Abstract
Background:
Progression of primary knee osteoarthritis (OA) is often quantified by measuring structural alterations of the joint such as those in tibiofemoral joint space width (JSW) over time. Limited information is available regarding changes that occur during the onset and progression of posttraumatic OA (PTOA) that are often associated with anterior cruciate ligament (ACL) injury. Furthermore, there is a paucity of information regarding JSW changes in healthy patients, making JSW interpretation challenging during early PTOA progression.
Purpose:
To evaluate tibiofemoral JSW after ACL injury, ACL reconstruction, and rehabilitation compared with healthy, matched controls.
Study Design:
Cohort study; Level of evidence, 2.
Methods:
A total of 39 ACL-injured patients and 32 matched controls were evaluated. Injured patients were assessed at presurgical baseline and after ACL reconstruction (mean follow-up, 46 months), as were controls. Bilateral, standing, fluoroscopy-assisted, and posterior-anterior metatarsal-phalangeal view knee radiographs were obtained at each visit and JSW was measured.
Results:
The JSW differences between knees in control patients were not significantly different and did not change over time. Baseline JSW differences in the ACL group were significantly different than in controls. Three patients (7.9% of total) had an increased JSW difference, and 1 patient (2.6%) had a decreased medial JSW difference. In the lateral compartment, 6 patients (15.8%) had a decreased JSW difference. At follow-up, 2 patients in the ACL group (5%) had a decreased medial JSW difference, and 3 (7.9%) had a significantly increased difference in relation to controls. Lateral compartment analyses revealed 7 (18.4%) patients with a significantly decreased JSW difference and no patients with an increased difference compared with controls.
Conclusion:
One third of ACL-injured knees underwent significant JSW change soon after injury; consequently, evaluation of within-knee JSW changes over time in ACL-injured patients may not be appropriate with a study based on case-control analysis. The JSWs in the healthy knee of ACL-injured patients do not change over time, allowing this knee to be used as a control for the injured knee. This is important when evaluating the earliest stages of PTOA after ACL injury, when patients are asymptomatic and intervention may be most beneficial.
Keywords: posttraumatic OA, ACL, assessment, joint space width
Much of what is known regarding the progression of human idiopathic osteoarthritis (OA) is derived from studies investigating the loss of articular cartilage during the latter stages of the disease. Progression of primary OA is often quantified through the assessment of imaging-based outcomes such as conventional radiography or magnetic resonance imaging (MRI).13 It has been reported that reliable and reproducible results may be obtained when measuring tibiofemoral joint space width (JSW) using fixed-flexion or semiflexed metatarsal-phalangeal (MTP) view radiographs of the knee.§ Although measurement of JSW from fluoroscopy-assisted MTP view radiographs is not without its limitations,28,29,39 use of this technique continues to be recommended over MRI-based measures for longitudinal studies of knee OA using articular cartilage structure modification measures (such as JSW change) as the primary outcome.6,12,13,16,22
Longitudinal evaluation of OA generally relies on the assessment of disease progression after patients seek treatment for their symptoms and substantial cartilage loss and bone remodeling have occurred. The successful identification and development of pharmacological and nonpharmacological treatments, biomarkers, and potential therapeutic targets rely on the evaluation of the disease from its onset and earliest progression, before substantial articular cartilage and bone changes. Consequently, the Osteoarthritis Research Society International–Food and Drug Administration Osteoarthritis Biomarkers Working Group has recently recommended that future studies consider patients at high risk for the development of posttraumatic OA (PTOA) as an important research focus group.21 The rationale for this recommendation is that patients at risk for PTOA are able to identify a single inciting or “index” event that is known to lead to manifestation of the disease as well as the ability to monitor the earliest stages of disease onset and progression before the patient becomes symptomatic.
Complete disruption of the anterior cruciate ligament (ACL) leads to the clinical manifestation of PTOA in 10% to 90% of injured patients at 10- to 20-year follow-up,25 making otherwise healthy ACL-injured patients exceptional candidates for inclusion in PTOA studies. Although posttraumatic models have been recommended for future OA investigations,2,21 there is limited information available regarding tibiofemoral JSW changes that occur during the onset and early progression of PTOA after injury to the ACL.2,11,25,26,30–32,36 Furthermore, there is a paucity of information regarding the temporal changes in JSW that occur naturally in healthy patients, making interpretation of the changes during the earliest stages of PTOA (when the patient is asymptomatic) challenging. To utilize ACL-injured patients in PTOA investigations, we must first understand the normal temporal pattern within which JSW ranges in healthy, noninjured knees as well as side-to-side JSW differences in these patients. In addition, it is imperative that we have an appreciation for the “short-term” changes in JSW that may occur during the initial time interval from the index ACL trauma and the point in time that we gain access to the patients as study participants. Unlike primary knee OA, which affects the medial compartment of the tibiofemoral joint with a higher prevalence than the lateral compartment,14 both the medial and lateral compartments appear to be equally affected in knee PTOA.37 It is therefore important to understand changes occurring in both compartments with PTOA investigations and not focus exclusively on the medial compartment as is routinely done in primary OA studies.
Consequently, the purpose of this investigation was to evaluate longitudinal changes in tibiofemoral JSW after ACL injury, surgical reconstruction, and rehabilitation using 2 different analysis techniques (intraknee JSW change from baseline and injured minus contralateral normal knee side-to-side JSW difference). The primary aim of this investigation was to characterize JSW changes occurring within the tibiofemoral joint soon after the index injury as well as at 4-year follow-up (during the earliest stages of the PTOA process).
MATERIALS AND METHODS
Study Design and Patient Population
A longitudinal study approved by our institutional review board was used for this investigation. Thirty-nine ACL-injured patients (20 women) were enrolled, with a mean 6 standard deviation age of 28.6 ± 6 11.9 years, body mass index (BMI) of 24.9 ± 3.6, and preinjury Tegner activity score of 7.6 ± 6 1.5. The control group was composed of 32 healthy patients (18 women) recruited from the surrounding university community and were matched by sex, age, BMI, and Tegner activity level (age, 26.7 ± 6.6 years; BMI, 23.4 ± 3.3; and Tegner activity level, 6.2 ± 1.3). All patients provided informed written consent to participate before enrollment.
