Sir,
Pulmonary manifestations are present in up to 50% of patients with systemic lupus erythematosus (SLE) and can involve pleura, parenchyma, airways, pulmonary vessels, and respiratory muscles.[1]
Acute lupus pneumonitis (ALP) and diffuse alveolar hemorrhage (DAH) are acute parenchymal lung diseases which may occur in SLE.[1]
We hereby present a case of a female participant with SLE associated to acute parenchymal lung involvement and hematological disorders.
A nonsmoker, 68-year-old woman, referred to our hospital with a 5-month history of fatigue and dyspnea that significantly worsened in the last week. She denied fever, cough, sputum, and hemoptysis.
She reported arterial hypertension and documented allergy to nonsteroidal anti-inflammatory drugs and several antibiotics. She denied any occupational exposure.
On physical examination, the patient showed hair loss. She had tachypnea (respiratory rate 25 breaths/min) despite breathing oxygen FiO260% by the venturi mask. On auscultation, a widespread vesicular murmur and Velcro-like in expiratory crackles were heard. Blood gas analysis revealed a severe hypoxemic respiratory failure (PaO2:65 mmHg; pCO2:45 mmHg; P/F ratio: 108).
A two-projection chest radiograph was performed revealing the right lung and left central pulmonary consolidation [Figure 1].
Figure 1.
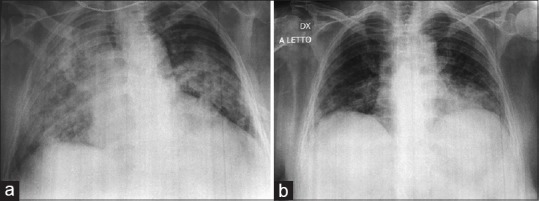
Two-projections chest X-ray performed the day of the admission showing the right lung (a) and left central pulmonary consolidation (b)
Laboratory findings were the following: white blood cells 7160/μL (86.7% neutrophils, 7.8% lymphocytes, and 4.8% monocytes), hemoglobin 7.3 g/dL, platelets 15000 per μl, and troponin I 0.00 ng/mL; N-terminal pro-B-type natriuretic peptide 132 pg/mL; increased serum inflammatory markers (C-reactive protein 53.8 and erythrocyte sedimentation rate 26 mm/h); pro-calcitonin 0.05 ng/mL. Moreover, there was an alteration of hemolysis indexes (erythropoietin 45.2 mU/mL, total reticulocytes 5.7%, lactate dehydrogenase 275 U/L; total bilirubin 1.50 mg/dL, and indirect bilirubin 0.99 mg/dL).
According to the hematological evaluation, the Coombs test was performed, and corticosteroid therapy (40 mg/die of intravenous methyl-prednisolone) was immediately started.
Direct and indirect Coombs tests were positive; therefore, blood transfusion was not performed.
Empirical antibiotic therapy was not prescribed because of the patient's documented multi-drug allergy.
Microbiological investigations on blood, urinary, and respiratory samples were carried out, and complete autoimmune tests were performed.
During the admission, patient clinical condition deteriorated; a worsening of thrombocytopenia (platelets 4000) and respiratory failure were revealed. Blood gas analysis in high-flow nasal cannula oxygen therapy (airflow 50 L/min, FiO290%) showed P/F ratio of 69.
Therefore, methylprednisolone therapy was increased to 80 mg/die.
Immunophenotyping of peripheral blood lymphocytes and bone marrow aspirate did not show abnormalities.
The microbiological examinations and sputum cytology were negative.
The rheumatological workup showed the following positive findings: antinuclear antibody (ANA) 1/640 and anti-double strand DNA (anti-dsDNA) 1145 UI/mL. Furthermore, platelet-specific antibodies were positive. Low serum C3 level was found.
In light of nonscarring alopecia, hemolytic anemia, thrombocytopenia, ANA and anti-dsDNA antibody level above laboratory reference range, a diagnosis of SLE was made.
The patient was treated by increasing steroid doses (until methylprednisolone up to 1 mg/kg/die intravenous) and intravenous immunoglobulin for 5 days with the improvement of general conditions.
Chest computed tomography (CT) showed “increased density areas mainly located in the left upper lobe, lingular, middle lobe, and anterior segments of both lower lobes associated with interstitial subpleural thickening [Figure 2].”
Figure 2.
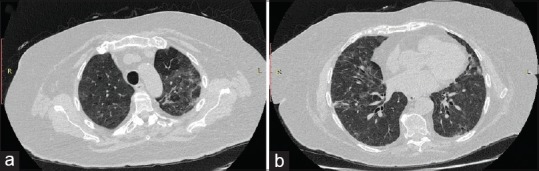
Chest computed tomography scan performed during the admission, revealing increased density areas mainly located in the left upper lobe, lingular, middle lobe (a), and anterior segments of both lower lobes (b) associated with interstitial subpleural thickening
Blood chemistry values (hemoglobin 9. 6 g/dL and platelets 302,000/μL) and blood gas analysis improved (at room air: pH 7. 48; pCO2 of 39 mmHg; pO2 of 72 mmHg; P/F ratio of 342).
