follow-up study. J Shoulder Elbow Surg. 2016;25(8):1362–70. doi: 10.1016/j.jse.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 20.Keener JD, Chalmers PN, Yamaguchi K. The Humeral Implant in Shoulder Arthroplasty. J Am Acad Orthop Surg. 2017;25(6):427–438. doi: 10.5435/JAAOS-D-15-00682. [DOI] [PubMed] [Google Scholar]
- 21.Lazarus MD, Cox RM, Murthi AM, Levy O, Abboud JA. Stemless Prosthesis for Total Shoulder Arthroplasty. J Am Acad Orthop Surg. 2017;25(12):e291–e300. doi: 10.5435/JAAOS-D-17-00088. [DOI] [PubMed] [Google Scholar]
- 22.Santos B, Quental C, Folgado J, Sarmento M, Monteiro J. Bone remodelling of the humerus after a resurfacing and a stemless shoulder arthroplasty. Clin Biomech (Bristol, Avon) 2018;59:78–84. doi: 10.1016/j.clinbiomech.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 23.Habermeyer P, Lichtenberg S, Tauber M, Magosch P. Midterm results of stemless shoulder arthroplasty: a prospective study. J Shoulder Elbow Surg. 2015;24(9):1463–72. doi: 10.1016/j.jse.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 24.Plachel F, Scheibel M. Humeral bone grafting in stemless shoulder arthroplasty. Obere Extrem. 2017;12(3):183–185. doi: 10.1007/s11678-017-0424-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Atoun E, Van Tongel A, Hous N, Narvani A, Relwani J, Abraham R, Levy O. Reverse shoulder arthroplasty with a short metaphyseal humeral stem. Int Orthop. 2014;38(6):1213–8. doi: 10.1007/s00264-014-2328-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moroder P, Ernstbrunner L, Zweiger C, Schatz M, Seitlinger G, Skursky R, Becker J, Resch H, Krifter RM. Short to mid-term results of stemless reverse shoulder arthroplasty in a selected patient population compared to a matched control group with stem. Int Orthop. 2016;40(10):2115–20. doi: 10.1007/s00264-016-3249-5. [DOI] [PubMed] [Google Scholar]
- 27.Wolfensperger F, Grüninger P, Dietrich M, Völlink M, Benninger E, Schläppi M, Meier C. Reverse shoulder arthroplasty for complex fractures of the proximal humerus in elderly patients: impact on the level of independency, early function, and pain medication. J Shoulder Elbow Surg. 2017;26(8):1462–8. doi: 10.1016/j.jse.2017.01.021. [DOI] [PubMed] [Google Scholar]
- 28.Singhal K, Rammohan R. Going forward with reverse shoulder arthroplasty. J Clin Orthop Trauma. 2018;9(1):87–93. doi: 10.1016/j.jcot.2017.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gallinet D, Ohl X, Decroocq L, Dib C, Valenti P, Boileau P. French Society for Orthopaedic Surgery (SOFCOT). Is reverse total shoulder arthroplasty more effective than hemiarthroplasty for treating displaced proximal humerus fractures in older adults? A systematic review and meta-analysis. Orthop Traumatol Surg Res. 2018;104(6):759–66. doi: 10.1016/j.otsr.2018.04.025. [DOI] [PubMed] [Google Scholar]
- 30.Grey B, Rodseth RN, Roche SJ. Humeral Stem Loosening Following Reverse Shoulder Arthroplasty: A Systematic Review and Meta-Analysis. JBJS Rev. 2018;6(5):e5. doi: 10.2106/JBJS.RVW.17.00129. [DOI] [PubMed] [Google Scholar]
- 31.Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics. 2002;25(2):129–33. doi: 10.3928/0147-7447-20020201-16. [DOI] [PubMed] [Google Scholar]
- 32.De Wilde LF, Van Ovost E, Uyttendaele D, Verdonk R. Results of an inverted shoulder prosthesis after resection for tumor of the proximal humerus. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(4):373–8. [PubMed] [Google Scholar]
- 33.Favard L, Lautmann S, Sirveaux F, Oudet D, Kerjean Y, Huguet D. Hemi arthroplasty versus reverse arthroplasty in the treatment of osteoarthritis with massive cuff tear. Shoulder prosthesis: two to ten year follow-up. In: Walch G, Boileau P, Mole D, editors. Montpellier, France: Sauramps Medical; 2001. pp. 261–8. [Google Scholar]
- 34.Lévigne C, Garret J, Boileau P, Alami G, Favard L, Walch G. Scapular notching in reverse shoulder arthroplasty: is it important to avoid it and how? Clin Orthop Relat Res. 2011;469(9):2512–20. doi: 10.1007/s11999-010-1695-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Melis B, DeFranco M, Lädermann A, Molé D, Favard L, Nérot C, Maynou C, Walch G. An evaluation of the radiological changes around the Grammont reverse geometry shoulder arthroplasty after eight to 12 years. J Bone Joint Surg Br. 2011;93(9):1240–6. doi: 10.1302/0301-620X.93B9.25926. [DOI] [PubMed] [Google Scholar]
- 36.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg. 2011;20(1):146–57. doi: 10.1016/j.jse.2010.08.001. [DOI] [PubMed] [Google Scholar]