Entry criteria for injured patients included age between 14 and 55 years, BMI between 18.5 and 30, Tegner activity score >5, no previous joint surgeries (to any joint) or knee injections, no relevant knee injuries other than the index injury, no abnormal clinical laxity of any ligament other than the ACL, no evidence of arthritis on baseline weight-bearing posterior-anterior MTP view radiographs, no obvious varus or valgus malalignment (2000 International Knee Documentation Committee [IKDC] knee examination criteria), less than 2/3 medial or lateral meniscectomy, and grade 3A or less articular cartilage lesions of the tibiofemoral or patellofemoral joints as proposed by the International Cartilage Repair Society (ICRS).
Entry criteria for control participants were similar to injured participants with the following exceptions: no subjective report of knee pain or dysfunction as determined by the Knee Injury and Osteoarthritis Outcome Score (KOOS)35 and IKDC subjective knee evaluation,20 no history of significant joint trauma (defined as that requiring physician referral and/or more than 3 days of modified activities of daily living), no abnormal findings with a clinical knee examination (IKDC), and no abnormal findings on baseline or follow-up MRI of either knee.
Surgical Procedure and Rehabilitation
The ACL reconstructions were performed by 1 of 2 experienced sports medicine fellowship–trained orthopaedic surgeons. Thirty-five of 39 (89.7%) ACLs were reconstructed with autologous bone–patellar tendon–bone (BPTB) autografts, 3 of 39 (7.7%) were BPTB allografts, and 1 of 39 (2.6%) was reconstructed with a semitendinosus gracilis 4-strand autograft. In all cases, the graft was tensioned to re-establish the anterior-posterior laxity of the contralateral/normal knee (±1 mm) evaluated under anesthesia immediately before surgery with the KT-1000/S arthrometer (MEDmetric Corp, San Diego, California).
The ACL-injured patients underwent arthroscopic reconstruction within 6 months of their injury (mean time between index injury and surgery, 70.1 days; range, 18–155 days), and all patients participated in a standardized postsurgical rehabilitation program.4 Injured patients were assessed at baseline (within 3 weeks before surgery) and at a mean follow-up of 46 ± 9.5 months. Matched control patients also underwent baseline and follow-up evaluations at a mean of 33 ± 6.6 months. Control patients underwent baseline and follow-up 3-T MRI to elucidate existing injuries (which would have excluded them) and ensure no new injuries were incurred during the study period. The ACL-injured patients also underwent bilateral 3-T MRI at follow-up.
Radiographic Procedures and Assessment of JSW Measurement Techniques
Bilateral posterior-anterior knee radiographs were obtained on all patients during each visit using a fluoroscopy-assisted, semiflexed MTP view technique (Figure 1) with an approach that has been previously described.15 After completion of all visits, radiographs were digitized with a Umax UTA-2100XL transparency scanner (Umax Technologies Inc, Dallas, Texas), and computer-assisted evaluation of JSWs of the medial and lateral compartments was performed using a previously validated measurement technique (midpoint technique)15 and criteria (Figure 2). The JSW distance was then calculated by averaging the distance from the distal end of the femur to the “superior” tibial rim as well as to the “inferior” rim along each compartment’s center line, resulting in the “midpoint” JSW (Figure 2). The accuracy of this JSW measurement technique has been shown to be 0.13 mm.15 Intraevaluator test-retest reliability was examined before formal JSW assessment and was found to be excellent (medial compartment mean reproducibility = 0.044 mm; lateral compartment mean reproducibility = 0.043 mm). Consequently, the calculated measurement resolution of this measurement technique was 0.17 mm (0.13-mm accuracy + 0.04-mm reproducibility = 0.17 mm). The same investigator (T.W.T.) acquired all radiographs and performed all digitizations and JSW analyses.
Figure 1.
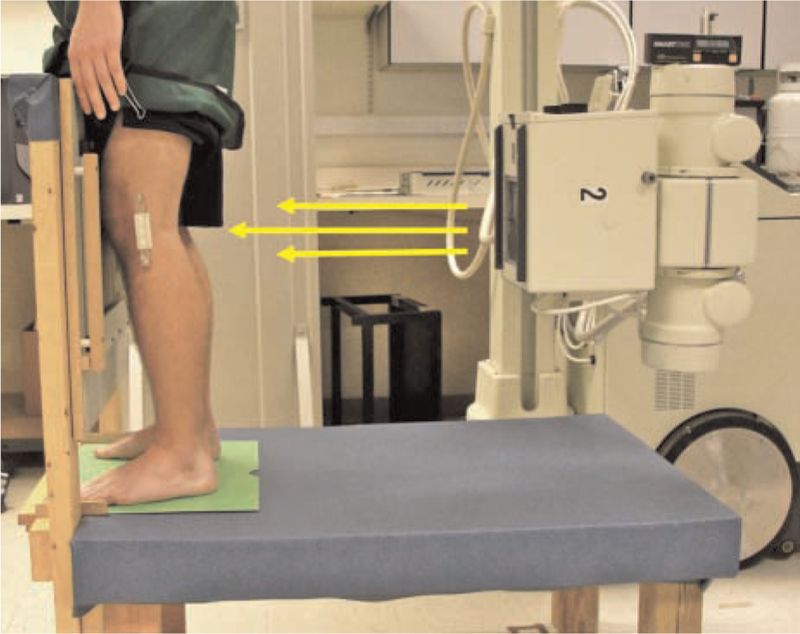
Technique for semiflexed metatarsal-phalangeal view knee radiograph.
Figure 2.

