Key Points
Question
To what extent do clinicians and surrogates in intensive care units incorporate critically ill patients’ values and preferences into treatment decisions?
Findings
In this secondary analysis of a cohort study, 249 clinician-family intensive care unit conferences were analyzed for statements that exchanged information about incapacitated patients’ treatment preferences and health-related values and applied them to deliberation and treatment planning. Most conferences lacked adequate communication, particularly in terms of deliberating about patients’ values and preferences and applying them to treatment decisions.
Meaning
Interventions are needed to better prepare surrogates for these difficult conversations and to improve clinicians’ communication skills.
Abstract
Importance
Little is known about whether clinicians and surrogate decision makers follow recommended strategies for shared decision making by incorporating intensive care unit (ICU) patients’ values and preferences into treatment decisions.
Objectives
To determine how often clinicians and surrogates exchange information about patients’ previously expressed values and preferences and deliberate and plan treatment based on these factors during conferences about prognosis and goals of care for incapacitated ICU patients.
Design, Setting, and Participants
A secondary analysis of a prospective, multicenter cohort study of audiorecorded clinician-family conferences between surrogates and clinicians of 249 incapacitated, critically ill adults was conducted. The study was performed between October 8, 2009, and October 23, 2012. Data analysis was performed between July 2, 2014, and April 20, 2015. Patient eligibility criteria included lack of decision-making capacity, a diagnosis of acute respiratory distress syndrome, and predicted in-hospital mortality of 50% or more. In addition to the patients, 451 surrogates and 144 clinicians at 13 ICUs at 6 US academic and community medical centers were included.
Main Outcomes and Measures
Two coders analyzed transcripts of audiorecorded conversations for statements in which clinicians and surrogates exchanged information about patients’ treatment preferences and health-related values and applied them in deliberation and treatment planning.
Results
Of the 249 patients, 134 (54.9%) were men; mean (SD) age was 58.2 (16.5) years. Among the 244 conferences that addressed a decision about goals of care, 63 (25.8%; 95% CI, 20.3%-31.3%) contained no information exchange or deliberation about patients’ values and preferences. Clinicians and surrogates exchanged information about patients’ values and preferences in 167 (68.4%) (95% CI, 62.6%-74.3%) of the conferences and specifically deliberated about how the patients’ values applied to the decision in 108 (44.3%; 95% CI, 38.0%-50.5%). Important end-of-life considerations, such as physical, cognitive, and social functioning or spirituality were each discussed in 87 (35.7%) or less of the conferences; surrogates provided a substituted judgment in 33 (13.5%); and clinicians made treatment recommendations based on patients’ values and preferences in 20 conferences (8.2%).
Conclusions and Relevance
Most clinician-family conferences about prognosis and goals of care for critically ill patients appear to lack important elements of communication about values and preferences, with robust deliberation being particularly deficient. Interventions may be needed to better prepare surrogates for these conversations and improve clinicians’ communication skills for eliciting and incorporating patients’ values and preferences into treatment decisions.
This secondary analysis of a cohort study examines communications between clinicians and surrogate decision makers on what the surrogates believe reflect the goals of care of critically ill patients.
Introduction
Critical care medicine’s rapidly advancing technology can help seriously ill patients sustain a life that they value at all costs, recover to a meaningful quality of life, or prolong their functional impairment at the end of life.1,2,3,4,5 This range of outcomes is possible because what constitutes a meaningful life, a good death, or intolerable suffering is personal. Because most critically ill patients are incapacitated and unable to communicate these values, their families and friends typically represent them as surrogate decision makers. International critical care societies recommend that clinicians and surrogates make health care decisions together using a process of shared decision making.6 Shared decision making consists of 3 elements: (1) information exchange about both clinical (ie, diagnosis, prognosis, and treatment options) and personal (ie, patients’ values and preferences) topics, (2) deliberation about how to apply patients’ values to the clinical situation, and (3) development of a treatment plan that respects patients’ preferences. Identifying and discussing patients’ values (ie, what is important to them) and preferences (ie, what treatment they want) are essential to shared, patient-centered decision making.
Previous research suggests that clinicians and surrogates do not follow existing recommendations for incorporating patients’ values and preferences in 12% to 50% of intensive care unit (ICU) family conferences about goals of care.7,8,9,10,11,12 These studies have several limitations. First, most were conducted with relatively small sample sizes in single regions of the United States. Second, some were conducted in simulation rather than actual practice. Third, these analyses provided limited insight about the extent to which clinicians and families incorporate information about patients’ values and preferences into deliberations and treatment planning.
We conducted a secondary analysis of a multicenter study of audiorecorded ICU family conferences to quantify the frequency and scope of information exchange, deliberation, and treatment planning related to the values and preferences of incapacitated patients at high risk of death.
