Abstract
Background:
Clinical scenarios of oral potentially malignant disorders (OPMDs) and oral squamous cell carcinoma (OSCC) vary between geographical districts within the same country. This could be attributed to common habits and other cultural factors, such as excessive consumption of tobacco products, leading to higher prevalence of tobacco-related lesions of the oral cavity. A better understanding of their pattern and behavior in each particular region may help in devising strategies for prevention and treatment.
Aims and Objectives:
The aim of the study is to assess the epidemiological profile and clinical characteristics of OPMD and OSCC among population in and around Bidar and Gulbarga districts of Karnataka, India.
Materials and Methods:
This was a retrospective, chart review study in the districts of Bidar and Gulbarga, Karnataka, India. Medical records of patients with clinical and histopathological diagnosis of OPMD or OSCC who attended a private dental school in Bidar and 20 private dental clinics in the districts of Bidar and Gulbarga between 2010 and 2017 were included in the study. Collected data were analyzed using Statistical Package Social Sciences software, version 20.0.
Results:
There were a total of 630 patients, with males representing 69.52% (n = 438; ratio of 2.28:1) of cases and mean age of 42.64 years. 375 (59.52%) patients had a diagnosis of OPMD with the most common subtype of oral submucous fibrosis (185/375; 49.33%) followed by leukoplakia (110/375; 29.33%) and lichen planus (80/375; 21.33%). Buccal mucosa was the most commonly affected site (33.01%). Of 630 patients, 255 (40.48%) had OSCC, with tongue being the most common site (36.86%).
Conclusion:
This study revealed for the first time that OPMD and OSCC are widespread in the districts of Bidar and Gulbarga. The available knowledge on the prevalence of these lesions could help in educating patients and implementing preventive measures by health-care providers to improve overall survival. Long-term follow-up studies are needed to better understand the disease pattern.
Keywords: Lichen planus, oral potential malignant disorder, oral squamous cell carcinoma, oral submucous fibrosis, prevalence
INTRODUCTION
Oral cancer (OC) is a universal health problem with significant impact on the developing countries including the Indian subcontinent. For the past decades, there has been a steady increase in OC incidence and mortality rates with around 575,000 new cases and 320,000 deaths worldwide reported annually.[1] In addition, recent epidemiological studies and cancer society's reports anticipated the number of OC cases to increase from 1 million in 2012 to 1.7 million in 2035.[2] In India, OC is the most frequent type of cancer accounting for up to 40% of all cancers. This can be attributed to the fact that most of OC cases are diagnosed at advanced stages. Of all OC cases, oral squamous cell carcinoma (OSCC) accounts for the majority of cases with incidence rates of 12.8 and 7.5/100,000 in men and women, respectively.[2,3]
According to the World Health Organization (WHO: 2007), oral potentially malignant disorder (OPMD) is defined as “the risk of malignancy being present in a lesion or condition either during the time of initial diagnosis or at a future date.” The WHO categorizes OPMD into two groups: (i) precancerous lesion, which is a benign lesion with morphologically altered tissue with greater than normal risk of transforming into malignancy and; (ii) precancerous condition, a disease or patients’ habit that does not necessarily alter the clinical appearance of local tissues but is associated with a greater than normal risk of precancerous lesion or cancer development in that tissue.[3] Overall OPMD can be detected in approximately 2.5% of the general population. Multiple conditions fall under OPMDs including oral submucous fibrosis (OSMF), leukoplakia, lichen planus and erythroplakia.[3,4,5]
OSMF is a potentially malignant condition of the oral cavity associated with areca nut usage in different forms. It is more common in men of Indian subcontinent and South Eastern Asia. Its clinical presentation includes palpable, fibrous bands and changes in the oral mucosa, combined with burning sensation and less frequently ulceration. Oral leukoplakia is another OPMD entity defined by the WHO as “a white plaque of questionable risk having excluded other known disease or disorders that carry no increased risk for cancer.” Oral leukoplakia is more prevalent in men and presents clinically as white, hyperkeratotic and well-defined plaques which could be homogeneous or nonhomogeneous. On the other hand, oral lichen planus (OLP) is a chronic, immune-mediated condition which is more common in female. It is characterized by Wickham keratotic striae, erythema and/or ulceration in the oral cavity more commonly in women. Lichen planus can also affect other body organs such as skin and genitalia.[2,3,4]
The early detection of OPMD can reduce the transformation risk to OSCC, thereby reducing cancer morbidity and mortality.[4,5] Nevertheless, OPMD and OSCC epidemiological and clinical spectrums vary in different geographical districts within the same country.[6,7,8] Multiple epidemiological studies on OPMD and OSCC and have been conducted previously in different parts of India. However, this is the first study looking into the districts and population of Bidar and Gulbarga of North Karnataka.[8,9,10] This pilot study was conducted to determine the epidemiological profile and clinical characteristics of OPMD and OC among the population of Bidar and Gulbarga districts of North Karnataka, India.