Finally, respiratory function tests were performed. Global spirometry parameters were in the normal range (forced expiratory volume in 1 s (FEV1) 86% of predicted values; forced vital capacity (FVC) 85% of predicted values, FEV1/FVC ration 84.01;), and diffusing capacity of the lungs for carbon monoxide was 39% of predicted value.
At discharge, a therapy with prednisone 25 mg/die and azathioprine 100 mg/die was prescribed.
During the follow-up visit, patient's clinical conditions and laboratory tests were found to be stable.
In line with the rheumatologist's recommendations, the corticosteroid and immunosuppressive treatment were continued.
On high-resolution CT scan, repeated after 40 days from the discharge, significant reduction of the ground glass areas and the persistence of nonspecific interstitial pneumonia were found [Figure 3].
Figure 3.
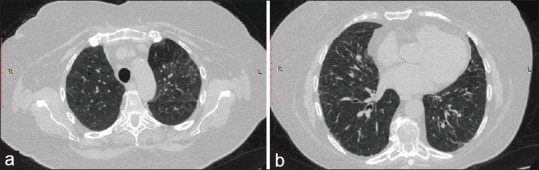
High-resolution chest computed tomography scan performed 40 days after discharge showed significant reduction of the ground glass areas (a) and the persistence of opacities (b)
ALP is reported to affect 1%–12% of SLE patients.[2] It can be the first expression of the disease in about 50% of participants.
In our patient, indirect hyperbilirubinemia plus positivity of the Coombs test suggested anemia as a complication of SLE (autoimmune hemolytic anemia; AIHA).
AIHA affects 5%–10% of SLE patients and up to 40% of SLE patients show thrombocytopenia.[3,4]
The concomitant or consecutive manifestation of AIHA and immune thrombocytopenia, which is called Evans' syndrome (ES), is a rare complication,[5] accounting for 0.47% in SLE.[6,7]
The ES could rise alone or in association with other diseases such as autoimmune conditions.[2] The multisystem involvement of SLE occurs in 3%–15% of ES patients during the follow-up.
Acute pulmonary involvement in SLE is characterized by a poor prognosis. Indeed, both ALP and DAH could be potentially fatal also because of opportunistic infections, cardiac and renal failure, diaphragmatic dysfunction, and drug toxicity that may occur.[2]
To conclude, in our patient, SLE started with the most life-threatening respiratory and hematological complications. The diagnosis was difficult because of the coexistence of ALP and ES, which is a rare event that quickly worsened the patient's clinical conditions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Carmier D, Marchand-Adam S, Diot P, Diot E. Respiratory involvement in systemic lupus erythematosus. Rev Mal Respir. 2008;25:1289–303. doi: 10.1016/s0761-8425(08)75093-9. [DOI] [PubMed] [Google Scholar]
- 2.Kamen DL, Strange C. Pulmonary manifestations of systemic lupus erythematosus. Clin Chest Med. 2010;31:479–88. doi: 10.1016/j.ccm.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Durán S, Apte M, Alarcón GS, Marion MC, Edberg JC, Kimberly RP, et al. Features associated with, and the impact of, hemolytic anemia in patients with systemic lupus erythematosus: LX, results from a multiethnic cohort. Arthritis Rheum. 2008;59:1332–40. doi: 10.1002/art.24020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sultan SM, Begum S, Isenberg DA. Prevalence, patterns of disease and outcome in patients with systemic lupus erythematosus who develop severe haematological problems. Rheumatology (Oxford) 2003;42:230–4. doi: 10.1093/rheumatology/keg069. [DOI] [PubMed] [Google Scholar]
- 5.Costallat GL, Appenzeller S, Costallat LT. Evans syndrome and systemic lupus erythematosus: Clinical presentation and outcome. Joint Bone Spine. 2012;79:362–4. doi: 10.1016/j.jbspin.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L, Wu X, Wang L, Li J, Chen H, Zhao Y, et al. Clinical features of systemic lupus erythematosus patients complicated with Evans syndrome: A case-control, single center study. Medicine (Baltimore) 2016;95:e3279. doi: 10.1097/MD.0000000000003279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michel M, Chanet V, Dechartres A, Morin AS, Piette JC, Cirasino L, et al. The spectrum of Evans syndrome in adults: New insight into the disease based on the analysis of 68 cases. Blood. 2009;114:3167–72. doi: 10.1182/blood-2009-04-215368. [DOI] [PubMed] [Google Scholar]


