Abstract
Introduction:
C1 lateral mass screws and C2 pedicle screws are usually chosen to fix atlantoaxial (C1–C2) instability. However, there are a few situations in which these screws are difficult to use, such as in a case with a fracture line at the screw insertion point and bleeding from the fracture site. A new technique using a unilateral C1 posterior arch screw and a C2 laminar screw combined with a contralateral C1 lateral mass screws–C2 pedicle screws procedure for upper cervical fixation is reported.
Case Report:
A 24-year-old woman had an irreducible C1–C2 anterior dislocation with a type III odontoid fracture on the right side due to a traffic accident. The patient underwent open reduction and posterior C1–C2 fixation. On the left side, a C1 lateral mass screws and a C2 pedicle screws were placed. Because there was bleeding from the fracture site and a high-riding vertebral artery was seen on the right side, a C1 posterior arch screw and a C2 laminar screw were chosen. Eight months after the surgery, computed tomography scans showed healing of the odontoid fracture with anatomically correct alignment.
Conclusions:
Although there have been few comparable studies, fixation with unilateral C1 posterior arch screw–C2 laminar screw could be a beneficial choice for surgeries involving the upper cervical region in patients with fracture dislocation or arterial abnormalities.
Keywords: Orthopaedics, rehabilitation, occupational therapy, surgery
Introduction
Instability of the atlantoaxial (C1–C2) complex can be caused by trauma, malignancy, inflammatory disease, or congenital malformations. As techniques for posterior fixation for instability of the atlantoaxial complex, the Magerl transarticular screw fixation technique1 and the Goel–Harms technique using a C1 lateral mass screw (LMS) and a C2 pedicle screw (PS; C1 LMS–C2 PS method)2,3 have been reported. However, these screw fixation techniques are associated with an increased risk of vertebral artery (VA) injury, which can be particularly problematic in patients with an anomalous VA location or abnormal bone morphology. To reduce the risk of VA injury, various techniques, for example, the use of bilateral laminar screws (LSs) crossing the C2 lamina,4 the use of a unilateral C2 PS combined with a contralateral C2 LS,5 and the use of a C1 posterior arch screw (PAS),6,7 have been reported. However, the clinical results of these methods have not been reported in detail.
In this report, the clinical and radiological results of a traumatic case with an atlantoaxial fracture dislocation and a type III odontoid fracture, treated by unilateral C1 PAS and C2 LS combined with the contralateral C1 LMS–C2 PS method, are reported.
Case report
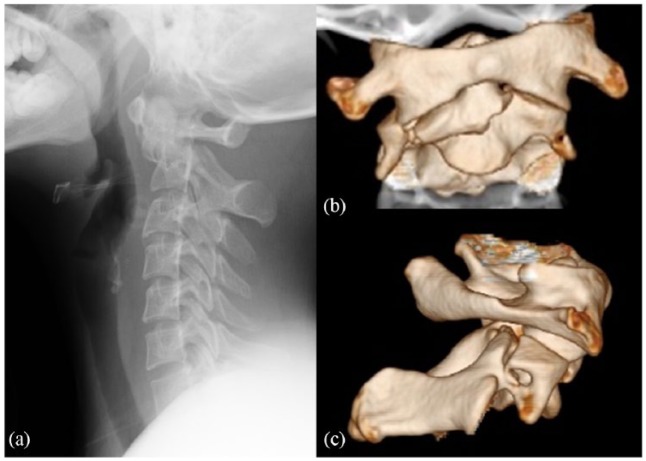
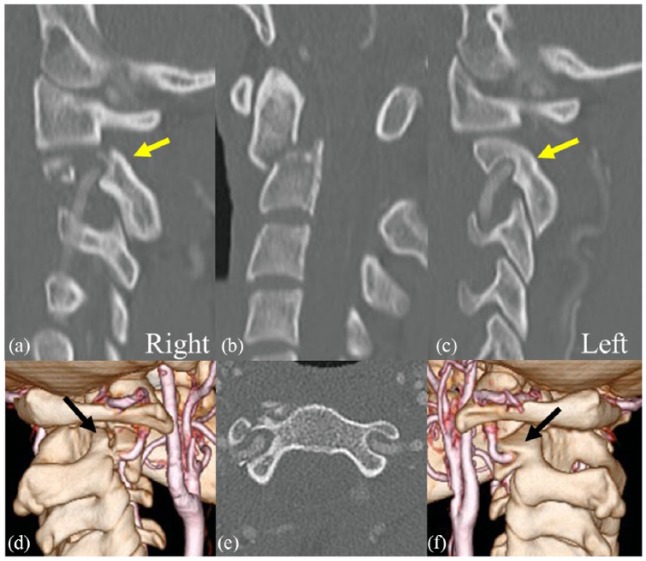
A 24-year-old woman (weight 48 kg, height 1.55 m) was injured in a traffic accident. She complained of upper cervical pain. Neurological examination was normal. A cervical spine radiograph (Figure 1(a)) and computed tomography (CT) scans (Figure 1(b) and (c)) showed C1–C2 fracture dislocation. Fractures were observed at the odontoid process, C2 transverse foramen, vertebral body, and right atlantoaxial joint (Figures 1(b) and (c) and 2(b)). This was a type III fracture based on the Anderson and D’Alonzo classification.8 C1 was displaced anteriorly relative to C2, with an irreducible intra-articular fracture of the right atlantoaxial joint (Figure 1(c) and 2(a)). CT angiography showed bilateral high-riding VAs (Figure 2(a), (b), (d), and (f)). Due to the irreducible intra-articular fracture of the right atlantoaxial joint, direct skull traction failed to achieve complete reduction of the C1–C2 dislocation, and thus, open reduction and posterior fixation of C1–C2 were performed.