MATERIALS AND METHODS
A human research ethical approval was obtained through the SB Patil Dental College and Hospital, Bidar. This was a chart review study of patients who attended a dental school and 20 private dental clinics with the intention to capture variable population distributed in the districts of Bidar and Gulbarga, Karnataka, India between 2010 and 2017.
Eligible cases included patients with oral lesions clinically and histopathologically consistent with either OPMD or OSCC of different grades. Histopathology slides were obtained and examined by two oral pathologists to confirm diagnoses.
A data collection sheet was created to collect data on patient age, gender, risk factors (smoking, smokeless tobacco and alcohol consumption), site of the lesion and histopathological diagnosis.[3] At the end of the study, data were collected and analyzed using Statistical Package for the Social Sciences software, version 20.0 (IBM Corp. Released 2011, IBM SPSS Statistics for windows version 20.0, Armonk, NY: USA) P < 0.05 was considered as statistically significant.
RESULTS
There were total of 630 subjects, with most of the cases reported in 2012–2013 (105), followed by 104 in 2016–2017 [Table 1]. Chi-square analysis which is a test of association was carried out to find out if there is any association between the variables. There was a statistically insignificant difference between the number of cases of OPMD and OSCC reported year wise (P = 1.000).
Table 1.
Number of cases reported year wise
| Year | OSMF | Leukoplakia | Lichen planus | OSCC | Total, n (%) | P |
|---|---|---|---|---|---|---|
| 2010-2011 | 27 | 18 | 11 | 36 | 92 (14.60) | Chi-square analysis showed P=0.737 |
| 2011-2012 | 28 | 14 | 12 | 34 | 88 (13.96) | |
| 2012-2013 | 31 | 19 | 14 | 41 | 105 (16.67) | |
| 2013-2014 | 19 | 12 | 8 | 27 | 66 (10.47) | |
| 2014-2015 | 26 | 16 | 9 | 38 | 89 (14.13) | |
| 2015-2016 | 24 | 15 | 10 | 37 | 86 (13.65) | |
| 2016-2017 | 30 | 16 | 16 | 42 | 104 (16.51) | |
| Total | 185 | 110 | 80 | 255 | 630 (100) |
OSCC: Oral squamous cell carcinoma, OSMF: Oral submucous fibrosis
There were 438 males (69.52%) and 192 females (30.48%), with a ratio of 2.28:1 [Table 2]. There was a statistically significant difference between the gender prediliction of OPMD and OSCC patients (P = 0.008).
Table 2.
Distribution of oral premalignant and malignant lesions gender wise
| Gender | OSMF | Leukoplakia | Lichen planus | OSCC | Total, n (%) | P |
|---|---|---|---|---|---|---|
| Male | 125 | 78 | 44 | 191 | 438 (69.52) | Chi-square analysis showed P=0.008 |
| Female | 60 | 32 | 36 | 64 | 192 (30.48) | |
| Total | 185 | 110 | 80 | 255 | 630 (100) |
OSCC: Oral squamous cell carcinoma, OSMF: Oral submucous fibrosis
Median age of patients was 43 years (ranged between 18 and 72 years; mean age of 42.64 years). Majority of patients were in the 40–50 years of age group (n = 180, 28.57%: males [n = 114, 63.33%], females [n = 66, 36.67%]) and least number were in <20 years of age group ([n = 18, 2.86%], males [n = 14, 77.78%], females [n = 4, 22.22%]) [Table 3]. There was a statistically significant difference between the age of OPMD and OSCC patients (P = 0.001).