Methods
Description of Parent Study
This secondary analysis evaluated data originally collected in a prospective cohort study designed to identify effective strategies for disclosing prognosis to surrogate decision makers of incapacitated, critically ill patients. Data collection occurred in 13 ICUs at 6 US academic and community medical centers between October 8, 2009, and October 23, 2012. Data analysis was performed between July 2, 2014, and April 20, 2015. Institutional review boards at University of California at San Francisco, Fresno; University of Washington; University of California, San Francisco; University of North Carolina at Chapel Hill; University of Pittsburgh; and Baystate Medical Center approved the study protocol. All participants or their surrogates provided written informed consent. Both participants and health care professionals received financial compensation
A full description of study methods has been published.13,14,15 To be eligible, patients (1) lacked decision-making capacity, as judged by the patient’s attending physician; (2) met conventional diagnostic criteria for acute respiratory distress syndrome; (3) had Acute Physiology Assessment and Chronic Health Evaluation II scores higher than 25, predicting 50% or greater in-hospital mortality; and (4) had 1 or more available family member or friend to represent them as a surrogate decision maker (hereafter termed family or surrogate). We included clinician-family conferences that took place on a weekday and were conducted in English.
Researchers recorded clinician-family conferences in which clinicians anticipated discussing patients’ prognosis and experienced medical transcriptionists transcribed the conversations. To ensure that conferences contained decision making about goals of care, we coded for evidence of decision making about resuscitation, life-support therapies, and treatment limitations; clinicians and surrogates discussed such treatment options in 98.0% of the recorded conferences (eTable in the Supplement). Trained study personnel abstracted patients’ demographic and clinical data from medical records. Clinicians and surrogates completed questionnaires providing their demographic data.
Measurements
We developed a quantitative coding scheme following Crabtree and Miller’s template method16 and a published framework for discussing incapacitated patients’ values and preferences with surrogate decision makers17 (Figure 1). Using this framework allowed us to describe the extent to which clinicians and surrogates explicitly followed recommended practices. A priori, we decided to code for maximal inclusiveness regarding whether patients’ values and preferences were discussed. Therefore, values were broadly defined as a patient’s lifestyle, activities, attitudes, beliefs, and feelings about what makes life worth living, including prior vocation, family ties, substance use, hobbies, functional status, and personality traits. Preferences refer to a patient’s previously stated wishes about life-extending treatments (ie, oral or written advance directives).18
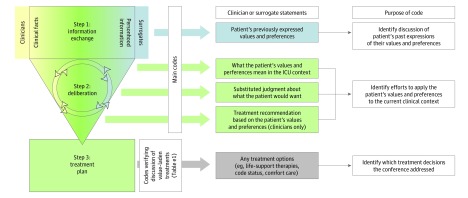
Figure 1. Main Coding Scheme and the Elements of Shared Decision Making.
The left-hand side shows the process of shared decision making. During information exchange, clinicians share clinical facts (ie, diagnosis, prognosis, treatment options [yellow]) and surrogates share personhood information (ie, values and preferences [blue]). During deliberation, they discuss how to apply the information to the decisions at hand, blending clinical and personhood information (green). The goal of this process is a patient-centered treatment plan (green). The center shows the main coding scheme, which focuses on communication about the patient’s values and preferences (blue and green), as well as secondary codes to verify that value-laden treatments were discussed. The right-hand column describes the purpose of each code.
A statement was any length of speech by an interlocutor that addressed a single idea. Therefore, an individual speech turn could receive multiple codes. To describe information exchange, we coded clinicians’ and surrogates’ statements about patients’ health-related values and past expressions of treatment preferences. To describe deliberation and treatment planning, we coded statements in which clinicians or surrogates attempted to apply patients’ values and preferences to the current clinical context. The 3 deliberative strategies included attempts to interpret how the patient might feel about the prognosis and treatment options based on his values and preferences (eg, “He would hate being attached to machines.”); statements about what treatment the patient might choose based on their values and preferences (ie, the surrogate’s substituted judgment, eg, “He would want us to stop life support and let him go.”); and clinicians’ treatment recommendations based on patients’ values and preferences (eg, “Based on what you’re telling me about how independent he is and how hard it’s been for him to accept help at home, I’m afraid we’re not going to get him back to a quality of life that’s acceptable to him. Perhaps we should consider making him comfortable.”) We did not develop separate codes for deliberation vs treatment planning because they were operationally indistinguishable in these conferences. Table 1 provides sample statements for each code.
Table 1. Sample Statements.
| Element of Shared Decision Making | Sample Statements | |
|---|---|---|
| Clinician | Surrogate | |
| Information exchange about values and preferences |
|
|
| Deliberation about values and preferences | ||
| Strategy 1: Interpreting how the patient might feel about the prognosis and treatment options |
|
|
| Strategy 2: Asking for/providing a substituted judgment about what treatment the patient might choose |
|
|
| Strategy 3: Making a treatment recommendation based on patient values and preferences |
|
|
Abbreviation: NA, not applicable.