Figure 1.
(a) Lateral radiographs before surgery showing that C1 is displaced anteriorly relative to C2. (b and c) Three-dimensional computed tomography (CT) images showing that C2 is fractured at the vertebral body, the right atlantoaxial joint and the transverse foramen.
Figure 2.
Computed tomography (CT) angiography images before surgery. (a, b and c) Sagittal, (e) axial and (d and f) oblique three-dimensional images showing high-riding vertebral arteries (VAs; arrow).
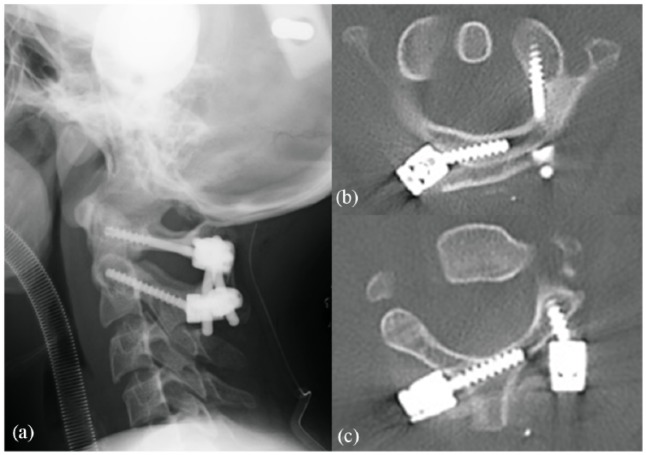
At the beginning of the operation, an attempt to re-position the C1–C2 dislocation was made. However, the atlantoaxial dislocation was not reduced by a combination of gentle manual traction and neck extension using a fluoroscope. The C1 lamina and C2 lamina were then exposed via a posterior approach, and a left LMS was then placed into C19 and a left PS was placed into C2. In addition to the thin lamina of C1, there was a risk of bleeding from the venous plexus at the fracture site by the insertion of an LMS to right C1, so it was considered difficult to insert an LMS on the right side of C1. Furthermore, because a high-riding VA was seen on the right side, a C1 PAS and a C2 LS were chosen. A high-speed burr was first used to open a small cortical window at an entry point of the posterior arch of C1 and the lamina of C2. After probing and tapping, screws of 3.5 mm in diameter and 18 mm in length (Medtronic Inc, Memphis, TN, USA) were inserted into the right sides of C1 and C2, respectively. The C1–C2 dislocation was successfully reduced through connecting rods between the C1 and C2 screws. After securing the rods, decortication and autologous iliac crest bone grafting were performed. Fluoroscopy was used intraoperatively to confirm anatomic alignment and correct placement of the implants. The postoperative lateral plain radiograph showed normal alignment of C1–C2 on the lateral image (Figure 3(a)), and postoperative axial CT images showed correct placement of the C1 LMS and LS (Figure 3(b)) and the C2 PS and LS (Figure 3(c)).
Figure 3.
(a) Postoperative lateral radiographs showing good reduction of dislocation. Postoperative axial computed tomography (CT) images 3 days after surgery showing correct placement of the implants at (b) C1 and (c) C2.