Scanned radiograph analyzed with a semiautomated technique. Calibration beads adhering to the medial aspect of the knee were used to adjust for magnification and to normalize measures between radiographs. A reference line was drawn through the midpoints of lines drawn across the tibial plateau and tibial shaft (at 1 times the distance of the tibial plateau line length down the tibia from the tibial plateau line). All additional lines were drawn in parallel to this line. The most prominent peaks of the tibial spines were identified, and medial and lateral compartment “mid-point” lines were drawn halfway between the tibial border and its respective tibial spine. Joint space width measurements were made in each compartment at the location of these midpoint lines.
Important underlying assumptions that are made when evaluating radiographic JSW in a prospective study of PTOA include the following: (1) When using a healthy, matched control group to establish a reference “normal” JSW range, it is assumed that both knees have similar JSW values and that the JSW values do not change over time. (2) When evaluating change in JSW from baseline through follow-up in ACL-injured patients, it is assumed that the JSW of the injured knee is not modified by the injury and consequently is “normal” at baseline (within the initial weeks to months after injury that are needed to gain access to patients for the purpose of research) and decreases over time in those patients with progressive PTOA. (3) When evaluating side-to-side JSW difference in ACL-injured patients (ie, injured knee minus contralateral normal knee JSW), it is assumed that the participant’s JSW in the uninjured knee remains constant over time.
To evaluate the first assumption (that the JSWs of control patients are the same bilaterally and do not change over time), between-knee JSW values in control patients were compared at baseline as well as within-knee changes in JSW from baseline to follow-up. To establish a normal tibiofemoral JSW range in healthy knees, JSW values in control patients were examined at all available time points (baseline and final follow-up), and 95% confidence intervals (CIs) were constructed for medial and lateral compartments (1.96 × measurement error). These intervals were used to determine if JSWs in the ACL group were abnormal, as an injured patient whose JSW measurement fell above or below the 95% CI was classified as “significantly different” from normal.
Evaluation of the second assumption (JSW values for ACL-injured knees are “normal” at baseline) was performed by examining between-knee JSW differences (injured minus normal knee) at baseline. The JSW difference values in the ACL group were then compared with side-to-side JSW difference values in the control group at baseline. To ascertain if the noninjured knee of ACL-injured patients underwent a response similar to that of control patients over time (assumption 3), within-knee JSW change from baseline to follow-up in the uninjured knee of ACL-injured patients was compared with within-knee JSW change values in control patients from baseline to follow-up.
Bicompartmental JSW was measured from digitized radiographs with a fixed-position (center of compartment) “midpoint” procedure for both knees of patients in the ACL and control groups using a computer-assisted, semi-automated technique with previously validated measurement criteria (Figure 2).15 Longitudinal JSW change in the medial and lateral compartments of ACL-injured patients was evaluated using 2 different techniques: (1) intraknee JSW change from baseline and (2) injured minus contralateral normal knee side-to-side JSW difference, compared with reference values and 95% CIs in control patients.
Data Analysis
The JSW refers to the cartilage thickness in a single knee’s medial or lateral compartment. Two different measures for evaluating change in JSW were considered. The first, change from baseline or intraknee JSW change, is simply the actual thickness at follow-up minus the baseline JSW. The second, the JSW difference, was determined by subtracting the JSW values of the injured knee’s medial and lateral compartments from the respective JSW value in the contralateral normal knee at the same point in time. In the control group, the side-to-side JSW difference was determined by subtracting JSW values in the left knees minus right knees for half of the patient group (randomly chosen) and JSW values in the right knees minus left knees for the remaining half to avoid a “side” bias in articular cartilage thickness as has been previously reported.1
Multilevel regression (SAS PROC MIXED, random intercept model, unstructured covariance matrix) was used for several of the analyses. Specifically, these analyses were conducted to evaluate the effect of group (case vs control) and time (baseline vs follow-up), which were performed separately for each compartment. This approach adjusts for the dependency of the repeated measurements per patient. The main advantage of multilevel regression over repeated analysis of variance (ANOVA) is that time can be included as a continuous variable (in our case, months since baseline) instead of grouping all results as being either baseline or follow-up, allowing a more sensitive evaluation of the effect of time given the range in the timing of the last follow-up. SAS version 9.2 was used for all analyses (SAS Institute, Cary, North Carolina).
Normal Ranges.
The longitudinal data of control patients were used for calculating the normal ranges. An initial set of multiple regressions was run to determine whether the measurements remained unchanged over time. The ranges are 95% CIs. The estimates of the standard deviation were based on multilevel regression models without any predictors and combined the between-patient variation as well as the within-patient variation, which would include such sources of variability as measurement error, within-patient differences between knees, as well as all factors affecting measurements taken over time.
Evaluating Assumptions Related to Using the Uninjured Knee for Calculating the Change in JSW.
The JSWs of ACL-uninjured knees were compared with the JSWs in the control group using a multilevel regression including sex, BMI, age, and time to follow-up as covariates.
Evaluating Assumptions Related to Using the Baseline JSW for Calculating the Change in JSW.
Within-patient comparisons were made using paired t tests in the ACL and control groups separately. The groups’ difference in JSW difference scores at baseline was compared using the Wilcoxon rank-sum test. A nonparametric test was preferred because the groups were found to have significantly different variances for JSW difference scores in the medial compartment (folded F test).
The statistical significance α level was set at .05 for all statistical analyses (indicating that any P value less than .05 is statistically significant).
RESULTS
Evaluation of baseline and follow-up MRI for the knees of control patients revealed no evidence of cartilage or meniscus lesions in either knee. Similarly, the healthy knees of patients in the ACL group were also found to be normal regarding MRI findings at follow-up. Of the 39 ACL-injured patients originally enrolled, 1 patient was lost to follow-up, and all subsequent statistical analyses were performed on 38 patients in the ACL group (20 women). One patient was deemed to have slightly more than 1/3 meniscectomy and was consequently graded as “2/3 removed” based on the 2000 IKDC surgical documentation criteria. No patients had more than 1/3 meniscectomy in both medial and lateral compartments combined. Fifteen patients had no tibiofemoral articular cartilage lesions (39.5% of total ACL group); 8 patients had grade 1A or B lesions (21.1%), 11 patients had grade II lesions (28.9%), and 4 patients had grade 3A lesions (10.5%) as their most significant lesion present.