Table 3.
Distribution of oral premalignant and malignant lesions according to age
| Age (years) | OSMF | Leukoplakia | Lichen planus | OSCC | Total, n (%) | P |
|---|---|---|---|---|---|---|
| 10-19 | 2 | 4 | 12 | - | 18 (2.86) | Chi-square analysis showed P=0.001 |
| 20-29 | 36 | 21 | 14 | 8 | 79 (13.17) | |
| 30-39 | 65 | 35 | 21 | 32 | 153 (24.28) | |
| 40-49 | 42 | 21 | 12 | 105 | 180 (28.58) | |
| 50-59 | 28 | 22 | 9 | 76 | 135 (21.43) | |
| Above 60 | 12 | 7 | 12 | 34 | 65 (10.32) | |
| Total | 185 | 110 | 80 | 255 | 630 (100) |
OSCC: Oral squamous cell carcinoma, OSMF: Oral submucous fibrosis
Most of the study subjects (65.08%) had more than one risk factor, i.e., alcohol consumption, tobacco in smoking and nonsmoking forms [Table 4]. There was a statistically significant difference between the risk factors of the OPMD and OSCC lesions (P = 0.001).
Table 4.
Risk factors of oral potentially malignant disorders and oral squamous cell carcinoma
| Risk factors | OSMF | Leukoplakia | Lichen planus | OSCC | Total, n (%) | P |
|---|---|---|---|---|---|---|
| Chewing tobacco | 32 | 68 | 23 | 168 | 291 (46.19) | Chi-square analysis showed P=0.001 |
| Smoking tobacco | 24 | 41 | 15 | 95 | 175 (27.78) | |
| Arecanut | 82 | 35 | 21 | 45 | 193 (30.63) | |
| Alcohol | 18 | 39 | 17 | 89 | 163 (25.87) | |
| Combination of risk factors | 28 | 47 | 22 | 108 | 405 (65.08) | |
| No history of habits | 35 | 18 | 32 | 12 | 97 (15.39) |
OSCC: Oral squamous cell carcinoma, OSMF: Oral submucous fibrosis
Oral lesions were categorized into two categories, OPMD and OSCC. Of 630 patients, 375 (59.52%) had OPMD with 247 (65.87%) males and 128 (34.13%) females. Buccal mucosa was the most common site for OPMD (33.01%), followed by the tongue (22.53%) and floor of the mouth (14.92%). The most common OPMD lesion was OSMF [Figures 1 and 2] (185, 49.33%) followed by leukoplakia (110, 29.33%) and lichen planus (80, 21.33%) [Figure 3]. Histopathologically, dysplasia was seen in 110 patients with OPMD. The dysplastic lesions were classified as low risk and high risk as proposed by Sadiq et al. (2005).[3] In our study, the low risk constituted 75% of patients, whereas the high-risk group constituted 25%. There were no patients with more than one lesion group. For OSMF, the most frequently affected age group was between 30 and 39 years (65, 35.13%), with men were mainly affected (125, 67.57%).
Figure 1.

Clinical Grade III oral submucous fibrosis clinical photograph
Figure 2.
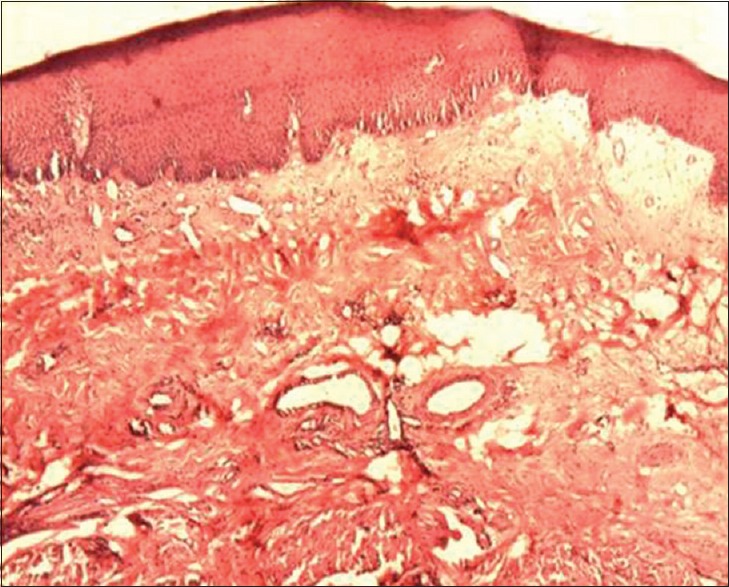
Photomicrograph of moderately advanced oral submucous fibrosis.jpg
Figure 3.