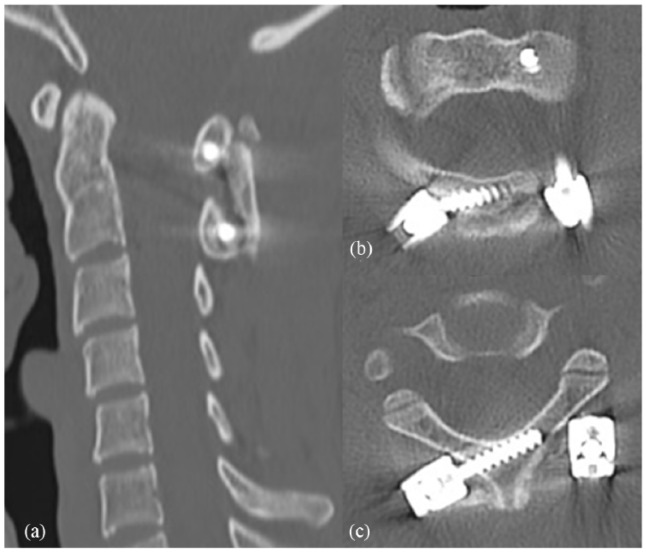
Postoperatively, the patient was immobilized in a Philadelphia cervical collar for 2 months. Eight months after the surgery, CT scans showed healing of the odontoid fracture with anatomically correct alignment and posterior fusion between the C1 posterior arch and C2 lamina (Figure 4), with no loosening of the C1 LMS and LS and the C2 PS and LS. Two years later, the patient was in good condition, having only slight neck pain when extending the cervical spine (Figure 5).
Figure 4.
(a) Sagittal and axial CT images of (b) C1 and (c) C2 at 8 months after surgery showing healing of the odontoid fracture with anatomically correct alignment.
Figure 5.

Lateral radiograph at 2 years after surgery.
The patient and her family were informed that data from the case would be submitted for publication and gave written, informed consent.
Discussion
Traumatic C1–C2 dislocation complicating an odontoid fracture is relatively rare and has a high mortality rate.10 Recent reports suggest that C1–C2 dislocation with an odontoid fracture is treated by fixation in a halo vest and C1–C2 posterior fixation.11,12 C1–C2 posterior fixation using the C1 LMS–C2 PS method is considered to be the most effective technique. However, in this case, it was difficult to insert a C1 LMS and C2 PS because of the morphology of the fracture dislocation, which was a burst of the right C2 facet to the transverse process and anterior dislocation, in addition to the high-riding VA at C2.
The C1 LMS technique is a common method for C1 fixation, but it is technically demanding. It is difficult to insert the screw, especially when the lateral mass is obscured by a thick posterior arch,13 anomalous VA,14–17 large paravertebral venous plexus,18 or a high risk of bleeding from the venous plexus, as in the present case. In such cases, a PAS may be an alternative. There are two methods of inserting a PAS. One method is inserting the PAS as an intralaminar screw to C1,6,19 and the other is inserting a bicortical PAS vertically from the dorsal side to the ventral side.7 The latter has a risk of dura mater damage and spinal cord injury, because the screw is inserted towards the spinal cord. The PAS that was used in the present case is safer than a bicortical PAS and the C1 LMS technique because it can be performed under direct visualization. In addition, the PAS in this method has the advantage of a lower risk of bleeding from the venous plexus at the time of screw insertion, because treatment around the venous plexus is unnecessary. We consider the following two points to be important at C1 PAS insertion. First, we rigorously examined the bone morphology and the VA courses by preoperative CT angiography and three-dimensional (3D) images. Second, we carefully checked with the sounder to ensure that the screw was not inserted into the spinal canal during insertion.
Literature on the use of PASs in the treatment of cervical fracture is scant.7,18 In the reported cases, both patients had type II odontoid fractures, and because they each had an anomalous VA, PASs were placed. Both cases had good results. There have been a few reports describing biomechanical testing of PAS fixation. Zarro et al.13 compared the pullout strength of C1 LMSs versus unicortical PASs, and they demonstrated that the PASs had significantly superior resistance to pullout in the axial direction compared with LMSs. Jin et al.6 examined morphometric analysis of the C1 posterior arch and demonstrated that 11% were not suitable for crossing screw placement because the posterior arch was flat, and the entry point was present on the same side. Therefore, a unilateral LMS combined with a unilateral PAS was used in the present case.