Normal JSW Ranges in Control Group
The JSW measures of knees in the control group were found to remain constant and did not change over time. The follow-up evaluation was performed on average 33 months after baseline and ranged from 18 to 44 months. For comparisons to baseline, the time effect was determined to be unchanged as 0.01 mm per year (P = .86) and 20.03 mm per year (P = .79) in the medial and lateral compartments, respectively. For side-to-side JSW differences, the temporal responses were unchanged as 0.01 mm per year for the medial compartment (P = .66) and 0.02 mm in the lateral compartment (P = .27). The observed means of all the JSW measurements were found to be close to the expected values of zero (Table 1). Zero was therefore used as the means for the “normal ranges” (95% CIs), with the standard deviations estimated by random intercept multilevel regressions without any predictors.
TABLE 1.
JSW Change Over Time and Side-to-Side Difference (mm) in Control Patientsa
| Mean ± SD | Range | 95% CI | Percentage of Control Knees Outside 95% CI | |
|---|---|---|---|---|
| Difference from baseline | ||||
| Medial compartment | 0.01 ± 0.25 | –0.59 to 0.65 | ±0.49 | 5 |
| Lateral compartment | −0.03 ± 0.34 | −1.13 to 0.85 | ±0.66 | 8 |
| Difference between knees | ||||
| Medial compartment | 0.01 ± 0.42 | −1.12 to 1.11 | ±0.82b | 5 |
| Lateral compartment | 0.02 ± 0.47 | −1.41 to 0.88 | ±0.92b | 2 |
Joint space width (JSW) measurements in the control group did not vary significantly over time (all P > .25).
These 95% CI values were used to establish a “normal” JSW range; anterior cruciate ligament−reconstructed patients falling outside these limits were considered as significantly different from the normal range.
Evaluating Assumptions Related to Using the Uninjured Knee for Calculating the Change in JSW
Actual JSW data were used as the outcome for these analyses. Sex was found to be a significant covariate (P < .10; women had smaller JSWs on average) but not BMI, age, or time to follow-up (all P >.15). Descriptive statistics for knees of control patients and uninjured knees of patients in the ACL group are provided for male and female patients in Table 2. The group differences within each category were generally about 0.1 mm. A multilevel regression model including the above covariates did not find a difference between the control group and the uninjured knee of the ACL group for either compartment (medial P = .30; lateral P = .35).
TABLE 2.
Actual JSW of Healthy Knees Across All Time Points (mm)a
| Male and Female, Mean ± SD | Male, Mean (Range) | Female, Mean (Range) | |
|---|---|---|---|
| Control group: left and right knees (n = 124) | |||
| Medial compartment | 3.6 ± 0.68 | 3.9 (2.2–5.2) | 3.4 (2.2–4.9) |
| Lateral compartment | 5.4 ± 0.68 | 5.6 (4.3–6.9) | 5.3 (3.7–7.4) |
| ACL group: uninjured knees (n = 77) | |||
| Medial compartment | 3.5 ± 0.62 | 3.8 (2.9–4.9) | 3.3 (2.3–5.1) |
| Lateral compartment | 5.3 ± 0.69 | 5.5 (4.3–7.0) | 5.1 (3.9–6.5) |
Joint space width (JSW) in control patients derived from each knee at baseline and follow-up. JSW in uninjured knees derived from the normal/healthy knee of patients in the anterior cruciate ligament (ACL) group at baseline and follow-up. JSW and range values of male and female patients derived from multilevel regression analysis.
Stability of the follow-up comparisons to the baseline measurement in patients in the ACL group was assessed in the same manner as with the control group data. The last follow-up occurred later for this group (mean, 46 months; range, 25–61 months). The yearly time effects of change in the uninjured knee were 20.04 mm per year in the medial compartment and −0.04 mm per year in the lateral compartment. Both results were not significant.
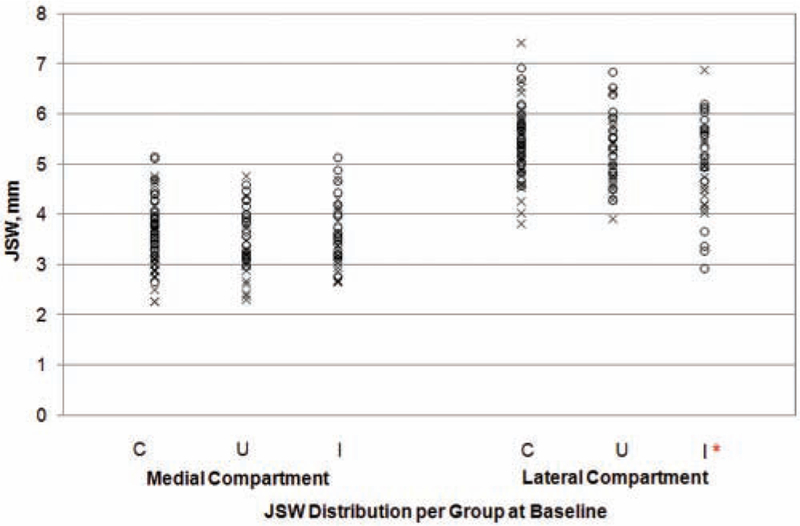
Baseline JSW Assumptions for the Evaluation of JSW Change Over Time
In patients in the ACL group, comparing within-patient JSW measurements at baseline revealed a significant mean decrease of 0.32 mm in the lateral compartment of injured knees (paired t test, P = .005), which is twice the smallest detectable difference of the JSW measurement technique (Table 3). In contrast, the mean baseline side-to-side JSW difference in the control group was −0.01 mm for the lateral compartment (P = .93). The 2 groups were found to have different side-to-side JSWs (Wilcoxon, P = .04) for the lateral compartment (Figure 3). When looking at the medial compartment, the JSW in separate knees and median JSW difference values were found to be similar in both groups (paired t test, P = .23 for ACL group and P = .99 for control group; Wilcoxon, P = .31). However, the variability was greater in the ACL group (folded F test, P = .048). This increased variability helps to explain the greater than expected number of medial measurements falling out of the 95% CI at baseline in Figures 4 and 5, as described in the next section.