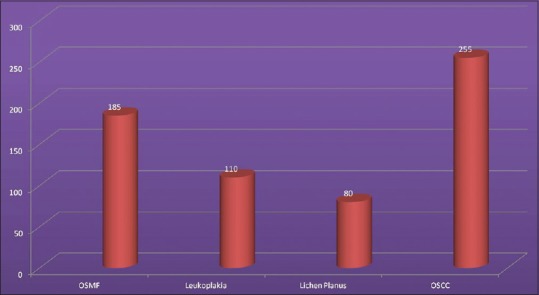
Bar graph showing distribution of lesions
There were 255 (40.48%) subjects with OSCC [Figures 4 and 5] with 191 (74.90%) males and 64 (25.10%) females. The most commonly affected age group was 41–50 years (105, 41.17%). For OSCC, the tongue was the most common site (36.86%) followed equally by buccal mucosa and floor of mouth (20.78%) [Table 5]. There was a statistically significant difference between the site distribution of the OPMD and OSCC lesions (P = 0.001).
Figure 4.

Oral carcinoma clinical photograph
Figure 5.
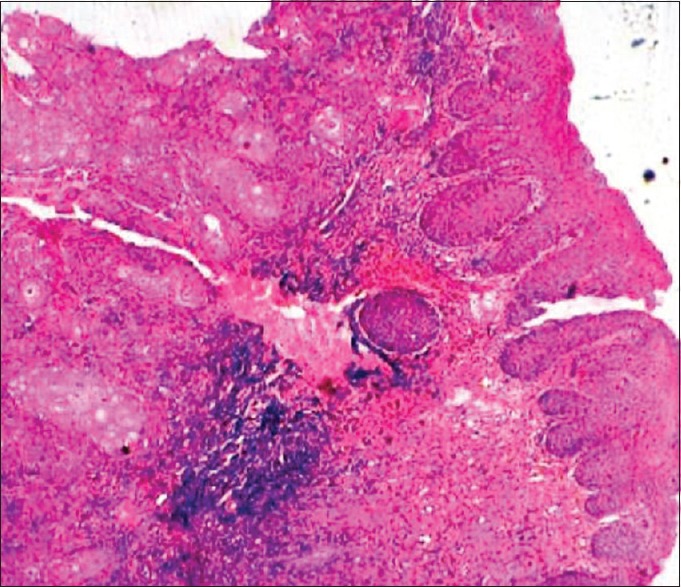
Photomicrograph of oral squamous cell carcinoma
Table 5.
Site distribution of oral premalignant and malignant lesions
| Site | OSMF | Leukoplakia | Lichen planus | OSCC | Total, n (%) | P |
|---|---|---|---|---|---|---|
| Buccal mucosa | 84 | 24 | 47 | 53 | 208 (33.01) | Chi-square analysis showed P=0.001 |
| Tongue | 26 | 12 | 10 | 94 | 142 (22.53) | |
| Palate | 42 | 21 | 2 | 21 | 86 (13.65) | |
| Lips | 21 | 12 | 6 | 23 | 62 (9.84) | |
| Gingiva | 2 | 2 | 8 | - | 12 (1.90) | |
| Floor of the mouth | 6 | 36 | - | 52 | 94 (14.92) | |
| Retromolar trigone | 4 | 3 | 7 | 12 | 26 (4.13) | |
| Total | 185 | 110 | 80 | 255 | 630 (100) |
OSCC: Oral squamous cell carcinoma, OSMF: Oral submucous fibrosis
Histopathological evaluation of OSCC cases showed that majority of the cases was well differentiated (170, 66.67%) [Table 6].
Table 6.