Applies to clinicians only.
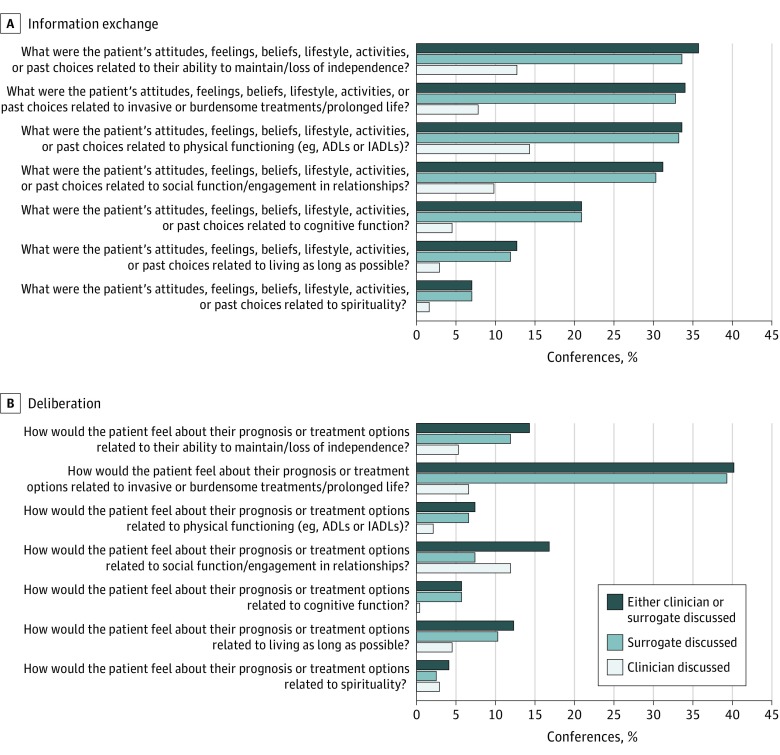
We subcoded for discussion of 7 categories of values, developed a priori based on the literature about what many patients near the end of life judge to be important (Figure 2).19,20,21,22,23 Statements received multiple codes if they addressed several values.
Figure 2. Frequency of Information Exchange and Deliberation in Clinician–Family Conferences (n = 244).
Information exchange (A) and (B) deliberation about common end-of-life values. ADLs, activities of daily living; IADLs, instrumental ADLs.
Coder Training and Coding Procedures
We used Atlas.ti, version 6.2 (Atlas.ti), for transcript data management. Two trained coders (L.P.S. and N.C.E.) initially coded a subset of 5 transcripts line by line, resolving any differences by discussion. We then used a bank of coded statements8 to test interrater reliability both before beginning to code (summary κ = 0.92) and midway through coding to assess for coder drift (summary κ = 0.89). The individual κ values for each of the main codes in Figure 1 were 0.78 or higher.
All transcripts were coded once. The 2 coders then reviewed all statements, discussed any differences, and resolved discrepancies by consensus.
Statistical Analysis
We used Stata, version 13.0 (StataCorp), to conduct all descriptive and inferential analyses. Proportions and 95% CIs were calculated based on whether the code was present vs absent at the conference level. We then computed means (SDs), medians, and interquartile ranges (IQRs) for the number of coded statements per conference. We used the Wilcoxon rank-sum test to test for associations between the number of deliberative statements in the conference and the presence of a treatment recommendation based on the patient’s values and preferences. Testing was 2-tailed, with a P value <.05 considered significant.
Results
Table 2 describes the study population. Overall, 275 of 405 (67.9%) eligible patients were enrolled in the parent study; 130 patients were not included because 21 clinicians and 109 surrogates declined to participate. Of 275 enrolled patients, 249 had an audiorecorded clinician-family conversation, which involved 450 surrogates and 141 clinicians.
Table 2. Patient, Surrogate, and Clinician Characteristics.