TABLE 3.
Baseline Side-to-Side Differences (mm)a
| Control Group (n = 32) | ACL Group (n = 38) | |
|---|---|---|
| Medial compartment | ||
| Mean ± SD | 0 ± 0.36 | 0.10 ± 0.58 |
| Median (25%, 75%) | 0.02 (−0.20, 0.27) | 0.05 (−0.33, 0.43) |
| Lateral compartment | ||
| Mean ± SD | −0.01 ± 0.51 | −0.32b 6 0.62 |
| Median (25%, 75%) | 0.10 (−0.38, 0.29) | −0.10 (−0.50, 0.02) |
Joint space width (JSW) in the anterior cruciate ligament (ACL)–injured group calculated as injured knee minus normal knee. Half of the JSW difference in the control group was the difference between right minus left knees, while the other half was left minus right knees (determined by randomization).
The ACL-injured knees were found to have a significantly different JSW (P = .005).
Figure 3.
Baseline side-to-side joint space width (JSW) distribution for knees in the control and anterior cruciate ligament (ACL) groups. *The JSW in the lateral compartment of ACL-injured knees was significantly different from that of the contralateral knee as well as from knees in control patients at baseline. C, control; U, uninjured knee in ACL group; I, injured knee in ACL group; x, female; o, male.
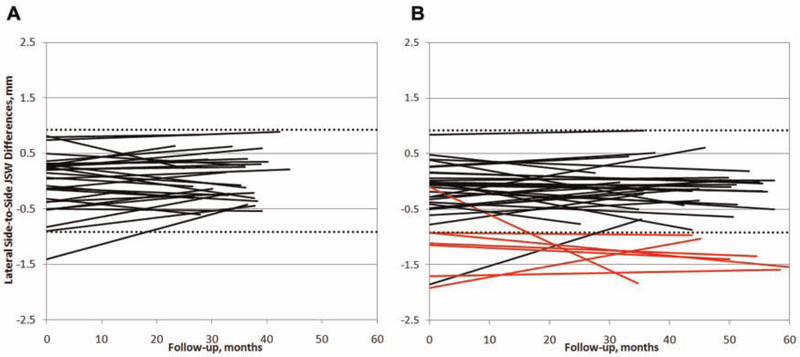
Figure 4.
Side-to-side joint space width differences in the lateral compartment for (A) control and (B) anterior cruciate ligament–reconstructed patients from baseline (0 months) through follow-up. Black lines depict values that are within the 95% confidence interval (CI) of values from control patients at final follow-up (within dotted lines), and red lines depict patients with values that are outside the 95% CI of controls at final follow-up.
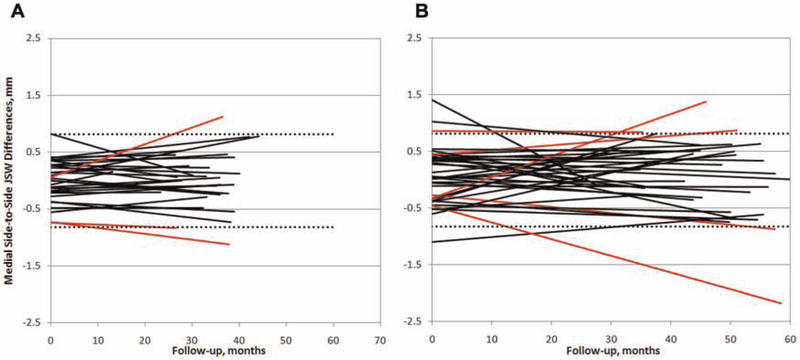
Figure 5.
Side-to-side joint space width differences in the medial compartment for (A) control and (B) anterior cruciate ligament–reconstructed patients from baseline (0 months) through follow-up. Black lines depict values that are within the 95% confidence interval (CI) of values from control patients at final follow-up (within dotted lines), and red lines depict patients with values that are outside the 95% CI of controls at final follow-up.
Patterns of Change in JSW
Twelve of the 38 (31.6%) patients in the ACL group displayed a significantly abnormal JSW difference compared with controls in either the medial or lateral compartment at baseline and/or follow-up. Analyses of side-to-side JSW difference in the lateral compartment revealed 7 patients in the ACL group who had a significantly narrowed JSW, with 6 of these patients presenting a narrowed JSW at base-line (Figure 4). Baseline analyses of the medial compartment revealed 3 patients who had an increased JSW compared with controls, 2 of whom returned to the “normal” range by follow-up and 1 patient who had a significantly narrowed JSW at baseline who also returned to the normal JSW difference range by the time of the follow-up visit. Two patients in the ACL group displayed a significantly narrower JSW difference at final follow-up, and 3 patients displayed an increase (Figure 5). No patients presented with one significantly increased and one significantly decreased compartment (no “teetering” effect within a knee was observed), and no patients displayed a combined increase or decrease in both compartments at final follow-up.
DISCUSSION
A development made with this investigation was characterization of the side-to-side JSW limits as a function of time in patients with normal knees (controls as well as the normal/healthy knee of ACL-injured patients) for both the medial and lateral compartments of the tibiofemoral joint. These data are important to consider when evaluating the initial changes of PTOA in patients who have suffered an ACL injury and have not experienced symptoms of the disease.