Histopathological categories of oral squamous cell carcinoma cases
| Histopathological category of SCC | n (%) |
|---|---|
| Well differentiated SCC | 170 (66.67) |
| Moderately differentiated SCC | 70 (27.45) |
| Poorly differentiated SCC | 15 (5.88) |
| Total | 255 (100) |
SCC: Squamous cell carcinoma
DISCUSSION
OSCC accounts for approximately 3% of all malignancies and more than 90% of all head and neck cancers. The National Cancer Registry Programme of the Indian Council of Medical Research released an alarming report pointing out an increase in cancer rate incidence in India, with over seven lakh people being registered yearly.[11] From all types of cancer, OSCC is the most common in males and third-most common in females.[11,12,13]
Both OPMD and OSCC have common risk factors such as tobacco in various forms, areca-nut, alcohol, chronic exposure to ultraviolet radiation, genetic abnormalities and human papillomavirus infection. Early stages of OSCC are typically managed with surgery and radiotherapy. Whereas in advanced stages, chemotherapy can be added. The mortality rate of OSCC continues to be the same for the past decades with a 5-year survival rate of 50%, even with the advancement in treatment modalities.
Pindborg in 1966 defined OSMF as “an insidious chronic disease affecting any part of the oral cavity and sometimes pharynx. Although occasionally preceded by and/or associated with vesicle formation, it is always associated with juxta-epithelial inflammatory reaction followed by fibroblastic changes in the lamina propria, with epithelial atrophy leading to stiffness of the oral mucosa causing trismus and difficulty in eating.” Lichen planus was first described in 1869 by Erasmus Wilson as “leichen planus,” “an eruption of pimples remarkable for their color, their figure, their structure, their habits of isolated and aggregated development, their habitat, their local and chronic character and for the melasmic stains which they leave behind them when they disappear.” Squamous cell carcinoma is defined as “a malignant neoplasm exhibiting squamous differentiation as characterized by formation of keratin and/or the presence of intercellular bridges.”
Clinically, we diagnosed OSMF as a lesion with palpable submucosal band in buccal and labial mucosa, restricted mouth opening, restricted tongue movement, leathery appearance of the mucosa, leukoplakia as a flat to slightly elevated, gray/white translucent plaque which was either fissured/wrinkled, OLP as a lesion with fine lacelike network of white lines, i.e., Wickham's striae, predominantly bilateral.
The early diagnosis of OPMD can be helpful in cancer prevention and reducing related mortality and morbidity. To achieve this goal, dentists play a pivotal role in educating the public, diagnosis and long-term follow-up of patients at risk and to avoid local recurrence and lymph node metastases.[8,9,14,15,16]
Most of the OPMD and OSCC prevalence literature have been carried out among patients visiting dental institutes which may result in masking the true prevalence of the disease. The main aim of the current study was to obtain epidemiological profile of OPMD and OSCC in the last 7 years in two districts of Karnataka to obtain a better estimate of total cases.[15,16] Based on our data, the prevalence of OPMD and OSCC in both districts might be linked to a rise in the usage of tobacco in various forms, areca nut and alcohol, compared to other districts. In addition, most of the OPMD cases were in the fourth decade similar to Misra et al.[7] However, Scott and Cheah and Waldern and Shafer found most of their cases in sixth and seventh decades, respectively, which might be due to the cumulative effect of tobacco carcinogens.[17,18]
Our findings of male preponderance are similar to Gowhar et al. and Maia et al.[5,19] This could be due to higher consumption of tobacco compared to females.
The mean age of OPMD and OSCC patients was 46.87 years. This is similar to Misra et al. who reported a mean age of 53.15.[7] The younger population involved in our study could be due to easier accessibility of tobacco products and alcohol to this age group in the study area.