| Characteristic | No. (%) | ||
|---|---|---|---|
| Patient (n = 249) | Surrogate (n = 450)a | Clinician (n = 141)b | |
| Male | 134 (54.9) | 155 (34.4) | 97 (68.8) |
| Race/ethnicity | |||
| Non-Hispanic white | 182 (74.6) | 340 (75.6) | 99 (70.2) |
| Non-Hispanic black | 29 (11.9) | 46 (10.2) | 5 (3.6) |
| Hispanic | 21 (8.6) | 42 (9.3) | 7 (5.0) |
| Asian/Pacific Islander | 8 (3.3) | 14 (3.1) | 25 (17.7) |
| Native American | 1 (0.4) | 1 (0.2) | 0 |
| Other/undocumented | 3 (1.2) | 7 (1.6) | 5 (3.5) |
| Age, mean (SD), y | 58.2 (16.5) | 49.4 (13.9) | 5 (3.5) |
| Admission source | |||
| Home | 130 (53.3) | NA | NA |
| Acute care facility | 96 (39.3) | NA | NA |
| Nursing facility | 11 (4.5) | NA | NA |
| Other | 4 (1.6) | NA | NA |
| Admission diagnosis | |||
| Cardiovascular or cardiovascular surgery | 87 (35.7) | NA | NA |
| Gastrointestinal or gastrointestinal surgery | 12 (4.9) | NA | NA |
| Genitourinary | 3 (1.2) | NA | NA |
| Hematologic | 1 (0.4) | NA | NA |
| Metabolic | 2 (0.8) | NA | NA |
| Neurologic or neurologic surgery | 11 (4.5) | NA | NA |
| Respiratory | 103 (42.2) | NA | NA |
| Trauma | 23 (9.4) | NA | NA |
| Other | 2 (0.8) | NA | NA |
| APACHE II score on day of conference, mean (SD) | 26.7 (6.7) | NA | NA |
| No. of ICU days at the time of conference, mean (SD) | 6.1 (3.3) | NA | NA |
| Died during this hospitalization | 108 (44.3) | NA | NA |
| Surrogate relationship to patient | |||
| Spouse/partner | NA | 99 (22.0) | NA |
| Child | NA | 162 (36.0) | NA |
| Sibling | NA | 55 (12.2) | NA |
| Parent | NA | 64 (14.2) | NA |
| Other relative | NA | 58 (12.9) | NA |
| Other relationship | NA | 11 (2.4) | NA |
| Not answered | NA | 1 (0.2) | NA |
| Surrogate educational level | |||
| Less than high school diploma | NA | 40 (8.9) | NA |
| High school diploma | NA | 113 (25.1) | NA |
| Some or all college | NA | 214 (47.6) | NA |
| Graduate or professional school | NA | 82 (18.2) | NA |
| Not answered | NA | 1 (0.2) | NA |
| Religiosity | |||
| Not religious | NA | 33 (7.3) | 31 (22.0) |
| Somewhat religious | NA | 65 (14.4) | 42 (29.8) |
| Religious | NA | 140 (31.1) | 43 (30.5) |
| Very religious | NA | 210 (46.7) | 24 (17.0) |
| Not answered | NA | 2 (0.4) | 1 (0.7) |
| Clinician staff position | |||
| Attending physician | NA | NA | 72 (51.1) |
| Fellow | NA | NA | 40 (28.4) |
| Resident | NA | NA | 27 (19.2) |
| Nurse practitioner | NA | NA | 2 (1.4) |
| Clinician medical specialtyc | |||
| Anesthesia | NA | NA | 6 (5.4) |
| Neurology | NA | NA | 1 (0.8) |
| Surgery | NA | NA | 23 (20.5) |
| Internal medicine | NA | NA | 74 (66.1) |
| Internal medicine and anesthesia | NA | NA | 3 (2.7) |
| Internal medicine and pediatrics | NA | NA | 2 (1.8) |
| None/not answered | NA | NA | 4 (3.6) |
| Clinician years in practice, mean (SD) | NA | NA | 8.6 (9.6) |
Abbreviations: APACHE, Acute Physiology Assessment and Chronic Health Evaluation; ICU, intensive care unit.
A total of 456 surrogates of 244 patients participated in the audiorecorded conferences, but 6 did not complete the baseline questionnaire, leaving 450.
A total of 142 unique clinicians of 244 patients participated in the audiorecorded conferences, but 1 did not complete the baseline questionnaire, leaving 141.
Applicable only if the clinician was an attending or fellow (n = 112).
Mean (SD) patient age was 58.2 (16.5) years; 134 patients (54.9%) were men, and 182 (74.6%) were non-Hispanic white. A total of 130 patients (53.3%) were admitted from home. One hundred eight patients (44.3%) died in the hospital. Mean age of the surrogate decision makers was 49.4 (13.9) years; 155 (34.4%) were men; and 261 (57.9%) were spouses or children of the patient. A total of 214 surrogates (47.6%) had at least some college education, and 350 (77.6%) described themselves as religious or very religious. Clinicians included attendings (72 [51.1%]), trainees (67 [47.5%]), and nurse practitioners (2 [1.4%]), of whom 86 (61.0%) were from nonsurgical specialties. Conferences occurred on ICU day 5.
Five of 249 (2.0%) conferences did not contain any discussion of goals of care (eTable in the Supplement). Thus, the reported statistics describe the 244 conferences in which goals of care were discussed. Among these 244 conferences, 63 (25.8%; 95% CI, 20.3%-31.3%) contained no information exchange or deliberation about patients’ values and preferences.