Before the initiation of the current study, we did not expect any injured patients to display “increased” JSW measurements. Previous studies using animal models of PTOA, reported by Calvo et al,9,10 have evaluated a “swelling” effect of articular cartilage that occurs during the earliest stages of the disease process. Distal femoral articular cartilage thickening in the medial compartment has also been reported in an MRI-based assessment of cartilage thickness after ACL disruption.17 This finding was observed over the initial 2 years after injury and was calculated as the within-knee difference from baseline. These previous findings support the current observation of significantly increased JSWs in the medial compartment at baseline and follow-up, which were noted in the present study at 4 years’ follow-up. These may be associated with the severity of the index injury event (as evidenced by bone marrow lesions and acute osteochondral fractures that are often noted on MRI after injury18) and healing response or other covariates such as abnormal joint kinematics as well as meniscus tears and articular cartilage defects that are associated with the ACL injury.
The higher percentage of JSW differences in ACL-injured knees falling outside the 95% CI (either above or below) of controls at baseline indicates that in a large proportion of patients, disruption of this ligament is associated with significant changes to the articular cartilage that appear as substantial JSW changes soon after injury and that these changes persist during healing and short-term follow-up. Bias may be introduced if baseline JSW values of the ACL-injured knee are considered “normal” and used as a reference for comparisons during healing or the progression of PTOA. Had within-knee change from baseline JSW been used as the definitive assessment to evaluate longitudinal JSW changes in patients in the ACL group in this study (in spite of the finding that the lateral JSW is not “normal” at baseline), the results would be quite different than comparisons based on side-to-side JSW difference. The within-knee “change from baseline” analyses of the lateral compartment produced 5 patients who experienced JSW narrowing and 4 who experienced an increased JSW at 4-year follow-up. In the medial compartment, 7 patients would be classified as having significant JSW narrowing, and 11 patients would appear to have experienced an increased JSW compared with controls. When examining the concurrence between the 2 JSW assessment procedures (side-to-side JSW difference and change from baseline), only 2 patients who experienced a decreased JSW in the medial compartment and 2 who experienced an increased JSW would be identified in common between the 2 techniques. Similar findings were also observed for the lateral compartment: Comparing the findings of the 2 assessment procedures resulted in a concurrence of 1 patient who experienced a decreased JSW between the 2 assessment techniques and no patients who experienced an increased JSW with both techniques (as the side-to-side JSW technique did not reveal any patients with an increased JSW in the lateral compartment). This demonstrates that using the more traditional approach of assessing JSW (within-knee change over time) may produce misleading results in studies of early knee PTOA. An example of this would be if JSW increased after injury (but before the patients’ baseline assessment) and returned to a “normal” state by the time of a longitudinal follow-up. The examiner would falsely classify this patient as having JSW narrowing (as the “increased” JSW returns to normal). Conversely, it may be that early increased JSW (from swelling of the articular cartilage, etc) is a substantial prognostic marker of the future onset and progression of PTOA. This increase in JSW could be erroneously categorized as “normal” if comparisons to the patients’ healthy limb are not made.
In the current study, JSW differences in the knees of control patients did not change significantly over time, nor did the noninjured knee of patients in the ACL group. This finding demonstrates that the JSW measured on the patients’ contralateral normal knee is a suitable control for the injured knee. Similar findings have been reported by Beattie et al,3 who evaluated minimum JSW in the medial compartment in the knees of 119 healthy participants based on sex and decade of life. Their results indicate that the JSW in the medial compartment is similar for male or female patients regardless of age (decade of life) as long as patients were free of underlying lesions. With the exception of the current study, we are not aware of any additional investigations that have evaluated longitudinal JSW changes in both medial and lateral tibiofemoral compartments in healthy patients or bilateral JSW similarity between healthy knees.
Results of the current study differ from those reported by Buckland-Wright and colleagues,7 who evaluated JSW and radiographic features in a cross-sectional study examining 19 patients after ACL rupture (verified by arthroscopic examination) at a mean follow-up interval of 34.3 months after injury. These authors found osteophyte formation in the medial compartment in 9 of 19 ACL-injured knees as well as “thickening” of the subchondral trabeculae in the medial compartment of all ACL-injured knees but no significant JSW changes in either medial or lateral compartments compared with the patients’ noninjured limb. Differences between our investigation and that of Buckland-Wright et al7 include study design (prospective cohort vs cross-sectional), JSW radiograph acquisition and analysis technique (they used fixed-flexion 53 macro-radiographs and fully automated assessment of minimum JSW), and treatment intervention (their ACL injuries were treated conservatively and were not surgically reconstructed). In addition, the severity of index injuries included in each study also differed between the investigations, as evidenced by different entry criteria. In the Buckland-Wright et al7 investigation, no meniscus or articular cartilage injuries were included. Our investigation allowed inclusion of less than 2/3 meniscectomy and articular cartilage lesions of ICRS grade 3A or less (noted at the time of arthroscopic examination); however, the majority of our patients sustained only minor injuries to their menisci and articular cartilage as was described above. It may be that concomitant injuries to the articular structures within the ACL-injured joint result in a different structural response of the involved articular cartilage. To lend additional support to this assertion, a recent review by Oiestad et al31 reported a lower prevalence of PTOA (0%−13%) at long-term follow-up after isolated ACL injuries and a substantially higher prevalence of PTOA (21%−48%) at long-term follow-up in patients who suffered combined injuries (ie, ACL and/or meniscus, articular cartilage lesions, etc). A limitation of the current study is the lack of adequate sample size required for subgroup analysis of isolated ACL injuries versus combined injuries. Very few patients with acute, isolated ACL injuries are evaluated in our clinic. The more common presentation is typically an ACL injury with combined injuries to the articular structures (menisci and/or articular cartilage), and consequently, examination of combined injuries provided a more appropriate study group for this investigation and forms the basis of a study with findings that are generalizable to a majority of those who suffer acute ACL tears during sport and activity. Additional limitations include unequal sample sizes of ACL and control groups as well as different follow-up intervals. It is unlikely that different follow-up intervals influenced our JSW measurement results, as control JSW values did not change over the study period. This finding also corroborates that of a previous study3 regarding the lack of JSW change in the medial compartment in healthy patients with no history of injury throughout later decades of life.