On analyzing risk factors, that majority of included patients had chewing tobacco habit in the form of gutkha (a chewable mixture of tobacco, betel nut and sweeteners in an attractive pack) and betel quid (betel leaf with slaked lime, betel nut and tobacco). In addition, alcohol consumption was a contributing factor in the causation of OPMD and OSCC, similar to the results reported by Ray et al.[20]
The most common site of OPMD and OSCC was buccal mucosa (33.01%), which is similar to what have been reported by Naga et al. and Gowhar et al. and related to the site used for chewing smokeless tobacco. The cultural habit of people of North Karnataka of using gutkha could be one of the main reason.[5,21]
When geographical variations were considered, Bhopal, in India had the highest incidence worldwide of both mouth cancers (9.6) and tongue (10.9) in males. Whereas the highest incidence of oropharyngeal cancers in males was seen in Trivandrum, India. The highest incidence of cancer in relation to tobacco usage was seen in the districts of Central, Southern and North East India. Pondicherry also showed a high incidence of mouth cancer among men (8.9/100,000).[22] In a study in Belgaum, Karnataka, tobacco chewing was found to be the main risk factor for OPMD and OSCC with leukoplakia, OSMF and OSCC accounting for the prevalence of 13.4%, 28.3% and 6.3%, respectively.[23]
Considering the current results, the use of recent advances in oral screening and detection aids such as Vizylite and Velscope for OPMD and OSCC at early stage could serve as a helpful adjunctive tool. The ease of use, accessibility and reasonably cheaper price could be attractive factors. However, the sensitivity and specificity of these adjunctive tools have been always in question. Along with improved diagnostic modalities and treatment strategies, patient education on cessation of smoking habits is very important in reducing risk of OSCC. Studies regarding prevalence patterns in different regions of India may aid in formulating such strategies.[20,21,22,23,24]
This study has several limitations. First, the study had a smaller sample size. Second, only patients who visited 20 dental clinics and one dental school were included. Third, a complete history of the disease and smoking history was not available for few patients.
The management of OSCC in developing countries as India is challenging compared to Western countries. Lack of resources, follow-up and access to care are some of the challenges to provide standard of care in addition to conducting clinical trials. Shortage in cancer treatment facilities, lack of standardized protocols for cancer management and cost are all limiting factors. Similar to other studies in India, few of our patients lost to follow-up. The most common treatment modality conducted for included cases was surgical excision which showed good overall response with low recurrence rate. Hence, it is recommended for constituting a multidisciplinary cancer units in regional hospitals all around India and epidemiological profile studies may help in formulating national cancer policies.[20,21,22]
CONCLUSION
The incidence of OPMD and OSCC in India is on the rise with a predilection for younger age groups, due to the increase in consumption of gutkhas and pan masala. Early recognition of OPMD and OSCC and implementing national preventive programs can reduce impending complications and increase the life expectancy of affected patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gaphor SM, Sabri ZA. Prevalence of oral premalignant and malignant lesions among referred Kurdish patients attending department of oral and maxilofasial in sulaimani teaching hospital. IOSR J Dent Med Sci (IOSR-JDMS) 2014;13:32–6. [Google Scholar]
- 2.Varshitha A. Prevalence of oral cancer in India. J Pharm Sci Res. 2015;7:845–8. [Google Scholar]
- 3.Sadiq H, Gupta P, Singh N, Thakar SS, Prabhakar I, Thakral J. Various grading systems of the oral epithelial dysplasia: A review. Int J Adv Health Sci. 2015;1:20–6. [Google Scholar]
- 4.Mortazavi H, Baharvand M, Mehdipour M. Oral potentially malignant disorders: An overview of more than 20 entities. J Dent Res Dent Clin Dent Prospects. 2014;8:6–14. doi: 10.5681/joddd.2014.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gowhar O, Ain TS, Singh NN, Sultan S. Prevalence of oral premalignant and malignant lesions in Moradabad, India - A retrospective study. Int J Contemp Med Res. 2016;3:2079–81. [Google Scholar]