Information Exchange About Patients’ Values and Preferences
In 167 (68.4%; 95% CI, 62.6%-74.3%) conferences, clinicians and surrogates exchanged information about the patient’s values and preferences. Within these conferences, clinicians asked a mean of 2.3 (median 1; interquartile range [IQR], 0-3) questions about patients’ values and preferences, and surrogates made a mean of 5.2 (median, 4; IQR, 2-7) statements reporting them. Further data are reported in Table 3.
Table 3. Frequency of Information Exchange and Deliberation About Patients’ Values and Preferences by Clinicians and Surrogates.
| Element of Shared Decision Making | Clinicians | Surrogates | Overall |
|---|---|---|---|
| Exchanged information About Patients’ Values and Preferences | |||
| Conferences, No. (%) | 106 (43.4) | 165 (67.6) | 167 (68.4) |
| Statements per conference among conferences with discussion, mean (SD) | 2.3 (3.6) | 5.2 (4.8) | 7.5 (7.8) |
| Deliberated About Patients’ Values and Preferences | |||
| Interpreted how patient might feel about the prognosis and treatment options | |||
| Conferences, No. (%) | 43 (17.6) | 79 (32.4) | 91 (37.3) |
| Statements per conference among conferences with discussion, mean (SD) | 0.7 (1.3) | 1.6 (1.6) | 2.3 (2.4) |
| Asked for/provided a substituted judgment about what treatment the patient might choose | |||
| Conferences, No. (%) | 40 (16.4) | 33 (13.5) | 50 (20.5) |
| Statements per conference among conferences with discussion, mean (SD) | 0.6 (1.1) | 0.5 (1.0) | 1.1 (1.8) |
| Made a recommendation based on patient values and preferences | |||
| Conferences, No. (%) | 20 (8.2) | NAa | NAa |
| Statements per conference among conferences with discussion, mean (SD) | 0.3 (0.6) | NAa | NAa |
Abbreviation: NA, not applicable.
Making a treatment recommendation applies to clinicians only.
The most commonly discussed values were independence, including willingness to live in a nursing home (87 [35.7%]), and avoiding burdensome treatments, including prolonged life support (83 [34.0%]) (Figure 2A). Many statements were general; for example, some families talked about patients’ level of functioning prior to hospitalization, saying things such as, “It's been years [since she was healthy] … It's always been something that's been preventing her from being active,” without explicitly addressing how patients felt about or coped with impaired functioning or reduced independence. In 20 (8.2%) conferences, the discussion was so general that it did not fit any of the 7 value categories. In these cases, conversation most typically centered on quality of life without specifying what constituted quality of life for that patient. For example, clinicians often asked questions such as, “[So] life was rich and full for her?” without exploring what made it that way.
Applying Values and Preferences to Decisions
In 136 (55.7%; 95% CI, 49.5%-62.0%) conferences, there was no deliberation about how to apply patients’ values and preferences in the current clinical situation. Among the 108 (44.3%; 95% CI, 38.0%-50.5%) conferences with some deliberation, clinicians made a mean of 1.6 (median, 1; IQR, 0-2) statements and surrogates made a mean of 2.1 (median, 1; IQR 1-3) statements about applying patients’ values and preferences to the current situation. Among these 108 conferences containing deliberation, clinicians used 1 of the 3 deliberative strategies in 37 (34.3%), 2 strategies in 24 (22.2%), and all 3 in 6 (5.6%) conferences, and surrogates offered deliberations without clinician facilitation in 41 (38.0%).
The most commonly used deliberative strategy was discussing how to interpret patients’ values and preferences in the current clinical situation (91 [37.3%] conferences). In 21 (8.6%) conferences, deliberations were generally about whether the likely outcome represented an acceptable quality of life, without specifying what would be acceptable or unacceptable about it. Of the 7 categories of values commonly important to patients near the end of life, discussions most often addressed how patients would feel about dying or being on prolonged life support (Figure 2B). Only 18 (7.4%) and 14 (5.7%) of the conferences, respectively, contained discussion of how patients would feel about living with prolonged physical or cognitive/emotional impairment.
Clinicians asked surrogates to make a substituted judgment about what treatment patients would choose 64 times within 40 (16.4%) conferences. In 2 of these conferences, the clinician was clarifying a substituted judgment the surrogate had already provided. In an additional 12 conferences, surrogates answered with a substituted judgment. In the remaining 26 conferences, the conversation turned to a different subject without the surrogate providing a substituted judgment.