However, the C2 LS method has become increasingly used as an alternative to a C2 PS since Wright4 introduced the technique. One major advantage of this method is the complete removal of risk to the VA with C2 screw placement as the anchor to obtain upper cervical stability. Although successful results of C1–C2 fixation using crossing C2 LSs have been reported,20,21 crossing C2 LSs cannot be used for all patients due to anatomical variations in the C2 lamina.22 Miyakoshi et al.5 reported that clinical and radiological outcomes of unilateral C2 PS–C2 LS were comparable to those of the bilateral C2 PS fixation technique for the C1 LMS–C2 PS method. Jin et al. reported that unilateral C1 PAS–C2 LS combined with unilateral C1–C2 PS provided the same acute stability as the PS, and no significant difference in acute stability was found between the two-screw techniques in a cadaveric model.23 We thus used a unilateral C2 PS and contralateral C2 LS when bilateral C2 PSs could not be introduced due to a small pedicle and/or anomaly of the VAs.
As suggested previously, the unilateral C1 PAS–C2 LS method should be used in the following situations: patients with a small pedicle of the vertebral arch, treatment of the dominant side in cases of asymmetrical VAs or the opposite side in cases of unilateral VA occlusion, patients with a high-riding VA,20,24 patients with a large paravertebral venous plexus,25 and patients with a fracture that extends near the LMS or PS insertion site, as in the present case. Treatment around the fracture site would be expected to cause bleeding, so this technique could avoid further bleeding. Although additional studies examining the biomechanical properties of these screws are needed, the results of previous reports indicate that placement of a unilateral C1 PAS–C2 LS combined with a unilateral C1 LMS–C2 PS constitutes an alternative method for C1–C2 fixation.
The transoral approach may be another option for access to the atlantoaxial segment. It has been reported that the transoral approach to the cervical spine can be used for the surgical treatment of a spectrum of disease, including traumatic, spondylotic, autoimmune, and neoplastic conditions.26 However, the transoral approach has technical difficulties and concerns regarding postoperative infection and dysphagia after violating the integrity of the oropharyngeal mucosa.27,28 Therefore, we did not chose the transoral approach in this case.
Conclusion
A novel technique using a unilateral C1 PAS–C2 LS method for the fixation of a C1–C2 fracture dislocation was presented. Although there have been few comparable studies, and long-term outcomes have yet to be reported, fixation with a unilateral C1 PAS–C2 LS could be an alternative to C1 LMS and C2 PS, and it could be a reasonable treatment option for surgery of the upper cervical region.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article
Informed consent: Written informed consent was obtained from the patient and her family for their anonymized information to be published in this article.
ORCID iDs: Yuichi Ono  https://orcid.org/0000-0001-9250-457X
https://orcid.org/0000-0001-9250-457X
Naohisa Miyakoshi  https://orcid.org/0000-0001-5175-3350
https://orcid.org/0000-0001-5175-3350
Ryota Kimura  https://orcid.org/0000-0001-6697-4527
https://orcid.org/0000-0001-6697-4527
Jumpei Iida  https://orcid.org/0000-0001-5378-8047
https://orcid.org/0000-0001-5378-8047
References
- 1. Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord 1992; 5(4): 464–475. [DOI] [PubMed] [Google Scholar]
- 2. Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001; 26: 2467–2471. [DOI] [PubMed] [Google Scholar]
- 3. Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994; 129(1–2): 47–53. [DOI] [PubMed] [Google Scholar]
- 4. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech 2004; 17(2): 158–162. [DOI] [PubMed] [Google Scholar]
- 5. Miyakoshi N, Hongo M, Kobayashi T, et al. Comparison between bilateral C2 pedicle screwing and unilateral C2 pedicle screwing, combined with contralateral C2 laminar screwing, for atlantoaxial posterior fixation. Asian Spine J 2014; 8(6): 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jin GX, Wang H, Li L, et al. C1 posterior arch crossing screw fixation for atlantoaxial joint instability. Spine (Phila Pa 1976) 2013; 38(22): E1397–E1404. [DOI] [PubMed] [Google Scholar]