In conclusion, one third of ACL-injured knees may undergo substantial JSW changes soon after injury, and consequently, it may not be appropriate to use the injured knee as a reference from which changes in JSW are determined in studies of the onset and early progression of PTOA. These results are the first to demonstrate that JSWs in the medial and lateral compartments of healthy knees are similar bilaterally, that they do not change significantly over time (in bilateral knees of healthy controls or the contralateral/healthy knee of ACL-injured patients), and that the 95% CIs of normal JSW values are approximately 5 times greater than the measurement accuracy (0.17 mm) associated with the JSW difference measurement technique for the medial (±0.82 mm) and lateral (±0.92 mm) compartments, respectively. These findings provide a scientific rationale for using JSW data obtained from the normal knee of ACL-injured patients as a suitable control limb for the injured knee. This is important when evaluating the earliest stages of PTOA after ACL injury, when patients are asymptomatic and intervention may be most beneficial.
ACKNOWLEDGMENT
The authors thank the National Institutes of Health/ National Institute of Arthritis and Musculoskeletal and Skin Diseases for funding this investigation (R01 AR051477-01). They also thank Trevor Andrews, PhD, and Jay V. Gonyea, BS, RT, MR, of the University of Vermont MRI Center for Biomedical Imaging (supported in part by Department of Energy grant SC 0001753) for their assistance with the optimization and acquisition of the articular cartilage–specific MRI sequences and Mack Gardner-Morse, MSME, for his assistance with the design and creation of the JSW analysis software.
source of funding: This study was funded by National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases grant R01 AR051477-01. The University of Vermont Center for Biomedical Imaging (MRI) was supported in part by Department of Energy grant SC 001753.
Footnotes
REFERENCES
- 1.Adam C, Eckstein F, Milz S, Putz R. The distribution of cartilage thickness within the joints of the lower limb of elderly individuals. J Anat 1998;193(Pt 2):203–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson DD, Chubinskaya S, Guilak F, et al. Post-traumatic osteoarthritis: improved understanding and opportunities for early intervention. J Orthop Res 2011;29(6):802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beattie KA, Duryea J, Pui M, et al. Minimum joint space width and tibial cartilage morphology in the knees of healthy individuals: a crosssectional study. BMC Musculoskelet Disord 2008;9:119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beynnon BD, Johnson RJ, Naud S, et al. Accelerated versus nonaccelerated rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind investigation evaluating knee joint laxity using roentgen stereophotogrammetric analysis. Am J Sports Med 2011;39(12):2536–2548. [DOI] [PubMed] [Google Scholar]
- 5.Botha-Scheepers S, Kloppenburg M, Kroon HM, et al. Fixed-flexion knee radiography: the sensitivity to detect knee joint space narrowing in osteoarthritis. Osteoarthritis Cartilage 2007;15(3):350–353. [DOI] [PubMed] [Google Scholar]
- 6.Buckland-Wright C Which radiographic techniques should we use for research and clinical practice? Best Pract Res Clin Rheumatol 2006;20(1):39–55. [DOI] [PubMed] [Google Scholar]
- 7.Buckland-Wright JC, Lynch JA, Dave B. Early radiographic features in patients with anterior cruciate ligament rupture. Ann Rheum Dis 2000;59(8):641–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buckland-Wright JC, Ward RJ, Peterfy C, Mojcik CF, Leff RL. Reproducibility of the semiflexed (metatarsophalangeal) radiographic knee position and automated measurements of medial tibiofemoral joint space width in a multicenter clinical trial of knee osteoarthritis. J Rheumatol 2004;31(8):1588–1597. [PubMed] [Google Scholar]
- 9.Calvo E, Palacios I, Delgado E, et al. High-resolution MRI detects cartilage swelling at the early stages of experimental osteoarthritis. Osteoarthritis Cartilage 2001;9(5):463–472. [DOI] [PubMed] [Google Scholar]
- 10.Calvo E, Palacios I, Delgado E, et al. Histopathological correlation of cartilage swelling detected by magnetic resonance imaging in early experimental osteoarthritis. Osteoarthritis Cartilage 2004;12(11):878–886. [DOI] [PubMed] [Google Scholar]
- 11.Chu CR, Beynnon BD, Buckwalter JA, et al. Closing the gap between bench and bedside research for early arthritis therapies (EARTH): report from the AOSSM/NIH U-13 Post-Joint Injury Osteoarthritis Conference II. Am J Sports Med 2011;39(7):1569–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cline GA, Meyer JM, Stevens R, Buckland-Wright C, Peterfy C, Beary JF. Comparison of fixed flexion, fluoroscopic semi-flexed and MTP radiographic methods for obtaining the minimum medial joint space width of the knee in longitudinal osteoarthritis trials. Osteoarthritis Cartilage 2006;14 Suppl A:A32–A36. [DOI] [PubMed] [Google Scholar]
- 13.Conaghan PG, Hunter DJ, Maillefert JF, Reichmann WM, Losina E. Summary and recommendations of the OARSI FDA Osteoarthritis Assessment of Structural Change Working Group. Osteoarthritis Cartilage 2011;19(5):606–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: arthritis data from the Third National Health and Nutrition Examination Survey 1991–94. J Rheumatol 2006;33(11):2271–2279. [PubMed] [Google Scholar]
- 15.Dupuis DE, Beynnon BD, Richard MJ, Novotny JE, Skelly JM, Cooper SM. Precision and accuracy of joint space width measurements of the medial compartment of the knee using standardized MTP semi-flexed radiographs. Osteoarthritis Cartilage 2003;11(10): 716–724. [DOI] [PubMed] [Google Scholar]