In 20 (8.2%) conferences, clinicians provided a treatment recommendation based on surrogates’ statements about patients’ values and preferences. These 20 conferences contained significantly more deliberative statements than those with deliberation but no treatment recommendation (mean, 6.3 [median, 6, IQR, 3-8] vs mean, 3.1 [median, 2, IQR, 1-4], P = .001, using Wilcoxon rank-sum test), indicating a strong association between more extensive deliberation and a patient-centered treatment recommendation. Of these, 3 included a reference to a prior conversation about the patient’s values and preferences, 1 responded directly to the values and preferences from information exchange, 5 occurred after deliberation about how to interpret the patient’s values and preferences, and 11 occurred after both deliberation about interpreting the patient’s values and preferences as well as discussion of a substituted judgment.
Discussion
In this large, multicenter study, there was no discussion of patients’ values and preferences in 63 (25.8%) clinician-family conferences about prognosis and goals of care. Furthermore, when discussion was present, it was often limited, especially in regard to deliberations: the median number of deliberative statements by clinicians was 1.6 and surrogates was 2.1; discussion of common end-of-life values was not systematic, with the patient's values related to physical, cognitive, and social functioning each discussed in 35.7% or less of the conferences; and only 8.2% resulted in clinicians explicitly basing a treatment recommendation on patients' values and preferences. These results suggest that clinicians and surrogates do not talk about patients’ values and preferences, making shared decision making impossible.
These findings expand on previous research showing that a significant proportion of clinician-family conferences about life-support decisions lack adequate communication about incapacitated, critically ill patients’ values and preferences.7,8,9,10,11,12 First, the size and diversity of our multicenter sample increased the likelihood that the results are generalizable to other institutions and populations across the country. Second, although prior research has focused on the presence or absence of discussion about patients’ values and preferences, our study delved deeper into the structure and content of those discussions.
Structurally, we found that information exchange about patients’ values and preferences occurred more often than explicit deliberation about how to apply them in the current clinical situation. Although deliberations tended to be brief, conferences that contained lengthier deliberations about how to interpret patients’ values and preferences in the current clinical context were more likely to result in clinicians making a patient-centered treatment recommendation. Overall, this finding suggests that explicit discussion about how to interpret patients' values and preferences in light of the clinical situation may be an important deliberative strategy for generating a patient-centered treatment plan. Further research is needed to assess association between questions such as, “How would your dad feel about having to go through a prolonged course of rehabilitation, probably in a nursing facility?” with the quality of shared decision making.24
In terms of content, we found that conversations frequently omitted considerations important to patients at high risk of death, especially those related to an acceptable level of functioning and quality of life. Without this information, clinicians cannot make patient-centered recommendations and surrogates cannot understand how treatments may reflect important patient values.25 One possible reason clinicians do not discuss these levels is that they are not explicitly thinking about the relationship between prognosis or treatment options and values and preferences. Starting to do so may help clinicians facilitate more patient-centered conversations. Engaging surrogates in robust deliberation that connects patients’ end-of-life values with a treatment plan may help clinicians feel more comfortable that surrogates understand the quality-of-life implications of their decisions. Including the surrogates may also mitigate many of their barriers to decision making, such as accepting a poor prognosis, understanding the risks and benefits of treatments, and agreeing on goals of care.26
There are several research and clinical implications of our findings. First, interventions should be developed to better prepare surrogates for these difficult conversations—a major focus of advance care planning research.27 Second, interventions are needed to teach clinicians communication skills for eliciting patients’ values and preferences and then incorporating them into a treatment plan. Third, increased awareness that patients’ values and preferences tend to be a blind spot in these conversations may prompt clinicians to discuss them. Until evidence from more definitive studies is available, we suggest that clinicians use 3 techniques: (1) asking what was important to patients about their previous functioning and quality of life, (2) asking how patients would feel about their expected level of function and lifestyle if they survive critical illness, and (3) providing (with surrogates’ permission) a treatment recommendation that draws on preceding conversation about patients’ values and preferences. This approach is supported by literature showing that palliative care clinicians help families understand prognostic information in light of patients’ values,28 family satisfaction is higher when the family talks more,29 and empowering patients and families is essential for shared decision making.30,31,32 A number of models are available to teach clinicians how to have these conversations.33
Limitations
Our study has several limitations. First, only 1 clinician-family conference was recorded for each patient, and it is possible that prior or subsequent family conferences contained richer discussion of patients’ values and preferences. Research is needed to describe how clinician-surrogate communication evolves over time. However, since 98% of the conferences contained discussion of treatment options, patients’ values and preferences should have been relevant for the included conferences. Second, the Hawthorne effect may have affected these conferences by prompting clinicians’ best efforts, meaning that our results may overestimate communication and underestimate the problem. Third, our results describe the context of acute critical illness and may not apply to other contexts of surrogate decision making, such as long-standing cognitive impairment (eg, dementia). Fourth, to our knowledge, no validated measures exist to assess the quality of communication about patients’ values and preferences. Therefore, we cannot definitively judge whether what we observed was sufficient. However, our analyses were based on the central elements of shared decision making, according to which we found quantitative gaps in communication. Moreover, our inclusive approach to coding statements about the patient as a person may mean our results underestimate the scope of problems related to incorporating patients’ values and preferences into treatment decisions.