- 7. Nagoshi N, Suda K, Morita T, et al. C1 posterior arch screw as an auxiliary anchor in posterior reconstruction for atlantoaxial dislocation associated with type II odontoid fracture: a case report and review of the literature. Springerplus 2014; 3: 672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg 1974; 56: 1663–1674. [PubMed] [Google Scholar]
- 9. Liu G, Buchowski JM, Shen H, et al. The feasibility of microscope-assisted ‘free-hand’ C1 lateral mass screw insertion without fluoroscopy. Spine (Phila Pa 1976) 2008; 33(9): 1042–1049. [DOI] [PubMed] [Google Scholar]
- 10. Pissonnier ML, Lazennec JY, Renoux J, et al. Trauma of the upper cervical spine: focus on vertical atlantoaxial dislocation. Eur Spine J 2013; 22(10): 2167–2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lenehan B, Guerin S, Street J, et al. Lateral C1-C2 dislocation complicating a type II odontoid fracture. J Clin Neurosci 2010; 17(7): 947–949. [DOI] [PubMed] [Google Scholar]
- 12. Fuentes S, Bouillot P, Palombi O, et al. Traumatic atlantoaxial rotatory dislocation with odontoid fracture: case report and review. Spine (Phila Pa 1976) 2001; 26(7): 830–834. [DOI] [PubMed] [Google Scholar]
- 13. Zarro CM, Ludwig SC, Hsieh AH, et al. Biomechanical comparison of the pullout strengths of C1 lateral mass screws and C1 posterior arch screws. Spine J 2013; 13(12): 1892–1896. [DOI] [PubMed] [Google Scholar]
- 14. Hong X, Dong Y, Yunbing C, et al. Posterior screw placement on the lateral mass of atlas: an anatomic study. Spine (Phila Pa 1976) 2004; 29(5): 500–503. [DOI] [PubMed] [Google Scholar]
- 15. O’Donnell CM, Child ZA, Nguyen Q, et al. Vertebral artery anomalies at the craniovertebral junction in the US population. Spine (Phila Pa 1976) 2014; 39(18): E1053–E1107. [DOI] [PubMed] [Google Scholar]
- 16. Uchino A, Saito N, Watadani T, et al. Vertebral artery variations at the C1–2 level diagnosed by magnetic resonance angiography. Neuroradiology 2012; 54(1): 19–23. [DOI] [PubMed] [Google Scholar]
- 17. Yamazaki M, Okawa A, Furuya T, et al. Anomalous vertebral arteries in the extra- and intraosseous regions of the craniovertebral junction visualized by 3-dimensional computed tomographic angiography: analysis of 100 consecutive surgical cases and review of the literature. Spine (Phila Pa 1976) 2012; 37(22): E1389–E1197. [DOI] [PubMed] [Google Scholar]
- 18. Carmody MA, Martin MD, Wolfla CE. Persistent first intersegmental vertebral artery in association with type II odontoid fracture: surgical treatment utilizing a novel C1 posterior arch screw: case report. Neurosurgery 2010; 67(1): 210–1, discussion 211. [DOI] [PubMed] [Google Scholar]
- 19. Donnellan MB, Sergides IG, Sears WR. Atlantoaxial stabilization using multiaxial C-1 posterior arch screws. J Neurosurg Spine 2008; 9(6): 522–527. [DOI] [PubMed] [Google Scholar]
- 20. Ma W, Feng L, Xu R, et al. Clinical application of C2 laminar screw technique. Eur Spine J 2010; 19(8): 1312–1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Peyriere H, Graillon T, Pesenti S, et al. Surgical management of post-traumatic atlantoaxial rotatory fixation due to C2 facet fracture: 5 clinical cases. Orthop Traumatol Surg Res 2017; 103(1): 67–70. [DOI] [PubMed] [Google Scholar]
- 22. Cassinelli EH, Lee M, Skalak A, et al. Anatomic considerations for the placement of C2 laminar screws. Spine (Phila Pa 1976) 2006; 31(24): 2767–2771. [DOI] [PubMed] [Google Scholar]
- 23. Jin GX, Huan W. Unilateral C-1 posterior arch screws and C-2 laminar screws combined with a 1-side C1–2 pedicle screw system as salvage fixation for atlantoaxial instability. J Neurosurg Spine 2015; 24: 315–320. [DOI] [PubMed] [Google Scholar]
- 24. Matsubara T, Mizutani J, Fukuoka M, et al. Safe atlantoaxial fixation using a laminar screw (intralaminar screw) in a patient with unilateral occlusion of vertebral artery: case report. Spine (Phila Pa 1976) 2007; 32(1): E30–E33. [DOI] [PubMed] [Google Scholar]
- 25. Ma XY, Yin QS, Wu ZH, et al. C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine (Phila Pa 1976) 2009; 34(4): 371–377. [DOI] [PubMed] [Google Scholar]
- 26. Menezes AH, VanGilder JC. Transoral-transpharyngeal approach to the anterior craniocervical junction. J Neurosurg 1988; 69(6): 895–903. [DOI] [PubMed] [Google Scholar]
- 27. Morgan S, Murphy G. The transoral approach to the cervical spine. J Neurosci Nurs 1992; 24: 269–272. [DOI] [PubMed] [Google Scholar]
- 28. Choi D, Crockard HA. Evolution of transoral surgery: three decades of change in patients, pathologies, and indications. Neurosurgery 2013; 73(2): 296–303, discussion 303. [DOI] [PubMed] [Google Scholar]