- 16.Duryea J, Neumann G, Niu J, et al. Comparison of radiographic joint space width with magnetic resonance imaging cartilage morphometry: analysis of longitudinal data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 2010;62(7):932–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frobell RB. Change in cartilage thickness, posttraumatic bone marrow lesions, and joint fluid volumes after acute ACL disruption: a two-year prospective MRI study of sixty-one subjects. J Bone Joint Surg Am 2011;93(12):1096–1103. [DOI] [PubMed] [Google Scholar]
- 18.Frobell RB, Roos HP, Roos EM, et al. The acutely ACL injured knee assessed by MRI: are large volume traumatic bone marrow lesions a sign of severe compression injury? Osteoarthritis Cartilage 2008;16(7):829–836. [DOI] [PubMed] [Google Scholar]
- 19.Hellio Le Graverand MP, Mazzuca S, Duryea J, Brett A. Radiographic-based grading methods and radiographic measurement of joint space width in osteoarthritis. Radiol Clin North Am 2009;47(4):567–579. [DOI] [PubMed] [Google Scholar]
- 20.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 21.Kraus VB, Burnett B, Coindreau J, et al. Application of biomarkers in the development of drugs intended for the treatment of osteoarthritis. Osteoarthritis Cartilage 2011;19(5):515–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Graverand MP, Buck RJ, Wyman BT, et al. Change in regional cartilage morphology and joint space width in osteoarthritis participants versus healthy controls: a multicentre study using 3.0 Tesla MRI and Lyon-Schuss radiography. Ann Rheum Dis 2010;69(1):155–162. [DOI] [PubMed] [Google Scholar]
- 23.Le Graverand MP, Mazzuca S, Lassere M, et al. Assessment of the radioanatomic positioning of the osteoarthritic knee in serial radiographs: comparison of three acquisition techniques. Osteoarthritis Cartilage 2006;14 Suppl A:A37–A43. [DOI] [PubMed] [Google Scholar]
- 24.Le Graverand MP, Vignon EP, Brandt KD, et al. Head-to-head comparison of the Lyon Schuss and fixed flexion radiographic techniques: long-term reproducibility in normal knees and sensitivity to change in osteoarthritic knees. Ann Rheum Dis 2008;67(11):1562–1566. [DOI] [PubMed] [Google Scholar]
- 25.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med 2007;35(10):1756–1769. [DOI] [PubMed] [Google Scholar]
- 26.Louboutin H, Debarge R, Richou J, et al. Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. Knee 2009;16(4):239–244. [DOI] [PubMed] [Google Scholar]
- 27.Mazzuca SA, Brandt KD, Buckwalter KA. Detection of radiographic joint space narrowing in subjects with knee osteoarthritis: longitudinal comparison of the metatarsophalangeal and semiflexed anteroposterior views. Arthritis Rheum 2003;48(2):385–390. [DOI] [PubMed] [Google Scholar]
- 28.Mazzuca SA, Brandt KD, Buckwalter KA, Lane KA, Katz BP. Field test of the reproducibility of the semiflexed metatarsophalangeal view in repeated radiographic examinations of subjects with osteoarthritis of the knee. Arthritis Rheum 2002;46(1):109–113. [DOI] [PubMed] [Google Scholar]
- 29.Mazzuca SA, Brandt KD, Buckwalter KA, Lequesne M. Pitfalls in the accurate measurement of joint space narrowing in semiflexed, anteroposterior radiographic imaging of the knee. Arthritis Rheum 2004;50(8):2508–2515. [DOI] [PubMed] [Google Scholar]
- 30.Mihelic R, Jurdana H, Jotanovic Z, Madjarevic T, Tudor A. Long-term results of anterior cruciate ligament reconstruction: a comparison with non-operative treatment with a follow-up of 17–20 years. Int Orthop 2011;35(7):1093–1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10 to 15 years of follow-up. Am J Sports Med 2010;38(11):2201–2210. [DOI] [PubMed] [Google Scholar]
- 32.Oiestad BE, Holm I, Engebretsen L, Risberg MA. The association between radiographic knee osteoarthritis and knee symptoms, function and quality of life 10–15 years after anterior cruciate ligament reconstruction. Br J Sports Med 2011;45(7):583–588. [DOI] [PubMed] [Google Scholar]
- 33.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol 2003;32(3):128–132. [DOI] [PubMed] [Google Scholar]
- 34.Reichmann WM, Maillefert JF, Hunter DJ, Katz JN, Conaghan PG, Losina E. Responsiveness to change and reliability of measurement of radiographic joint space width in osteoarthritis of the knee: a systematic review. Osteoarthritis Cartilage 2011;19(5):550–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 36.Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five- to fifteen-year evaluations. Am J Sports Med 2000;28(4):446–452. [DOI] [PubMed] [Google Scholar]
- 37.Sward P, Kostogiannis I, Neuman P, Von Porat A, Boegard T, Roos H. Differences in the radiological characteristics between post-traumatic and non-traumatic knee osteoarthritis. Scand J Med Sci Sports 2010;20(5):731–739. [DOI] [PubMed] [Google Scholar]
- 38.Takahashi T, Yamanaka N, Ikeuchi M, Yamamoto H. Reproducibility of joint space width and the intermargin distance measurements in patients with medial osteoarthritis of the knee in various degrees of flexion. Skeletal Radiol 2009;38(1):37–42. [DOI] [PubMed] [Google Scholar]
- 39.Vignon E, Brandt KD, Mercier C, et al. Alignment of the medial tibial plateau affects the rate of joint space narrowing in the osteoarthritic knee. Osteoarthritis Cartilage 2010;18(11):1436–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ward RJ, Buckland-Wright JC, Wolfe F. Relationships between tibial rim alignment and joint space width measurement reproducibility in non-fluoroscopic radiographs of osteoarthritic knees. Osteoarthritis Cartilage 2005;13(11):945–952. [DOI] [PubMed] [Google Scholar]
- 41.Wolfe F, Lane NE, Buckland-Wright C. Radiographic methods in knee osteoarthritis: a further comparison of semiflexed (MTP), schuss-tunnel, and weight-bearing anteroposterior views for joint space narrowing and osteophytes. J Rheumatol 2002;29(12):2597–2601. [PubMed] [Google Scholar]