Fifth, the parent study did not collect long-term outcomes data, so we were unable to investigate associations between communication about patients’ values and preferences and eventual patient and family outcomes. Sixth, this study did not address other important dimensions of shared decision making, relationships between them (eg, how discussion of treatment options and discussion of values and preferences affect each other), or why clinicians and surrogates struggle to discuss patients’ values and preferences. These topics are important areas for further study. Seventh, because these conversations are culturally embedded, populations with different cultural norms require separate study.
Conclusions
Intensive care unit family conferences about goals of care appear to rarely follow recommended practices for shared decision making based on patients’ values and preferences. The biggest gaps noted in our study occurred in deliberating how patients would feel facing the current situation, particularly regarding their expected level of functioning if they survive critical illness. Without a shared understanding of patients’ values and preferences in these areas, clinicians and families are likely to struggle to agree on a patient-centered treatment strategy. This situation merits development of interventions to better prepare surrogates to represent patients’ values and preferences in ICU family conferences and train clinicians to facilitate these conversations. For now, we recommend that clinicians should ask questions and recommend treatment based on their best understanding of how patients would feel about their expected lifestyle and functioning after critical illness.
eTable. Frequency of Discussion of Treatment Options
References
- 1.Dowdy DW, Eid MP, Sedrakyan A, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005;31(5):611-620. doi: 10.1007/s00134-005-2592-6 [DOI] [PubMed] [Google Scholar]
- 2.Pandharipande PP, Girard TD, Jackson JC, et al. ; BRAIN-ICU Study Investigators . Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306-1316. doi: 10.1056/NEJMoa1301372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Herridge MS, Tansey CM, Matté A, et al. ; Canadian Critical Care Trials Group . Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293-1304. doi: 10.1056/NEJMoa1011802 [DOI] [PubMed] [Google Scholar]
- 4.Sacanella E, Pérez-Castejón JM, Nicolás JM, et al. Functional status and quality of life 12 months after discharge from a medical ICU in healthy elderly patients: a prospective observational study. Crit Care. 2011;15(2):R105. doi: 10.1186/cc10121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guentner K, Hoffman LA, Happ MB, et al. Preferences for mechanical ventilation among survivors of prolonged mechanical ventilation and tracheostomy. Am J Crit Care. 2006;15(1):65-77. [PubMed] [Google Scholar]
- 6.Kon AA, Davidson JE, Morrison W, Danis M, White DB; American College of Critical Care Medicine; American Thoracic Society . Shared decision making in ICUs: an American College of Critical Care Medicine and American Thoracic Society policy statement. Crit Care Med. 2016;44(1):188-201. doi: 10.1097/CCM.0000000000001396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White DB, Braddock CH III, Bereknyei S, Curtis JR. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med. 2007;167(5):461-467. doi: 10.1001/archinte.167.5.461 [DOI] [PubMed] [Google Scholar]
- 8.Scheunemann LP, Cunningham TV, Arnold RM, Buddadhumaruk P, White DB. How clinicians discuss critically ill patients’ preferences and values with surrogates: an empirical analysis. Crit Care Med. 2015;43(4):757-764. doi: 10.1097/CCM.0000000000000772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohan D, Alexander SC, Garrigues SK, Arnold RM, Barnato AE. Communication practices in physician decision-making for an unstable critically ill patient with end-stage cancer. J Palliat Med. 2010;13(8):949-956. doi: 10.1089/jpm.2010.0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uy J, White DB, Mohan D, Arnold RM, Barnato AE. Physicians’ decision-making roles for an acutely unstable critically and terminally ill patient. Crit Care Med. 2013;41(6):1511-1517. doi: 10.1097/CCM.0b013e318287f0dd [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douglas SL, Daly BJ, Lipson AR. Neglect of quality-of-life considerations in intensive care unit family meetings for long-stay intensive care unit patients. Crit Care Med. 2012;40(2):461-467. doi: 10.1097/CCM.0b013e318232d8c4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Curtis JR, Engelberg RA, Wenrich MD, Shannon SE, Treece PD, Rubenfeld GD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med. 2005;171(8):844-849. doi: 10.1164/rccm.200409-1267OC [DOI] [PubMed] [Google Scholar]