- 6.Hosagadde S, Dabholkar J, Virmani N. A clinicopathological study of oral potentially malignant disorders. J Head Neck Physicians Surg. 2016;4:29–34. [Google Scholar]
- 7.Misra V, Singh PA, Lal N, Agarwal P, Singh M. Changing pattern of oral cavity lesions and personal habits over a decade: Hospital based record analysis from Allahabad. Indian J Community Med. 2009;34:321–5. doi: 10.4103/0970-0218.58391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Langdon JD, Russel RC, Williams NS, Bulstrode CJ. London: Hodder Headline Group; 2000. Oral and Oropharyngeal Cancer Practice of Surgery. [Google Scholar]
- 9.Kiran G, Shyam ND, Rao J, Krishna A, Reddy BS, Prasad N. Demographics and histopathological patterns of oral squamous cell carcinoma at a tertiary level referral hospital in Hyderabad, India: A 5 year retrospective study. J Orofac Res. 2012;2:198–201. [Google Scholar]
- 10.Markopoulos AK. Current aspects on oral squamous cell carcinoma. Open Dent J. 2012;6:126–30. doi: 10.2174/1874210601206010126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dikshit R, Gupta PC, Ramasundarahettige C, Gajalakshmi V, Aleksandrowicz L, Badwe R, et al. Cancer mortality in India: A nationally representative survey. Lancet. 2012;379:1807–16. doi: 10.1016/S0140-6736(12)60358-4. [DOI] [PubMed] [Google Scholar]
- 12.Brandizzi D, Gandolfo M, Velazco ML, Cabrini RL, Lanfranchi HE. Clinical features and evolution of oral cancer: A study of 274 cases in Buenos Aires, Argentina. Med Oral Patol Oral Cir Bucal. 2008;13:E544–8. [PubMed] [Google Scholar]
- 13.New Delhi: Indian Council of Medical Research; 1992. Indian Council of Medical Research. National Cancer Registry Programme - Biennial Report (1988- 89) of the National Cancer Registry Programme. [Google Scholar]
- 14.Huber MA. A review of premalignant oral conditions. Tex Dent J. 2006;123:502–9. [PubMed] [Google Scholar]
- 15.Ikeda N, Handa Y, Khim SP, Durward C, Axéll T, Mizuno T, et al. Prevalence study of oral mucosal lesions in a selected Cambodian population. Community Dent Oral Epidemiol. 1995;23:49–54. doi: 10.1111/j.1600-0528.1995.tb00197.x. [DOI] [PubMed] [Google Scholar]
- 16.Goyal D, Goyal P, Sing HP, Verma C. Precancerous lesions of oral cavity. Oral Surg Oral Med Oral Pathol IJMDS. 2012;2:70–1. [Google Scholar]
- 17.Scott J, Cheah SB. The prevalence of oral mucosal lesions in the elderly in a surgical biopsy population: A retrospective analysis of 4042 cases. Gerodontology. 1989;8:73–8. doi: 10.1111/j.1741-2358.1989.tb00407.x. [DOI] [PubMed] [Google Scholar]
- 18.Waldron CA, Shafer WG. Leukoplakia revisited. A clinicopathologic study 3256 oral leukoplakias. Cancer. 1975;36:1386–92. doi: 10.1002/1097-0142(197510)36:4<1386::aid-cncr2820360430>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 19.Maia HC, Pinto NA, Jdos SP, de Medeiros AM, da Silveira ÉJ, Miguel MC, et al. Potentially malignant oral lesions: Clinicopathological correlations. Einstein (Sao Paulo) 2016;14:35–40. doi: 10.1590/S1679-45082016AO3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ray JG, Ganguly M, Rao BS, Mukherjee S, Mahato B, Chaudhuri K, et al. Clinico-epidemiological profile of oral potentially malignant and malignant conditions among Areca nut, tobacco and alcohol users in Eastern India: A hospital based study. J Oral Maxillofac Pathol. 2013;17:45–50. doi: 10.4103/0973-029X.110720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naga SD, Gundamaraju KK, Bujunuru SR, Navakoti P, Kantheti LC, Poosarla C. Prevalence of oral potentially malignant and malignant lesions at a tertiary level hospital in Hyderabad, India. J NTR Univ Health Sci. 2014;3:S13–6. [Google Scholar]
- 22.Kulkarni MR. Head and neck cancer burden in India. Int J Head Neck Surg. 2013;4:29–35. [Google Scholar]
- 23.Keluskar V, Kale A. An epidemiological study for evaluation of oral precancerous lesions, conditions and oral cancer among Belgaum population with tobacco habits. Biosci Biotech Res Comm. 2010;3:50–4. [Google Scholar]
- 24.Messadi DV. Diagnostic aids for detection of oral precancerous conditions. Int J Oral Sci. 2013;5:59–65. doi: 10.1038/ijos.2013.24. [DOI] [PMC free article] [PubMed] [Google Scholar]