- 13.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Quality of communication in the ICU and surrogate’s understanding of prognosis. Crit Care Med. 2015;43(3):542-548. doi: 10.1097/CCM.0000000000000719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ernecoff NC, Curlin FA, Buddadhumaruk P, White DB. Health care professionals’ responses to religious or spiritual statements by surrogate decision makers during goals-of-care discussions. JAMA Intern Med. 2015;175(10):1662-1669. doi: 10.1001/jamainternmed.2015.4124 [DOI] [PubMed] [Google Scholar]
- 15.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Prior advance care planning is associated with less decisional conflict among surrogates for critically ill patients. Ann Am Thorac Soc. 2015;12(10):1528-1533. doi: 10.1513/AnnalsATS.201504-253OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crabtree BF, Miller WL, eds. Doing Qualitative Research. 2nd ed Thousand Oaks, CA: Sage Publications, Inc; 1999. [Google Scholar]
- 17.Scheunemann LP, Arnold RM, White DB. The facilitated values history: helping surrogates make authentic decisions for incapacitated patients with advanced illness. Am J Respir Crit Care Med. 2012;186(6):480-486. doi: 10.1164/rccm.201204-0710CP [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Llewellyn-Thomas HA, Crump RT. Decision support for patients: values clarification and preference elicitation. Med Care Res Rev. 2013;70(1)(suppl):50S-79S. doi: 10.1177/1077558712461182 [DOI] [PubMed] [Google Scholar]
- 19.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061-1066. doi: 10.1056/NEJMsa012528 [DOI] [PubMed] [Google Scholar]
- 20.Karel MJ, Moye J, Bank A, Azar AR. Three methods of assessing values for advance care planning: comparing persons with and without dementia. J Aging Health. 2007;19(1):123-151. doi: 10.1177/0898264306296394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ditto PH, Druley JA, Moore KA, Danks JH, Smucker WD. Fates worse than death: the role of valued life activities in health-state evaluations. Health Psychol. 1996;15(5):332-343. doi: 10.1037/0278-6133.15.5.332 [DOI] [PubMed] [Google Scholar]
- 22.Hawkins NA, Ditto PH, Danks JH, Smucker WD. Micromanaging death: process preferences, values, and goals in end-of-life medical decision making. Gerontologist. 2005;45(1):107-117. doi: 10.1093/geront/45.1.107 [DOI] [PubMed] [Google Scholar]
- 23.Patrick DL, Starks HE, Cain KC, Uhlmann RF, Pearlman RA. Measuring preferences for health states worse than death. Med Decis Making. 1994;14(1):9-18. doi: 10.1177/0272989X9401400102 [DOI] [PubMed] [Google Scholar]
- 24.Schwarze ML, Campbell TC, Cunningham TV, White DB, Arnold RM. You can’t get what you want: innovation for end-of-life communciation in the intensive care unit. Am J Respir Crit Care Med. 2016;193(1):14-16. doi: 10.1164/rccm.201508-1592OE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Volandes AE, Barry MJ, Wood F, Elwyn G. Audio-video decision support for patients: the documentary genré as a basis for decision aids. Health Expect. 2013;16(3):e80-e88. doi: 10.1111/j.1369-7625.2011.00727.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.You JJ, Downar J, Fowler RA, et al. ; Canadian Researchers at the End of Life Network . Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA Intern Med. 2015;175(4):549-556. doi: 10.1001/jamainternmed.2014.7732 [DOI] [PubMed] [Google Scholar]
- 27.Sudore RL, Fried TR. Redefining the “planning” in advance care planning: preparing for end-of-life decision making. Ann Intern Med. 2010;153(4):256-261. doi: 10.7326/0003-4819-153-4-201008170-00008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Norton SA, Metzger M, DeLuca J, Alexander SC, Quill TE, Gramling R. Palliative care communication: linking patients’ prognoses, values, and goals of care. Res Nurs Health. 2013;36(6):582-590. doi: 10.1002/nur.21563 [DOI] [PubMed] [Google Scholar]
- 29.McDonagh JR, Elliott TB, Engelberg RA, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med. 2004;32(7):1484-1488. doi: 10.1097/01.CCM.0000127262.16690.65 [DOI] [PubMed] [Google Scholar]
- 30.Joseph-Williams N, Elwyn G, Edwards A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns. 2014;94(3):291-309. doi: 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- 31.Barratt A. Evidence based medicine and shared decision making: the challenge of getting both evidence and preferences into health care. Patient Educ Couns. 2008;73(3):407-412. doi: 10.1016/j.pec.2008.07.054 [DOI] [PubMed] [Google Scholar]
- 32.Légaré F, Ratté S, Stacey D, et al. Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev. 2010;(5):CD006732. [DOI] [PubMed] [Google Scholar]
- 33.Arnold RM, Back AL, Barnato AE, et al. The Critical Care Communication project: improving fellows’ communication skills. J Crit Care. 2015;30(2):250-254. doi: 10.1016/j.jcrc.2014.11.016 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Frequency of Discussion of Treatment Options